PULMONARY PATHOLOGY
description
Transcript of PULMONARY PATHOLOGY

PULMONARY PATHOLOGY
LECTURE 6 RESPIRATORY SYSTEMDEPARTMENT OF HEALTH SCIENCESDR SHAIWEEK OF NOVEMBER 10, 2013

OBJECTIVES Upper Respiratory Tract Disorders
Inflammatory conditions Neoplasms
Lung Diseases COPD Emphysema Asthma Bronchitis Neoplasms Interstitial diseases

INFLAMMATORY CONDITIONS UPPER RESPIRATORY TRACT
Rhinitis: Inflammation of nasal mucosa Acute or chronic
Acute Aetiology: infection (viral: rhinovirus, respiratory syncytial
virus, influenza, corona) or allergy (hay fever) type I hypersensitivity reaction Signs: blocks nasal airways
Chronic infection / allergy causing chronic inflammation
Signs: Macroscopic: nasal polyps, microscopic: oedematous tissue with inflammatory cells, eosinophils


SINUSITIS Inflammation of the sinuses
Acute Acute maxillary sinusitis (ethmoid & frontal less common) Aetiology: 2nd ary to rhinitis
Pathogenesis: inflammation in sinus lining, mucosa swells> stasis of maxillary sinus secretions> 2nd ary bacterial infection> purulent mucous
Chronic Chronically thick & inflammed mucosa of sinus Aetiology: acute sinusitis, cigarette smoke, industrial exposure,
polyps



NECROTIZING LESIONS A. Mucormycotic lesions
Opportunistic* fungal infections of nose from immunosuppression> fatal unless treated rapidly
B. Lymphoma Progressive ulceration & destruction of structures in nose,
sinus, form of T cell lymphoma Histologically: infiltration of lymphocytes, plasma cells,
blast cells, lymphoid cells, fatal if untreated

NEOPLASMS 1. Nasopharyngeal angiofibroma
Males, age 10 – 25 yo Mimics malignant tumour during puberty Ulceration & bleeding common
2. Plasmacytomas Malignant tumour Composed of monoclonal plasma cells* Presents as soft, haemorrhagic nasal mass
3. Olfactory neuroblastoma Rare, upper nasal cavity Haemorrhagic mass, bone destruction, metastases in
20% cases

4. Nasopharyngeal Carcinoma Squamous or anaplastic carcinoma of nasopharynx Abundant lymphoid tissue in stroma Associated with Epstein-Barr virus Small, undetected until lymph node swelling
metastases in neck Prognosis: good with radiation therapy 5 year survial: 80% if localized, 50% if advanced

THE LARYNX – INFLAMMATORY CONDITIONS A. Acute Laryngitis
Acute inflammation of larynx, infective, allergic or irritative (eg smoking)
Sequelae Resolution: without complications Spread: tracheobronchitis develops Airway obstruction: layngeal oedema eg Haemophilus
influenza
B. Croup Acute inflammation & obstruction of RESP TRACT (larynx,
trachea, bronchi) Children 6 months to 3 years

Croup aetiology: viral with 2ndary bacterial infection
Signs of obstruction: stridor (difficulty breathing), tachycardia, cyanosis, restlessness
Management: humidification, intubation or tracheostomy*

REACTIVE NODULES Polyps: common benign lesions associated
with URTI (upper respiratory tract infections) after vocal abuse> polypectomy
Singer’s Nodules: smooth, round nodules at junction between anterior 1/3 and posterior 2/3 of vocal cords
Singers, oedematous connective tissue with submucosal fibrosis covered by squamous epithelium


PAPILLOMAS Papilloma: warty papillomas on the larynx due to infection
with Human Papillomavirus (HPV 11, 16), Solitary lesions
Juvenile Papillomatosis: multiple soft, pink papillomas on vocal cords in children
Histologically: florid viral warts, persistent & recurrent, requires multiple excisions

SQAUMOUS CELL CARCINOMA OF LARYNX 2% of cancers, incidence 2 per 100,000 per year
worldwide > 40 years age, males more than females Risk factors: smoking, radiation Affected sites: supraglottic region (30%) eg epiglottis Glottic region (60%) true vocal cords, anterior and
posterior commissures Subglottic region (10%): below the true vocal cords,
above the 1st tracheal ring Macroscopically: ulcerated, gray papillary lesions Microscopically: Well differentiated, keratinizing
squamous carcinomas Spread: local, lymph, haematogenous

