Pediatrics 2010 Ravichandiran 60 6
-
Upload
bocahbritpop -
Category
Documents
-
view
220 -
download
0
Transcript of Pediatrics 2010 Ravichandiran 60 6
-
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
1/9
DOI: 10.1542/peds.2008-3794; originally published online November 30, 2009;2010;125;60Pediatrics
Shouldice, Hosanna Au and Kathy Boutis
Nisanthini Ravichandiran, Suzanne Schuh, Marta Bejuk, Nesrin Al-Harthy, MichelleDelayed Identification of Pediatric Abuse-Related Fractures
http://pediatrics.aappublications.org/content/125/1/60.full.htmllocated on the World Wide Web at:
The online version of this article, along with updated information and services, is
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.Boulevard, Elk Grove Village, Illinois, 60007. Copyright 2010 by the American Academypublished, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
publication, it has been published continuously since 1948. PEDIATRICS is owned,PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/content/125/1/60.full.html -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
2/9
Delayed Identification of Pediatric Abuse-RelatedFractures
WHATS KNOWN ON THIS SUBJECT: Patient assessment byphysicians of children who are at risk for abuse is suboptimal,
and, therefore, abusive fractures are at risk for escaping
detection or delayed recognition. It is unknown, however, how
often this occurs.
WHAT THIS STUDY ADDS: Approximately 20% of abusive
fractures were missed at initial physician visits. Boys who
present to a nonpediatric ED with an extremity fracture seem to
be at highest risk of the abusive etiology of the fracture escaping
of detection by a physician.
abstractOBJECTIVES: Because physicians may have difficulty distinguishing
accidental fractures from those that are caused by abuse, abusive
fracturesmay be at risk fordelayed recognition;therefore, the primary
objective of this study was to determine how frequently abusive frac-
tures were missed by physicians during previous examinations. A sec-
ondary objective was to determine clinical predictors that are associ-
ated with unrecognized abuse.
METHODS:Children who were younger than 3 years and presented toa large academic childrens hospital from January 1993 to December
2007 and received a diagnosis of abusive fractures by a multidisci-
plinary child protective team were included in this retrospective re-
view. The main outcome measures included the proportion of children
who had abusive fractures and had at least 1 previous physician visit
with diagnosis of abuse not identified and predictors that were inde-
pendently associated with missed abuse.
RESULTS:Of 258 patients with abusive fractures, 54 (20.9%) had at
least 1 previous physicianvisit at which abuse was missed. The median
time to correct diagnosis from the first visit was 8 days (minimum: 1;
maximum: 160). Independent predictors of missed abuse were malegender, extremity versus axially located fracture, and presentation to a
primary care setting versus pediatric emergency department or to a
general versus pediatric emergency department.
CONCLUSIONS: One fifth of children with abuse-related fractures are
missed during the initial medical visit. In particular, boys who present
to a primary care or a general emergency department setting with an
extremity fracture are at a particularly high risk for delayed diagnosis.
Pediatrics2010;125:6066
AUTHORS:Nisanthini Ravichandiran,
a
Suzanne Schuh,MD,a Marta Bejuk, MD,a Nesrin Al-Harthy, MD,a
Michelle Shouldice, MD,b Hosanna Au, MD,b and
Kathy Boutis, MD, MSca
Divisions ofaPediatric Emergency Medicine andbPediatric
Medicine and Suspected Child Abuse and Neglect, Hospital for
Sick Children, University of Toronto, Toronto, Ontario, Canada
KEY WORDS
pediatrics, child abuse, bone fractures, diagnosis
ABBREVIATIONS
EDemergency department
SCANSuspected Child Abuse and Neglect
HSCHospital for Sick Children
ORodds ratio
CIconfidence interval
www.pediatrics.org/cgi/doi/10.1542/peds.2008-3794
doi:10.1542/peds.2008-3794
Accepted for publication Jul 28, 2009
Address correspondence to Kathy Boutis, MD, MSc, 555
University Ave, Toronto, ON, M5G 1X8, Canada. E-mail:
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright 2009 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The authors have indicated they have
no financial relationships relevant to this article to disclose.
