Pollen allergy in Europe - European Academy of Allergy … · Web viewStrannegard IL et al....
Transcript of Pollen allergy in Europe - European Academy of Allergy … · Web viewStrannegard IL et al....
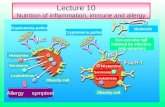
Allergenic Pollen in Europe Allergenic Pollen in Europe and in the Mediterranean Areaand in the Mediterranean Area
Carlos Nunes Center of Allergy and Immunology of Algarve
R Jose Antonio Marques 3 C – 48500-700 PortimaoPortugal
e.mail: [email protected]
Clinical importance of Pollinosis is confined to flowered plants (namely the division of Spermatophyte) with, primarily, produced wind-dispersed pollens. Although such (anemophilous) form a floral minority everywhere, prodigious outputs of pollen continue to ensure their reproductive success. Higher plants (as in tropical areas) exclusively use insects or bats, birds, etc. as self-directed vectors for pollen dispersal. Such species (entomophilous) produce relative few pollens grains but have evolved large, brightly, coloured blossoms and sweet nectars to attract conveyor organisms. Some other plants with grouped and showy flowers in aggregate (amphiphilous) such acacias, goldenrods, sumac and wild grapes, whom have only a minority of grains windborne by insects? Only in large group have potency for air contamination?Pollen prevalence at any site will reflect the strength and proximity of upwind sources and the activity of crosswinds both vertical and horizontal.Pollens level are influenced strongly by the depth of the volume of air in which free mixing can occur, and this, in turn can reflect the prevailing profile of the lower atmosphere.Overall, levels of airborne pollen are increased by warm, dry, clear conditions and fall during unseasonable, cold or wet periods. Determinants of pollens output anemophilous species are not well understood but appear to include temperature, humidity, rainfall and light intensity. Anemophilous annuals, which must complete their life cycles in a single season, generally shed pollen in late spring to mid or late summer, depending on their seed germination dates. When winter is harsh prevail blossom loss, which can be extensive, and flowering conditions can be unpredictable making tree pollination variable in date and intensity.Others species with perennial rootstocks, such as grasses, nettles, hemp, plantains, etc., generally follow flowering from early spring to mid summer.Despite several decades of active studies related to aerobiology, pollen prevalence data continue to offer:
1
Clues to potential offenders in new population centres Evidence of extension exposure trends in communities even those with established
database Insight into a short period exposure burdens for clinical observations and
investigative useWe should recognise that a network of pollens counters throughout several stations across Europe is very important. Also we should note that without a common volumetric (volume-dependent like a Burkard) denominator samples from those stations couldn’t be compared.
For practical reasons related to promote adequate information to patients suffering from pollinosis, we know that most pollen is released in the early morning hours with the rise in temperature and decline in relative humidity. With dispersal by wind currents, pollen levels usually peak in the afternoon or early evening. Wind can carry pollen for miles, resulting in high pollen counts far from the source. Pollens from trees and grasses are most problematic in spring and early summer, respectively; weed pollens predominate in midsummer.
Clinically important Pollinosis is primarily due to flowering plants with wind-dispersed pollens. Although these anemophilous species form a minority of flowering plants, they produce prodigious amounts of pollen. Entomophilous (insect-pollinated) plants produce relatively few pollen grains. Plants having only a portion of their pollen grains airborne are termed amphiphilous. Their role in Pollinosis is not clear.Although pollen grains can travel several hundred miles, concentrations of windborne pollens generally decrease sharply within a few hundred meters of their source.Intact pollen grains are presumed to be the primary carriers of allergen, but some allergens have been associated with particles of the pollens grain and their activity has been found in submicronic particles. Furthermore, allergens might be eluted from pollen grains deposited on humid surfaces, with dispersion of the resultant extract in droplets.Most airborne pollens range in size from 12 to 70 m and certain features make identification.Trees and other woody plants are the earliest to undergo pollination each growing season. Tree pollination especially varies in date and intensity. Non-woody perennial species (e.g., grasses) generally follow the trees from late spring to midsummer. In southern Europe grasses may pollinate from April to July.Establishing a dose-response relationship between pollen exposure and symptoms is difficult. The range of severity for individuals is quite broad, and symptoms often reflect concurrent exposure to several allergens. Response usually increases with ongoing short-term exposure (priming), and exposure involves aerosol fractions besides intact pollen grains. Pollens usually penetrate to the level of the glottis. As we have said above,
2
most particles of grain pollens deposit in the nose, pharynx, oesophagus, stomach, and eyes.The protein molecules in pollens capable of sensitising patients generally range in size from 10,000 to 40,000 Daltons. Once the pollen grain is in contact with the upper airway mucous membranes, symptoms develop within a few minutes, suggesting that these proteins are rapidly eluted. Although individuals are exposed to many potentially allergenic pollens, only a relatively few pollens produce symptoms. This relative restriction of sensitisation reflects the broad patterns of cross-reactivity among proteins derived from different but taxonomically related plants.Methods for assessing cross-reactivity among pollen extracts and their implication in individual symptoms are very interesting. In clinical practice this characteristic is essential to understand clinical symptoms after food ingestion in individuals sensitised to some pollens grains that have allergens commons to determinate grain pollen. The methodology may be divided into approaches that measure all proteins or antigens (e.g., gel diffusion against animal antisera, isoelectric focusing, and crossed immunoelectrophoresis (CIEI) and those that examine the allergenic relationships of the extracts (e. g., RAST inhibition and crossed radioimmunoelectrophoresis (CRIEI). RAST inhibition cannot demonstrate to what extent individual allergens in two pollen extracts are related or unique. CRIE, although less quantitative than RAST, offers the advantage of separately analysing each allergen. These methods demonstrate considerable cross-reactivity within and between many plant families.For the Cupresssaceae, cedars, cypresses, and junipers are important in pollinosis; other conifers have only minor allergenic significance. Marked cross reactivity occurs within the cypress family, with little cross-reactivity extending to other conifersThe Fagaceae (beech) and Betulaccae (birch) families produce pollens that strongly cross-react. Birch species appear to be the most closely related to each other. Immunotherapy for one may be adequate to treat allergy to others and may also be sufficient to treat allergy to beech family members.The Salicaccae (willows, poplars, and aspens) strongly cross-react with each other and show some degree of cross-reactivity with the birch and beech families, Oleaceae (olive, ash, and privet) show strong cross-reactivity. Reports of cross-reactivity in the Aceraccae (maple and box elder) are conflicting.Of the Poaceae, the subfamily Festucoideac contains most of the grasses important in causing allergic symptoms in the Europe. These grasses demonstrate extensive cross-reactivity. For most allergic patients, treatment and testing may be conducted with one or a few members of this family. Purified Lolium (rye) allergens have been obtained, termed Lol p 1, 11, and 111 (formerly rye 1, 11, and 111). Eighty-five to 95% of patients exhibit reactivity to the grass group 1 allergens (Lol p 1 and its homologs). A subfamily, Eragostoideae, contains one predominant allergenic member, Bermuda grass. Separate
3
testing and treatment is necessary for Bermuda, Bahia, and Johnson grasses because of their low degree of cross reactivity with the Festucoideae.In the Urticaceae and Asteraceae families, nettle and pellitory show a lack of cross-allergenicity. A 12,000 dalton allergen has been purified from pellitory. Among the composites, major allergens have been identified from the tribe Ambrosicae. The most important is Ambrosia artemisia (short ragweed) allergen Amb a 1 (antigen E). Other purified antigens include Amb a 11 (antigen K), Amb a 111 (Ra3), Amb a V (Ra5), and Amb a VI (Ra6). Several other allergens have been partially characterized. Some antigenic differences exist between giant and short ragweed species. In areas where Asteraceac other than ragweed are clinically significant, adequate immunotherapy will not be achieved by using ragweed extracts alone if pollen levels are significant.The Chenopodiaceous and Amaranthaceae families contain major inducers of pollinosis in the central Europe. Members of the Chenopodiaceous are closely related and cross-react strongly with the amaranth family.
Pollen CalendarsPollen Calendars
In 1989, the executive officers of both the EACCI “Aerobiology” Subcommittee and the IAA “European Allergy Network” Working Group agreed that the submitted material, information and contributions should be integrated as much as possible into one collaborative report. The Regional European Pollen Calendars are combined with the national and aerobiological reports on pollinosis in Europe with the aim to have data to perform regional, national and European pollens calendars.The data should be related to continuous volumetric data collected with a Burkard or Lanzoni pollen trap, over periods from 3 to 5 years.The calendars should integrate a data selection of the 15 taxa considered comprised ten prescribed taxa selected on the basis of either their abundant airborne occurrence and/or their allergenic significance; and five additional taxa selected from ten allergenically less important, or aerobiologically less frequent taxa.In 1999 an European pollens calendar was made and published with the name of “The European Pollen Calendar” by EAACI with the participation of European Federation of Asthma and allergy associations (EFA) an UCB Institute.
JanuaryHazel flowers between December and April. The symptoms of pollinosis, which start in January/February and last up to two mouths, can occur far from hazel trees. As a consequence of its early pollination and its allergenic cross-reactivity with birch, hazel can induce the start of sensitization to birch. Cypress flowers from February until April.
4
FebruaryAlder flowers between February and April. Alder-pollen allergens cross-react with birch and hazel. Parietaria flowers from January to November. It is found throughout Europe but prevalently in Mediterranean areas. Asthma associated with rhinoconjunctivitis is the main symptom of Parietaria pollinosis.Although not highly allergenic, mimosa has been known to cause proximity pollinosis; its best to avoid smelling these flowers.
MarchGrasses start to pollinate along the Mediterranean coasts. Hazel and alder are in flower in central and northern Europe. Birch starts to flower along the coasts of the Black Sea.Adhere to your treatment plan and enjoy spring.
AprilBirch flowers in central Europe, and the hay fever season with clinical symptoms caused by Parietaria pollen begins in southern areas. Parietaria is a major cause of seasonal asthma: symptoms can start to appear at a threshold concentration of about 30 pollen granules/m³.Entomophilous plants (plants pollinated by insects, e.g., roses and orchids) tend to be very colorful so as to attract insects. They are less allergenic and produce much less pollen than anemophilous plants; their pollen is heavier and less likely to be released into the air.
MayThe concentration of grass pollen reaches its peak in Mediterranean areas. Olive trees start to flower around the Mediterranean, and birch starts to flower in central and northern Europe. Symptoms of olive allergy can occur after a brief exposure, and subjects allergic to other pollens are at a grater risk. Olive pollen can cause conjunctivitis and in a high percent of cases, cough and/or asthma.
JuneThis is the peak season for grass pollination in northern Europe. The concentrations of olive and Parietaria pollen are still high in southern Europe.
JulyMugwort pollination starts in mid-July and ends in mid-October. Allergy is usually associated with sensitization to other pollens, so symptoms can last beyond the flowering period. Mugwort pollen is relatively heavy and not easily dispersed into the air, but large quantities are produced. In July concentrations of grass pollen are still high in northern Europe. Parietaria continues to be present in southern areas, and starts to appear in southern parts of the British Isles.
5
AugustPollen concentrations are low in Mediterranean areas. High concentrations of mugwort pollen are found in central and northern Europe. The ragweed pollen season starts in central Europe. Grasses are also flowering in the archipelagoes off the east coast of Sweden.
September There is a low pollination month in central and northern Europe. Ragweed pollination continues in central Europe. In Mediterranean areas, mugwort pollen makes its appearance; there is a second wave of Parietaria flowering (less intense than the spring flowering), and the Chenopodiaceae are in flower.Rain-washes pollen out of the air, but it can be followed by a burst of blooming and pollination. There is more pollen in the air on windy days.
OctoberParietaria and mugwort are still flowering around the Mediterranean. There are pockets of ragweed and mugwort pollination in central Europe.Parietaria still flowers around Mediterranean coastal waters.
NovemberThe long pollination season in the Mediterranean areas is drawing to a close, and the pollination cycle resumes with the onset of cypress flowering.
DecemberAtmospheric pollen concentrations are very low at this time of the year.
RECOMMENDED FURTHER READING
D’Amato G.,Spieksma F.Th.M.Bonini S. - Allergenic pollen and pollinosis in Europe. Blackwell Science, Oxford, UK, 1991D’Amato G.,Spieksma F.Th.M.,Liccardi G. et al - Pollen-related allergy in Europe. Position Paper of the European Academy of Allergology and Clinical Immunology. Allergy 1998; 53:567-78.Respiratory allergy. European Federation of Asthma and Allergy Associations. 2000European Allergy White Paper. The UCB Institute of Allergy. Belgium, 1997Muilenberg M, Burge Harriet – Aerobiology. Lewis Publishers. USA. 1996Mc Michael A.J., Haines A., Sloff R and Kovats S. –Climate Change and Human Health. WHO/EHG/96.7 - WHO, WMO and UNEP, Geneva, Switzerland, 1996 Mandrioli P., Comtois P, Levizzani V. – Methods in Aerobiology. Pitagora Editrice. Bologna. Italy. 1998.
*****
6
Pollen allergy in EuropePollen allergy in Europe
Celso PereiraImmunoallergology DepartmentCoimbra University HospitalApartado 90573001-301 Coimbra / Portugale.mail: [email protected]
The first historical report related to pollens was in the 16th century, by Botal describing a patient with “aversion to roses”. It was only 200 years later that the seasonal disease was described by Hebergen. The methodology of Backley in 1873 was the ancestor of the pollen diagnosis and since that, it has been an increasing interest in these matter 1. The advances on aeropallinology, pollen counts, and pollen calendars are now widespread throughout Europe. There is much data available concerning pollen concentration of different species with a methodology that permit to compare the distinct national networks in Europe 2. It is very difficult to compare the different clinical studies available on literature, because of the heterogeneity of the design, the very discrepant samples, and the different aeroallergens tested. The Position paper published in 1998 is a relevant document that extensively analyses all the studies concerning pollen sensitisation in Europe 3.The EFA study, performed in 2000 4, showed the impact of the allergic diseases in 10 countries, and this information was consistent with the European Allergy White Paper contents 5. Pollen allergy is increasing throughout Europe in spite off a decrease in the grassland and tree land. It is also important to stress the changes related to the forest fires, the desertification, the agricultural methods and cultivation, the demographic pressure, the importation of non-natives species, etc.There are obvious differences concerning pollen allergy in Europe. In the 5 main geographic areas defined by G D´Amato, birch is the main pollen inducing sensitisation in the Artic and Scandinavia; birch, grasses and pollen from trees of deciduous forests in the Central area; grasses, mugwort and ragweed in the Eastern countries; grasses and pollen trees in the Central Mountainous areas; finally in the Mediterranean area the main pollens inducing allergic diseases are grasses, Parietaria, Olea and Cupressus 3.The ECRHS performed in 12 countries on individuals ranging from 20 to 44 years showed specific IgE levels to Phleum pratensis ranging from 3.8% in Ireland to 15.6% in Switzerland 6. In this country a large study performed in 9651 individuals, from 1991 to 1993, revealed similar values 7. The skin sensitisation to grasses was similar in adults and in children, 12.7% and 12.4% respectively.
7
In an interesting study of a cohort including 1456 subjects, in the Isle of Wight (UK) from 1989 to 1990 the children were submitted to skin prick tests at the age of 4 years 8. Sensitisation to grasses was 7.8% (981 out of 1218 individuals), and 40% of the children presented the diagnosis of bronchial asthma.Pollen allergy sensitisation was demonstrated in 1101 random children aged 8 to 11 years from Freiburg school (Germany). 19.7% were sensitised and the allergic rhinitis diagnosis was present in 8.7% of the sample 9. The rates of sensitisation were low in Sosnowiec, Poland, on a random sample of 2000 children, 10.3-10.8% 10.
A study performed in Wien (Austria), in adult individuals, showed sensitisation to grasses in 17% healthy individuals. Concerning allergic respiratory allergy, the SPT positive to grass pollen were highly increased in patients with rhinitis (60%) and bronchial asthma (33%) 11.In the allergic population attending an Allergy outpatient department, the values of pollen sensitisation are obviously higher. The allergic sensitisation are higher in urban than in rural areas. This issue depends on several factors, mainly the pollution, particularly vehicle emissions, and the increased concentration of ozone in the air 12. The risk is also increased in people living in towers at higher levels, and in urban areas with wide greenland zones 13.In patients allergic to pollen living in Budapest, the sensitisation to grasses and Ambrosia was respectively 67.6% and 59% 14, whereas in Warsaw, Poland, the major sensitisation was due to grasses (89%) and Artemisia (42%), respectively 15.Concerning asthma patients from Germany, the allergic sensitisations to grasses were higher in Hamburg (north) than in Erfurt, 24% and 19% respectively. Birch allergy was also higher in Hamburg (19%) than in Erfurt (8%) 16.Betulaceae importation to the south of Europe was responsible for the increase of sensitisations rates in Italy 17,18. There was an increase in Cupressus allergy in coastal region of Imperia (north Italy) besides the stabilization on pollen counts 18. The allergic patients from Rome, showed a similar pattern of sensitisation with an increased rate from 9.3% from 1994 to 1996 to 30.4% in 1999 19,20.The sensitisation to Cupressus pollen is more frequent in the Mediterranean area and is responsible for an increase of clinical symptoms of allergy such as conjunctivitis and cough, but can also be related to rhinitis and/or bronchial asthma 21. Parietaria is a widespread pollen in the south of Europe, mainly in the coastal areas reaching the highest ratios of allergic sensitisation, and inducing bronchial symptoms usually severe in adolescent and young adult patients. However, there is an obvious increase in children 21.Olea sensitisation is also common in the south of Europe,However,in a Swiss study performed in Locarno,53.9% of the pollen allergic patients were positive to this specie 22.Consecutive patients evaluation is one of the strategies that can permit to obtain the prevalence of aeroallergens in specific areas or countries with samples defined by the clinical epidemiology. The performance of SPT with a wide number of different allergens, according to
8
pollen counts and geographical particularities, allow obtaining a better vision of the sensitisation in specific populations.In 1995 the Spanish Allergologica study evaluated the allergic sensitisation in 10 regions 23. Grass pollen was the major allergen inducing allergic complaints with a prevalence ranging within 22% to 77%. Olea europea allergy was more frequent in the southern areas, related to the olive tree culture, being irrelevant on the north. Parietaria sensitisation ranged from 0.9% to 43.1%, being more frequent in the coastal southern areas. Allergy to Compositae (Artemisia vulgaris) and Chaenopodium pollen was reported to the southern regions and the continental northern area of Aragon.
An interesting study in Liguria, Italy, evaluated during 10 years the airborne pollen concentration and the skin sensitisation to aeroallergens 18. Parietaria, grass and Olea pollen allergy were the most prevalent in the sensitised patients, but there were no differences between the individuals living in the coastal areas and those living on the inland areas. Cupressaceae and Compositae sensitisation was also relevant, mainly in the coastal regions, probably related to the higher population density and the higher levels of particle pollutants 12.In Thessalonic, Greece, the Compositae sensitisation is frequent and corresponds to the 3 and 5 most prevalent pollen allergies, Chaenopodium (18.3%) and Artemisia (15.1%). Plantago was also a relevant pollen in this area and was responsible for 14.6% of sensitisations 25.An interesting prospective study was conducted in 5 centres (Isle of Wight, Vienna, Freiburg, Athens, and Kaunas) showed high sensitisation rates in Austria and UK and relatively low in Greece 26. Grass pollen was strongly associated with hay fever in all centers and with birch pollen in Austria and with Parietaria in Greece.Portugal is characterized by different geographical conditions associated to distinct patterns of the flora distribution and different botanical species. In allergic patients the grass pollen allergy ranges from 18.7% in Setúbal, (south coastal area), to 53.9% in Cova da Beira, in the inland central country 26. In pollen allergic patients the grass pollen is also the most important pollen in all studies. In Coimbra, a study performed in 100 patients allergic to grass pollen, revealed that the allergen that induced higher skin reactivity was Agrophyron repens, followed by Agrostis alba, Cynosurus c., Anthoxanthum, Poa pratensis and Lolium perenne.Madeira had the highest Parietaria sensitisation prevalence in Portugal, corresponding to 53.4% of a consecutive 100 allergic rhinitis patients. Most of them were also positive to grass pollen, the most prevalent allergen (61.3%) 27. Cova da Beira is an inland central region of Portugal, characterized by a dry hot summer and a cold rainy winter 26. This area had the highest pollen counts in Portugal and pollen allergy is frequent in allergic patients. Grasses, Parietaria and Olea were the 3 most prevalent allergens in urban areas, 54.6%, 34.6% and 33.3% respectively. In opposite, in the rural areas, a significant decrease on the same pollen sensitisation was observed, 42.6%, 16.6% and 27.5%, respectively. Compositae and Chaenopodiaceae sensitisation was also observed: Artemisia
9
vulgaris (13.4%), Chaenopodium album (6.7%) rectively. Plantago lanceolata was responsible for 12.7% of positive SPT in all patients. Sensitisation to pollens tree allergens, such as Robinia pseudoacacia, Platanus acerifolia, Tilia cordata, Pinus radiata and Betula pubescens had the following results: 6.4%, 5,8%, 4.9%, 4.4% and 4.3% respectively.In these area, sensitisation to pollens was also the most prevalent in children 28. Besides grasses, Parietaria judaica and Olea europeae were the most relevant pollen sensitisation even in children younger than 5 years: 43.5%, 23.4% and 19.8% respectively.Platanus allergy has an enormous importance in Madrid, Spain, 29 but this sensitisation can increase in other areas of the south of Europe, because it is being implemented as an ornamental tree in a lot of urban areas, as well as other highly allergenic species. Compositae and Plantaginacea are other families that are increasingly relevant in the allergic patients and could be important allergens in the next years.
There is an highly heterogeneity of sensitisation throughout Europe. The genetic, the climate, the geography, the native and the imported flora, the pollution and the demography are responsible for these different patterns. It is very important to design studies that could be compared and could be representative of the different countries or regions.The increase in allergic diseases in all Europe, particularly pollen allergy, must be an incentive to these kinds of studies. The Iberian Chapter of SLAAI will perform a study concerning the prevalence of aeroallergens sensitisation with the same methodology and representative for 2 countries: Portugal and Spain. It is highly recommendable that this kind of strategy could be enhanced and developed in a large number of Countries in Europe in order to obtain a better knowledge of the allergic sensitisation and reinforce the targets of interest implementing measures that could reduce the high risk of exposure to allergens.
References
1. Alergia y polinosis. In JM Giner, JSC García, CN Camacho, LO Llopis, AE Gea, FS Soto, JG Sellés, Eds. Polen y Alergias. Guia de las plantas de polen alergógeno de la Región de Murcia y España. DM, Librero-Editor, Murcia, Spain, 2001: 19-26.2. D’Amato G.,Spieksma F.Th.M.Bonini S. Allergenic pollen and pollinosis in Europe. Blackwell Science,Oxford,UK,19913. D’Amato G.,Spieksma F.Th.M.,Liccardi G. et al . Pollen-related allergy in Europe.Position Paper of the European Academy of Allergology and Clinical Immunology. .Allergy 1998;53:567-78.4. Respiratory allergy. European Federation of Asthma and Allergy Associations. 20005. European Allergy Wite Paper. The UCB Institute of Allergy. Belgium, 1997.6. Chinn S, Burney P, Sunyer J, Jarvis D, Luczynska C. Sensitization to individual allergens and bronchial responsiveness in the ECRHS. Eur Respir J 1999; 14: 876-84.
10
Wuthrich B. Epidemiology of allergies in Switzerland. Ther Umsch 2001; 58: 253-8Arshad SH, Tariq SM, Matthews S, Hakim E. Sensitization to common allergens and its association with allergic disorders at age 4 years: a whole population birth cohort study. Pediatrics 2001; 108: E33Riedinger F, Kuehr J, Strauch E, Schulz H, Ihorst G, Forster J. Natural history of hay fever and pollen sensitization, and doctor´s diagnosis of hay fever and pollen asthma in German schoolchildren. Allergy 2002; 57: 488-92.May KL. Allergy to Artemisia vulgaris in the region of Warsaw. Allergol Immunopathol (Madr) 1990; 18: 57-60.Zwick H, Popp W, Jager S, Wagner C, Reiser K, Horak F. Pollen sensitization and allergy in children depend on the pollen load. Allergy 1991; 46: 362-6. D’Amato G. Urban air pollution and plant-derived respiratory allergy. Clin Exp Allergy 2000;30:628-36.Mezei G, Jaraine KM, Medzihradszky Z, Cserhati E. Seasonal allergic rhinitis and pollen count (a 5-year survey in Budapest). Orv Hetil. 1995 Aug 6; 136: 1721-4. May KL. Allergy to Artemisia vulgaris in the region of Warsow. Allergol Immunopathol (Madr) 1990; 18: 57-60.Nowak D, Heinrich J, Jorres R, et al. Prevalence of respiratory symptoms, bronchial hyperresponsiveness and atopy among adults: west and east Germany. Eur Respir J 1996; 9: 2541-52.17. Moverare R, Westritschinig K, Svensson M, et al. Different IgE reactivity profiles in birch pollen-sensitive patients from six European populations revealed by recombinant allergens: an imprint of local sensitization. Int Arch Allergy Immunol 2002; 128: 325-3518. Ariano R, Passalacqua G, Panzani R et al. Airborne pollens and prevalence of pollinosis in westetern Liguria: a 10 year study. J Investig Allergol Clin Immunol 1999; 9: 229-34.Sposato B, Mannino F, Terzano C. Significant increase of incidence of cypress pollen allergy in the city of Rome. Recenti Prog Med 2001; 92: 541.20. Papa G, Romano A, Quarantino D, et al. Prevalence of sensitization to Cupressus sempervirens: a 4-year retrospective study. Sci Total Environ 2001; 270: 83-7 22. Frei T, Torricelli R, Peeters AG, Wuthrich B. The relationship between airborne pollen distribution and the frequency of specific pollen sensitisation at two climatically different locations in Switzerland. Aerobiologia 1995; 11: 269-73.23. Alergologica. Factores Epidemiológicos Clínicos y Socioeconómicos de las enfermedades alérgicas en España. SEAIC. Nilo Industria Gráfica, Madrid, Spain. 1995Gioulekas D, Papakosta D, Damialis A, Spieksma F, Giouleka P, Patakas D. Allergenic pollen records (15 years) and sensitization in patients with respiratory allergy in Thessaloniki, Greece Allergy 2004; 59: 174-84.Loureiro G, Blanco B, São Braz MA, Pereira C. Reactividade cutânea a aeroalergénios numa população alérgica da Cova da Beira. Revista Portuguesa de Imunoalergologia 2003; 9: 107-16.
