PHARMACY UPDATES METFORMIN INDUCED LACTIC ACIDOSIS PARTICULARITIES AND … · 2017-10-27 ·...
Transcript of PHARMACY UPDATES METFORMIN INDUCED LACTIC ACIDOSIS PARTICULARITIES AND … · 2017-10-27 ·...
Rev. Med. Chir. Soc. Med. Nat., Iaşi – 2013 – vol. 117, no. 4
PHARMACY UPDATES
1035
METFORMIN INDUCED LACTIC ACIDOSIS –
PARTICULARITIES AND COURSE
Anca-Monica Strugaru1, Gina Botnariu
3, Luminita Agoroaei
2,
Ioana-Cezara Grigoriu1,Elena Butnaru
2
University of Medicine and Pharmacy “Grigore T. Popa”- Iași Faculty of Pharmacy
1. Ph.D. student
2. Discipline of Toxicology
Faculty of Medicine
3. Discipline of Diabetes, Nutrition and Metabolic Diseases
METFORMIN INDUCED LACTIC ACIDOSIS – PARTICULARITIES AND COURSE (Ab-
stract): Diabetes mellitus is a widespread disease with many serious chronic complications. An
improvement in the oral antidiabetic medication in respect to its mechanism of action and toxi-
cology was needed in order to have effective therapies with high compliance and minimum
side effects. In this context, metformin is a widely used oral antidiabetic drug, which, through
its mechanism of action, has no risk of hypoglycemia. However, a rare but serious side effect
of biguanides is lactic acidosis. This paper presents a number of 13 cases of metformin-
associated lactic acidosis, which outline the circumstances triggering the adverse event and the
clinical therapeutic measures applied in the poisoned patients. The main situations that favor
metformin-associated lactic acidosis are renal impairment and tissue hypoxia, and the interven-
tion is adapted to the particular patient condition and symptoms, such as marked hypotension
and cardiac arrest. Although there are commonalities in describing the consulted patients, the
final prognosis is not dependent on the dose or metformin plasma levels, but rather on the asso-
ciated pathologies and medication. Keywords: DIABETES MELLITUS, METFORMIN,
LACTIC ACIDOSIS, RENAL IMPAIRMENT, HYPOXIA
Diabetes is probably one of the first ill-
nesses known to man. It was mentioned for
the first time in Egyptian manuscripts 3000
years ago, and in 1988 type 2 diabetes was
described as a component of the metabolic
syndrome. It represents one of the most
common forms of diabetes, characterized
by hyperglycemia, insulin resistance and
insulin deficiency. This illness results from
the interaction of genetic, social and behav-
ioral risk factors.
It is estimated that, in the year 2011, 366
million people had diabetes. This number is
thought to rise up to 552 by 2030. For the
same year, 2010, it is stated that the number
of deaths attributed to diabetes at a global
level is around 3.96 million for 20-79 age
group that is roughly 6.8% of the global
mortality rates for all age categories (1).
Metformin, a biguanide compound with
antidiabetic action, was first described in
the literature in 1922 by Werner and Bell,
as a product in the synthesis of N, N-
dimetilguanidine. In 1929, researchers
Slotta and Tschesche observed the sub-
stance to lower blood glucose in rats, and
they described the substance as the most
effective biguanide compound of the ones
Anca-Monica Strugaru et al.
1036
they studied (2).
Metformin has been accepted as an an-
tihyperglycemic agent in England in 1958,
in Canada in 1972, and in USA in 1995.
Currently, metformin is the first-line drug
in patients with type 2 diabetes who do not
have specific contraindications. Only in
2005 more than 42 million prescriptions for
metformin were issued in the United States
(3).
Besides its use in diabetic patients, met-
formin is also effective in polycystic ovary
syndrome and is being researched as an
antiviral and anticancer adjuvant.
Metformin activates an important en-
zyme called protein kinase AMP-activated
(AMPK), which plays an essential role in
body energy balance by regulating the
metabolism of carbohydrates and lipids.
Latest researches show that metformin
inhibits mitochondrial respiration by acti-
vating AMPK and the synthesis of fatty
acids. Metformin improves hyperglycemia
by reducing insulin resistance and plasma
insulin levels in the fasting state.
Known side effects of metformin in-
clude abdominal discomfort, nausea, vom-
iting, diarrhea, constipation, flatulence,
indigestion, heartburn (4). Another adverse
effect that may occur in long term metfor-
min administration is vitamin B12 deficien-
cy. Studies confirm that metformin can
cause malabsorption of vitamin B12 and
thus lower serum levels of this vitamin (5).