60 RAVICHANDIRAN et alat Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
3/9
Although fractures are a common pre-
senting finding in child abuse,1,2 clini-
cians may have difficulty differentiat-
ing abuse-related fractures from
those that are caused by accidental
trauma24; however, this distinction is
crucial because of its impact on con-sequences for the child.5,6 Whereas
accidental injuries carry only their
inherent risks, repeat injury occurs
in 35% of all abuse cases, and 5% to
10% of patients will die if there is no
intervention.7
Despite the serious risks associated
with delayed recognition of abusive
fractures, patient assessment for this
diagnosis is often suboptimal.14,8 One
study found that of 100 children who
were younger than 3 years and pre-
sented to an emergency department
(ED) with long bone fractures, 31 had
indicators suggestive of abuse but only
1 was referred to child protection ser-
vices for additional assessment.2 Ban-
askiewitz et al3 demonstrated that in
infants who were younger than 1 year,
the possibility of abuse was underesti-
mated by ED clinicians in 28% of
cases when compared with a retro-
spective diagnosis by a child protec-
tion team pediatrician. Moreover, re-
search conducted in a pediatric ED
demonstrated that 42% of charts re-
viewed did not have adequate docu-
mentation to explain the cause of the
fractures, and inflicted injuries were
therefore not adequately ruled out.1
This evidence suggests that abusive
fractures arelikely at risk for escapingdetection or delayed recognition; how-
ever, the frequency with which this oc-
curs remains unknown. The primary
objective of this study was to deter-
mine the proportion of abuse-related
fractures that were missed at previ-
ous physician encounters. The clinical
factors that may have contributed to
the reasons for the diagnostic delay
were also examined.
METHODS
Patient Population
Children who were younger than 3
years,2,911 had abusive fractures that
occurred from January 1993 to Decem-
ber 2007, and were referred to amultidisciplinary hospital-based Sus-
pected Child Abuse and Neglect (SCAN)
team at the Toronto Hospital for Sick
Children (HSC) were included. HSC
SCAN consists of specialty pediatri-
cians, psychologists, social workers,
and nurse practitioners. Members of
HSC SCAN team are the only child
abuse specialists in the Greater To-
ronto Area and are involved in the as-
sessment of most cases of suspected
abuse in that area. The HSC SCAN
teams assessment results in a classi-
fication of these fractures as abusive,
indeterminate, or accidental. The study
sample included only cases for which
the first physician visit was primarily
for an isolated fracture. Cases were
excluded when the childs clinical pre-
sentation was predominantly consis-
tent with some other type of trauma,
medical records were inaccessible,
only metaphyseal corner chip frac-
tures (usually asymptomatic) were
present, or the cause of the fracture
was indeterminate or accidental.
Definitions
Fractures were determined to be abu-
sive when at least 1 of the following
criteria was met2,6,12: (1) confession of
intentional injury by an adult caregiver;
(2) inconsistent/inadequate history
provided; (3) inappropriate delay in
seeking medical care; (4) associated
inadequately explained injuries; (5)
in the absence of bone disease, pres-
ence of fractures uncommon for
accidental injury and frequently re-
ported in abusive injury (eg, meta-
physeal limb fractures, posterior rib
fractures not caused by birth trau-
ma)6,13,14; and (6) witness to abuse
came forward.
A case was considered recognized
when a referral to local child protec-
tion authorities was made the first
time the child presented to a physician
with the index fracture(s). This is in
contrast to missed when the child
had at least 1 physician encounter forthe index fracture(s) before the visit
when the abuse was confirmed. In all
missed cases, the signs andsymptoms
compatible with a fracture and/or a
radiograph diagnosis were present at
the initial visit, but the possibility of
abuse was not raised. Thereafter, 1
of the following occurred: (1) the child
improved clinically but experienced re-
peat trauma and the HSC SCAN team
found the previous fracture(s) abu-
sive; (2) recognition of red flags and
referral to the SCAN team at a routine
follow-up for the index fracture(s) led
to recognition of abuse; (3) the childs
continued symptoms resulted in re-
peat unscheduled visits and a referral
to the SCAN team with recognition of
the index fracture(s) as abuse-related;
(4) the index radiographs initially read
as normal by the primary treating phy-
sician were found by a radiologist to
have a fracture that required a repeat
visit, when the suspicion for abuse was
raised; (5) the perpetrator later con-
fessed or a witness came forward;
and/or (6) abuse was suspected in a
sibling and review of the patients frac-
tures yielded abuse as the cause. The
determination of missed versus recog-
nized cases was made independent of
the knowledge of potential predictors.Because specific income of the fam-
ily was not available, this was esti-
mated on the basis of median income
of families in a given postal code.15
On the basis of the 2006 Ontario me-
dian household income of $60 455,
median income was then additionally
classified as low ($45 341.25), mid-
dle ($45 341.25$90 682.50), or high
($90 682.50).16 Income classifica-
ARTICLES
PEDIATRICS Volume 125, Number 1, January2010 61at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
4/9
tion was used as a surrogate mea-
sure of socioeconomic status.17
Social concerns were defined as any
primary caregiver who had 1 of
the following: young single parent
(younger than 20 years and no live-in
partner at the time of the childs eval-
uation); previous contact with child
protection services; or history of incar-
ceration, substance abuse problem,
living in group housing (eg, shelter), or
domestic violence. A positive skeletal
survey was defined as additional frac-
tures other than the index fracture(s).
