Primary Care Provider Productivity: the Effect on...
Transcript of Primary Care Provider Productivity: the Effect on...

Running head: PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 1
Primary Care Provider Productivity: the Effect on Patient Satisfaction in the
Military Health System
MAJ Jarrod McGee, Capt. Michael McLain, MAJ Marc Skinner
Army-Baylor University Graduate Program in Health and Business Administration
The views expressed in this paper are those of the authors and do not necessarily reflect the
official policy or position of the Department of the Army, Department of Defense, or the United
States Government.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 2
Abstract
1. Purpose / Hypothesis: In May 2014, Defense Secretary, Chuck Hagel, ordered a
comprehensive review of the Military Health System, which compared it to three civilian
healthcare organizations of similar size, budget, and scope. In response to the survey, the
Army Surgeon General stated the need to improve both access and patient satisfaction. The
purpose of this study is to determine the impact of provider productivity on patient
satisfaction. After an extensive literature review, we hypothesized, as provider productivity
increased, patient satisfaction would increase as well.
2. Participants: This study uses a simple random sample of all Army health care encounters.
3. Design / Methods: This study was a quasi-experimental, one-group post-test only design,
using secondary data from the Army Provider Level Satisfaction Survey tool and the Practice
Management Revenue Model. The unit of analysis was at the individual provider level. The
data was cross-sectional, and includes survey results from July 1, 2014, through December
31, 2014. We conducted an associative, multiple linear regression using SPSS v21.0.
4. Findings / Results: Provider productivity levels have no statistically significant effect on
patient satisfaction scores.
5. Conclusions: Leaders should not adjust provider productivity goals with an expectation of
affecting patient satisfaction scores.
6. Value / Relevance: Our research provides military health care leaders with the ability to
evaluate their physicians’ productivity levels and patient satisfaction scores, with confidence
that productivity levels do not affect patient satisfaction.
Keywords: patient satisfaction, productivity, military health system

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 3
Primary Care Provider Productivity: the Effect on Patient Satisfaction in the
Military Health System
In May 2014, Defense Secretary, Chuck Hagel, ordered a comprehensive review of the
Military Health System. The review compared the Military Health System to three private health
systems of similar size and scope: Kaiser Permanente; Intermountain Healthcare; and Geisinger
Health System (Kime, 2014). In October 2014, the Army Surgeon General received the results
of the Military Health System review. While the Military Health System performed on par with
the three comparable civilian institutions, there were still areas for improvement.
A few areas of particular concern to the Surgeon General are patient satisfaction and
access to care. In the Army Surgeon General’s Written Statement of Testimony to the House of
Representative’s Defense Subcommittee on Appropriations, she stated, “we will make the right
care available at the right time.” Furthermore, when discussing patient satisfaction, she stated,
“…my personal belief is that we can get better – we must be better” (Horoho, 2012, p. 6).
In his article for the Military Health System, Sauer noted the argument that increased
productivity, when measured as relative value units, comes at the expense of patient satisfaction
(2008). His study was performed at one Army Medical Treatment Facility, and he found that
lower productivity was significantly correlated with lower satisfaction (Sauer M. C., 2008). The
intended purpose of this study will examine the question of how provider productivity affects
patient satisfaction in primary care clinics in the Military Health System, with a 5% significance
level. At this stage in the research, the effects of productivity on satisfaction will be defined in
terms of monetized relative value units per full-time equivalent and patients’ overall satisfaction
with their health care providers.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 4
This study will contribute to the body of knowledge regarding the effect of productivity
on patient satisfaction, and will provide evidence to MEDCOM leadership regarding the effects
of provider productivity on patient satisfaction in a primary care setting. Furthermore, other
military health systems may be able to evaluate their respective services to determine if
increasing productivity and satisfaction, concurrently, is possible. Together, the study will allow
the service Surgeons General and other military leaders to remain competitive when compared to
their civilian counterparts, consistent with Secretary Hagel’s review of the Military Health
System.
Literature Review
This study will examine the research question of how provider productivity affects
patient satisfaction in primary care clinics in the Military Health System. Studies have reported a
positive relationship between productivity and patient satisfaction (Sauer M. C., 2008;
Glenngård, 2013). However, studies have also shown no relationship between productivity and
patient satisfaction (Mandel, et al., 2003; Wood, et al., 2009). Based on the results of the limited
studies available, we hypothesize that as provider productivity increases, so will patient
satisfaction. The remainder of this literature review will discuss the factors that affect patient
satisfaction, tied closely to the conceptual model used to frame this study, followed by the
empirical model showing how we will test the effect of provider productivity on patient
satisfaction.
Conceptual Model
In their seminal article explaining the framework for the study of access to medical care,
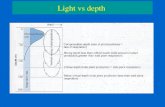
Aday and Andersen presented a conceptual model (Figure 1), which we have elected to use the
as the conceptual model for this study. According to Aday and Andersen, health policy, the

