Physician's Weekly Updates: Business of Medicine
-
Upload
physicians-weekly -
Category
Documents
-
view
225 -
download
4
description
Transcript of Physician's Weekly Updates: Business of Medicine

visit www.physiciansweekly.com 1PB
updates
www.physweekly.com/business-of-medicine
BUSINESS of MEDICINE
updatesLearn to RelaxNurses
to the Rescue

visit www.physiciansweekly.com 32
Win a MiniClick here to enter and win
www.physiciansweekly.com

visit www.physiciansweekly.com 32
Director, Business Dev. dave dempsey Mark elms andy skean dennis turner
Project Manager diana Marganski
Director of Finance tom Campbell
Sales
President Clay Romweber
VP, Product Marketing & Development tom Richards
VP, Operations & Infrastructure derek Mirdala
Management
Editorial Director Keith d’Oria
Senior Editor Janine anthes
Associate Editor Chris Cole
Creative Director Jonathan Nichol
Associate Art Director timothy Hodges
Interactive Marketing Spc sally Ladd
Production Director George Camba
Production Specialist Lacey archer
Administrative Assistant erika Kaufman
Editorial
Vice President denise Halverson
Project Administrator Lauri Hutchinson
Mngr Hospital Relations Jacquie Jacovino
Institutional Relations amy Johnson Michelle McKenna sadie steib Judy Wengryn
Customer Service
Table of Contents
A Message From the EditorWe at Physician’s Weekly are proud to present this monograph on the business of medicine. Created with the assistance of key opinion leaders and experts in the field, these features discuss challenges and opportunities that are occurring in a changing healthcare environment. Physician’s Weekly will continue to feature topics that affect medical professionals beyond the realm of patient care in the upcoming months. Your feedback and opinions are welcome, email [email protected]. Thanks for reading!
sincerely,
Keith d’Oria Editorial Director, Physician’s Weekly
4
At the Boiling Point: Physiucian Burnout & Work-Life Balance— Colin P. West, Md, PhD
12
Improving Collaboration Between Emergency Physicians & Hospitalists— Alpesh Amin, MD, MBA,
MACP, SFHM & Charles V. Pollack Jr., MA, MD, FACEP, FAAEM, FAHA
8
Hospitalists & the Intensivist Shortage— Eric M. Siegal, MD, SFHM
16
The Impact of the Next Generation of Nursing— Courtney H. Lyder,
ND, GNP, FAAN Physician’s Weekly™ (ISSN 1047-3793) is published by Physician’s Weekly, LLC, a division of M/C Holding Corp. The service is free for qualifying institutions. Please contact us at [email protected] for more information. Offices: Physician’s Weekly, LLC, 5 Commerce Way, Suite 202, Hamilton, NJ 08691; and 180 Mount Airy Road, Suite 102, Basking Ridge, NJ 07920. Reproduction without written permission from the publisher is prohibited. Copyright 2013, Physician’s Weekly, LLC.
Publication of an advertisement or other product mention in Physician’s Weekly should not be construed as an endorsement of the product or the manufacturer’s claims. The appearance of or reference to any person or entity in this publication (including images) does not constitute an expressed or implied endorsement of the product mentioned. The reader is advised to consult appropriate medical literature and the product information currently provided by the manufacturer of each drug to verify indications, dosage, method, duration of administration, and contraindications. All editorial is developed independent of influence from advertising brands/companies.

visit www.physiciansweekly.com 54
Boiling Point Physician Burnout & Work-Life Balance
At the
4
Click here to view this article online.