11
27. Oliveira S, Camara R, Camara I, Carvalho M, Borges F. Pollen sensitisation prevalence on rhinitis patients- immunoallergology attendance- Funchal Hospital. Allergy 2003; 58 (suppl 74): 395.28. Pereira C, Loureiro G, São Braz MA, Blanco B. Aeroallergens sensitization in allergic paediatric population of Cova da Beira, Portugal. Differences concerning environment exposure. Allergy 2003; 58 (suppl 74): 148.29. Varela Losada S. Polinosis por Platanus. Alergología e Inmunología Clínica 2003; 18: 81-5.
*****
GRASS POLLEN ALLERGENSGRASS POLLEN ALLERGENS
Marta Orta, M.D, Elena Ordoqui, M.D.Centro Médico de Alergia y AsmaPamplona (Spain)E-mail: [email protected]
The botanical group of Poaceae is one of the most numerous in Nature, comprising nearly 700 genus and about 12.000 species. Grasses account about 20% of plant life in the planet, being useful as basic food source for animals (pasture) and humans (cereals).In Table I (1) components of Gramineae family are shown, distinguishing Cynodon as the only one of allergenic interest not included in subfamily Pooideae.
TABLE I- GRAMINAE FAMILY
Family Subfamily Tribe Genus Species Common name
(Spanish)Lolium perenne Centeno silvestre
Poeae Dactylis glomerata Caracolillo(Festuceae) Festuca pratensis Cañuela
Poa pratensis Espiguilla
Agrostidae Phleum pratense Hierba timotea
Alopecurus pratense Cola de zorro
Agrostis alba Rastrero12
POOIDAE Avena sativa AvenaGRAMINEAE (Festucoideae) Aveneae Holcus lanatus Heno-lanota
Anthoxantum odolatun Grama de colorPhalariss acuatica Hierba
canariaArrenatherumelatius AvenillaTrisetum flavescens Falsa
avena
Triticeae Triticum sativum TrigoSecale cereale CentenoHordeum vulgare Cebada
Arundinae Agrospyron cristatum Grama de botica
Phalarideae Phragmites communis Carrizo
Bromeae Anthoxantum odoratum Grama de olor
Chlorideae Bromus inermis Espiguillas
CHLORIDOIDEAE Andropogoneae Cynodon dactylonGrama común
PANICOIDEAE Maydeae Sorghum helepnse SorgoZea mays Maíz
Wild grasses are a common cause of allergy in Europe. The best known are Cocksfoot (Dactylis glomerata), Timothy grass (Phleum pratense), Kentucky blue grass (Poa pratensis) and Lawn (Cynodon Dactylon), all easily distinguishable in ditches, meadows or embankments.
Grass pollen grains have a granulated surface, with one single pore. There’s a high cross reactivity between different genus of Poaceae. They have about 20-45 m diameter, permitting the entrance quite deep into the airways, through the aerosolization of little sized particles of about 0.6 to 2.5 m. Each pollen grain spreads over 700 starch granules where allergens responsible of sensitization and symptoms are vehicled (2).
Fig. 1 Fig. 2Optical microscope pollen view Electronic microscopic pollen view
13
There are different maps of pollinisation in Europe, here represented the peaks of pollinisation of grasses during April, May and June, although due to the huge number of species of Poaceae known, pollen can be found in the air over 6-10 months of the year depending on different areas.
Fig. 3
www.alergiainfantillafe.org
It’s been calculated that patients sensitized can have symptoms with a concentration from 10 to 50 grains of grass pollen, depending on the particular severity of the allergy of each patient, the concomitance with other allergies to plants pollinating at the same time, weather conditions or level of exposure (for example higher levels when cutting the lawn). The recognized allergens are usually the most numerous or the most sensitizing. A major allergen is defined because of its higher prevalence or the increased IgE percentage against it in a determined population. The standarization methods are usually directed to their detection, so that polisensitized patients can suffer a misdiagnosis or a therapeutic failure for that reason. Major allergens are usually more specific while minor usually include several panallergens responsible for most phenomena of cross reacting among pollens and vegetable foods (3).
Table II resumes what actually known about grass pollen allergens, where Lolium and Cynodon species are the most studied. There are more than 12 allergen families identified in grasses. Two majoritary allergens (Groups 1 and 5) and two panallergens responsible of cross reacting (Groups 7 and 12) are the best known (1) although there is a variety of proteins of different sizes, structures and physicochemical properties existing as multiple isoforms (3).
TABLE II- GRASS POLLEN ALLERGENS14
Pollen Allergen Biologic function Mw(kDa) Sequency IgE prevalence(%)C dactylon Cyn d 1, 7, 12
7 Calcium binding 12 C 10 12 Profilin 14 C 20
D glomerata Dac g 1, 2, 3, 5
H lanatus Hol l 1 34 C 67 Hol l 5 30 C 64
H vulgare Hor v 5 30 C +
L perenne Lol p 1, 2, 3, 5, 10, 11 10 Citochrome C 12 P - 11 Trypsine inhibitor 16 C 65
O sativa Ory s 1 35 C +
Ph aquatica Pha a 1 34 C 77 Pha a 5 31-33 C 42
Phl pratense Phl p 1, 2, 4, 5, 6, 7, 12, 135 Ribonuclease 32-38 C 806 P particle associated 13 C 757 Calcium binding 6-8 C 1012 Profilin 14 C 2013 Poligalacturonase 55-60 C 50
P pratensis Poa p 1, 5, 1010 Citochrome C 12 P -
S halepense Sor h 1 35 C +
Z mays Zea m 1 Expansine 17-33 C + Zea m 12 Profilin 14 C +
Grass pollen allergens 1 and 5
They are recognized by about 80-90% of people sensitized to grass pollen having specific IgE against them. The recognizition of only one grass species seems to be sufficient for in vitro diagnosis of grass pollen allergy. With purified Lol p 1 and Lol p 5, many more than 50% of grass positive sera are detected. Around 80% of the IgE response to grass pollen is directed to these major allergens as it has been shown in inhibition assays (4).
Grass group 1 pollen allergens are 27-35 kDa glycoproteins, functionally belonging to the group of - expansins (5). The different species show a high homology (Lol p 1 is very similar to Phl p 1 as an example), not so evident in other species such as Cynodon, where Cyn d 1 is only 50% similar to Lol p 1. This fact and the apparent absence of Cyn d 5, show specific sensitization
15
patterns for Cynodon dactylon. - expansins are defined by their characteristic sequence and by their unique rheological effects on plant cell walls, which include the rapid induction of cell wall extension and the enhancement of wall stress relaxation. These proteins (divided into and families) are believed to be the key catalysts of cell wall loosening, necessary for plant cell growth, cell separation (abscission) and other related processes (studies done over Zea m1 allergen). - expansins are more common than , presenting a high concentration, solubility and a weak interaction with cellular walls, what lets them to be more allergenic because of their high biodisponibility (6).
Grass group 5 allergens seem to be exclusive of the Poaceae subfamily. Their molecular weight is 28-40 kDa, not having any glycosilation in its molecule. They have RNAse activity and are suggested to participate in defense reactions of the plant (7). The more relevant characteristic of this group of allergens is the high presence of different allergenic isoforms. Data obtained from studies in Phleum show there are two separate groups of isoallergens Phl p 5a (31 kDa) and Phl p 5b (28 kDa). Although there not seems to be any difference among isoforms when binding IgE, there are studies where different T cell recognition patterns have been found, what can be interesting to develop different therapeutic strategies based on recombinant allergens (8). Their concentration in the pollen grain is high and they are weakly associated to starch particles in aerosols what enhances their allergenicity.
Grass pollen panallergens
Two big groups can be distinguished:- Group 7: calcium-binding proteins.- Group 12: profilins
Calcium-binding proteins (group 7)
The group is integrated by 32 subfamilies, having from 2 to 8 calcium-binding sites, and present in different vegetal species. Their capacity of binding calcium (Ca++) makes them different whether it is in the molecule or not. Phl p 7, proved to be a primary sensitizing allergen from inhibition studies (9), and Cyn d 7 are the two better known allergens, although only 10 to 20% of the grass pollen allergic patients are sensitized to them. They seem to be clinically relevant, responsible for high cross reacting with other pollen antigens. They are also considered to be homologous with some human proteins, being able to cause autoimmune diseases with IgE production such as severe atopic dermatitis (10).
Profilins (Group 12)
16
They are present in many biological systems, having a relevant role in actin-binding regulation, although not yet completely understood (11). They have been proved to mediate in the grass pollen tube growth, but only about 20% of patients are sensitized to them as an allergen. They are considered as extremely ubiquitous, present in different tissues such as storage ones, and possibly responsible of cross-reacting between pollen and vegetable foods as Rosaceae or legumes (12). The photo shows the molecular model of the Phleum profilin (Phl p 11), courtesy of Bial-Aristegui R+D department (Bilbao, Spain).
Fig 4.
Other relevant allergens
There are sometimes IgE binding carbohydrates of the antigenic molecule, which can explain some other cross-reacting phenomena, due to the fucose and xylose residues not present in mammalian molecules, although their clinical relevance remains still unknown (13).
Bibliography
1.- Barber D. Gramíneas: alergenos y reactividad cruzada. Alergología e Inmunología Clínica 2003; 18: 12-16.2.- Taylor PE, Flagan RC, Valenta R et al. Release of allergens as respirable aerosols: Alind between grass pollen and asthma. J Allergy Clin Immunol 2002; 109: 51-56.3.- Andersson K, Lidholm J. Characteristics and immunobiology of grass pollen allergens. Int Arch Allergy Immunol 2003; 130: 87-107.4.- Van Ree R., Van Leeuwen WA, Aalberse RC. How far can we simplify in vitro diagnostics for grass pollen allergy?: A study with 17 whole pollen extracts and purified natural and recombinant major allergens. J Allergy Clin Immunol 1998; 102: 184-190.
17
5.- Grobe K, Becker WM, Schlaak M et al. Grass group I allergens (β- expansins) are novel, papain-related proteinases. Eur J Biochem 1999; 263: 33-40.6.- Cosgrove DJ. Cell wall loosening by expansins. Plant Physiol 1998; 118: 333-339.7.- Bufe A, Schramm G, Keown MB et al. Major allergen Phl p Vb in timothy grass is a novel Rnase. FEBS Lett 1995: 363: 6-12.8.- Würtzen P, Wissenbach M, Ipsen H et al. Highly heterogeneous Phl p 5- specific T cells from patients with allergic rhinitis differentially recognize recombinant Phl p 5 isoallergens. J Allergy Clin Immunol 1999; 104: 115-122.9.- Tinghino R, Twarsdosz A, Barletta B et al. Molecular, structural and immunologic relationships between different families of recombinant calcium-binding pollen allergens. J Allergy Clin Immunol 2002; 109: 314-320.10.- Valenta R, Natter S, Seiberler S et al. Isolation of cDNAs coding for IgE autoantigens: a link between atopy and autoimmunity. Int Arch Allergy Immunol 1997; 113: 209-212.11.- Rothkegel M, Mayboroda O, Rohde M et al. Plant and animal profilins are functionally equivalent and stabilize microfilaments in living animal cells. Journal of Cell Science 1996; 109: 83-90.12.- Vidali L, McKenna ST, Hepler PK. Actin polymerisation is essential for pollen tube growth. Mol Biol Cell 2001; 12: 2534-2545.13.- Van Ree R. Carbohydrate epitopes and their relevance for the diagnosis and treatment of allergic diseases. Int Arch allergy Immunol 2002; 129: 189-197.
*****
Oral Allergy Syndrome (OAS)Oral Allergy Syndrome (OAS)
Philippe GEVAERT, MD PhD
Oral Allergy syndrome (OAS; also known as pollen-food allergy syndrome) is a symptom complex almost exclusively localized to the oropharynx and is a “mucosal equivalent of urticaria. The syndrome is usually caused by certain fresh fruits and vegetables in individuals who are sensitive to pollens, but also occurs in subjects allergic to shell-fish and eggs. Typical symptoms of OAS include itching of the mouth and/or throat, and swelling of the lips. Rarely, oedema of the glottis and systemic anaphylaxis may occur.
18
Prevalence
In an initial report, Amlot1 reported about 80 adult food-allergic patients who were experiencing frequent symptoms of oral irritation and throat tightness. One fifth of the patients experienced other symptoms of food allergy (gastro-intestinal, respiratory, or cutaneous) immediately following the initial oral symptoms on at least one occasion. Another study reported that approximately 35% of patients with pollen allergy were also sensitive to fresh fruits and vegetables2. Subsequently, Ortolani3 described 262 patients with OAS, most of whom had allergic rhinitis. Foods most commonly implicated were fruits, nuts and vegetables (i.e. apple 53%, peach 40%, hazelnut 37%).
PathogenesisCurrently, it is believed that the local oral symptoms in OAS are caused by a high concentration of mast cells in the oropharyngeal mucosa. Interaction between specific IgE found on the surface of these cells and allergens rapidly released from the offending food or fruit might explain the early onset of OAS symptoms.
Cross-reactivity
OAS is an IgE-mediated allergy caused by homologous proteins and cross-reacting antigenic determinants in pollen and various fruits, vegetables, and nuts. Birch sensitive patients frequently react to fresh apple, hazelnuts, cherry, celery, and carrot, whereas ragweed-sensitive patients might react to banana, kiwi, and melons. On the one hand, synthesis of IgE stimulated by a cross-reactive allergen in pollen can result in a diverse pattern of sensitisations against various foods. On the other hand, even anaphylactic reactions may occur after consumption of a food containing a cross-reactive allergen for the first time. Frequent cross-reactivity was observed within botanical families (e.g. apple and pear; melon, apricot, peach and plum), and with certain aeroallergens, especially birch and grass pollens.
Table I. Clusters of hypersensitivity- Hazelnut, walnut, brazil nut, and almond reciprocally, and even nuts combined with apple
and stone fruits. - Apple and pear - Kiwi fruit and avocado - Potato-and carrot - Parsley and celery - Celery, mugwort and spices - Apple, carrot and potato - Cherry and apple - Melon, watermelon and tomato - Lettuce and carrot
19
- Tomato and peanut - Celery, cucumber, carrot and watermelon
Molecular biology-based approaches have also improved knowledge about cross-reactivity among allergens4. The identification of allergens in fruits and vegetables showed IgE cross-reactivities with the important birch pollen allergens, Bet v 1 and Bet v 2 (birch profilin). Many other cross-reactive antigens have also been identified and characterised. Depending on the main cross-reactive allergen, different symptoms may be observed. Bet v 1 in apples, cherries, peaches and plums primarily causes mild symptoms such as the oral allergy syndrome. However, Bet v 1 associated with other allergens may cause generalised symptoms. Sensitisation to Bet v 2 is more often associated with generalized symptoms, in particular urticaria and angioedema. Lipid-transfer proteins are relevant apple and peach allergens and, considering their ubiquitous distribution in tissues of many plant species, could be a novel pan-allergen of fruits and vegetables.
Diagnosis
Evaluation of a patient with pollen-food allergy syndrome should include a careful history to determine the triggering foods and characteristics of the reactions, diagnostic tests that might include skin prick testing with fresh, raw, or both fruits (although this is not standardized), and possibly oral food challenges5;6.
Management
For patients with mild pollen-food allergy syndrome, treatment should be individualized with understanding that the risk of progression to a severe reaction is not known. As with other manifestations of food allergy, the mainstay of treatment in OAS is strict avoidance of the offending food. Elimination need not be lifelong as the natural history of food allergy, especially in children, is gradual loss of sensitivity to most food including fruit and vegetables. As tolerance seldom develops to fish and nuts, it is recommended that these foods be avoided permanently if implicated in OAS. Drug therapy (antihistamines, adrenaline) may be necessary to treat angioedema or anaphylaxis. Treatment of atopic problems due to the associated pollen allergy (e.g. allergic rhinitis, asthma is also necessary. A few open studies have demonstrated the therapeutic potential in pollen-related food allergy: in at least 50 % of the cases, tree pollen immunotherapy led to an improvement of associated food allergies. However, these results have to be confirmed in placebo-controlled studies. Further studies to define clinical features and the natural course of pollen-food allergy syndrome and the development of improved diagnostic tests will be necessary to develop a more specific approach for the diagnosis and management of these patients. As we are facing an increase of pollen allergies, a shift in sensitisation patterns and changes in nutritional habits, the occurrence new, unknown cross-reactions is expected.
20
References
1. Amlot PL, Kemeny DM, Zachary C, Parkes P, Lessof MH. Oral allergy syndrome (OAS): symptoms of IgE-mediated hypersensitivity to foods. Clin Allergy 1987; 17(1):33-42.
2. Bircher AJ, Van Melle G, Haller E, Curty B, Frei PC. IgE to food allergens are highly prevalent in patients allergic to pollens, with and without symptoms of food allergy. Clin Exp Allergy 1994; 24(4):367-374.
3. Ortolani C, Ispano M, Pastorello E, Bigi A, Ansaloni R. The oral allergy syndrome. Ann Allergy 1988; 61(6 Pt 2):47-52.
4. Bousquet J, van Cauwenberge P, Khaltaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 2001; 108(5 Suppl):S147-S334.
5. Ma S, Sicherer SH, Nowak-Wegrzyn A. A survey on the management of pollen-food allergy syndrome in allergy practices. J Allergy Clin Immunol 2003; 112(4):784-788.
6. Osterballe M, Scheller R, Stahl SP, Andersen KE, Bindslev-Jensen C. Diagnostic value of scratch-chamber test, skin prick test, histamine release and specific IgE in birch-allergic patients with oral allergy syndrome to apple. Allergy 2003; 58(9):950-953.
*****
SAMPLING TECHNIQUES FOR BIOAEROSOLSSAMPLING TECHNIQUES FOR BIOAEROSOLS
Rui BrandaoUniversidade de Évora, Portugal
Bioaerosols consists of particles of biological origin or activity finely divided and suspended in the air or other gaseous environment. Particle sizes may range from aerodynamic diameters of ca.0.5 to 100 m and they may affect living things through infectivity, allergenicity, toxicity, pharmacological or other processes [Cox et al., 1995].
In general, the first aim of sampling bioaerosols is to determine which species within some selected group are present and how their atmospheric concentration changes. Some
21
sampling strategies include surveys over space, time, or both and often complex processes are required to identify the collected material.
Many devices are in use for sampling airborne particles and they differ according to several sampling principles (gravitational settling, filtration, electrostatic precipitation, etc). There is no universal sampler and each field of application has developed its own sampling methods. Therefore a sampling device or method should be selected only after the purpose of sampling has been established, the characteristics of the particles are known, and the methods for handling the samples chosen.
The athmospheric physicist and aerobiologist P. Mandrioli had systematized recently, in a clear and practical way, the diversity of equipments and sampling devices according to 2 main classes[Mandrioli et al., 1998]:
1) Deposition Samplers: based on simple methods of collecting bioaerosols through an exposure of a horizontal surface for particle gravitational settling. Particles settle at their terminal velocity and are retained by an adhesive on the sampling surface. Ex: Durham and Tauber traps and Petri dishes
2) Impaction Samplers: includes a wide spectrum of devises that have in common a impaction sampling on a solid surface. There are several classes namely:
- Suction samplers in which air containing the material to be sampled is drawn through an orifice usually by suction from a vacuum pump. Examples: 1 to 7 Day Recording Volumetric Spore Trap; Airborne Bacterial Sampler MK-ll; Surface Air System SAS; Slit-to-agar impactor sampler;
- Cascade impactors are suction samplers composed of one or more deposition surfaces. In the most widely utilised device, particles are deposited on Petri dishes with nutrient media for culture of the viable fraction. In other models, particles are impacted on glass or stainless steel collection plates allowing observation and analysis. Examples: Andersen Microbial Air Sampler; Marple Personal Cascade Impactor; Marple 290 Personal Cascade Impactor; Burkard personal sampler.
- Filter samplers: Filtration is the commonest method for removing particles from the air drawn in by suction. The air passes through a fibrous or porous medium that impacts or sieves the particles. They have the advantage of a high particle retention capability both on the surface and inside the filtration mass, and the disadvantage of an undefined pore diameter and retention of particles within the filter depth. Examples: Filter cassettes made by several manufacturers; Cour Samplers used in some mediterranean countries namely at the Portuguse Aerobiology Network in the year of 1999-2000;
22
- Inertial samplers: In these devices the impaction surface is in motion rather than the particles. The most famous is the Rotorod Sampler developed at the Stanford Research Institute;
- Cyclone Samplers in which particle discrimination is carried out thanks to the centrifugal force generated either by the rotating air mass or by the spiral trajectory in which they are forced to move. Example: Cyclone sampler manufactured by Burkard Manufacturing Co., Ltd, Hertfordshire, U.K. ;
- Liquid impingers operate by drawing a stream of air into the bottom of a container of liquid and allowing it to rise through the liquid as buoyant bubbles. During the process particles are transferred to the liquid and retained. These instruments have been recommended for sampling delicate organisms such as algae. Examples: The All Glass Impinger (AGI-30) sold by Ace Glass; The Burkard Multi-stage liquid impinger by Burkard Manufacturing Co., Ltd, Hertfordshire, U.K.
SAMPLING TECHNIQUES FOR AIRBORNE POLLEN
The Hirst spore trap (Hirst, 1952) is the standard sampler to record the atmospheric concentration of pollen grains and fungal spores. It is a suction sampler based on the basic principle of the impaction, with a 2x14 mm intake orifice through which the sampled air is impacted onto a collection surface moving at 2 mm h-1.
The most used commercial models available at the present time are the Burkard Volumetric Spore Trap designed by Burkard Manufacturing Company Limited UK and the VPPS 2000 Volumetric Spore Trap designed by Lanzoni S.R.L. Italy. These samplers have the possibility to run for a week or to incorporate a daily mechanism. The air flow exhaled is 10 litres per minute.
Recently, some portable personal sampling devices have been designed to do samples in any place without power supply. The most used commercial models are those designed by Burkard Manufacturing Co. with the Personal trap, by Lanzoni S.R.L. Italy with the VPPS 1000 model, and by Coppa S.R.L. Italy, with the Partrap FA52. The air flow is the same as the Hirst type sampler.
The Hirst sampler designed by Burkard Co. or Lanzoni S.R.L. (they have the same sampling features) and in use at the Portuguese Aerobiological Network or other European networks consists of a impaction unit which consists of an adhesive-coated transparent tape (a Melinex tape) placed on a drum rotating once every 7 days, a wind-vane mounting unit and the
23
motor housing unit (figure 1). A vane tail keeps the cylindrical housing facing the wind. The motor housing contains a vacuum pump and equipment for measuring the rate of suction.
Adhesive coatings
Currently a wide variety of adhesives exist which are used in different places for aerobiological sampling with such samplers: vaseline, petrolatum white, silicone fluid, and a mixture of vaseline and parafine. Moreover, other adhesives in use are glycerol, glycerol jelly and gum resins.
It is very important to use an adhesive that does not vary with different meteorological conditions. Some comparative studies have already been done using different media in order to evaluate the efficiency and the possible standardization of their use, (Kapyla, 1989; Galan and Dominguez-Vilches, 1997).
It could be inferred from the results of these studies that the differences which exist between the efficiency of one adhesive or another are normally small and depend on the local climatic conditions (Galan and Dominguez-Vilches, 1997).
Drum preparation
In weekly samplers the Melinex tape is mounted on a drum (figure 1). The Melinex tape is 336 mm long which correspond with the seven days of a week. Ones the tape is on the drum then the adhesive must be applied with the aid of a brush. If a vaseline is used the person who is mounting the tape apply it by slightly and continuously turning the drum without stopping ensuring that a very fine and uniformed layer is obtained. In the case of silicone fluid let the brush slide slowly only once and exclusively in one direction. It does not matter the thickness of the layer of silicone because within 30 sec the tape dries and it is ready to be used.
24
Lid Assembly
Rotation lock
Build-in Motor
Wind vane
Trapping surface
Lid
Start reference pointer
Figure 1: The Burkard 7-Day Volumetric Spore Trap (left) with Lid Assembly with drum (right) [adapted from “A Guide to Trapping and Counting, The British Aerobiological Federation]
Slide mounting
As the drum rotes at a 2 mm per hour, and the Melinex tape is 336 mm long, the operator must cut in the laboratory seven 48 mm pieces (each one corresponds to one day) with the aid of a transparent ruler. These pieces of tape are mounted on the slides with a mounting media (a diagram of this process can be visualized at http://www.rpa.uevora.pt). The most frequent mounting media are: glycerol jelly, polyvinyl alcohol, polyvinyl lactophenol. It is important to add phenol to this media to avoid microbial growth [Galán, 2001]. In the case of pollen grain collection, basic fucsin is often used to stain the samples.
Site location
Three main criteria should be considered when one choose the sampling site: 1) it should be representative, 2) accessible and 3) within reach of a power supply. The sampler should be positioned on a site where local air circulation is not influenced by nearby obstacles, preferably in the middle of a roof terrace at a height of 15-20 m above ground level and far from walls and rails [Mandrioli, 1998]. Site specifications and its surrounding vegetation should be taken into due account in the interpretation of aerobiological results, because some particular situations could lead to pollen overload. Since aerobiological studies have been traditionally applied to allergy, most of the samplers are placed under urban conditions, on the top of hospitals or other public buildings. However, the urban climate features special temperature regimes and air flows in cities that we must take into account when a sampler is installed
The terrain nature will have a great influence on the air flow. Solid obstacles projected into the wind cause eddies which may break away from the surface and travel down wind. The
25
roughness of the ground produces a certain amount of turbulence in the lowest layer of the atmosphere which promotes the mixing and dispersion of particles. This effect will be greater for a city with lot of buildings than for an open ground with few obstructions in a rural area [Galán, 2001].
Another factor is the location of the sampler in respect to the particle source. A sampler closer to ground level detects higher concentrations of pollen from plants close to the sampling site, while a sampler situated higher above ground level detects pollen grains from a wider ranging area.
In a rural area, the researchers must consider the topographic wind effects. The sampler must be installed in an open place and the interpretation of the sampler results depends on the topography of the site: the coast, with land and sea breezes, the mountains and valleys with local wind systems, etc
REFERENCES
British Aerobiology Federation (1999) – Airborne Pollen and Spores: A Guide to Trapping and Counting. Edit. by National Pollen and Hayfever Bureau, Rotherham, U.K.
Cox, C.; Wathes, C. (1995) – Bioaerosols Handbook. CRC Press Inc., 621 p.Galán, C.(2001) – The Use of the Hirst Volumetric Trap: operation, adhesive coatings, drum
preparation, slide mounting and Site location (printed material for didactical purpose), Universidad de Córdoba, Cordoba.
Galán, C.; Domínguez-Vilches, E.(1997) – The capture media in Aerobiological Sampling. Aerobiologia, 3(3)
Käpilä, M.(1989) – Adhesives and mounting media in aerobiological sampling. Grana 28:215-218
Mandrioli, P.; Comtois, P.; Levizzani, V.(1998) – Methods in Aerobiology. Pitagora Edit. Bologna, 262p.
