Present epidemiology of chronic subdural hematoma in Japan ......CLINICAL ARTICLE J Neurosurg...
Transcript of Present epidemiology of chronic subdural hematoma in Japan ......CLINICAL ARTICLE J Neurosurg...

CLINICAL ARTICLEJ Neurosurg 128:222–228, 2018
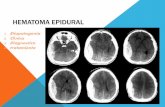
ChroniC subdural hematoma (CSDH) is an abnormal collection of encapsulated liquefied hematoma in the subdural space that may result in brain com-
pression and subsequent neurological deficits. CSDH is one of the most common neurosurgical conditions and can usually be treated with relatively simple and effective sur-gical procedures.25 However, previous studies on CSDH have been based on small sample sizes or were limited
to high-volume centers. Aging of the population may lead to epidemiological changes with respect to CSDH, and in Japan the population is aging more rapidly than anywhere else in the world. The objectives of this study were to elu-cidate the current epidemiology and changing trends for CSDH in Japan. We analyzed patient information derived from a Japanese administrative database associated with the diagnosis procedure combination (DPC) system.
ABBREVIATIONS CSDH = chronic subdural hematoma; DPC = diagnosis procedure combination; ICD-10 = International Statistical Classification of Diseases and Related Health Problems, 10th Revision; mRS = modified Rankin Scale. SUBMITTED March 11, 2016. ACCEPTED September 28, 2016.INCLUDE WHEN CITING Published online February 3, 2017; DOI: 10.3171/2016.9.JNS16623.
Present epidemiology of chronic subdural hematoma in Japan: analysis of 63,358 cases recorded in a national administrative databaseHiroyuki Toi, MD,1 Keita Kinoshita, MD,1 Satoshi Hirai, MD,1 Hiroki Takai, MD,1 Keijiro Hara, MD,1 Nobuhisa Matsushita, MD,1 Shunji Matsubara, MD,1 Makoto Otani, MD,2 Keiji Muramatsu, MD,2 Shinya Matsuda, MD,2 Kiyohide Fushimi, MD,3, and Masaaki Uno, MD1
1Department of Neurosurgery, Kawasaki Medical School, Kurashiki, Okayama; 2Department of Preventive Medicine and Community Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Fukuoka; and 3Department of Health Policy and Informatics, Tokyo Medical and Dental University, Tokyo, Japan
OBJECTIVE Aging of the population may lead to epidemiological changes with respect to chronic subdural hematoma (CSDH). The objectives of this study were to elucidate the current epidemiology and changing trends of CSDH in Japan. The authors analyzed patient information based on reports using a Japanese administrative database associated with the diagnosis procedure combination (DPC) system.METHODS This study included patients with newly diagnosed CSDH who were treated in hospitals participating in the DPC system. The authors collected data from the administrative database on the following clinical and demographic characteristics: patient age, sex, and level of consciousness on admission; treatment procedure; and outcome at dis-charge.RESULTS A total of 63,358 patients with newly diagnosed CSDH and treated in 1750 DPC participation hospitals were included in this study. Analysis according to patient age showed that the most common age range for these patients was the 9th decade of life (in their 80s). More than half of patients 70 years old or older presented with some kind of distur-bance of consciousness. Functional outcomes at discharge were good in 71.6% (modified Rankin Scale [mRS] score 0–2) of cases and poor in 28.4% (mRS score 3–6). The percentage of poor outcomes tended to be higher in elderly patients. Approximately 40% of patients 90 years old or older could not be discharged to home. The overall recurrence rate for CSDH was 13.1%.CONCLUSIONS This study shows a chronological change in the age distribution of CSDH among Japanese patients, which may be affecting the prognosis of this condition. In the aging population of contemporary Japan, patients in their 80s were affected more often than patients in other age categories, and approximately 30% of patients with CSDH re-quired some help at discharge. CSDH thus may no longer have as good a prognosis as had been thought.https://thejns.org/doi/abs/10.3171/2016.9.JNS16623KEY WORDS chronic subdural hematoma; epidemiology; Japan; national administrative database; trauma
J Neurosurg Volume 128 • January 2018222 ©AANS 2018, except where prohibited by US copyright law
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

Epidemiology of CSDH in Japan
J Neurosurg Volume 128 • January 2018 223
MethodsDPC System