visit www.physiciansweekly.com 54
Boiling Point Physician Burnout & Work-Life Balance
Burnout appears to be more common among physicians than among other workers throughout the country, particularly for those in specialties at the front line of care access.
P revious research has indicated that many physicians throughout the united states experience professional burnout, a syndrome
characterized by emotional exhaustion, depersonali-zation, and a low sense of personal accomplishment. studies suggest that burnout can reduce quality of care and increase risks for medical errors, among other negative consequences. Furthermore, there are other adverse personal consequences for physicians that have been linked to burnout, including contri-butions to broken relationships, problematic alcohol use, and suicidal ideation.
“We have limited data characterizing physician burnout, but few studies have evaluated rates of burnout among u.s. physicians nationally,” says Colin p. West, Md, phd. “previous investiga-tions have speculated on which medical or surgical specialty areas are at higher risk, but these analyses have not been definitive.” He adds that research is also lacking on how rates of burnout for physicians compare with rates for u.s. workers in other fields.
Medical Specialty Matters in BurnoutIn the Archives of Internal Medicine, dr. West and colleagues published a study on burnout involving a large sample of u.s. physicians from all specialty disciplines using the american Medical association physician Masterfile. surveys were used to assess the prevalence of emotional exhaustion, enthusiasm dissipation, cynicism, depression, suicidal tenden-cies, negative views on work-life balance, and low professional esteem among physicians.
COLIN P. WEST, MD, PHDAssociate Professor of Medicine & Biostatistics
Department of Internal Medicine Mayo Clinic
visit www.physiciansweekly.com 5

visit www.physiciansweekly.com 76
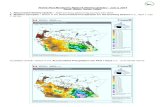
after collecting responses from 7,288 physicians from various healthcare settings, 45.8% reported experi-encing at least one symptom of professional burnout. “We observed substantial differences in burnout by specialty,” says dr. West (Figure). The highest rates of burnout were seen in physicians at the front lines of care, most notably family doctors, general internists, and emergency physicians. In addition, the following was observed among surveyed physicians:
37.9% reported high levels of emotional exhaustion.
29.4% reported that cynicism was an issue.
12.4% reported having a low sense of personal accomplishment.
Importantly, dr. West notes that not all physicians reported an equal tendency toward professional unhappiness. “Our findings suggest that while many of the medical community’s first responders were more likely to suffer from some form of burnout, others were less likely to experience such issues.” These specialists included dermatologists, pediatricians, and preventive medicine physicians.
Burnout Among Physicians vs General WorkersThe study by dr. West and colleagues also compared physician burnout data with survey data from 3,442 working americans. In these analyses, physicians were more likely to have symptoms of burnout and to be dissatisfied with work-life balance than general workers. “It’s not surprising that many physicians are experiencing more stress than other u.s. workers because the healthcare system and consumers are increasingly putting higher demands and expectations on physicians,” dr. West says. “The implications are important. These findings raise concerns about the negative impact physician distress can have on quality of care.”
Increasing Efforts to Find SolutionsWith data showing that front-line physicians are experiencing greater distress than other working americans, dr. West says it is critical to target future research efforts on potential solutions for physicians. “When combined with positive changes in the

visit www.physiciansweekly.com 76
healthcare environment, our findings emphasize the need to help physicians learn how to reach out to friends, family members, and work colleagues to get help when symptoms of burnout emerge.”
Medical and physician support programs are already in place in every state throughout the country and have reported many successes in helping physicians with burnout and other kinds of stress-related problems. The challenge, according to dr. West, is that physi-cians—just like other people in general—often have trouble finding where to turn for help. support systems are available for physicians, he says, but they must be encouraged to look at their own stresses, determine what kind of help they need, and feel comfortable reaching out for that help when it is needed.
With increasing evidence that physician burnout adversely affects quality of care, findings from the study by dr. West and colleagues suggest that this problem threatens the foundation of the u.s. medical care system. “The problem of burnout won’t go away anytime soon as healthcare reform efforts are likely to increase demand for front-line care providers,” says dr. West. “It’s important to remember that the origins of burnout are rooted in the environment and care delivery system rather than in the personal characteristics of a few suscep-tible people. policy makers and healthcare organi-zations must address this problem for the sake of physicians and their patients.
Colin P. West, MD, PhD, has indicated to Physician’s Weekly that he has or has had no financial interests to report.
Readings & Resources
Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377-1385. Available at: http://archinte.jamanetwork.com/article.aspx?articleid=1351351.
West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463-471.
Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721.
Dyrbye LN, Massie FS Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173-1180.

