Poster # 170; Abstract 7533 Relapsed/Refractory CLL or SLL ...€¦ · Poster # 170; Abstract 7533...
Transcript of Poster # 170; Abstract 7533 Relapsed/Refractory CLL or SLL ...€¦ · Poster # 170; Abstract 7533...

100
50
-50
-100
0
Best
% C
hang
e in
Tar
get N
odal
Les
ions
Patients
100
50
-50
-100
0
Best
% C
hang
e in
Tar
get N
odal
Les
ions
Patients
Overall Response Rate (Investigator Assessment per modified IWCLL/IWG Criteria)
CI= confidence interval; CR= complete response; CRi = CR with incomplete marrow recovery; LNRR = lymph node response rate (i.e. >50% decrease in target nodal lesion); ORR= overall response rate; PR= partial response; PRwL = PR with lymphocytosis
• For patients with 17p deletion treated with duvelisib (n=20), the ORR was 80% (95% CI: 63, 98), which included 2 (10%) CRi, 13 (65%) PR, and 1 (5%) PRwL
Progression-Free Survival Per Investigator Assessment
Growth &survival ofmalignant
B cells
Recruitment ofmalignant B cells
Recruitment & differentiation of cellssupporting B cell growth & survival
Tumor-associatedmyeloid cell
PI3K-γ
PI3K-γ
Tumor Microenvironment (TME)
BCR
Cytokinereceptor
Cytokines
Cytokines
Migration, activation, andM2 polarization signals
Cytokinereceptor
CD40R CD40L
Anti-tumorimmune response
CXCL13
CXCR5 CXCR4
CXCL12
CXCR4
CXCL12
CD4+ T cell
PI3K-δ PI3K-γ
Malignant B cell
PI3K-δPI3K-γ
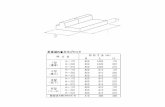
Category N = 89
Median Age (years) 68
Min, Max 39, 90
≥ 65 years, % 61
Sex, %
Male 63
Female 37
Race, %
White 92
Other 5
Unknown 3
Background
The Efficacy of Duvelisib Monotherapy Following Disease Progression on Ofatumumab Monotherapy in Patients with Relapsed/Refractory CLL or SLL in the DUOTM Crossover Extension Study
Bryone Kuss1; Matthew S. Davids2; Peter Hillmen3; Carol Moreno4; James H. Essell5; Nicole Lamanna6; Zsolt Nagy7; Ulrich Jaeger8; Constantine Tam9; Stephan Stilgenbauer10; Paolo Ghia11; Julio Delgado12; Diep Le13; Brenda Jeglinksi13; Marco Montillo14
1Flinders Medical Centre, Bedford Park, AUS; 2Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, MA; 3St. James’s Institute of Oncology, The Leeds Teaching Hospitals, Leeds, UK; 4Hospital de la Santa Creu i Sant Pau, Barcelona,Spain; 5Oncology Hematology Care, SCRI, Cincinnati, Ohio, USA; 6New York Presbyterian, Columbia University Medical Center, New York, NY; 71st Department of Internal Medicine, Semmelweis University, Budapest, HUN; 8Department of Medicine I, Division of Hematology and Hemostaseology, Medical University of Vienna, Vienna, AUT; 9Peter MacCallum Cancer Centre, St Vincent’s Hospital and University of Melbourne , Melbourne, AUS; 10Department III of Internal Medicine, University Hospital Ulm, Ulm, GER; 11Università Vita-Salute San Raffaele and IRCCS Istituto Scientifico San Raffaele, Milan, ITA;
12Hospital Clinic, Barcelona, SPA; Flinders Medical Centre (FMC), Bedford Park, AUS; 13Verastem Oncology, Needham, MA; 14Niguarda Cancer Center, ASST Grande Ospedale Metropolitano Niguarda, Milan, ITA