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 5
characteristics of the health delivery system, characteristics of the population at risk, and
utilization of health services all affect patient satisfaction (1974). The model includes
Figure 1. Conceptual model of the factors that affect patient satisfaction. The overall model is
adapted from Aday and Andersen (1974). *We have further modified the model to include the
construct of provider productivity, which was adapted from Bravo, Harmon, and Wood (2014).
**The characteristics of the population at risk was adapted from Andersen and Newman (1973).
***Health policy was adapted from Kim (2014).
adaptations from Kim (2014) regarding health policy. We have adapted the Aday and Andersen
conceptual model to include provider productivity. We based this decision on the unpublished

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 6
work of Bravo, Harmon, and Wood (2014, p. 8), in which they posited a conceptual model of
productivity that was driven by patient and provider demographics, pay structure, and the
environment of care.
Health policy. The construct of health policy is characterized as the starting point for
entry into the health care system, with policies and regulations all making an impact (Aday &
Andersen, 1974; Longest, 2010). For the purposes of this study, health policy is an inclusion
criterion. All patients were TRICARE beneficiaries for our dependent variable, and all providers
were Department of Defense employees (active duty military, General Schedule civilians) and
contract personnel for our primary independent variable.
Characteristics of the health delivery system. Aday and Andersen describe the
characteristics of the health delivery system as primarily organizational or structural components
of the health delivery system (1974). The unit of analysis for the characteristics of the health
delivery system is at the structural level, not the individual level (Aday & Andersen, 1974, p.
213). Tucker reported that 48.9% of the variance in patient satisfaction was explained by the
variance in the characteristics of the health delivery system (2002). The independent variables
Tucker operationalized were communication, access, and telephone access. In the only other
study we identified that investigated a characteristic of health services, Mandel and colleagues
found a significant strong and negative correlation between the number of physicians in a clinic
and patient satisfaction (2003).
Characteristics of the population at risk. The characteristics of the population at risk
is based on the work of Andersen and Newman (1973), and includes predisposing, enabling, and
illness level factors regarding an individual’s propensity to seek health care. The effect of the
characteristics of the population at risk on patient satisfaction has been well studied.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 7
Unfortunately, the majority of studies have investigated primarily predisposing variables from
the Andersen and Newman model (1973), and results are conflicting. For example, sex and age
of the patient have been reported to significantly affect patient satisfaction (Barido, Campbell-
Gauthier, Mang-Lawson, Mangelsdorff, & Finstuen, 2008; Mangelsdorff, Finstuen, Larsen, &
Weinberg, 2005; Tucker, 2002; Wood, et al., 2009). Authors have also reported that sex and age
have no effect on patient satisfaction (Jackson, Chamberlin, & Kroenke, 2001; Hochman, Itzhak,
Mankuta, & Vinker, 2008). In another study investigating patient satisfaction with nurse
practitioners as the primary care provider, marital status, and education levels, both predisposing
variables, were significantly associated with patient satisfaction (Agosta, 2009). Lin and
colleagues demonstrated a statistically significant increase in patient satisfaction when the post-
visit patient-assessed length of appointment time exceeded pre-visit patient expectations (2001).
While fewer in number, studies that have investigated the illness level variables from the
Andersen and Newman model (1973) also report conflicting results. Health status has been
reported as having a significant, positive correlation with patient satisfaction (Jackson,
Chamberlin, & Kroenke, 2001; Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005; Tucker,
2002). In fact, Jackson, Chamberlin, and Kroenke reported that the variable of unmet patient
expectations was the strongest independent correlate with patient satisfaction (2001). In contrast
to these studies, Barido and colleagues reported that health status was inversely related to patient
satisfaction (2008).
Utilization of health services. The concept of utilization of health services is meant to
measure the effect of utilization of health care services (Aday & Andersen, 1974). It is where the
structural aspects of health delivery systems and the individual aspects of the patient come
together to produce utilization (Aday & Andersen, 1974). The utilization portion of the

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 8
framework consists of four variables: type, site, purpose, and time interval. Type refers to the
“kind of service received and who provided it” (Aday & Andersen, 1974, p. 214). In the
Veteran’s Administration health care system, patients assigned to a physician-led panel were
found to be 13% less satisfied with their care (Stefos, et al., 2011). Stefos and colleagues also
reported that larger panel sizes were significantly correlated to lower patient satisfaction scores
(2011). Agosta reported that nurse practitioners working in a primary care capacity have
comparable patient satisfaction outcomes to physicians (2009). Finally, Barido and colleagues
reported increased patient satisfaction when patients were seen by their primary care provider
(2008).
Site refers to the location in which care was received. Tucker reported increased patient
satisfaction among military beneficiaries abroad, as well as increased satisfaction when the
location of the health clinic was deemed convenient (2002). Mangelsdorff and colleagues
reported that in the Military Health System, facility size was not a significant predictor of patient
satisfaction (Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005). However, in a similar study
further refining a model of patient satisfaction, patient satisfaction was higher when patients
were seen in large facilities with better access to specialty care among military beneficiaries
(Barido, Campbell-Gauthier, Mang-Lawson, Mangelsdorff, & Finstuen, 2008).
Purpose refers to the reason for the visit or acuity of the condition. Patients with a self-
reported poorer health status often report increased overall patient satisfaction with the care they
receive (Mangelsdorff & Finstuen, 2003; Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005;
Barido, Campbell-Gauthier, Mang-Lawson, Mangelsdorff, & Finstuen, 2008). Hochman and
colleagues reported a significant effect between physician communication skills and patient

