Pharyngeal flap versus sphincter pharyngoplasty for the treatment of velopharyngeal insufficiency: A...
Click here to load reader
-
Upload
jessica-collins -
Category
Documents
-
view
216 -
download
1
Transcript of Pharyngeal flap versus sphincter pharyngoplasty for the treatment of velopharyngeal insufficiency: A...

Journal of Plastic, Reconstructive & Aesthetic Surgery (2012) 65, 864e868
Pharyngeal flap versus sphincter pharyngoplasty forthe treatment of velopharyngeal insufficiency:A meta-analysis*
Jessica Collins a, Kevin Cheung a, Forough Farrokhyar b, Nick Strumas a,*
aDepartment of Surgery, Division of Plastic and Reconstructive Surgery, McMaster University, Hamilton, Ontario, CanadabDepartment of Surgery and Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ontario, Canada
Received 20 September 2011; accepted 26 January 2012
KEYWORDSPharyngeal flap;Sphincterpharyngoplasty;Velopharyngealinsufficiency;Meta-Analysis
* Presented at: The 16th Congress of(May 22nde27th 2011).* Corresponding author. Health Scie
Canada. Tel.: þ1 905 525 9140x73594E-mail address: nstrum@mcmaster
1748-6815/$-seefrontmatterª2012Bridoi:10.1016/j.bjps.2012.01.020
Summary Background: Velopharyngeal insufficiency (VPI) has been reported in 5e20% ofpatients following cleft palate repair. Since VPI can limit communication, determining whichoperative procedure leads to the greatest improvement is of utmost importance. Since thereis no consensus, this meta-analysis aims to determine which procedure results in the mostsignificant resolution of VPI.Methods: Two independent assessors undertook a literature review for articles that compareprocedures aimed at treating VPI. Study quality was determined using validated scales. Levelof agreement was assessed using intra-class coalition coefficient analysis. The heterogeneitybetween studies was evaluated using I2 and Cochran’s Q-statistic. Random effect model anal-ysis and forest plots were used to report a pooled odds ratio (OR) and 95% confidence intervals(CI) for treatment effect. A p-value of 0.05 was considered for statistical significance.Results: Two randomised controlled trials (RCTs) comparing pharyngeal flap to sphincter phar-yngoplasty were obtained. A total of 133 patients were included, with follow-ups at 3e4months. The pooled OR was determined to be 2.95 (95% CI: 0.66e13.23) in favour of thepharyngeal flap.Conclusions: Based on these RCTs, which currently compose the highest quality data thatcompares pharyngeal flap versus pharyngoplasty, the pooled treatment effect suggestsa possible trend favouring pharyngeal flap.ª 2012 British Association of Plastic, Reconstructive and Aesthetic Surgeons. Published byElsevier Ltd. All rights reserved.
the International Confederation for Plastic Reconstructive and Aesthetic Surgery, Vancouver, Canada
nces Centre, McMaster University, 1200 Main Street West, Room 4E9, Hamilton, Ontario L8N 3Z5,; fax: þ1 905 521 9992..ca (N. Strumas).
tishAssociationofPlastic,ReconstructiveandAestheticSurgeons.PublishedbyElsevierLtd.All rightsreserved.

