Pulmonary Pathophysiology. Histology of the lung Respiratory epithelium Connective tissue fibers,...
-
Upload
avice-mason -
Category
Documents
-
view
219 -
download
0
Transcript of Pulmonary Pathophysiology. Histology of the lung Respiratory epithelium Connective tissue fibers,...
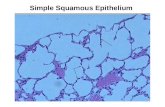
Histology of the lung
• Respiratory epithelium
• Connective tissue fibers, and cartilage:
support and maintain open air way
• Alveolar cells (type I and type II)
Function of the lung
• Gas exchange
• Protection against infection by alveolar macrophages
• Surfactant secretion: allow expansion of alveoli with air
Lung function tests
• Tidal volume (TV): it is the amount of gas
inhaled or exhaled with each resting breath.
• Residual volume (RV): it is the amount of gas
remaining in the lungs at the end of maximum
exhalation.
• Vital capacity (VC): it is the total amount of
gas that can exhaled following maximum
inhalation.
• Total lung capacity (TLC): it is the amount of
gas in the lung at the end of maximum
inhalation.
TLC = RV+ VC
Reduction of Pulmonary Function
• Inadequate blood flow to the lungs:
hypoperfusion
• Inadequate air flow to the alveoli:
hypoventilation
Noso-comial infections
• Factors that reduce airflow also compromise
particle clearance and predispose to infection.
• High rate of pneumonia in hospital patients due
in large part to impaired ventilation and
clearance.
• Restricted lung movement and ventilation
may arise due to:
• Positioning
• Constricting bandages
• Central nervous system depression
• Coma
1- Dyspnea: subjective sensation of uncomfortable
breathing, feeling “short of breath”
• Ranges from mild discomfort after exertion to
extreme difficulty breathing at rest.
• Usually caused by diffuse and extensive rather
than focal pulmonary disease.
Causes of Dyspnea :
– Airway obstruction
–Greater force needed to provide adequate
ventilation
–Wheezing sound due to air being forced
through airways narrowed due to constriction
or fluid accumulation
– Decreased compliance of lung tissue
Signs of dyspnea:
• Flaring nostrils
• Use of accessory muscles in breathing
• Retraction (pulling back) of intercostal spaces
2- Cough
• Attempt to clear the lower respiratory
passages by forceful expulsion of air
• Most common when fluid accumulates in
lower airways
Causes of Cough:
• Inflammation of lung tissue
• Increased secretion in response to mucosal irritation
• Inhalation of irritants
• Intrinsic source of mucosal disruption – such as tumor
invasion of bronchial wall
• Excessive blood hydrostatic pressure in pulmonary
capillaries
– Pulmonary edema – excess fluid passes into airways
• When cough can raise fluid into pharynx, the
cough is described as a productive cough, and
the fluid is sputum.
– Production of bloody sputum is called hemoptysis
• Not threatening, but can indicate a serious
pulmonary disease
–Tuberculosis, lung abscess, cancer, pulmonary
infarction.
• If sputum is purulent------- infection of lung or airway is
indicated.
• Cough that does not produce sputum is called a dry, or
nonproductive cough.
• Acute cough is one that resolves in 2-3 weeks from onset
of illness or treatment of underlying condition.
• Acute cough caused by upper respiratory tract (URT)
infections, allergic rhinitis, acute bronchitis, pneumonia,
congestive heart failure, pulmonary embolus, or
aspiration.
• A chronic cough is one that persists for more than
3 weeks.
• In nonsmokers, almost always due to postnasal
drainage syndrome, asthma, or gastroesophageal
reflux disease
• In smokers, chronic bronchitis is the most
common cause, although lung cancer should be
considered.
3- Cyanosis
• When blood contains a large amount of unoxygenated
hemoglobin, it has a dark red-blue color which gives skin a
characteristic bluish appearance.
• Most cases arise as a result of peripheral vasoconstriction –
result is reduced blood flow, which allows hemoglobin to give
up more of its oxygen to tissues- peripheral cyanosis.
• Best seen in nail beds
• Due to cold environment, anxiety, etc.
• Central cyanosis can be due to :
– Abnormalities of the respiratory membrane
– Mismatch between air flow and blood flow
– Expressed as a ratio of change in ventilation (V) to
perfusion (Q) : V/Q ratio
• Pulmonary thromboembolus ---- reduced blood
flow
• Airway obstruction ---- reduced ventilation
• In persons with dark skin can be seen in the whites of the
eyes and mucous membranes.