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 9
satisfaction, but no effect between patient satisfaction and either the purpose of the encounter or
number of prior encounters (2008).
Patient Satisfaction. Patient satisfaction is increasingly used to measure perceived
quality of health care delivery and as an outcome measure. With an ever-increasing focus on
productivity, the twin goals of productive providers and satisfied patients can seem as diametric
goals (Glenngård, 2013; Wood, et al., 2009). Patient satisfaction is defined as an attitudinal
response towards the health care system that is optimally measured shortly after a specific
episode of care (Aday & Andersen, 1974, p. 215). Mangelsdorff and Finstuen (2003) conducted
a study of patient satisfaction in the Military Health System that established who should be
surveyed, when and where the survey should be conducted, as well as survey content. Content
included data such as patient demographics, health status, satisfaction, and familiarity with
benefits (Mangelsdorff & Finstuen, 2003). This model established that the attitude of patient
satisfaction could be predicted based on three constructs: patient demographics, beliefs about the
care itself, and situational factors (Mangelsdorff & Finstuen, 2003). Demographics included age,
health status, and sex. The care itself included patient perceptions regarding the thoroughness of
treatment, how well the treatment met patient needs, overall perceived quality of care, and
explanation of procedures and tests. Situational factors included time spent waiting for the
provider and the size of the facility. This model was subsequently refined to reflect the evolution
in the field of measuring patient satisfaction, as well as changes in health policy concerns
(Mangelsdorff & Finstuen, 2003; Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005; Barido,
Campbell-Gauthier, Mang-Lawson, Mangelsdorff, & Finstuen, 2008).
The first refinement we identified (Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005)
confirmed the earlier model, with addition of several variables into each of the three constructs

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 10
of patient demographics, beliefs about the care itself, and situational factors. For patient
demographics, this refinement confirmed health status and gender, but the authors chose to
stratify age from a continuous variable into a nominal variable of age group, as predictors of
patient satisfaction. Furthermore, beneficiary category (e.g., active duty service member, active
duty family member, retiree, retiree family member) was added to the predictive model. Branch
of service was reported as a non-significant predictor variable for patient satisfaction. Among
beliefs about the care itself, four from the original model (recommend provider, thoroughness of
treatment, how well needs were met, and overall quality of care) remained significant predictors
of patient satisfaction. Two new predictors were identified: how well health care delivery met
needs and the provider’s interest in patient (Mangelsdorff, Finstuen, Larsen, & Weinberg, 2005).
Replication of situational variables demonstrated mixed results. The variable of time spent
waiting for a provider was divided into two variables: satisfaction with the number of minutes
spent waiting for a provider, and satisfaction with the number of days between scheduling the
appointment and the actual day of the visit. Under this refined model, only number of minutes
wait past appointment time, rate number of days between appointment and day saw provider, and
reason for visit (i.e., acuity) were significant predictors of patient satisfaction (Mangelsdorff,
Finstuen, Larsen, & Weinberg, 2005).
The last refinement we identified provided further confirmation of the empirical model of
patient satisfaction (Barido, Campbell-Gauthier, Mang-Lawson, Mangelsdorff, & Finstuen,
2008). Among the patient demographic variables, age group, health status, and gender remained
significant predictors, while beneficiary status and branch of service were not significant
predictors of patient satisfaction. Barido and colleagues confirmed satisfaction with care
received, recommend provider, thoroughness of treatment, overall quality of care, how much

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 11
helped by care, advice received, attention to what patient said, and friendliness and courtesy as
significant beliefs about the care itself variable predictors of patient satisfaction (2008). For
situational variables, the authors confirmed that waiting time, size of facility, and reason for visit
were all significant predictors of patient satisfaction.
Patient satisfaction is positively correlated with time spent with patients (Feddock, et al.,
2005; Leiba, Weiss, Carroll, Benedek, & Bar-dayan, 2002; Sauer M. C., 2008; Morrell, Evans,
Morris, & Roland, 1986). Hochman and colleagues reported a significant effect between
physician communication skills and patient satisfaction, but no effect between patient
satisfaction and either the purpose of the encounter or number of prior encounters (2008). This
represents conflicting evidence, as Mangelsdorff and colleagues found the opposite, that patient
satisfaction was significantly correlated to the purpose of the encounter (2005).
The research detailed in the previous paragraphs provided the foundation for the present
patient satisfaction survey tool in use by the U.S. Army: the Army Provider Level Satisfaction
Survey. The most recent iteration of the Army Provider Level Satisfaction Survey consists of 27
questions, which collects data from the constructs of beliefs about the care itself and situational
variables. Altarum, an independent organization, maintains patient satisfaction data linked to a
specific provider by a specific appointment. Patient demographic and health care utilization data
is maintained in a separate data repository, the Military Health System Mart, and can also be
linked to a specific encounter. In spite of these rich sources of data, little is known about the
effect of provider productivity on patient satisfaction.
Provider Productivity. Productivity, as an evidence-based construct, lacks peer-
reviewed evidence regarding reliability and validity of measures used (McGlynn, 2008). There
is also a lack of consensus regarding which measure of productivity is most effective (Fetter,