Lactic acidosis is a rare but serious ad-
verse effect of metformin associated with
its therapeutic use and overdose (6).
Lactic acidosis can be classified as fol-
lows: Type A (associated or caused by
inadequate oxygen transport to tissues) and
Type B (with adequate oxygen transport to
tissues). Type B has 3 sub-categories: B1 -
lactic acidosis associated with a disease
(eg, diabetes, asthma etc.), B2 - lactic aci-
dosis caused by drugs or toxins (e.g., cya-
nide, metformin, epinephrine, etc.), B3 -
lactic acidosis caused by congenital meta-
bolic disorders.
Depending on the cause, hyper-
lactatemia is defined as lactate levels be-
tween 2 and 5 mmol/L, although it is men-
tioned that lactic acidosis is present when
lactate levels are above 5 mmol/L and arte-
rial pH is lower than 7.35. These defini-
tions can however be arbitrary (7).
The lactate is the final product in anaer-
obic metabolism (it represents the product
obtained from the reduction of pyruvate by
lactate dehydrogenase enzyme). It is initial-
ly obtained in skeletal muscles, intestine,
brain and circulating erythrocytes, with a
production of approximately 1 mmol/kg/h.
The healthy liver takes the largest part of
the lactate and recycles it through three
main pathways: conversion to glucose (Co-
ri cycle), pyruvate oxidation, which can
then be oxidized to CO2 (Krebs cycle), and
transamination to alanine. The reduced
oxygen transport to tissues and cells cause
damage in oxidative phosphorylation, with
increasing intracellular amounts of NADH,
cofactor in the conversion of pyruvate to
lactate. Due to the close connection with
anaerobic metabolism the lactate was con-
sidered to be the end product of glycolysis
due to hypoxia (7).
Risk factors for the development of
metformin-associated lactic acidosis, such
as kidney failure, pre-existing heart dis-
ease, chronic lung injury with hypoxia, and
congestive heart failure, are usually con-
sidered contraindications to metformin
therapy. Age may be associated with de-
creased renal functions and the increase of
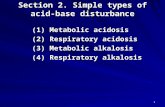
co morbidities (8). Figure 1 outlines the
mechanism of lactic acidosis production, in
Metformin induced lactic acidosis – particularities and course
1037
particular circumstances.
In patients who develop severe lactic
acidosis the symptoms are characteristic:
agitation, confusion, absent corneal reflex-
es, fixed dilated pupils, lethargy, convul-
sions, coma, and ultimately death (10).
Fig. 1. Lactic acidosis and the circumstances
which may increase the risk associated with metformin therapy (9)
We analyzed 13 cases of acute metfor-
min poisoning associated with lactic acido-
sis reported in the literature.
The circumstances that led to lactic aci-
dosis are presented in Table I. This severe
adverse effect also occurred in attempted
suicide by drug overdoses and chronic
administration to treat hyperglycemia.
Also, metformin-associated lactic acidosis
was present both in patients with or without
renal impairment. With regard to associated
medication, incriminated in the develop-
ment and/or worsening of metformin-
induced adverse effects, a definite link has
been established in the case of creatine co
administration (11).
The most frequent symptom of metfor-
min poisoning is gastrointestinal upset
when nausea, vomiting, diarrhea, ab-
dominal cramps, anorexia, epigastric dis-
comfort and pain, and loss of appetite oc-
cur. The occurrence of lactic acidosis caus-
es lethargy, confusion, dyspnea, hypother-
mia, hypotension, and hemodynamic insta-
bility. Table II lists all clinical observations
in patients with acute metformin poisoning.
The laboratory parameters reported for
acute metformin poisoning illustrate the
presence and course of lactic acidosis from
the time of diagnosis to the end of drug
treatment and hemodialysis. Table III
shows the evolution of laboratory values in
the patients. The therapeutic approach en-
tailed the normalization of acid-base im-
balance, the acceleration of lactate metabo-
lism process, the elimination of metformin,
simultaneously treating related diseases.
Following the patients evolution, metfor-
min-associated lactic acidosis proved re-
versible when diagnosis and initiation of
treatment are immediate so that therapeutic
measures to be effective.
Anca-Monica Strugaru et al.