The DPC system is the national administrative database of a case-mix classification system developed in Japan for acute inpatient care and payment.11 The DPC system was introduced in 2003 and has been widely adopted in Japan, and the number of patients registered in the DPC system has increased over time. Currently, 1750 acute-care hos-pitals are participating in the project, and more than 90% of acute inpatient care and payments are covered by the system in Japan.11 The DPC administrative database in-cludes the discharge summary and claim information for each patient, including principal diagnosis, comorbidities at the time of admission, and complications encountered during hospitalization.11 These data are coded using the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) code. The database also contains detailed medical information, such as all surgical procedures, medications, and devices used. Finally, the DPC database also includes the quantity and date of all care delivered on a daily basis during hos-pitalization.18 The DPC has been used previously in clini-cal studies, including analyses of aneurysmal subarach-noid hemorrhage, care practices for acute cholecystitis, and outcomes and etiologies of acute abdominal pain.5,17,18
PatientsThis study included patients with newly diagnosed
CSDH who were treated in one of the 1750 DPC participa-tion hospitals during the period from April 2010 through March 2013. These hospitals are situated throughout Japan and play leading roles in providing acute care and advanc-ing medical research. The principal diagnosis of CSDH was recorded using the ICD-10 code of S0650, indicating “traumatic chronic subdural hematoma.” There was no re-striction on patient age.
Study DesignThis retrospective study was a project of the Chugoku
and Shikoku regional meeting of the Japan Neurological Society, and the DPC system was used to identify patients for study inclusion. Treatment strategy was determined on the basis of the recommendations of the surgeon. The use of DPC data was permitted by all institutions and hos-pitals that provided detailed data. Data were collected and analyzed by a research team in the Department of Preventive Medicine and Community Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan. The research proto-col of the study was approved by the ethics committee of Tokyo Medical and Dental University, Tokyo, Japan.
Data CollectionWe collected data from the administrative database on
the following clinical characteristics of patients: age, sex, level of consciousness on admission, treatment procedure, outcomes at discharge, location to which the patients were discharged, and CSDH recurrence rate. Each patient’s outcome status was recorded using the modified Rankin
Scale (mRS), which is the most frequently used stroke out-come measure. An mRS score of 0 indicates no disability; a score of 1 or 2 indicates slight disability (i.e., the patient requires some help with daily activities but can perform basic care for him- or herself); a score of 3–5 indicates moderate disability (i.e., the patient requires some help in daily activity) to severe disability (i.e., the patient requires constant specific care or is bedridden); and a score of 6 indicates death.29
ResultsPatient Characteristics
Table 1 shows the characteristics of patients with CSDH. A total of 63,358 patients with newly diagnosed CSDH treated in one of the 1750 DPC participation hos-pitals were enrolled during the period from April 2010 through March 2013. Patient age (mean ± SD) was 76.0 ± 12 years. When patient age was stratified by decade, 4.2% of patients were in their 50s, 14.8% in their 60s, 32.9% in their 70s, 36.8% in their 80s, and 8.5% in their 90s. Analy-sis of CSDH according to patient age groups showed that patients in their 80s were the most common in the present study. Patients 70 years or older accounted for 78.2% of all cases. The study included 43,311 men (68.4%) and 20,047 women (31.6%); the frequency of male sex was more than twice that of female sex. In this study, 20,406 patients
TABLE 1. Characteristics of 63,358 patients with CSDH
Characteristic Value
No. of hospitals 1750No. of patients 63,358Mean age ± SD, yrs 76.0 ± 12Age group, yrs 50s 60s 70s 80s 90s
2690 (4.2%)9375 (14.8%)
20,847 (32.9%)23,288 (36.8%)
5414 (8.5%)Sex Male Female
43,311 (68.4%)20,047 (31.6%)
Disturbance of consciousness on admission Yes No
54.4%45.6%
Surgical treatment Burr hole Craniotomy Other
57,345 (20.3%)926 (1.5%)
5087 (8.0%)Outcome, mRS score 0 1 2 3 4 5 6
9716 (28.1%)10,218 (29.5%)
5202 (15.0%)3630 (10.5%)3902 (11.3%)1357 (3.9%)588 (1.7%)
Recurrence 7983 (12.6%)
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