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 12
Averill, Lichtenstein, & Freeman, 1984). Giuffrida and Gravelle (1999), consistent with the
McGlynn (2008) study, determined that there was no general reason to use any method versus
another when measuring productivity. Lack of uniformity in measuring productivity makes
comparison of studies of health care provider productivity challenging. One measure of
productivity in common use outside of academia is the relative value unit (Dummit, 2009).
A relative value unit is a number assigned to diagnosis and procedure codes, which ranks
the resources used to provide the service provided (Dummit, 2009). In a volume-driven health
care delivery model, the more patients a physician can evaluate, diagnose, and treat will increase
the number of relative value units, that is, increase productivity. Wood and colleagues
corroborated this effect, as they found a significant association between decreased physician time
with the patients (increased number of appointments) and increased relative value units (2009).
In a study within the Military Health System, Bravo, Harmon, and Wood posited a
conceptual model for productivity (2014). The model was tested to determine if physician pay
scale was associated with productivity and was not significant. While the Bravo, Harmon, and
Wood (2014) model has not been tested for validity, we determined it had face validity and chose
to incorporate it into the Aday and Andersen (1974) conceptual model (Figure 1). One weakness
we identified with the Bravo, Harmon, and Wood (2014) study is the model does not account for
variations in provider practice patterns. Smith and colleagues (1995) reported that physician
practice patterns (e.g., time spent with patient, and tests/radiographs in clinic) account for 84.9%
of the variance in productivity, while clinic characteristics (e.g., nurse to physician ratio, clerk to
physician ratio, and cancelled visits) explain only 8.2% of the variance in productivity (1995).
Provider Productivity and Patient Satisfaction. The majority of studies regarding the
effect of productivity on patient satisfaction have been limited in both complexity of productivity

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 13
measure and scope. Studies have reported conflicting results regarding the association between
productivity and patient satisfaction. Sauer (2008) and Glenngård (2013) reported a positive
relationship between productivity and patient satisfaction. Mandel and colleagues (2003) and
Wood and colleagues (2009) reported no relationship between productivity and patient
satisfaction. There is no clear agreement on how productivity influences patient satisfaction.
Further confounding the issue is lack of agreement on how to operationally define productivity.
Baily and Garber define productivity for health care providers as “the physical inputs
used (labor, capital, and supplies) to achieve a given level of health outcomes in treating a
specific disease” (1997, p. 146). Therefore, we chose to use a monetized relative value unit per
normalized full-time equivalent as our primary independent variable. This will directly measure
productivity while accounting for patient acuity and non-clinical provider activities.
Sauer conducted a study within the Military Health System involving a single military
treatment facility finding a statistically significant weak and direct correlation (r = 0.318, p <
0.01) between patient satisfaction and the number of encounters per provider per day (2008).
Furthermore, Sauer also reported that 16% of the variance in patient satisfaction accounts for, or
is shared with, the variance in the characteristics of health care delivery constructs of relative
value units per day and the number of provider encounters per day (2008). Glenngård (2013)
found similar results as Sauer (2008), with a direct relationship between productivity, defined as
volume of encounters, and patient satisfaction. However, there was a significant inverse
relationship between physician productivity and the enabling and illness level constructs of
social deprivation and illness, respectively (Glenngård, 2013). Finally, Wood and colleagues
concluded that there was “little or no clinically meaningful association between physician
productivity and patient satisfaction” (2009, p. 503).

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 14
Empirical Model
Our empirical model (Figure 2) shows how we are testing the effects of provider
productivity on patient satisfaction. Our dependent variable, patient satisfaction with provider, is
question four from the Army Provider Level Satisfaction Survey. The raw data for satisfaction is
a five-point Likert scale ranging from completely dissatisfied to completely satisfied. The data
was delivered from the Defense Health Agency with satisfaction scores aggregated to the
provider, with patient identifying information stripped. The data was already transformed from a
five-point Likert scale into a percentage, determined by dividing the number of surveys with
question four marked as satisfied or completely satisfied by the total number of surveys returned.
Our primary independent variable is revenue per full-time equivalent. This data is readily
available from the Practice Management Revenue Model, hosted by the U.S. Army’s Command
Management System website. Our control variables are the following: provider type (by
specialty for physicians, by work site for nurse practitioners and physician assistants), region
(U.S. Army Medical Command regions), personnel category (officer, civilian, and contractor),
facility size (medical center, medical activity, and health clinic), patient-centered medical home
status, and fellowship status. Of these, patient-centered medical home status, fellowship status,
and personnel status have not been included as control variables in previous studies. We
included patient-centered medical home status because we hypothesized that care rendered in a
patient-centered medical home would be perceived as higher quality (increased patient
satisfaction). We included fellowship status as a control variable because we hypothesized that
with the increased training required to become a fellow should result in superior outcomes, and
therefore increased patient satisfaction. We included personnel category as a control variable

