Preferred Drug List (Formulary) - corporate · Generic Drugs (Tier 1) n Copays for generic drugs...
Transcript of Preferred Drug List (Formulary) - corporate · Generic Drugs (Tier 1) n Copays for generic drugs...

Generic Drugs (Tier 1) n �Copays�for�generic�drugs�are�the�lowest.
n �Most�generic�drugs�are�on�the�preferred�drug�list�and�available�at�the�lowest�copay.
Preferred Brand Name Drugs (Tier 2)
n �Copays�for�preferred�brand�name�drugs�are�higher�than�generic�drugs.
n �When�a�generic�version�of�a�preferred�brand�name�drug�becomes�available,�the�brand�name�version�moves�from�Tier�2�to�Tier�3�(non‑preferred�brand�name�drugs).
Non-Preferred Brand Name Drugs (Tier 3)*
*Non-preferred brand name drugs are not part of the preferred drug list but are covered at the highest copay.
n �Copays�for�non‑preferred�brand�name�drugs�are�the�highest.
n �If�your�brand�name�drug�has�a�generic�equivalent,�the�brand�name�drug�will�not�be�on�the�preferred�drug�list�and�will�be�a�Tier�3�drug.
n �You�will�pay�the�lowest�copay�(Tier�1)�if�you�choose�the�generic�version�of�a�drug�and�the�highest�copay�if�you�choose�the�brand�name�(Tier�3)�version�of�a�drug.
n �Some�plans�require�members�who�choose�a�Tier�3�drug�over�its�generic�equivalent�(Tier�1)�to�pay�the�highest�copay�PLUS�the�difference�in�cost�between�the�brand�name�drug�and�the�generic�drug.�Please�refer�to�your�member�contract�for�details.
Prescription�drugs�can�account�for�a�large�percentage�of�your�health�care�costs.�By�using�the�CareFirst�BlueCross�BlueShield�(CareFirst)�preferred�drug�list,�also�called�a�formulary,�you�can�discuss�with�your�physician�and�your�pharmacist�about�how�to�make�safe�and�cost‑effective�decisions�to�better�manage�your�health�care.
What is a preferred drug list?CareFirst’s�preferred�drug�list�is�part�of�the�3‑Tier�Prescription�Drug�Program�that�consists�of�both�generic�(Tier�1)�and�preferred�brand�name�(Tier�2)�drugs�that�are�selected�for�their�effectiveness�and�affordability.�Non‑preferred�brand�name�(Tier�3)�drugs�are�not�part�of�the�preferred�drug�list,�but�are�covered�by�your�pharmacy�benefits�at�the�highest�copay.�
How do drugs get on the preferred drug list?The�preferred�drug�list�is�based�on�current�medical�research�and�input�from�a�committee�of�doctors�and�pharmacists�who�serve�the�CareFirst�region.�Drugs�are�selected�for�their�quality,�effectiveness�and�cost.��The�preferred�drug�list�changes�frequently�in�response�to�Food�and�Drug�Administration�(FDA)�requirements.�The�list�is�also�adjusted�when�a�generic�drug�is�introduced�for�a�brand�name�drug.�When�that�happens,�the�generic�drug�will�be�added�to�the�Tier�1�list�and�the�brand�name�drug�will�automatically�move�from�Tier�2��to�Tier�3.
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield

Prior AuthorizationSome�prescriptions�require�advance�approval�before�they�can�be�dispensed.�Prior�Authorization�is�used�to�ensure�that� you� meet� necessary� medical�criteria� to�obtain�a�particular�drug.�When�you�receive�a�prescription�for�one�of�these�drugs,�please�explain�to�your�physician�that�prior�authorization�is�needed�before�benefits�will�be�available�to�you.�Without�proper�authorization,�you� will� pay� the� full� price� of� the�prescription� rather� than�only�your�copay�or�coinsurance�amount.
Your�physician�must�call�to�begin�the�prior�authorization�process.�If�you�are�already�at�the�pharmacy,�they�too�can�call�your�doctor�to�start�the�process.�Members�with�questions�about�prior�authorization�should�call�Argus�Health�Systems,�Inc.�at�(800)�241‑3371.�
The�drugs�listed�to�the�right�require�prior�authorization.�This�list�is�subject�to�your�benefit�plan�and�may�change�periodically.�For�the�most�up‑to‑date�prior�authorization�list,�visit�the�prescription�drug�web�site�at�www.carefirst.com/rx.