*****
MOULD SPORE COUNTS IN FUNCHAL MOULD SPORE COUNTS IN FUNCHAL 2003-2004 YEARS STUDY2003-2004 YEARS STUDY
26
Sofia Camacho1, Irene Câmara1, Rita Câmara2, Susana Oliveira2, Miguel Pinheiro de Carvalho1, Fernando Drummond Borges2.
1Centro de Estudos da Macaronésia (CEM), Universidade da Madeira.2Unidade de Imunoalergologia, Hospital Central do Funchal.
Background: Aerobiological and epidemiological research has been made in Funchal till now in order to detect pollen and fungi airborne and the prevalence of allergic disease.Purpose: Analysis of airborne fungal spores observed in Funchal city during one-year study.Methods: Aerobiological records of mould spores were conducted by a Burkard sampler between April 2003 and March 2004. Parallel records of meteorological parameters were obtained at Meteorology Institute and correlated with aerobiological data.Results: The fungal counts obtained during the study were equalled 11.862 spores/m3/year. Three main classes were identified: Deuteromycetes (55,4%), Ascomycetes: (23,0%) and Basidiomycetes: (20,6%). Cladosporium, Torula, Fusarium and Alternaria were the most prevalent Deuteromycetes, whereas Leptosphaeria (Ascomycete) and Coprinus (Basidiomycete) were the most frequent types within their class. Despite the maximum number recorded being during springtime, there is a continuous presence of sporomorphs in the atmosphere all the year round. The relation between airborne fungi variation and daily climatic factors, namely temperature and relative humidity was shown.Conclusion: The tendency to an increasing number of airborne fungi every year could be explained by meteorological and outdoor conditions. An integrative analysis of aerobiological data, epidemiological studies and the influence of environment should provide a better approach of the allergic disease.
*****
ENVIRONMENTAL CHARACTERIZATION AND ALLERGICENVIRONMENTAL CHARACTERIZATION AND ALLERGIC DISEASE DISEASE IN MADEIRA ISLANDIN MADEIRA ISLAND
Susana Oliveira1, Rita Câmara1, Irene Câmara2, Mariana Rodrigues3, Mário Morais Almeida4, José Rosado Pinto4 Fernando Drummond Borges1.1Immunoallergy Unit 3Statistic and Research Department – Funchal Hospital (HCF), 2Biology Department – UMa, 4Immunoallergy Department – Dona Estefânia Hospital.
27
Background: Interaction between meteorology, outdoor / indoor characteristics and genetics predisposition for the allergic disease condition the disease prevalence. Purpose: Environmental characterization: meteorology, aerobiology, airborne pollution and indoor conditions in order to find an explanation to the atopy and allergic disease prevalence. Methods: Analysis of thirty-year meteorology, airborne pollen and mould sampling (Burkard), airborne pollution studied on the context of ISAAC and indoor conditions studied during PAC-Study. Results: Madeira has a subtropical climate with low temperature amplitude; mean annual temperature – 19,5ºC (maximum mean temperature – 22ºC and minimum mean temperature – 17ºC) and a moderate rainfall. Year round there’s high mean relative humidity of 67%. The airborne level spores mould varies between 6584 to 11925 spores/m3/year.
Deuteromycetes is the most prevalent class, and in this class Cladosporium type is the most prevalent. Highest incidence of mould spores occurs on springtime. The most prevalent pollen families are Urticaceae and Pteridophyta with a mean grain pollen/m3/year = 1246. The highest pollen concentration occurs on springtime and autumn. Regarding pollution we have mean NO2
level = 22,5 g/m2 air. Indoors conditions characterization: mean temperature = 21ºC, mean relative humidity = 74% and house dust mite concentration shows Der p1 higher than Der f1. Mean of house dust mite concentration found was for mattress Der p1 = 19,76 g/g of dust, Der f1 = 0,30 g/g of dust; and for floor: Der p1 = 2,11 g/g of dust, Der f1 = 0,08 g/g of dust. Conclusion: The outdoor conditions, namely subtropical climate, significant level of pollen, mould spores and NO2, corroborated by indoor conditions, like high relative humidity and dust mites concentration, enhance the 1genetic predisposition supposed by the frequency of HLADr B1*7 found in this population, for house dust mites atopy (general population = 50% and asthmatic population = 80%) and allergic disease prevalence (asthma = 14% and rhinitis = 20% - ISAAC – 1st phase).
1Spínola H, Brehm A, Williams F, Jesus J, Middleton D (2002). "Distribution of HLA alleles in Portugal and Cabo Verde. Relationships with the slave trade route". Annals Hum. Genet. 66: 285-296. *****
INDOOR CHARACTERIZATION – AEROALLERGENSINDOOR CHARACTERIZATION – AEROALLERGENS SENSITIZATIONSENSITIZATION
28
Susana Oliveira1, Rita Câmara1, Maria João Castro1, Mariana Rodrigues2 Fernanda Vila3, Cátia Cardoso3; Ana Carvalho Marques3; Fernando Drummond Borges1.1Unidade de Imunoalergologia, 2Serviço de Estatística e Apoio à Investigação, 3Serviço de Pediatria – Hospital Central do Funchal.
Background: Indoor home conditions of allergic patients associated with an increased sedentary life style, could be a trigger for allergic illness. Purpose: Indoor characterization from Immunoallergy outpatients and correlation with their atopy incidence. Methods: Questionnaire systematic application in order to characterize indoors conditions of Immunoallergy outpatients. Skin Prick Test (SPT) with commercial extracts (dust mites, moulds and cockroach). Statistic analysis and correlation between indoor conditions and sensitization was done. Results: Patients population: n=193. Male – 47,7% and female – 52,3%. Mean age = 15 years old (8 months – 80 years). Home place: urban, suburban and rural, equitable distribution. Basic sanitation inexistent in 10% (n=20) of the population. House floor was predominantly: wood (44%) and mosaic (40,4%). Only 4,1% (n=8) of the individuals bedroom have carpet. The majority of the houses has 2 or 3 sleeping rooms and almost of the population shares the room with one more person. In average the mattress has 5 years, it is predominantly springs (90,2%) and is not shared in 81,1% of cases. Pillow is used by 89,6% of patients, whose average age is 3 years, and being scum in 51,8% of cases. The eider down is used by 61,7% of the population. In almost half of patient room there are soft toys (n=90) in number >=5 (47,8 %). Indoor humidity is present in 57,9% and cockroach in 48,2 % of houses. In studied population 75% have SPT positive to at least one tested allergen. Positive sensitization was: house dust mite 77,2% cockroach 26,2% and mould 23,4%. For allergens like house dust mite the only significant Pearson correlation founded was for >=5 soft toys (<0,001) indoor. There were not found other significant correlation to this allergen or between indoor humidity and mould sensibilization. Pearson correlation was significant (<0,001) for home occurrence cockroach and positive SPT to this aeroallergen. Conclusion: Incidence for sensitization to the tested aeroallergens was similar to that found in PAC-study. The reason for no significant Pearson correlation between other indoor conditions beside soft toys >5 and house dust mite sensitization could be explained by some previous environment control already done. Finally, the inexistence of significant correlation between indoor humidity and moulds atopy could be explained by the lacking of moulds standardized extracts for prick test and regional variation. The correlation found for indoor cockroach and sensitization for this specific allergen could be justified, in one hand by high prevalence of indoor cockroach and in another hand, by extermination difficulties.
*****
29
MOLD SPORE COUNTS IN FUNCHALMOLD SPORE COUNTS IN FUNCHAL 2003-2004 YEARS STUDY2003-2004 YEARS STUDY
Sofia Camacho1, Irene Câmara1, Rita Câmara2, Susana Oliveira2, Miguel Pinheiro de Carvalho1, Fernando Drummond Borges2.
1Centro de Estudos da Macaronésia (CEM), Universidade da Madeira.2Unidade de Imunoalergologia, Hospital Central do Funchal.
Background: Aerobiological and epidemiological research has been made in Funchal till now in order to detect pollen and fungi airborne and the prevalence of allergic disease.Purpose: Analysis of airborne fungal spores observed in Funchal city during one year study. Methods: Aerobiological records of spores were conducted by a Burkard sampler between April 2003 and March 2004. Parallel records of meteorological parameters were obtained at Meteorological Institute and correlated with aerobiological data.Results: The fungal counts obtained during the study were equalled 11.862.126 spores/m3/year. Three classes were identified: Deuteromycetes 55,44%, Ascomycetes: 23,05% and Basidiomycetes: 20,63%. Cladosporium, Torula, Fusarium and Alternaria were the most prevalent Deuteromycetes, whereas Leptosphaeria (Ascomycete) and Coprinus (Basidiomycete) the most frequent types within their class. Despite the maximum number recorded being during springtime, there is a continuous presence of sporomorphs in the atmosphere all around the year. The relation between increasing airborne fungi and daily climatic factors, namely temperature and humidity was shown.Conclusion: The tendency of the increasing number in airborne fungi every year could be explained by meteorological and outdoor conditions. An integrative analysis of aerobiological data, epidemiological studies and the influence of environment should provide a better approach of the allergic disease.
*****
Respiratory Allergy to MouldsRespiratory Allergy to Moulds
A.C. LoureiroImmunoallergogy Service
30
Coimbra-Portugal
Respiratory repercussions caused by exposure to fungal allergens are varied and can commonly trigger asthma, rhinitis, hypersensitivity pneumonitis and allergic bronchopulmonary aspergillosis. In 1982 a new clinical entity was established - allergic fungal sinusitis.
Fungi are uni or multicellular organisms that live in organic materials in decomposition. They are dispersed, as spores or fragments of mycelia, both outdoor and indoor, and form a kingdom of living organisms which is relatively unknown.It was only in 1966, with Whittaker, that an independent fungus kingdom was established, due to the identification of the characteristic and distinct means of reproduction and nourishment, which differ from the ones observed in plants and animals1. The classification of fungi and its knowledge is not totally established, particularly in the lower taxonomic categories. Four subgroups in the fungus kingdom are recognised under the general designations of Ascomycota, Basidiomycota, Zygomycota and Mitosporic fungi. This classification is based in the characteristics of their reproductive organs – teleomorph or perfect form, with the division by meiosis – corresponding to the first three subgroups. The fourth subgroup includes all those whose the perfect form is not known – the anamorph or imperfect fungi– in which multiplication is made by mitosis. However, many perfect fungi are currently known by the most common names of their imperfect forms2.About 250,000 species of fungi are known today, being about 100 species related to the allergic pathology documented by hypersensitivity skin prick tests and/or bronchial or nasal provocative tests. The first description that associates fungi with allergic pathology was reported by Maimonides in the 12th century, but it was only in 1873 that Blackley established a relationship between allergic disease and the inhalation of Penicillium spores 3.The concentration of fungus spores in the air depends on factors related to their growth, being the temperature, the humidity and the presence of organic substratum the most relevant ones, and factors related to their dispersion like the wind, the rain and the turn over of the soils.
The knowledge in fungal allergy has improved as more advanced methods of spores counts and standardization of allergen extracts had been developed. Furthermore, the implementation of epidemiological studies has contributed to a more correct clarification of their clinical relevance.Aerobiological studies have shown that spores can be in the air virtually all year-round. In countries with temperate climate the number of spores reaches a peak in the months of July and October, being Cladosporium more predominant during the day, and Sporobolomyces during the night, with a decline in the winter months. Some fungi as Fusarium and Phoma betae, are easily dispersed by humidity and rain, or by dry and windy weather, as Cladosporium, Alternaria Epicoccum or Helminthosporium 4.
31
The spores of Cladosporium and Alternaria are more frequent. The Cladosporium ones can reach 24000/m3 having, nevertheless, the daily average counts of 5000/m3. The counts of Alternaria spores are lower, with an average counts of 150/m3 5.Generally fungi species found indoors are correlated with the ones found outdoors, though in lower quantities. The most frequently identified are Cladosporium, Aspergillus and Penicillium6.There are various methods for fungi identification. The collection of air samples based on volumetric or gravimetrical methods can be directly processed for microscopic identification or for culture media and further analysis. The morphologic differences of the spores of varied genera are often so insignificant that they cannot be characterized correctly, such as Penicillium and Aspergillus. In this case, culture is nedeed to identify them. Sporulation characteristics are better analysed in the culture, but this technique is time consuming and the diversity of the culture media used is another disadvantage.The more frequent fungi identified through culture in the homes of asthmatic patients living in the Central Region of Portugal were Rhizopus nigricans (42,3%), Aspergillus níger and Mucor racemosus (15,4%), Penicillium notatum (13,4%) and Fusarium culmorum (5,7%)7.The use of inquiries has been carried out in epidemiological studies in order to get an indirect characterization of fungus presence. However, some studies did not point out a significant correlation between asthma prevalence and its seriousness and the presence of visible colonies of fungi, seepage and mould smell8.
In spite of the fact that fungi are associated with allergic diseases, their clinical relevance is difficult to establish. In fact, though the concentration of spores in the environment is generally superior to the pollen spores, only some fungi like Alternaria alternata, Aspergillus fumigatus and oryzae, Cladosporium herbarum, Penicillium notatum and citrinum, Candida albicans and Cryphonectira parasitica can trigger allergy and have a characterization of their allergens, although an incomplete one9.The prevalence of sensitisation to fungi determined by skin tests of allergy is not well known. According to the population studied and the allergen extract used, the prevalence of sensitisation to fungus can vary from 3 to 91%10. In fact, even in the same population the use of different extracts of Cladosporium herbarum can lead to variations of prevalence from 12 to 65%. In Portugal, studies pointed out values of allergy prevalence to fungi in the general population from 2% to 3%, and 21% in an atopic population, being bronchial asthma the predominant allergic pathology 11. In the central region, in a population aged 20 to 44 years, we observed a prevalence of sensitisation to Alternaria alternata and to Cladosporium herbarum of 1%, determined by allergy skin prick tests and by RAST 7. It was observed a prevalence of 8,1% to Alternaria alternata and of 6,9% to Cladosporium herbarum in a student population12. An adult allergic population showed a sensitising prevalence from 1% to 4,2% to Alternaria alternata and from 1,8% to 3,8% to Cladosporium herbarum13.
32
These variations in the prevalence values of allergy to fungi seem to be also influenced by the age of the studied population. In fact, it often occurs in children and bronchial asthma seems to be the most frequent clinical expression of fungus exposure especially to Alternaria and Cladosporium14.Allergic bronchopulmonary aspergillosis is a clinical entity associated to exposure to Aspergillus fumigatus.The Pathophysiology is not still full clarified, but it can be characterized by bronchial colonization of asthmatic patients, with subsequent release of mycotoxins and proteolytic enzymes which cause eosinophilic inflammation, depending on the activation of CD4 lymphocytes, restricted to antigens HLA – DR2 e DR5 – and increase of interleukins concentrations IL4, IL5, of IgE and IgG115.There is no correlation between the intensity of exposure to the spores of Aspergillus fumigatus and the prevalence of sensitivity to this fungus determined by skin prick tests 16. In addition to Aspergillus (fumigatus, terreus, oryzaeochraceus) other species have been reported in clinical cases similar to APBA, like Curvularia lunata, Dreschlera hawiiensis, Geotrichum candidum and Stemphylium lanuginosum, belonging to allergic bronchopulmonary mycoses.17
A set of criteria, major and minor, has been proposed to evaluate the diagnosis. Under these criteria it is possible to establish subcategories that could have implications either in the diagnosis or in the prognostic. The presence of bronchial asthma is considered one of the major criteria for the diagnosis. In some series positive skin tests to Aspergillus is from 20% to 30%. The valorisation of this association (bronchial asthma and positive skin prick tests to Aspergillus) may open the way to further studies, particularly in CT scan, in order to establish an early diagnosis 18.Frequent inhalation of organic particles can cause a group of lung diseases known as hypersensitivity pneumonitis or extrinsic allergic alveolitis. Presently there are an increasing number of etiologic agents. They are generally present in the descriptions of isolated clinical cases or in small series and need a better characterization 19,20.Hypersensitivity is a complex syndrome with clinical presentation, seriousness and diverse evolutions, according to the responsible etiologic agent, the time, and the degree of exposure. Bird fancier´disease and farmer lung have been deeply studied and thus provided a better knowledge of this clinical entities 21.Fungi found in diverse environments have also been considered as etiologic agents. It was clearly demonstrated that fungi found in working environments have implications in some diseases. Pathophysiology seems to be focused on the release of pro-inflammatory cytokines (TNT, IL1, IL2, IL3, IL12, IF and GM-CSF) influenced by T lymphocyte and on the formation of immune complexes likely to cause a constant release of these cytokines. In more evolutional forms to fibrosis, IL8 will have a significant contribution. On the other hand, the conteregulation of granuloma formation will have a participation of IL10 and of IL6.The diagnosis is established by
33
the conjugation of clinical, laboratorial radiographic, and histological criteria. Provocative tests, specially those made in the working environment have a diagnostic interest.The prognostic seems to be different, depending on the causal agent22. Extrinsic allergic alveolitis among pigeon breeders seems to have a more serious prognosis. It was demonstrated that there is a decrease in FEF50 and in FEV1 in the exposed subjects, when compared to the general population 23.Allergic fungal sinusitis was first described by Katzenstein in 1983 and characterized as an inflammatory response to the colonies set in the paranasal sinusis24. The presence of mechanical factors like polyps and septal deviation, or inflammatory factors like chronic sinusitis, lead to the obstruction of the paranasal sinuses and create optimal conditions for fungal growth. The most important fungi associated with this pathology belong to Bipolaris, Curvularia, Drechslera, Exserohilum and Alternaria species. Aspergillus species are also frequently present with a frequence varying from 10% to 20%. Fungal allergic sinusitis seems to be more frequent in hot climates with high air humidity. It is commonly found in young atopic subjects with chronic sinusitis and polyps25.Several diagnostic criteria have been proposed. However, the demonstration of sinusitis image and the presence of allergic mucin and hyphae, in the absence of immunodeficiency, are essential. Fungus culture or the demonstration of other fungal elements in the nasal lavage is not relevant for most authors 26.
References
1. Whittaker RH. New Concepts of Kingdoms of Organisms. Science. 1969; 163:150-60.2. Sutton DA, Fothergill AW and Rinaldi MG. 1998. Introduction, p 3-11. In Mitchell CW (Ed).
Guide to Clinically Significant Fungi. The Williams & Wilkins Co. Baltimore, Md.3. Blackley CH. Experimental Researchs on the Causes and Nature of Catarrhus Aestivus
(Hay Fever or Hay Asthma). Ballière. Tindall and Cox. London. (Rep: Dawson, London 1959).
4. Solomon W, Platts-Mills T. 1998. Aerobiology and Inhalant allergens, p 367-403. In Midleton E Jr, Reed CE, Ellis EF, Adkinson NF Jr, Yunginger JW, Busse WW (Ed Allergy Principles and Pratice. 5th. Mosby.
5. Lacey J. 1997. Fungi and Actynomycetes as Allergens, .858-87. In Kay AB (Ed.). Allergy and Allergic Diseases. Blackwell Science.
6. Takahashi T. Airborne Fungalcolony-Forming units in Outdoor and Indoor Environments in Yokohama, Japan. Mycopathology. 1997;139:23-33.
7. Chieira C, Loureiro AC, Paiva J, Todo Bom A, Pereira AC, Faria E, Ribeiro H, Gertrudes Almeida M, Baptista-Ferreira JL, Robalo Cordeiro AJA. Fungos e Alergia Respiratória. Via Pneumológica. 1990; 2: 103-10.
34
8. Garret MH, Rayment PR, Hooper Ma, Abranson MJ and Hooper BM. Indoor Fungal Spores, House Dampness and Associations with Environmental Factors and Respiratory Health in Children. Clin Exp Allergy. 1998; 28: 459-67.
9. Philip JT, Geoffrey AS and Jonathan MS. 2001. Allergens and Pollutants, p 213-42. In Stephen Holgate, Martin K Church, Lawrence M Lichtenstein (Ed). Allergy. Mosby.
10. Horner WE, Helbling A, Salvaggio JE, Lehrer SB. Fungal Allergens. Clin Microbiol Rev, 1995; 40: 161-79.
11. Palma Carlos AG, Sousa Uva A. 1984. Mould Allergy in Portugal, p 105. In Knud Wilken-Jensen and Suzanne Gravesen (Ed) Atlas of Moulds in Europe Causing Respiratory Allergy. Foudation for Allergy Research in Europe. ASK Publishing.
12. AC Loureiro, Graça Loureiro, B Tavares, I Carrapatoso, C Chieira. Sensibilização a Fungos. Rev Port Imunoalergol, 1999; 7 (2):120.
13. Loureiro AC, Chieira C, Pereira AC, Todo Bom A, Faria E, Alendouro P, Tavares B, Victor L Rodrigues, Salvador M Cardoso, Robalo Cordeiro AJA. Estudos Epidemiológicos da Asma Brônquica numa População Adulta. Rev Port Imunoalergol, 1996; 4 (1):35-54.
14. Tariq SM, Mathews SM, Stevens M and Hakin EA. Sensitization to Alternaria and Cladosporium by age of 4 years. Clin Exp Allergy, 1996; 26:794-8.
15. Chauhan B, Knutsen AP, Hutcheson PS, Slavin RG, Bellone CJ. T Cell Subsets, Epitope Mapping, and HLA- Restrction in Patiennts with Allergic Bronchopulmonary Aspergillosis. J Clin Invest, 1996; 97 (10): 2324-31.
16. Beaumont F, Kauffman HF, DeMonchy JGR, Sluiter HJ and DeVries K. Volumetric Aerobiological Survey of Conidial Fungi in the North-East Netherlands II. Comparison of Aerobiological Data and Skin tests with Mold Extracts in an Asthmatic Population. Allergy, 1985; 40: 181-6.
17. Elliot MW and Newman Taylor AJ. Allergic Bronchopulmonary Aspergillosis. Clin Exp Allergy, 1997; 27 (S1): 55-9.
18. Angus RM, Davies ML, Cowan MD, McSharry C, Thomson NC. Computed Tomografic Scanning of the Lung in Patients with Allergic Bronchopulmonary Aspergillosis and in Asthmatic Patients with a Positive Skin Test to Aspergillus fumigatus. Thorax, 1994; 49 (6): 586-9.
19. Winck JC, Delgado L, Murta R, Lopez M, Marques JA. Antigen Characterization of Major Cork Moulds in Suberosis (Cork Worker´pneumonitis) by Immunobloting. Allergy, 2004;59:739-45.
20. Morais A, Winck JC, Delgado L, Palmares MC, Fonseca J, Moura e Sa J, Marques JA. Suberosis and Bird Fancier´s Disease: A Comparative Study of Radiological, Functional and Bronchoalveolar Profiles. J Invest Allergol Clin Immunol, 2004;14:26-33.
21. John E Salvaggio and David J Hendrik. 2001. Extrinsic Allergic Alveolitis, p 37-53. In Stephen Holgate, Martin K Church, Lawrence M Lichtenstein (Ed). Allergy. Mosby.
35
22. Grammar LC, Roberts M, Lerner C, Patterson R. Clinical and Serologic Follow-Up of Four Children and Five Adults with Bird-Fancier’s Lung. J Allergy Clin Immunol, 1990; 85 (3): 655-60.
23. Segorbe Luís A, Franco A, Pereira C, Robalo Cordeiro C, Fernandes A, Loureiro C, Todo Bom A, Fava Abreu, Morais T, Garção F, Paiva Carvalho J, Oliveira LC, Robalo cordeiro AJ. Estudo da Repercussão Ventilatória no Criador de Pombos Assintomático. Archivos Bronconeumologia, 1993; 29 (S1):7.
24. Katzenstein AL, Sale SR, Greenberger PA. Pathologic Findings in Allergic Aspergillus Sinusitis: A Newly Recognized Form of Sinusitis. Am J Surg Pathol, 1983; 7: 439-43.
25. DeShazo RD, Chapin K, Swain RE. Fungal Sinusitis. N Engl J Med, 1997; 337: 254-9.26. DeShazo RD, Swain RE. Diagnostic Criteria for Allergic Fungal Sinusitis. J Allergy Clin
Immunol, 1995; 96: 24-35.
*****
Mite allergen characterization and monitoringMite allergen characterization and monitoring
Ronald van Ree, PhD
House dust mites were identified as a cause of allergy and asthma in the mid-sixties by Voorhorst and Spieksma(1,2). The major allergenic species in temperate climates are Dermatophagoides pteronyssinus and Dematophagoides farinae. In tropical environments Blomia tropicalis has been identified as an important species(3). The first allergens identified in Dermatophagoides pteronyssinus house dust mites were at that time called P1 and Dpx(4,5). At present these allergens are designated Der p 1 and Der p 2, respectively, following the guidelines of the IUIS Allergen Nomenclature Committee (www.allergen.org).Their homologues in Dermatophagoides farinae are Der f 1 and Der f 2. Although almost 20 different allergens have been identified in both mite species since, group 1 and group 2 allergens are still regarded as the most important allergens(6-8). Several other allergens have been reported to be “major allergens”, like group 5, group 7, group 10 and group 14 allergens (www.allergome.org). So far, stable consensus about the importance of the broad spectrum of house dust mite allergens exists for group 1 and group 2. The third allergen for which consensus can probably be reached that it is a true major allergen is the group 7 allergen (8). For most of the other allergens identified so far, reported prevalence of recognition have been less
36
consistent. Most likely, these are explained by the different areas where studies were performed and/or the size of the group of patients that were studied.
Biological function of mite allergensGroup 1 mite allergens were shown to share homology with the family of cystein proteases (9). The major house dust mite allergen has indeed been shown to possess cystein protease activity(10). Enzymatic activity of Der p 1 has been proposed as a pro-inflammatory activity contributing to its allergenicity. Cleavage of CD25 (IL2 receptor), CD23 (low-affinity IgE receptor), and permeabilization of tight junctions have all been implicated to favour a role of Der p 1 as a major allergen(11-17). Group 1 house dust mite allergens are secreted and are highly abundant in mite faecal particles. In contrast, Der p 2 is a body protein of which the exact function has not yet been elucidated, although homology has been found with human epididymous protein(18). In general, IgE titres against Der p 2 tend to be slightly stronger than those observed against Der p 1(8). The reason for this apparent higher allergenicity is not clear. Der p 3, 6 and 9 all are active serine proteases: trypsine, chymotrypsine and elastase (www.allergome.org). Their importance as mite allergens is not well established yet but it certainly is thought to be less than of Der p 1 and 2. Der p 4 is again an enzyme, i.e. an amylase(19). Der p 5 and Der p 7 do not share homology with any known proteins and their function is therefore still unknown. Der p 8 again is an enzyme, i.e. glutathion-S-transferase (20). Group 10 and group 11 are both structural proteins, i.e. tropomyosin(21)and paramyosin (www.allergome.org), respectively. Over recent years, new molecular biology techniques have resulted in identification of many new allergens from house dust mite. Here it suffices to state that it is not yet really clear what their importance for mite allergy will turn out to be.