H. Toi et al.
J Neurosurg Volume 128 • January 2018224
(32.2%) had hypertension and 9601 (15.2%) had diabetes mellitus. Oral medications taken at the onset of CSDH symptoms were as follows: 1660 patients (2.6%) were tak-ing aspirin; 645 (1.0%), clopidogrel; 542 (0.9%), cilostazol; 1663 (2.6%), warfarin; and 126 (0.2%), dabigatran.
Disturbance of Consciousness on AdmissionOverall, 54.4% of patients showed disturbance of con-
sciousness on admission. Stratified by age group, the per-centages were 37.5%, 50.6%, 63.4%, and 73.5% for patients under 70 years or in their 70s, 80s, or 90s, respectively. The percentage showing disturbance of consciousness dis-played a tendency to increase with age. In particular, more than half of patients 70 years of age or older presented with some kind of disturbance of consciousness.
TreatmentMost of the patients (57,345 [90.5%]) underwent single
burr hole drainage and irrigation or other burr hole pro-cedures. Only 926 patients (1.5%) underwent craniotomy (Table 1).
Treatment OutcomesPatient mRS score at discharge was 0 in 9716 cases
(28.1%), 1 in 10,218 cases (29.5%), 2 in 5202 cases (15.0%), 3 in 3630 cases (10.5%), 4 in 3902 cases (11.3%), 5 in 1357 cases (3.9%), and 6 in 588 cases (1.7%) (Table 2). Accord-ing to mRS scores dichotomized into good (mRS score 0–2) or poor (mRS score 3–6), functional outcome at dis-charge was good in 71.6% of cases and poor in 28.4%. Approximately 30% of patients with CSDH required some help at discharge. Age-specific frequencies of poor out-come at discharge were 11.7%, 20.4%, 37.4%, and 56.8% for patients under 70 years, or in their 70s, 80s, or 90s, re-spectively (Fig. 1). The frequency of poor outcome tended to increase with age.
Discharge to HomeThe age-specific rates of discharge to home were ana-
lyzed (Fig. 2). More than 90% of patients under 70 years old were discharged to home. A tendency toward lower rates was seen with increasing patient age. Approximately 30% of patients in their 80s and 40% of those in their 90s
could not be discharged to home and were transferred to a rehabilitation hospital or nursing home.
Recurrence RateRecurrence of CSDH in this study was defined as re-
operation on the ipsilateral side, and 4572 patients (7.2%) underwent reoperation for recurrent CSDH during the same hospitalization as the first operation. In addition, 3733 patients (5.9%) underwent reoperation for recurrent CSDH in a readmission. The overall recurrence rate for CSDH was 13.1% (8305/63,358 cases) (Table 2). This re-currence rate included second recurrences as well as first, counted as separate recurrence events. The association be-tween oral medication and recurrence is shown in Table 3. With respect to antithrombotic agents—namely aspi-rin, clopidogrel, cilostazol, warfarin, and dabigatran—no significant difference was identified between the group taking oral antithrombotic medications and the group not taking these agents. However, rates of discontinuation or decreases in the intake of medications in the perioperative period were unclear. Goreisan, ibudilast, and Adona were taken by 9685 patients (15.3%), 3326 patients (5.2%), and 3276 patients (5.2%), respectively. One can speculate that those drugs may have been prescribed for the purpose of preventing recurrence.
The age-specific recurrence rate of CSDH is shown in Fig. 3. A tendency toward higher recurrence rates was ini-tially seen with increasing patient age, although a decreas-ing trend was observed in patients over 80 years old.
FIG. 1. Age-specific mRS score at discharge. The percentage of poor outcomes shows a tendency to increase with age.