ACIPHEX*
ACTIQ*
AFINITOR
APLENZIN*
ARANESP*�
AVINZA*�
AVITA*�
AVONEX*�
BETASERON*�
BRAVELLE�
CELEBREX*�
CESAMET*�
CETROTIDE�
CIMZIA�PRE‑FILLED�SYRINGE*�
COPAXONE�
DAYTRANA*�
DIFFERIN*�
ENBREL
EPIDUO*
EPOGEN*�
EXTAVIA*
FENTORA*�
FLECTOR�PATCH*�
FOLLISTIM�AQ*�
FORTEO*�
GENOTROPIN*
GLEEVEC�
GONAL‑F�
HUMATROPE*
HUMIRA
HYCAMTIN�
INCRELEX*�
KADIAN*�
KAPIDEX*
KINERET*
LANTUS*
LEUKINE*
LOVAZA*�
LUVERIS*
MENOPUR�
NEULASTA*�
NEUMEGA*�
NEUPOGEN�
NEXAVAR�
NEXIUM*�
NORDITROPIN
NOVAREL*
NUTROPIN*
NUVIGIL*
OMNITROPE*
ONSOLIS*
OPANA*�
OVIDREL�
PEG‑INTRON*�
PEGASYS�
PREGNYL*
PREVICID�30MG*
PRILOSEC�10MG*
PRILOSEC�40MG*�
PROCRIT�
PROVIGIL*�
REBIF�
REPRONEX�
RETIN‑A�CREAM�AND�GEL*
RETIN‑A�LIQUID*�
RETIN‑A�MICRO�GEL*
REVLIMID�
SAIZEN*
SEROSTIM�
SIMPONI*
SPRYCEL
SUTENT
SYMLIN*
TARCEVA
TASIGNA
TAZORAC
TEMODAR�
TEV‑TROPIN*
THALOMID
TRETIN‑X*
TYKERB
VOLTAREN�GEL*
VOTRIENT
XELODA
ZEGERID*
ZIANA*
ZOLINZA
ZORBTIVE*
*Non-preferred brand name drugs are not part of the preferred drug list.
Quantity LimitsCertain�prescription�drugs�may�only�be�prescribed�in�limited�quantities.�These�limits�are�set�to�ensure�that�alternatives�are� regularly� reconsidered� by� your�physician.�This�list�is�subject�to�change�and�will�be�periodically�updated.
For�the�most�up‑to‑date�list�of�drugs�with�quantity� limits,�visit� the�prescription�drug�web�site�at�www.carefirst.com/rx.
ACCU‑CHEK�
METER��
TEST�STRIPS��
AMERGE*��
ANZEMET*��
AXERT*��
CAVERJECT*
CIALIS*
CIPRO�XR*
DEPO‑PROVERA*
EDEX*
EMEND
EPIPEN;�EPIPEN�JR.
ESTRING*��
FLECTOR�PATCH*��
FROVA*��
GLUCOMETER�
DEX�TEST�
SENSORS*��
GLUCOMETER�
ELITE�TEST�
STRIPS*��
GLUCOMETER�
ENCORE�TEST�
STRIPS*��
IMITREX*�
(ALL�FORMS)��
KYTRIL*�
LEVITRA*��
MAXALT*
MIGRANAL*��
MUSE*��
ONETOUCH�
METER��
TEST�STRIPS��
OXYCONTIN*�
PROQUIN�XR*��
RELENZA*��
RELPAX*��
SANCUSO*
SEASONALE*
TAMIFLU*
TORADOL*�
TREXIMET*��
VIAGRA��
XIFAXAN*��
ZITHROMAX�
SUSP*�
ZITHROMAX�
TABLETS*�
ZMAX*��
ZOMIG*
*Non-preferred brand name drugs are not part of the preferred drug list.
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield

Maintenance DrugsA�maintenance�drug�is�a�prescription�drug�anticipated�to�be�required�for�six�months�or�more�to�treat�a�chronic�condition.�Maintenance�drugs�can�be�ordered�up�to�a�90‑day�supply.�For�the�most�up‑to‑date�list�of�maintenance�medication,�visit�the�prescription�drug�web�site�at�www.carefirst.com/rx.
