Pigmented Bowen's Disease (Squamous Cell Carcinoma in situ): A Mimic of Malignant Melanoma
-
Upload
ravi-krishnan -
Category
Documents
-
view
213 -
download
1
Transcript of Pigmented Bowen's Disease (Squamous Cell Carcinoma in situ): A Mimic of Malignant Melanoma
© 2001 by the American Society for Dermatologic Surgery, Inc. • Published by Blackwell Science, Inc.ISSN: 1076-0512/01/$15.00/0 • Dermatol Surg 2001;27:673–674
CASE REPORT
Pigmented Bowen’s Disease (Squamous Cell Carcinoma in situ): A Mimic of Malignant Melanoma
Ravi Krishnan, MD, Alan Lewis, MD, Ida F. Orengo, MD, and Ted Rosen, MD
Baylor College of Medicine, Houston, Texas
background.
Darkly pigmented individuals may manifest un-usual or uncharacteristic presentations of various skin condi-tions, including heavy pigmentation of cutaneous tumors.
objective.
To increase the awareness of an unusual presenta-tion of Bowen’s disease in a darkly pigmented individual.
methods.
We report the case of a 52 year old black womanthat presented with a lesion clinically consistent with malignant
melanoma. However, histopathologic examination revealedpigmented Bowen’s disease.
results.
A biopsy is almost always indicated to confirm the di-agnosis of lesions in darkly pigmented individuals.
conclusion.
This case is presented to reinforce the idea thatpigmented Bowen’s disease should be considered in the differ-ential diagnosis of malignant melanoma.
Case Report
A 52-year-old black woman presented with a 1-yearhistory of gradually enlarging dark brown plaques onher perianal skin. The lesions were slightly painful andmoderately pruritic. The patient had no family or per-sonal history of cutaneous malignancy. Her past medi-cal history was remarkable for an unspecified uterinetumor for which she underwent a hysterectomy 20years ago. She denied a history of genital warts or anyother lesions. Otherwise the patient was in good health.
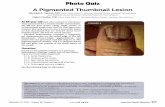
On physical examination, two dark brown plaques (7cm
�
6 cm and 1 cm
�
2 cm) with erosions were notedon the left buttock, near the anus (Figure 1). No othergenital lesions were seen. No genital warts were noted.
The skin biopsy specimen demonstrated acanthosis,hyperkeratosis, and marked atypia of keratinocytes inthe epidermis. Atypical mitoses were also observed.There was no evidence of dermal invasion. Some kera-tinocytes had swollen nuclei and contained coarsekeratohyaline granules. The papillary dermis con-tained a dense infiltrate of lymphocytes and numerousscattered melanophages. The plaques were removedby Mohs micrographic surgery and there was no evi-dence of recurrence at 18-months follow-up.
Discussion
Pigmented Bowen’s disease is an unusual form of squa-mous cell carcinoma in situ that is characterized by a
hyperpigmented appearance. This disorder is exceed-ingly uncommon and represents less than 2% of casesof Bowen’s disease.
1
To our knowledge, there havebeen only two other reported cases of pigmented Bo-wen’s disease involving the anogenital region.
2,3
De-spite the relative infrequency of pigmented Bowen’sdisease, an awareness of this disorder is important be-cause of its ability to closely resemble malignant mela-noma.
Pigmented Bowen’s disease commonly presents as ahyperpigmented, sharply marginated plaque with asurface that may be velvety, verrucous, or flat.
1–8
Scal-ing and erosions may be present as well.
1
The lesionsare generally asymptomatic, however, they may causepruritus or burning pain.
2
Pigmented Bowen’s diseasealmost exclusively affects intertriginous areas.
4
Since Bowen’s disease is much more common inCaucasians than in blacks,
5
many of the generaliza-tions regarding the presentation of Bowen’s diseaseare derived from the manner in which this disordermanifests itself in Caucasian patients. However, someof these generalizations do not accurately describeblack patients. For example, in Caucasian patients,Bowen’s disease ordinarily develops on sun-exposedareas and is rarely pigmented.
2
In contrast, in the rela-tively few cases of black patients with Bowen’s dis-ease, it has been noted that sun-protected areas aremore frequently affected and that the pigmented vari-ant is not uncommon.
