Pediatrics in Review 1999 McGowan e6 e15
-
Upload
hirofreeze -
Category
Documents
-
view
8 -
download
1
description
Transcript of Pediatrics in Review 1999 McGowan e6 e15

Neonatal HypoglycemiaJane E. McGowan, MD*
OBJECTIVES
After completing this article, readers should be able to:
1. Describe the most common cause of prolonged neonatalhypoglycemia.
2. List the signs of hypoglycemia.3. Describe the condition that has been implicated as a mechanism of
hypoglycemic brain injury.
Case StudyA term male infant was born afteran uneventful pregnancy to a28-year-old gravida I woman whohad no evidence of hyperglycemiaand no chronic diseases. The infanthad Apgar scores of 7 and 9 at1 and 5 minutes, respectively. Hisgrowth parameters were in the nor-mal range, with weight at the 60thpercentile, head circumference at the50th percentile, and length at the50th percentile. The baby was takento the well baby nursery, examinedand bathed, and then taken to themother for nursing at about 2 hoursof age. He appeared slightly jitteryat that time and was not very inter-ested in nursing or very aware.A blood glucose concentration of1.39 mmol/L (25 mg/dL) wasobtained using a One Touch® instru-ment. The baby was fed 25 mL of5% dextrose in water. The bloodglucose concentration obtained1 hour later was 2.22 mmol/L(40 mg/dL), and the baby nursed forabout 5 minutes at each breast withapparent satisfaction. Jitteriness and“lack of interest” were improved.
Normal nursery routine was fol-lowed, with no comment in the chartby the nursing staff about theinfant’s feeding or behavior until thesecond day of life when he againappeared jittery and fussy. Glucoseconcentration at that time was1.11 mmol/L (20 mg/dL). The infantwas fed by breast or bottle (routine20 kcal/oz house formula) alternat-ing every 2 hours, and clinical signs
improved. One Touch® glucose con-centrations obtained over the next24 hours were variable, but overallthe concentration increased, with apredischarge, preprandial value of2.78 mmol/L (50 mg/dL).
The family failed to return to thehospital clinic the next day, but didsee their primary care physician onthe fifth day of life at which timethe infant acted hungry, was notedto be “very active,” and weighed113.4 g more than birthweight. At2 weeks of life, the parents notedthe infant to be very fussy and jit-tery and to experience staring spells.At a local emergency department, hewas noted to have lost weight,appeared somnolent but fussy whenaroused, and started having tonic-clonic jerking movements of allextremities. A “glucose concentra-tion” was less than 0.55 mmol/L(10 mg/dL). The infant was treatedwith intravenous glucose, and theapparent seizure resolved. Over thenext several weeks, the infantreturned to the emergency depart-ment several times with similarepisodes.
When finally examined by theprimary care physician, the infanthad gained 283.5 g and appeared“puffy.” An “office glucose concen-tration” was 1.94 mmol/L (35 mg/dL). The infant was referred to apediatric endocrinologist, who notedthat the infant’s weight wasapproaching the 90th percentile,there was definite hepatomegaly,and the infant appeared “apathetic.”In the hospital, several serum glu-cose concentrations were measuredat less than 2.22 mmol/L (40 mg/dL), with plasma insulin concentra-tions all greater than 144 pmol/L(20 mcU/mL).
The infant was treated with dia-zoxide with only limited successover the next 3 months. Develop-ment continued but was “slow.” Hewas treated in the local emergencydepartment three times for tonic-clonic seizures, all requiring intrave-nous glucose to correct severe hypo-glycemia. At 5 months of age, theinfant underwent a subtotal pancrea-tectomy. While recovering, he had asevere, prolonged seizure and wasnoted to be in shock, requiring tworounds of resuscitation.Escherichiacoli meningitis was diagnosed andtreated successfully.
At 1 year of age, the infantshowed little developmental gainfrom 6 months of age. At 5 years ofage, he exhibited extremely poorgrowth, had diabetes mellitus thatnecessitated insulin treatment, andrequired pancreatic enzyme replace-ment with feedings to treat malab-sorptive diarrhea. He was almostcompletely deaf and had markeddevelopmental delay. His parentssought legal counsel, claiming thatthe treating physicians in the birthhospital failed to diagnose a “hyper-insulinism” condition that then ledto delayed diagnosis and treatment,followed by severe neurologicdamage.
Questions to consider (feel free tosend in your answers to these ques-tions and any questions of your ownfor the “experts” to consider anddiscuss about this case):
1. What is the likely diagnosisfor this infant’s hypoglycemia?
2. What diagnostic tests couldhave been done in the birth hospitalto determine whether the infant had
*Associate Professor of Pediatrics, MCPHahnemann University and St.Christopher’s Hospital for Children,Philadelphia, PA.
ABBREVIATIONSAGA: appropriate for gestational
ageATP: adenosine 59-triphosphateIDM: infant of a diabetic motherIUGR: intrauterine growth
retardationLGA: large for gestational ageNMDA: N-methyl-D-aspartateSGA: small for gestational age
ARTICLE
e6 NeoReviews July 1999 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

transient or persistenthypoglycemia?
3. What could have been doneprior to discharge from the birthhospital to provide evidence of theinfant’s ability to maintain a normalblood glucose concentration with anormal feeding schedule?
4. What did the pancreaticpathology examination likely showat the time of subtotalpancreatectomy?
5. How would you assess theclinical outcome in relation to theprimary diagnosis and its complica-tions versus theE coli meningitisand shock?
William W. Hay, Jr, MDCoeditor
IntroductionGlucose is the major source ofenergy for organ function. Althoughall organs can use glucose, thehuman brain uses it almost exclu-sively as a substrate for energymetabolism. Because cerebral glyco-gen stores are limited, maintenanceof adequate glucose delivery to thebrain is an essential physiologicfunction. The high brain-to-bodyweight ratio in the newbornresults in a proportionately higherdemand for glucose compared withthe capacity for glucose productionthan that encountered in the adult,with cerebral glucose use accountingfor as much as 90% of total glucoseconsumption. Although alternatefuels, such as lactate and ketonebodies, can be used as a substratefor energy production, the new-born’s immature counterregulatoryresponse limits the availability ofthese molecules. Thus, newborns areextremely susceptible to any condi-tion that impairs the establishmentof normal glucose homeostasis dur-ing the transition from intrauterineto independent extrauterine life.