Cross reactivity to foodsIt is well-established that IgE antibodies to pollen frequently cross-react to plant foods. The best example of a cross-reactive allergen in pollen is Bet v 1. Cross-reactivity of IgE antibodies results in allergy to fruits like apple, cherry and peach and to hazelnut and some vegetables like carrot and celery. Also for IgE antibodies against house dust mites cross-reactivity to foods has been reported on several occasions. The muscle protein tropomyosin (group 10 in mites) is instrumental in cross-reactivity between house dust mites and foods from invertebrate animal origin like shrimps, molluscs, lobster, crab and snails(22-28). Tropomyosin is the major allergen of shrimp and of several the other listed sea foods(29). It is not always clear what the primary sensitizer is, but most likely both seafood tropomyosin and house dust mite tropomyosin can act as such. As an inhalant allergen however, tropomyosin most likely plays a minor role. It has been claimed that mite immunotherapy can cause snail and shrimp allergy by induction of cross-reactive IgE antibodies to allergens like tropomyosin(30). This however still waits for confirmation in double-blind clinical trials.
37
Diagnosis and therapy using major mite allergensAt present routine diagnosis and immunotherapy are carried out with house dust mite extracts. Depending on the company, purified mite-body extracts or whole-culture extracts are used. It is important to realise that these different approaches will result in different ratios between secreted allergens (like Der p 1) and non-secreted allergens (like Der p 2). This can influence the performance of diagnostic tests and the efficacy of immunotherapy. It is therefore important to monitor the major allergen levels. To better control the major allergen content of house dust mite diagnostics and therapeutics, the application of recombinant mite allergens has been proposed. Most major allergens have been cloned and expressed in several different expression systems. Of course the feasibility of such approaches will depend on the quality of recombinant allergens and on the number of allergens needed to replace extracts. Several studies have been carried out to compare the sensitivity of diagnostics based on extracts and on combinations of recombinant major allergens. It has been claimed that the combination of Der p 1, 2 and 7 will result in sensitivity over 95% compared to extract (8). Although these results look very promising, some reservation is still needed. Diagnostics based on house dust mite extracts do not always reach saturation for all allergens. The sensitivity of major allergen combinations compared to extracts might therefore be overestimated.Pittner et al. have proposed that component-resolved diagnosis (as they have designated diagnosis with multiple individual major allergens) can be used to distinguish patients with a good prognosis for immunotherapy from those that can better not be treated by immunotherapy(31). It was suggested that patients with IgE antibodies to mite allergens with a broad spectrum of cross-reactivity (e.g. to tropomyosin) are less likely to benefit from immunotherapy than those who only recognize mite allergens like Der p 1 and Der p 2. This hypothesis is in line with the concept that immunotherapy is most successful in mono-sensitized patients. Nevertheless it needs to be confirmed by well-controlled clinical trials.So far, no attempts have been made to replace mite extracts for immunotherapy. Whether Der p 1 and Der p 2 will be sufficient to replace mite extracts or allergens like Der p 7 need to be included will have to be established in clinical trials. Another interesting aspect of the application of recombinant allergens is the possible absence of naturally occurring adjuvant activity in extracts. Again, only well-controlled trials with recombinant allergens can demonstrate whether they will be an efficient replacement of current extract-based products.
Monitoring of mite allergensAs long as diagnosis and immunotherapy are carried out with extracts, measurement of major allergens like Der p 1 and Der p 2 will be of great importance. At present several different assays for their measurement are available. An EU-funded project is currently comparing these assays and developing candidate certified references based on recombinant versions of Der p 1 and Der p 2(32). This project will provide the tools to reliably standardize extract-based products for diagnosis and immunotherapy.
38
References
(1) Voorhorst R, Elias RW, Spieksma FT. [Housedust, a source of allergens and of misunderstanding]. Ned Tijdschr Geneeskd 1966; 110(1):46-8.
(2) Voorhorst R, SPIEKSMA-BOEZEMAN MI, Spieksma FT. IS A MITE (DERMATOPHAGOIDES SP.) THE PRODUCER OF THE HOUSE-DUST ALLERGEN? Allerg Asthma (Leipz ) 1964; 10:329-34.
(3) Thomas WR, Hales BJ, Smith W. Blomia tropicalis: more than just another source of mite allergens. Clin Exp Allergy 2003; 33(4):416-8.
(4) Chapman MD, Platts-Mills TA. Purification and characterization of the major allergen from Dermatophagoides pteronyssinus-antigen P1. J Immunol 1980; 125(2):587-92.
(5) Lind P. Purification and partial characterization of two major allergens from the house dust mite Dermatophagoides pteronyssinus. J Allergy Clin Immunol 1985; 76(5):753-61.
(6) Thomas WR, Smith WA, Hales BJ, Mills KL, O'Brien RM. Characterization and immunobiology of house dust mite allergens. Int Arch Allergy Immunol 2002; 129(1):1-18.
(7) Thomas WR, Smith W. Towards defining the full spectrum of important house dust mite allergens. Clin Exp Allergy 1999; 29(12):1583-7.
(8) van Ree R, van Leeuwen WA, Bulder I, van Oort E, Kramer M, Shen HD et al. Recombinant allergens for the diagnosis and treatment of house dust mite allergy. Which allergens are essential? In: Bienenstock J, Ring J, Togias AG, editors. Allergy Frontiers and Futures. Cambridge, MA: Hogrefe & Huber, 2004: 55-9.
(9) Chua KY, Stewart GA, Thomas WR, Simpson RJ, Dilworth RJ, Plozza TM et al. Sequence analysis of cDNA coding for a major house dust mite allergen, Der p 1. Homology with cysteine proteases. J Exp Med 1988; 167(1):175-82.
(10) Schulz O, Sewell HF, Shakib F. A sensitive fluorescent assay for measuring the cysteine protease activity of Der p 1, a major allergen from the dust mite Dermatophagoides pteronyssinus. Mol Pathol 1998; 51(4):222-4.
(11) Gough L, Schulz O, Sewell HF, Shakib F. The cysteine protease activity of the major dust mite allergen Der p 1 selectively enhances the immunoglobulin E antibody response. J Exp Med 1999; 190(12):1897-902.
39
(12) Wan H, Winton HL, Soeller C, Tovey ER, Gruenert DC, Thompson PJ et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J Clin Invest 1999; 104(1):123-33.
(13) King C, Brennan S, Thompson PJ, Stewart GA. Dust mite proteolytic allergens induce cytokine release from cultured airway epithelium. J Immunol 1998; 161(7):3645-51.
(14) Comoy EE, Pestel J, Duez C, Stewart GA, Vendeville C, Fournier C et al. The house dust mite allergen, Dermatophagoides pteronyssinus, promotes type 2 responses by modulating the balance between IL-4 and IFN-gamma. J Immunol 1998; 160(5):2456-62.
(15) Schulz O, Sewell HF, Shakib F. Proteolytic cleavage of CD25, the alpha subunit of the human T cell interleukin 2 receptor, by Der p 1, a major mite allergen with cysteine protease activity. J Exp Med 1998; 187(2):271-5.
(16) Asokananthan N, Graham PT, Stewart DJ, Bakker AJ, Eidne KA, Thompson PJ et al. House dust mite allergens induce proinflammatory cytokines from respiratory epithelial cells: the cysteine protease allergen, Der p 1, activates protease-activated receptor (PAR)-2 and inactivates PAR-1. J Immunol 2002; 169(8):4572-8.
(17) Gough L, Sewell HF, Shakib F. The proteolytic activity of the major dust mite allergen Der p 1 enhances the IgE antibody response to a bystander antigen. Clin Exp Allergy 2001; 31(10):1594-8.
(18) Thomas WR, Chua KY. The major mite allergen Der p 2--a secretion of the male mite reproductive tract? Clin Exp Allergy 1995; 25(7):667-9.
(19) Mills KL, Hart BJ, Lynch NR, Thomas WR, Smith W. Molecular characterization of the group 4 house dust mite allergen from Dermatophagoides pteronyssinus and its amylase homologue from Euroglyphus maynei. Int Arch Allergy Immunol 1999; 120(2):100-7.
(20) O'Neill GM, Donovan GR, Baldo BA. Cloning and characterization of a major allergen of the house dust mite, Dermatophagoides pteronyssinus, homologous with glutathione S-transferase. Biochim Biophys Acta 1994; 1219(2):521-8.
(21) Asturias JA, Arilla MC, Gomez-Bayon N, Martinez A, Martinez J, Palacios R. Sequencing and high level expression in Escherichia coli of the tropomyosin allergen (Der p 10) from Dermatophagoides pteronyssinus. Biochim Biophys Acta 1998; 1397(1):27-30.
(22) Ayuso R, Reese G, Leong-Kee S, Plante M, Lehrer SB. Molecular basis of arthropod cross-reactivity: IgE-binding cross-reactive epitopes of shrimp, house dust mite and cockroach tropomyosins. Int Arch Allergy Immunol 2002; 129(1):38-48.
40
(23) Aalberse RC, Akkerdaas J, van Ree R. Cross-reactivity of IgE antibodies to allergens. Allergy 2001; 56(6):478-90.
(24) Leung PS, Chen YC, Mykles DL, Chow WK, Li CP, Chu KH. Molecular identification of the lobster muscle protein tropomyosin as a seafood allergen. Mol Mar Biol Biotechnol 1998; 7(1):12-20.
(25) Guilloux L, Vuitton DA, Delbourg M, Lagier A, Adessi B, Marchand CR et al. Cross-reactivity between terrestrial snails (Helix species) and house-dust mite (Dermatophagoides pteronyssinus). II. In vitro study. Allergy 1998; 53(2):151-8.
(26) Martinez A, Martinez J, Palacios R, Panzani R. Importance of tropomyosin in the allergy to household arthropods. Cross-reactivity with other invertebrate extracts. Allergol Immunopathol (Madr ) 1997; 25(3):118-26.
(27) Leung PS, Chow WK, Duffey S, Kwan HS, Gershwin ME, Chu KH. IgE reactivity against a cross-reactive allergen in crustacea and mollusca: evidence for tropomyosin as the common allergen. J Allergy Clin Immunol 1996; 98(5 Pt 1):954-61.
(28) Witteman AM, Akkerdaas JH, Van Leeuwen J, van der Zee JS, Aalberse RC. Identification of a cross-reactive allergen (presumably tropomyosin) in shrimp, mite and insects. Int Arch Allergy Immunol 1994; 105(1):56-61.
(29) Shanti KN, Martin BM, Nagpal S, Metcalfe DD, Rao PV. Identification of tropomyosin as the major shrimp allergen and characterization of its IgE-binding epitopes. J Immunol 1993; 151(10):5354-63.
(30) van Ree R, Antonicelli L, Akkerdaas JH, Garritani MS, Aalberse RC, Bonifazi F. Possible induction of food allergy during mite immunotherapy. Allergy 1996; 51(2):108-13.
(31) Pittner G, Vrtala S, Thomas WR, Weghofer M, Kundi M, Horak F et al. Component-resolved diagnosis of house-dust mite allergy with purified natural and recombinant mite allergens. Clin Exp Allergy 2004; 34(4):597-603.
(32) van Ree R. The CREATE project: EU support for the improvement of allergen standardization in Europe. Allergy 2004; 59(6):571-4.
*****
41
INDOOR POLLUTION AND IMMUNOLOGIC CHANGESINDOOR POLLUTION AND IMMUNOLOGIC CHANGES
Mário Morais-Almeida MDImmunoallergy Department, Dona Estefânia Hospital, Lisbon, Portugal([email protected])
The development and phenotypic expression of allergic disease depends on a complex interaction between genetic and several environmental factors, such as exposure to food and inhalant allergens and also to non-specific adjuvant factors (e.g. tobacco smoke, air pollution and infections). The first year of life seems to be a particularly vulnerable period and there is evidence that sensitisation is related to the level of allergen exposure during early life. At present, atopic heredity seems to result in the best predictive discrimination as regards development of allergic disease at birth.1 Early sensitisation, either to aeroallergens as to foods, atopic dermatitis and allergic rhinitis are predictors for later development of allergic lower airway disease. Various environmental factors, pollutants, that may enhance sensitisation include tobacco smoke, NO2, SO2, ozone, and diesel particles; within them, at an indoor perspective, passive smoking is by far the best-established risk factor, particularly in early childhood.2 The indoor environment probably plays a larger role than outdoor air pollution in the development of allergic disease, and are usually considered as a major risk factor for asthma prevalence increase.3 Expanding the concept, the mother is not only a source of genetic information, but also an "environmental factor", as there is a very close continuous immune interaction between her and the offspring.2 Intrauterine environment may play a significant role, particularly tobacco smoke during pregnancy, and its respiratory effects on infant. Maternal allergenic exposure during pregnancy is also an important factor because of materno-fetal immunologic interactions.4,5
Outdoor pollution acts by enhancing bronchial responsiveness, allergenic sensitisation and worsening respiratory diseases.6 Its effect is probably less important in infants and small children who are living indoor most of the time. Infection seems to have a complex action: some respiratory virus act to induce asthma or sensitisation; other kind of infections (viral, microbial, parasites) can have a protector effect. Exposure to tobacco smoke, particularly maternal smoking, is identified in all studies, as one of the most important factors to be considered in childhood asthma.4,5
42
Bronchial asthma represents a major health problem. Last decades increase in the prevalence and severity of this disease is widely accepted, particularly at paediatric age, leading to a high rate of school absenteeism, emergency room visits and hospital admissions.7 Asthma is the main cause of hospital admission in children with chronic disease and, parallel to a decrease in the global number of admissions at paediatric age, studies showed an increase in asthma admissions.9,10 The reasons that justify this fact are yet to be determined. Some studies report not only an increase in the number of admissions, but also mainly an increase in readmissions to hospital, suggesting that the increase in asthma severity is more important than the increase in incidence.8,10
There are few studies evaluating risk factors associated with hospital admission for childhood asthma, but in the majority of them identified: age under 4 years, male gender, black race, low socio-economic status, absence of specialised medical care, prior asthma hospitalisation, environmental tobacco-smoke exposure and indoor allergen sensitisation.7-13
From our own experience, in a case-control study, performed in a sample of children admitted to hospital for acute asthma, comparing with a group of asthmatic outpatients (matched by age, gender and socio-economic status), by logistic regression analysis, we identified as significant and independent risk factors for hospital admission: prior asthma hospitalisation and last-year admission, environmental tobacco-smoke exposure, allergen sensitisation, maternal asthma and onset of symptoms before 12 months of age. As it was found by others, attendance at day-care or kindergarten and large family size were identified as protective factors.14
Environmental tobacco-smoke exposure adversely affects asthmatic children in several ways, including increase total IgE and specific IgE antibody responses, eosinophilia, decrease in lung function, increase in bronchial hyperreactivity, increase in attack number and emergency-room visits.11,12,15-18 Chilmonczyk et al,17 in a retrospective study including 199 asthmatic children, found a relationship between tobacco-smoke exposure and asthma morbidity, through measurement of urine cotinine levels. Other authors have tried to correlate passive smoking to asthma morbidity. Azizi et al,11 in a study performed in Kuala Lumpur, with 158 hospitalised children, found a relative risk of 1.9 for passive smoking. Macarthur et al,12 also identified passive tobacco-smoke as a risk for asthma readmission to hospital.
The mechanisms by which passive smoking is associated with an increase in the severity of childhood asthma are still unclear. A possible mechanism could be the direct effect on bronchial mucosa, triggering the inflammatory process, as tobacco smoke had two main effects on the respiratory tract: 1) induction of inflammation, and 2) mutagenic / carcinogenic effects.19
43
It also could enhance allergenic sensitisation, by the disruption of the bronchial epithelium, increasing the permeability to antigens. Another hypothesis could be that this disruption of bronchial epithelium promotes the appearance of respiratory infections, common triggers of asthma exacerbations.
It has been demonstrated that cigarette smoking affects the immune system. Impairment of alveolar mononuclear cell function, may contribute to the higher rate of respiratory infections; however, increased susceptibility of smokers to infections of other origin (e.g. wound-related) implies that tobacco effect is not restricted to the respiratory immune competent cells. Cigarette smokers with no chronic obstructive pulmonary disease, exhibit impaired NK cytotoxic activity in peripheral blood and unbalanced systemic production of pro- and anti-inflammatory cytokines.20
Epidemiologic studies have suggested that tobacco passive exposure increases the prevalence and severity of allergic diseases, as bronchial asthma, but also atopic dermatitis.21 It was proved that, even in healthy non-atopic children, exposure to ETS causes changes in cellular infiltrates which partly resemble those seen in the nasal mucosa of allergic children.22 Seymour et al, in a murine model, that included generation of and exposure to environmental tobacco smoke (ETS) followed by aerosolised allergen challenge, showed that "second-hand smoke" up-regulates the allergic response to inhaled allergen.23 Rumold et al,24 found that ETS, in mice, can induce allergic sensitisation to a normally harmless antigen, and that may explain why second-hand smoke is a major risk factor for the development of allergy in children.25
Despite all the understanding related with the effect of ETS on allergic disease expression, there is scarce information about the immunological effects of maternal smoking on the fetus. Noakes et al, compared, for the first time, cord blood mononuclear cell cytokine responses to ovalbumin or house dust mite and mitogens in neonates whose mothers smoked throughout pregnancy, controlled with responses of neonates never exposed to maternal smoke, concluding that maternal cigarette smoking can modify aspects of fetal immune function and highlight the need for further studies in this area.26
The importance of tobacco-smoke exposure lies in the fact that it is potentially avoidable. In a prospective study including 807 asthmatic children, Murray et al16 found a decrease in the severity of asthma and an improvement in functional respiratory parameters with reduction of smoke exposure. This study allows us to enhance the importance of establishing preventive anti-smoking campaigns, aiming mainly at asthmatic children’s parents. The identification of severity risk factors for asthma, related to hospital admission, allows the establishment of preventive measures, namely in high-risk children, with emphasis on medication planning and the establishment of education programs such as environmental tobacco-smoke avoidance and limitation of aeroallergen exposure.
44
Given the documented health risks to the mother and infant and the significant number of women who continue to smoke in the postpartum period, it is imperative that health care providers continue to assess smoking status and provide smoking-cessation counselling at every consultation.Among many as ETS, other significant indoor pollutants / irritants are associated with the allergic respiratory symptoms occurrence and severity, namely to asthma current symptoms: wood-smoke pollution related to cooking,27 new surface materials in the home (linoleum flooring, synthetic carpeting, particleboard, wall coverings, furniture, paint),28,29 building quality,30 formaldehyde,31 …
REFERENCES 1. Tariq SM, Matthews SM, Hakim EA, et al. The prevalence of and risk factors for atopy in early childhood: a whole population birth cohort study. J Allergy Clin Immunol 1998;101:587-93.2. Bjorksten B. The environmental influence on childhood asthma. Allergy 1999;54(Suppl.49):17-23.3. Global Strategy for Asthma Management and Prevention. National Institutes of Health, National Heart, Lung, and Blood Institute. Guidelines for the diagnosis and management of asthma, NIH, Publication Number 02-3659;2002.4. Gilliland FD, Li Y-F, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med 2001;163:429-36.5. Jaakola J, Gissler M. Maternal smoking in pregnancy, fetal development, and childhood asthma. Am J Public Health 2004;94:136-40. 6. Rusznak C, Devalia JL, Davies RJ. Airway response of asthmatic subjects to inhaled allergen after exposure to pollutants. Thorax 1996;51:1105-8.7. To T, Dick P, Feldman W, et al. A cohort study on childhood asthma admissions and readmissions. Pediatrics 1996;98:191-5.8. Jónasson G, Lødrup Carlsen KC, Leegaard J, et al. Trends in hospital admissions for childhood asthma in Oslo, Norway, 1980-95. Allergy 2000;55:232-9.9. Mitchell EA, Bland JM, Thompson JMD. Risk factors for readmission to hospital for asthma in childhood. Thorax 1994;49:33-36.10. Sporik R, Platts-Mills TA, Cogswell JJ. Exposure to house dust mite allergen of children admitted to hospital with asthma. Clin Exp Allergy 1993;23:740-6.11. Azizi BH, Zulkifli HI, Kasim S. Indoor air pollution and asthma in hospitalized children in a tropical environment. J Asthma 1995;32:413-8.12. Macarthur C, Calpin C, Parkin PC, et al. Factors associated with pediatric asthma readmissions. J Allergy Clin Immunol 1996;98:992-3.
45
13. Nelson RP, DiNicolo R, Fernández-Caldas E, et al. Allergen-specific IgE levels and mite allergen exposure in children with acute asthma first seen in an emergency department and in nonasthmatic control subjects. J Allergy Clin Immunol 1996;98:258-63.14. Gaspar AP, Morais-Almeida MA, Pires GC, et al. Risk factors for asthma admissions in children. Allergy Asthma Proc 2002;23:295-301.15. Magnusson CG. Maternal smoking influences cord serum IgE and IgD levels and increases the risk for subsequent infant allergy. J Allergy Clin Immunol 1986;78:898-904.16. Murray AB, Morrison BJ. The decrease in severity of asthma in children of parents who smoke since the parents have been exposing them to less cigarette smoke. J Allergy Clin Immunol 1993;91:102-10.17. Chilmonczyk BA, Salmun LM, Megathlin KN, et al. Association between exposure environmental tobacco smoke and exacerbations of asthma in children. N Engl J Med 1993;328:1665-9.18. Ronchetti R, Macri F, Ciofetta G, et al. Increased serum IgE and increased prevalence of eosinophilia in 9-year-old children of smoking parents. J Allergy Clin Immunol 1990;86:400-7.19. Behr J, Nowak D. Tobacco smoke and respiratory disease. Eur Respir Mon 2002;21:161-79.20. Zeidel A, Beilin B, Yardeni I, et al. Immune response in asymptomatic smokers. Acta Anaesthesiol Scand 2002;46:959-64.21. The effect of environmental tobacco smoke on eczema and allergic sensitization in children.Kramer U, Lemmen CH, Behrendt H, et al. Br J Dermatol 2004;150:111-8.22. Vinke JG, KleinJan A, Severijnen LW, et al. Passive smoking causes an 'allergic' cell infiltrate in the nasal mucosa of non-atopic children. Int J Pediatr Otorhinolaryngol 1999;51:73-81.23. Seymour BW, Pinkerton KE, Friebertshauser KE, et al. Second-hand smoke is an adjuvant for T helper-2 responses in a murine model of allergy. J Immunol 1997;159:6169-75.24. Rumold R, Jyrala M, Diaz-Sanchez D. Secondhand smoke induces allergic sensitization in mice. J Immunol 2001;167:4765-70.25. Kulig M, Luck W, Lau S, et al. Effect of pre- and postnatal tobacco smoke exposure on specific sensitization to food and inhalant allergens during the first 3 years of life. Multicenter Allergy Study Group, Germany. Allergy 1999;54:220-8.26. Noakes PS, Holt PG, Prescott SL. Maternal smoking in pregnancy alters neonatal cytokine responses. Allergy 2003;58:1053-8.27. Schei MA, Hessen JO, Smith KR, et al. Childhood asthma and indoor woodsmoke from cooking in Guatemala. J Expo Anal Environ Epidemiol 2004;14(Suppl.1):S110-7.28. Jaakkola JJ, Parise H, Kislitsin V, et al. Asthma, wheezing, and allergies in Russian schoolchildren in relation to new surface materials in the home. Am J Public Health 2004;94:560-2.29. Diez U, Rehwagen M, Rolle-Kampczyk U, et al. Redecoration of apartments promotes obstructive bronchitis in atopy risk infants--results of the LARS Study. Int J Hyg Environ Health 2003;206:173-9.
46
30. Emenius G, Svartengren M, Korsgaard J, et al. Building characteristics, indoor air quality and recurrent wheezing in very young children (BAMSE). Indoor Air 2004;14:34-42.31. Doi S, Suzuki S, Morishita M, et al. The prevalence of IgE sensitization to formaldehyde in asthmatic children. Allergy 2003;58:668-71.
*****
The central role of IgE in allergic disease – but what isThe central role of IgE in allergic disease – but what is around? around? A phenotype-tailored therapy for allergic diseases A phenotype-tailored therapy for allergic diseases
Sergio Bonini and Ginevra Menghi
San Raffaele H, INMM-CNR, Rome, Italy
The genetic susceptibility to mount a specific IgE antibody response to environmental allergens is one of the major pathophysiological features of allergic subjects, which is eventually able to initiate a cascade of pathogenetic mechanisms and to trigger symptoms upon natural or experimental allergen exposure. Several genetic and environmental factors may influence the sensitisation process. Among these special attention has recently been devoted to the protective role of an early microbial exposure1-3.
However, there are substantial differences in the quality and intensity of the final outcome of an IgE-allergen interaction, not only depending on the degree of sensitisation, but also on the type, load and route of allergen reaction, as well as on the reactivity of target tissues and organs participating in it. Accordingly, in some subjects the presence of IgE antibodies to allergens is not associated with clinical manifestations, in other causes mild reversible symptoms, in others induces persistent allergic inflammation and tissue remodelling, in others, finally, is only an epiphenomenon without causal relationships to disease4-5.
With reference to this last evenience, we should like to note that a polyclonal IgE activation is a frequently associate hallmark of allergic patients, but distinct from the specific IgE response to a given allergen. In fact, different genetic and environmental factors influence the typical Th2 cytokine profile of allergic subjects which results in: polyclonal IgE activation; eosinophil overproduction, activation and tissue recruitment; mast cell and basophil overexpression and
47
priming6. Interestingly enough, the Th2 profile may be documented in allergic subjects even in the absence of specific IgE antibodies, as it occurs in some forms of non allergic asthma, in non-allergic rhinitis with eosinophilia, in nasal polyps, in vernal keratoconjunctivitis, in atopic eczema, etc7.
Due the redundancy of factors influencing the allergic response (including endocrine8 and neural factors9-11 which we recently called attention on), the clinical value of any nosography, diagnostic or therapeutic approach only focussing on specific IgE is limited. Further diagnostic markers should be available in clinical practice to better dissect the heterogeneous allergic phenotype12 and to implement a more selective treatment based on the pathophysiological abnormalities preferentially involved in individual cases13.
Personal studies cited
Matricardi PM, Rosmini F, Riondino S, Fortini M, Ferrigno L, Rapicetta M, Bonini S. Exposure to foodborne and orofecal microbes versus airborne viruses, in relation to atopy and allergic asthma: epidemiological study. Br Med J. 2000; 320: 412-17.