1038
TABLE I
Particularities of triggering metformin induced lactic acidosis
Reference Treatment
with metformin Associated pathology Associated medication
Van Velzen,2008 (12) chronic treatment renal failure caused
by diclofenac various drugs
Saidi,2010 (11) 500 mg x 2/day * creatine
Yang,2009 (13) suicide attempt diabetic nephropathy *
Van Sloten,2012 (14) chronic treatment * *
Kreshak,2010 (15) chronic treatment
coronary heart disease,
peripheral vascular disease, hypertension,
hypercholesterolemia,
osteoarthritis
lisinopril, aspirin, metoprolol, clopidogrel, acetaminophen,
hydrocodone
Akoglu,2011 (16) suicide attempt:
144.5 g * *
Browers,2009 (17) chronic treatment total colectomy, acute renal
failure enalapril, atorvastatin, glicazid
Dell' Aglio,2010 (6) overdose: 75-100 g * *
Perrone,2011 (3) overdose * overdose of: risperidone, sertraline,
hydrochlorothiazide, glyburide
Perrone,2011 (3) chronic treatment multiple pathology,
final stage renal disease
amiodarone, clonidine,
valsartan, gabapentin, glyburide,
furosemide, atorvastatin, lisinopril,
amlodipine, omeprazole
Perrone,2011 (3) chronic treatment hypertension,
final stage renal disease *
Al-Makadma,2010 (18) suicide attempt:
40-45 g * *
Kim,2008 (19) overdose: 30 g hypertension carvedilol (Dilatrend®)
* Not specified.
TABLE II
The symptoms of acute metformin poisoning associated with lactic acidosis
Reference
Symptoms Other
symptoms gastro-
intestinal renal
central nerv-
ous system
cardio-
vascular Lungs
Van Velzen,2008
(12) * * confusion * * loss of appetite
Saidi,2010 (11) * oliguria and
then anuria
drowsiness,
malaise
cardiac
arrest
pulmonary
edema anorexia
Yang,2009 (13) * oliguria lethargy * * loss of appetite,
hypothermia
Van Sloten,2012
(154) * * delirium * * acute prostatitis
Kreshak,2010 (15) * * * * *
bilateral vision
loss without
associated pain,
hypothermia
Akoglu,2011 (16) * * * * * Hypothermia
Browers,2009 (17)
nausea,
vomiting,
abdominal
pain,
diarrhea
* * * * *
Dell' Aglio,
2010 (6) * * lethargy * * *
Perrone,2011 (3) * * lethargy * * *
Perrone,2011 (3) * * * *
Kussmaul
type breath-
ing, diffuse
rales
in the chest
weakness,
dry mucous
Perrone,2011 (3) * * * * dyspnea *
Al-Makadma,2010
(18) * *
marked
irritability,
deterioration of
consciousness
* * *
Kim,2008 (19) * * irritability * * *
* Not specified.
Metformin induced lactic acidosis – particularities and course
1039
TABLE III
The recorded laboratory values in patients with acute metformin intoxication
Synthesizing the data in the literature it
comes out that metformin-associated lactic
acidosis is a very rare complication when
no co morbidity is present (chronic kidney
disease, myocardial infarction, sepsis,
which can cause lactic acidosis even in the
absence of metformin use).
Associated pathologies and particular
conditions were encountered in case of:
creatine administration, kidney damage
Anca-Monica Strugaru et al.
1040
caused by associated medication (e.g.,
diclofenac), kidney failure. The literature
mentions that approximately 25% of the
patients treated with metformin have at
least one contraindication for this drug,
contraindication that may favor the occur-
rence and even worsen the evolution of a
lactic acidosis case (13, 20). This compli-
cation may occur both in case of metformin
overdose and during chronic treatment with
normal therapeutic doses. No correlations
were found between metformin plasma
levels and the severity of lactic acidosis
poisoning (20). This supports the im-
portance of associated pathology and clear
contraindications in the administration of
metformin.
It is known that tissue hypoxia and kid-
ney disease are common factors for lactic
acidosis. Moreover, patients suffering from
diabetes may have an ineffective glycemic
control with high levels of glycated hemo-
globin which causes kidney damage due to
diabetic nephropathy. Thus, attempting an
effective metformin treatment in the pres-
ence of early chronic complications of
diabetes can have serious consequences.
According to studies, even with prompt
intervention, the mortality rate of lactic
acidosis ranges between 60% and 90%
(11).
