Primary posterior oro pharyngeal wall tuberculosis
-
Upload
satish-mehta -
Category
Documents
-
view
212 -
download
0
Transcript of Primary posterior oro pharyngeal wall tuberculosis
PRIMARY POSTERIOR ORO PHARYNGEAL WALLTUBERCULOSIS
Satish Mehta, Ex-Assistant Professor,S. B. S. Mann, Professor & Head, Dept. of OtolaryngologyRam Kumar, Ex-Senior Resident, Dept. of PathologyNaresh K. Panda, Assistant Professor, Dept. of OtolaryngologyPostgraduate Institute of Medical Education and Research,Chandigarh-160 012, India
Tuberculosis involvement of pharynx is a rare entity. Whenever encountered, it isusually associated either with pulmonary tuberculosis or cervical lymphadenopathy.Isolated involvement of posterior oropharyngeal wall tuberculosis is presented in thispaper.
Introduction
Isolated tuberculous infection of pharynx israre. Trenis (1940) reported two cases ofnasopharyngeal tuberculosis with positivesputum for AFB. Savic et al (1961) could traceonly 4 cases in a review of world literature from1950 to 1960 and recorded one case of theirown in which nasopharyngeal involvementprobably developed secondary tohaematogenous spread from a pulmonaryfocus. Mair and Johannessen (1970) describeda patient with nasopharyngeal tuberculosis whohad a history of pulmonary tuberculosis andtubercular spondylitis. Raizada et al (1984)reported a patient of primary nasopharyngealtuberculosis and cervical lymphadenopathy butno pulmonary lesion. Hadad et al (1987)reported a case of tuberculosis of soft palate.We report an unusual case of oral tuberculosisinvolving the posterior oropharyngeal wall. It isthe first such case at our centre and as far aswe know, in the literature.
Case Report
A 35 year old man presented with a 10 yearhistory of persistent more throat. This hadbecome worse over the preceding 3 years andhe had noticed occasional blood stained saliva.
A tonsillectomy 3 years ago at one of theprivate hospitals produced no relief.
His general condition was good. The generaland systemic exmination was normal, howeverexamination of the throat revealed diffuse, palegranular lesion in the oropharynx (Fig, 1). Thelesion which measured 3x3 cms, wasmontender and bled on touch. There was nocervical lymphadenopathy.
The complete haemogram and urineexamination were normal. The erythrocytesedimentation rate was 62 mm for first hour. Aregular strength purified protein derivative(PPD) test was positive, with a red, induratedarea which measurd 14mm in diameter. Therewas a scar mark of the BCG vaccination on theleft arm. The chest radiographs with specialapical views, were normal.
Serological tests for Treponema pallidum wasnegative. Kveim-siltzbach test was negativeafter 6 weeks. A biopsy of the lesion revealed.multiple epitheloid cell granulomatas andforeign body giant cells (Fig. 2).A diagnosis of oral tuberculosis was made andthe patient was put on antitubercular therapy.The follow up after 13 months showed normalmucosa with some evidence of scarring.
IJO & HNS/Vol. 48, No. 3, July-Sept., 1996 230
Primary Posterior Oro Pharyngeal Wall Tuberculosis—Satish Mehta et al.
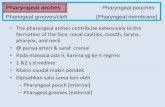
Fig.1 : Clinical photograph showing tuberculousgranuloma of the posterior oropharyngeal wall
Discussion
Non Pulmonary tuberculosis is rarelyencountered in modern practice except byspecialists in the field. Tuberculosis of pharynxis said to present as an ulcerated or lupoidlesion or as granuloma. It is almost alwayssecondary to tuberculosis elsewhere orassociated with cervical lymphadenopathy.Noone (1979).
Intact mucosa of oral cavity is resistant toinvasion by mycobacterium tuberculous. Evensaliva is supposed to have inhibitory effect ontubercle bacillus Piasesk (1987) but smallbreaches in the mucosa due to chronic irritationor inflammation may furnish favourable site forlocalisation of organisms. Other predisposingfactors like poor dental hygiene, dentalextraction or leucoplakia have also beenmentioned. Tyldesley (1978).