Matricardi PM, Bonini S.High microbial turnover rate preventing atopy: a solution to inconsistencies impinging on the Hygiene hypothesis?
Clin Exp Allergy 2000; 30: 1506-1510.3. Matricardi PM, Rosmini F, Panetta V, Ferrigno L, Bonini S.
Hay fever and asthma in relation to markers of infection in the United States.
J Allergy Clin Immunol 2002; 110: 381-387164. Bonini Se, Bonini St, Vecchione A, Naim DM, Allansmith MR, Balsano F.
Inflammatory changes in conjunctival scrapings after allergen provocation in humans.J Allergy Clin Immunol. 1988; 82: 462. 16
Bonini St, Bonini Se, Bucci MG, Berruto A, Adriani E, Balsano F, Allansmith MR. Allergen dose response and late symptoms in a human model of ocular allergy. J Allergy Clin Immunol. 1990; 86 (6): 869-876.
Ruffilli A, Bonini Se.Susceptibility genes for allergy and asthma.Allergy. 1997; 52: 256-73.
Bonini St, Bonini Se, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O, Rama P, Magrini L, Juhas T, Bucci MG.Vernal keratoconjunctivitis revisited: a case series of 195 patients with long-term followup.
48
Ophthalmology 2000; 107: 1157-63.Bonini St, Lambiase A, Schiavone M, Centofanti M, Bonini Se.
Estrogen and progesteron receptors in vernal keratoconjunctivitis.Ophthalmology. 1995; 102: 1374-79.
Bonini Se, Lambiase A, Bonini St, Angelucci F, Magrini L, Manni L, Aloe L.Circulating nerve growth factor levels are increased in humans with allergic diseases and asthma.Proc Natl Acad Sci. USA 93, 1996; 10955-60.
Bonini S.Do neurotrophins play a role in allergic diseases and asthma?Clin Exp Allergy 2003; 33: 543-545.
Micera Micera A, Vigneti E, Pickholtz D, Reich R, Pappo O, Bonini S, Maquart FX, Aloe L, Levi-Schaffer F.Nerve growth factor displays stimulatory effects on human skin and lung fibroblasts, demonstrating a direct role for this factor in tissue repair.
Proc Natl Acad Sci USA 2001; 98(11): 6162-7.Bonini S, Matricardi PM, Torre A, Rasi G.
The heterogeneity of allergic phenotypes. Genetic and environmental interactionsAnn Allergy Asthma Immunol 2001; 87 (Suppl 3): 48-51.
Bonini Se, Rasi G.Who benefits from immunotherapy?
Allergy. 1997; 52: 693-94. *****
Mechanisms of Immunotherapy Mechanisms of Immunotherapy
Professor Anthony Frew, School of Medicine, University of Southamptone-mail [email protected]
Introduction Specific allergen immunotherapy (SIT) involves the administration of allergen extracts to modify or abolish symptoms associated with atopic allergy. The process is specific, in that the treatment is targeted at those allergens recognised by the patient and physician as responsible for symptoms. A decision to use SIT therefore demands a careful assessment of the patient’s
49
condition and the role of allergic triggers. This form of therapy was first attempted at the end of the 19th century and then reported in the second decade of the 20th century by Noon and Freeman at St Mary's Hospital, London [1]. Immunotherapy then became popular in North America and in Europe but some differences in practice have gradually developed either side of the Atlantic. Typically, patients are started on a very low dose of allergen, given by subcutaneous injection. The dose is then increased in a series of weekly injections until a plateau or maintenance dose is achieved. The maintenance dose is then given at 4-6 weekly intervals for 3 to 5 years. Alternative induction regimes may give several doses on each day, or may give the whole series of incremental injections in a single day (rush protocols). The main drawback to rush and semi-rush protocols is the risk of adverse reactions, which are much commoner than in conventional protocols. On the other hand, full protection can be attained in a few days as compared to the three months required in the conventional regime.
Mechanisms
Several mechanisms have been proposed to explain the beneficial effects of immunotherapy. Early studies showed that SIT induces allergen-specific IgG antibodies. This led to suggestions that SIT might work by inducing antibodies which would intercept the allergen and “block” the allergic response. In patients treated for venom anaphylaxis, the development of allergen-specific IgG antibody correlates with clinical efficacy but for other allergens, the magnitude of the IgG response is not closely related to the degree of efficacy. Moreover, the rise in IgG follows rather than precedes the onset of clinical benefit. Allergen-specific IgE levels rise temporarily during the initial phase of SIT, but fall back to pre-treatment levels during maintenance therapy [2]. The immediate skin test response can be reduced after SIT but this effect is relatively small compared to the degree of clinical benefit. In contrast, the late-phase skin test response is virtually abolished after successful SIT. Similar patterns are observed for late-phase nasal and airway responses [3].
With the recognition of the role of T-cells as orchestrators of the allergic response, investigators have turned to study the effects of SIT on cellular responses to allergen. Both in the skin and in the nose, successful SIT is accompanied by a reduction in T-cell and eosinophil recruitment in response to allergen challenge. In parallel, there is a shift in the balance of Th1 and Th2 cytokine expression in the allergen-challenged site. Th2 cytokine expression is not affected but there is an increased proportion of T-cells expressing the Th1 cytokines IL-2, IFN- and IL-12 [4-6]. These findings suggest that SIT has a modulatory effect on allergen-specific T-cells, which would explain why the clinical and late-phase responses are attenuated without such a large effect on allergen-specific antibody levels.
50
SIT for venom hypersensitivityAnaphylaxis to hymenoptera venom is relatively rare, but can be fatal. Venom-specific IgE antibodies can be found in 30-40% of adults for a few months following a sting, but these usually disappear in a few months. Some individuals react more vigorously with high concentrations of venom-specific antibodies, which may persist for many years without further exposure to stings. This group of patients are at risk of anaphylaxis to subsequent stings and a small number die from anaphylaxis each year. The introduction of pure venom SIT preparations has led to a substantial improvement in the effectiveness of SIT for venom allergy. Desensitisation with venom extracts accelerates the rate at which the risk decreases and has been shown to provide protection against field and laboratory stings. After completing venom SIT, there is a residual risk of about systemic reactions of 10%, but these are typically mild. Consideration should also be given to providing injectable adrenaline and other anti-allergic medication for use in the event of a sting during therapy.
SIT for allergic rhinitis
SIT has been widely used to treat allergic rhinitis. As with other uses of SIT, it is important to select patients appropriately. The allergic basis of the rhinitis should be carefully assessed both on history and on skin tests or blood tests, and other causes should be excluded. Tests of nasal sensitivity are not used in routine clinical practice but may be useful for assessing effectiveness in clinical trials.
The effectiveness of SIT in seasonal allergic rhinitis has been confirmed in many trials, using grass, ragweed and birch pollen. Moreover, SIT has been shown to be clinically effective even in patients with severe seasonal rhinitis that is resistant to conventional drug therapy [8]. Limited data is available regarding the long term efficacy of rhinitis, but a recent study demonstrate that the effects last for at least six years after discontinuing therapy [9]. The benefits of SIT for perennial rhinitis are less than for seasonal rhinitis. In part this reflects the difficulty in determining the extent to which allergy is responsible for perennial symptoms. Allergy to house dust mite is common and dose not always cause symptoms. Conversely, there are other causes of perennial rhinitis including vasomotor instability, infection, aspirin sensitivity etc. Nevertheless, clinical trials have shown a definite benefit in appropriately selected subjects. Clearer evidence has been obtained in rhinitis due to pet allergy. Several studies have shown a marked improvement in tolerance of cat exposure after SIT, confirmed both on challenge tests and simulated natural exposure [7].
As with any therapy, the risks and cost-effectiveness of SIT need to be assessed on a case by case basis. Current drug therapy for rhinitis can be very effective, but a significant proportion of rhinitis patients experience nose bleeds from intranasal steroids and drowsiness from their
51
antihistamines. Others find pharmacotherapy inconvenient or ineffective. Moreover, we are now more aware of the adverse effects of rhinitis on quality of life. SIT offers a useful option for these patients as well as a logical approach to dealing with the underlying problem.
SIT for asthma
Immunotherapy was widely used to treat allergic asthma in the UK prior to 1986 but evidence of severe adverse reactions, including a small number of fatalities has led to SIT being abandoned for asthma treatment in the UK, although asthma remains a common indication for SIT in North America and continental Europe [8,9].
Current drug therapies for asthma are aimed at suppressing the airways inflammation that is a characteristic feature of asthma. None of these treatments are curative and asthma recurs rapidly on ceasing treatment. Moreover, none of the current drug therapies is directed against agents that might cause asthma. Allergen avoidance has been proposed as a potentially useful manoeuvre in those with allergic asthma, but while extreme forms of allergen avoidance (e.g. admission to hospital, sending children to holiday homes at altitude), can improve the control of asthma, there is little evidence that such benefit can be achieved by the degree of allergen avoidance that can be achieved in suburban homes. There is thus scope for improving asthma care and for identifying allergen-specific therapies. SIT offers the possibility of deviating the immune response away from the allergic pattern and towards a more protective or less damaging response. However, SIT remains controversial as a treatment for asthma because of the potential side-effects. Many trials of SIT have studied laboratory surrogate markers of efficacy such as changes in IgG subclasses, in vivo challenges of the nose or skin test responses. While such measures undoubtedly do change during SIT, and may shed light on the mechanism of successful SIT, they cannot be used to provide direct evidence of clinical effectiveness in asthma.
Comparison of SIT with other types of treatment for asthmaThe majority of clinical trials of SIT for asthma have compared SIT either with historical controls or with a matched placebo-treated group. To date, the effectiveness of specific SIT in asthma has rarely been compared with conventional management (with avoidance measures and conventional inhaled or oral drugs). One recent study assessed SIT in asthmatic children receiving conventional drug therapy and found no additional benefit in patients who were already receiving optimal drug therapy [10]. There are some significant criticisms of this study and further work of this type is urgently needed. It is also important that trials include analysis of cost-benefit and cost-effectiveness since purchasers of health care are increasingly demanding this evidence before agreeing to fund therapies.
52
Effects on natural history of allergic diseaseA proportion of patients with allergic rhinitis go on to develop asthma each year. It has been suggested that SIT may modify the natural history of asthma in children who are known to be atopic but have not yet developed asthma. This annual rate of progression has been estimated at 5% in college students [11] but this is perhaps surprisingly an area of considerable ignorance. A number of long term epidemiological studies are now in progress, under the auspices of the ISAAC programme and should soon shed light on the rate of progression at different ages and the extent of regional and international variation. Only limited data is available to support the proposition that SIT may alter the natural rate of progression. An early open study using uncharacterised mixed allergen extracts supported this view, but among other problems, this study failed to allow for the spontaneous improvement that often occurs in asthmatic patients [12]. New evidence is now emerging to indicate that SIT can modify the natural history of allergic disease through childhood and into adult life [13]. If this is confirmed, it will have a major bearing on the economic and clinical arguments surrounding SIT and asthma. There is as yet no evidence to support claims that SIT is different from drug therapy in terms of influencing the evolution of established asthma. Studies that have investigated withdrawal of therapy have found rapid recurrence of asthma symptoms although rhinitis symptoms seem to show much more sustained relief after SIT.
In summary, SIT is a controversial type of treatment for asthma. While it seems entirely logical to try to treat allergic disorders by specifically suppressing the immune response to the triggering agents, the critical issue is whether SIT in its present form is the best option for managing patients with asthma. To assess this requires proper comparisons of best current SIT versus best current drug therapy, with robust endpoints including symptoms, objective measures of lung function, evaluation of cost:benefit ratios, safety, and quality of life. In vitro and in vivo measures such as skin test responses or allergen-specific IgG4 measurements are not sufficiently specific or sensitive to serve as surrogates for clinical efficacy. To date there have been relatively few well controlled studies of SIT in asthma but there is increasing evidence that SIT is beneficial in mite-induced and pollen-induced asthma. The clinical efficacy of SIT in adult asthmatic patients sensitive to cats or moulds is less certain, and no comparative studies with conventional treatment have been performed. Further clinical trials are indicated, particularly in mild to moderate childhood asthma and also in patients with atopic disease who have not yet developed asthma but are at high risk of progression to asthma.
SafetyThe main factor cited against the widespread adoption of SIT for asthma is the risk of serious adverse reactions. In the UK between 1957 and 1986 twenty-six fatal reactions due to SIT were reported to the Committee on Safety of Medicines [14]. In 17 of the fatal cases, the indication for SIT was documented; 16 of these 17 patients were receiving SIT to treat asthma. Similarly, in the
53
AAAAI confidential inquiry into SIT-associated deaths, asthma appeared to be in virtually all the fatal cases [15]. In those where asthma was not cited as a contributory factor, documentation of asthma status was missing and certainly bronchospasm was a cardinal feature of the clinical course of the anaphylactic reactions. The incidence of systemic reactions in patients receiving SIT for asthma varies between series and has been reported to range from 5% to 35%. The central issue in using safety as an endpoint is to recognise that all treatments carry risks. Where differential risks exist between therapies, a more risky therapy can only be justified if that therapy offers substantial additional benefit over the safer therapy. The science of assessing risk-benefit ratios is still in its infancy and we have to recognise that even when faced with the same facts, different patients and agencies can come to widely varying risk assessments.
Separately, it is generally agreed that immunomodulatory treatments should not be used in patients with autoimmune disorders or malignant disease. While there is no hard evidence that SIT is actually harmful in these groups, it seems unwise to attempt manipulation of the immune system in such patients, not least because of the risk that spontaneous and unrelated variations in the autoimmune disorder or cancer may be blamed on SIT. Other medical contraindications to SIT include the coexistence of significant cardiac disease which may be exacerbated by any adverse reactions to SIT. Patients on beta-blockers should also not receive SIT. Although they are not at increased risk of adverse reactions, they will not respond to the epinephrine which would be needed to treat adverse reactions to SIT.
Future directionsDevelopments in molecular biology should lead to improvements in conventional SIT. Possible avenues include the use of recombinant allergens, which would allow much better standardisation of allergen vaccines, as well as some fine tuning of vaccines for patients with unusual patterns of reactivity. Most allergic patients react to the same components of an allergen extract, the so-called major allergens, which are defined as those allergens recognised by over 50% of sera from a pool of patients with clinically significant allergy to the material in question. However, not all patients recognise all major allergens and some patients only recognise allergens which are not recognised by the majority of allergic patient sera. This latter group may not respond to standard extracts, but might be better treated by a combination of allergens to which they are sensitive. Until the advent of molecular cloning, this has been impossible to achieve. The availability of recombinant allergens for SIT should thus lead to better characterisation of the range of sensitivities, and ultimately to better vaccine products.
Since the epitopes recognised by IgE molecules are usually three dimensional whereas the epitopes recognised by T cells are short linear peptide fragments of the antigen, it should be possible to use peptide fragments of allergens to modulate T cells without risking anaphylaxis. Two distinct approaches have been tested. Either large doses of natural sequence peptides are
54
given, deceiving the T-cell into high dose tolerance [16], or else an altered peptide ligand can be given. Both approaches require consideration of the MHC type of the individual undergoing treatment. By sequential alteration of Der p peptides, it is possible to suppress proliferation of T-cell clones recognising native Der p peptides, as well as suppressing their expression of CD40 ligand and their production of IL-4, IL-5 and IFN-. These anergic T-cells do not provide help for B-cells to switching class to IgE, and importantly this anergy cannot be reversed by providing exogenous IL-4 [17].
From epidemiological and experimental studies, we know that vaccination with mycobacteria has anti-allergic properties. In Japan, early vaccination with BCG was associated with a substantial reduction in the risk of developing allergy [18] although similar associations were not evident in Sweden [19]. In the laboratory, it has been shown that administration of BCG before or during sensitisation to ovalbumin reduces the degree of airway eosinophilia that follows subsequent challenge with ovalbumin (Fig 6). This effect is not mediated through any direct effect on IgE production, or blood eosinophil numbers, but is mediated through IFN- and can be reversed by exogenous IL-5 [20].
Two new approaches using DNA vaccines are also undergoing serious consideration. The first of these is a general approach, using CpG oligodeoxynucleotides (ODN). This technology is essentially a refinement of vaccination adjuvant technology, since CpG ODN have been shown to be the principal activity from Complete Freund’s Adjuvant. Pre-administration of CpG ODN prevented both airways eosinophilia and bronchial hyperresponsiveness in a mouse model of asthma [21]. Moreover, these effects were sustained for at least six weeks after CpG ODN administration [22]. Experiments are also being conducted with CpG ODN coupled to ragweed allergen, which enhances immunogenicity in terms of eliciting a Th1-type response to the ragweed allergen, but reduces its allergenicity [23]. Anti-sense DNA vaccines could also be used to downregulate airway adenosine receptors. In animal models of asthma this leads to a reduction in allergen-induced airway responses [24]. A contrasting approach is to use allergen-specific naked DNA sequences as vaccines. This technology is still in its infancy, but preliminary data suggest that giving naked DNA leads to production of allergens from within the airways epithelial cells [25,26]. Due to the different handling pathways for endogenous and exogenous allergens, it seems that the endogenously produced allergen elicits a Th1-type response and if this can be reproduced in allergic humans, it is hoped that this may overcome the existing Th2 –pattern response and eliminate the allergy. However, the potential for generating a powerful Th1-type response to ubiquitous agents means that this approach will need careful evaluation in animal models before it can be pursued in man.
Another approach that has reached clinical trials is to use a monoclonal antibody directed against IgE. By raising antibodies against the portion of IgE which is recognised by the high
55
affinity Fc receptor, it is possible to derive anti-IgE antibodies which bind free IgE molecules but do not cross link IgE bound to the mast cell or basophil surface. Treatment with humanised monoclonal anti-IgE antibodies is extremely effective in reducing the serum concentration of free IgE, although the IgE seems to remain in the circulation in the form of immune complexes. Treatment with anti-IgE reduces immediate and late-phase responses to inhaled allergen [27,28]. When given over a 12 week period to patients with steroid-dependent asthma it was possible to achieve substantial reductions in the dosage of oral and inhaled steroids [29]. Anti-IgE should also work in patients with milder asthma, who are generally more likely to be atopic. However, the costs and inconvenience of anti-IgE may preclude its use in patients with milder disease. On the other hand, anti-IgE has the advantage over SIT of being a general therapy, and may work in patients with multiple allergic sensitisation, who are more difficult to treat with conventional SIT. Further work is needed to define the groups of patients who will benefit most from this approach.
ConclusionsDespite a century of use, the precise mechanisms of action of SIT remain uncertain. SIT is established as a treatment for allergic rhinitis and for venom hypersensitivity, but is more controversial when used to treat allergic asthma. When used in appropriately selected patients, SIT is effective and acceptably safe, but care is needed to recognise and treat adverse reactions. Appropriate training of allergists and SIT clinic support staff is essential. Future directions in SIT include the development of better standardised vaccines, and the use of recombinant allergens, both of which should improve the safety profile of SIT. In parallel, the development of more general immunomodulatory therapies may allow a more general approach to be taken, which would be particularly advantageous for those patients with sensitisation to multiple allergens.
Table 1
Possible mechanisms of immunotherapy
Induction of IgG (blocking) antibodies Reduction in specific IgE (long-term) Reduced recruitment of effector cells Altered T-cell cytokine balance (shift to Th1 from Th2) T-cell anergy
56
References
1. Freeman J. Vaccination against hay fever: report of results during the first three years. Lancet 1914; 1:1178.
2. Creticos P et al. Dose-response of IgE and IgG antibodies during ragweed immunotherapy. J.Allergy Clin.Immunol. 1984; 73:94-104.
3. Iliopoulos O et al. Effects of immunotherapy on the early, late and rechallenge nasal reaction to provocation with allergen: changes in inflammatory mediators and cells. J.Allergy Clin.Immunol. 1991; 87:855-866.
4. Durham SR et al. Grass pollen immunotherapy inhibits allergen-induced infiltration of CD4+ T-lymphocytes and eosinophils in the nasal mucosa and increases the number of cells expressing mRNA for interferon-gamma. J.Allergy Clin.Immunol. 1996; 97:1356-65.
5. McHugh SM et al. Bee venom immunotherapy induces a shift in cytokine responses from a Th2 to a Th1 dominant pattern: comparison of rush and conventional immunotherapy. Clin.Exp.Allergy 1995; 25:828-38.
6. Ebner C et al. Immunological changes during specific immunotherapy of grass pollen allergy: reduced lymphoproliferative responses to allergen and shift from Th2 to Th1 in T-cell clones specific for Phl p1, a major grass pollen allergen. Clin.Exp.Allergy 1997; 27:1007-15.
7. Varney VA et al. Clinical efficacy of specific immunotherapy to cat dander: a double blind placebo controlled trial. Clin.Exp.Allergy 1997; 27:860-7.
8. Bousquet J et al. WHO position paper. Allergen immunotherapy: therapeutic vaccines for allergic disease. Allergy 1998; 53(S44):1-42.
9. Abramson M et al.. Immunotherapy in asthma: an updated systematic review. Allergy 1999; 54:1022-41.
10. Adkinson NF et al. A controlled trial of immunotherapy in allergic children. N Engl J Med 1997; 336:324-331.
11. Horak F. Manifestation of allergic rhinitis in latent sensitised patients. A prospective study. Arch. Otorhinolaryngol. 1985; 242:242-249.
12. Johnstone DE, Dutton A. (1968) The value of hyposensitization therapy for bronchial asthma in children. A 14 year study. Pediatrics 42:793-.
13. Des Roches A et al. Immunotherapy with a standardised Dermatophagoides pteronyssinus extract. VI. Specific immunotherapy prevents the onset of new sensitisations in children. J.Allergy Clin.Immunol. 1997; 99:450-3.
14. Committee on the Safety of Medicines. CSM update: immunotherapy. Br.Med.J. 1986; 293:948.15 Stewart GE, Lockey RF. Systemic reactions from allergen immunotherapy. J.Allergy
Clin.Immunol. 1992; 90:567-578.16. O'Hehir RE et al. Clonal analysis of differential lymphokine production in peptide and
superantigen-induced T-cell anergy. Int.Immunol. 1991; 3:819-26.
57
17. Fasler S et al. Antagonistic peptides specifically inhibit proliferation, cytokine production, CD40L expression and help for IgE synthesis by Der p1-specific human T-cell clones. J.Allergy Clin.Immunol. 1998; 101:521-30.
18. Shirakawa T et al. The inverse association between tuberculin responses and atopic disorder. Science 1997; 275:77-9.
19. Strannegard IL et al. Prevalence of allergy in children in relation to prior BCG vaccination and infection with atypical mycobacteria. Allergy 1998; 53:249-54.
20. Erb KJ et al. Effect of BCG infection on antigen-induced airways eosinophila in ovalbumin-sensitised mice. J.Exp.Med. 1998; 187:561-9.
21. Kline JN et al. Modulation of airway inflammation by CpG oligodeoxynucleotides in a murine model of asthma. J.Immunol. 1998; 160:2555-.
22. Sur S et al. Long-term prevention of allergic lung inflammation in a mouse model of asthma by CpG oligodeoxynucleotides. J.Immunol. 1999; 162:6284-93.
23 Tighe H et al. Conjugation of immunostimulatory DNA to the short ragweed allergen Amb a1 enhances its immunogenicity and reduces its allergenicity. J.Allergy Clin.Immunol. 2000; 106:124-34.
24. Metzger WJ, Nyce JW. Oligonucleotide therapy of allergic asthma. J.Allergy Clin.Immunol. 1999; 104:260-6.
25. Hsu CH et al. Immunoprophylaxis of allergen-induced IgE synthesis and airway hyperresponsiveness in vivo by genetic immunisation. Nat.Med. 1996; 2:540-4.
26. Hartl A et al. Immune responses after immunisation with plasmid DNA encoding Bet v 1, the major allergen of birch pollen. J.Allergy Clin.Immunol. 1999; 103:107-13.
27. Boulet LP et al. Inhibitory effects of an anti-IgE antibody E25 on allergen-induced early asthmatic response. Am.J.Respir.Crit.Care Med. 1997; 155:1835-40.
28. Fahy J et al. The effect of an anti-IgE monocloncal antibody on the early and late-phase responses to allergen inhalation in asthmatic subjects. Am.J.Respir.Crit.Care Med. 1997; 155:1828-34.
29. Milgrom H et al. Treatment of allergic asthma with monoclonal anti-IgE. N.Engl.J.Med. 1999; 341:1966-73.
*****
Allergy Allergy asthma asthma and the role of environmentand the role of environment in sportsmen in sportsmen
58
Luís Delgado, MD PhD
Department of Immunology, Faculty of Medicine, University of PortoAllergy, Asthma & Sports Unit, Immunoallergology, S.João Hospital, Porto, Portugal
Physical exercise plays a greater role in our current lifestyle than ever before, and has a positive effect on our health and general well-beingwell being. However, allergy and asthma can affect any susceptible person during exercise, both at the recreational or professional level. Allergic diseases and asthma represent major health burdens in the 21st century, due to their increasing prevalence and high social and individual costs.
During training, athletes are repeatedly exposed to allergens, cold air and pollutants, which can have a significant effect on those with allergic diseases or asthma. Several recent studies have shown a high prevalence of asthma and exercise-induced bronchoconstriction in elite athletes. The prevalence rate is particularly high in endurance athletes, winter sport athletes, swimmers and athletes with concomitant risk factors, such as atopy. Further, the prevalence of asthma in athletes is increasing (9.7% in 1976 to 16.7% in 1996, in US Olympic athletes). The prevalence of allergic rhinitis is also high in athletes (25–56% in Olympic athletes), and a significant proportion of athletes with rhinitis may have sub-clinical bronchial obstruction. Severeal allergic symptoms may also be induced by heavy exercise following allergen exposure, e.g. exercise-induced food-dependent anaphylaxis.
In spite of the increased prevalence, allergic diseases and asthma are under-diagnosed and under-treated in athletes. This may be due to atypical or unusual symptoms, reluctance to take medication and/or poor knowledge of doping regulations. The best criteria for diagnosing exercise-induced bronchoconstriction in athletes and the implications of treatment on exercise performance are still under discussion. However, if appropriately detected and managed, allergic disorders and asthma should not constitute a limiting factor in exercise performance in athletes.
In addition, as athletes are often role models for young people, they may influence other patients with allergic diseases or asthma to lead as normal a life as possible.
References
59
Bonini S, Brusasco V, Carlsen K-H, Delgado L, Giacco SD, Haahtela T, Rasi G, van Cauwenberge PB. Diagnosis of asthma and permitted use of inhaled 2-agonists. Allergy 2004; 59: 33-6.