In a primary care office, children are
assessed by a family physician or
pediatrician. In general EDs that
serve all ages, children are seen by
ED physicians.
Case Selection, Data Collection,
and Review
Once the HSC SCAN team has reviewed
a case, referral information is entered
into a database. This database was
searched for eligible patients, and
study-specific information of identified
cases was collected from original pa-
tient records (Fig 1). Information col-
lected by 2 research assistants (Ms
Ravichandiran andDr Bejuk) whowere
trained in the methods of chart ab-
straction included relevant patient
and family demographics, social his-
tory, history of present illness, details
of the childs injury(ies), subsequent
clinical course, and details from previ-
ous visits related to the index frac-
ture(s). For missed cases, the clinical
data from the initial physician visit(s)
before the visit when abuse was diag-nosed were reviewed by 1 SCAN physi-
cian (Dr Al-Harthy), who was masked
to the final SCAN opinion and the pur-
pose of the study, to ascertain the
presence of indicators of abuse that
should have led to a referral to a child
protective team at that visit.
An a priori defined list of potential pre-
dictors that were independent of the
outcome of a missed diagnosis of
abuse was selected by 3 expert mem-
bers of the HSC SCAN team1,2,6,10,12,18,19
and later modified in accordance with
the available data. For example, al-
though race3,8,12 has been strongly as-
sociated with referrals to child protec-
tive teams, this information is notcollected by the reviewing HSC SCAN
team. The final list of predictors is de-
tailed in Table 1. Some of the variables
used routinely in ascertaining abuse
could not be considered as predictors
because they are not independent of
the outcome.
After data collection was complete, in-
formation on each patient was re-
viewed for accuracy and completeness
by a pediatric ED physician (Dr Boutis)in collaboration with the 2 research
assistants. Missing data were imputed
by inserting the respective median
(categorical) or mean (continuous
data) value from the group data into
blank cells.20 Permission for this re-
search was obtained from our re-
search ethics board.
Analysis
The sample size was calculated by us-ing the methods by Hsieh21 and the fol-
lowing parameters were used:
.05, and .20, estimated proportion
of missed abusive fractures of 20%,22
and an odds ratio (OR) of 2.023 of
missed abuse corresponding to an in-
creaseof1SDfromthemeanvalueofa
covariate.21 In this study, there are
multiple covariates and a possibility of
some unknown correlation between
covariates. Thus, a conservative valueof .5 was estimated, and the ad-
justed minimal total sample size is
therefore 182.
A univariate analysis was used to as-
sess whether a particular variable
was associated with the outcome vari-
able of interest, missed case of abu-
sive fracture (Table 1). For the latter,
Pearson2 test was used for categor-
ical values and independent Students
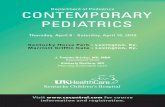
FIGURE 1Patient inclusion/exclusion flow diagram.
62 RAVICHANDIRAN et alat Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
5/9
ttest for continuous variables. Inde-
pendent variables with P .20 and any
relevant interaction and confounding
terms were entered into a multivariate
logistic regression model using the
forward selection method (Table 2).24
Approximately 14 missed cases per
variable were entered into the model,
meeting the minimal criteria of 10
events per variable to minimize over-
fitting of the data.2527 Wald and Like-
lihood ratio testing were then used
to iteratively remove noncontributory
variables from the model.24 Goodness
of fit of the final model to the data was
tested by using the Hosmer-Lemeshow
test. A receiver operating characteris-
tic curve was plotted to check the pre-
dictive ability of the model. Odds of a
case being missed for a given variable
were reported with respective 95%
confidence intervals (CIs). All analyses
were performed by using SPSS 13 for
Windows (SAS Institute, Cary, NC).
