Postauricular fascial flap and suture otoplasty: A prospective outcome study of 227 patients
-
Upload
manish-sinha -
Category
Documents
-
view
215 -
download
2
Transcript of Postauricular fascial flap and suture otoplasty: A prospective outcome study of 227 patients

Journal of Plastic, Reconstructive & Aesthetic Surgery (2012) 65, 367e371
Postauricular fascial flap and suture otoplasty: Aprospective outcome study of 227 patients*
Manish Sinha, Bruce Richard*
Birmingham Children’s Hospital, Steelhouse Lane, Birmingham B4 6NH, UK
Received 6 July 2011; accepted 12 September 2011
KEYWORDSOtoplasty;Prominent earcorrection;Suture otoplasty;Post auricular flap;Mustarde’s Technique
* Presented at the 2010 winter mee* Corresponding author. Tel.: þ44
3338131.E-mail address: Bruce.Richard@bc
1748-6815/$-seefrontmatterª2011Bridoi:10.1016/j.bjps.2011.09.018
Summary The anterior scoring technique is criticised for a higher risk of haematoma relatedcomplications while the suture techniques for suture-extrusion and recurrence. Horlock et. al.described a suture otoplasty with addition of a postauricular fascial flap to reduce sutureextrusion and noted recurrence rates of 8%. We report the senior author’s experience with thistechnique in 227 consecutive cases. All cases were done by or under supervision of the seniorauthor and the data collected prospectively. Complications, recurrence, revision rate andresults as recorded were analysed. A total of 10 (7 early 3 late) complications were recorded(4.4%). Suture extrusion (n Z 6, 2.64%), Keloids (n Z 3, 1.32%), Infection, anterior skinnecrosis (n Z 1 each, 0.44%). A total of 6 unilateral and 5 bilateral cases had a recurrence(3.67% total ears) and 97% of recorded outcomes were reported as good or excellent results.The low complication rate seems to support the hypothesis that the fascial flap prevents sutureextrusion and reduces risk of recurrence. Lack of Anterior dissection avoids risks of bleedingand haematoma.ª 2011 British Association of Plastic, Reconstructive and Aesthetic Surgeons. Published byElsevier Ltd. All rights reserved.
Introduction
The postauricular fascial flap as an adjunct to suture oto-plasty was described by Horlock et. al. in 2000.1 Increas-ingly this technique has gained popularity in the recent pastand in a straw poll of the plastic surgeons attending the
ting of BAPRAS in London.121 3338132; fax: þ44 121
h.nhs.uk (B. Richard).
tishAssociationofPlastic,Reconstruc
2010 Winter Meeting of British Association of PlasticReconstructive and Aesthetic Surgeons, nearly halfacknowledged using it regularly.
Anterior scoring has been criticised for a higher risk ofhaematoma related complications while suture techniquesfor suture-extrusion and related complications of recur-rence.1 The senior author having had an opportunity totrain in both these techniques preferred Mr. Gault’s tech-nique and believes that this technique not only producesa good aesthetic outcome but also decreases the risks ofsevere and difficult to correct complications of anteriorscoring like anterior skin necrosis and folds in the cartilagewith scarring.
tiveandAestheticSurgeons.PublishedbyElsevierLtd.All rightsreserved.

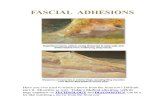
Figure 1 Incision. Figure 3 Elevation of posterior skin.
368 M. Sinha, B. Richard
This study was undertaken to report experience of usingthis technique in 227 consecutively operated patients.
Material and methods
During November 2002 to April 2010, 227 patients under-went prominent ear correction under care of the seniorauthor at Birmingham Children’s Hospital by the sutureotoplasty technique. The data was collected prospectivelyand maintained in a database held at a central server andupdated at each point of contact with the patient. Thisdata was analysed and information supplemented froma retrospective review of notes of all the patients who hadany complication.
Technique
The technique as described by Horlock et al1 was usedexcept that no skin excision was undertaken in any case. Incases operated under local anaesthetic, EMLATM cream wasapplied pre-operatively and a field block was administeredby Lignocaine 2% with 1:80,000 adrenaline infiltration. Incases with general anaesthetic a local infiltration of thesame agent was used.
Figure 2 Subdermal plane dissection.
A posterior linear incision was used in all cases(Figure 1). A plane was developed at the subdermal level(Figure 2) to reflect posterior skin up to helical rim(Figure 3). An incision was made through the adipo-fascial layer and the perichondrium (Figure 4). This thinand pliable flap was then reflected back posteriorly up tothe concho-mastoid groove till periosteum was encoun-tered over the mastoid (Figure 5). Blunt dissection wasdone to allow placement of concho-mastoid sutures andthe Auricularis Posterior muscle was preserved. Three tofour mattress sutures were inserted to create an anti-helical fold using 4/0 Ti-cron TM (Covedien) on a roundbody needle. The sutures were placed in a cranio-caudaldirection to recreate a smooth anti-helical fold (Figures6,7 and 8). Concho-mastoid sutures were used as neces-sary (Figure 9). The postauricular flap was then drapedover the sutures and anchored with 4/0 vicryl TM (Ethi-con) (Figure 10). The skin was sutured with subcuticular4/0 vicryl and a traditional dressing of jellonet, pro-flavine wool and a padded head bandage was used in allcases.
Patients were reviewed in 8e10 days in a nurse leddressing clinic and advised that it was not necessary towear a head band during night time.
Figure 4 Incision of the adipo-fascial flap.