Glucose Homeostasis inUteroGlucose is one of the major sub-strates for fetal metabolism. Undernormal conditions (ie, normal mater-nal glucose levels), virtually all ofthe glucose used by the fetus is sup-plied from the maternal circulationvia facilitated diffusion across the
placenta. This results in a fetalblood glucose concentration ofapproximately 70% of the maternalvalue. Although the enzymes neces-sary for both gluconeogenesis andglycogenolysis are present in thehuman fetus by the end of the firsttrimester, several studies have dem-onstrated that there is no significantglucose production in the fetusunless there is a sustained decreasein umbilical glucose uptake. Glucoseutilization rates in the fetus havebeen estimated at 4 to 6 mg/kg perminute. Approximately 60% to 70%of fetal glucose utilization isaccounted for by oxidation of glu-cose carbon to CO2, with theremainder available for synthesis ofglycogen and other macromolecules.In the human fetus, oxidation ofglucose accounts for approximately80% of fetal oxygen consumption,demonstrating that glucose is themajor substrate for fetal oxidativemetabolism.
The rate at which the fetus usesglucose is primarily a function ofglucose concentration, althoughchanges in insulin concentrationmay have a modest influence aswell. Studies have demonstrated thatlevels of fetal pancreatic insulinsecretion correlate with changes infetal glucose concentration, but thepancreatic response is blunted com-pared with the newborn or adult.Insulin secretion in response to fetalhyperglycemia increases glucoseutilization and oxidation rates, but ithas little effect on fetal metabolicrate or the rate of oxygen consump-tion, suggesting that oxidation ofother substrates is reduced underthese conditions. Decreased oxida-tion of substrates such as aminoacids and lactate results in increasedavailability of those substrates fortissue accretion and may account inpart for the increased somaticgrowth associated with fetalhyperinsulinemia.
In animal models, administrationof glucagon does not appear to havea direct effect on fetal glucosemetabolism. However, the ratio ofinsulin to glucagon in the fetal cir-culation plays a critical role in regu-lating the balance between glucoseconsumption and energy storage.The high insulin:glucagon ratio inthe fetal circulation results in activa-
tion of glycogen synthesis and sup-pression of glycogenolysis by regu-lating the activity of the hepaticenzymes used for these processes.Predominance of insulin maintainsglycogen synthase in its active formand glycogen phosphorylase in itsinactive form via cAMP-dependenteffects on specific protein kinasesand phophorylases, thus enhancingglycogen synthesis and minimizingglycogenolysis. In most species,including humans, hepatic glycogenstores accumulate slowly duringearly and midgestation, with a rapidincrease in hepatic glycogen contentoccurring during the last 30% offetal life. The marked increase inglycogen synthesis during thisperiod is associated with an increasein circulating concentrations of bothinsulin and cortisol. Because theincrease in cortisol seems to be nec-essary for maximal activation ofglycogen synthase, fetal adrenal dys-function may limit hepatic glycogenaccumulation late in gestation.Under conditions associated withdecreased fetal glucose concentra-tions and increased glucagon secre-tion, such as chronic hypoglycemiaor hypoxemia, glycogen phosphory-lase is activated, and synthase isconverted to its inactive form,thereby suppressing glycogen syn-thesis and stimulating glycogenoly-sis with subsequent depletion offetal glycogen stores. The high insu-lin:glucagon ratio also suppresseslipolysis, which allows for additionalenergy to be stored in the form ofsubcutaneous fat. Thus, the fetalhormonal and metabolic milieuestablishes a ready substrate supplythat can be used during the meta-bolic transition from fetus tonewborn.
Glucose Homeostasis in theNewbornThe relative dependence of the fetuson a constant supply of maternalglucose necessitates significantchanges in regulation of glucosemetabolism at birth following theabrupt interruption of umbilical glu-cose delivery. Although the exacttrigger is unknown, a number ofphysiologic changes equip the new-born for maintenance of glucosehomeostasis. Increased catechol-
ENDOCRINOLOGYHypoglycemia
NeoReviews July 1999 e7 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

amine concentrations immediatelyfollowing delivery stimulate gluca-gon secretion, with a subsequentdecrease in the insulin:glucagonratio. Glycogen synthase is inacti-vated and glycogen phosphorylase isactivated, leading to stimulation ofglycogenolysis and inhibition of gly-cogen synthesis. Release of glucosefrom glycogen provides a rapidlyavailable source of glucose for thenewborn in the first few hours post-partum. However, it has been esti-mated that term infants have onlyenough hepatic glycogen to maintainthe glucose supply for about10 hours. Therefore, other mecha-nisms are required to maintain glu-cose homeostasis. The high gluca-gon:insulin ratio postpartum alsoinduces synthesis of the enzymesrequired for gluconeogenesis. Withthe combination of the release offatty acids stimulated by the highcatecholamine concentrations thatleads to a marked increase in glyc-erol availability and the availabilityof free amino acids in the circula-tion, the infant becomes capable ofsignificant gluconeogenesis by 4 to6 hours of life. However, enzymeactivities do not reach adult levelsuntil 1 to 2 weeks of age.
Basal glucose utilization rates inthe newborn infant are 4 to 6 mg/kgper minute, almost twice the weight-specific rates in adults. During thefirst few hours of life, blood glucoseconcentrations fall from the fetalvalue, which reflects the mother’sblood glucose concentration, to aslow as 1.7 mmol/L (30 mg/dL)before the infant attains the meta-bolic transition to independent glu-cose production and establishespostnatal glucose homeostasis. Untilan exogenous supply of substrate isprovided, either by enteral feedingsor administration of intravenous flu-ids, hepatic glucose output serves asthe most significant source of glu-cose to meet metabolic demands. Tomaintain normal levels of hepaticglucose production, the infant musthave adequate stores of glycogenand gluconeogenic precursors(eg, fatty acids, glycerol, aminoacids, and lactate), appropriate con-centrations of the hepatic enzymesrequired for gluconeogenesis andglycogenolysis, and a normally func-tioning endocrine system. Absence
of any of these requirements leadsto disruption of glucose homeostasis,most commonly resulting in neona-tal hypoglycemia.