visit www.physiciansweekly.com 98
The growing intensivist shortage is challenging hospitals’ ability to care for critically ill patients. despite numerous recommendations that
intensivists manage critically ill adults, the majority of american hospitals cannot meet this standard. as a consequence, hospitalists have become de facto intensivists in many hospitals, with 75% reporting that they practice in the ICu. While legitimate concerns have been raised whether hospitalists are uniformly qualified to practice in the ICu, the issue has become moot at many hospitals where intensiv-ists are either in short supply or entirely absent.
efforts are needed to ensure that hospitalists manage critically ill patients safely, effectively, and seamlessly. In the Journal of Hospital Medicine and Critical Care Medicine, the society of Hospital Medicine and the society of Critical Care Medicine co-published a position paper on training the hospitalist workforce
to address the intensivist shortage. In this paper, we discussed the potential value of hospitalists in the ICu and the importance of enhancing hospitalists’ skills to provide critical care services.
Adding Value & Enhancing Skills of HospitalistsHospital medicine and critical care medicine share similar structures, competencies, and values, posi-tioning hospitalists as a logical solution to the inten-sivist shortage. Many of the competencies needed for practicing critical care medicine are encompassed in internal medicine training as well as in core competencies in hospital medicine. The ideology and mechanics of high-performing hospitalist and intensivist programs are similar, yet despite these commonalities, hospitalists remain largely untapped as a potential source of new intensivists.
Exploring Alternative Critical Care ModelsWith no solution to the intensivist shortage in sight, alternative critical care delivery models are needed. We proposed a 1-year critical care fellowship track for experienced internal medicine hospitalists.
ERIC M. SIEGAL, MD, SFHMDirector, Critical Care Service
Aurora St Luke’s Medical Center
Clinical Associate Professor of Medicine University of Wisconsin School of Medicine and Public Health
Hospitalists & the Intensivist Shortage

visit www.physiciansweekly.com 98
although critical care medicine is a 2-year fellow-ship, only 1 year of clinical rotations is required for board eligibility. Furthermore, a 1-year critical care training track already exists for other medical specialists and should be relevant and available to experienced hospitalists as well. Bringing qualified hospitalists into the critical care workforce through rigorous sanctioned and accredited 1-year training programs could open a new intensivist training pipeline. It can also offer more critically ill patients the benefit of providers who are unequivocally qualified to care for them.
Thinking Outside the Box to Alleviate the ShortageThe key is for hospitals, clinicians, and other key constituents to think outside the box when devel-oping strategies to address the intensivist shortage. Rigorously training hospitalists as intensivists could dramatically alleviate some of the burden and should be part of a broader initiative to reform critical care training through a unified, cross-disciplinary approach to developing an intensivist workforce.
Readings & Resources
Siegal EM, Dressler DD, Dichter JR, et al. Training a hospitalist workforce to address the intensivist shortage in American hospitals: a position paper from the Society of Hospital Medicine and the Society of Critical Care Medicine. J Hosp Med. 2012;7:359-364. Available at: www.medscape.com/viewarticle/768430 .
Kelley MA, Angus D, Chalfin DB, et al. The critical care crisis in the United States: a report from the profession. Chest. 2004;125:1514-1517.
Krell K. Critical care workforce. Crit Care Med. 2008;36:1350-1353.
Mayglothing JA, Gunnerson KJ, Huang DT. Current practice, demographics and trends of critical care trained emergency physicians in the United States. Acad Emer Med. 2010;17:325-329.
Murin S. Hospitalists in the intensive care unit: an intensivist perspective. The Hospitalist. 1999;3:5.
Eric M. Siegal, MD, SFHM, has indicated to Physician’s Weekly that he has no financial disclosures to report.
Hospitalists & the Intensivist Shortage
Click here to view this article online.

visit www.physiciansweekly.com 1110
Emergency Physicians & Hospitalists
Improving Collaboration Between
10
Click here to view this article online.