Figure 5 Elevation of the flap.
Figure 6 Mustarde’s Sutures being placed.
Figure 8 Mustarde’s Sutures being placed.
Figure 9 Conco-Mastoid suture and row of Mustarde’ssutures placed. The flap ready to be draped over.
Postauricular fascial flap and suture otoplasty 369
Results
227 patients underwent prominent ear correction by thistechnique. Of 227 cases, 19 were unilateral and 208 bilat-eral giving a total of 435 ears. The age range was 6e16years with a male to female ratio of 5:3. 60% of cases were
Figure 7 Mustarde’s Sutures being placed.
done under General Anaesthetic. In bilateral cases, 42%were operated by a registrar, 32% by the consultant and in26% cases, one ear was operated by each. In unilateralcases, 58% were operated by consultant and 42% by regis-trars. The less experienced registrars were directly
Figure 10 Flap re-draped anchored with 40 vicryl sutures.

Table 1 Comparison of results.
n ears Suture Extrusion Recurrence Keloid Haematoma Skin Necrosis
Horlock et. al. 20011 51 101 0 8.9% 0 0 0Mandal et. al. 20067 41 82 7.3% 4.9% 0 1 0Present Study 2010 227 435 2.64% 3.7% 1.32% 0 0.44%
370 M. Sinha, B. Richard
supervised by the senior author but once gaining confidencewith the technique, operated with consultant present butnot scrubbed.
In total 10 patients (14 ears) had complications (4.4%patients, 3.2% ears). 6 patients (2.64% patients) had sutureextrusions (all managed as out-patients and with only onerecurrence of deformity) and one patient had a headbandage related bilateral anterior skin ulcers that healedwith conservative measures uneventfully. We came acrossthree patients who developed keloid scarring (1.32 %patients)
There were 6 unilateral and 5 bilateral recurrencesrepresenting 4.8% patients and 3.7% ears (Table 1). All butone of these required correction and were operated witha simple re-do of the original technique with a satisfactoryoutcome. 97% of patients had a good or excellent outcomenoted at the time of final review by the clinician.
Discussion
More than 200 techniques have been described in thepublished literature for prominent ear correction indicatingthat there is no single, widely accepted procedure that isuniformly accepted.2 These techniques are generallydivided into cartilage sparing or cartilage cutting tech-niques. Anterior scoring techniques are prone to risk ofanterior haematoma and related complications like skinnecrosis or deformed cartilage that may be difficult tocorrect surgically.3e5 Mustarde’s technique of suture oto-plasty although inherently safer as compared to anteriorscoring, has a variable suture extrusion rate and a recur-rence rate of up to 24%.6
In our series, recurrence of deformity remained rare andwas not associated with the earlier part of the series,suggesting no ‘learning curve’ for the risk of recurrence. 6recurrences were in the hands of the consultant and 10 inthe hands of registrars. This was correlated with highernumber of ears operated by registrars and proportionately,the two groups had a similar rate of complications. All butone patient needed operative correction by a simple redoof the original technique leading to a satisfactory outcome.
Of the six patients who had suture extrusion, four wereoperated by registrars and two by consultant. Four patientshad a single episode of a single suture extrusion and in twocases, up to four suture extrusions were noted in up to 3episodes. The earliest case of suture extrusion was noted at3 months but one patient presented 3 years from the dateof operation. All these cases were managed conservativelywith removal of sutures in the outpatient clinic and nonerequired any operative intervention. Only one out of thesesix cases went on to develop recurrence and the rest healeduneventfully maintaining their operative correction.