Blood Blood�Thinners�(Anticoagulants)‑�Coumadin�Only
Stroke�Prevention
Central Nervous SystemAlzheimer’s�Drugs
Anti‑Parkinson�Drugs
Attention�Deficit�Disorders�(ADD)
Seizure�Medications�(Anticonvulsants)
Chest Pain & Heart Disease (Nitrates)Diabetes & High Blood SugarAntidiabetic�Drugs
Blood�Sugar�Test�Strips
DiseasesArthritis�(Rheumatoid)
Bone�Disease�(Paget’s)
Bone�Disease
Gout
Hepatitis
Multiple�Sclerosis�Drugs
Myasthenia�Gravis�Drugs
Thyroid�Disease
ENT (Ear/Nose/Throat)Allergies�&�Colds�(Nasal)
Allergies�(Oral)
EyeGlaucoma�Drugs
Heart Rhythm DisordersHigh Blood Pressure & Heart DiseaseACE�Inhibitors
Alpha�Beta�Blockers
Angiotensin�II�Blockers
Beta�Blockers
Calcium�Channel�Blockers
Combination�Drugs
Sympatholytics
Water�Pills�Or�Diuretics
High Cholesterol Drugs (Antilipemics)HIV & AIDSCombination�Drugs
Non‑Nucleoside�Reverse�Transcriptase�Inhibitors
Nucleoside�Reverse�Transcriptase�Inhibitors
Protease�Inhibitors
HormonesGrowth
Hormone�Replacement�Drugs
Male
Miscellaneous
Immune SystemAnti‑Rejection�(Immunosuppressants)
InfectionsTuberculosis�(Antituberculosis�Drug)
Low Blood PressureMental Health/SchizophreniaMental HealthAntidepressants
Antipsychotic�Drugs
Manic‑Depression�or�Bipolar�Drugs
NarcolepsyOB-GYNBirth�Control�Patch�(Monophasic�Contraceptives)
Birth�Control�Pills�(Monophasic�Contraceptives)
Birth�Control�Pills�(Progestin�Only)
Birth�Control�Pills�(Triphasic�Contraceptives)
Birth�Control�Ring�(Monophasic)
Breast�Cancer�(Anti‑Estrogens)
Endometriosis
Female�Hormones�(Estrogens)
Female�Hormones�(Progestins)
Female�Hormones�(Replacement�Combination)
Prenatal�Vitamins
Pain Management (Analgesics)- Only Non-Narcotic DrugsPain Management (COX 2)Respiratory ProblemsAsthma�&�COPD�(Miscellaneous�Inhalers)
Asthma�(Bronchodilators)
Asthma�(Methylxanthines)
Asthma�(Oral�Bronchodilators)
Asthma�(Steroid�Inhalers)
Miscellaneous�Drugs�
Stomach & Digestive DisordersAcid�&�Stomach�Ulcers
Bowel�&�Colon�Disease
Malabsorption�Disease
Severe�Heartburn�&�Reflux
SupplementsPotassium�(Eff�.�Tablet)
Potassium�(Liquid)
Potassium�(Tablets)
Vitamin�D
UrologyBladder�Control�(Antispasmodics)
Bladder�Control�(Cholinergic�Agents)
Prostate�Disease�(Benign�Prostatic�Hypertrophy)
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield

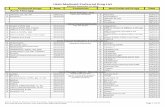
BloodBlood� Thinners/Modifiers,�Stroke�Preventioncilostazolpentoxifyllineticlopidinewarfarinanagrelide
●�ARIXTRA�●�COUMADIN�●�FRAGMIN�●�LOVENOX�●�PLAVIX
AGRYLINPLETAL�TICLIDTRENTAL
Blood�Stimulators ●�NEUPOGEN●�PROCRIT
●�ARANESP●�EPOGEN●�NEULASTA
Bone DiseaseArthritishydroxychloroquinemethotrexateleflunomide
●�ENBREL●�HUMIRA
ARAVACUPRIMINE●�KINERETRHEUMATREXDOSE�PACK
Osteoporosisestradiolestradiol�transdermalalendronate�calcitonin�nasal�spray
PREMARINEVISTA
ACTONELBONIVACLIMARA●�FORTEOFOSAMAXFOSAMAX�PLUS�DMIACALCIN
Central Nervous SystemAttention�Deficit�Disorderamphetamine/dextroamphetaminedextroamphetaminemethylphenidatemethylphenidate�sr
CONCERTA ADDERALLDAYTRANA�DESOXYNDEXEDRINEFOCALINRITALINSTRATTERA
Sedativeschloral�hydrateflurazepamtemazepamzolpidemzaleplon
AMBIENDALMANELUNESTARESTORILROZEREMSONATA