RESULTS
This study included 258 eligible pa-
tients with abusive fractures (Fig 1).
A comparison of characteristics of
missed and recognized cases is de-
tailed in Tables 1 and 2. Of the 258 pa-
tients, 54 (20.9% [95% CI: 15.8 26.0])
had at least 1 previous physician visit
at which abuse was missed. Of the 145
children with an abusive extremity
fracture, 41 (28.3% [95% CI 20.8 35.8])
were missed. From the initial visit for
the index fracture(s), the median delay
of the diagnosis of abuse was 8 days
(minimum: 1; maximum: 160), and the
median number of physician visits was
1 (minimum: 1; maximum: 3). Of the
children who re-presented for medical
care after the abusive cause of the
fracture was missed, 9 (16.7%) pre-
sented with new abusive injuries. In 7
of these cases, there was a different
fracture; 1 child had serious abdomi-nal injuries, and another had serious
head trauma that resulted in death.
Incorrect interpretation of the radio-
graph findings by the physician re-
sulted in 18 (33.3%) missed cases
(Fig 2), 7 of which were skull fractures.
In 7 (13.0%), the initial imaging series
was incomplete and the abuse-related
fracture was therefore not seen. This
subgroupreturnedto an ED because of
persistence of symptoms, more exten-sive imaging was performed, the frac-
ture was detected, and a referral to
the SCAN team was made. The exact
reasons that the remaining 29 cases
were missed are not certain because
of a lack of available data; however,
inadequate screening or accepting im-
plausible mechanisms may have con-
tributed to missing these cases. SCAN
documentation revealed that these
children had risk factors for abuse: 25(86.2%) of 29 were nonambulatory; in
26 (90.0%) of 29, parental report of
mechanism did not explain injuries;
and 14 (48.3%) of 29 had social con-
cerns. Furthermore, review of the ini-
tial visit records demonstrated that 13
(50.0%) of 26 had incomplete docu-
mentation of the preceding events or
possible related risk factors for abuse.
The univariate analysis demonstrated
that 3 variables were found to be sig-nificantly associated with a missed di-
agnosis of abuse: male gender, initial
presentation to a nonpediatric ED, and
an extremity fracture (Table 1). The
probability of missing this diagnosis
for each predictor after adjustment
for all significant predictors is summa-
rized in Table 3. No statistically signifi-
cant interaction terms or confounding
variables were identified in this analy-
TABLE 1 Characteristics of Missed and Recognized Abuse Cases
Characteristic Recognized
Cases
(n 204)
Missed
Cases
(n 54)
Pfor Univariate
Analysis of
Independent
Variables
Potential predictors independently associated with
missed abuse
Age, mean
SD, mo 8.28
7.05 9.24
8.31 .3910Male gender, % 44.4 60.8 .0250a
Pediatric ED setting at initial visit, % 89.9 10.1 .0001a
Injury event reported, % 41.5 38.9 .8840
Extremity fracture, % 51.0 75.9 .0010a
Parents living apart, % 26.5 31.5 .4410
Low socioeconomic status, % 27.4 22.4 .6100
Additional baseline characteristics (not independently
associated with missed abuse)
Nonambulatory, % 71.6 66.7
No. of fractures on initial radiograph, median (range) 1 (2) 1.0 (2)
Positive skeletal survey,n(%) 82 (40.1) 34 (63.0)
No. of fractures on skeletal survey, median (range) 1 (25) 2 (26)
Lack of plausible mechanism, % 98.5 94.4
Delay in seeking care, % 29.5 38.9
Single caregiver, % 26.0 29.8Social concerns, % 43.6 50.9
a Statistically significant.