DISORDERS OF THE LUNGS Atelectasis
Defective expansion & collapse of lungs As a result of:
Obstruction {of large bronchial tubes leads to resorption of air from lung distal to obstruction- inhaled foreign bodies, bronchial cancer, TB, large lymph nodes, lung cancer}
Compression {compression of lung by accumulation of fluid or air in pleural cavity}
Scarring {causes contraction of parenchyma} Surfactant loss {failure of lung expansion}
Outcomes: expansion may be aided by physiotherapy and bronchoscopy mediated removal

ATELECTASIS

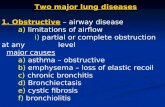
CHRONIC OBSTRUCTIVE PULMONARY DISEASE Obstructive vs restrictive lung diseases
Obstructive: obstruction to air flow within lungs, although lungs may be hyper inflated. If chronic > COPD chronic obstructive pulmonary disease
Restrictive: obstruction to EXPANSION of lungs (fibrosis or oedema) so that they can only take in a limited amount of air Lungs are under inflated, rate of airflow unaffected
Eg: pulmonary fibrosis Both obstructive & restrictive lung disease:
impairs pulmonary function

Mechanisms: by which airflow may be reduced in COPD causing 2 clinical pictures
1) increased airway resistance, by narrow airways eg bronchitis, bronchiectasis, asthma results in hypercapnea* hypoxemia*, cyanosis
2) decreased outflow pressure due to loss of elastic recoil of lungs, eg emphysema
Diagnosis & treatment: CHEST X RAY * SEE hyperinflation, flat hemi diaphragms, reduced peripheral
vascular markings, bullae And lung function tests Physiotherapy Bronchodilators Antibiotics Note: respiratory centers of some patients with COPD are
insensitive to CO2 , relying on hypoxic drive to maintain respiration. Therefore, it is dangerous to give 02 without careful observation

LOBAR ATELECTASIS

EMPHYSEMA Permanent dilatation of any part of the air spaces DISTAL to
terminal bronchiole with or without destruction of tissue, but with NO SCARRING
Common conditions, increasing with age, males more than females
Aetiology: includes smoking, atmospheric pollution, family history
Associated with chronic bronchitis, and alpha 1 anti trypsin deficiency
Pathogenesis: extra cellular proteases secreted into lung by inflammatory cells are inhibited by protease inhibitors (alpha 1 anti trypsin)
Theses inhibitors are inactive (by smoke) or absent, resulting in continued activity of proteases with destruction of lung parenchyma
Leads to loss of elastic recoil in lungs and decreased area of available gaseous exchange.


TYPES OF EMPHYSEMA Defined by location of damage in respiratory
acinus 1. Centrilobar: dilatation of respiratory
bronchioles at centre of acinus, lesions in upper lobes
2. pan lobar: dilatation of terminal alveoli, later affects bronchioles and whole acinus, affects lower lobes
3. paraseptal: air spaces at periphery of loules, adjacent to pleura
4. irregular: scarring, trapped air following lung fibrosis

CENTRILOBAR EMPHYSEMA

CLINICAL FEATURES Early stage: rapid respiratory rate enables
individuals to maintain blood oxygenation, so levels of C02 and 02 are near normal, “breathless pink puffers” not cyanoses, but on exertion, hypoxic
Later stage: reduced O2 uptake even at rest. Devline in respiratory function, cyanosis, hypercapnea, cor pulmonale (right heart failure)
CXR: Hyperinflated, trachea descended (decreased
distance

CHRONIC BRONCHITIS Cough productive of sputum on most days for 3 months of the
year for at least 2 successive years Middle aged men, associated with smoking Pathogenesis:
Irritation by cigarette smoke causes inflammation of the respiratory bronchioles (bronchiolitis) and increased mucus secretion
Hyper secretion of mucus associated with hypertrophy, and hyperplasia of bronchiole mucus secreting glands
The Reid index: gives the ratio of gland to wall thickness in the bronchus,
It is significantly increased in chronic bronchitis Bronchiolar obstruction must be extensive and widespread to give
symptoms
Clinical features: early stages: chronic cough with sputum Later stages: disease progresses to more severe, hypoxaemia,
cyanosis, hypercapnea, cor pulmonale, respiratory failure