Incidence, Diagnosis, andClinical Presentation
INCIDENCE
Estimates of the incidence of hypo-glycemia in the newborn dependboth on the definition of the condi-tion and the methods by whichblood glucose concentrations aremeasured. The overall incidence hasbeen estimated at 1 to 5 per 1,000live births, but it is higher in at-riskpopulations. For example, 8% oflarge-for-gestational-age infants (pri-marily infants of diabetic mothers[IDMs]) and 15% of preterm infantsand infants who have intrauterinegrowth retardation (IUGR) havebeen reported as having hypoglyce-mia; the incidence in the entire pop-ulation of “high-risk” infants may beas high as 30%.
LABORATORY DIAGNOSIS
The concentration of blood glucoseat which the diagnosis of neonatalhypoglycemia should be made hasbeen highly controversial. Hypogly-cemia in term infants has beendefined as a blood glucose value ofless than 2.0 mmol/L (,35 mg/dL)or as a plasma glucose value of lessthan 2.2 mmol/L (,40 mg/dL).However, a recent survey of pedia-tricians in the United Kingdom dem-onstrated no consensus as to thelevel of blood glucose that they con-sidered “hypoglycemia”. They citedconcentrations ranging from1 mmol/L (20 mg/dL) to 4 mmol/L(70 mg/dL) as the lower limit ofnormal. Further, definitions of hypo-glycemia are based primarily onpopulation studies of blood orplasma glucose concentrations dur-ing the first 48 to 72 hours of life,with hypoglycemia being defined asa blood glucose level more than2 standard deviations below the pop-ulation mean. Such definitions haveonly limited physiologicsignificance.
Physiologically, hypoglycemia ispresent when glucose delivery isinadequate to meet glucose demand
and can occur over a range of glu-cose concentrations, depending onthe status of the infant. For example,a 2-hour-old healthy infant who hasa blood glucose of 1.7 mmol/L(30 mg/dL) might not demonstrateimpaired organ function, but astressed infant might demonstratephysiologic hypoglycemia at a bloodglucose concentration of 2.8 mmol/L(50 mg/dL) if the rate of glucosedelivery to specific organs (eg, thebrain) is less than the rate of glu-cose utilization. No studies to datehave established an absolute bloodglucose concentration at whichshort- or long-term organ dysfunc-tion invariably occurs, although ani-mal studies suggest that concentra-tions less than 1 mmol/L (,20 mg/dL), if sustained over a number ofhours, may be associated with inevi-table brain injury. Without specificevidence to support an absolutethreshold value, no single blood glu-cose value can be used to definephysiologic hypoglycemia.
The definition of “normal” bloodglucose concentrations for a givenpopulation of newborns alsodepends on the feeding practices inthat population. For example, themean value for normal blood glu-cose concentrations in term infantsdetermined from studies 30 yearsago was significantly lower thanvalues determined in the past10 years. This is not because of achange in neonatal physiology, butbecause pediatricians no longer fol-low the practice of withholdingfeedings from healthy newborns fora prolonged period after delivery.Rather than reflecting “normal” neo-natal glucose homeostasis, theseearly values demonstrated the effectsof the interference of medical practi-tioners in the normal transition topostnatal metabolism. Similarly,early data that demonstrated lowerblood glucose values in populationsof preterm infants compared withterm infants was interpreted errone-ously to mean that low-birthweightinfants tolerated hypoglycemia betterthan normal-weight neonates. Infact, these data reflected failure ofhepatic glucose production in pre-term infants in response to an inade-quate supply of exogenous substrate.At that time, standard feeding prac-tices had not been established for
ENDOCRINOLOGYHypoglycemia
e8 NeoReviews July 1999 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

this population, and reliable intrave-nous (IV) nutrition was not avail-able. Finally, the time at which theblood glucose concentration is mea-sured affects the value considered“normal”; blood glucose concentra-tions increase over the first 24 to48 hours of life in healthy terminfants, probably as a result of boththe increasing volume of enteralfeeding and initiation of gluconeo-genesis. Thus, a value that would beconsidered “low normal” at 3 hoursof life might be termed “hypoglyce-mic” at 18 hours.
Making a firm diagnosis of hypo-glycemia is complicated further bythe limitations of methods used tomeasure blood glucose concentra-tions rapidly. Although the “goldstandard” remains the hexokinasemethod used by many diagnosticlaboratories, this approach is imprac-tical as a screening tool because ofthe time required to process thesample and to perform the assay.Furthermore, if the sample is nottransported rapidly to the laboratoryand processed quickly, the glucosewill be metabolized by red bloodcells, thereby falsely decreasing theglucose concentration. Placing thespecimen in a tube that contains aglycolytic inhibitor such as sodiumfluoride can prevent this problem,but such tubes are either not readilyavailable or simply not used.
Most nurseries use glucose oxi-dase/peroxidase chromogen teststrips to screen high-risk newbornsfor low blood glucose concentra-tions. A drop of blood placed on thereagent-impregnated paper strip forthe specified time will induce acolor change that correlates withblood glucose concentration. Theactual blood glucose concentrationcan be estimated by comparisonwith a standard chart or determinedmore precisely by “reading” thecolor of the strip with a reflectancecolorimeter that has been calibratedusing a standard solution. Althoughuse of a reflectance colorimeter toread the test strips improves preci-sion, multiple studies comparingvarious methods have found that thecorrelation between “real” bloodglucose values and values obtainedusing test strips remains highly vari-able. This is especially true at lowblood glucose concentrations.
Reagent test strip results also aresusceptible to variations in the tech-nique used to obtain the sample (eg,variability in the amount of bloodapplied to the strip or contaminationof the sample by residual isopropylalcohol on the skin). It has beenestimated that screening withreagent strips will detect approxi-mately 85% of cases of hypoglyce-mia, although the false-positive ratemay be as high as 25%. Thus, toensure accurate detection of lowblood glucose concentrations, a con-firmatory sample should be sent to acentral laboratory if a test stripvalue is consistent with hypoglyce-mia or if the test strip result is inthe normal range but clinical find-ings raise the suspicion ofhypoglycemia.