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 15
because we hypothesized that due to frequent reassignments for active duty providers, patient
satisfaction would be decreased for that provider type.
Figure 2. Empirical model showing the tested effect of facility type, provider type, and our
primary independent variable of revenue per full-time equivalent on patient satisfaction with
their provider, as measured by the Army Provider Level Satisfaction Survey, question four.
*Dependent Variable. **Primary Independent Variable. ***Control Variables. PCMH = patient-
centered medical home, MTF = military treatment facility, FTE = full-time equivalent, APLSS =
Army provider level satisfaction survey.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 16
Methods
Our research design is a quasi-experimental, one-group post-test only, using secondary
data from the Army Provider Level Satisfaction Survey tool and the Practice Management
Revenue Model. The data is cross-sectional and includes survey results from July 1, 2014,
through December 31, 2014. The patient satisfaction data is aggregated to the individual
provider; therefore, our unit of analysis is at the individual provider level.
The Army Provider Level Satisfaction Survey is offered to a random sample of patients.
Military treatment facility commanders can select which providers are surveyed, but the
selection of the patients is a random process. The data for this study was a simple random
sample, including all survey results across the military health system.
Inclusion and exclusion criteria are found in Figure 3. Since our research question was specific
to primary care providers, we excluded all providers not assigned to a primary care product line.
For data quality issues, we excluded all providers with fewer than ten responses (Glenngård,
2013). The U.S. military has a unique requirement to ensure all service members are medically
fit to deploy in support of a wide variety of national interests around the globe. In order to
ensure deployment needs are met, some medical providers work in a readiness or training
capacity. Those providers may be primary care providers, but they do not function primarily to
diagnose or treat. Accordingly, we excluded all providers who were not assigned to primary care
clinics. The Practice Management Revenue Model had limited missing data regarding the
facility size where 36 providers worked, and since that was a control variable, those records were
excluded. The Practice Management Revenue Model also had missing data or error terms
returned for a small number of providers’ revenue per full-time equivalent, and because that was
our primary independent variable, those records were excluded. Finally, due to the presence of

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 17
substantial outliers in our dependent variable, we elected to exclude plus and minus three
standard deviations of productivity (Field, 2009).
Figure 3. Inclusion and exclusion criteria.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 18
A list of all of our variables is shown in Table 1. We used question four from the Army
Provider Level Satisfaction Survey, satisfaction with provider, as our dependent variable. Since
our literature review identified that no measure of productivity is preferred over another
(Giuffrida & Gravelle, 1999), we elected to use revenue per full-time equivalent as our primary
independent variable. The remaining variables were used as control variables.
We analyzed the data using IBM SPSS v21.0, with an alpha significance level of .05.
Categorical control variables were dummy coded using the following variables as the base
variable: southern region for region, medical center for facility size, active duty for personnel
category, and primary care physician for provider type. We checked the data for assumptions,
and then conducted univariate and bivariate analysis. Finally, we performed a multiple linear
regression to analyze the association between our dependent and independent variables.

Running head: PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 19
Table 1
Table of Variables Included in the Empirical Model
Note. APLSS = Army Provider Level Satisfaction Survey, PMRM = Practice Management Revenue Model
Concept Measure/
Variable
Variable
Name
Use in
Analysis
Level of
Measure
Type of
Data
Measurement
Units
Data
Source Reference
Patient
Satisfaction
Satisfaction
with Provider sat DV continuous interval percent APLSS
(Barido, Campbell-
Gauthier, Mang-
Lawson,
Mangelsdorff, &
Finstuen, 2008)
Provider
Productivity
Revenue/Full-
time
Equivalent
rev IV continuous Ratio dollars
PMRM (Glenngård, 2013)
Utilization
of Health
Services
Facility Type MTF Control categorical nominal
0 = medical
center, 1 =
medical activity,
2 = Army Health
Clinic
PMRM
(Barido, Campbell-
Gauthier, Mang-
Lawson,
Mangelsdorff, &
Finstuen, 2008;
Gates, 2008)
Utilization
of Health
Services
Provider
Type doc Control categorical nominal
0 = physician, 1
= nurse
practitioner, 2 =
physician
assistant
PMRM
(Barido, Campbell-
Gauthier, Mang-
Lawson,
Mangelsdorff, &
Finstuen, 2008)
Patient
Satisfaction
# Surveys per
Provider SurvNum Control continuous Ratio number APLSS NA