Meta-analysis of VPI treatment 865
Introduction
Velopharyngeal insufficiency (VPI) refers to a failure of thevelum and lateral and posterior pharyngeal walls to sepa-rate the oral cavity from the nasal cavity during speech anddeglutination. This incomplete closure of the velopharynxcan occur secondary to a structural defect (i.e., gross tissuedefect, short soft palate, deep nasopharynx, hypertrophiedtonsils, and cleft palate) or after procedures that changethe anatomy (i.e., adenoidectomy).1 Following cleft palaterepair, VPI remains unresolved in 5e20% of patients.2
Untreated, VPI can have a significant functional impacton breathing, eating, and speech. Speech in VPI is charac-terised by hypernasal resonance, decreased intraoralpressure for pressure consonants, and compensatory artic-ulation errors. Diagnosis can be made clinically and char-acterised with video nasopharyngoscopy orvideofluoroscopy.1,3
Surgery is the definitive treatment of VPI with the goal ofcreating a functional seal between the nasopharynx and theoropharynx during speech while avoiding nasal airwayobstruction; however, the optimal technique is unknown.While there are numerous variations, the two most commonsurgical techniques include pharyngeal flap and sphincterpharyngoplasty. The pharyngeal flap procedure consists ofsuturing a flap from the posterior pharyngeal wall to theposterior border of the soft palate. This flap, whichincludes mucosa and superior pharyngeal constrictormuscle, may be superiorly or inferiorly based. It functionsas an obturator, allowing the pharyngeal port to be closedby the medial movement of the lateral pharyngeal walls onboth sides of the flap. In contrast, the sphincter phar-yngoplasty procedure involves the elevation of bilateralsuperiorly-based palatopharyngeal mucosa and muscleflaps, whose distal ends are sutured to the contralateralside onto the posterior pharyngeal wall.4 This createsa transverse mound of tissue as the flaps cross over eachother, leading to a smaller central port and a shorterdistance between the palate and posterior pharyngeal wall.These techniques may be highly dependent upon surgeonexperience5 and the age of the patient,6,7 and may requireindividual tailoring to the size and nature of the velophar-yngeal defect.8,9
Evidence from the literature regarding the most effec-tive surgical technique has been largely based on retro-spective studies. Conclusions have been mixed,4 and fewrandomised studies exist.10 The purpose of this study is todetermine the optimal surgical procedure for the treat-ment of VPI following cleft palate repair.
Methods
This systematic review was performed in accordance witha protocol that prescribed search strategy, eligibilitycriteria, outcomes and statistical analyses. Our aim was toperform a pooled analysis of the outcomes.
Literature search
Cochrane, Medline, Embase, and Cinahl databases wereindependently reviewed by two of the authors (J.C. and
K.C.). Search terms included: cleft palate, velopharyngealinsufficiency, palatopharyngeal incompetence, pharyngealflap, and sphincter pharyngoplasty. These were arrangedusing varying combinations of Boolean operators ‘‘AND”,‘‘NOT”, and ‘‘OR”. Additional searches were performedmanually through reference lists of review articles andrelevant studies. Titles and abstracts were independentlyscanned for relevance by two authors. A review of thecomplete article was carried out if relevance was not clearbased on the abstract alone.
Study eligibility criteria
To be selected, studies had to meet the following inclusioncriteria: 1) The studied population included non-syndromicpediatric patients of any gender who had undergone priorcleft palate repair (any type of cleft palate, any type ofrepair); 2) the patients demonstrated residual velophar-yngeal insufficiency significant enough to require surgicalcorrection; 3) the operative plan had to be eithera pharyngeal flap (superiorly or inferiorly based) orsphincter pharyngoplasty, and these two procedures had tobe compared to each other; 4) outcome measures neededto include the degree of velopharyngeal insufficiencyresolution; 5) specific follow-up times had to be docu-mented; 6) studies had to be of a relatively high level ofevidence (randomised controlled trials [RCTs] andprospective cohort studies). Exclusion criteria consisted of:1) syndromic patients; 2) adult patients; 3) patientsundergoing concomitant cleft palate and velopharyngealinsufficiency surgery; 4) patients undergoing repeatedvelopharyngeal insufficiency surgery; 5) an operative planconsisting of a different procedure than a pharyngeal flapor sphincter pharyngoplasty (e.g., posterior pharyngealwall augmentation); 6) outcomes with no reported methodsof evaluation or follow-up times. Any disagreements inarticle selection between the two authors were resolvedthrough discussion until consensus was obtained.
Outcome measures
The primary outcome targeted for analysis was velophar-yngeal insufficiency resolution. This was defined in thearticles with outcome measures including perceptualspeech parameters, sleep studies, nasalance measuresand/or endoscopic features. For each selected article, dataon velopharyngeal insufficiency resolution after pharyngealflap or sphincter pharyngoplasty, as well as follow-up times,were collected.