TABLE 2. Outcome and CSDH recurrence
Variable Value
Outcome, mRS score 0 1 2 3 4 5 6
9716 (28.1%)10,218 (29.5%)
5202 (15.0%)3630 (10.5%)3902 (11.3%)1357 (3.9%)588 (1.7%)
Recurrence Same hospitalization Readmission Total*
4572 (7.2%)3733 (5.9%)
8305/63,358 (13.1%)
* Including second recurrences as separate events.FIG. 2. Age-specific rates of discharge to home. The percentage of pa-tients discharged to home shows a tendency to decrease with age.
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

Epidemiology of CSDH in Japan
J Neurosurg Volume 128 • January 2018 225
DiscussionEtiology of CSDH in Japan
Although there have been many studies published on the topic of CSDH, this is by far the largest to date. A me-ta-analysis published in 2014 included data from 34,829 cases,1 and individual studies have included 1000 cases at the most. The present study included data from over 63,000 cases. No previous reports have included anywhere near as many cases. Moreover, the data analyzed in this study were gathered from a national database that includ-ed almost all of the CSDH cases of our country and are characterized by a very high level of accuracy.
The patients were identified for inclusion in the study using the ICD-10 code S0650, indicating “traumatic chronic subdural hematoma.” We selected a single ICD-10 code to prevent the inclusion of patients with other con-ditions, such as acute subdural hematoma and subdural hygroma. Although additional patients with CSDH might have been missed because of being assigned other ICD-10 codes, we believe that the numbers are small and the influ-ence of any such omission is minimal because of the large number of patients included in the study.
We investigated the current etiology and treatment out-comes of CSDH in Japan using a national administrative database. The annual incidence of CSDH in contemporary Japan is reported as 20.6 per 100,000 population.10 The current Japanese population is around 120 million, and it is assumed that the annual incidence of CSDH in Japan (num-ber of newly diagnosed cases) is approximately 24,000. We identified approximately 63,000 CSDH patients entered into the database for our 3-year study period, so we pre-sume that this database covers approximately 90% of the cases of CSDH that occur in Japan in a year.
In this study spanning April 2010–March 2013, analy-sis of CSDH according to patient age (in decades) showed that the 80s was the most common age range. Our results can be compared with those of several previous studies
that investigated the etiology of CSDH in Japan. In the early 1970s, Hirakawa et al. reported that CSDH patients in their 50s were the most common (Fig. 4A),8 while in 1981, Fujioka et al. reported that CSDH patients in their 60s were the most common (Fig. 4B).4 Continuing this pattern, Nioka et al. reported in 1995 that CSDH patients in their 70s were the most common (Fig. 4C).20 Data ob-tained from the present study in 2010–2013 are shown in Fig. 4D. The age of the patient population has shown increases with the aging of the overall population in Ja-pan. Although the numbers of cases in previous reports were limited, those studies, in combination with the pres-ent one, seem to reveal a change in the age distribution of CSDH among Japanese patients.
The mean age of CSDH patients has been reported as 60.4 years in India,19 64.3 years in Brazil,27 68.9 years in Switzerland,14 69.0 years in Korea,23 69.3 years in Can-ada,8 71.4 years in Germany,26 and 72.7 years in Spain.6 Analysis according to patient age (in decades) showed that patients in their 60s were the most common in Brazil.27
The male/female ratio was reported as 4.8:1 in Brazil,27 4.2:1 in Canada,9 3.4:1 in India,19 2.6:1 in Korea,23 2.4:1 in Germany,26 1.9:1 in Switzerland,14 and 1.7:1 in Spain.6 The male/female ratio was 2.2:1 in the present study. The per-centage of female CSDH patients has shown a tendency to increase over time in Japan, while the percentage of male CSDH patients has thus shown a corresponding decrease (Fig. 5). The percentage of female CSDH patients report-edly tends to increase with the aging of society,20 so this chronological change was considered to reflect that condi-tion in Japan.