TABLE 2 Fracture Locations of Recognized
Versus Missed Cases
Fracture
Location
Recognized
Abuse
Cases
(n 204)
Missed
Abuse
Cases
(n 54)
Clavicle,n(%) 8 (3.92) 2 (3.70)
Humerus,n(%) 32 (15.70) 13 (24.10)
Forearm,n(%) 19 (9.30) 7 (13.00)
Wrist,n(%) 0 (0.00) 1 (1.90)
Digits,n(%) 0 (0.00) 1 (1.90)
Femur,n(%) 48 (23.50) 9 (16.70)
Tibia/fibula,n(%) 24 (11.80) 11 (20.40)
Scapula,n(%) 0 (0.00) 2 (3.70)
Skull,n(%) 73 (35.80) 15 (27.80)
Sternum,n(%) 4 (2.00) 0 (0.00)
Totala 208 61
a Numbers exceed total number of patients because some
patients had1 fracture.
ARTICLES
PEDIATRICS Volume 125, Number 1, January2010 63at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
6/9
sis. In the resultant model, the Hosmer-
Lemeshow goodness-of-fit test did not
reject the null hypothesis of good fit
(P .718), and the predictive ability of
the model is good (area under the
curve: 0.841). Applying this model pre-
dicts that if all 3 factors were present,then the probability that an abusive
fracture would be missed is 50%.
Sixteen charts were missing and un-
available for review, and if we assume
that all were recognized abuse, then
the proportion of missed abuse would
decrease only to 54 (19.1%) of 274. Of
the 139 initial visits that occurred out-
side HSC, 3 of 45 of the missed and 15
of 94 of the recognized first physician
visit documents were not available for
detailed review. In 2 (0.8%) of the 258
cases, the initial clinical setting could
not be determined. In 16 (6.2%) cases,
it was uncertain whether an injury was
reported. Forty (15.5%) had living sta-
tus of parents unavailable. Finally, a
postal code was not recorded for 49
(19.0%) cases. Sensitivity analyses
with and without imputed data for
these missing variables were per-
formed and did not reveal any signifi-
cant differences; therefore, only unim-
puted results are presented.
DISCUSSION
This study is the first to report the fre-
quency of delayed recognition of abu-
sive fractures in children. One fifth of
children with abusive fractures were
missed at initial physician visits, which
is comparable to that reported for
other types of abuse12,19; however, we
do not know how many cases of abu-
sive fractures are never detected. We
also found that boys, children who
present to a nonpediatric ED or a pri-
mary care setting, and/or those with
an extremity fracture seem to be at the
highest risk of the abusive etiology of
the fracture escaping of detection by a
physician at an initial visit.
In 17% of missed abuse cases, chil-
dren sustained repeat injuries be-tween their initial visit and their even-
tual diagnosis of abuse; previously
missed fractures that led to serious
abusive injuries were also found by
Oral et al.28 The skeletal survey that
was performed during subsequent vis-
its may have a major impact on the
correct diagnosis. In this study, two
thirds of patients had healing frac-
tures identified on the survey, and this
is higher than that reported previous-ly.5,22 This highlights the importance of
having a low threshold to consider a
skeletal survey for children who may
be at risk for abuse5,14,22 before dis-
missing the fractures as accidental.
In the 54 missed cases, approximately
one third of the fractures were not
detected on the initial radiographs
by front-line physicians in a country
where immediate radiology interpre-
FIGURE 2A, Missed versus recognized abusive fracture cases. B, Recognized versus missed abusive fracture cases by presentation site.
TABLE 3 Predictor Variables That Were
Independently Associated WithMissed Abuse
Predictor OR 95% CI
Male vs female gender 2.00 1.033.80
Setting
Primary care office vs
pediatric ED
5.20 1.7715.39
General ED vs pediatric ED 7.20 3.0017.30
Extremity vs axial skeleton
fracture
2.30 1.104.77
64 RAVICHANDIRAN et alat Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
7/9
tations are not routine practice in the
ED or office setting. Pediatricians have
limited skills in the recognition of frac-
tures on radiographs.29 This is true
particularly of skull fractures,30 and
identification of this type of fracture,
especially in very young infants, mayprompt the physician to assess for
other maltreatment risk factors.31 This
study suggests that front-line physi-
cians should strongly consider con-
sulting a radiologist when the pres-
ence of a fracture may lead to
increased suspicion of abuse.
In our study, abuse was more likely to
be missed when a child presented to a
general ED or primary care setting.