Quality assessment
The two authors assessed article quality using validatedDetsky and MINORS scales. Detsky is a validated scale thatcan be used for RCTs, with global scores of 20 for positivetrials and 21 for negative trials.11 MINORS is also a validatedscale and the global ideal score is 16 for non-comparativestudies and 24 for comparative studies.12 Intra-class coali-tion coefficient analysis was applied to calculate the levelof agreement in quality assessment between the twoauthors using SPSS version 18.0 (SPSS Inc, Chicago, IL).

866 J. Collins et al.
Statistical analysis
Heterogeneity analysis was performed using Cochran’s Q-statistic to determine if the selected articles were homo-geneous enough to be analyzed together in the meta-analysis. This is a chi-squared test used to evaluate thestatistical significance of the heterogeneity betweenstudies, and a p-value of less than 0.1 was deemed to showheterogeneity. As part of this analysis, heterogeneity wasquantified by calculating I2, which is the percentage ofvariability in results due to heterogeneity rather thansampling error or chance.
In the presence of heterogeneity or if the sample sizeswere too small, a random effect model would be used asopposed to a fixed effect model. A meta-analysis of pooledodds ratios was then performed. An a of 0.05 was consid-ered a criterion for statistical significance. Forest plotswere produced, from which the odds ratio (the ratio of theodds of VPI resolution after a pharyngeal flap, to the oddsof VPI after a sphincter pharyngoplasty) with 95% confi-dence interval (CI) and p-value were reported. RevMan 5.0was used for data analysis (Review Manager, softwaredeveloped for The Cochrane Collaboration).
Results
A total of 621 titles and abstracts were obtained throughliterature searches and were scanned by two of the authors(Figure 1). Six hundred and nine of these were excluded dueto the following reasons: 1) repeating articles; 2) non-comparative studies (studies discussing only one type ofprocedure); 3) review articles discussing the topic but notstudying a specific group of patients; 4) articles discussingpalatoplasty alone; and 5) articles discussing procedures forvelopharyngeal insufficiency other than a pharyngeal flapor sphincter pharyngoplasty. The remaining 12 studies werethen reviewed in their entirety, and seven more articleswere rejected since they either discussed primary palato-plasty or procedures other than a pharyngeal flap orsphincter pharyngoplasty, or applied specific selectioncriteria to determine which of the two procedures to carryout. Out of the five remaining papers, three were RCTs13e15
Figure 1 Literature search results and article exclusionprocess.
and two were retrospective non-randomised case series(non-RCTs).16,17 A final round of article exclusion was thenperformed where the two non-RCT/non-prospective cohortstudies were excluded due to their retrospective method-ology and consequent lower level of evidence. Further-more, since patient pool duplication in two14,15 of the threeRCTs was deemed possible,c the earlier of the two RCTsfrom the same authors14 was excluded.d
The two authors (J. C. and K. C.) independently assessedthe quality of the studies. The intra-class coalition coeffi-cient was 0.977 (95% CI: 9.0%e99.0%). This indicated a highlevel of agreement (97.7%) between the two reviewers, buta wide confidence interval was obtained because of thesmall number of studies.
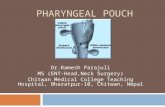
Heterogeneity analysis for the two RCTs13,15 showed a p-value of 0.10 and an I2 value of 64% (Figure 2). Sincea certain degree of heterogeneity was present, and samplesizes were small, a random effect model was used asopposed to a fixed effect model.
Data on VPI resolution after pharyngeal flap or sphincterpharyngoplasty, as well as follow-up times, were collectedfrom both RCTs (Table 1). Abyholm et al.13 evaluatedpatients at both three months and one year, whereas Ysunzaet al.15 performed their follow-up at four months; the three-month follow-up data from Abyholm et al. was thereforeused for consistencywith that of Ysunza et al. The forest plotof this data was produced through a random effect modelanalysis (Figure 2). The odds ratio was found to be 2.95 (95%CI: 0.66e13.23) in favour of the pharyngeal flap.