CLINICAL PRESENTATION
Although hypoglycemia often isclassified as “symptomatic” or“asymptomatic”, these terms actuallyreflect the presence or absence ofphysical signs that accompany a lowblood glucose concentration. A vari-ety of signs may be seen in cases ofsevere or prolonged hypoglycemiaand in infants who have mild-to-moderate hypoglycemia and are oth-erwise physiologically stressed.Most findings are nonspecific andresult from disturbances in one ormore aspects of central nervous sys-tem function. These include abnor-mal respiratory patterns, such astachypnea, apnea, or respiratory dis-tress; cardiovascular signs, such as
tachycardia or bradycardia; and neu-rologic findings, including jitteri-ness, lethargy, weak suck, tempera-ture instability, and seizures. Manyof these signs can result from othercommon neonatal disorders, includ-ing sepsis, hypocalcemia, and intra-cranial hemorrhage. Hypoglycemiaalways must be considered in aninfant who exhibits one or more ofthese signs because untreated hypo-glycemia can have serious conse-quences, and the treatment is fast,relatively easy, and has limited sideeffects. However, given current stan-dards for newborn care, most casesof hypoglycemia in the neonate arediagnosed during routine screeningof infants considered to be at riskbut who appear physiologically nor-mal at the time of evaluation.
Etiology
PREMATURITY AND IUGR
The causes of neonatal hypoglyce-mia can be categorized according toassociated disturbances in one ormore of the processes required fornormal hepatic glucose productionthat may lead to transient or pro-longed episodes of hypoglycemia(Table 1). Hepatic glycogen storesare limited in both preterm infants,who have not experienced the periodof rapid glycogen accumulation dur-ing late gestation, and small-for-gestational age (SGA) infants, whohave not had adequate substrate sup-ply available for glycogen synthesis,
TABLE 1. Etiologies of Neonatal Hypoglycemia
ETIOLOGYDURATION OFHYPOGLYCEMIA
Prematurity, intrauterine growth retardation Transient*
Asphyxia, hypothermia Transient
Sepsis Transient
Infant of diabetic mother Transient
Erythroblastosis fetalis Transient
Exposure to beta-agonist tocolytics Transient
Familial hyperinsulinism Prolonged
Inborn errors of metabolism Prolonged
*Generally <7 d duration.
ENDOCRINOLOGYHypoglycemia
NeoReviews July 1999 e9 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

which puts these newborns at riskfor hypoglycemia. IUGR due to pla-cental insufficiency with preserva-tion of normal head size puts anadded demand on the infant’salready low glycogen stores becauseof the increased brain-to-bodyweightratio. Postterm infants and infants ofmultiple gestations also may be atrisk because of the presence of rela-tive placental insufficiency. In addi-tion to decreased glycogen availabil-ity, studies in preterm and IUGRinfants have found altered patternsof insulin secretion, substrate metab-olism, and hormonal responses tochanges in blood glucose concentra-tion compared with appropriate-for-gestational age (AGA) term infants.
Infants who have experiencedperinatal stress due to asphyxia orhypothermia or who have increasedwork of breathing due to respiratorydistress may have “normal” glyco-gen stores, but the amount of glyco-gen available may be inadequate tomeet their increased requirement dueto higher-than-normal levels of glu-cose utilization. Hypoglycemia mayoccur in these infants once availableglycogen has been used to meet theinitial postnatal metabolic demands,particularly if there has been aperiod of hypoxemia with associatedrapid consumption of glucose viaanaerobic metabolism.
It is uncommon for inadequatelevels of gluconeogenic precursorsto be a limiting factor in hepaticglucose production in the newbornbecause even preterm infants appearto have sufficient fatty acids, glyc-erol, amino acids, lactate, and pyru-vate available. However, gluconeo-genic enzymes are induced moreslowly in preterm infants. Further,production of ketone bodies is rela-tively diminished in response tohypoglycemia. Term infants mayhave augmented release of ketonebodies when blood glucosedecreases, but the concentrations ofketones correlate poorly with thedegree of hypoglycemia. As a result,the contribution of gluconeogenesisto hepatic glucose production maybe limited in some newborns.
IDMS
Several groups of infants are atincreased risk for hypoglycemia due
to alterations in hepatic enzymefunctions that impair glycogenolysis,gluconeogenesis, or both. Hepaticfunction can be affected by a num-ber of endocrine and metabolic dis-turbances, the most common beinghyperinsulinism. IDMs may haveincreased secretion of pancreaticinsulin because of exposure toincreased maternal glucose concen-trations in utero. Placental glucosetransport is increased, leading tofetal hyperglycemia, which in turnstimulates secretion of insulin by thefetal pancreas. IDMs also haveexaggerated pancreatic insulin secre-tion in response to a given glucoseload compared with nonIDMs. Otherdiabetes-induced alterations inmaternal metabolism, such aschanges in serum amino acids, mayplay a role in the metabolic alter-ations found in IDMs.
After delivery, increased bloodglucose concentrations no longer arepresent, but the hyperinsulinemiapersists, thus maintaining a highinsulin:glucagon ratio postnatally.As a result, glycogenolysis andlipolysis are inhibited, gluconeo-genic enzymes are not induced, andhepatic glucose production remainsat low levels in the face of decreas-ing blood glucose concentrations.Insulin also increases peripheral glu-cose utilization in insulin-sensitivetissues such as skeletal muscle, con-tributing to rapid depletion of avail-able glucose. The combined effectsof increased glucose utilization andinhibited hepatic glucose productionresult in hypoglycemia, which maypersist for 24 to 72 hours beforeinsulin secretion patterns normalize.
ERYTHROBLASTOSIS FETALISAND BETA-AGONIST TOCOLYTICAGENTS
Although maternal diabetes is themost common cause of hyperinsulin-ism in the newborn, postnatal insulinsecretion may be abnormal due toseveral other disorders. Infants whohave erythroblastosis fetalis haveincreased levels of insulin and anincrease in the number of pancreaticbeta cells. The mechanism for thisdevelopment is unclear, but one pos-sibility is that glutathione releasedfrom hemolyzed red cells inactivatesinsulin in the circulation, which trig-
gers more insulin secretion andupregulates the beta cells. Exchangetransfusions may exacerbate theproblem because transfused bloodusually is preserved with a combina-tion of dextrose and other agents.During the exchange, the infantreceives a significant glucose load,with subsequent exaggerated insulinresponse from the hyperplastic pan-creas. At the end of the exchange,the rate of dextrose administrationreturns to baseline, but insulin levelsremain elevated, leading to furtherhypoglycemia.
Use of beta-agonist tocolyticagents such as terbutaline also isassociated with hyperinsulinemia inthe newborn, especially if the agentwas used for more than 2 weeks andwas discontinued less than 1 weekprior to delivery. Affected infantsalso appear to have reduced glyco-gen stores, which further aggravatesthe hyperinsulinemia and its effectson decreasing glucoseconcentrations.