These results support those by Trokelet al,23 who found lower rates of abuse
in patients who had traumatic brain
injury or femur fracture and pre-
sented to general hospitals compared
with their pediatric counterparts. This
could suggest that abuse may be
missed in these settings. Clinicians
who work in these areas may lack ex-
pertise in the recognition of abuse-
related fractures despite the presence
of indicators for abuse.1,2,32
This re-search supports the need for quality
improvement programs at general
hospitals and primary care settings.
Children with extremity shaft frac-
tures caused by abuse were also found
to be at increased risk for having
physicians attribute their injuries to
accidental causes. Although extremity
fractures are the most common skele-
tal injuries that occur in abused chil-
dren,2
radiology literature demon-strates that these injuries also have
the lowest specificity for abuse.14 No
fracture on its own can distinguish an
accidental from a nonaccidental trau-
ma,31 but the likelihood of abuse in-
creases when there is a fracture in a
nonambulatory child and when the
fracture type includes the femur or hu-
merus in infants who are younger than
18 months.31,33,34 Indeed, in this study,
these types of fractures in nonambula-
tory children were commonly seen in
cases for which abuse was missed. Inaddition, many of the missed extremity
fractures had associated risk factors
for abuse that were not adequately
screened for at the initial physician
visit; therefore, the possibility of abuse
should be carefully considered for
children with extremity fractures, and
associated risk factors should be
excluded.
An abuse-related fracture was almost
twice as likely to be missed in a boyversus a girl. Although the reason for
this is unclear, injuries in general oc-
cur more often in boys,35 which may
bias a clinician in assuming that the
cause of a fracture is accidental.
This study has limitations that warrant
consideration. This was a retrospec-
tive study with its inherent limitations,
such as missing data, and thus absent
data may have biased predictor vari-
able results. Although our case classi-fication was based on current avail-
able standards for the diagnosis of
abuse, there may have been ascertain-
ment errors. Children with abusive
fractures that were never referred to
the SCAN team and were assumed to
be accidental were not included in this
review; however, given that ED records
are often incomplete,1 a retrospective
assessment by the child protection
team of all of the nonreferred caseswould have resulted in only specula-
tive assignments of cause. Finally, al-
though most cases of abusive frac-
tures are seen by our SCAN team, some
of the less complex cases may not have
been seen. This introduces the poten-
tial for referral bias, and it may result
in an overestimation of the proportion
of cases that are missed at an initial
physician visit; however, child abuse is
underrecognized,12 and there is also
the possibility that we are underesti-
mating the proportion of casesmissed.
CONCLUSIONS
Our results suggest that a consider-
able proportion of abuse-related pedi-
atric fractures are missed during the
initial visit. We can make the following
suggestions that may facilitate the di-
agnoses of abusive fractures. A de-
tailed review of the mechanism and
screening for other risk factors ofabuse should be included in the initial
assessment of a young child with frac-
tures. Children who are nonambula-
tory are at especially high risk, and
consultation with the child protection
team in these cases is often appropri-
ate. Clinicians should have a low
threshold to perform a skeletal survey
in potentially vulnerable populations,
and a radiologists review of any imag-
ing that may change suspicion forabuse is recommended. Finally, appro-
priate targeted education or practice
guidelines may help in achieving bet-
ter outcomes in clinical settings that
are susceptible to missing abusive
fractures.
ACKNOWLEDGMENTS
This research was supported by a
grant from the Canadian Hospitals In-
jury Reporting and Prevention Pro-
gram (CHIRPP).
We acknowledge the efforts of Dr S.
Walter and Mr A. O. Odueyungbo for
statistical expertise and critical review
of the analysis.
ARTICLES
PEDIATRICS Volume 125, Number 1, January2010 65at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
8/9
REFERENCES
1. Oral R, Blum KL, Johnson C. Fractures in
young children: are physicians in emer-
gency departments and orthopedic clinics
adequately screening for possible abuse?