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 20
Table 1, continued
Table of Variables Included in the Empirical Model
Note. PMRM = Practice Management Revenue Model, SRMC = Southern Region Medical Command, WRMC = Western Region
Medical Command, NRMC = Northern Region Medical Command, ERMC = European Region Medical Command, PRMC = Pacific
Region Medical Command, NCR = National Capital Region, PCMH = Patient-Centered Medical Home
Concept Measure/
Variable
Variable
Name
Use in
Analysis
Level of
Measure
Type of
Data
Measurement
Units
Data
Source Reference
Utilization
of Health
Services
Region reg Contol categorical Nominal
0 = SRMC, 1 =
WRMC, 2 =
NRMC, 3 =
ERMC, 4 =
PRMC, 5 = NCR
PMRM (Tucker, 2002)
Utilization
of Health
Services
Personnel
Category PersCat Control categorical Nominal
0 = AD, 1 = GS,
2 = contractor PMRM NA
Utilization
of Health
Services
Fellowship
Status fellow Control categorical Binary 0 = no, 1 = yes PMRM NA
Utilization
of Health
Services
PCMH PCMH Control categorical Binary 0 = no, 1 = yes PMRM (Lewis & Holcomb,
2012)

Running head: PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 21
Results
Descriptive statistics for our continuous variables, including the mean, median, standard
deviation, and range, are shown in Table 2. Descriptive statistics for our categorical variables,
including frequencies and percentages, are shown in Table 3. There were no missing data points
for any variable. Mean patient satisfaction is 92%, with a standard deviation of 8%. Our
primary independent variable, provider productivity, has a mean of $351,177, with a standard
deviation of $236,071.
Table 2
Table of Central Tendencies and Dispersion for Continuous Variables
Patient Satisfaction Productivity Number of Surveys
Mean .92 $351,177 55
Median .94 $318,178 48
Std. Deviation .08 $236,071 36
Range .69 $4,095,338 252
Minimum .31 $10,422 10
Maximum 1.00 $4,105,760 262
Note: Adjusted R2 = .048, F(23, 1113) = 3.516, p < .001
The frequency distribution for the dependent variable of patient satisfaction with provider
has a negative skew, which is consistent with the literature (Glenngård, 2013; Tucker, 2002).
Our overall model is significant (see note in Table 4); however, the coefficient of multiple
determination is only .048, meaning the model accounts for just 4.8% of the variance in patient
satisfaction.
Table 4 shows the multiple linear regression results with the primary independent
variable of revenue per full-time equivalent being neither significant nor meaningful. The
following control variables have a statistically significant inverse association with patient

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 22
Table 3
Table of Frequencies for Categorical Variables
Frequency Percent
Provider Type Family Physician 309 27.2
Internist 144 12.7
Field Surgeon 20 1.8
Flight Surgeon 13 1.1
Pediatrician 152 13.4
Nurse Practitioner: Primary Care 173 15.2
Nurse Practitioner: Internist 16 1.4
Nurse Practitioner: Pediatrics 10 .9
Physician Assistant: Primary Care 259 22.8
Physician Assistant: Internist 7 .6
Physician Assistant: Flight
Surgeon 34 3.0
Total 1137 100.0
Personnel
Category
Active Duty Officer 536 47.1
General Schedule Civilian 511 44.9
Contractor 90 7.9
Total 1137 100.0
PCMH No 295 25.9
Yes 842 74.1
Total 1137 100.0
Region Southern 455 40.0
Western 289 25.4
Northern 196 17.2
European 43 3.8
Pacific 76 6.7
Capital 78 6.9
Total 1137 100.0
Facility Type MEDCEN 467 41.1
MEDDAC 495 43.5
Clinic 175 15.4
Total 1137 100.0
Fellowship Status No 1135 99.8
Yes 2 .2
Total 1137 100.0
Note: Adjusted R2 = .048, F(23, 1113) = 3.516, p < .001
PCMH = Patient-Centered Medical Home, MEDCEN = Medical Center, MEDDAC = Medical
Activity

