Percutaneously adjustable pulmonary artery band
-
Upload
ali-ahmadi -
Category
Documents
-
view
215 -
download
0
Transcript of Percutaneously adjustable pulmonary artery band

PERIOPERATIVE MANAGEMENT -
Percutaneously Adjustable Pulmonary Artery Band Ali Ahmadi, MD, Joachim Rein, MD, Klaus Hellberg, MD, and Christian Bastanier, MD Department ot Cardiovascular Surgerv, Robert-Bosch Hospital, SATA Clinic of Cardiovascular Surgery, and Department of Pe&atric Cardiology, Stuttgart, Germany
Background. Pulmonary artery banding, originally in- troduced to palliate increased pulmonary blood flow, is now primarily used for complex congenital cardiac de- fects with a prohibitive risk in the early repair, such as tricuspid atresia, or occasionally to prepare the left ven- tricle for eventual arterial switch. Conventional banding is, however, often poorly tolerated, and the precise ad- justment required to reduce pulmonary blood flow or sufficiently challenge the left ventricle is difficult and can cause life-threatening hemodynamic changes.
Methods. We designed a band that allows accurate tightening and is reversible during the operation and at the bedside with the chest closed, allowing precise grad- ual adjustment over days, thereby minimizing cardiovas-
I? ulmonary artery banding has been proposed as a
preliminary procedure either to reduce pulmonary artery pressure, such as in patients requiring an eventual Fontan procedure, or to prepare the left ventricle for a future arterial switch in neonates older than 4 weeks with transposition of the great arteries and intact ventricular septum [l-3]. However, not only are the acute hemody- namic changes induced by effective banding only poorlv tolerated, but the dynamic postoperative respiratory and circulatory changes can often cause changes to the gra- dient across the band, necessitating later readjustment 141. There exists ample experimental evidence that slog progressive tightening of a pulmonary artery band is well tolerated [5]. Several techniques have been proposed to constrict the pulmonary arterv percutaneously over time, and various methods have betn tried in selecied cases [3, 4, 6-81.
We have developed a percutaneously adjustable band that allows extremely precise adjustment, which is also reversible. This device was tested in an animal model [Y, lo] and subsequently applied clinically in a patient. The design of this device and a description of the patient form the subject of this report.
Description of the Device and Technique
The device consists essentiallv ot a circular band covered by a synthetic cuff (Figs 1, 2):Adjustment is achieved bq means of a screw contained within a cylindrical body. One end of the band is threaded, and a connecting piece
cular instability. This design is the extension of previous work done by one of us on an adjustable annuloplasty ring.
Results. The band has been used for a 16-month-old child with tricuspid atresia type 1C who had undergone two failed attempts at banding. Hemodynamic measure- ments after 3 months confirmed achievement of the desired pulmonary pressure.
Conclusions. This design, the simple insertion, and the ability to finely readjust the banding over days, com- bined with excellent patient tolerance, encourage further use of our adjustable band.
(Am Thmzs Surg 1995;6O:S520-2)
allows coupling with a flexible tube as a guide. A screw- driver that is also flexible but does not allow torsion is inserted through this guide to engage the screw. This guide exits the chest, and after multiple adjustments have been made it can be unscrewed and removed in its entirety. The other end of the band, which completes the circle, has a ridge that also engages the thread of the screw, and the screwdriver thus either tightens or broad- ens the circle. Blood flow is thereby regulated by the well-defined principles of Poiseuille’s law. To insert the device the band is opened and the free end fed around the pulmonary trunk. The covering allows this to be done atraumatically. The free end is then inserted into a slit on the adjusting body to complete a ring, and the circum- ference can then be changed by tightening the screw. The toothed portion of the coil then exits progressively from the device when tightened and enters a hollow cylinder, bvhich prevents injury to the surrounding structures.
Case Report
A full-term female infant neonate weighing 2.6 kg was referred to our unit with congestive cardiac failure, neonatal sepsis, renal failure, and necrotizing enteroco- litis. tchocardiographic diagnosis documented addi- tional tricuspid atresia type lC, with both atria1 and ventricular septal defects. The child was intubated from 2 days after birth due to respiratory failure and was still ventilator dependent.
At the age of 3 weeks pulmonary artery banding was performed; the distal pulmonary artery pressure, which equaled systemic pressure, wab reduced to a mean of 20 mm Hg. The child continued to have failure to thrive. Echocardiography performed at 10 months suggested an ineffective banding with questionable constriction of the
0003-4975/95/$9.50 SSDI 0003-4975(95)00771-7

