Persistent headache and migraine Dr Salwa Kamourieh MBBS ...
Transcript of Persistent headache and migraine Dr Salwa Kamourieh MBBS ...

Persistent headache and migraine
Dr Salwa Kamourieh MBBS PhD MRCPUCL Queen Square Institute of Neurology &
The National Hospital for Neurology and NeurosurgeryLondon, UK
With thanks to Dr Manjit Matharu

Participation in advisory boards and funding for educational sessions from:
• Lundbeck
• London Metropolitan Medical
Disclosure Statement

• One of the commonest symptoms that clinicians evaluate̶ General Practice: 4.44 consultations/100 registered patients̶ Neurology: 20-25% of referrals
• One-year prevalence of headache disorders is 50%:
• Headache is highly disabling– Migraine is one of the 20 most common causes of years of life lived with disability– 100000 are absent from work or school everyday, contributing to 25 million lost work or school days
every year
Headache: A Common and Disabling Problem
18%
41%
5%6%
40%
3%
0%
10%
20%
30%
40%
50%
Episodic Migraine Episodic Tension-TypeHeadache
Chronic Daily Headache
FemaleMale

Headache: A Misdiagnosed and Undertreated Problem
• The American Migraine Prevalence and Prevention (AMPP) Study ̶ Surveyed 120,000 households̶ Only 52% of those meeting criteria for migraine had been diagnosed̶ Only 12% of patients were on preventative treatment for migraine
• Effective treatment is often possible but depends on correct diagnosis• Headache disorders have a large differential diagnosis (>300 causes) so need to
be approached systematically

International Classification of Headache Disorders (ICHD 3)
Part I: Primary Headache Syndromes Part II: The Secondary Headaches1. Migraine2. Tension-type headache3. Trigeminal autonomic cephalalgias
• Cluster headache• Paroxysmal hemicrania• Short-lasting unilateral headache attacks• Hemicrania continua
4. Other primary headaches
5. Head and/or neck trauma6. Cranial or cervical vascular disorder7. Non-vascular intracranial disorder8. Substance use or its withdrawal9. Infection10. Disorder of homoeostasis11. Headache or facial pain attributed to disorder of
cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures
12. Psychiatric cause
Part III: The Cranial Neuralgias
Provides a framework for headache diagnosis
Primary
Secondary

Secondarycauses ruled out
Primary headachedisorders
Long-lasting headacheDuration >4 hours
Migraine
Tension-type headache
New dailypersistent headache
Hemicraniacontinua
Short-lasting headacheDuration <4 hours
Other primaryheadache
With or withoutmedication overuse
Trigeminal autonomic Cephalalgia
Cluster headache
Paroxysmal hemicrania
SUNCT
Stabbing headache
Cough headache
Exertional headache
Sex headache
Hypnic headache
Nummular Headache
Primary thunderclap headache
Cold stimulusheadache
External pressureheadache
Clinical Approach to Headache

Prevalence of headaches in hypermobile disorders• “Of all the complications that may arise in JHS, chronic pain is arguably the most menacing and difficult
to treat.” Rodney Grahame (1)
• Sparce literature with several limitations:• Case definitions of JHS/EDS/BJH variable• International Classification of Headache Disorders (ICHD) diagnostic criteria generally not utilised• Small series, often poorly controlled
• 51 EDS patients (13 classic type, 28 EDS-HT, 1 with JHS, 7 vascular type, 2 unclassified type) showed that headache and neck pain is present in 30-40% of cases. (2)
• 28 JHS female patients and 232 matched controls: prevalence of migraine 75% in JHS, 43% in controls (OR 3.19) (3)
• 170 JHS female patients and 50 female hospital staff (controls): prevalence of migraine 40% in JHS, 20% in controls (4)
(1) Grahame R. Curr Pain Headache Rep. 2009;13(6):427-33.(2) Sacheti A, et al J Pain Symptom Manage 1997;14:88-93.(3) Bendik EM, et al. Cephalalgia 2011;31:603-613.(4) Hakim AJ, Grahame R. Rheumatology (Oxford). 2004;43(9):1194-5.