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 23
Table 4
Inferential Statistics and Regression Results
Model
Unstandardized
Coefficients
Standardized
Coefficients
b Std. Error beta
(Constant) .929 .009
Number of Surveys .000 .000 .051
Productivity 3.88 x 10-9
.000 .012
PCMH -.012 .006 -.070
Western Region -.004 .006 -.023
Northern Region .004 .007 .022
European Region .015 .013 .037
Pacific Region .011 .009 .035
Capital Region -.006 .011 -.020
MEDDAC .006 .005 .041
Clinic .014 .008 .069
Civilian -.005 .005 -.032
Contractor -.021 .009 -.077*
Internist .012 .008 .051
Field Surgeon -.041 .017 -.072*
Flight Surgeon -.035 .021 -.050
Pediatrician .000 .007 .001
Nurse Practitioner, Primary Care -.010 .007 -.049
Nurse Practitioner, Internist .027 .019 .042
Nurse Practitioner, Pediatrics .015 .024 .019
Physician Assistant, Primary Care -.034 .006 -.187**
Physician Assistant, Internist .033 .028 .034
Physician Assistant, Flight Surgeon -.032 .014 -.071*
Fellowship Trained .022 .052 .012
Note: Adjusted R2 = .048, F(23, 1113) = 3.516, p < .001
* p < .05
** p < .001
PCMH = Patient-Centered Medical Home, MEDDAC = Medical Activity
satisfaction: contractor (personnel status), field surgeon (provider type), physician assistant-
primary care (provider type), and physician assistant-field surgeon (provider type). Interestingly,
we found that the control variable patient-centered medical home approached significance at p
= .051.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 24
Discussion
The results of the study demonstrate that while the model is significant, it is not
meaningful and only accounts for 4.8% of the shared variance of patient satisfaction. Health
care leaders and administrators should not direct efforts to alter provider productivity goals and
expect an improvement in patient satisfaction. The results of this study are both consistent, and
conflicting, with the published literature. Additionally, our results provide preliminary evidence
that the number of surveys returned does not affect patient satisfaction, that fellowship status
does not affect patient satisfaction, and that personnel status does not affect patient satisfaction.
Literature
The lack of consensus among current literature made it inevitable that our results would
both support and refute the results of other studies. Perhaps the most significant result of our
study that stands in opposition to Sauer (2008) and Glenngård (2013) is the lack of significant
association between patient satisfaction and provider productivity. Although Sauer (2008)
developed a significant model dealing with health care delivery characteristics, 16% of the
variance was attributed to patient satisfaction. These results stand in contrast to the 4.8% shared
variance of our model. Additionally, counter to Tucker (2002), region of care did not have a
significant effect on the patient satisfaction with their provider.
The lack of significant effect that provider productivity has on satisfaction within our
model is concurrent with the results of Mandel et al. (2003) and Wood et al. (2009). The data for
patient satisfaction was skewed to the left, consistent with results reported by Glenngård (2013)
and Tucker (2002). Patients had a tendency to report higher scores on the satisfaction scale than
lower.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 25
Other than Glenngård’s (2013) use of 10 surveys for inclusion/exclusion criteria, we
identified no sources that discussed the correlation between patient satisfaction and the number
of surveys that a provider receives. Our research shows that there was no significant association
between patient satisfaction with the number of surveys returned. There was also a gap in the
literature regarding the effect of personnel categories, active duty, civilian, and contract
providers, on patient satisfaction. While our results demonstrate no significant association
between fellowship trained providers and patient satisfaction, these results need to be interpreted
cautiously as there were only two providers out of 1137 that were fellowship trained.
Limitations
The primary limitation of this study is the lack of generalizability. Our research does
permit good generalizability to primary care within the military health system. Evidence based
managers should use due diligence when attempting to apply these results to health care
providers working in specialty care clinics, and to health care facilities outside of the military
health system. The study was designed to reveal associative properties and should not be used as
a predictive model to help improve future patient satisfaction outcomes. There are other factors
which could have added to the merit of the study, including patient demographic information and
information regarding the beliefs about the care itself.
Conclusions
While our model was significant, it was not meaningful. The coefficient of multiple
determination of 4.8% shows that a substantial amount of variance is unaccounted for with our
model. Provider productivity has neither a significant, nor a meaningful impact on patient
satisfaction.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 26
Recommendations
The purpose of this study was to investigate leadership directed objectives and to
discover whether productivity has a significant impact on satisfaction. As such, the results of
this research should temper leadership expectations on adjusting productivity measures for the
purpose of improving satisfaction; the evidence is growing demonstrating no significant
association between productivity and patient satisfaction. Further research is needed on the
impact of patient demographics, provider demographics, and alternative product lines on patient
satisfaction. We recommend including command climate survey results into future studies as
provider satisfaction with their current command structure would likely have an impact on their
interaction with patients and consequently the patient’s satisfaction with the provider.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 27
References
Aday, L. A., & Andersen, R. (1974). A framework for the study of access to medical care. Health
Services Research, 208-220.
Agosta, L. J. (2009). Patient satisfaction with nurse practitioner-delivered primary healthcare
services. Journal of the American Academy of Nurse Practitioners, 21, 610-617.
doi:10.1111/j.1745-7599.2009.00449.x
Andersen, R., & Newman, J. F. (1973). Societal and individual determinants of medical care
utilization in the United States. The Milbank Memorial Fund Quarterly. Health and
Society, 51(1), 95-124. doi:10.1111/j.1468-0009.2005.00428.x
Baily, M. N., & Garber, A. M. (1997). Health care productivity. Brookings Papers on Economic
Activity, 143-201.
Barido, G. T., Campbell-Gauthier, G. D., Mang-Lawson, A. M., Mangelsdorff, A. D., &
Finstuen, K. (2008). Patient Satisfaction in military medicine: model refinement and
assessment of continuity of care effects. Military Medicine, 173(7), 641-646.
Bravo, Harmon, & Wood. (2014). The effect of general schedule pay structure on physician
productivity. San Antonio: Army-Baylor University Graduate Program in Health and
Business Administration.
Dummit, L. A. (2009). The basics: relative value units. Washington, D.C.: The George
Washington University.
Feddock, C. A., Hoellein, A. R., Griffith, C. H., Wilson, J. F., Bowerman, J. L., Becker, N. S., &
Caudill, T. S. (2005). Can physicians improve patient satisfaction with long waiting
times? Evaluation & The Health Professions, 28(1), 40-52.
doi:10.1177/0163278704273084