Ann Thorac Surg 1995;60:!%2U-2
CASTAtiEDA FESTSCHRIFT AHMADI ET AL S521 ADlUST.ABLE PULMONARY ARTERY BAND
right main pulmonary arter\,. Catheterization confirmed these findings. Pulmonary artery and systemic pressures were identical (75134 mm Hg; mean, 54 mm Hg), and the pulmonary vascular resistance was calculated at 8.6 Wood units. Revision of the banding was carried out. During this second procedure all attempts at reducing mean pulmonary artery pressure to 25 mm Hg or less led to a precipitous drop in the arterial 0, saturation to less than 70%. The band therefore had to be fixed at a mean pulmonary artery pressure of 33 mm Hg. Dissection of the right main pulmonary artery also revealed a mark- edly diminished diameter of the whole right main pul- monan; artery to one third that of the left pulmonarh artery..A lung biopsy was also performed and showed grade I to II arterial changes according to the Heath- Edwards classification.
Due to this unusual situation \ve decided to repeat banding with the percutaneously adjustable band, which was carried out when the infant was at 16 months of age. At operation via median sternotomy, the presenting side of the existing band was transected anteriorlv and one loose end thereof was tied to the free end of ihe adjust- able band, which could then quite easilv and safeI\, be fed around the main pulmonary arterv. ?he mechanism of the band was tested by both tightening and loosening it. The flexible connector M’as then screbved onto the band, and the free end thereof was brought out to exit the anterior chest wall in the third intercostal space paraster- nally, well awav from all vital structures. A catheter wab placed in the main pulmonarv artery to allow me;lhure- ment of pressure downstream to the band, enabling later adjustment under continuous pulmonar\ artem preshure and arterial oxvgen saturation control.
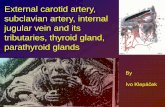
Fig 3. The patient in the intensive care unit with guide still in plac-c,.
During the course of the next 2 days further adjust- ments were made using the pulmonary artery pressure and oxygen saturation as a guide (Fig 3). At the time of extubation, which was successfully performed on the second postoperative day, the distal pulmonary artery pressure had been reduced from 30 to 16 mm Hg and the adjusting mechanism could be removed.
Heart catheterization 3 months after operation con- firmed the findings recorded at the last adjustment, with a distal pulmonary artery pressure of 24/7 mm Hg, a proximal pressure of 93 mm Hg, and a pulmonary vas- cular resistance of 2.6 Wood units. The child is now under consideration for a Fontan procedure (Fig 4).
Comment
Since the original description of pulmonary artery band- ing by Muller and Dammann in 1952, the indications for Ihis intervention have shifted progressively from use in simple cases of left to right shunt, to more complex conditions with a prohibitive risk in the early definitive operation [4].
7’his is particularly pertinent to infants with tricuspid atresia and an increased pulmonary blood flow, as was trut‘ in our case. In these patients the objective is the >ame as originally proposed, namely, to reduce pulmo-

5522 CASTANEDA FESTSCtiRlI-I AHMADI El Al ADJUSTABLE I’ULMOhARY ARTERY BAND
Ann Thorac Surg 1995;6O:S520-2
Fig 4. Angiography showing the main pulmonary artery stenosed by the adjustable band Cleft lateral rGcwJ. The #ding fubc and thy snewdriz~er are already ronoz~i.
nary blood flow and to thereby- protect the pulmonary vasculature against irreversible damage. The procedure is also indicated as a preliminary step toward eventual arterial switch in selected cases of transposition of the great arteries with intact ventricular septum to prime the left ventricle to a state able to sustain the required left-sided pressures eventually. In particular, these com- plex cases tolerate banding poorly [2] as the band is either too loose to achieve a significant reduction in pulmonary blood flow or sufficiently challenge the left ventricle, or conversely too tight, which may precipitate hemodynamic embarrassment incompatible with life.
We believe that this problem is best solved by an adjustable device that allows precise and gradual band- ing of the pulmonary arten/ over some time, which mav be performed at the bedside with a closed chest over h
few days, thereby permitting gradual adjustment to the new demands on the circulation. In the past several such solutions have been proposed and also occasionally ap- plied clinically [3, 4, 6-81.
The accuracy of the adjustment obtainable with this device, both intraoperatively and postoperatjvq with a closed chest, combined with the simplicity with which all parts except the ring itself are removed is anencourage- ment for the continued use thereof in selected cases.
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
IO.
Yacoub MH, Bernard A, Lange I’, et al. Clinical and hemo- dynamic results of the two-stage anatomic correction of simple transposition of the great arteries. Circulation 1980;62 (Suppl l):lYO-6. llbawi MN, Idriss FS, DeLeon SY, et al. Preparation of the left ventricle for anatomical correction in patients with simple transposition of the great arteries: surgical guide- lines. I Thorac Cardiovasc Sure. 1987:94:87-94. Higashidate M, Beppu T, l<ai Y,’ et al. Percutaneously adjustable artery band. J. Thorac Cardiovasc Surg 1989;97: 864-Y. Solis E, Bell D, Alboliras H, et al. Left ventricular preparation with an extrathoracically adjustable balloon occluder. Ann Thorac Surg 1987;44:58-61. Lang PE, Niirnberg JH, Sievers HH, et al. Response of the right ventricle to progressive pressure loading in pigs. Basic Res Cardiol 1985;80:436-44. Shane RA, Kimmel GO, Jaques WE, et al. Adjustable pros- thesis for pulmonary artery banding: comparison with um- bilical tape and Teflon bands. Circulation 1967;35(Suppl 1):148. Park SC, Griffith BP, Siewers RD, et al. A percutaneously adjustable device for banding of the pulmonary trunk. Int J Cardiol 1985;9:477-84. Muraoka R, Yokota M, Aoshima et al. Extrathoracically adjustable pulmonary artery banding. J Thorac Cardiovasc Surg 1983;86:582-6. Ahmadi AA. Entwicklung und experimentelle Untersu- chung einer dynamischen atrio-ventrikulaeren Klappenpro- these zur operativen Behandlung der Mitral- undtikuspidal- insuffizienz. PhD Thesis. Freiburg: University of,F;eiburg i. Br, 1988. , I
Ahmadi AA, Spillner G, Johannesson T. Hemodynamic changes following experimental production and correction of acute mitral regurgitation with an adjustable ring pros- thesis. Thorac Cardiovasc Surg 1988;36:313-7.