HYPERINSULINISM
Hypoglycemia that persists for morethan 5 to 7 days is uncommon andmost often is due to hyperinsulin-ism. Some infants who have IUGRor perinatal asphyxia demonstratehyperinsulinemia that may persistfor as long as 4 weeks, but suchcases are relatively rare, and theunderlying mechanism is unclear.Several types of congenital hyperin-sulinism have been described andare said to be the most commoncause of hypoglycemia persistingbeyond the first week of life.
The autosomal recessive form ofcongenital hyperinsulinism has beenlinked to a defect in the sulfonylureareceptor or K1-ATP channel. A sin-gle mutation on the short arm ofchromosome 11 has been describedin the Ashkenazi Jewish population,but cases in other ethnic groupshave been associated with a numberof other mutations in the sameregion. An autosomal dominant formof hyperinsulinemia also has beendescribed. The mutation(s) responsi-ble for the autosomal dominant formof hyperinsulinism has not yet beenidentified, but the disorder differsfrom the autosomal recessive formin that it does not appear to result
ENDOCRINOLOGYHypoglycemia
e10 NeoReviews July 1999 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

from abnormal sulfonylurea receptorfunction. A syndrome of congenitalhyperinsulinemia and asymptomatichyperammonemia associated withmutations in the glutamate dehydro-genase gene also has been described.Beckwith-Weidemann syndrome isassociated with hyperplasia of multi-ple organs, including the pancreas,with consequent increased insulinsecretion. Rarely, hyperinsulinemiamay result from localized islet celladenomas within an otherwise nor-mal pancreas.
INBORN ERRORS OFMETABOLISM
Inborn errors of metabolism mayaffect either the availability of glu-coneogenic precursors or the func-tion of the enzymes required forproduction of hepatic glucose. Meta-bolic defects that may present withhypoglycemia include some formsof glycogen storage disease, galac-tosemia, fatty acid oxidation defects,carnitine deficiency, several of theamino acidemias, hereditary fructoseintolerance (fructose-1,6-diphos-phatase deficiency), and defects ofother gluconeogenic enzymes.Finally, endocrine disorders such ashypopituitarism and adrenal failurealso can result in hypoglycemiabecause of the absence of the appro-priate hormonal response to hypo-glycemia and subsequent failure toactivate hepatic glucose production.However, these conditions are veryrare and should be considered afterruling out more common etiologies.
DETERMINING ETIOLOGY
Obtaining a careful perinatal historyis the first step in determining theetiology of hypoglycemia in thenewborn. The presence of risk fac-tors, such as abnormal results on amaternal glucose tolerance test,maternal administration of drugsassociated with neonatal hypoglyce-mia, or prematurity, makes the diag-nosis relatively simple. Growthparameters should be plotted toestablish if the infant is SGA, AGA,or LGA. Sepsis should be suspectedstrongly in the term infant who hashypoglycemia but no other apparentrisk factors. If hypoglycemia persistsfor more than 1 week, the possibili-ties of hyperinsulinemia, other endo-
crine disorders, and inborn errors ofmetabolism should be investigated,especially if the hypoglycemia isrefractory to standard treatment.
Unfortunately, it often is difficultto document hyperinsulinemiabecause insulin levels must bedrawn during episodes of hypogly-cemia to demonstrate the presenceof inappropriate insulin secretion.Levels of the binding protein forinsulin-like growth factor 1 (IGFBP-1) are decreased in the presence ofhyperinsulinemia, making measure-ment of serum levels of IGFBP-1useful in confirming the diagnosis ofhyperinsulinemia. Serum and urinetests for specific metabolic andendocrine disorders, such as serumamino acid profiles and measure-ment of cortisol and growth hor-mone levels, also may be necessaryto elucidate the etiology of neonatalhypoglycemia.
ManagementThe goals in treating the infant whohas hypoglycemia are to normalizeblood glucose concentrations asquickly as possible and to avoidfurther episodes of hypoglycemia byproviding adequate substrate untilnormal glucose homeostasis can beestablished. The method chosen toachieve this goal is a function ofboth the clinical status of the infantand the suspected etiology of thehypoglycemia.
ENTERAL FEEDING
In term infants who have asymptom-atic mild hypoglycemia, an initialattempt at enteral feeding may besuccessful in reaching target bloodglucose values. Although a promptincrease in blood glucose concentra-tions can be achieved following afeeding with a 5% dextrose andwater solution, the dextrose ismetabolized rapidly, and hypoglyce-mia may recur before normal feed-ings can be established. Use of astandard infant formula will providenot only carbohydrate in the form oflactose but also protein and fat,which are metabolized more slowlyand, therefore, will provide a sus-tained supply of substrate. Fat intakealso decreases cellular glucoseuptake and stimulates gluconeogene-
sis, further contributing to a restora-tion of normal glucose homeostasis.It is estimated that blood glucoseconcentrations should increase byapproximately 1.67 mmol/L (30 mg/dL) within the first hour after afeeding of 30 to 60 mL of standardinfant formula.
IV THERAPY
Infants whose blood glucose concen-trations normalize following anenteral feeding should continue tohave blood glucose concentrationschecked before each feeding for12 to 24 hours. If the postprandialconcentration is normal, but thevalue before the next feeding isagain in the hypoglycemic range,enteral feeding should be considereda failure, and the infant is a candi-date for IV therapy. Prompt provi-sion of IV glucose in these circum-stances will avoid repeated episodesof preprandial hypoglycemia. Thismay be important because follow-upstudies of infants who have recur-rent hypoglycemia indicate that mul-tiple episodes of low blood glucoseconcentrations are more likely to beassociated with adverse neurodevel-opmental outcomes than a singleepisode.
IV therapy should be the firsttreatment modality used in symp-tomatic infants, infants unable totolerate enteral feedings, and thosein whom the disturbance in glucosehomeostasis is severe or is expectedto last more than a few hours. Thelatter category includes preterminfants, infants who have IUGR,infants of women who have poorlycontrolled diabetes, and infants whohave underlying etiologies for hypo-glycemia, such as sepsis, known orsuspected inborn errors of metabo-lism or endocrine defects, orerythroblastosis.