CSDH Treatment OutcomesThe percentage of patients with good outcomes has
been reported as 88.3% in Brazil,27 80.0% in Korea,23 72.3% in India,19 and 72.1% in France.12 Moriyama et al. reported that 14.5% of patients had poor outcomes (mRS score 3–6) at discharge in the 1990s.16 The present study demonstrated that 71.6% of CSDH patients had good out-comes at discharge (mRS score 0–2), while 28.4% had
TABLE 3. CSDH recurrence according to oral medications taken by patients
Medication Recurrence Rate
Aspirin + −
192/1660 (11.6%)8113/61,698 (13.1%)
Clopidogrel + −
64/645 (9.9%)8241/62,713 (13.1%)
Cilostazol + −
75/542 (13.8%)8230/62,816 (13.1%)
Warfarin + −
239/1663 (14.4%)8066/61,695 (13.1%)
Dabigatran + −
16/126 (12.7%)8289/63,232 (13.1%)
+ = patients taking the specified medication; − = patients not taking the speci-fied medication.
FIG. 3. Age-specific rates of CSDH recurrence. A tendency toward a higher recurrence rate was seen with increasing patient age, although a decreasing trend was observed in patients more than 80 years old.
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

H. Toi et al.
J Neurosurg Volume 128 • January 2018226
poor outcomes (mRS score 3–6). The frequency of poor outcomes has been increasing (Fig. 6). We speculate that this result might be closely related to the increasing age of CSDH patients in contemporary Japan. Generally, CSDH is regarded as a disease with a relatively good prognosis, but in contemporary Japan, with its aging population, ap-proximately 30% of patients with CSDH required some help at discharge, and 30% of patients in their 80s and 40% of those in their 90s could not be discharged to home. It is thus difficult to say that CSDH is still associated with a good prognosis.
CSDH Recurrence RateThe CSDH recurrence rate has been reported as 11.5%–
27% in other countries,9,22,23,26 compared with 11.4%2 and 11.1%20 in the 1990s in Japan. The present study demon-strates a CSDH recurrence rate of 13.1% in the current Jap-anese population. However, this recurrence rate includes second recurrences as separate events, so the actual pro-portion of patients who suffer recurrence might be lower. In spite of the aging of the population of Japan, no signifi-cant change in recurrence rate was observed. We can spec-ulate that this result might be closely related to advances in surgical procedures and postoperative management.
FIG. 4. Changes in age distribution of CSDH in Japan. Comparison of data from studies published in 1972 (A, Hirakawa et al.8), 1981 (B, Fujioka et al.4), and 1995 (C, Nioka et al.20), and the present study (D, covering the period from 2010 to 2013) reveals an increase in the most common age range for CSDH patients in Japan.
FIG. 5. Changes in the male/female ratio of patients with CSDH from studies published in 1972, 1981, and 1995 and the present study. The percentage of female CSDH patients shows a tendency to increase, and the percentage of male CSDH patients shows a tendency to decrease, over time.
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

Epidemiology of CSDH in Japan
J Neurosurg Volume 128 • January 2018 227
A tendency toward a higher recurrence rate was seen with increasing patient age, but a decreasing trend was also observed in patients older than 80 years. The very el-derly might include a higher proportion of patients in poor condition for whom reoperation is contraindicated.
Many authors have reported on the relationship be-tween CSDH recurrence and the use of oral antithrombot-ic agents, but findings regarding an association between CSDH recurrence and antithrombotic drugs have been contradictory.3,7,13,15,21,24,28,30 In our study, CSDH recurrence tended to be less frequent among patients taking aspirin and clopidogrel and it tended to be higher in the those tak-ing goreisan, ibudilast, and Adona. Because of the DPC data features, however, it was not clear whether these med-ications were continued either during hospitalization or af-ter discharge, so we cannot draw any reliable conclusions concerning the relationship between recurrence and oral medications from our DPC data. A more careful investiga-tion of the relationship between CSDH recurrence and oral pharmacotherapies is thus warranted. Whether the out-come of recurrent CSDH is poor remains unclear because the present study was limited by the fact that analyzing the outcomes of only patients with recurrence was impossible. This issue is extremely important, and we hope to investi-gate it in a future study.