• Primary headache syndromes• Migraine• New daily persistent headache
(NDPH)• Tension-type headache
• Orthostatic Headaches• Spontaneous intracranial hypotension• Headache secondary to Postural
tachycardia syndrome (PoTS)
• Headaches due to structural disorders• Temporomandibular dysfunction• Cervicogenic headache • Chiari malformations• Craniocervical instability• Trigeminal neuralgia• Neck-tongue syndrome• Cervical artery dissection
Causes of headache disorders in hypermobile syndromes.

MigraineICHD-III Diagnostic criteria: 1• Episodic attacks of headache lasting 4-72 hours with the following features:
• Further sub-classified on basis of aura and frequency of headaches• Headaches ≤15 days/month: episodic migraine• Headaches ≥15 days/month: chronic migraine
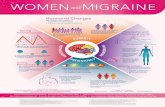
• Overall prevalence of migraine: 12-15%• Chronic migraine: 0.9-2.2%
Headache has at least two of the following characteristics:n Unilateral locationn Pulsating qualityn Moderate or severe pain intensityn Aggravation by routine physical activity
During headache at least one of the following:n Nausea and/or vomitingn Photophobia and phonophobia
ICHD = International Classification of Headache Disorders1. Headache Classification Subcommittee of The International Headache Society. The International Classification of Headache Disorders 3rd edition. Cephalalgia. 2018;38:1-211.

Migraine – a polyphasic brain disorder• A complex clinical syndrome characterised by headache with specific features and associated symptoms
StructuralFunctional
BehaviouralEnvironmental
Adapted from Blau JN. Lancet 1992; 339: 1202–7

TGVS=trigemino-vascular system.Adapted from Pietrobon D, Striessnig J. Nat Rev Neurosci. 2003;4:386-398.
VasodilationNeurogenic
Inflammation
HeadachePain
Abnormal cortical activity
Hyperexcitable brain (Ca++, Glu, ¯Mg++)
Cortical Spreading Depression
Activation/Sensitization of TGVS
Abnormal brain stem function
Excitation of brain stem, PAG, etc.
Central Sensitization
Pathophysiology of Migraine
Matharu et al, Brain 2004Hadjikhani et al, PNAS 2001

Multifaceted Approach to Management of Migraine
Headache Management
Education and Support
Lifestyle modification and
trigger management
Pharmacological Treatments
Psychological and behavioural
treatments
Surgical treatments

Pharmacological treatments
Lifestyle Pharmacological therapy
Acute/abortive
Long term preventative
Offer combination therapyTriptan + NSAID / Paracetamol
NSAID/ Paracetamol + antisickness
• Paracetamol• NSAIDs (high dose & soluble)• Prokinetics (Domperidone/ Metoclopramide)• Triptans
• >5 days/month • “low and slow”• Aim for optimum dose/time• Can take 2-12 weeks• If effective 6-12 months
Opiate-based and mixed analgesics should be avoided.

Non-specific Treatments• Paracetamol 1g• NSAIDs (high-dose & soluble):
• Aspirin 600-900mgs• Ibuprofen 600-800mgs• Naproxen 500-1000mgs• Tolfenamic acid 200mgs
• +/- Anti-emetics:• Domperidone 10mgs• Metoclopramide 10mgs• Ondansetron 4mg• Prochlorperazine 5mg
Specific Treatments• Ergot derivatives
• Ergotamine 1-2mg tablets/suppository• Dihydroergotamine
• Triptans (5-HT1B/D) • Sumatriptan• Rizatriptan• Zolmitriptan• Almotriptan• Eletriptan• Naratriptan• Frovatriptan
• Ditans (5-HT1F receptor agonists)• Lasmiditan
• Gepants (CGRP receptor antagonists)• Rimagepant• Ubrogepant
• Neuromodulation• Remote Electrical Neuromodulation (REN) • Transcranial magnetic stimulation
Abortive Treatments in Migraine