Administration of an initial bolusof 200 mg/kg of 10% dextrose andwater (2 mL/kg of D10W) should befollowed by continuous infusion ofdextrose calculated to deliver 5 to8 mg/kg per minute of glucose (ie, arate equivalent to the glucose utili-zation rate of a healthy infant). The“mini-bolus” approach has beenshown to return blood glucose con-centration to normal more rapidlythan a constant infusion alone. The
ENDOCRINOLOGYHypoglycemia
NeoReviews July 1999 e11 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

“mini-bolus” dose also is designedto avoid overshooting the desiredglucose concentration. By limitingthe amount of glucose given as abolus, it is possible to avoid induc-ing iatrogenic hyperglycemia, whichmight stimulate excess insulin secre-tion and induce rebound hypoglyce-mia. The blood glucose concentra-tion should be checkedapproximately 30 minutes after thebolus, then every 1 to 2 hours untilstable and in the normal range. If asubsequent value falls in the hypo-glycemic range, the bolus should berepeated and the infusion rateincreased by 10% to 15%. It is notuncommon for infants who havetransient or sustained hyperinsulin-emia to require as much as 12 to15 mg/kg per minute of IV glucoseto maintain normoglycemia. In suchcases, it may be necessary to placean umbilical venous catheter or aperipheral central venous catheter(so-called PIC line) to allow admin-istration of IV solutions with dex-trose concentrations greater than12.5%.
Unless there are concerns aboutfluid overload or the ability to toler-ate enteral nutrition, infants requir-ing IV therapy for hypoglycemiashould be permitted to continuefeedings. There are several benefitsto this practice. First, it will allowan easier transition from a parenteralto an enteral source of carbohydrateonce blood glucose concentrationshave stabilized. Second, providingsome carbohydrate as galactose (oneof the sugars that comprise lactose)may be useful in IDMs and otherinfants who have hyperinsulinemia;
studies have shown that the pancre-atic insulin response to galactose isless than the response to an equiva-lent amount of glucose. When a nor-mal blood glucose concentration hasbeen established and the requirementfor IV glucose has been stable for12 to 24 hours, the infant can beweaned from this therapy by mea-suring preprandial blood glucoseconcentrations and decreasing theinfusion rate by 10% to 20% eachtime the blood glucose is greaterthan 2.8 to 3.4 mmol/L (.50 to60 mg/dL). Failure to tolerate wean-ing from IV glucose indicates thepresence of a pervasive disorder,such as a metabolic defect or idio-pathic hyperinsulinemia, and shouldprompt further evaluation.
OTHER AGENTS
Several other agents have been usedto treat refractory hypoglycemia,most often encountered in one of thehyperinsulinemic states (Table 2).Corticosteroids (hydrocortisone, 5 to15 mg/kg per day in two to threedivided doses, or prednisone,2 mg/kg per day) are associatedwith decreased peripheral glucoseutilization and increased blood glu-cose concentrations, but they have avariety of other metabolic effectsthat must be considered. Administra-tion of corticosteroids as an adjunctto IV glucose may be useful whenglucose requirements are greaterthan 15 mg/kg per minute.
Glucagon will produce a rapidrise in blood glucose in infants whohave adequate glycogen stores, butthis is only a transient effect, and
caregivers must be prepared to man-age hypoglycemia when it recurs.Preterm infants and infants whohave IUGR have limited glycogenstores and are unlikely to experiencean increase in blood glucose concen-tration following administration ofglucagon. An initial dose of30 mcg/kg may produce a responsein some infants, but those who havehyperinsulinemia may require a10-fold higher dose to overcome theeffects of high circulating insulinlevels and stimulate glycogenolysis.Administration of glucagon is mostuseful in those infants who havesevere hypoglycemia as a temporiz-ing measure until stable IV accesscan be obtained (eg, while awaitingthe arrival of a transport team).
Several other agents may be valu-able for management of infants inwhom the diagnosis of hyperinsulin-emia is confirmed and who remainpersistently hypoglycemic in spite ofadministration of IV glucose at15 to 20 mg/kg per minute. Diazox-ide at a dose of 5 mg/kg every8 hours will inhibit pancreatic insu-lin secretion. Somatostatin or itslong-acting analogue octreotide alsoinhibits insulin release as well asgrowth hormone and glucagonsecretion and is used most oftenpreoperatively in infants requiringpancreatectomy for refractory hypo-glycemia and hyperinsulinemia. Sub-total (95%) or near-complete pancre-atectomy may be required tomanage cases of hyperinsulinemiadue to gene mutations or islet celladenomas. However, hypoglycemiarecurs in up to 33% of surgicallytreated patients, and 40% to 60%
TABLE 2. Adjunct Therapies for Hypoglycemia
THERAPY EFFECT DOSAGE
Corticosteroids Decrease peripheral glucoseutilization
Hydrocortisone 5 to 15 mg/kg per dayor
Prednisone 2 mg/kg per day
Glucagon Stimulates glycogenolysis 30 mcg/kg if normal insulin300 mcg/kg if increased insulin
Diazoxide Inhibits insulin secretion 15 mg/kg per day
Somatostatin (long-acting:octreotide acetate)
Inhibits insulin and growthhormone release
5 to 10 mcg/kg every 6 to 8 h
Pancreatectomy Decreases insulin secretion —
ENDOCRINOLOGYHypoglycemia
e12 NeoReviews July 1999 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

develop diabetes mellitus later inlife.
Consequences ofHypoglycemia
HYPOGLYCEMIC BRAIN INJURY
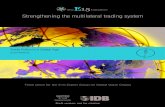
Although hypoglycemia is associ-ated with a number of physiologicchanges, the most profound effectsare seen in the brain, where glucoseis the major substrate for energymetabolism and both local energystores and the supply of alternatesubstrates are limited. Severe hypo-glycemia in the newborn is associ-ated with selective neuronal necrosisin multiple brain regions, includingthe superficial cortex, dentate gyrus,hippocampus, and caudate-putamen.The initiating events in hypoglyce-mic encephalopathy still are notunderstood completely, but braininjury appears to result from a num-ber of processes that are initiatedwhen blood glucose concentrationsdecrease (Figure). A moderatereduction in blood glucose concen-tration is associated with compensa-tory increases in cerebral blood flowthat have been assumed to represent
a means of maintaining delivery ofcerebral glucose. In preterm new-borns, such changes in cerebralblood flow may predispose to intra-ventricular hemorrhage and mayhave little effect on neuronal glu-cose supply because transfer of glu-cose across the blood-brain barrierdepends on the activity of the glu-cose transporters on the vascularendothelium and cell membranes.Glucose transporter levels aredecreased in the fetus and newborncompared with older infants andmay be rate-limiting for cerebralglucose uptake.