Future Prospects for CSDH in JapanThe next 2 decades will see dramatic changes and
transitions in Japanese health care needs as a result of epidemiological transitions. In Japan, the post–baby boom generation will enter their 80s in 2030. At this time, the proportion of very elderly CSDH patients is predicted to increase explosively.
ConclusionsIn summary, this study showed the presence of chrono-
logical changes in the age distribution of CSDH among Japanese patients. In contemporary Japan, with its aging population, CSDH patients were most frequently in their 80s, and approximately 30% of patients with CSDH still required some help at discharge. The prognosis for CSDH is thus currently difficult to describe as good.
References 1. Almenawer SA, Farrokhyar F, Hong C, Alhazzani W,
Manoranjan B, Yarascavitch B, et al: Chronic subdural hema-toma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg 259:449–457, 2014
2. Asano Y, Hasuo M, Takahashi I, Shimosawa S: [Recurrent cases of chronic subdural hematoma—its clinical review and serial CT findings.] No To Shinkei 44:827–831, 1992 (Jpn)
3. Baraniskin A, Steffens C, Harders A, Schmiegel W, Schro-ers R, Spangenberg P: Impact of pre-hospital antithrombotic medication on the outcome of chronic and acute subdural he-matoma. J Neurol Surg A Cent Eur Neurosurg 75:31–36, 2014
4. Fujioka S, Matsukado Y, Kaku M, Sakurama N, Nonaka N, Miura G: [CT analysis of 100 cases with chronic subdural hematoma with respect to clinical manifestation and the enlarging process of the hematoma (author’s transl).] Neurol Med Chir (Tokyo) 21:1153–1160, 1981 (Jpn)
5. Fukuhara T: Geographical analysis of aneurysmal subarach-noid hemorrhage in Japan utilizing publically-accessible DPC database. PLoS One 10:e0122467, 2015
6. Gelabert-González M, Iglesias-Pais M, García-Allut A, Martínez-Rumbo R: Chronic subdural haematoma: surgical treatment and outcome in 1000 cases. Clin Neurol Neuro-surg 107:223–229, 2005
7. Gonugunta V, Buxton N: Warfarin and chronic subdural hae-matomas. Br J Neurosurg 15:514–517, 2001
8. Hirakawa K, Hashizume K, Fuchinoue T, Takahashi H, No-mura K: Statistical analysis of chronic subdural hematoma in 309 adult cases. Neurol Med Chir (Tokyo) 12:71–83, 1972
9. Jack A, O’Kelly C, McDougall C, Findlay JM: Predicting recurrence after chronic subdural haematoma drainage. Can J Neurol Sci 42:34–39, 2015
10. Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T: [Epidemiology of chronic subdural hemato-mas.] No Shinkei Geka 39:1149–1153, 2011 (Jpn)
11. Kubo T, Fujino Y, Murata A, Ichimiya Y, Kuwabara K, Fu-jimori K, et al: Prevalence of type 2 diabetes among acute inpatients and its impact on length of hospital stay in Japan. Intern Med 50:405–411, 2011
12. Leroy HA, Aboukaïs R, Reyns N, Bourgeois P, Labreuche J, Duhamel A, et al: Predictors of functional outcomes and recurrence of chronic subdural hematomas. J Clin Neurosci 22:1895–1900, 2015
13. Lindvall P, Koskinen LO: Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci 16:1287–1290, 2009
14. MacFarlane MR, Weerakkody Y, Kathiravel Y: Chronic sub-dural haematomas are more common on the left than on the right. J Clin Neurosci 16:642–644, 2009
15. Mori K, Maeda M: Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo) 41:371–381, 2001
16. Moriyama T, Teramot S, Kondo T, Izumi J, Matsumori K, Endo M, et al: [Chronic subdural hematoma in the elderly patients—studies on incidence and outcome (part 1).] Iryo 45:14–21, 1991 (Jpn)
17. Murata A, Okamoto K, Matsuda S, Kuwabara K, Ichimiya Y, Matsuda Y, et al: The care processes for acute cholecystitis according to clinical practice guidelines based on the Japa-nese administrative database. Tohoku J Exp Med 227:237–244, 2012
18. Murata A, Okamoto K, Mayumi T, Maramatsu K, Matsuda S: Age-related differences in outcomes and etiologies of acute abdominal pain based on a national administrative database. Tohoku J Exp Med 233:9–15, 2014
19. Nayil K, Ramzan A, Sajad A, Zahoor S, Wani A, Nizami
FIG. 6. Changes in the discharge mRS score for CSDH patients. Com-parison of the rate of poor outcomes reported by Moriyama et al., in their study published in 1991, and the rate from the present study, based on data from 2010–2013, demonstrates an increase in the proportion of patients suffering poor outcomes.