Pediatr Emerg Care. 2003;19(3):148153
2. Taitz J, Moran K, OMeara M. Long bone frac-
tures in children under 3 years of age: is
abuse being missed in emergency depart-
ment presentations? J Paediatr Child
Health. 2004;40(4):170174
3. Banaszkiewicz PA, Scotland TR, Myerscough
EJ.Fractures in children younger than age1
year:importanceof collaboration withchild
protection services.J Pediatr Orthop.2002;
22(6):740744
4. Lane WG, Dubowitz H. What factors affect
the identi fication and reporti ng of child
abuse-related fractures? Clin Orthop Relat
Res.2007;461:219225
5. Leventhal JM. The field of child maltreat-ment enters its fifth decade. Child Abuse
Negl.2003;27(1):1 4
6. Leventhal JM, Thomas SA, Rosenfield NS,
Markowitz RI. Fractures in young children:
distinguishing child abuse from uninten-
tional injuries. Am J Dis Child. 1993;147(1):
8792
7. Johnson CF, Oral R.Diagnosis and Manage-
ment of Child Abuse of Children. Columbus,
OH: Ohio State University Print Shop; 1999
8. Lane WG, Rubin DM, Monteith R, Christian
CW. Racial differences in the evaluation of
pediatric fractures of physical abuse.JAMA.2002;288(13):16031609
9. Akbarnia B, Torg JS, Kirkpatrick J. Manifes-
tation s of the battered child syndrome.
J Bone Joint Surg Am. 1974;56(6):1159
1166
10. Fong CM, Cheung HM, Lau PY. Fractures as-
sociated with non-accidental injury: an or-
thopaedic perspective in a local regional
hospital. Hong Kong Med J. 2005;11(6):
445451
11. Worlock P, Stower M, Barbor P. Patterns of
fractures in accidental and non-accidental
injuries in children: a comparative study.Br Med J (Clin Res Ed). 1986;293(6539):
100102
12. Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay
TC. Analysis of missed cases of abusive
head trauma [published correction ap-
pears inJAMA.1999;282(1):29].JAMA.1999;
281(7):621626
13. Kleinman PK. Diagnostic Imaging of Child
Abuse. 2nd ed. St Louis, MO: Mosby; 1998
14. Kleinman PK, Marks SC Jr, Richmond JM,Blackbourne BD. Inflicted skeletal injury: a
postmortem radiologic-histopathologic
study in 31 infants. AJR Am J Roentgenol.
1995;165(3):647 650
15. Statistics Canada. Census Tract Profiles,
2006 Census. Ottawa, Ontario, Canada; 2006.
Available at: www12.statcan.ca/english/
census06/data/profiles/ct/Index.cfm?
LangE. Accessed August 8, 2008
16. Statistics Canada. Study: Income Inequal-
ity and Redistribution. Ottawa, Ontario,
Canada; 2007. Available at: www.statcan.
gc.ca/daily-quotidien/070511/dq070511b-
eng.htm. Accessed September 12, 2008
17. Heisz A. Income inequality and redistribution;
1976 to 2004. Analytical Studies Branch Re-
search Paper Series.2007;(298):158
18. dos Santos LM, Stewart G, Meert K, Rosen-
berg NM. Soft tissue swelling with fractures:
abuse versus nonintentional. Pediatr Emerg
Care.1995;11(4):215216
19. King WK, Kiesel EL, Simon HK. Child abuse
fatalities: are we missing opportunities for
intervention. Pediatr Emerg Care. 2006;