Capão-Filipe M, Moreira A, Delgado L, Rodrigues J, Vaz M. Exercise-induced bronchoconstriction and respiratory symptoms in elite athletes. Allergy 2003; 58: 1196.
Carlsen K-H. Asthma and allergy in sportsmen. ACI International 2001; 13: 140-6.
Delgado L, Capão-Filipe M, Moreira A. Rhinitis and its impact in sports. ACI International 2004 (in press).
Gioulekas D, Damialis A, Papakosta D, Syrigou A, Mpaka G, Saxoni F, Patakas D. 15-Year aeroallergen records. Their usefulness in Athens Olympics, 2004. Allergy 2003; 58:933–938.
Katelaris CH, Carrozzi FM, Burke TV. Allergic rhinoconjunctivitis in elite athletes. Optimal management for quality of life and performance. Sports Med 2003;33(6):401-6.
Katelaris CH, Carrozzi FM, Burke TV, Byth K. A springtime olympics demands special consideration for allergic athletes. J Allergy Clin Immunol 2000 Aug;106(2):260-6
Pedersen BK, Hoffman-Goetz L. Exercise and the immune system: regulation, integration, and adaptation. Physiol Rev 2000; 80: 1055-81.
Storms WW. Review of exercise-induced asthma. Med Sci Sports Exerc 2003; 1464-70.
*****
60
Particulate Air Pollution and Asthma Particulate Air Pollution and Asthma
Anthony J. Frew MD FRCP Professor of Allergy & Respiratory MedicineInflammation, Infection & Repair Division (AIR), Mailpoint 810, Southampton General Hospital, Southampton SO16 6YD UK e-mail: [email protected]
Asthma is an increasing problem throughout the developed world. The rate of increase suggests that environmental factors have played a critical, and several plausible arguments have been put forward, including the possibility that air pollution may have influenced the development and expression of asthma and other allergic diseases. Clean air legislation has dramatically reduced the black smoke and sulphur dioxide that used to pollute our cities, but we now experience new forms of air pollution, particularly “summer smogs” in which fine particulates and ozone accumulate over our cities during periods of high pressure in the summer. In cities such as Los Angeles or Mexico City, the ozone concentrations commonly reach levels that are associated with adverse affects on normal and asthmatic subjects.
The functional responses of asthmatic patients to ozone, NO2, and SO2, have been extensively assessed in controlled exposure studies. Ozone has direct effects on the airways, causing reduced inspiratory capacity. This effect is more marked in patients with asthma and is biologically important in that epidemiological studies have shown direct and linear associations between ozone concentrations and admission rates for asthma and related respiratory diseases [1]. In human exposure studies, ozone induces an acute neutrophilic inflammatory response [2] together with release of chemokines (IL-8 and GRO-) [3]. NO2 has less direct effect on human airways, but increases patients’ sensitivity to inhalation allergen challenge [4].
Concerns have also been raised about the effects of particulate pollution, especially diesel exhaust particles. It has been shown that individuals living close to traffic routes in Japan are more likely to be sensitised to mountain cedar than those who live in areas with lower concentrations of DEP [5]. In vitro, DEP act as an adjuvant for the production of IgE [6] and stimulate cultured epithelial cells to release IL-8, GM-CSF and sICAM-1 [7]. Human exposure studies have found an acute inflammatory response to DE (PM10 300g/m3) in the airways of normal healthy subjects with increase numbers of neutrophils, mast cells and T
73
cells, as well as upregulation of the adhesion molecule ICAM-1 [8]. However, in asthmatic subjects, exposure to DE increased bronchial reactivity, but did not induce an acute neutrophil influx or any worsening of the pre-existent eosinophilic inflammation. Further work is needed to enable us to explain the epidemiological findings of increased clinical sensitivity to ambient PM pollution among asthmatics. Possible explanations include damage to cilia, epithelial cell activation, induction of epithelial apoptosis, and/or mucus gland hyperplasia.
Health effects of Particulate MatterOver 60 epidemiological studies conducted in different parts of the world have demonstrated a consistent association between ambient levels of air particles and various health outcomes, including mortality, increased exacerbation of asthma, chronic bronchitis, respiratory tract infections, ischaemic heart disease and stroke [9]. Over the last ten years major concerns have been raised about the health effects of fine particulates (less than 10 microns in aerodynamic diameter – PM10). In 1993, a seminal paper described an association of PM10 levels with cardiovascular and respiratory mortality and morbidity in six US cities [10]. Initially this observation met with some scepticism but the association has subsequently been confirmed in a wide number of settings and in different countries. Interestingly, the association seems to also apply across settings even where the composition of PM is quite different.
The precise mechanisms underlying the cardiovascular effects of PM remain uncertain. Current attention is particularly focused on ultrafine particles (diameter < 0.05-0.10 m) which are highly reactive and are present in large numbers in the urban environment. Ultrafine particles can penetrate through the epithelium and vascular walls and enter the blood stream, and in animal models, that have been reported to produce alterations in blood coagulability and increased rates of cardiovascular disorders as well as increased carcinogenicity [11], and potentiation of autoimmune disorders [12],
Epidemiological studies have reported that patients with asthma are adversely affected by PM pollution. As with the cardiovascular effects, there seems to be no threshold below which PM effects disappear. Across the full range of PM concentrations, there is a clear and detectable gradient for asthma symptoms, lung function and hospital admissions. For every 10 g/m3 increase in PM concentrations, there is a 3% increase in asthma attacks, a 3.4% increase in emergency room visits for asthma, a 2.9% increase in bronchodilator use, and a 0.15% decrease in FEV1. This problem is accentuated by the fact that about 63% of US patients with asthma live in areas that fail to meet the US EPA standards for PM pollution.
Reports from Japan suggest that children living close to roads with heavy traffic are more likely to develop allergies. A higher prevalence of allergy to cedar pollen has been observed in
74
people living close to motorways, as compared with people living in a more rural environment close to a cedar forest and being exposed to the same number of cedar pollens [13].
The role of DEP in the increased prevalence of asthmaDiesel exhaust is a major contributor to particulate pollution. Diesel exhaust particles (DEP) may promote inflammation and the allergic state through three broad mechanisms. (1) DEP may act as a carrier for the transport of allergens into the airways by adsorbing allergenic proteins onto their surface. (2) DEP may act as an adjuvant in promoting the switching of B cells to produce allergen-specific IgE. (3) DEP may affect a number of downstream immunological mechanisms, leading to increased prevalence or increased severity of allergic and asthmatic disorders.
DEP as a carrierSome allergens, such as the major rye grass pollen allergen Lol p1, bind specifically to DEP [14]. In an in vitro study of allergen adsorption to indoor-suspended particulate matter (ISPM) and DEP, cat, dog and birch pollen major allergens (Fel d1, Can f1 and Bet v1) were all found on the surface of ISPM whereas house dust mite allergen (Der p1) was not. However, all four allergens were found to be absorbed to DEP [15]. By acting as a carrier of allergens, DEP might deliver allergenic material to the airways in increased amounts during pollution episodes, and trigger asthma attacks in those who are sensitised [14].
DEP as an adjuvant for IgECo-presentation to the immune system of allergens and DEP may lead to an altered immune response to the allergen. Allergenic proteins can be identified bound to DEP and SPM, while in urban areas pollen grains can become coated with fuel residues and combustion products. Birch pollen grains collected during the pollen season in the north of Stockholm were found to be coated with a complex mixture, about 80% of which consisted of n-alkanes and n-alkenes, but methylketones, ethers, alcohols and amino alcohol were also identified [16]. When these DEP and pollen grains are ingested by antigen-presenting cells, the allergenic proteins will undergo processing in an environment which is simultaneously affected by one or more components of the DEP. Moreover, the binding of pollen or other inhaled allergens to DEP may modulate the allergenic epitopes and thereby increase their allergenicity [17].
DEP have been shown to have a direct enhancing effect on IgE production. This effect seems to be driven by polyaromatic hydrocarbons (PAH) on the surface of the DEP rather than their carbon core, since PAH extracted from DEP enhance IgE production from purified human B-cells stimulated by IL-4 [18]. Importantly, PAH-DEP did not induce IgE production in unstimulated B-cells, indicating that the PAH only enhance ongoing IgE production. Phenanthrene, a major polyaromatic hydrocarbon and an important component of DEP, had a similar effect on IgE
75
production by a human B cell line [19]. In vivo, DEP enhanced total IgE and cedar pollen-specific IgE production in mice given ovalbumin (OA) mixed with DEP either intraperitoneally or intranasally [20,21]. In order to elucidate which part of the DEP particle (the carbon core or the adsorbed organic chemicals) is responsible for the adjuvant effect, mice were immunised four times with either OA, OA with DEP or OA with carbon black (CB). Specific IgE for OA was then analysed. Both DEP and CB showed an adjuvant activity for specific IgE production after intra-nasal instillation, indicating that they were both responsible for the effect [22]. This effect has been confirmed in other studies in mice [23]. The effect of DEP on antibody responses is dose- and time-dependent [24,27]. Even at low doses that have little demonstrable effect on IgE, exposure to DEP enhances the effect of allergen challenge on the airways, with increased eosinophilic inflammation and goblet cell hyperplasia [24,25].
In humans, diesel particles have been shown to potentiate nasal IgE production four days after challenge with DEP[28]. There was also an increase in the number of IgE-secreting cells in lavage but no increase in IgA-secreting cells. Similarly, nasal challenge with a combination of DEP and allergen has been shown to induce higher ragweed-specific IgE and IgG4 responses compared with DEP or ragweed alone but with similar total IgE levels [29]. There was also a change in the cytokine pattern favouring allergic sensitisation. This implies that synergism between DEP and natural allergens may be a key feature in increasing the prevalence of allergen-induced respiratory disease.
DEP and allergic inflammation/downstream mediator effects In addition to these allergen-specific effects, exposure to DEP alone causes an inflammatory response in the airways, which may then prime the airways and increase the magnitude of the response to allergen challenge. Inhalation of DEP damages the bronchial epithelium and cilia, thereby impairing their ability to act as a biological barrier against inhaled substances [30]. Allergens may therefore remain on the epithelial surface for longer, perhaps allowing them to diffuse into the epithelial layer and increasing the probability of them coming into contact with cells of the immune system. Other mechanisms which might affect asthma development after DEP exposure may include up-regulation of histamine receptor gene expression [31] and increased penetration of allergen across the respiratory mucosa [32].
The cytotoxicity of DEP, their phagocytosis, and the resulting immune response have been studied in human bronchial and nasal epithelial cell cultures. DEP exposure led to time- and dose-dependent membrane damage. Transmission electron microscopy showed that DEPs underwent endocytosis by epithelial cells and were then translocated through the epithelial cell sheet. Flow cytometric measurements confirmed the time and dose dependency of this
76
phagocytosis and its non-specificity (DEPs, carbon black, and latex showed similar responses) DEP led to a time-dependent increase in IL-8, GM-CSF, and IL-1beta release. This inflammatory response occurred later than phagocytosis and appeared to depend on the extent of adsorbed compounds, as in this study carbon black had no effect on cytokine release, [33] even though it was phagocytosed to a similar degree.
Exposure to DEP attenuated the ciliary beat frequency of human bronchial epithelial cells and increased the release of IL-8, GM-CSF and soluble ICAM-1. The observations support the concept that DEP exposure may lead to functional changes and the release of pro-inflammatory mediators, which may influence the development of airway disease, especially in those disorders in which neutrophils are implicated [34].
The epithelial cells of asthmatic subjects seem to be more sensitive than those of non-atopic non-asthmatics. When cultured human bronchial cells were exposed to DEP for 24 hours. The ciliary beat frequency was similarly attenuated in both groups but the asthmatic cell cultures constitutively released significantly greater amounts of IL8, GM-CSF, and sICAM-1 and RANTES compared to cells from non-asthmatics. In response to10 g/ml of DEP exposure there was a significant increase in the release of IL-8, GM-CSF, and sICAM-1 in cells from asthmatics. However, exposure to doses of 50 and 100 g/ml led to a decrease in the release of IL-8 and RANTES. In contrast these higher concentrations of DEP led to a significant increase in the release of IL-8 and GM-CSF in the cells cultured from non-asthmatics [35]. In another study the cytokine response to DEP was shown to be synergistic with the response to TNF [36].
These effects may be mediated through the transcription factor NF-kB. Using electrophoretic mobility shift assay, DEP has been shown to increase binding to the specific motif of NF-kB but not of transcription factor AP-1 [37]. Moreover, DEP can modulate chemokine pathways at the transcriptional level [38].
In vitro, DEP induce eosinophil degranulation and adhesiveness to epithelial cells without changing the eosinophil survival rate. These results indicate that DEPs may play a significant role in the promotion of airway hypersensitivity induced by enhanced eosinophil infiltration and degranulation [39].
DEP may also act through the complement system [40]. Pre-treatment of human serum with DEP extracts (500 - 2.500 g/ml) demonstrated activation of the alternative complement pathway, resulting in a dose-dependent reduction in haemolytic activity (of up to 20%).
Finally, it is important to remember that PM pollution episodes do not exist in isolation, and in most PM episodes, there will also be an increase in gaseous pollutants. Patients with asthma
77
have been found to be more adversely affected than the normal population to inhalation of gaseous components of air pollution [41,42] and in particular acid aerosols [43]. Various studies have shown that overall lung deposition is increased in patients with obstructed airways and abnormal geometry . A 30% reduction in airway cross sectional area results in a deposition increase in the bifurcating airways by more than 100% [44]. This will contribute to the deposition of PM and enhance both the immunological changes and non-specific inflammatory effects brought about in the airways by particulate pollution.
Conclusion:Asthma is a chronic inflammatory disorder involving recruitment and activation of mast cells, eosinophils and T cells, associated with the development of bronchial hyperresponsiveness and variable airflow obstruction. All forms of the disease are characterised by enhanced production in the airways of Th-2 cytokines encoded in a cluster on chromosome 5q31-33. While the human exposure studies discussed above implicate air pollutants in the acute inflammatory response, questions remain about the chronic effects of air pollutants on the lung. Patients with chronic, severe asthma have thickened airways with thickening and increased density of the sub-basement membrane (SBM) collagen layer, as well as increases in smooth muscle, and in microvascular and neural networks. The deposition of interstitial (repair) collagens in the lamina reticularis and an associated increase in the number of myofibroblasts is a unique feature of asthma, irrespective of aetiology, and is thought to be due to altered signalling between the bronchial epithelium and underlying mesenchymal cells [Davies]. These studies have demonstrated that the asthmatic bronchial epithelium is more susceptible to oxidant-induced injury and that epithelial repair in asthma is attenuated [Bucchieri] The injured epithelium becomes a potent source of growth factors such as PDGF, bFGF, TGF that cause increased proliferation and biosynthetic activity of the underlying myofibroblasts which are responsible for increased matrix deposition and airway remodelling.
While traditionally it has been thought that airway inflammation precedes, and is responsible for, airways remodelling, a recent study in children found that children who subsequently developed asthma had airway eosinophilia and increased epithelial SBM collagen thickening present up to 4 years before asthma was clinically expressed. Air pollution could contribute to this process: in rats, DEP exposure has been found to cause increased collagen deposition in the airways during lung development. Thus, remodelling of the airways in asthma may occur in parallel with inflammation, while epithelial stress and injury, such as that caused by the air pollutants DEP, ozone, or NO2 may activate or reactivate morphogenetic mechanisms that cause structural changes in the airways [. Further studies in humans will no doubt help to elucidate the relevant mechanisms, but for the moment, some caution is needed in defining appropriate air quality standards.
78
References1. Bascom R, et al. (1996) Am.J.Respir.Crit.Care Med. 153:3-50 and 153:477-498.2. Balmes JR, Chen LL, Scannell C et al. (1996) Am.J.Respir.Crit.Care Med. 153:904-9.3. Salvi SS, Semper AE, Blomberg A, et al. (1999) Am J Respir Cell Mol Biol 20:984-991 4. Devalia JL, Rusznak C, Herdman MJ, et al. (1994). Lancet 344:1668-71.5. Ishizaki T, Koizumi, Ikemori, et al. Ann Allergy 1987;58:265-270.6. Takenaka H, Zhang K, Diaz-Sanchez D et al . J Allergy Clin Immunol 1995;95:103-115.7. Bayram H, Devalia JL, Sapsford RJ, et al . Am J Respir Cell Mol Biol 1998; 18:441-448.8. Salvi S, Blomberg A, Rudell B, et al . Am J Respir Crit Care Med 1999; 159:702-709.9. Salvi S, Holgate S. Clin Exp Allergy, 1999.10. Dockery DW, Pope CA, Xu XP, et al An association between air pollution and mortality in six
US cities. N Engl J Med 1993;329:1753-1759.11. Camner P, Pershagen G, Ahlborg U, et al. Health effects of diesel exhaust emissions. Stockholm: 1988. 1988:8.
12. Yoshino S, Sagai M et al Enhancement of collagen induced arthritis by diesel exhaust particles; J Pharmacol Exp Ther 1999 290:524 – 9
13. D´Amato G, Liccardi G, D´Amato M. Environment and development of respiratory allergy: I. Outdoors. Monaldi Archives for Chest Disease 1998;49: 406-411.
14. Knox RB, Suphioglu C, Taylor P, Desai R, et al. Major grass pollen allergen Lol p 1 binds to diesel exhaust particles: implications for asthma and air pollution. Clin Exp Allergy 1997;27: 246-251.
15. Ormstad H, Johansen BV, Gaarder PI. Airborne house dust particles and diesel exhaust particles as allergen carriers. Clin Exp Allergy 1998;28: 702-708.
16. Henricsson S, Westerholm R, Nilsson S, Berggren B. Chemical characterisation of extractable compounds found in the coating of birch (Betula) pollen. Grana 1996;35: 179-184.
17. Kainka-Stanicke E, Behrendt H, Friedrichs K, Tomingas R. Morphological alterations of pollen and spores induced by airborne pollutants: observations from two different polluted areas in West Germany. Allergy 1998; 43:57.
18. Takenaka H, Zhang K, Diaz-Sanchez D, et al. Enhanced human IgE production results from exposure to the aromatic hydrocarbons from diesel exhaust: Direct effects on B-cell IgE production. J Allergy Clin Immunol 1995;95: 103-115.
19. Tsien A, Diaz-Sanchez D, Ma J, Saxon A. The organic component of diesel exhaust particles and phenanthrene, a major polyaromatic hydrocarbon constituent, enhances IgE production by IgE-secreting EBV-transformed human B cells in vitro. Toxicol Appl Pharmacol 1997;142: 256-263.
79
20. Muranaka M, Suzuki S, Koizumi K, Takafuji S, et al. Adjuvant activity of diesel-exhaust particulates for the production of IgE antibody in mice. J Allergy Clin Immunol 1986;77: 616-623.
21. Maejima K, Tamura K, Taniguchi Y, et al. Comparison of effects of various fine particles on IgE antibody production in mice inhaling Japanese Cedar pollen allergens. J Toxicol Environmental Health 1997;52: 231-248.
22. Nilsen A, Hagemann R, Eide I. The adjuvant activity of diesel exhaust particles and carbon black on systemic IgE production to ovalbumin in mice after intranasal instillation. Toxicology 1997;124: 225-232.
23. Lovik M, Hogseth A-K, Gaarder PI, et al. Diesel exhaust particles and carbon black have adjuvant activity on the local lymph node response and systemic IgE production to ovalbumin. Toxicology 1997;121: 165-178.
24. Takano H, Yoshikawa T, Ichinose T,et al. Diesel exhaust particles enhance antigen-induced airway inflammation and local cytokine expression in mice. Am J Respir Crit Care Med 1997;156: 36-42.
25. Ichinose T, Takano H, Miyabara Y, et al. Murine strain differences in allergic airway inflammation and immunoglobulin production by a combination of antigen and diesel exhaust particles. Toxicology 1997;122: 183-192.
26. Miyabara-Y effects of diesel exhaust on allergic airway inflammation in mice. J Allergy Clinical Immunology 1998; 102:805-12
27. Fujimaki H, Nohara O, Ichinose T, et al. IL-4 production in mediastinal lymph node cells in mice intratracheally instilled with diesel exhaust particulates and antigen. Toxicology 1994;92: 261-268.
28. Diaz-Sanchez D, Dotson AR, Takenaka H, Saxon A. Diesel exhaust particles induce local IgE production in vivo and alter the pattern of messenger RNA isoforms. J Clin Invest 1994;94: 1417-25.
29. Diaz-Sanchez D, Tsien A, Fleming J, Saxon A. Combined diesel exhaust particulate and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T helper cell 2-type pattern. J Immunol 1997;158: 2406-13.
30. Wolff RK. Effects of airborne pollutants on mucociliary clearance. Environmental Health Perspectives 1986;66:223-37.
31. Terada N Hamano N, Maesako KI,et al Diesel exhaust particulates upregulate histamine receptor mRNA and increase histamine induced IL-8 and GMCSF production in nasal epithelial cells. Clin Exp Allergy 1999; 29:52-59
32. Gorski P, Tarkowski M. et al Non specific environmental factors and asthma development. Polish J Occup Med Environ Health 1992;5: 227-236
33. Boland S Baeza Squiban A Fournier T et al Diesel exhaust particles are taken up by human airway epithelial cells in vitro and alter cytokine production. Am J Physiol 1999, L604 –13
80
34. Bayram H, Devalia JL, Sapsford RJ,et al. The effect of diesel exhaust particles on cell function and release of inflammatory mediators from human bronchial epithelial cells in vitro. Am J Respir Cell Mol Biol 1998;18: 441-448.
35. Bayram H, Devalia JL, Khair OA et al Comparison of ciliary activity and inflammatory mediator release from bronchial epithelial cells of nonatopic nonasthmatic subjects and atopic asthmatic patients with the effect of diesel exhaust particles in vitro. J Allergy Clin Immunol 1998; 102:771-82
36. Steerenberg PA, Zonnenberg JAJ, Dormans JAMA, et al. Diesel exhaust particles induced release of interleukin 6 and 8 by (primed) human bronchial epithelial cells (BEAS 2B) in vitro. Exp Lung Res 1998;24: 85-100.
37. Takizawa H,Ohtoshi T, Kawasaki S, et al Diesel exhaust particles induce NF- kappa B activation in human bronchial epithelial cells in vitro. J Immunol 1999; 162: 4705-11
38. Fahy-O, Tsicopoulos A, Hammad, et al Effects of diesel organic extract on chemokine production by peripheral blood mononuclear cells. J Allergy Clin Immunol 1999; 103: 1115-24
39. Terada et al Maesako K, Hiruma K Diesel exhaust particulates enhance eosinophil adhesion to nasal epithelial cells and cause degranulation. Int Arch Allergy Immun 1997; 114: 167-74
40. Kanemitsu H, Nagasawa S, Sagai M, Mori Y. Complement activation by diesel exhaust particles (DEP). Biol Pharm Bull 1998;21: 129-32
41. Hobbs CH, Mauderly JL. Risk assessment for diesel exhaust and ozone: the data from people and animals. Clin Toxicol 1991; 29: 375-84
42. Rusznak C, Devalia JL, Davies RJ. The impact of pollution on allergic disease. Allergy 1994; 49: 21-27
43. US Environmental Protection Agency. Toxicological studies of particulate matter. 11-1-11-231 1996. Triangle Park NC US Environmental Protection Agency. Air Quality criteria for particulate matter; vol II.
44. Kim CS, HU SC, Regional deposition of inhaled particles in human lungs: comparison between men and women. Am J Physiol 1998; 84:1834-44
45. Davies DE, Polosa R, Puddicombe. S.M., Richter A, Holgate ST. The epidermal growth factor receptor and its ligand family: their potential role in repair and remodelling in asthma. Allergy 1999; 54:771-83.
46. Bucchieri F, Puddicombe S, Lordan JL, Richter A, Buchanan D, Wilson SJ, Ward J, Zummo G, Howarth PH, Djukanovic R, Holgate ST, Davies DE. Asthmatic bronchial epithelium is more susceptible to oxidant-induced apoptosis. Am J Respir Cell Mol Biol 2002; 27:179-85.
47. Polosa R, Puddicombe SM, Krishna MT, Tuck AB, Howarth PH, Holgate ST, Davies DE. Expression of c-erbB receptors and ligands in the bronchial epithelium of asthmatic subjects. J Allergy Clin Immunol 2002; 109:75-81.
81
*****
FACULTYFACULTY
Luísa Geraldes, Ana Todo Bom, Isabel Carrapatoso, Fernando Rodrigues,Rosário Cunha, Celso Chieira.
Immunoallergology Department. Coimbra University Hospital
Introduction: There is reported high sensitization to grass pollen all over the Europe. The different species have close cross reactivity associated to the strong homology between their protein contents. Despite these evidences, different pattern reactions can be triggered by local environmental exposure to some gramineae species.AimThe aim of this study is to evaluate the gramineae species cutaneous sensitization in patients observed in the Immunoallergology Department due to allergic respiratory disease. Establish a correlation between in vivo (skin prick test) and in vitro (radioallergosorbent test) tests and analyse by immunoblotting the main proteins identified.
Methods: A total of 100 consecutive adults with positive 22 gramineae skin prick test were evaluated. The following gramineae were investigated: Dactylis glomerata, Festuca pratensis, Lolium perene, Phleum pratensis, Secale cereale, Triticum sativum, Zea mays, Hordeum vulgaris, Avena sativa, Salsola kali, Cynodon dactylon, Humulus lupulus, Phragmitis communis, Agrpyron repens, Arrhenatherum el, Bromus mollis, Agrostis alba, Cynosurus cristatus., Alopercus pratense, Anthoxanthum oduratum., Holcus lanatus e Poa pratensis. A test was considered positive whenever the papule diameter was 3 mm higher than negative control. According to the skin prick test results the patients were distributed in 4 groups; negative, 3<5 mm; 5<8 mm; 8 mm. Detection of antigen-specific IgE was made by radioallergosorbent test (RAST/ UniCAP System) and the main protein identification by SDS-PAGE/Immunoblotting (Alablot DPC- Amerlab) for Phleum pratensis, Secale cereale e Poa pratensis.
Results: The average papule value for histamine was 6,1 mm. The skin prick tests positivity range from higher than 90% for Festuca pratensis, Lolium perene, Triticum sativum, Arrhenatherum el, Cynosurus cristatus, Anthoxanthum oduratum, Holcus lanatus to 53% for Humulus lupulus e Salsola kali. Mean diameter values range from 9,7mm for Arrhenatherum el
82
to 4,9mm for Humulus lupulus. It was possible to establish a close connection between in vivo and in vitro tests for all the grass species tested. The proteins most identified by blotting were those considered the major allergens ( 27 to 40 MW).