Demographics and Baseline Characteristics
• Duvelisib is an oral dual inhibitor of PI3K-δ and PI3K-γ being developed for treatment of hematologic malignancies, including relapsed/refractory (R/R) CLL/SLL
• The Phase 3 DUOTM Study (NCT02004522; Study IPI-145-07) in patients with R/R CLL/SLL met its primary endpoint, with duvelisib monotherapy demonstrating a statistically significant improvement in PFS vs ofatumumab monotherapy (Flinn ASH 2017)
• In DUO, the most common ≥ Gr 3 AEs were hematologic and included neutropenia (30%), anemia (13%), and thrombocytopenia (8%); the most common severe non-hematologic AEs were diarrhea (15%), pneumonia (14%), and colitis (12%)
CategoryDuvelisib monotherapy
N=160Ofatumumab monotherapy
N=159
Median PFS (months) 13.3 * 9.9
95% CI 12.1, 16.8 9.2, 11.3
ORR, % 74 * 45
95% CI 66.9, 80.6 37.5, 53.0
LNRR, % 85 * 16
95% CI 79.5, 90.5 10.1, 21.4
DUO™ Study
Study IPI-145-12
Crossover Study
Ofatumumab IVAdministration same as DUON=8
Duvelisib25 mg BID continuouslyN=89
Duvelisib25 mg BID PO continuously N=160
Ofatumumab IV- 300 mg IV infusion on Day 1- 2000 mg IV weekly (x7) then monthly (x4)N=159
Relapsed or Refractory
CLL/SLL patients
319 Patients Randomized 1:1
Category N = 89
Diagnosis, %
CLL 99
SLL 1
High-Risk Cytogenetics, %
17p deletion present (per central lab) 20
Years from Initial Diagnosis
Median 7
Min, Max 0.5, 22.0
Current Stage – Rai, (n=38), %
I 16
II 34
III 13
IV 37
Current Stage – Binet, (n=51), %
A 0
B 74
C 26
Baseline Lymphocytes (×109/L)
Median 13.96
Min, Max 0.0, 273.2
Prior Treatment N = 89
Median number of prior anticancer therapies
3
Min, Max 2-8
Received ≥ 3 prior lines of therapy, % 61
Prior Therapies, %
Purine Analog 73
Alkylator 96
Cyclophosphamide 72
Bendamustine 38
Chlorambucil 29
Monoclonal antibody 100
Ofatumumab 100
Rituximab 87
Obinutuzumab 2
Alemtuzumab 1
Baseline Characteristics Disease History Prior to DUO Entry
Prior Anticancer Therapy
Efficacy
DUO Study Pre-crossoverOfatumumab
N=89%
Study IPI-145-12 Post-crossoverDuvelisib
N=89%
ORR 28 73
95% CI 19, 37 64, 82
CR 1 0
CRi 0 5
PR 27 57
PRwL 0 11
LNRR 27 73
Percent Change in Nodal Target Lesions (Ofatumumab Pre-crossover)
Percent Change in Nodal Target Lesions (Duvelisib Post-crossover)
Safety
Preferred TermAll Grades
%Grade 3
%Grade 4
%
Hematologic Neutropenia 25 12 10
Nonhematologic Diarrhoea 38 17 0
Pyrexia 23 3 0
Rash 21 5 0
Colitis 11 9 0
Vomiting 11 0 0
Asthenia 11 0 0
Cough 11 0 0
Decreased appetite 10 0 0
Nausea 10 0 0
Pneumonia 10 9 0
0 10 20 30 40 50 60 70 80 90 100
Infection SOC
Neutropenia
Diarrhea
Colitis
Skin reaction SOC
Pneumonia
Transaminitis
Pneumonitis
% of Patients
Adverse Events of Interest
Treatment-Emergent AEs by Grade (>10% Overall) All Causalities
Note: AEs coded using MedDRA version 16.1. Percentages are based on the number of treated patients.