Horlock et. al.1 reported a zero% suture extrusion rateand 8% recurrence with post auricular flap refinement ofMustarde’s technique in 51 patients. Mandal et. al.7 re-ported a similarly operated cohort of 41 patients witha 7.3% suture extrusion and 4.9% recurrence. Our resultscompare favourably at 2.64% suture extrusion and 3.7%recurrence rate in 435 ears of 227 patients. In terms ofrecurrence, our study with a large number of patientsyields a 95% Confidence Interval of 2.1 to 5.9 meaningthereby one should expect a recurrence rate of 2.1e5.9%with this technique as a guide. The 95% Confidence Intervalfor suture extrusion is 0.5% to 2.97%.
We agree with Horlock and co-worker’s observation thatit is difficult to attribute the reduced recurrence rate solelyto the addition of the fascial flap. We also agree with theirobservation that the post-auricular fascial flap is a simpleand quick additional step that adds an additional vascu-larised layer between the skin closure and the sutures.Mandal and co-workers believe that the fascial flap acts asa double breasting layer over the sutures preventingextrusion, increasing post-auricular support, and reducingrecurrence. The data presented in this paper would appearto support their belief. We also have a number of anecdotalcases from colleagues who tried this technique with nofascial flap and found a higher risk of infection withextruded sutures, frequently requiring a repeat proceduresome months later. There is no data collected on thesecases from colleagues to be able to quantify this.
97% of patients at the time of final review were noted tohave a good to excellent outcome as assessed by theclinician. This was a subjective assessment made by theclinician. Objective assessment of aesthetic outcome wasnot in the scope of this paper. Schaverien et al.8 using thesame technique on 60 patients reported a consistent post-operative correction with excellent patient and parentsatisfaction.
Conclusion
This is the largest reported series of prominent earcorrection by Posterior auricular flap and suture otoplastytechnique in 227 cases, 435 ears. A large proportion ofcases were operated by trainees and we have found thistechnique to be simple, safe and easy to learn. The tech-nique avoids the dangers of anterior dissection as in ante-rior scoring and minimises the risks of anterior skin necrosisand cartilage necrosis. It maintains all the benefits ofMustarde’s original technique and reduces the rate ofsuture extrusion and recurrence. In all the cases of recur-rence that have needed reoperation, we have found thata simple re-do of the original procedure was possible and

Postauricular fascial flap and suture otoplasty 371
sufficient to correct the prominence. This, we believe isanother strength of the technique.
Conflict of interest
None declared.
Funding
None declared.
Acknowledgement
Patients and parents for consenting to publications ofimages, Dr. Paul Davies for statistical analysis, Deb andLisa, Clinical Nurse Specialists, Kerry & Jackie, Secretariesand Department of Clinical Photography at BirminghamChildren’s Hospital.
References
1. Horlock N, Misra A, Gault DT. The postauricular fascial flap as anadjunct to Mustarde and Furnas type otoplasty. Plast ReconstrSurg 2001 Nov;108(6):1487e90. discussion 1491.
2. Bajaj Y, Rokade A, De PR. Otoplasty: experience with a modifi-cation using a drill, and literature review. J Laryngol Otol 2007Jan;121(1):61e4.
3. Reynaud JP, Gary-Bobo A, Mateu J, Santoni A. Chondritespostoperatoires de l’oreille externe: 2 cases from a series of 200cases (387 otoplasties). Ann Chir Plast Esthet 1986;31:170.
4. Calder JC, Naasan A. Morbidity of otoplasty: a review of 562consecutive cases. Br J Plast Surg 1994;47:170.
5. Jeffery SL. Complications following correction of prominentears: an audit review of 122 cases. Br J Plast Surg 1999;52:588.
6. Tan KH. Long-term survey of prominent ear surgery: a compar-ison of two methods. Br J Plast Surg 1986;39:270.
7. Mandal A, Bahia H, Ahmad T, Stewart KJ. Comparison ofcartilage scoring and cartilage sparing otoplastyea study of203 cases. J Plast Reconstr Aesthet Surg 2006;59(11):1170e6.
8. Schaverien MV, Al-Busaidi S, Stewart KJ. Long-term resultsof posterior suturing with postauricular fascial flap oto-plasty. J Plast Reconstr Aesthet Surg 2010 Sep;63(9):1447e51.