Conclusion: In portuguese patients there are an high sensitization pattern to most grass species. Despite this, Festuca pratensis, Lolium perene, Triticum sativum, Anthoxanthum oduratum, Holcus lanatus should be considered in the skin prick tests battery, mainly in patients with strong seasonal clinical worsening. The IgE determination can give secure information about grass pollen allergy. The specific protein identification give important informations to the understanding the sensitization mechanisms
*****
Exposure to endotoxin, atopy and work-related symptomsExposure to endotoxin, atopy and work-related symptoms
among hop growers among hop growers
Anna Góra, Czesława Skórska, Zofia Prażmo, Ewa Krysińska-Traczyk, Jolanta Sitkowska, Radosław Śpiewak, Jacek Dutkiewicz
Institute of Agricultural Medicine, P O Box 185, Jaczewskiego 2, 20-950 Lublin, Poland
BACKGROUND: Hop (Humulus lupulus) is perennial plant cultivated extensively in Germany, Czech Republic, UK and USA. Hop cones are commonly used as a flavouring agent in breweries. Poland is five biggest hop producer in the word. Some studies suggest that hop may have allergic properties. However, still little is known on the exposure of hop growers to bioaerosols and its impact on health. The aim of the study was to asses the prevalence of work related symptoms and their relation to atopy and endotoxin exposure.
METHODS: 69 farmers from 19 randomly selected hop farms in Eastern Poland were examined. All participants were interviewed using the standardized questionnaires. The skin prick test with occupational allergens (hop and microbial) was performed. The atopy was define by at least one positive skin-prick for one ore more of eight airborne allergens. Air samples for determination of endotoxin were collected in all farms.
83
RESULTS: Atopy was found in 23 out of 69 (33%) examined hop growers. The prevalence of chronic bronchitis and physician diagnosed asthma were 23% and 3% respectively. 36 out of 69 (52%) farmers reported work-related symptoms. The most common was: respiratory symptoms reported by 39% of hop growers, skin, eyes and nose symptoms – reported by 33% and general symptoms – by 26%. Thirteen out of 36 (36%) symptomatic farmers were atopics. Eight farmers (12%) reacted to SPTs with occupational allergens: 5 (7%) farmer reacted to hop allergens and 6 farmers (9%) reacted to antigens of microbe commonly found in work environment. Moreover, positive reactions to microbial allergens were significantly more frequent in a group of farmers with respiratory symptoms (18%) compared to those without symptoms (2%; p < 0.05). The concentrations of airborne endotoxin ranged from 26 to 6250 ng/m3 (median 52.2 ng/m3).Among hop growers with endotoxin exposure higher than 200 ng/m3 the prevalence of work related symptoms and positive skin prick reactions were lower compared to the rest of the group (34% vs. 65%; p<0,05) and (17% vs. 3% p>0,05%)Conclusion: Despite relatively lower exposure to endotoxin, compared to farmers in other branches of agriculture, over 50% of hop growers complained of work-related symptoms. The inverse relation between occurrence of work-related symptoms and endotoxin concentration may be partly due to healthy worker effect.
*****
Asthma risk factors in patients with seasonal Asthma risk factors in patients with seasonal rhinoconjunctivitis in Ankara rhinoconjunctivitis in Ankara
B. Bozkurt, G Karakaya, A F KalyoncuHacettepe University, School of Medicine, , Dept of Chest Diseases, Adult Allergy Unit, Ankara, Turkey
Background: Asthma and seasonal rhinoconjunctivitis (SR) are frequently seen co-morbid conditions. In some instances, asthma can follow SR. The purpose of this survey was to determine the asthma risk factors in patients diagnosed with SR in our allergy clinic.
84
Methods: A retrospective study was conducted based on clinical records of 955 patients diagnosed with SR at our clinic between 1 January-31 December 2003. Out of 955 patients, 774 were enrolled since data were available only for these. Logistic regression model was developed to assess the independent association between asthma and the factors which were significantly associated with asthma.
Results: The mean age of the patients was 29.1±9.29 and 485 of them were females. There was a history of family atopy in 56.8% of the patients. The major initial complaints of the patients were nasal in 82.3%, respiratory in 9.7%, cutenous in 6.2% and ocular symptoms in 1.8% . The mean duration of the symptoms was 6.8 years . The patients have been symptomatic with a mean of 3.5±1.7 months a year. Skin prick tests (SPT) were performed with 14 common aeroallergens, and were positive in 685 patients (90.3%), where the allergen spectrum was 88.8% pollen, 15.1% mites, 16.2% cockroach, 13.1% pet animals and 1.2% mould. The most common accompanying allergic diseases were food hypersensitivity (14%), asthma (13.4%) and drug hypersensitivity (9.6%). Older age (OR: 1.77, 95%CI: 1.06-2.94), presence of family atopy (1.72, 1.04-2.85), respiratory symptoms (2.10, 1.75-2.50), ocular symptoms (0.77, 0.61-0.98) and metal allergy (0.25, 0.07-0.89) were associated with the development of asthma in patients with SR.
Conclusion: SR is a disease of the younger age group that could progress to an asthma. History and allergen spectrum of patients should carefully be evaluated in order to determine the risk factors for SR patients.
*****
Pollen concentrations from March to April in Vilnius,Pollen concentrations from March to April in Vilnius, Lithuania: Lithuania: A two year study A two year study
R. Dubakiene1, S. Miseviciute2
1Vilnius University , Allergy Center, Vilnius, Lithuania; 2Vilnius University hospital "Santariskiu Klinikos", Pulmonology and allergology, Vilnius, Lithuania, [email protected]
Background: The amount of people with allergy to pollen is constantly increasing. The role of pollen is well known in development of such diseases as allergic rhinitis or bronchial asthma.
85
People who suffer from these diseases well know that their symptoms begin in particular season.
Aim: This study was designed to calculate the airborne pollen concentrations during pollen season in Lithuania.
Materials and methods: Materials for comparing pollen concentrations were gained from the joint-stock company IFE Baltic, where the pollen grains were picked by pollen calculator (Burkard Sporen Falle). The calculator was set in 30 meters high. The roll with different pollen used to be taken from the calculator every week and the pollen were differentiated and calculated with the help of microscope.
Results: The period from late March to April is the season of blowing in Lithuania. The bloom of trees begins in March and finishes in July. The peak of trees bloom is in May. The bloom of herbage begins in May and finishes in early autumn. The peak is in June. Main pollen of these months are Corylus, Alnus, Betula, Tilia (trees) and Gramineae, Plantago, Rumex (herbage).
Conclusions: Thus, knowing the concentrations of pollen in different months helps us to create the local scheme of pollen widespreading and use it in everyday allergologist work. *****
FOOD ALLERGY AND ITS RELATIONSHIPS TO OTHERFOOD ALLERGY AND ITS RELATIONSHIPS TO OTHER ALLERGIC DISEASES IN THE POPULATION OF SCHOOLALLERGIC DISEASES IN THE POPULATION OF SCHOOL CHILDREN IN POLAND CHILDREN IN POLAND
Jazwiec-Kanyion B. Department of Epidemiology, Institute of Occupational Medicine and Environmental Health, Sosnowiec, Poland
Introduction: In contrast to respiratory allergies, epidemiology of food allergy (FA) in Poland has been little studied. The aim of the study was to investigate the prevalence of FA and its relationships to other allergic diseases among school children living in Silesian voivodeship – the most industrialised part of Poland. In 2001 we carried out a cross-sectional health survey on children 6-7 years old and children 13-14years old living in the city of Sosnowiec.
Methods: Using the CESAR (Central European Study on Air Pollution and Respiratory Health) and ISAAC (International Study of Asthma and Allergies in Childhood) questionnaire we invited
86
for the study all 2500 canditate children. Completed questionnaire was returned by parents of 2000 children (response rate 80%). For statistical analysis computer program STATA 8.0 was employed. Prevalence rates were calculated and chi square tests were used to compare the rates between groups. P values < 0.05 was regarded as statististically significant.
Results: Replies to the questionnaire were received from 519 children 6-7 years old and 1481 children 13-14 years old. The prevalence of FA and other allergic diseases (in %) are shown below.
6-7 yrs 13-14yrsFA 17.1 7.3Asthma 5.0 3.6Atopic dermatitis 19.3 11.9 Pollen allergy 10.3 10.8 Pets allergy 8.8 8.6 Dust allergy 9.5 8.2
Conclusions: Our study suggested that the prevalence of FA and atopic dermatitis was a significantly higher in 6-7 years old group of children. Prevalences of food allergy were more often reported among children with asthma (9.8%), atopic dermatitis (45.3%), pollen allergy (29.5%), pets allergy (26.5%) and dust allergy (27.3%).
*****
RELATIONSHIP BETWEEN RAGWEED POLLENS IN TUSCANYRELATIONSHIP BETWEEN RAGWEED POLLENS IN TUSCANY (ITALY) AND AIR MASSES COMING FROM BALKANS(ITALY) AND AIR MASSES COMING FROM BALKANS
L. Cecchi*, M. Morabito^, M.P. Domeneghetti°, G. Bartolini*, M. Petralli*, T. Torrigiani*, M. Onorari° and S. Orlandini*
* Interdepartmental Centre of Bioclimatology – University of Florence, Italy^ Institute of Biometeorology – National Research Council, Italy° Articolazione Funzionale regionale di Aerobiologia ARPAT - Department of Pistoia, Italy
Ragweed (Ambrosia) is spreading in northern Italy, particularly in north-east; however, many pollens produced by ragweed have been also detected in Tuscany in the last four years although only few plants have been found in the region.
87
The aim of the study was to evaluate the origin of the ragweed pollens, analasying the meteorological conditions during the peak of pollens at a mesoscale level. Pollens have been collected using volumetric pollen particles samplers VPPS 2000 (Lanzoni) in the cities of Florence, Pistoia and Montecatini. Weather maps based on AVN model (Aviation Model) of the National Center of Environmental Prediction regarding the synoptical situation at 00 UTC and at 12 UTC of the 500 hPa geopotential and air temperature and wind direction at 850 hPa have been also evaluated.In the period under investigation (1999-2003) a strong association between the peaks of ragweed pollens and air masses originating from east-northeast has been observed.The highest peak occurred in the period 30th August- 4th September 2002 and was associated with air masses coming from Balkans, after persistent period characterized by low atmospheric circulation. In that occasion, the easterly air flow was due to a specific circulation pattern characterized by a low pressure located between the Ionic Italian coast and Greece. The peaks of ragweed pollens was always observed two days after the arrival of east-northeast air mass. The finding that pollen count decreased suddenly when air flow coming from Balkans stops, strengths our hypotesis. Furthermore, in the same period of 1999 and 2001, characterized by low atmospheric circulation, no ragweed pollens were detected in Tuscany.These data suggests that ragweed pollens collected in Tuscany might come from the east, probably from Balkans. In conclusion, this study highlights the importance of the collaboration between allergologist, meteorologists and aerobiologist, with the aim of forecast the pollination season even at a mesoscale level. *****
Allergic diseases –an increasing problem in Serbia andAllergic diseases –an increasing problem in Serbia and MontenegroMontenegro
L.Burazer¹,O.Vuckovic¹,M.Gavrovic² and T.Cirkovic²
¹Institute of Immunology and Virology-Torlak, Belgrade²Faculty of Chemistry, University of BelgradeSerbia and Montenegro
Epidemiology studies the relationship among factors influencing diseases in human populations. Changes in the burden of diseases over time are of particular interest and it is
88
concern that atopic diseases have been increasing , over the past few decades, both in Europe and world-wide. (1).The possibility for partial monitoring of the number of patients with allergy problems appears in 1998. , when Torlak Institute-Department of Allergology started with in vitro diagnostics using Pharmacia UNI – CAP –100 SYSTEM (Uppsala, Sweden). 5360 adult and pediatric patients were tested in the period between 1998 to 2002. The tests were performed on the subjects between ages from 5 to 60 years. All subjects had a previously positive prick test results. Skin prick tests were performed with a standard battery (histamine phosphate, PBS, grass pollen, tree pollen, weed pollen, home dust, Dermatophagoides pteronyssinus, bed line dust , animal hair ,mold, bacteriae, bee venom, wasp venom, hornet venom, cockroach) of glicerinated extracts (Torlak Institute, Belgrade).Histamine phosphate at 1 mg/ml and PBS were used, respectively , as positive and negative controls. Specific IgE and total IgE detection of patients’ sera were performed by means of Pharmacia UNI-CAP-100 System (Uppsala, Sweden).The results were expressed as CAP scores from class 0 to 6, according to the manufactures instruction.The dominant inhalatory allergen is Dermatophagoides pteronyssinus ,d1, making about 21% of the total analyses performed. The next significant group of inhalatory allergen are grass pollen ,gx1, (10%) , then there are weed pollen ,wx1, (8%), followed by tree pollen ,tx5, (3,6% )There is dominant allergen within each group of pollens. Within the grass pollen group, the dominant allergen is Dctylis glomerata ,g3, making about 33% of the total analyses performed. Ambrosia ellatior ,w1,is a dominant allergen in the weed allergen group making about 46% of the total analyses performed , while the most frequent allergen within the tree pollen group is the lime-tree, t208, about 12%. The number of tested patients refers primarily to the bigger cities of Serbia in which allergology service is developed and it also directs us that we must spread it onto the entire territory of Serbia and Montenegro.
*****
Prostaglandin EP Receptor Agonists Differentially ModulateProstaglandin EP Receptor Agonists Differentially Modulate Aspirin-induced Generation of 15-HETE in Aspirin-sensitiveAspirin-induced Generation of 15-HETE in Aspirin-sensitive Asthmatics.Asthmatics.
M. Jędrzejczak, A. Ptasinska, B. Bieńkiewicz, M. Borowiec, L. DuBuske*, M.L. Kowalski
Medical University of Lodz, Poland*Immunology Research Institute of New England, Fitchburg, MA, USA
89
Rationale. Aspirin triggers generation of 15-hydroxyeicosaterraenoic acid (15-HETE) in peripheral blood leukocytes from aspirin-sensitive (AS) but not aspirin-tolerant (AT) patients with asthma/rhinosinusitis. The aim of this study was to determine the effect of prostaglandin EP receptor agonists (misoprostol and sulprostone) on aspirin-induced 15-HETE generation. Methods. Peripheral blood leukocytes (PBLs) were isolated from AS and AT patients with asthma, and the 15-HETE release into the cell supernatant was measured with a specific immunoassay (Assay Design, MA). Results. Incubation of PBLs from AS asthmatics with 200μM of lysine-aspirin significantly increased generation of 15-HETE (mean increase +260%) but lysine-aspirin did not affect 15-HETE generation in PBLs from AT asthmatics. Preincubation of cells with misoprostol or sulprostone did not affect basal 15-HETE in AS or AT patients. However, both misoprostol and sulprostone inhibited in a dose-dependent manner the ASA-induced increase in 15-HETE generation in AS asthmatics (maximal inhibition being 89% and 80% after misoprostol and sulprostone respectively). In contrast in AT patients preincubation of PBLs with misoprostol or sulprostone resulted in a significant increase in generation of 15-HETE after addition of 200μM lysine-aspirin. The maximal increase of 15-HETE generation was observed with 10 μg/ml of misoprostol or sulprostone (+73% and +86% respectively). Conclusions. Our data suggest that aspirin-triggered 15-HETE release is differentially regulated by prostaglandin EP receptors in PBLs from AS and AT asthmatics.
*****
Allergic diseases –an increasing problem in Serbia andAllergic diseases –an increasing problem in Serbia and MontenegroMontenegro
L.Burazer¹,O.Vuckovic¹,M.Gavrovic² and T.Cirkovic²
¹Institute from Immunology and Virology-Torlak, Belgrade ²Faculty of Chemistry, University of Belgrade Serbia and Montenegro
90
Epidemiology is study the relationship of between factors influencing diseases in human populations. Changes in the burden of diseases over time are of particular interest and concern that atopic diseases have been increasing, both in Europe and world-wide, over the past few decades (1).
The possibility for partial monitoring of the number of patients with allergy problems appears in 1998, when Torlak Institute-Department of Allergology started with in vitro diagnostics use Pharmacia UNI – CAP –100 SYSTEM (Uppsala, Sweden). 5360 adult and pediatric patients were tested in the period between 1998 to 2002.
The test was performed on the subjects between ages 5 to 60 years. All subjects had a previously positive prick test results. Skin prick tests were performed with a standard battery (histamine phosphate, PBS, grass pollen, tree pollen, weed pollen, home dust, Dermatophagoides pteronyssinus, bed line dust, animal hair, mold, bacteriae, bee venom, wasp venom, hornet venom, cockroach) of glicerinated extracts (Torlak Institute, Belgrade).Histamine phosphate at 1 mg/ml and PBS were used, respectively, as positive and negative controls. Specific IgE and total IgE detection of patients sera were performed by means of Pharmacia UNI-CAP-100 System (Uppsala, Sweden).The results were expressed as CAP scores from class 0 to 6, according to the manufacturer’s instruction.
The dominant inhalatory allergen is Dermatophagoides pteronyssinus ,d1, making about 21% of the total analyses performed. The next significant group of inhalatory allergen are grass pollen ,gx1, (10%) , then there are weed pollen ,wx1, (8%), followed by tree pollen ,tx5, (3,6% )There is dominant allergen within each group of pollens. Within the grass pollen group, the dominant allergen is Dctylis glomerata ,g3, making about 33% of the total anayses performed. Ambrosia ellatior ,w1,is a dominant allergen in the weed allergen group making about 46% of the total analyses performed , while the most frequent allergen within the tee pllen group is the lime-tree,t208, about 12%.
The number of tested patients refers primarily to the bigger cities of Serbia in which allergology service is developed and it also directs us that must spread onto the entire territory of Serbia and Montenegro. *****
91
THE BECLOMETAZONE’S IMPACT ON IMMUNE AND CYTOKINTHE BECLOMETAZONE’S IMPACT ON IMMUNE AND CYTOKIN STATUS OF PATIENTS WITH ALLERGIC RHINITISSTATUS OF PATIENTS WITH ALLERGIC RHINITIS
Romanyuk L.I., Ohrimenko V.P., Oliinyk A.Y.*, Gryshilo A.P.
City Allergology Center, Kyiv, Ukraine
Aim: To study the changes of immune status at Allergic Rhinitis (AR) patients before/after treatment using beclometazone.Because the pathogenetic mechanisms of allergic inflammation are considered to be the co-operative interaction of the immune system cells, which ensure the cytokine secretion, as well as reception. Here we refer Interferon–γ, the Tumor Necrosis Factor α, IL-1α, IL-4. Thus, the complex indication of the blood serum cytokine of AR may serve a marker of inflammatory reaction level. Local corticosteroids effectively reduce the inflammatory phenomena.Methods and materials:73 AR patients (18-50 y.o., 35-m, 38–w)Depending on the applied therapy, patients were divided:I group: patients (40) have got mono therapy of local beclometazone. II group: patients (33) have got systemic corticosteroids as a traditional therapy.A control group included 20 practically healthy people, blood donors.Indication of subpopulations of T-lymphocytes (CD3+, CD4+, CD8+), B-lymphocytes (CD 20+), IgG, IgE, the immunoferment analysis (IFA) in a blood serum was applied with a help of “Protein profile” (St-Petersburg). The composition of the researched serum cytokines was studied with the application of the spectral and calorimetric method, using reagents set for IFA “Protein profile”.
The results and conclusion:The application of beclometazone in therapy of AR patients promotes the normalization of immunologic reactivity of human organism (the level of T-, B-lymphocytes, IgG and IgE), it improves of the cytokines level: IL1α, IL4 and TNF–α in a blood serum, as well as reduces the Interferon–γ concentration. Table 1-3.
Table 1The subpopulation T-lymphocytes composition of patients with Allergic Rhinitis in a treatment period (M±m)
The subpopulation composition of T-lymphocytes (%)
92
Group of examined persons
Number of persons
CD3+ CD4+ CD8+ CD4+\ CD8+
Control 20 60,3±1,2 35,4±1,3 25,1±1,5 1,50±0,04I gr. (Beclometazone) Before treatment 40 35,4±1,1* 25,8±0,7* 17,5±1,2 1,40±0,09 After treatment 40 63,1±1,3** 36,9±1,1** 24,2±0,4** 1,50±0,01*
*II gr.(basis- treatment) Before treatment
33 36,3±1,1* 25,9±0,8* 18,2±1,3* 1,39±0,07*
After treatment 33 48,2±1,1 29,5±0,9 20,1±0,9 1,35±0,01Note: * - the authenticity of distinctions in comparison with the indicators of control
group (р<0,05); ** - the authenticity with data before treatment (р<0,05)
Table 2.The state of В-lymphocites of immune system of patients with Allergic Rhinitis in a treatment period (M±m)
Group of examined persons
Number of persons
CD20+
(%)IgG(%)
IgE common(ке\л)
Control 20 15,9±3,2 11,4±0,9 26,3±1,5I gr. (Beclometazone) Before treatment 40 18,7±0,8 15,5±0,4* 59,3±2,3* After treatment 40 16,1±0,5** 11,9±0,2** 30,1±2,9*II gr.(basis- treatment) Before treatment 33 18,5±0,4 16,1±0,3* 64,8±2,7* After treatment 33 17,9±0,5 15,1±0,2** 49,4±2,5**Note: * - the authenticity of distinctions in comparison with the indicators of control group (р<0,05). ** - the authenticity with data before treatment (р<0,05).
Table 3.The indicators of production of some cytokines of patients with Allergic Rhinitis before and after treatment (M±m)
93
Indicators Healthy people, п=20 (control)
Patients with allergic rhinitis got beclometazone, п=40 (I group)
Patients with allergic rhinitis got common therapyп=33 (II group)
Before treatment
After treatment
Before treatment
After treatment
IL-1α80,4±10,1 733,4±101,5 450,1±50,1 731,2±100,4 690,1±16,7spontaneous
induced 1855,0±9 4725±670,0 3525,0±550,0
4720±650,0*
2010±10,5
In vivo 30,0±2,2 11,0±1,4* 21,1±5,7 11,2±1,2* 25,1±9,2IL-4, pg\ml 25,1±1,5 81,3±12,4* 25,7±0,9** 80,9±11,9* 75,1±15,1ФНО-α, pg\ml 25,0±4,0 560±11,7* 25,1±10,2** 561±11,9* 230,1±0,2*
INF-γ, pg\ml 127,8±14 64,6±6,3* 139,1±11,4 69,1±2,1* 81,1±1,1*
Note: *- the authenticity of difference of control group, р<0,05; ** - the authenticity of difference of group of patients after treatment, р<0,05
*****
AALLERGICLLERGIC S SENSITIZATIONENSITIZATION TOTO M MOLDSOLDS
Susana Andrade1, Celso Pereira1, Ana Todo Bom1, Fernando Rodrigues2, Rosário Cunha2, Celso Chieira1 1Immunoallergology Department; 2 Immunology Laboratory. Coimbra University Hospital
INTRODUCTION: A causative relationship between allergic sensitization and allergic symptoms is widely documented for allergens from house dust mites, animal dander and pollens. There is increasing evidence of the implication of molds, such as Alternaria, Cladosporium and Aspergillus, in allergic respiratory manifestations. Polysensitization, inadequate allergenic extract purification and standardization, allied to high prevalence of cross-reactivity among different species, have limited the clinical characterization of fungal allergy. Previous epidemiologic studies revealed a considerable variability concerning the percentages of mold sensitization. OBJECTIVE: The purpose of this study was to identify the mold species most frequently implicated in allergic sensitization in a group of patients with cutaneous hypersensitivity to these allergens. Moreover, we aimed to assess the allergic respiratory symptoms reported and to evaluate the
94
correlation between in vivo and in vitro diagnosis, respectively skin prick test and detection of allergen-specific serum IgE antibodies. MATERIAL AND METHODS: We selected a hundred consecutive patients admitted to our department presenting allergic respiratory symptoms and with documented sensitization to at least one mold specie, assessed by skin prick test using commercial extracts (Alk-Abelló – Madrid, Spain), that included: Alternaria alternata, Aspergillus fumigatus, Aspergillus niger, Cladosporium herbarum, Curvularia spicifera, Fusarium moniliforme, Penicilium notatum, Penicillium roqueforti, Rhizopus nigricans and Candida albicans. Fourty patients sensitized to one of the first four species collected blood samples for specific IgE assay by Pharmacia UniCAP®
System.RESULTS: The species more frequently involved in mold sensitization were: Aspergillus fumigatus (37%), Cladosporium herbarum (34%), Alternaria alternata (34%) and Aspergillus niger (31%). Low rates of skin test reactivity were reported. Mean weal diameters between 3 and 5 mm above negative control were shown in 70 to 90% of the patients. Alternaria revealed higher allergenicity. 32% of the patients were monosensitized to a single specie. Polysensitization to other inhalant allergens was demonstrated in almost 90% of the patients, particularly dust mites. There were only four positive serum IgE findings (>0,35 KU/L) to Aspergillus fumigatus, two of them occurring in patients with negative skin test. Three patients had positive IgE antibodies to Cladosporium (two with negative skin prick test). The two patients showing serum IgE to Alternaria had cutaneous reactivity to this mold. It was not found serum specific IgE to Aspergillus niger. Prevalence of allergic rhinitis ranked first in clinical findings in the second group of patients (83,8%), followed by sinusitis (62,2%) and asthma (54,1%).DISCUSSION AND CONCLUSIONS: This study confirmed previous observations that Aspergillus, Cladosporium, Alternaria represent the most common fungal allergens, diagnosed both through in vivo or in vitro assays for IgE determination, and support an important lack of correspondence between skin test and serum allergen-specific IgE. The important role of moulds in severity of allergic diseases reinforces the need of standardized, stable and well-characterized allergen extracts to be used in more effective and reliable in vivo and in vitro diagnosis. It also strengthens the need to complement both methods in order to properly identify fungal diseases. Moreover, a clear correlation of fungal sensitization and respiratory symptoms could not be established.
*****
ALLERGIC CONTACT DERMATITIS TO MANGO – A CASEALLERGIC CONTACT DERMATITIS TO MANGO – A CASE REPORTREPORT
95
Susana Oliveira1, Anabela F. Faria2, Rita Câmara1, Fernando Drummond Borges1, L. M. Camacho de Freitas2.1Immunoallergy Unit, 2Dermatology Department – Funchal Hospital.