5
This correlates with our pa-tient’s presentation.
The differential diagnosis of pigmented Bowen’sdisease includes superficial spreading melanoma, pig-mented basal cell carcinoma, melanocytic nevus, seb-orrheic keratosis, and bowenoid papulosis.
1,3,6
Thesedisorders can be diffrentiated on the basis of clinicalfeatures and histopathology.
R. Krishnan, MD, A. Lewis, MD, I.F. Orengo, MD, and T. Rosen,MD have indicated no significant interest with commercial supporters.Address correspondence and reprint requests to: Ida Orengo, MD, De-partment of Dermatology, Baylor College of Medicine, One BaylorPlaza, Houston, TX 77025.
674
krishnan et al.: pigmented bowen’s disease
Dermatol Surg 27:7:July 2001
Histologically, pigmented Bowen’s disease typicallydemonstrates full-thickness epidermal dysplasia char-acterized by irregular keratinocyte maturation, abnor-mal keratinization, and disorganized architecture.
1–8
Hyperkeratosis, parakeratosis, and acanthosis may bepresent. Nuclear atypia and mitoses are also com-monly seen. The dermis shows no evidence of invasionand often contains a dense infiltrate of lymphocytes orhistiocytes.
5
In addition to these features, which arecommon to all Bowen’s disease, the pigmented formof Bowen’s disease shows an abundance of melanin-rich cells. Significant quantities of melanin may befound within the epidermal cells of the basal layer,
2,7
within highly dendritic, nonneoplastic melanocytesthat are present in the affected epithelium,
3,4
or withindermal melanophages.
1,4
The mechanism responsible for pigmentation in Bo-wen’s disease is not yet fully elucidated. Burkitt has
proposed that the hyperpigmentation of anogenitalBowen’s disease might be secondary to elevated tem-perature or simply an extension of the hyperpigmenta-tion that is naturally found in the anogenital area.
1
Ithas also been hypothesized that the neoplastic cellsmay produce factors that induce the proliferation ofmelanocytes and stimulate melanin production.
1
Fur-thermore, it has been observed that some pigmentedBowen’s disease arises from seborrheic keratoses.
4
This suggests the possibility that more than one mech-anism of hyperpigmentation may exist.
Since the presence of additional pigment does notalter the metastatic potential of Bowen’s disease,
1
theprinciples governing the treatment of nonpigmentedBowen’s disease are applicable. In this particular case,surgical excision was the treatment of choice. Otherviable therapeutic modalities include cryotherapy,electrodesiccation and curettage, application of topi-cal 5-fluorouracil, laser therapy, and radiotherapy.
3,7,8
References
1. Ragi G, Turner MS, Klein LE, Stoll HL. Pigmented Bowen’s diseaseand review of 420 Bowen’s disease lesions. J Dermatol Surg Oncol1988;14:765–9.
2. Papageorgiou PP, Koumarianou AA, Chu AC. Pigmented Bowen’sdisease. Br J Dermatol 1998;138:515–8.
3. Wagner RF, Grande DJ. Solitary pigmented Bowen’s disease of thescrotum. J Dermatol Surg Oncol 1986;12:1114–5.
4. Marschall SF, Ronan SG, Massa MC. Pigmented Bowen’s diseasearising from pigmented seborrheic keratoses. J Am Acad Dermatol1990;23:440–44.
5. Mora RG, Perniciaro C, Lee B, Cancer of the skin in blacks. III. Areview of nineteen black patients with Bowen’s disease. J Am AcadDermatol 1984;11:557–62.
6. Scarborough DA, Bisaccia EP, Yoder FW. Solitary pigmented Bo-wen’s disease. Arch Dermatol 1995;34:116–8.
7. Amagai N, Feldman D, Lobel S, Williams C. Irregularly pigmentedhyperkeratotic plaque on the thumb. Arch Dermatol 1995;129:1045–1048.
8. Kamiya M, Maehara R, Iizuka S, et al. Pigmented squamous cell car-cinoma with dendritic melanocyte colonization in the external audi-tory canal. Pathol Int 1999;49:909–12.
Figure 1. A 7 cm � 6 cm large, black, verrucous plaque near theanal opening.