If glucose supply to the brain isnot maintained, there may be adecrease in cerebral electrical activ-ity, membrane breakdown withrelease of free fatty acids, andaltered amino acid metabolism,including increased production ofglutamate. Glutamate, which is oneof the excitatory amino acid neuro-transmitters found only in the cen-tral nervous system, is believed toplay a major role in the pathophysi-ology of hypoglycemic brain injury.Hypoglycemia is associated withincreased glutamate concentrations
in the synaptic cleft, most likely dueto a combination of increased gluta-mate release from presynaptic neu-rons and decreased adenosine59-triphophate (ATP)-dependent glu-tamate uptake by glial cells. Gluta-mate binds to postsynaptic receptors,triggering release of second messen-gers via the metabotropic glutamatereceptors and changes in transmem-brane ion fluxes via the ionotropicglutamate receptors. Although thereare several types of ionotropicreceptors, theN-methyl-D-aspartate(NMDA)-type glutamate receptor,which is associated with an ionchannel that transports sodium andcalcium into the cell and potassiumout of the cell, predominates inimmature brain. In all species stud-ied, including humans, the numberof functional NMDA receptorsincreases during brain development,subsequently decreasing to adultlevels.
The increased number of NMDAreceptors in the late fetal and earlynewborn periods most likely reflectsthe role of the receptor as one of theprimary mediators of long-termpotentiation, a process that is associ-ated with synaptogenesis and mem-
ory formation. NMDAreceptor activity alsomay be involved inregulating the processof apoptosis, or pro-grammed cell death,via changes in cyto-plasmic and nuclearcalcium concentrations.In the human fetus, thethird trimester of fetaldevelopment and earlyneonatal period arecharacterized by activeformation and modifi-cation of synaptic con-nections and arboriza-tion of dendritesassociated withincreased NMDAreceptors. Thus, nor-mal levels of NMDAreceptor activity arecritical to the develop-ment of the immaturebrain. However, excessactivation of NMDAreceptors by glutamateincreases cytoplasmicconcentrations of
FIGURE. Proposed mechanism for the pathogenesis of hypoglycemic brain injury in the newborn.ATP 5 adenosine 59-triphosphate; PCr5 phosphocreatine. Used with permission of Ross ProductsDivision, Abbott Laboratories Inc., Columbus, OH 43216. FromSemin Neonat Nutr Metab.1997;4, Ross Products Division, Abbott Laboratories Inc.
ENDOCRINOLOGYHypoglycemia
NeoReviews July 1999 e13 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

sodium and calcium to levels thatexceed the capacity of neuronalhomeostatic mechanisms, therebyaltering transmembrane ion gradi-ents. Hypoglycemia specificallyincreases the sensitivity of NMDAreceptors to activation by glutamate,which may result in a lower thresh-old for glutamate-induced excitotox-icity. During hypoglycemia, energy-dependent mechanisms for restoringnormal transmembrane gradients ofsodium and calcium cannot operatebecause of the depletion of ATP andphosphocreatine associated withhypoglycemia. Excess calciuminflux activates cellular phospho-lipases and proteases, alters mito-chondrial metabolism, triggers freeradical formation, changes patternsof synaptic transmission, and even-tually may result in selective neuro-nal necrosis.
There is increasing evidence thatspecific changes in mitochondrialfunction may play a significant rolein the early events leading to hypo-glycemic encephalopathy. Decreasedfluxes of substrate through the tri-carboxylic acid cycle results indecreased availability of reducingequivalents in mitochondria. As aresult, there is incomplete reductionof molecular oxygen within mito-chondria and increased formation ofoxygen free radicals, which damageboth mitochondrial membranes andmitochondrial DNA. Fragmentationof mitochondrial DNA interfereswith synthesis of electron transportchain enzymes, such as subunits ofcytochrome oxidase and nicotin-amide adenine dinucleotide(NADH)-dehydrogenase that arecoded for by the mitochondrialgenome. Thus, the ability of the cellto restore ATP levels is impaired.Local depletion of high-energyphosphates as well as changes in themitochondrial membranes lead todecreased sequestration of calciumby the mitochondria as cytoplasmiccalcium. Mitochondrial dysfunctionalso may contribute directly to neu-ronal necrosis by initiating the pro-cess of apoptosis. Recent studieshave indicated that release of cyto-chrome c from mitochondria isrequired to activate the enzymes thattrigger apoptosis and that cyto-chrome c is released as oxidativephosphorylation fails.
Hypoglycemia also could exacer-bate brain injury during periods ofcerebral hypoxia in immature brain.As in hypoglycemia, cerebralhypoxia is associated with depletionof high-energy phosphates, increasedextracellular glutamate concentra-tions, activation of ionotropic gluta-mate receptors, and increased intra-cellular sodium and calcium. Inaddition, anaerobic glycolysis duringhypoxia accelerates depletion of glu-cose in the brain. Thus, the combi-nation of hypoglycemia and hypoxiamight be expected to act synergisti-cally in producing neuronal injury.Although hypoglycemia appears tobe neuroprotective during cerebralischemia in adults, studies in imma-ture animals have demonstrated thatconcurrent hypoglycemia exacer-bates hypoxic-ischemic brain injury,possibly by accelerating depletion ofhigh-energy phosphates. Hypoglyce-mia also abolishes hypoxic vasodila-tation of cerebral blood vessels, thusimpairing compensatory mechanismsthat might otherwise improve oxygendelivery to the brain during periods ofhypoxemia. Although further investi-gation is necessary, these results indi-cate that maintenance of normoglyce-mia is especially critical in infants atrisk for episodes of hypoxemia, suchas those who have significant respira-tory distress.