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 28
Fetter, R. B., Averill, R. F., Lichtenstein, J. L., & Freeman, J. L. (1984). Ambulatory visit groups:
a framework for measuring productivity in ambulatory care. Health Services Research,
19(4), 415-437.
Field, A. (2009). Discovering Statistics Using SPSS, 3rd. ed. Thousand Oaks, CA: SAGE
Publications Inc.
Gates, T. M. (2008). Quantitative analysis of contributing factors affecting patient satisfaction in
family medicine service clinics at Brooke Army Medical Center. San Antonio: Army-
Baylor University Graduate Program in Health and Business Administration.
Giuffrida, A., & Gravelle, H. (1999). Measuring performance in primary care: econometric
analysis and DEA. Heslington: The University of York.
Glenngård, A. H. (2013). Productivity and patient satisfaction in primary care - conflicting or
compatible goals? Health Policy, 111, 157-165.
Hochman, O., Itzhak, B., Mankuta, D., & Vinker, S. (2008). The relation between good
communication skills on the part of the physician and patient satisfaction in a military
setting. Military Medicine, 173(9), 879-881.
Horoho, P. (2012). Written Statement of Lieutenant General Patricia D. Horoho, Testimony for
Committee on Appropriations Subcommittee on Defense. Washington, D.C. : United
States House of Representatives, Second Session, 112th Congress.
Jackson, J. L., Chamberlin, J., & Kroenke, K. (2001). Predictors of patient satisfaction. Social
Science and Medicine, 52, 609-620.
Kim, F. S. (2014, December). 201440 HCA 5411 01. Retrieved from Baylor University Canvas
data: https://baylor.instructure.com/courses/11098/files

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 29
Kime, P. (2014, Oct 23). 'We cannot accept average,' surgeons general say. Retrieved Jan 10,
2015, from The Military Times:
http://archive.militarytimes.com/article/20141023/BENEFITS06/310230040/-We-cannot-
accept-average-surgeons-general-say
Leiba, A., Weiss, Y., Carroll, J. S., Benedek, P., & Bar-dayan, Y. (2002). Waiting time is a major
predictor of patient satisfaction in a primary military clinic. Military Medicine, 167(10),
842-845.
Lewis, P. C., & Holcomb, B. (2012). A model for patient-centered army primary care. Military
Medicine, 177-183.
Lin, C.-T., Albertson, G. A., Schilling, L. M., Cyran, E. M., Anderson, S. N., Ware, L., &
Anderson, R. J. (2001). Is patients' perception of time spent with the physician a
determinant of ambulatory patient satisfaction? Archives of Internal Medicine, 161, 1437-
1442.
Longest, B. B. (2010). Health policymaking in the United States (Fifth ed.). Chicago: Health
Administration Press.
Mandel, D., Zimlichman, E., Wartenfeld, R., Vinker, S., Mimouni, F. B., & Kreiss, Y. (2003).
Primary care clinic size and patient satisfaction in a military setting. American Journal of
Medical Quality, 18(6), 251-255.
Mangelsdorff, A. D., & Finstuen, K. (2003). Patient satisfaction in military medicine: status and
an empirical test of a model. Military Medicine, 168, 744-749.
Mangelsdorff, A. D., Finstuen, K., Larsen, S. D., & Weinberg, E. J. (2005). Patient satisfaction in
military medicine: model refinement and assessment of department of defense effects.
Military Medicine, 170(4), 309-314.

PROVIDER PRODUCTIVITY AND PATIENT SATISFACTION 30
McGlynn, E. A. (2008). Identifying, categorizing, and evaluating health care efficiency
measures. Rockville, MD: Agency for Healthcare Research and Quality.
Morrell, D. C., Evans, M. E., Morris, R. W., & Roland, M. O. (1986). The "five minute"
consultation: effect of time constraint on clinical content and patient satisfaction. British
Medical Journal, 292, 870-873.
Sauer, M. (2008). Patient Satisfaction and Productivity. Fort Jackson: Unites States Army.
Sauer, M. C. (2008). Patient satisfaction and productivity. San Antonio: Army-Baylor University
Graduate Program in Health and Business Administration.
Smith, D. M., Martin, D. K., Langefeld, C. D., Miller, M. E., & Freedman, J. A. (1995). Primary
care physician productivity: the physician factor. Journal of General Internal Medicine,
10, 495-503.
Stefos, T., Burgess, J. F., Mayo-Smith, M. F., Frisbee, K. L., Harvey, H. B., Lehner, L., . . .
Moran, E. (2011). The effect of physician panel size on health care outcomes. Health
Services Management Research, 24, 96-105. doi:10.1258/hsmr.2011.011001
Tucker, J. L. (2002). The moderators of patient satisfaction. Journal of Management in Medicine,
16(1), 48-66.
Wood, G. C., Spahr, R., Gerdes, J., Daar, Z. S., Hutchinson, R., & Stewart, W. F. (2009). Patient
satisfaction and physician productivity: complementary or mutually exclusive? American
Journal of Medical Quality, 24(6), 498-504.