Background: Allergic Contact Dermatitis (ACD) is an inflammatory reaction that follows absorption of antigen applied to the skin surface and recruitment of previously sensitised, antigen specific T lymphocytes into the skin. ACD affects 20% of children at some time during childhood. Diagnosis is based upon the distribution of eczematous lesions rather than the appearance of individual lesions. There are many instances where the allergens are not found by history and epicutaneous testing is required. Treatment requires moderately potent topical steroid ointments. Allergen avoidance is the mainstay of prevention.Case report: An 11-year-old girl went to the Dermatology Department for evaluation of an edematous and vesiculous reaction on her face and left wrist, probably after contact with mango tree (Mangifera indica). These lesions appeared one or two days after the patient’s stayed on a mango tree tilled ground where she also had a hand contact with the relating fruit (with peel), without ingestion. Apparently without any other associated symptoms. The patient denied contact with new topical products. The personal history revealed mild intermittent allergic rhinitis. The patient referred a small portion of mango ingestion, some months before the presented episode, without clinical manifestations. Other personal facts seemed irrelevant. The family history revealed that the father and one uncle had asthma. The following study was performed: IgA, IgM, IgG, Total IgE and specific IgE determinations (Dermatophagoides pteronyssinus, Dermatophagoides farinae, Parietaria, Grasses mixture, Mugwort, Birch, Candida albicans, Aspergillus fumigatus, Mango, Latex (CAP system)), tool parasitologic test, skin prick tests (SPT) using commercial extracts and fresh mango and epicutaneous testing, performed according to the Portuguese Contact Dermatitis Research Group (GPEDC) - standard series and fresh mango. All tests, but epicutaneous testing, were normal or negative (SPT); epicutaneous testing were strongly positive to mango flesh, mango-tree leaf and mango-tree stem. Concerning to the SPT it outstands that about 72 hours after SPT execution papulo-vesiculous reaction appeared on the face (flare-up) and on the forearm (where the SPT were performed with the flesh and the peel of the mango – prick-prick). Treatment was performed with topical steroid and oral anti-histaminic with a rapid symptoms resolution.Conclusion: The ACD to mango corresponds to a rare situation. Most frequently, the case reports are characterized by papulo-vesiculous reaction localized on the lips or peri-bucal region, which occur, normally, after fruit direct contact with bucal mucous membrane or after ingestion. The described case is rare, not only in it’s clinical presentation but also with concern to the allergenic contact route, which we supposed to be airborne transportation.
*****
96
INDOOR CHARACTERIZATION - AEROALLERGENSINDOOR CHARACTERIZATION - AEROALLERGENS SENSITIZATIONSENSITIZATION
Susana Oliveira1, Rita Câmara1, Maria João Castro1, Mariana Rodrigues2 Fernanda Vila3, Cátia Cardoso3; Ana Carvalho Marques3; Fernando Drummond Borges1.1Unidade de Imunoalergologia, 2Serviço de Estatística e Apoio à Investigação, 3Serviço de Pediatria – Hospital Central do Funchal.
Background: Indoor home conditions of allergic patients associated with an increased sedentary life style, could be a trigger for allergic illness. Purpose: Indoor characterization from Immunoallergy outpatients and correlation with their atopy incidence. Methods: Questionnaire systematic application in order to characterize indoors conditions of Immunoallergy outpatients. Skin Prick Test (SPT) with commercial extracts (dust mites, mould and cockroach). Statistic analysis and correlation between indoor conditions and sensitization was done. Results: Patients population: n=193. Male – 47,7% and female – 52,3%. Mean age = 15 years old (8 months – 80 years). Home place: urban, suburban and rural, equitable distribution. Basic sanitation inexistent in 10% (n=20) of the population. House floor was predominantly: wood (44%) and mosaic (40,4%). Only 4,1% (n=8) of the individuals have carpet. The majority of the houses has 2 or 3 sleeping rooms and almost of the population shares the room with one more person. In average the mattress has 5 years, it is predominantly springs (90,2%) and is not shared in 81,1% of cases. Pillow is used by 89,6% of patients, whose average age is 3 years, and being scum in 51,8% of cases. The eider-down is used by 61,7% of the population. In almost half of patient room there are soft toys (n=90) in number >5 (47,8 % ). Indoor humidity is present in 57,9% and cockroach in 48,2 % of houses. In studied population 75% have SPT positive to at least one tested allergen. Positive sensitization was: house dust mite 77,2% cockroach 26,2% and mould 23,4%. For allergens like house dust mite the only significant Pearson correlation founded was for more than 5 soft toys (<0,001). There were not found other significant correlation to this allergen or between indoor humidity and mould sensibilization. Pearson correlation was significant (<0,001) for home occurrence cockroach and positive SPT to this aeroallergen. Conclusion: Incidence for sensitization to the tested aeroallergens was similar to that found in PAC-study. The reason for no significant Pearson correlation between other indoor conditions beside soft toys >5 and house dust mite sensitization could be explained by some previous
97
environment control already done. The inexistence of significant correlation between indoor humidity and moulds atopy could be explained by the lacking of moulds standardized extracts for prick test. The correlation found for indoor cockroach and sensitization for this specific allergen could be justified, in one hand by high prevalence of indoor cockroach and in another hand by extermination difficulties. *****
SomeSome activation marcers activation marcers and factors of intercellularand factors of intercellular cooperation cooperation (Fas-receptor,(Fas-receptor, ICAM-1 ICAM-1 and cytokinesand cytokines)) in in patients with patients with CChronic hronic UUrogenital Chlamydiosisrogenital Chlamydiosis
V . V . Driyanskaya , G. N.Drannik, V.S.PapakinaInstitute of Urology; Institute of Nephrology AMS of Ukraine; Kiev, Ukraine.
The molecular activity of apoptosis (A) under study is one of the most intensively developing areas in biology and medicine. It has been shown that many pathogens, intracellular ones (Chlamydia relate to them) in particular, are able to modulate A that allows than to withstand the defensive factors of a macroorganism. It is known that A can depend on cytokine level and ICAM.
The aim of this work is to investigate the level of mononuclear cells expressing Fas-receptor (CD95+) (pro-apoptotic factor) and also adhesive molecules ICAM-1 (CD54+) in patients with chronic inflammatory diseases of urinary system (CIDUS) of chlamydial (group1 - 15 patients) and other (gr. 2 –15 patients) etiology in comparison with healthy donors (group 3 – 10 donors). The laboratory recognition of contagions was performed by means of cytoscopy, PLR, IFA. The antigen expression was studied using the immunofluorescence method with mAb; spontaneous and induced synthesis of interleukins-1,-2,-10, γ-IFN and TNF-α was defined by ELISE-method on STAT FAX-303 PLUS test-system of “IMMUNOTECH” (France) and “PROTEIN CONTUR” (St-Petersburg, Russia); spectrophotometry was used to determine the NO-level.
The investigation demonstrated the objective elevation in marking level of blood lymphocyte activation in patients of both groups with CIDUS; at the same time, the number of CD95+ (37±3,1%) and CD54+ (35±2,5%) cells in gr.1 objectively exceeded these reading both in healthies (15±1,6% и 19±2,6% respectively) (p<0,001) and in patients of gr. 2 (28±1,8% и 27±2,0% respectively) (р<0,05). The high level of proapoptotic marker CD95+ in patients with chlamydial infection can be partly explained by the increased NO-production, in spite of the decreased production of pro-inflammatory cytokines (IL-2, γ-IFN) that we had previously
98
detected, the reduction in IL-10 and absence of deviation from normal production of TNF-α.. It cannot be excluded that the increased expression of adhesive molecules in patients with CIDUS, which testify to the activation of cells, can exert antiapoptotic action (in spite of the high level of readiness to A) described by some authors. *****
ALLERGIC RHINITIS AND OXIDANT/ANTI-OXIDANT BALANCE ALLERGIC RHINITIS AND OXIDANT/ANTI-OXIDANT BALANCE
(1) Vlaski E, (1) Stavric K, (2) Isjanovska R, (1) Seckova L, (3) Kacarski D
(1) University Children’s Hospital, Skopje, R. Macedonia (2) Institute of epidemiology and biostatistics with medical informatics, Skopje, R. Macedonia (3) PHO Zeleznicar, Skopje, R. Macedonia
Objective: As the role of respiratory oxidant/anti-oxidant balance in allergic rhinitis is suggested, the aim of the study was to examine the impact of air pollution and acetaminophen consumption as factors which may increase oxidative stress and fruit, vegetables intake as factors which may increase anti-oxidants on current allergic rhinitis and ever-diagnosed hay fever in children.
Material and methods: The self-reported data of 3026 children 13/14 years old from Skopje obtained from ISAAC phase 3 questionnaires in 2002 were analysed. The relationship between sneezing or a runny or blocked nose apart from a cold in the last 12 months (AR12), ever-diagnosed hay fever and factors which affect oxidant/anti-oxidant balance (exposure to passive smoking at home, gas cooking at home, frequency of trucks passage through residential street, frequency of acetaminophen use in the last 12 months, frequency of fruit and vegetables intake in the last 12 months) was determined. Chi-square and odds ratios in logistic regression for statistic analysis of the data were used.
Results: It was established that current acetaminophen use at least once monthly and at least once yearly, compared to never use of acetaminophen, significantly increased the risk of AR12 (at least once monthly: OR=2.43 95%CI 1.75-3.37 p<0.001; at least once yearly: OR=1.45 1.21-1.75 p<0.001). Related to ever-diagnosed hay fever, only current acetaminophen use at least once monthly was associated with increased risk of this disease (OR=2.32 1.41-3.81 p=0.001). A significant association between allergic rhinitis or ever-diagnosed hay fever and other investigated parameters was not found.
99
Conclusion: Our results confirm only the suggestion that acetaminophen use is positively associated with allergic rhinitis in children.
**********
INDOOR CHARACTERIZATION - AEROALLERGENSINDOOR CHARACTERIZATION - AEROALLERGENS SENSITIZATIONSENSITIZATION
Susana Oliveira1, Rita Câmara1, Maria João Castro1, Mariana Rodrigues2 Fernanda Vila3, Cátia Cardoso3; Ana Carvalho Marques3; Fernando Drummond Borges1.1Unidade de Imunoalergologia, 2Serviço de Estatística e Apoio à Investigação, 3Serviço de Pediatria – Hospital Central do Funchal.
Background: Indoor home conditions of allergic patients associated with an increased sedentary life style, could be a trigger for allergic illness. Purpose: Indoor characterization from Immunoallergy outpatients and correlation with their atopy incidence. Methods: Questionnaire systematic application in order to characterize indoors conditions of Immunoallergy outpatients. Skin Prick Test (SPT) with commercial extracts (dust mites, moulds and cockroach). Statistic analysis and correlation between indoor conditions and sensitization was done. Results: Patients population: n=193. Male – 47,7% and female – 52,3%. Mean age = 15 years old (8 months – 80 years). Home place: urban, suburban and rural, equitable distribution. Basic sanitation inexistent in 10% (n=20) of the population. House floor was predominantly: wood (44%) and mosaic (40,4%). Only 4,1% (n=8) of the individuals bedroom have carpet. The majority of the houses has 2 or 3 sleeping rooms and almost of the population shares the room with one more person. In average the mattress has 5 years, it is predominantly springs (90,2%) and is not shared in 81,1% of cases. Pillow is used by 89,6% of patients, whose average age is 3 years, and being scum in 51,8% of cases. The eider down is used by 61,7% of the population. In almost half of patient room there are soft toys (n=90) in number >=5 (47,8 %). Indoor humidity is present in 57,9% and cockroach in 48,2 % of houses. In studied population 75% have SPT positive to at least one tested allergen. Positive sensitization was: house dust mite 77,2% cockroach 26,2% and mould 23,4%. For allergens like house dust mite the only significant Pearson correlation founded was for >=5 soft toys (<0,001) indoor. There were not
100
found other significant correlation to this allergen or between indoor humidity and mould sensibilization. Pearson correlation was significant (<0,001) for home occurrence cockroach and positive SPT to this aeroallergen. Conclusion: Incidence for sensitization to the tested aeroallergens was similar to that found in PAC-study. The reason for no significant Pearson correlation between other indoor conditions beside soft toys >5 and house dust mite sensitization could be explained by some previous environment control already done. Finally, the inexistence of significant correlation between indoor humidity and moulds atopy could be explained by the lacking of moulds standardized extracts for prick test and regional variation. The correlation found for indoor cockroach and sensitization for this specific allergen could be justified, in one hand by high prevalence of indoor cockroach and in another hand, by extermination difficulties. *****
ALLERGENIC POLLEN AND URBAN AIR POLLUTIONALLERGENIC POLLEN AND URBAN AIR POLLUTION IN IN THE MEDITERRANEAN AREA THE MEDITERRANEAN AREA
D’Amato Gennaro
Division of Pneumology and AllergologyHigh Speciality Hospital A. Cardarelli Napoli ItalyAddress: Rione Sirignano,1080121 Napoli Italyfax+39.081.7473331e.mail: [email protected]
Key words: Allergenic pollen; Outdoor air-pollution; Pollinosis; Respiratory allergy; Seasonal allergy.
Address for correspondence:Prof. Gennaro D’Amato Director, Division of Pneumology and AllergologyHospital A.CardarelliVia Rione Sirignano,1080121 Napoli, Italy
101
Fax +39 081 7473331e.mail: [email protected]
Pollen allergy has a remarkable clinical impact all over Europe and there is a body of evidence suggesting that the prevalence of respiratory allergic reactions induced by pollens in Europe is on the increase, a trend that is clearly evident also in the Mediterranean area ( 1-7 ) . Since airborne-induced respiratory allergy do not recognises national frontiers, and like most diseases that can be prevented by avoiding exposure to the causative agent, the study of pollinosis cannot be limited to national boundaries. In Europe, the main pollination period covers about half the year, from spring to autumn, and the distribution of airborne pollen taxa of allergological interest is related to five vegetational areas (Table I). Because of its climatic conditions, characterized by mild winters and sunny days with dry summers, the vegetation of the Mediterranean area is different from that of central and northern Europe. Allergenic-pollen-producing plants typical of the Mediterranean climate are Parietaria, Olive and Cupressaceae. However, during the last thirthy years or so, aerobiological and allergological studies have been developed rapidly in most parts of Europe and also in Mediterranean area. This has led to an increased density of observational networks of pollen-counting stations, and also to the need for multilateral exchange and cooperation in aerobiological and allergological studies.The allergenic content of the atmosphere varies according to climate, geography and vegetation. Data on the presence and prevalence of allergenic airborne pollens, obtained from both aerobiological studies and allergological investigations, make it possible to design pollen calendars with the approximate flowering period of the plants in the sampling area. In this way, even though pollen production and dispersal from year to year depends on the patterns in preseason weather and on the conditions prevailing at the time of anthesis, it is usually possible to forecast the chances of encountering high atmospheric allergenic pollen concentrations in different areas.Aerobiological and allergological studies show that the pollen map of Europe and of Mediterranean area is changing also as a result of cultural factors (for example importation of plants such as birch and cypress for urban parklands) and greater international travel (e.g. the colonization by ragweed in France, northern Italy, Austria, Hungary etc.).By virtue of aerobiological sampling of the pollen content of the atmosphere of various Mediterranean cities, have been identified three pollen seasons (3,6,7):
102
- a low winter pollen season (from December to the end of March) marked by the presence of the pollens of such trees as Cupressaceae (Cupressus and Juniperus), Corilaceae (Hazel), Acaciae (Mimosa) and some Betulaceae.- A high spring-summer pollen season (from April to July), of marked allergological interest,
dominated by the pollination of Grasses, Parietaria and Olea (Olive). Slightly overlapping this season, from March to May, Platanus flowers, and has some allergenic importance in some Mediterranean areas as Southern France, Spain etc.
- A summer-autumn season (from August to October) marked by the second, less pronounced, peak of Parietaria and sometimes of Gramineae and the pollens of herbaceous plants, such as mugwort (Artemisia) and Chenopodiaceae.
Grass pollen is by far the most important cause of pollinosis throughout the European continent and also in the Mediterranean area. It is interesting to note that in various European cities, whilst the prevalence of allergic rhinitis and allergic asthma is increasing, the atmospheric concentration of grass pollen is decreasing (3,8). The decrease in grass pollen concentrations has been attributed to substantial decreases in the area of grassland over large areas of the continent. In fact, the last 25 years have seen a reduction in grassland of about 40% (8). However, the observation that cases of allergic rhinitis and asthma induced by grass pollen are increasing is probably related to various factors, including increased air pollution (8-10). Parietaria is a genus of the Urticaceae family, and P. officinalis and judaica are the most common allergenic species of this genus. P. judaica grows in coastal Mediterranean areas such as Spain, southern France, Italy, Yugoslavia, Albania, Greece .This allergenic plant, which is responsible for many cases of severe pollinosis, has two very long flowering periods. Its pollen appears first at the beginning of the spring and persists during the spring and summer months, often reaching a peak level with daily mean values of more than 5 hundred pollen grains per cubic meter of air at the end of April or in May, depending on the climate of the area. A shorter pollination period is observed from the end of August to October.In the Oleaceae family, the most allergenic pollen is produced by Olea europaea, the olive tree, which in the Mediterranean area has been recognized as being one of the most important causes of seasonal respiratory allergy (11). The olive pollination season lasts from April to the end of June and sometimes causes severe symptoms (oculorhinitis and/or bronchial asthma). Olive tree, like Birch, has reproductive rhythms of high and low years for the abundance of pollen and subsequent seed. The alternating patterns may be modified or even obscured by the influences of weather during the times of pollen formation and dispersal.Frequently the sensitization to pollen allergens of Olea is associated with other atopic sensitizations such as allergy to grasses and it is frequently difficult to know whether sensitization to grasses prevails or whether it is Olive that prevails.Another interesting aspect of olive allergy is that in subjects with sensitization to the allergens of this pollen the clinical symptoms are frequently not limited to the pollination season (May-June) but are present all year round without an explanation.As for Birch, which is the most potent of the pollen-allergen-producing trees in northern Europe, this arboreal plant is spreading down into the Mediterranean area. For example Birches are
103
becoming increasingly abundant in northern Italy where landscape artists tend to use them in new urban parks. The typical peaks of birch pollens are recorded in northern Europe during May, whereas in sourthern Europe the birch pollen concentration generally peaks in April. This tendency for spring-pollinating plants, like birch and grass, to flower earlier in the warmer southern regions of Europe is reversed for the Autumn-pollinating types such as mugwort ( 3).Cypress pollination is characterized by a wide variability with very high concentrations in Mediterranean coastal areas, where it frequently induces rhinoconjunctivitis. This pollen taxa is the most common airborne allergen of the winter months in some Mediterranean cities.The increasing epidemiologic impact of pollinosis induced by Cupressaceae plants is related to the increasing use of these species for gardening and reforestation (12). So again, like with birch, we have a case of fashion influencing the epidemiology of pollen-induced disorders.Pollen grains from herbs like mugwort (Artemisia) and Plantain (Plantago) are of limited but, nevertheless, real clinical importance. Mugwort in particular has a marked sensitizing capacity. In the same Compositae family of Mugwort, we find also ragweed (Ambrosia), which is colonizing Europe, and not only Central Europe, but also some parts of the Mediterranean area such as northern Italy. Interaction between urban air pollution and pollen allergyStudies have demonstrated that urbanization and high levels of vehicle emissions and westernised lifestyle is correlated with the increasing frequency of pollen-induced respiratory allergy and people who live in urban areas tend to be more affected by pollen-induced respiratory allergy than those of rural areas (13). In urban cities of the Mediterranean area among the components of air pollution there are frequently high concentrations of ozone favoured by sunny days and ultraviolet radiations. In particular, ozone trends depend not only on substrate supply (emissions of nitrogen dioxide by cars), but also on weather conditions and sunny days facilitate the transformation of nitrogen dioxide into ozone, thereby producing the so called “Los Angeles smog”.There is a growing body of evidence that components of air pollution interact with inhalant allergens carried by pollen grains and may enhance the risk of both atopic sensitization and exacerbation of symptoms in sensitized subjects (14,15), since urban air pollution affects both airborne allergenic pollen and the airways of exposed subjects. Pollen allergy has been one of the most frequent models used to study the interrelationship between air pollution and respiratory allergic diseases. Pollen grains or plant-derived paucimicronic components carry allergens that can produce allergic symptoms (15,16). They may also interact with air pollution (particulate matter, ozone ) in producing these effects. (Table II). Furthermore airway mucosal damage and impaired mucociliary clearance induced by air pollution may facilitate the access of inhaled allergens to the cells of the immune system (14-16) (Table III). In addition, vegetation reacts with air pollution and environmental conditions and influence the plant allergenicity. Several factors influence this interaction, including type of air pollutants, plant species, nutrient balance , climatic factors, degree of airway sensitization and hyperresponsiveness of exposed subjects. The city of Naples serves as a good model with which to study the interaction between pollen-derived allergen and air pollution.It has
104
about 2 million inhabitants and very dense traffic. It is located in a coastal area enclosed on three sides by hills and mountains. The year-long sunny days favour high levels of ozone. This situation, on days with absence of wind and rain, favours critical episodes of air pollution.The climate also favours the pollination of Parietaria, which grows in abundance throughout the city ( 2,6 ). About 30% of inhabitants are allergic to this plant and more than 50% of these Parietaria pollen-allergic subjects experience bronchial asthma and its equivalent, with high level of bronchial hyperresponsiveness ( 2,6,15 ).
During Spring the prevalence of Parietaria-induced allergic respiratory disorders tends to increase and there is a peak in the number of emergency room visits for allergic asthma attacks when there is an increase in airborne concentrations of Parietaria pollen grains and a parallel increase of ozone levels from April to June. This parallel increase usually starts in February and peaks between May and June when Parietaria pollen grains reach levels of about 1000 grains/m3 of air. After July the production and release of Parietaria pollen usually decreases, while ozone levels remain high also in autumn during which the concentration of Parietaria pollens is low. There is also a diurnal correlation of both peaks, since Parietaria pollen and ozone reach their highest levels in morning. Parietaria peaks earlier than ozone because of the time required for the photochemical reaction to develop.
.So, the conditions of Naples favour the interaction between Parietaria pollen, ozone and inhalable PM and on sunny days in the atmosphere of Naples there is a parallel increase of ozone , PM10 and of Parietaria pollen grains. This parallel increase usually starts in January or February and the increasing trend reaches June or July. At this time the production and release of Parietaria pollen usually decreases, while ozone and PM10 are high also in Autumn and frequently also during Winter.
____________________________________________________________Table I - Vegetational areas and prevalent distribution of allergenic plants in Europe:- Arctic: birch- Central: deciduous forest, birch, grasses- Eastern: grasses, mugwort, ragweed- Mountains: grasses (with a pollination season delayed by three-four weeks in comparison
with areas at sea level). - Mediterranean: Parietaria, olive trees, grasses and also cypress.________________________________________________________________
TABLE II The rationale for the interrelationship between agents of air pollution and pollen allergens in inducing respiratory allergy: 1 – Air pollution can interact with pollen grains, leading to an increased release of antigens characterized by modified allergenicity.
105
2 – Air pollution can interact with allergen-carrying paucimicronic particles derived from plants. The paucimicronic particles, pollen-originated or not, are able to reach peripheral airways with inhaled air, so inducing asthma in sensitized subjects. 3 – Air pollution, and in particular ozone, particulate matter and sulphur dioxide, have been shown to have an inflammatory effect on the airways of exposed, susceptible subjects, causing increased permeability, easier penetration of pollen allergens in the mucous membranes and easier interaction with cells of the immune system. There is also evidence that predisposed subjects have increased airway reactivity induced by air pollution and increased bronchial responsiveness to inhaled pollen allergens. 4, Some components of air pollution seem to have an adjuvant immunologic effect on IgE synthesis in atopic subjects. In particular diesel exhaust particles (17,18), which can interact in atmosphere with pollens or paucimicronic particles (16)._______________________________________________________________________Table III Possible mechanisms of pollutant enhancement of responses to pollen allergens:- increased epitelial permeability- pollutant induced airway inflammation “priming” the subsequent allergen-induced
responses- enhanced oxidative stress in the airways.
References
1)
2) D’Amato G, Lobefalo G. Allergenic pollens in the Mediterranean area. J Allergy Clin Immunol 1989;83:116-122.
3) D’Amato G, Dal Bo S, Bonini S. Pollen-related allergy in Italy. Ann Allergy 1992;68:433-437.
4) D’Amato G.,Spieksma F.Th.M.,Liccardi G. et al . Pollen-related allergy in Europe.Position Paper of the European Academy of Allergology and Clinical Immunology. .Allergy 1998;53:567-78.
5) European Community Respiratory Health Survey. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks and the use of asthma medications in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 1996;9:687-695.
6) The International Study of Asthma and Allergy in Childhood (ISAAC). Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis and atopic eczema. Lancet 1998;351:1225-32.
7) D’Amato G.,Spieksma F.Th.M.Bonini S. Allergenic pollen and pollinosis in Europe. Blackwell Science,Oxford,UK,1991
8) D’Amato G.,Bonini S,Bousquet J,Durham SR,Platts-Mills TAE . Pollenosis 2000-Global Approach. JGJ Editions,Naples,Italy,200
9) Emberlin J, Savage M,Jones S. Annual variations in grass pollen seasons in London 1961-1990, trends and forecast models. Clin Exp Allergy 1993;23:911-918.
106
10) D’Amato G. Urban air pollution and plant-derived respiratory allergy. Clin Exp Allergy 2000;30:628-36.
11)D’Amato G.,Holgate ST. The impact of air pollution on respiratory health. European Respiratory Monograph n.21 .Sheffield, UK,2002
12) Liccardi G, D’Amato M,D’Amato G. Oleaceae pollinosis: a review. Int Arch Allergy Immunol 1996;111:210-217
13)Mari A, Di Felice G,Afferni C et al. Assessment of skin prick test and serum specific IgE detection in the diagnosis of Cupressaceae pollinosis. J Allergy Clin Immunol 1996;98:21-31.
14) Ishizaki T., Koizumi K., Ikemori R.,Ishiyama Y.,Kushibiki E. Studies of prevalence of japanese cedar pollinosis among residents in a densely cultivated area. Ann Allergy 1987;58:265-270.
15)Devalia JL,Rusznak C, Davies RJ. Allergen/irritant interaction-its role in sensitization and allergic disease. Allergy 1998;53:335-345.
16) D’Amato G, Liccardi G, D’Amato M,Cazzola M. The role of outdoor air pollution and climatic changes on the rising trends in respiratory allergy. Respir Med. 2001;95:606-611.
17)Knox RB, Suphioglu C, Taylor P et al. Major grass pollen allergen Lol p1 binds to diesel exhaust particles: implications of asthma and air pollution. Clin Exp Allergy 1997;27:246-251
18) Diaz-Sanchez D,Tsien A, Fleming J, Saxon A. Combined diesel exhaust particulate and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T helper cell 2-type pattern. J Immunol 1997;158:2406-2413
19) Salvi SS,Frew A, Holgate S. Is diesel exhaust a cause for increasing allergies? Clin Exp Allergy 1999;29:4-8
********
EAACI would like to specialy thank the Portuguese Society of Allergy and Clinical Immunology for the provision of the material from the course.
107