Discussion
The aim of this meta-analysis was to determine which ofthe two most common operative procedures for the treat-ment of velopharyngeal insufficiency is more effective:pharyngeal flap or sphincter pharyngoplasty. Aftera systematic literature review followed by a few rounds ofarticle exclusion, with exclusion of potentially duplicatedresults,14 the data from two RCTs13,15 comparing these twotechniques were pooled and analyzed. The analysis wasperformed using a random effect model because of lowhomogeneity and the small number of studies.
Since two of the three RCTs were reported by the samegroup of authors,14,15 it is possible that some of their casesmay have been duplicated, therefore affecting our resultsif both RCTs were included in our study. As described byTramer et al.,16 who examined the impact of duplicate datain meta analyses, inclusion of duplicates can lead to over-estimation of efficacy and safety of treatment. Althoughnarrowed confidence intervals and more precise pointestimates are desirable effects of pooling data througha meta-analysis, exaggeration of the accuracy of the pointestimate (narrower confidence interval) as a result of anartificially inflated sample size can be misleading.16
c We were unsuccessful in contacting the senior author of thestudies in references 14 and 15 for clarification.d It is of note that inclusion of this potentially duplicate RCT in
a separate statistical analysis did not change the conclusion of thisstudy; the odds ratio was slightly changed and the confidenceinterval was more narrow (odds ratio 2.45; 95% CI 0.85e7.07), stillin favour of the pharyngeal flap.

Figure 2 Forest plot for the number of patients with resolution of VPI after pharyngeal flap and sphincter pharyngoplastyprocedures at follow-up times of 3e4 months for the RCTs of Abyholm13 and Ysunza.15 Odds ratio and 95% confidence intervals foreach study and for the meta-analysis as a whole are shown.
Meta-analysis of VPI treatment 867
The results of the two-RCT13,15 analysis indicate thatpatients who have undergone a pharyngeal flap are threetimes more likely to have VPI resolution at 3e4 monthspost-operatively when compared to those who haveundergone a pharyngoplasty. However, this result did notreach statistical significance. Possible explanations include:no significant difference between the two techniques, orinsufficient statistical power to demonstrate a significantdifference. While the methodological qualities of the RCTswere sufficient for inclusion in the meta-analysis, smallmethodological flaws may have impacted the results of thisstudy.
The study by Abyholm et al.13 received the highestquality ratings from the two authors performing the qualityassessment. This international multi-center RCT showedclear patient inclusion and exclusion criteria with detailedexplanations for excluded patients. Randomisation of theprocedure allocation sequence was conducted usingcomputer-generated random numbers, with allocationconcealment through sealed envelopes. The two proce-dures were standardised between surgeons. Blinded asses-sors used objective measures such as speech,nasoendoscopy, and sleep studies to evaluate patients forVPI resolution. Appropriate statistical tests were used, anda sample size calculation was performed using data froma previous retrospective pilot study done at the sameinstitution. This analysis indicated the need for 133 patientsper group for a b-power of 80%, an a of 0.05, a 20%difference in proportion, and a 10% expected loss to follow-up rate. However, the sample size needed for statisticalsignificance was not achieved. Although this is the only trueweakness of this paper, it is significant since low power canlead to b error, indicating that the achieved significantresults might have been due to chance.
Table 1 RCTs selected for analysis: Name of first author,follow-up time, number of patients included in the studies(N), and percentage of patients with VPI resolution afterpharyngeal flap and sphincter pharyngoplasty procedures.