BRONCHIAL ASTHMA Increased irritability of bronchial tree, with
narrowing of airways, may reverse spontaneously or after broncho dilator treatment.
Triggers Allergy: allergans* trigger IgE mediated type I
hypersensitivity (dust mites, food, animal danders, drugs)
Infection: respiratory tract infection can trigger bronchoconstriction
Occupational exposure: allergens, direct irritation
Drugs: beta antagonists, aspirin Irritant gases: sulphur dioxide, nitric oxide,
ozone smog Psychological stress, cold air, exercise


Asthma is associated with atopic disease, eczema, hay fever, some allergies
Asthma can be classified as
1) Extrinsic (atopic): early onset asthma, triggered by allergens, individuals have IgE levels raised, commonest type of asthma
2) Intrinsic: non atopic: late onset asthma, triggered by infection of URT. IgE levels are normal, no family history,skin testing is negative
Pathogenesis: both types, obstruction is caused by a combination of bronchospasm, oedema, mucus plugging

Phases 1: early (15 minutes): rapid onset of
bronchoconstriction, caused by histamine release from mast cell degranulation, the allergen binds to IgE antibodies on surface of mast cells
2. late (5 hours): second wave of bronchoconstriction, after initial recovery, inflammatory mediators released by mast cells cause activation of macrophages & chemotaxis of polymorphs & eosinophils into bronchial mucosa, these cells release inflammatory mediators causing 2nd wave of bronchoconstriction
3. prolonged hyperreactivity (days): exaggerated response of airway on further re exposure to allergen. There is persistent inflammation leading to bronchial wall damage.

STRUCTURAL CHANGES IN ASTHMA Immune cell infiltration: bronchial mucosa is
infiltrated with eosinophils, mast cells, lymphoid cells, macrophages
Mucosa oedema & hypersecretion of mucus: plugs airways
Hypertrophy of bronchial smooth muscle due to recurrent bronchoconstriction
Focal necrosis of airway epithelium Deposition of collagen in epithelium Sputum contains Charcot-Leyden crystals
(from eosinophil granules) & Curschmann’s spirals (mucus plugs from small airways)


CLINICAL FEATURES OF ASTHMA Mild: intermittenet* episodes of bronchospams Moderate: severe and irreversible asthma in
middle age (chronic asthma) Status asthmaticus: severe, acute distress,
does not respond to drug therapy, air entry inadequate> silent chest is ominous sign*, death from respiratory insufficiency
Signs: wheeze, barrel chest Complications: cor pulmonale, pulmonary
hypertension Management: successfully managed with b2
adrenoreceptor agonists, corticosteroids, aminophylline, anticholinergics, cromoglycate

BRONCHIECTASIS
Irreversible dilatation of bronchi
Congenital: cystic fibrosis, kartageners syndrome (bronchiectasis, dextro cardia, sinusitus)
Acquired: infection (whooping cough, pneumonia, measles) and obstruction (inhaled foreign body)
Haemophilus influenza and pseudomona aeruginosa are commonest pathogens

CYSTIC FIBROSIS Hereditary multisystem disease Lack of production of abnormally thick mucus,
primarily affecting lungs & pancreas
Commonest autosomal recessive disorder, 1/2000 newborns incidence.
1/25 Caucasians* are heterozygous* carriers of CF gene

CF PATHOGENESIS Mutated gene on chromosome 7, encodes for
protein termed “cystic fibrosis transmembrane regulator” CFTR
Commonest mutation is deletion of phenylalanine residue at position 508
Normaly this protein enables transport of chloride ions across cell membranes
In CF: a defective CFTR results in impaired chloride transport, which prevents furtehr release of sodium and water to liquefy mucus
Net result: production of EXTEREMELY THICK mucus by exocrine glands

Mucus obstructs: bronchi, intestine, pancreas
Leading to: congested lungs, meconium ileus in newborn bowel, malabsorption and failure to thrive
Respiratory issues: repeated infections (s. aureus, pseudomonas), bronchiectasis, hyper inflation of lungs from trapped air, hypoxia scarring and destruction of pulmonary vascular bed.