Diabetes and High Blood SugarAnti‑Diabetic�Drugsacarboseglipizideglyburideglimepirideglyburide/metformin�metformin�nateglinide
ACTOSAVANDAMETAVANDARYLAVANDIABYETTADUETACTJANUMETJANUVIAPRANDIN
AMARYLDIABETAGLUCOPHAGEGLUCOTROLGLUCOVANCEONGLYZAPRECOSESTARLIXSYMLIN
Insulin ●�LEVEMIR●�NOVO�INSULIN●�NOVOLOG
●�HUMALOG●�HUMULIN●�LANTUS
Ear/Nose/Throat (ENT)- AllergyCold�‑�Nasalfluticasoneflunisolide
ASTELIN BECONASE�AQ�FLONASENASACORT�AQNASARELNASONEX
Oralclemastine�fumaratefexofenadine
ALLEGRA‑DALLEGRACLARINEXXYZAL
High Blood Pressure and Heart DiseaseACE�Inhibitorscaptoprilenalaprillisinoprilramipril
MULTA�Q ACCUPRILALTACEMONOPRILPRINIVILVASOTEC�ZESTRIL
Angiotensin�Receptor�Blockers
AVAPRODIOVAN
ATACANDCOZAARMICARDIS
High Cholesterol DrugsStatinslovastatinsimvastatinpravastatin
LIPITORNIASPANTRICOR
ADVICORCRESTORLESCOL�XLMEVACORVYTORINZOCOR
InfectionsCephalosporins CECLOR
CEFTINCEFZILDURICEFLORABIDOMNICEFSUPRAXVANTIN
cefaclorcefadroxilcefdinir�cefuroximecephalexin
Quinolonesciprofloxacin LEVAQUIN AVELOX
CIPROCIPRO�XRFLOXIN
Macrolideserythromycinclarithromycinazithromycin
BIAXIN�BIAXIN�XLZITHROMAX
Penicillinpenicillinamoxicillinamoxicillin/clavulanate
AUGMENTIN�XR AMOXILAUGMENTIN�ES
Generic Drugs (Tier 1)
Lowest Copay
Preferred Brand Name Drugs
(Tier 2) Middle Copay
Non-Preferred Brand Name Drugs
(Tier 3) Highest Copay
Generic Drugs (Tier 1)
Lowest Copay
Preferred Brand Name Drugs
(Tier 2) Middle Copay
Non-Preferred Brand Name Drugs
(Tier 3) Highest Copay
Three Tier Preferred Drug List**
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield
List�is�not�all‑inclusive.�For�the�most�complete�and�up‑to‑date�formulary,�please�visit�www.carefirst.com/rx

Three Tier Preferred Drug List**
Mental HealthAntidepressants APLENZIN
CELEXACYMBALTAPAXILPAXIL�CRPROZACWELLBUTRIN�SR/XLZOLOFT
citalopramfluoxetinesertralinevenlafaxineparoxetinebupropion
Antipsychoticschlorpromazinefluphenezinehaloperidolrisperidone
EFFEXOR�XR�LEXAPRO
SEROQUEL
OB/GYNFertility●�chorionic�gonadotropinclomiphene●ganirelix
●BRAVELLE●CETROTIDE●GONAL‑F●MENOPUR●OVIDREL●REPRONEX
CLOMID�FOLLISTIM�AQLUVERIS●NOVAREL●PREGNYL�
Pain ManagementMigrainesumatriptan
●MIGRANAL AMERGEAXERTFROVARELPAX●IMITREXMAXALT�TREXIMETZOMIG
NSAID/COX‑II�Inhibitorsibuprofennabumetonenaproxendiclofenacpiroxicammeloxicam
CELEBREXMOBIC
Respiratory Problems - AsthmaCOPD�Problemscromolyn�sodiumipratropium�bromide
ADVAIRCOMBIVENTSPIRIVA
INTAL
Bronchodilatorsmetaproterenol
PROAIR�HFASEREVENTVENTOLIN�HFA
FORADILMAXAIR�AUTOHALERPROVENTIL�HFAXOPENEX
Inhaled�Steroids FLOVENT�HFAPULMICORT
AEROBIDASMANEXQVAR
Asthma�‑�Miscellaneous�Drugs
SINGULAIR ACCOLATEZYFLO
Stomach and Digestive DisordersAcid�and�Stomach�Disorderscimetidinenizatidinelansoprazolepantoprazole
ACIPHEXKAPIDEXNEXIUMPREVACIDPREVPAC�PRILOSECPROTONIXZEGERID
UrologyProstate�Diseasedoxazosinterazosinfinasteride
AVODARTFLOMAX
CARDURAHYTRINPROSCAR
**This list represents the most frequently prescribed drugs in each category. Discuss with your physician if there are specific alternatives to your current medication on lower tiers. ● Self-Administered Injectable Drugs (Some plans may require a coinsurance payment.)