Author Follow-up N Pharyngealflap
Sphincterpharyngoplasty
Abyholmet al.13
3 months 63 26/32 (82%) 13/31 (42%)
Ysunzaet al.15
4 months 70 31/35 (89%) 30/35 (85%)
The 2004 study by Ysunza et al.15 was a single-centerRCT with clear inclusion and exclusion criteria and noexcluded patients. However, since the randomisation ofprocedure allocation and concealment methods were notdescribed, it is impossible to determine if these wereadequately conducted. Of note, randomisation of proce-dure allocation was done through block randomization intheir 2002 study.14 No details on the standardisation of thetwo procedures were given. Evaluation for VPI resolutionwas carried out by blinded speech pathologists thatassessed patients using objective measures such as speech,video nasopharyngoscopy, and multiview video fluoroscopy.Appropriate statistical tests were employed, but samplesize calculation was not performed, which could lead tob error. One could infer that the authors used the poweranalysis of their 2002 study; however, this should have beenmentioned if this were the case. This analysis indicateda need for 23 patients in each group to achieve a b-power of80%, an a of 0.05 and a 20% difference in proportion. With35 patients in each group, this requirement was fulfilled.However, a wide range in sample size calculations existsbetween Abyholm et al.13 and Ysunza et al.14 questioningthe most appropriate sample size. Since details of thecalculations are incomplete, it is difficult to explain sucha difference in numbers.
In addition to the RCTs described above, retrospectivenon-randomised case series have also attempted to compareboth procedures, without demonstration of clear superiorityof one procedure over the other. De Serres et al.17 compared18 patients who underwent a pharyngeal flap and 16 whounderwent sphincter pharyngoplasty. They were evaluatedat >7 months post-operatively through speech, nasoendo-scopy and video fluoroscopy. Patients with pharyngoplastyhad a higher VPI resolution rate (50%) than those withpharyngeal flap (22%), although these results were notstatistically significant. Pensler et al.18 compared 75pharyngeal flaps to 10 sphincteroplasties. Although nospecific follow-up times were mentioned, VPI improvementevaluated by speech was similar in both groups, with 75%improvement in the former and 70% in the latter. Anotherstudy byWilliams et al.19 compared 12 pharyngeal flaps to 12sphincteroplasties, although the latterwasonly used for gapsof 1 cmor less. Post-operative follow-up of 1e7 years showedVPI improvement rates of 83% for the flaps and 67% for thesphincteroplasties, although statistical significance was notdiscussed. After investigating 65 patientswhohadundergonepharyngeal flap and 123 patients with sphincteroplasties,

868 J. Collins et al.
Witt et al.20 described persistent VPI requiring surgicalrevision in 20% of pharyngeal flaps and 16% ofsphincteroplasties.
With regard to complications, the incidence of sleepapnea was noted to be similar in both groups, or slightlyhigher in the pharyngeal flap group. Abyholm et al.13 foundthat both procedures rarely resulted in clinically significantsleep apnea, and that no difference was found in its long-term incidence. Complications and re-operations werelow in both groups with no statistically significant differ-ences. Moreover, lengths of stay were similar in bothgroups. Ysunza et al.14,15 reported that there were nocomplications and no cases of sleep apnea post-operativelyin either group. The latter was credited to thorough eval-uation of patients for the need of adenoidectomy andtonsillectomy prior to their VPI procedure, as well as theoptional use of nasopharyngeal tubes in the post-operativeperiod. De Serres et al.17 reported post-operative obstruc-tive sleep symptoms in 17% of pharyngeal flap and 13% ofsphincteroplasty patients. However, sleep study-provenobstructive sleep apnea was found in all 17% of patientsin the flap group, but in none of the sphincteroplastypatients. Pensler et al.18 reported sleep apnea in 4% of thepharyngeal flap group and none in the sphincteroplasties.
Although the pharyngeal flap was found to be favouredin this meta-analysis, it is important to keep in mind thatfurther studies are needed before accepting these resultsas conclusive. Future RCTs regarding this topic should bethorough in their methodology to ensure high accuracy intheir results, since even the two RCTs used for this analysisshowed weaknesses in their design as described in ourquality analysis. These weaknesses cannot be eliminatedwhen pooling the data from these studies, and thereforethis may also affect the results of this meta-analysis.
Conclusion
The results of this meta-analysis of RCTs, which currentlycompose the highest quality data comparing the twotechniques, demonstrate a possible trend favouring thepharyngeal flap over sphincter pharyngoplasty for velo-pharyngeal insufficiency resolution, with no significantincrease in complication rates. As there is currentlya paucity of additional high-level evidence to support theclaims that one of these procedures is superior to the other,a further methodologically sound RCTwith longer follow-upis required to expand the evidence base on VPI treatment.