Some studies have even pointed out a
biological explanation for metformin-
associated lactic acidosis. The genetic
changes that may occur in the OCT1 pro-
tein may affect the pharmacokinetics of
metformin. OCT1 or the organic anion
transporter 1 facilitates the hepatic uptake
of metformin and a single polymorphic
nucleotide of OCT1 may be associated with
increased intracellular levels of metformin,
and therefore an increased risk of develop-
ing metabolic acidosis at therapeutical
plasmatic concentrations (14).
Intervention regimens for metformin as-
sociated lactic acidosis include the intrave-
nous administration of sodium bicarbonate.
It aims to correct acidosis and restore fluid
and electrolyte balance, but sodium bicar-
bonate can present some disadvantages: the
occurrence of hypervolemia caused by
sodium, the aggravation of intracellular
acidosis, and the decomposition of oxy
hemoglobin.
Hemodialysis is another treatment used
in metformin-associated lactic acidosis, but
since metformin has a large volume of
distribution, hemodialysis only removes a
small amount of the drug; this therapeutic
approach is effective especially when cor-
recting the serious effects associated with
acidosis. When initiating hemodialysis a
rebound effect was observed. Metformin is
stored in the intestine and erythrocytes and
produces and increases the serum lactate
concentration. Continued hemodialysis is
recommended when subsequently serum
lactate levels normalize and lactic acidosis
is corrected.
Metformin itself does not cause hypo-
glycemia but the treatment plan typically
includes an antidiabetic sulfonylurea. The
situations in which metformin alone can
cause hypoglycemia are: fasting, sustained
physical exercise, kidney failure. Hypogly-
cemia may occur under these conditions
and can be corrected by administering in-
travenous glucose. However, some authors
assert that the administration of glucose
may worsen lactic acidosis because intra-
cellular glucose metabolism is directed
towards the formation of lactate.
In addition, it was found that insulin has
beneficial effects in metformin-associated
lactic acidosis, but blood glucose levels
should be monitored closely (17).
Metformin induced lactic acidosis – particularities and course
1041
Impaired vision in metformin therapy is
also very rare, but reversible by optimal
intervention. It is explained by the occur-
rence of metformin-associated lactic acido-
sis, which causes damage to retinal cells,
whose function may be pH dependent (15).
Blood pH adjustment resulted in the re-
sumption of normal function and return of
normal vision.
Hypothermia is another symptom seen
in metformin-associated lactic acidosis and
it is also reversible. It is probably related to
severe hypoglycemia and an acid-base
imbalance in the blood.
It must be pointed out that according to
studies metformin-associated lactic acido-
sis is rare, with a frequency of 1 to 9 pa-
tients per 100,000 people (6). If with
chronic metformin administration lactic
acidosis is an exceptional phenomenon, its
occurrence being attributed especially to
present co morbidities, in the cases of acci-
dental or suicidal metformin overdoses,
lactic acidosis is very likely to occur, and
the state of the patient and the severity of
poisoning are differentiated on a case to
case basis.
The minimum diagnostic tests in case of
metformin overdose include the determina-
tion of serum electrolytes, serum bicar-
bonate, renal function tests, arterial blood
gas test to determine pH, and determination
of blood glucose and serum lactate. Fur-
thermore, all patients with acidosis should
be tested for possible salicylates intoxica-
tion, to exclude this variant (6).
In conclusion, the phenomenon of lactic
acidosis may be associated with metformin
administration, but there are a variety of
special conditions that have an influence on
its occurrence and outcome. Thus, we can
conclude that there is no correlation be-
tween the amount of ingested metformin,
plasma metformin and lactate levels, and
the degree of patient impairment and out-
come.
REFERENCES
1. Roglic G, Unwin N. Mortality attributable to diabetes: Estimates for the year 2010. Diabetes Res Clin
Pract 2010; 87: 15-19.
2. ***, http://www.news-medical.net/health/Metformin-History.aspx.
3. Perrone J, Phillips C, Gaieski D. Occult metformin toxicity in three pacients with profound lactic
acidosis. J Emerg Med 2011; 40(3): 271-275.
4. Mahmood K, Naeem M, Rahimnajjad NA. Metformin: The hidden chronicles of a magic drug. Eur J
Intern Med 2013; 24: 20-26.
5. Mahajan R, Gupta K. Revisiting Metformin: Annual Vitamin B12 Supplementation may become
Mandatory with Long-Term Metformin Use. J Young Pharm 2010; 2(4): 428-429.