INFECTIONS OF THE LUNG Pneumonia is defined as the consolidation of lung
tissue caused by the formation of intra-alveolar inflammatory exudates, from a long standing lung infection
Risk factors Suppressed cough in coma Impaired mucociliary clearance (smoke, gases,
viruses, immotile cilia) Pulmonary oedema from Rt sided cardiac failure Impaired alveolar macrophages (alcohol, smoke, 02
toxicity) Immunosuppresion, drugs, instrumentation, disability,
immobility

CLASSIFICATION OF PNEUMONIA Bacterial pneumonia (80%)
Clinical: fever, short of breath, cough, sputum, coarse/crackles Bronchopneumonia
Infection on bronchi, but inflammatory exudate into alveoli, patchy consolidation of lung
Affects young or hospital acquired
Pathogenesis: patients develop retention of secretions which gravitate to dependent parts of the lungs and becomes infected
Macroscopically: bilateral, multiple areas of consolidation, bronchial mucosa is inflamed and pus around peripheral bronchi
Microscopically: acute inflammation of bronchi, inflammatory exudate in lumina and alveoli

OUTCOMES OF PNEUMONIA Resolves Bronchial damage Lung fibrosis Lung abcess formation Empyema (pus in pleural cavity) Pericarditis Death

LOBAR PNEUMONIA Uniform consolidation of part of a lobe, from
infection. 20-50 years age, poor social conditions Pneumococcus, klebsiella Pathogenesis:
Organisms enter distal air spaces without colonization of bronchi
Infection spreads rapidly into alveolar spaces Macroscopically: whole lobe becomes
consolidated and airless Microscopically: alveoli are filled with
inflammatory exudate

PULMONARY TUBERCULOSIS TB Chronic granulomatous infection of lung from
Mycobacterium Tuberculosis Leading cause of death in parts of Africa and Asia Affects older people, HIV infected, immigrant
populations (Hajj issue) Spread by:
Inhalation of M. tuberculosis droplets (commonest) Ingestion of spoiled food or milk Inoculation of skin* Transplacental (congenital)

PATHOGENESIS OF TB DESTRUCTION FROM HYPERSENSITIVITY reaction of host
directed against bacterial wall constituents Sequence 1. 0-10 days, mycobacteria start inflammatory response.
Neutrophils phagozytose organisms, but cannot destroy them, so engulfed bacteria are drained into lymph nodes
2. after 10 days: development of T cell mediated immune response (type IV hypersensitivity), to bacillary* cell wall results in cytokine release, leading to activation of macrophages> chronic inflammatory pattern, dominated by epitheliod cells which form GRANULOMAS
Central core of necrotic caseous tissue containing viable mycobacteria
Tuberculous granulomas are termed TUBERCLES

MORPHOLOGY OF TB Macroscopically: granulomas are pin sized
white/gray tubercles in tissues Microscopically: granulaomas are the
histological hallmark of TB Granuloma: central area of caseous necrosis,
surrounded by 3 layers 1st layer: activated macrophages (Langhans giant cells) Middle layer: lymphocytes Outer layer: fibroblastic tissue
Healing of granuloma is slow, with progressive fibrosis and calcification (CXR)
The central necrotic area may remain caseous and REACTIVATION results in secondary infection

PRIMARY AND SECONDARY TB Primary TB: 1st encounter with organism,
resulting in development of small parenchymal focus, large lymph drainage
Secondary infection: reactivation of previously infected indvidual, results in large localized parencyymal reaction, minimal lymph node involvement

NEOPLASTIC DISEASES OF LUNG Bronchogenic Carcinoma
Commonest cause of death from neoplasm in UK >30,000 cases per year Males more, 40-70 years peak
Risk factors Cigarette smoking (early start-increased risk), decline if smoking
stops Occupational: asbestos*, nickel, radioactive material Environmental: radon Pulmonary fibrosis
Histological types (4) 1. squamous cell carcinoma (50%) 2. small cell carcinoma (oat cell, 20%) 3. adenocarcinoma (20%) Large cell anaplastic carcinoma (10%)