CLINICAL CONSEQUENCES
The physiologic disturbances associ-ated with acute hypoglycemia in thenewborn result in a stress response,with release of catecholamines andglucagon and subsequent lipolysisand glycogenolysis in an attempt toincrease substrate availability fornormal metabolic processes. Thus,even in asymptomatic hypoglycemia,there are significant short-termeffects on the infant that may resultin depletion of endogenous sub-strate, leaving the infant unpreparedto handle subsequent physiologicstress. In term infants, a brief periodof increased sympathetic activityand altered hepatic metabolism usu-ally is tolerated well. However, inthe preterm or SGA infant, theadded physiologic stress associatedwith a low blood glucose concentra-tion may be sufficient to precipitatecardiorespiratory instability and
complicate acute management sig-nificantly. Prompt, rapid normaliza-tion of low blood glucose concentra-tions is required to minimize thehormonal and metabolic derange-ments. If a normal blood glucoseconcentration can be achieved in atimely manner, the acute effects of asingle episode of hypoglycemia canbe minimized.
The long-term effects of neonatalhypoglycemia remain controversial.Repeated episodes of symptomatichypoglycemia, as are seen in infantswho have persistent hyperinsulinism,have been associated with selectiveneuronal necrosis and long-termimpairment of cognitive and motorfunction. Early studies also reportedpoor neurodevelopmental outcomesin IDMs. However, more recent datasuggest that hypoglycemia alonedoes not alter long-term outcome inIDMs; rather, adverse outcomeswere related to the presence of con-genital anomalies.
Very few data are availableregarding the long-term outcome inthe vast majority of hypoglycemicinfants who have asymptomatichypoglycemia that is detected onroutine screening and is treatedpromptly. Studies in normal adultshave shown that cognitive functionis impaired during mild insulin-induced hypoglycemia (blood glu-cose values, 3.4 mmol/L[,60 mg/dL]). Adult diabetics whohave a history of recurrent episodesof hypoglycemia have been found tohave persistent cognitive deficits aswell as mild cortical atrophy, find-ings that have not been observed indiabetics who have not experiencedsignificant hypoglycemia.
Most studies in newborns,although unavoidably limited inscope, have failed to demonstrateany long-term sequelae in terminfants who have experienced briefepisodes of hypoglycemia. Changesin brainstem auditory evokedresponses (BAERs) were reported inseveral infants (1 to 5 d old) duringepisodes of hypoglycemia ofunspecified etiology. AbnormalBAERs were detected at blood glu-cose concentrations ranging from0.7 to 2.5 mmol/L (12 to 45 mg/dL),and in two infants they remainedabnormal for several hours after glu-cose had been administered. How-
ENDOCRINOLOGYHypoglycemia
e14 NeoReviews July 1999 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

ever, no long-term follow-up wasreported on these infants. A secondstudy, which analyzed factors affect-ing outcome at 18 months of age ina cohort of preterm infants, foundthat those who had at least oneblood glucose value less than2.6 mmol/L (46 mg/dL) on 5 ormore days had significantly lowerscores on standardized tests of men-tal and motor development and athreefold higher incidence of cere-bral palsy than those who had fewerepisodes of hypoglycemia or thosewho had experienced a single epi-sode of more severe hypoglycemia.The differences remained significantwhen other risk factors such as birth-weight and intraventricular hemor-rhage were accounted for. Thus, thereis evidence to suggest that mild-to-moderate hypoglycemia may affectoutcome, at least in high-risk infants.
ConclusionDisturbances of glucose homeostasisthat result in hypoglycemia are com-
mon among newborns. Awareness ofrisk factors that predispose infants tohypoglycemia allows for screeningof those at risk so that clinicallyundetectable hypoglycemia can betreated promptly, thereby preventingthe development of severe or symp-tomatic hypoglycemia, which isassociated with adverse outcomes.However, management of high-riskinfants is complicated by the lack ofa consensus on the blood glucosevalue that constitutes hypoglycemiaas well as the inaccuracies in meth-ods used to measure blood glucosevalues. A further unresolved issue iswhether asymptomatic hypoglycemiais associated with permanent effectson brain function in the newborn.No conclusive studies demonstratelong-term effects of asymptomatichypoglycemia in term infants, but itis likely that hypoglycemia contrib-utes to abnormal neurodevelopmen-tal outcome in infants who haveother risk factors for brain injury,such as prematurity or hypoxic-ischemic brain injury. In these
infants, maintaining blood glucoseconcentrations well above thethreshold for hypoglycemia mayimprove neurologic outcome. Fur-ther studies are necessary to deter-mine the consequences of hypogly-cemia in term infants.
SUGGESTED READINGAynsley-Green A. Glucose, the brain, and the
pediatric endocrinologist.Horm Res.1996;46:8–25
Kalhan S, Saker F. Metabolic and endocrinedisorders, part one: disorders of carbohy-drate metabolism. In: Fanaroff AA, MartinRJ, eds.Neonatal-Perinatal Medicine:Diseases of the Fetus and Newborn. 6thed. St. Louis, Mo: Mosby-Year Book Inc;1997
Stanley CA. Hyperinsulinism in infants andchildren.Pediatr Clin North Am.1997;44:363–374
Williams AF. Hypoglycemia in the Newborn:A Review. WHO Publications #5778, 1997
ENDOCRINOLOGYHypoglycemia
NeoReviews July 1999 e15 at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

DOI: 10.1542/pir.20-7-e61999;20;e6Pediatrics in Review
Jane E. McGowanNeonatal Hypoglycemia
ServicesUpdated Information &
http://pedsinreview.aappublications.org/content/20/7/e6including high resolution figures, can be found at:
Referenceshttp://pedsinreview.aappublications.org/content/20/7/e6#BIBLThis article cites 2 articles, 0 of which you can access for free at:
Permissions & Licensing
http://pedsinreview.aappublications.org/site/misc/Permissions.xhtmlin its entirety can be found online at: Information about reproducing this article in parts (figures, tables) or
Reprintshttp://pedsinreview.aappublications.org/site/misc/reprints.xhtmlInformation about ordering reprints can be found online:
at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from

DOI: 10.1542/pir.20-7-e61999;20;e6Pediatrics in Review
Jane E. McGowanNeonatal Hypoglycemia
http://pedsinreview.aappublications.org/content/20/7/e6located on the World Wide Web at:
The online version of this article, along with updated information and services, is
Pediatrics. All rights reserved. Print ISSN: 0191-9601. Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 1999 by the American Academy of published, and trademarked by the American Academy of Pediatrics, 141 Northwest Pointpublication, it has been published continuously since 1979. Pediatrics in Review is owned, Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly
at Indonesia:AAP Sponsored on January 7, 2015http://pedsinreview.aappublications.org/Downloaded from