Generic Drugs (Tier 1)
Lowest Copay
Preferred Brand Name Drugs
(Tier 2) Middle Copay
Non-Preferred Brand Name Drugs
(Tier 3) Highest Copay
Generic Drugs (Tier 1)
Lowest Copay
Preferred Brand Name Drugs
(Tier 2) Middle Copay
Non-Preferred Brand Name Drugs
(Tier 3) Highest Copay
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield

CareFirst BlueCross BlueShield is an independent licensee of the Blue Cross and Blue Shield Association. ® Registered trademark of the Blue Cross and Blue Shield Association. ®’ Registered trademark of CareFirst of Maryland, Inc.
BRC5943‑4P�(11/10)
Using Generic DrugsDid�you�know�that�switching�to�a�generic�drug�could�save�you�money�in�out‑of‑pocket�prescription�costs?�Generic�drugs�are�made�with�the�same�active�ingredients�as�brand‑name�drugs�and�have�the�same�effects�in�the�body.�The�difference?�Name�and�price.
Brand�name�drugs�are�protected�by�patents�for�up�to�20�years�and�until�the�patent�expires,�no�other�companies�can�produce�the�generic�equivalent.�This�keeps�the�cost�to�the�consumer�higher.�However,�when�the�patent�expires,�the�drug�is�able�to�be�released�by�other�companies,�thus�creating�competition.
Facts About Generics n �Clinically�the�same�as�brand‑name�drugs,�but�may�look�different�because�
inactive�ingredients,�like�color,�can�differ�between�manufacturers.
n �Required�by�the�Food�and�Drug�Administration�(FDA)�to�have�the�same�quality,�strength,�purity�and�stability�as�brand‑name�drugs.
n �Endorsed�by�the�American�Medical�Association,�the�largest�organization�of�medical�doctors,�as�acceptable�for�the�American�public.
n �Routinely�used�by�most�hospitals�when�treating�patients.
n �Held�to�the�same�federal�FDA�standards�for�safety�and�performance�as�brand�name�drugs.�
n �Deliver�the�same�amount�of�active�ingredients�in�the�same�time�as�brand�name�drugs.�
n�Companies�that�make�brand�name�drugs�are�linked�to�an�estimated�50�percent�of�generic�drug�production.�
n �Sell�for�30‑75�percent�less�that�brand�name�drugs.�
For�more�information�about�generic�drugs,�visit�our�prescription�drug�web�site�at�www.carefirst.com/rx,�and�click�on�“Learn�About�Generic�Drugs.”
The�preferred�drug�list�changes�frequently�in�response�to�FDA�requirements.�The�list�is�also�adjusted�when�a�generic�drug�is�introduced�for�a�brand�name�drug.�When�that�happens,�the�generic�drug�will�be�added�to�the�Tier�1�list�and�the�brand�name�drug�will�automatically�move�from�Tier�2�to�Tier�3.�For�the�most�recent�information�about�the�preferred�drug�list,�visit�the�prescription�drug�web�site�at�www.carefirst.com/rx.
Need more information?
On the Phone…
If� you� have� questions� about�your�prescription�drug�coverage�or� the� preferred� drug� list,� call�Argus� Health� Systems,� Inc.� at�(800)�241‑3371.
You� should� contact� your�physician�or�pharmacist�if�you�have� questions� regarding� the�type�of�drug,�side�effects,�drug��interactions,�storage,�etc.�
By Mail…If�you�have�questions�
about�your�mail�order�benefits,�call�Walgreens�Mail�Service�at�(800)�745‑6285.�
On the Web…
For�the�most�recent�information�regarding�the�3‑tier�prescription�drug�program,�changes�to�the�preferred�drug�list,�etc.�visit�the�prescription� drug� web� site� at�www.carefirst.com/rx.
Preferred Drug List (Formulary)CareFirst BlueCross BlueShield