LOCATION OF TUMOURS Central/hilar tumours (70%): main bronchi extending
into bronchial lumen, invading adjacent lung Peripheral tumours (30%) in peripheral alveoli, occurs
in relation to scars, extending into pleural surface
ROUTE OF SPREAD AS FOLLOWS LOCAL: central tumours invade locally through bronchial
wall into surrounding lung or alongside the bronchi Direct extension into pleura is a feature of advanced
disease LYMPHATIC TRANSCOELOMIC : tumour cells spread within pleural
cavity, causing malignant pleural effusions HAEMATOGENOUS: to brain, bone, liver, adrenal glands

HISTOLOGICAL TYPES Squamous cell carcinoma Commonest, from metaplastic squamous epithelium,
as a result of cigarette smoke Tumours arise in carina, features of bronchial
obstruction, RESECTABLE
Histologically: range from well diffeerntiated (high keratin producing) to poorly differentiated (few keratin producing cells)


Small cell (OAT CELL) carcinoma Highly malignant tumours, from bronchial endocrine
cells Type of neuro endocrine tumour Associated with ECTOPIC* hormones (acth, pth) Macroscopically: centrally located, metastases are
present at diagnosis usually Microscopically: cells are round, little cytoplasm,
nuclei resemble OAT GRAINS
Large cell anaplastic carcinoma Poorly differentiated, of squamous or adenocarcinoma
origin Lesions composed of large cells with nuclear
pleomorphism and giant cells Poor prognosis

OAT CELL CARCINOMA

Adenocarcinoma Derived from glandular cells, like mucous
goblet cells, or type II pneumocytes Slow growth Males and females Linked to passive smoking

CLINICAL FEATURES OF LUNG CANCER NO EARLY SYMPTOMS Pulmonary symptoms: cough, dyspnoea*, chest pain,
haemoptysis* Metastatic symptoms: in 70% at time of presentation
Metastases: pathological fractures, hepatomegaly, brain signs
Local spread: horner’s syndrom (cervical ganglion invasion), hoarseness voice, pericarditis
Endocrine: inappropriate ADH secretion, ectopic ACTH, hypercalcemia
Neurological: sensory and motor neuropathy, proximal myopathy, cerebellar degeneration, dermatomyositis, lambert eaton syndrome (small cell tumours)
Finger clubbing, wrist HPOA

DIAGNOSIS & MANAGEMENT Clinical features CHEST X RAY AND CT Histological confirmation by bronchoscopy and pleural
effusion cytology*
Either operable or inoperable Success in surgery depends on:
Tumour must be within lobar bronchus at least 2cm distal to carina
No direct extension to chest wall, diaphragm or percardium No involvement of great vessels of heart No malignant pleural effusion No distant metastases No nodal involvement Only 20% success after surgery


DIFFUSE INTERSTITIAL DISEASE Interstitial lung diseases are a group of NON
infectious, NON malignant disorders in which there is inflammation of alveolar walls with a thickening of interstitium between alveoli, usually with fibrosis

CHRONIC PULMONARY FIBROSIS A progressive diffuse fibrosis of lung interstitium
occurring as a result of chronic interstitial disease Aetiology
Idiopathic (eg sarcoidosis) Dust inhalation: famers lungs, bird fanciers lungs Iatrogenic: drugs (methotrexate, cyclophosphamide, radiation) Pathogenesis: neutrophil migration, enlargement and
desquamation of type I alveolar cells, accumulation of fibroblasts
Morphology Macroscopically: lung becomes a mass of cystic airspaces,
separated by collagen scarring Microscopically: cystic spaces are lined by cuboidal epithelium,
reduced lung function Signs: dyspnoea, cough, finger clubbing, restrictive lung
function tests

PNEUMOCONIOSES Group of lung diseases from chronic exposure
to inorganic dusts A) coal workers pneumoconiosis: coal
dusts B) silicosis: inhalation of quartz dust
(stone and sand) C) asbestosis: 1890s, miners, ships,
buildings D) sarcoidosis: multisystem diseases,
giant cell granulomatous inflammation in lungs, Histology: non caseating histiocytic granulomas,
cough, lung shadows on chest x ray, enlargement of hilar lymph nodes