NICE Headache Guidelines: Abortive Treatments of Migraine• Offer combination therapy for the acute treatment of migraine with:
• an oral triptan and an NSAID, or • an oral triptan and paracetamol
• For people who prefer to take only one drug, consider monotherapy with an oral triptan, NSAID, aspirin (900 mg) or paracetamol for the acute treatment of migraine
• Consider an anti-emetic in addition to other acute treatment for migraine even in the absence of nausea and vomiting.
• Do not offer ergots or opioids for the acute treatment of migraine.
• Contraindications to triptans include ischaemic heart disease, cerebrovascular disease, previous myocardial infarction, and uncontrolled or severe hypertension.
• The cardiovascular risk of triptans is very low in the absence of these contra-indications.
http://guidance.nice.org.uk/CG150

NICE Headache Guideline: Prophylactic Treatments of Migraine
• Offer Topiramate or propranolol
• If both Topiramate and propranolol are unsuitable or ineffective, consider:• Acupuncture • Amitriptyline
• Riboflavin (400 mg once a day)
• Botulinum toxin type A is recommended for the prophylaxis of chronic migraine:• that has not responded to at least three prior pharmacological prophylaxis therapies and• whose condition is appropriately managed for medication overuse
• Fremanezumab (Ajovy) is recommended for the prophylaxis of chronic migraine:• that has not responded to at least three prior pharmacological prophylaxis therapies
http://guidance.nice.org.uk/CG150 http://guidance.nice.org.uk/TA260

• Antidepressants• TCAs: Amitriptyline• SNRIs: Venlafaxine, Duloxetine
• Beta-blockers• Propranolol.
• Serotonin antagonists• Pizotifen
• Anticonvulsants• Topiramate, Valproate
• Ca Channel blockers• Flunarizine
• Angiotensin-based• Candesartan, Lisinopril
• Neutriceuticals (metabolic)• Magnesium, Riboflavin, CoEnzyme Q10
• Injectable treatments• Botulinum toxin type A (chronic migraine)
Preventive Treatments in Migraine: The Future• CGRP receptor antagonists
• Atogepant
• CGRP monoclonal antibodies• Erenumab• Fremanuzemab• Galcanezumab• Eptinezumab
• Neuromodulation• Supraorbital nerve stimulation• Occipital nerve stimulation

Migraine in hypermobile syndromes • Comparison of headache in JHS and controls (1)
• Migraine presentation in hypermobile syndromes is more florid, frequent (1.7 fold) and disabling compared (3 fold) to non-hypermobile patients.
• Medication overuse headache likely to be a contributor in patients suffering from recurrent/chronic musculoskeletal pain
• Management of migraine in HSD/hEDS:• Preventive treatments: avoid antihypertensives (Betablockers/Candesartan)• Acute treatments: medication overuse headache can be challenging to address
Headache characteristic JHS (n=28) Controls (n=232) P valueMigraine
Migraine without auraMigraine with aura
75%90%43%
43%91%24%
<0.01
Mean headache frequency days/month (SD) 10.5 (9.5) 5.6 (7.9) 0.01
Mean MIDAS score 36.6 (30.3) 9.3 (16.2) <0.01Medication use n(%)
Preventive treatmentsAbortive treatments
71%82%
44%82%
<0.010.97
(1) Bendik EM, et al. Cephalalgia 2011;31:603-613.

Migraine
• Lasts 4-72 hrs• >2 of the following 4:
– Unilateral– Throbbing– Moderate or severe intensity– Aggravation by movement
• >1 of the following:– Nausea and/or vomiting– Photophobia and phonophobia
Tension-type Headache
• Lasts 30mins-7days• >2 of the following 4:
– Bilateral– Not throbbing– Mild or moderate– Not aggravated by movement
• Both of the following:– No nausea or vomiting– One or neither of photophobia or
phonophobia
ICHD = International Classification of Headache Disorders1. Headache Classification Committee; Olesen J, et al. The International Classification of Headache Disorders: 3rd Edition Celphalalgia 2013.
Tension-type headache is a featureless headache
What is Tension-type Headache?