visit www.physiciansweekly.com 1110
A s hospital care is increasingly being driven by emergency physicians and hospitalists, ongoing collaboration between these entities
is vital to enhancing patient care, education, and quality and safety outcomes.
The number of hospitalized patients being co-managed by emergency physicians (eps) and hospitalists is increasing throughout the united states, as primary care providers and medical subspecialists limit their inpatient duties. In fact, emergency medicine and hospital medicine are second only to primary care as the largest group of physicians in the country. “It’s not uncommon
for patients to be admitted through the ed and discharged after several days, after being seen only by eps and hospitalists,” says Charles V. pollack Jr., Ma, Md, FaCep, FaaeM, FaHa. “Both specialties are typically represented 24 hours a day in hospitals.”
In many cases, eps and hospitalists are often the only attending physicians after hours in the hospital. “They share a common practice space and govern decisions about the use of the most expensive care in medicine,” dr. pollack says. “However, the collabo-ration between eps and hospitalists has traditionally been limited to bedside conversations when patients are admitted from the ed to hospital medicine services. This leaves hospitals vulnerable to missing opportunities to improve quality of care while also reducing costs of care.”
Stop, Collaborate, & ListenWith the growing importance of shared patient care between eps and hospitalists, improved collabora-tion is essential and overdue. to further expand
Alpesh Amin, MD, MBA, MACP, SFHMThomas and Mary Cesario Endowed Chair, Department of Medicine
Professor of Medicine, Business, Public Health, & Nursing Science
Executive Director, Hospitalist Program University of California, Irvine
Charles V. Pollack Jr., MA, MD, FACEP, FAAEM, FAHAProfessor of Emergency Medicine, Pennsylvania Hospital
University of Pennsylvania Perelman School of Medicine
As hospital care is increasingly being driven by emergency physicians and hospitalists, ongoing collaboration between these entities is vital to enhancing patient care, education, and quality and safety outcomes.
Emergency Physicians & Hospitalists
Improving Collaboration Between

visit www.physiciansweekly.com 1312
upon the need for better collaboration between eps and hospitalists, dr. pollack co-authored a review on the topic and a call to action with alpesh amin, Md, MBa, MaCp, sFHM, in issues of the Journal of Emergency Medicine and the American Journal of Medicine. dr. amin says this collaboration is important to enhancing care. “Better collaboration can facilitate communication, develop teamwork, improve efficiency, and encourage fewer break-downs in care,” he says. “The goal should be to provide seamless opportunities for care and to help develop clinical pathways and guidelines across these specialties.”
to achieve the most efficient hospital care and optimize outcomes, eps and hospitalists need to move out of their “silos,” according to drs. amin and pollack. “efforts are needed to ensure that these specialties work well together in a concerted effort to meet quality, customer service, length of stay, and throughput demands,” adds dr. amin.
“The collaboration needs to be well organized, with concrete interventions for enhancing this alliance [table 1].”
“Hospitalists, eps, and a combination of the two are increasingly managing cardiovascular disease, stroke, COpd, and pneumonia, among other common disease states presenting to eds,” explains dr. pollack. “simple interventions to increase collabora-tion between eps and hospitalists are available and should be implemented. It’s more important than ever to ensure that patients are managed consis-tently across a continuum of care. This can best be accomplished by having eps and hospitalists work together throughout hospitalizations so we can opti-mize follow-up care and perhaps avoid preventable readmissions.”
Establishing Protocols for Collaborationdrs. amin and pollack agree that eps and hospital-ists need to take extra steps toward collaborating to ensure consistency of care as patients are transitioned from eds to hospital settings. “after developing consistent pathways, information can be collected to measure outcomes,” says dr. amin. “processes and protocols can then be refined to further improve the quality of care.”
to establish these protocols, dr. pollack suggests that physicians from both specialties, led by a physi-cian champion from each group, meet outside of clinical shift hours to discuss the best available clin-ical evidence on the evaluation and management of common diagnoses that present to the ed and often require admission. “Buy-in from the entire team is crucial,” he says. “all constituents need to be aware of the increased collaborative efforts and why they’re being implemented. to improve care, standardiza-tion must be developed and ongoing. every ep and hospitalist should be empowered to contribute to these efforts. By harnessing our collective resources and recognizing this important ongoing need, we can avoid working in silos while simultaneously enhancing patient outcomes and satisfaction as well as quality of care.”