References
On histological section the characteristictubercle with caseation is virtuallypathognomonic; however, if caseation does notdevelop, the hard tubercle may beindistinguishable from other granulomatouslesions. Principal among these are sarcoidosis,syphilis, leprosy and nonspecific granulomatousresponse to foreign bodies, lipids and certainfungi (Robins, 1974).
The present case was unusal in many ways.The lesion was primarily in posteriororopharyngeal wall, it was granular andpainless. The long history and limitations oflesion to the mucosa of pharynx are unusualfeatures. The absence of primary lesion in thelungs or systemic manifestations and absenceof cervical lymphadenopathy did not suggesttuberculosis. All these factors emphasize theimportance for high degree of suspicion oftuberculosis in such a lesion.
Fig. 2 : Shows multiple epitheloid granulomawith langhan's giant cells (H & Ex40)
1. Trenis JW (1940) : Tuberculosis of the nasopharynx positive sputum with a roentgenoraphicallynegative chest. Am J. Med. Sci. 199: 312-318.
2. Savic D, Kosanovic M, Crejic D (1961) : Isolated tuberculosis of nasopharynx. Srp Arch CelokLek 89: 99-101.
3. Mair IWS, Johnnessen TA (1970) : Nasopharyngeal tuberculosis. Arch Otolaryngol92: 392-393.
4. Raizada RM, Behl R., Bongade V., and Khan N. (1984) : Primary Nasopharyngeal tuberculosis.Ear Nose and Throat Journal 63, 171-174.
IJO & HNS/Vol. 48, No. 3, July-Sept., 1996 P31
Primary Posterior Oro Pharyngeal Wall Tuberculosis—Satish Mehta et al.
5. Naddad NM, Zaytoun MG and Hadi U (1987) : Tuberculosis of soft palate Am unusualpresentation of oral tuberculosis. Otol—Head & Neck Surgery 97 (1) 91-92
6. Noone, P. (1979) : In Scott Brown's disease of Ear, Nose and Throat, 4th edition, Vol 1,Butterworths, London.
7. Piasesk Zeland E., Zeland, J. (1937) : On inhibitory effect of human saliva on growth oftubercle bacilli. Tubercle, 19 : 24.
8. Tyldesley, WA (1978) : Oral tuberculosis: an unusual presentation. Br. Med. J. 2: 928.9. Robbins S. I. (1974) : Pathogenic basis of disease, Saunders, Philadelphia.
PRIMARY CHRONIC MUCORMYCOSIS
K. K. Handa, Senior ResidentAru Handa, Ex ResidentNaresh Panda, Assistant ProfessorS. B. S. Mann, Professor & Head,Dept. of Otolaryngology,Postgraduate Institute of Medical Educationand Research, Chandigarh 160012, India
Mucormycosis generally presents as an acute fulminating infection which is seen indiabetics or in patients with underlying debilitating disease. Here we report a rare caseof chronic primary mucormycosis. This case merits consideration as the presentationwas chronic and indolent and also there was no underlying primary cause.
Key words: Chronic mucormycosis, paranasal sinus.
Introduction
Mucormycosis is a oppurtunistic infectioncaused by fungi belonging to Mucoracae family.They include species of Rhizopus, absidia andmucor. The recognition of the pathogenicity ofmucor began in 1815 when Meyer foundphycomycetes organism in the lung of a blueJay. The first report of human rhinocerebralmucormycosis was made by Paltauf in 1885. Hedescribed a patient with disseminated infectionof pharynx larynx, brain and lungs. Baker (1971)has identified 6 forms of mucormycosis cranialor rhinocerebral, pulmonary, gastrointestinal,disseminated cutaneous and focal forms. The
rhinocerebral form has been classicallydescribed as an acute fulminating and oftenrapidly fatal disease most often associated withuncontrolled diabetes mellitus but also seen inseverely debilitated or immunocompromisedpatients. The presentation of rhinocerebralmucormycosis is usually acute infection andthere are very few case reports of chronicpresentation of mucormycosis. Similarly primarymucormycosis i.e. mucormycosis in anotherwise healthy individual is also a relativelyrare disease. We report here an unusual case ofchronic primary mucormycosis which issignificant from the point of view of rarity of itspresentation.
!JO & HNS/Vol. 48, No. 3, July-Sept., 199fi 232