ICHD-III Diagnostic criteria: 1
• Lasts 30mins-7days• >2 of the following 4:
– Bilateral– Not throbbing– Mild or moderate– Not aggravated by movement
• Both of the following:– No nausea or vomiting– One or neither of photophobia or phonophobia
TTH in Hypermobile Disorders
• Overall prevalence of TTH: 40%• TTH shows no increased prevalence in cases
compared to controls 2
Management
• Abortive Treatments– Simple analgesics (Paracetamol, Aspirin, NSAIDs)– Combination analgesics, Triptans, Opiates and
muscle relaxants should not be used
• Preventive Treatments– Amitriptyline*
• Non-Pharmacological Treatments– Acupuncture*– Cognitive behavioural therapy*– Relaxation training– EMG feedback
Tension-type Headache (TTH)
ICHD = International Classification of Headache Disorders1. Headache Classification Subcommittee of The International Headache Society. The International Classification of Headache Disorders 3rd edition. Cephalalgia. 2018;38:1-211.2. Bendik EM, et al. Cephalalgia 2011;31:603-613.

• Epidemiology 2• Rare; 1-yr prevalence 0.03-0.1%• Female: Male ratio 1.3-2.5:1
• ICHD Criteria 1• Distinct and clearly remembered onset, with pain becoming continuous and unremitting within 24 hours• Lasts more than three months.
• Causes 2• Primary (30%)• Secondary (70%)• CSF pressure disorders: Low/elevated CSF pressure headache• Infections (32%): Chronic meningitis, Sphenoidal sinusitis• Vascular disorders: Cerebral venous thrombosis, Carotid or vertebral artery dissection, Temporal arteritis• Leptomeningeal metastasis• Stressful life event (28%)
New Daily Persistent Headache
ICHD = International Classification of Headache Disorders1. Headache Classification Subcommittee of The International Headache Society. The International Classification
of Headache Disorders 3rd edition. Cephalalgia. 2018;38:1-211.2. Yamani N, Olesen J. J Headache Pain. 2019;20(1):80.

• Investigations• MRI brain (with contrast) and MRV• Lumbar puncture• Further investigations guided by clinical picture
• Management of Primary variant• Depends of clinical phenotype
• Migraine phenotype: migraine treatments• TTH phenotype: TTH treatments
– Generally refractory to medical treatments
New Daily Persistent Headache
ICHD = International Classification of Headache Disorders1. Headache Classification Subcommittee of The International Headache Society. The International Classification
of Headache Disorders 3rd edition. Cephalalgia. 2018;38:1-211.2. Yamani N, Olesen J. J Headache Pain. 2019;20(1):80.

NDPH and Cervical spine hypermobility 1
• 12 patients assessed for joint hypermobility
• 10 met criteria for benign joint hypermobility (Beighton score ≥ 4/9)
• 11 had cervical spine hypermobility
• NDPH by activating cervical afferents (particularly C1-C3 nerves) that converged on the spinal nucleus of the trigeminal nerve, producing both neck pain and headaches.
NDPH and pro-inflammatory cytokines 2
• In 19 out of 20 NDPH patients, TNF-α levels were high in CSF samples with normal serum levels.
• Pain might be due to chronic central nervous system inflammation, cytokine production and persistent glial activation that arise in response to precipitating events
New daily persistent headache (NDPH) in hypermobile disorders
(1) Rozen TD, Roth JM, Denenberg N. Cephalalgia. 2006;26(10):1182-5.(2) Rozen T, Swidan SZ. Headache. 2007;47(7):1050-5.

Comorbid disorders impacting on Headache disorders.• Anxiety disorders
• Anxiety in 32% of JHS patients as compared to 12% within a control population.1
• Sleep disorders• Periodic limb movements are found in 67% of adults with EDS compared to 8% in controls 2
• Sleep disturbances including sleep apnoea, restless leg syndrome, and snoring frequently co-occur in patients with migraine and other headache disorders
• Mast cell activation syndrome (MCAS)• 24-66% of EDS patients have MCAS/histamine sensitivity 3,4
• Histamine is potent trigger for headaches
• Medication overuse headache 5• Develops through chronic overuse of acute medication taken to treat headache or other pain
1) Hakim AJ, Grahame R. Rheumatology (Oxford). 2004;43(9):1194-5.2) Verbraecken J et al. Clin Genet. 2001;60(5):360-5.3) Song B, et al. Proc (Bayl Univ Med Cent). 2020;34(1):49-53.4) Cheung I, Vadas P.J Allergy Clinical Immunol. 2015;135(2)5) Headache Classification Subcommittee of The International Headache Society. The International Classification of Headache Disorders 3rd edition. Cephalalgia. 2018;38:1-211