• Lack of cyanosis does not mean oxygenation is normal!!
• In adults not evident until severe hypoxemia is
present
• Clinically observable when reduced hemoglobin
levels reach 5 g/ dl.
• Severe anemia and carbon monoxide poisoning give
inadequate oxygenation of tissues without cyanosis
• Individuals with polycythemia may have cyanosis
when oxygenation is adequate.
4- Pain
• Originates in pleurae, airways or chest wall
• Inflammation of the parietal pleura causes sharp or
stabbing pain when pleura stretches during inspiration
– Usually localized to an area of the chest wall, where a
pleural friction rub can be heard
– Laughing or coughing makes pain worse
– Common with pulmonary infarction due to embolism
• Inflammation of trachea or bronchi produce a
central chest pain that is pronounced after
coughing
– Must be differentiated from cardiac pain
• High blood pressure in the pulmonary circulation
can cause pain during exercise that often
mistaken for cardiac pain (angina pectoris).
5- Clubbing
• The selective bulbous enlargement of the end of a digit
(finger or toe).
• Usually painless
• Commonly associated with diseases
that cause decreased oxygenation
– Lung cancer
– Cystic fibrosis
– Lung abscess
– Congenital heart disease
Introduction:
• Daily 10,000 liters of air - filtered..!
• Pneumonia: Inflammation of lung.
• Respiratory tract infections – commonest in medical
practice.
• Enormous morbidity & mortality.
Etiology:
• Decreased general resistance
• Virulent infection - Lobar pneumonia
• Clearing mechanism
– Decreased Cough Reflex
– Injury of the cilia and mucosa
– Low alveolar defense
– Pulmonary edema or congestion
– Obstructions
– Retention of secretions
Patterns of infections:
• Airway - Bronchitis, Bronchiectasis
• Parenchyma
– Pneumonia
• Bronchopneumonia
• Lobar pneumonia
– Lung abscess
– Tuberculosis
Pneumonia
• Pathology:
– Alveolar
• Bronchopneumonia (Streptococcus pneumoniae, Haemophilus
influenza, Staphylococcus aureus)
• Lobar (Streptococcus pneumoniae)
– Interstitial (Influenza virus, Mycoplasma pneumoniae)
• Pathogenesis
– Inhalation of air droplets
– Aspiration of infected secretions or objects
– Hematogenous spread
Bronchopneumonia
• Suppurative inflammation of lung tissue caused by
Staph, Strep, Pneumo & H. influenza
• Patchy consolidation – not limited to lobes.
• Usually bilateral
• Lower lobes common, but can occur anywhere
• Complications:
– Abscess
– Empyema
– Dissemination
Lobar Pneumonia:
• Fibrinosuppurative consolidation – whole lobe
• Rare due to antibiotic treatment.
• ~95% - Strep pneumoniae
• The course runs in four stages:
– Congestion.
– Red Hepatization.
– Gray Hepatizaiton.
– Resolution.
Lung Abscess:• Focal suppuration with necrosis of lung tissue• Organisms commonly cultured:
– Staphylococci– Streptococci– Gram-negative– Anaerobes– Frequent mixed infections
• Mechanism:– Aspiration
– Post pneumonic
– Septic embolism
– Neoplasms
• Productive Cough, fever.
• Clubbing
• Complications: Systemic spread, septicemia.
Pulmonary tuberculosis
• Caused by Mycobacterium tuberculosis.
• Transmitted through inhalation of infected droplets
• Primary
– Single granuloma within parenchyma and hilar
lymph nodes (Ghon complex).
• Infection does not progress (most common).
• Progressive primary pneumonia
• Miliary dissemination (blood stream).
Pulmonary tuberculosis
• Secondary
– Infection (mostly through reactivation) in a
previously sensitized individual.
– Pathology
• Cavitary fibrocaseous lesions
• Bronchopneumonia
• Miliary TB
Opportunistic pneumonias
• Infections that affect immunosuppressed patients
• Associated disorders:
– AIDS
– Iatrogenic
• Cancer patients
• Transplant recipients
Usual interstitial pneumonia / idiopathic pulmonary fibrosis
• Progressive fibrosing disorder of unknown cause
• Adults 30 to 50 years old
• Respiratory and heart failure (cor pulmonale) ~ 5 y