6. Dell'Aglio D, Perino L, Todino J, Algren A, Morgan B. Metformin overdose with a resultant serum
pH of 6.59: Survival without sequalaee. J Emerg Med 2010; 39: 77-80.
7. Carrillo-Lopez H, Chavez H, Jarillo-Quijada A. Acid-Base Balance and Disorders. In: Fuhrman B
editor. Pediatric Critical Care. Philadelphia: Elsevier, 2011, 963-977.
8. Lin YC, Lin LY, Wang HF, Lin HD. Fasting Plasma Lactate Concentrations in Ambulatory Elderly
Pacients With Type 2 Diabetes Receiving Metformin Therapy: A Retrospective Cross-sectional
Study. J Chin Med Assoc 2010; 73(12): 617-622.
9. Scheen AJ, Paquot N. Metformin revisited: A critical review of the benefit-risk balance in at-risk
patients with type 2 diabetes. Diabetes Metab 2013; 39: 179-190.
Anca-Monica Strugaru et al.
1042
10. Dart R (editor). Medical Toxicology. New York: Lippincott Williams & Wilkins, 2003.
11. Saidi H, Mani M. Severe metabolic acidosis secondary to coadministration of creatine and metformin,
a case report. Am J Emerg Med 2010; 28: 388.e5-388.e6.
12. Van Velzen A, van Riel A, de Vries I, Meulenbelt J. The dangers of metformin: Fatal lactic acidosis
with therapeutic use due tot renal failure. Toxicol Lett 180S 2008; S32-S246: C57.
13. Yang PW, Lin KH, Lo SH, Wang LM, Lin HD. Successful Treatment of Severe Lactic Acidosis
Caused by a Suicide Attempt with a Metformin Overdose. Kaohsiung J Med Sci 2009; 25(2): 93-97.
14. Van Sloten TT, Pijpers E, Stehouwer CDA, Browers MCGJ. Metformin-associated lactic acidosis in a
pacient with normal kidney function. Diabetes Res Clin Pract 2012; 96: e57-e58.
15. Kreshak A, Clark R. Transient vision loss in a pacient with metformin-associated lactic acidosis. Am J
Emerg Med 2010; 28: 1059.e5-1059.e7.
16. Akoglu H, Akan B, Piskinpasa S et al. Metformin-associated lactic acidosis treated with prolonged
hemodialysis. American J Emerg Med 2011; 29: 575.e3-575.e5.
17. Brouwers MCGJ, Schaper N, Keeris L. Does glucose infusion exacerbate metformin-associated lac-
tate acidosis? A case report. Diabetes Res Clin Pract 2009; 85: e1-e3.
18. Al-Makadma Y, Riad T. Successful management of high-dose metformin intoxication. Role of vaso-
presin in the management of severe lactic acidosis. M. E. J. Anesth 2010; 20 (6): 873-875.
19. Kim E, Choi S, Kim OJ, Kim KH. Treatment of lactic acidosis due to metformin overdose: A case
report. Abstracts / Toxicology Letters 180S 2008; S32–S246: A14.
20. Locatelli CA, Vecchio S, Petrolini et al. Metformin-related lactic acidosis: A case series. Toxicol Lett
196S 2010; S37-S351: P105-031.
INHALED CORTICOSTEROIDS AND PNEUMONIA
Inhaled corticosteroids (ICS) are used for treatment of chronic bronchitis, emphysema and
asthma. But prolonged treatment increases the risk of associated pathologies: vitamin D de-
ficiency, bone fractures, type 2 diabetes and pneumonia. A study, conducted by Dean Eurich
and colleges during 5 year, has showed an increased risk of recurrent pneumonia for elderly
patients which used ICS in the treatment of chronic obstructive pulmonary disease. The
study has included 653 recurrent pneumonia cases and 6244 controls and show that 14% of
current ICS users had developed recurrent pneumonia compared to 9% never -users. These
findings suggest that ICS use increases the risk of recurrent pneumonia with 90% for the pa-
tients who survived after an initial episode of pneumonia. These data are useful in establish-
ing optimal regimens, depending on patient characteristics (Eurich DT, Lee C, Marrie TJ et
al. Inhaled Corticosteroids and Risk of Recurrent Pneumonia: A Population-Based, Nested
Case-Control Study. Clinical Infectious Diseases, 2013; DOI: 10.1093/cid/cit472).
Cătălina Luncă
NEWS