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC

H. Toi et al.
J Neurosurg Volume 128 • January 2018228
F, et al: Subdural hematomas: an analysis of 1181 Kashmiri patients. World Neurosurg 77:103–110, 2012
20. Nioka H, Matsuda M, Handa J: [A review of cases of a chron-ic subdural hematoma: an analysis of findings in two age groups.] Jpn J Neurosurg (Tokyo) 4:359–363, 1995 (Jpn)
21. Okano A, Oya S, Fujisawa N, Tsuchiya T, Indo M, Nakamura T, et al: Analysis of risk factors for chronic subdural haema-toma recurrence after burr hole surgery: optimal manage-ment of patients on antiplatelet therapy. Br J Neurosurg 28:204–208, 2014
22. Phang I, Sivakumaran R, Papadopoulos MC: No association between seniority of surgeon and postoperative recurrence of chronic subdural haematoma. Ann R Coll Surg Engl 97:584–588, 2015
23. Ro HW, Park SK, Jang DK, Yoon WS, Jang KS, Han YM: Preoperative predictive factors for surgical and functional outcomes in chronic subdural hematoma. Acta Neurochir (Wien) 158:135–139, 2016
24. Rust T, Kiemer N, Erasmus A: Chronic subdural haematomas and anticoagulation or anti-thrombotic therapy. J Clin Neu-rosci 13:823–827, 2006
25. Santarius T, Kirkpatrick PJ, Kolias AG, Hutchinson PJ: Working toward rational and evidence-based treatment of chronic subdural hematoma. Clin Neurosurg 57:112–122, 2010
26. Schwarz F, Loos F, Dünisch P, Sakr Y, Safatli DA, Kalff R, et al: Risk factors for reoperation after initial burr hole trephi-nation in chronic subdural hematomas. Clin Neurol Neuro-surg 138:66–71, 2015
27. Sousa EB, Brandão LFS, Tavares CB, Borges IBC, Freire Neto NG, Kessler IM: Epidemiological characteristics of 778 patients who underwent surgical drainage of chronic subdu-ral hematomas in Brasília, Brazil. BMC Surg 13:5, 2013
28. Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M,
Yamagata S: Independent predictors for recurrence of chron-ic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery 63:1125–1129, 2008
29. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J: Interobserver agreement for the assessment of handi-cap in stroke patients. Stroke 19:604–607, 1988
30. Wada M, Yamakami I, Higuchi Y, Tanaka M, Suda S, Ono J, et al: Influence of antiplatelet therapy on postoperative recurrence of chronic subdural hematoma: a multicenter retrospective study in 719 patients. Clin Neurol Neurosurg 120:49–54, 2014
DisclosuresThe authors report no conflict of interest concerning the materi-als or methods used in this study or the findings specified in this paper.
Author ContributionsConception and design: Toi. Acquisition of data: Kinoshita, Hirai, Takai, Hara, Matsushita, Matsubara, Otani, Muramatsu, Matsuda, Fushimi. Analysis and interpretation of data: Toi, Muramatsu. Drafting the article: Toi. Critically revising the article: Toi. Approved the final version of the manuscript on behalf of all authors: Toi. Statistical analysis: Toi. Administra-tive/technical/material support: Otani, Matsuda, Fushimi. Study supervision: Uno.
CorrespondenceHiroyuki Toi, Department of Neurosurgery, Kawasaki Medical School, 577 Matsushima, Kurashiki, Okayama 701-0192, Japan. email: [email protected].
Unauthenticated | Downloaded 07/25/21 08:30 PM UTC