Why are primary headache disorders over-represented in hypermobile syndromes?• Abnormal vascular endothelial function
• Showering of the cerebral vasculature with atheroemboli, which might trigger attacks of aura in these patients. (1)
• Dysautonomia• Khurana and Eisenburg found that 23 of 24 patients (96%) with POTS had a diagnosis of migraine or probable migraine.
(2)• Kanjwal et al. demonstrated that migraine occurred in 73% of patients with both JHS and POTS as compared to 23% of
those with POTS but without JHS (P<0.001). (3)
• Pro-inflammatory cytokines • Pain might be due to chronic central nervous system inflammation, cytokine production and persistent glial activation
that arise in response to precipitating events (4)
• Centrally mediated pain neuromatrix dysregulation• Altered modulation of pain in JHS patients with fibromyalgia may lower the threshold for primary headache syndromes
and other pain syndromes. (1) Martin VT, Neilson D. Headache. 2014;54(8):1403-11.(2) Khurana RK et al. Cephalalgia. 2011;31(4):409-15.(3) Kanjwal K et al. Indian Pacing Electrophysiol J. 2010;10(4):173-8.(4) Rozen T, Swidan SZ. Headache. 2007;47(7):1050-5.

• According to the World Heath Organisation:
• In the Global Burden of Disease Study, updated in 2013, migraine on its own was found to be the sixth highest cause worldwide of years lost due to disability (YLD).
• Headache disorders collectively were third highest.
• Impose a recognizable burden on sufferers including sometimes substantial personal suffering, impaired quality of life and financial cost. Repeated headache attacks, and often the constant fear of the next one, damage family life, social life and employment.
• The long-term effort of a chronic headache disorder may predispose to other illnesses. For example, anxiety and depression are significantly more common in people with migraine than in healthy individuals.
• In the United States of America and the United Kingdom, only half of those identified with migraine had seen a doctor for headache-related reasons in the previous 12 months, and only two-thirds had been correctly diagnosed. Most were solely reliant on over-the-counter medications.
• Appropriate treatment of headache disorders requires training of health professionals, accurate diagnosis and recognition of the conditions, appropriate treatment with cost-effective medications, simple lifestyle modifications, and patient education.
Not only is headache painful, but it is also disabling
https://www.who.int/news-room/fact-sheets/detail/headache-disorders

• Lack of knowledge among health-care providers is the principal clinical barrier.• Undergraduate medical education • Worldwide only 40% of those with migraine or TTH are professionally diagnosed
• Poor awareness extends to the general public.• Headache disorders are not perceived by the public as serious since they are mostly episodic, do not cause
death, and are not contagious. • Are people aware of treatments out there
• Many governments, seeking to constrain health-care costs, do not acknowledge the substantial burden of headache on society.• Direct costs of treating headache are small in comparison with the huge indirect-cost savings that might be
made (eg, by reducing lost working days) if resources were allocated
Barriers to effective care
https://www.who.int/news-room/fact-sheets/detail/headache-disorders

Headache in EDS and HSD• Headaches are common in Hypermobile Disorders (particularly Hypermobile Spectrum Disorder/Ehlers
Danlos Syndrome)
• There is large differential diagnosis for headaches in hypermobile disorders.
• Individual EDS/HSD patients often have multiple causes for headaches.
• Clinicians looking after these patients need to carefully assess for the various potential causes of headaches and implement appropriate management strategies.
• Pathophysiology of headaches and non-headache manifestations is often interrelated
• A multidisciplinary approach is ideally required as the multisystem involvement often impacts on headaches
• More research needs to be done regarding the interrelationships between hypermobile disorder and headache/neck pain as this may represent a subgroup of patients with a different pathogenesis and treatment.

Thank you