Funding
None.
Conflict of interest
None.
References
1. Johns DF, Rohrich RJ, Awada M. Velopharyngeal incompetence:a guide for clinical evaluation. Plast Reconstr Surg 2003;112:1890e7.
2. Sullivan SR, Marrinan EM, Mulliken JB. Pharyngeal flapoutcomes in nonsyndromic children with repaired cleft palateand velopharyngeal insufficiency. Plast Reconstr Surg 2010;125:290e8.
3. Marsh JL. The evaluation and management of velopharyngealdysfunction. Clin Plast Surg 2004;31:261e9.
4. Sloan GM. Posterior pharyngeal flap and sphincter phar-yngoplasty: the state of the art. Cleft Palate Craniofac J 2000;37:112e22.
5. Witt P, Wahlen J, Marsh JL, Grames LM, Pilgram TK. The effectof surgeon experience on velopharyngeal functional outcomefollowing palatoplasty: is there a learning curve? Plast ReconstrSurg 1998;102:1375e84.
6. Kirschner RE, Randall P, Wang P, et al. Cleft palate repair at 3to 7 months of age. Plast Reconstr Surg 2000;105:2127e32.
7. Marrinan EM, LaBrie RA, Mulliken JB. Velopharyngeal functionin nonsyndromic cleft palate: relevance of surgical technique,age at repair, and cleft type. Cleft Palate Craniofac J 1998;35:95e100.
8. Peat BG, Albery EH, Jones K, Pigott RW. Tailoring velophar-yngeal surgery: the influence of etiology and type of operation.Plast Reconstr Surg 1994;93:948e53.
9. Shprintzen RJ, Lewin ML, Croft CB, et al. A comprehensivestudy of pharyngeal flap surgery: Tailor made flaps. CleftPalate J 1979;16:46e55.
10. Nasser M, Fedorowicz Z, Newton JT, Nouri M. Interventions forthe management of submucous cleft palate. Cochrane Data-base Syst Rev 2008:CD006703.
11. Detsky AS, Naylor CD, O’Rourke K, McGeer AJ, L’Abbe KA.Incorporating variations in the quality of individual randomizedtrials into meta-analysis. J Clin Epi 1992;45:255e65.
12. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): Development and validation ofa new instrument. ANZ J Surg 2003;73:712e6.
13. Abyholm F, D’Antonio L, Davidson Ward SL, et al. Pharyngealflap and sphincterplasty for velopharyngeal insufficiency haveequal outcome at 1 year postoperatively: results of a random-ized trial. Cleft Palate Craniofac J 2005;42:501e11.
14. Ysunza A, Pamplona C, Ramırez E, et al. Velopharyngealsurgery: a prospective randomized study of pharyngeal flapsand sphincter pharyngoplasties. Plast Reconstr Surg 2002;110:1401e7.
15. Ysunza A, Pamplona MC, Molina F, et al. Surgery for speech incleft palate patients. Int J Pediatr Otorhinolaryngol 2004;68:1499e505.
16. Tramer MR, Reynolds DJM, Moore RA, McQuay HJ. Impact ofcovert duplicate publication on meta-analysis: a case study. BrMed J 1997;315:635e40.
17. de Serres LM, Deleyiannis FW, Eblen LE, et al. Results withsphincter pharyngoplasty and pharyngeal flap. Int J PediatrOtorhinolaryngol 1999;48:17e25.
18. Pensler JM, Reich DS. A comparison of speech results after thepharyngeal flap and the dynamic sphincteroplasty procedures.Ann Plast Surg 1991;26:441e3.
19. Williams H, Woolhouse F. Comparison of speech improvementin cases of cleft palate after two methods of pharyngoplasty.Plast Reconstr Surg 1962;30:36e42.
20. Witt PD, Myckatyn T, Marsh JL. Salvaging the failed phar-yngoplasty: Intervention outcome. Cleft Palate Craniofac J1998;35:447e53.