Abbreviation: SOC = system, organ, class
• Few discontinuations due to AEs of interest• Three patients with severe opportunistic infections - Pneumocystis jirovecii pneumonia (PJP) (n=2): 1 not receiving prophylaxis at the
time of onset - Pneumonia cytomegaloviral (n=1) • 1 AE on study leading to death assessed as related to duvelisib: PJP (noted above)
• In this extension study, duvelisib monotherapy achieved robust responses in 89 R/R CLL/SLL patients who had disease progression following ofatumumab treatment on the DUO study
- ORR: 73% on duvelisib (28% on prior ofatumumab)
- Median PFS: 15 months on duvelisib (9 months on prior ofatumumab)
- 83% of evaluable patients had >50% reduction in target nodal lesions
• The safety profile of duvelisib monotherapy was manageable and consistent with what was observed in the Phase 3 DUO study
• These data further support the potential clinical benefit of duvelisib monotherapy in patients with R/R CLL/SLL
Conclusions
Presented at the 2018 American Society for Clinical Oncology Annual Meeting • Chicago, Illinois, USA • June 1-5, 2018
Patient Enrollment and Disposition
Poster # 170; Abstract 7533
Study Enrollment by Region/Country
• 89 of 101 patients treated with ofatumumab with confirmed disease progression on DUO elected to enroll in Study IPI-145-12
• As of 19 July 2017, 60 (67%) patients have discontinued duvelisib, 32 (36%) due to AEs, 16 (18%) due to PD, 4 (5%) due to death, and 8 (9%) for other reasons (e.g. voluntary withdrawal)
• 29 (33%) patients remain on duvelisib
17%11%
12%
13%8%
9%
6%
8%
5%
3%
9%
US (n=7; 8%)Australia (n=5; 6%)New Zealand (n=4; 5%)
Hungary (n=15; 17%) Italy (n=12; 13%) Spain (n=11; 12%)France (n=10; 11%)
Belgium (n=8; 9%) UK (n=8; 9%)Austria (n=7; 8%)Germany (n=2; 3%)
28% (24/87 evaluable patients) had a >50% reduction in target nodal lesions
83% (65/78 evaluable patients) had a >50% reduction in target nodal lesions
100
Prob
abili
ty o
f Pro
gres
sion
-Fre
e Su
rviv
al
89 65 55 42 25 20 10 5 2 1 089 82 63 54 31 13 4 3 2 1 0
Time (months)Number at Risk
80
60
40
20
0 3 6 9 12 15 18 21 24 27 300
Ofatumumab (N= 89) DUO Study Pre-crossoverDuvelisib (N= 89) Study IPI-145-12 Post-crossoverTreatment
≥ Grade 3 AEsAEs leading to discontinuation (any Grade)
Median PFS (months) (95% CI)Ofatumumab (Pre-crossover): 9 (9, 11)Duvelisib (Post-crossover): 15 (10, 17)
Key Efficacy Results from the DUOTM Study (Flinn ASH 2017)
All results per blinded independent review committee*statistically significant vs ofatumumab: p<0.0001LNRR = lymph node response rate (i.e. >50% decrease in target nodal lesion)
• Study IPI-145-12 (NCT02049515) is an open-label, optional, crossover extension study where patients with radiologically confirmed disease progression on DUO were given the option to receive the opposite treatment
• Herein we present data for the 89 patients who voluntarily crossed over following radiologically confirmed disease progression on ofatumumab on DUO and received duvelisib on Study IPI-145-12
• To further characterize duvelisib, an ad-hoc analysis was performed for ORR and PFS for the 89 patients while receiving ofatumumab pre-crossover in the DUO study
• Eligible patients enrolled within 3 months of radiologically-confirmed disease progression on the DUO study (excluding Richter’s transformation or prolymphocytic leukemia)
• Duvelisib 25 mg BID was administered until PD, intolerance, death, or study withdrawal • All patients received mandatory prophylaxis for PJP
Study Design
For more [email protected]
Copies of this poster obtained through Quick Response (QR) Code are for personal use only and may not be reproduced without permission from ASCO® and the author of this poster.