visit www.physiciansweekly.com 1312
Establish a Culture of Collaboration
dr. amin adds that both hospitalists and eps are instrumental in helping their hospitals be successful. “The more these entities collaborate, the more likely that their institutions and their patients will benefit.” dr. pollack says the standard care protocol
of having eps only call on hospitalists when patients require admission to the hospital is an obsolete concept. “Through better collaboration between our specialties, there is hope that we can maximize our treatment capabilities for the patients presenting to our institutions. The only way this can happen is if there’s a conscious, deliberate effort to establish a culture of collaboration.”
Readings & Resources
Pollack C, Amin A, Talan D. Emergency medicine and hospital medicine: a call for collaboration. The Journal of Emergency Medicine. 2012;43:328-334. Available at www.jem-journal.com/article/S0736-4679%2812%2900140-0/abstract
Hamel M, Drazen J, Epstein A. The growth of hospitalists and the changing face of primary care. N Engl J Med. 2009;360:1141-1143.
Kuo Y-F, Sharma G, Freeman J, Goodwin J. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102-1112.
Pines JM, Batt RJ, Hilton JA, Terwiesch C. The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011;58:331-340.
Alpesh Amin, MD, MBA, MACP, SFHM, has indicated to Physician’s Weekly that he has no financial interests to disclose.
Charles V. Pollack Jr., MA, MD, FACEP, FAAEM, FAHA, has indicated to Physician’s Weekly that he has received grant/research support from Luitpold Pharma. He has also served as a consultant for Janssen.

visit www.physiciansweekly.com 1514
The patient protection and affordable Care act will mean the addition of as many as 35 million americans with health insur-
ance into a healthcare system already stretched to capacity with overcrowded eds, shrinking resources, and a dramatic shortage of primary care physicians (pCps). even before health reform, the association of american Medical Colleges estimated that an addi-tional 45,000 pCps would be needed by
2020 to keep up with demand. Yet, fewer and fewer medical school students are choosing primary care medicine.
Qualified, Experienced Nurses Can HelpThe professionals most qualified to fill this physician shortage are nurse practitioners (Nps), registered nurses who have completed graduate-level educa-tion, and nurses who have already worked 10 or more years and have accumulated practical, bedside
experience that complements what was learned in the classroom. pCps everywhere would be wise
COURTNEY H. LYDER, ND, GNP, FAANDean and Professor, UCLA School of Nursing
UCLA Los Angeles Health System
The Impact of the Next Generation
of Nursing
14

visit www.physiciansweekly.com 1514
to look at Nps as a natural complement to their practice and a logical partner in caring for their patients. Nurse practitioners are already tasked with delivering some medical care, including:
• Prescribing or renewing prescriptions for most drugs.
• Ordering blood tests.
• Performing routine medical examinations.
• Monitoring chronic conditions.
• Counseling patients about prevention.
• Treating colds, sore throats, and the flu.
Many states have expanded the scope of Np duties and responsibilities. For example, Montana allows Nps to work without any physician supervision. By contrast, texas requires physicians’ direct, on-site supervision at least 20% of the time. additionally, 28 states are debating whether to further loosen restrictions that prevent Nps from performing more tasks independently.
The influx of newly insured patients into the health-care system will also profoundly affect where people receive care. some patients will prefer to receive
treatment for minor conditions in convenient settings like retail clinics. Nurses and Nps will again be called upon to fill this important role so that physicians can focus on areas where their expertise can be best put to use.
Redefined & Expanded Nursing Rolespresently, nurses make up the largest segment of the healthcare workforce. Without too much fanfare and away from the media spotlight, nurses are rede-fining and expanding their roles. They are champi-oning quality-of-care improvements, spearheading research innovation, advocating for patient rights, and making contributions in ways that redefine their profession. They’ve been doing all of this while not surrendering their historical role as patient advocates and trusted bedside clinicians.
today’s shortage of pCps will be exacerbated unless we look to nurses and Nps to fill the gaps in providing care. By partnering physicians and nurses together and seeking out new ways to care for patients that leverage the best that each profession has to offer, it’s likely that nursing’s greatest role lies ahead.
Readings & Resources
Institute of Medicine. The future of nursing: leading change, advancing health. Washington, DC: National Academies Press, 2010.
Kaiser Family Foundation. Improving access to adult primary care in Medicaid: exploring the potential role of nurse practitioners and physician assistants. March 2011. Available at: www.kff.org/medicaid/upload/8167.pdf .
Health Resources and Services Administration. The registered nurse population: findings from the 2008 National Sample Survey of Registered Nurses. September 2010. Available at: bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf .
California Health Care Foundation. Scope of practice laws in health care: rethinking the role of nurse practitioners. January 2008. Available at: www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/S/PDF%20ScopeOfPracticeLawsNursePractitionersIB.pdf .
Courtney H. Lyder, ND, GNP, FAAN, has indicated to Physician’s Weekly that he has no financial disclosures to report.
Click here to view this article online.

www.physweekly.com
get connected.
email like plus read tweet feed