22(4):211214
20. Fung KY, Wrobel BA. The treatment of miss-
ing values in logistic regression. Biometri-cal Journal.2007;31(1):35 47
21. Hsieh FY. Sample size tables for logistic re-
gression.Stat Med. 1989;8(7):795802
22. Dalton HJ, Slovis T, Helfer RE, Comstock J,
Scheurer S, Riolo S. Undiagnosed abuse in
children younger than 3 years with femoral
fracture.Am J Dis Child.1990;144:875878
23. Trokel M, Wadimmba A, Griffith J, Sege R.
Variation in the diagnosis of child abuse in
severely injured infants [pubished correc-
tion appear s in Pediatrics. 2006;118(3):
1324].Pediatrics.2006;117(3):722728
24. Kleinbaum DG, Kupper LL, Muller KE, NizamA. Applied Regression Analysis and Other
Multivariable Methods. 3rd ed. Pacific
Grove, CA: Brooks/Cole Publishing Company;
1998
25. Bagley SC, White H, Golomb BA. Logistic re-
gression in the medical literature: stan-
dards foruse andreporting,with particular
attention to one medical domain.J Clin Epi-
demiol. 2001;54(10):979985
26. Concato J, Feinstein AR, Holford TR. The risk
of determining risk with multivariable mod-
els.Ann Intern Med.1993;118(3):201210
27. Peduzzi P, Concato J, Kemper E, Holford TR,
Feinstein AR. A simulation study of the num-
ber of events pervariable in logistic regres-
sion analysis.J Clin Epidemiol.1996;49(12):
13731379
28. Oral R, Yagmur F, Nashelsky M, Turkmen M,
Kirby P. Fatal abusive head trauma cases:
consequence of medical staff missing
milder forms of physical abuse. Pediatr
Emerg Care.2008;24(12):816 821
29. Ryan LM, DePiero AD, Sadow KB, et al. Rec-ognition and management of pediatric frac-
tures by pediatr ic resid ents. Pediatrics.
2004;114(6):15301533
30. Chung S, Schamban N, Wypij D, Cleveland R,
Schutzman SA. Skull radiograph interpreta-
tion of children younger than two years:
how good are pediatric emergency physi-
cians?Ann Emerg Med. 2004;43(6):718722
31. Kemp AM, Dunstan F, Harrison S, et al. Pat-
terns of skeletal fractures in child abuse:
systematic review.BMJ.2008;337:a1518
32. Ziegler DS,Sammut J, Piper AC.Assessment
and follow-up of suspected child abuse inpreschool children with fractures seen in a
general hospital emergency department.
J Paediatr Child Health. 2005;41(56):
251255
33. Leventhal JM, Martin KD, Asnes AG. Inci-
dence of fractures attributable to abuse in
young hospitalized children: results from
analysis of a United States database. Pedi-
atrics.2008;122(3):599 604
34. Loder RT, Feinberg JR. Orthopaedic injuries
in children with nonaccidental trauma: de-
mographics and incidence from the 2000
kids inpatient database. J Pediatr Orthop.
2007;27(4):421426
35. Cramer KE, Scherl SA. Orthopedic Surgery
Essentials: Pediatrics. Philadelphia, PA: Lip-
pincott Williams & Wilkins; 2003
66 RAVICHANDIRAN et alat Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/ -
8/10/2019 Pediatrics 2010 Ravichandiran 60 6
9/9
DOI: 10.1542/peds.2008-3794
; originally published online November 30, 2009;2010;125;60PediatricsShouldice, Hosanna Au and Kathy Boutis
Nisanthini Ravichandiran, Suzanne Schuh, Marta Bejuk, Nesrin Al-Harthy, MichelleDelayed Identification of Pediatric Abuse-Related Fractures
ServicesUpdated Information &
lhttp://pediatrics.aappublications.org/content/125/1/60.full.htmincluding high resolution figures, can be found at:
References
l#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.htmat:This article cites 28 articles, 5 of which can be accessed free
Citations
l#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.htmThis article has been cited by 14 HighWire-hosted articles:
Subspecialty Collections
e_neglect_subhttp://pediatrics.aappublications.org/cgi/collection/child_abusChild Abuse and Neglectthe following collection(s):This article, along with others on similar topics, appears in
Permissions & Licensing
mlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhttables) or in its entirety can be found online at:Information about reproducing this article in parts (figures,
Reprintshttp://pediatrics.aappublications.org/site/misc/reprints.xhtml
Information about ordering reprints can be found online:
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.Grove Village, Illinois, 60007. Copyright 2010 by the American Academy of Pediatrics. Alland trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elkpublication, it has been published continuously since 1948. PEDIATRICS is owned, published,PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
at Indonesia:AAP Sponsored on June 22, 2014pediatrics.aappublications.orgDownloaded from
http://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/content/125/1/60.full.html#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.html#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.html#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/site/misc/reprints.xhtmlhttp://pediatrics.aappublications.org/site/misc/reprints.xhtmlhttp://pediatrics.aappublications.org/site/misc/reprints.xhtmlhttp://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/http://pediatrics.aappublications.org/site/misc/reprints.xhtmlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/site/misc/Permissions.xhtmlhttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/cgi/collection/child_abuse_neglect_subhttp://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.html#related-urlshttp://pediatrics.aappublications.org/content/125/1/60.full.html#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.html#ref-list-1http://pediatrics.aappublications.org/content/125/1/60.full.htmlhttp://pediatrics.aappublications.org/content/125/1/60.full.html