Pediatric Seating and Mobility · 2020‐04‐03 4 Ameria Video 10 Before and After 11 Goals Of...
Transcript of Pediatric Seating and Mobility · 2020‐04‐03 4 Ameria Video 10 Before and After 11 Goals Of...

2020‐04‐03
1
Pediatric Seating and MobilityEvaluation to Delivery
2
Sally Mallory, PT, ATP, CPST214-763-9173
Thank you to our contributors• All of the children and their families, caregivers and therapists
• Missy Ball, PT
• Sally Mallory, PT, ATP, CPST
• Jo McConnell, PT
• Bente Storm, PT
• Helle Rasmussen, PhD, PT
• Lynda Reagan, PT
• Megan Salley, MOTR/L
• Elaine Westlake, PT, DPT, MA
• Julie Kobak, MA, CCC-SLP
1
2
3

2020‐04‐03
2
4
5
Our family of products
4
5
6

2020‐04‐03
3
Team approach
child
Family
Therapists
Equipment Specialist
Teachers
Manufacturer
8
The Seating Process
Referral
Client Interview
Physical Assessment
Determination of Equipment
Measurement and Translation to Equipment Choices
Simulation
Prescription with Letter of Medical Necessity
Follow-Up
Ordering and Assembling
Delivery, Check Out, Training
Client Interview• General Information
• Medical History
• Environmental Accessibility
• Client / Caregiver Goals
• Existing Mobility Equipment Issues
• Transportation
• Self-management Skills
• Funding
7
8
9

2020‐04‐03
4
Ameria Video
10
Before and After
11
Goals Of Seating
• Promote normal skeletal alignment & accommodate structural issues
• Promote functional posture & movement
• Facilitate balance in muscle tone
• Promote healthy skin
• Consider comfort & future growth/changes of client
• Promote healthy physiological functioning
• Promote greatest independence in ADL/mobility
• Accessibility in client environments & easy transport
10
11
12

2020‐04‐03
5
3
• Always start with a stable base
o Stable base (pelvis, thighs and feet)
o Balance (trunk, shoulders and head)
o Mobility (head, arms and hands)
Create a Good Functional Sitting Position
Skeletal alignment/mobility
ROM limitations
Neuro-motor status (muscle tone)
Primitive reflexes
Movement abnormalities
Muscle strength/endurance
Sensory issues
Respiratory/cardiovascular issues
Bowel/bladder management
Activities of daily living
Skin integrity
Mat Assessment
Mat Assessment
15
13
14
15

2020‐04‐03
6
Mat Assessment
16
17
Mat Assessment
18
Mat Assessment
16
17
18

2020‐04‐03
7
2
Skeletal Alignment• Typical alignment and considerations
o Child and adult
• Atypical alignment
o Causes and possible solutions
Skeletal System: Child Spine
Birth• 270 cartilaginous bones• Spine-kyphotic
Birth to 3 years• 1 month- cervical lordosis• 12-15 months- pseudo lumbar lordosis• 3 years- true lumbar lordosis
11-19 years• 75% of height attained• 50% of adult weight• Bone ossification complete by 20 year
20-25 years• 206 bones calcified
Spinal Column Development
2
19
20
21

2020‐04‐03
8
2
• Pelvis influences spine
• Lower extremity alignment influences pelvis
• Influence pelvis thru sacrum not lumbar spine
• Maintain normal curves of spine
• Head balances on spine
• Holistic approach
Skeletal System: Adult Spine
Normal Seated Posture
2
Pelvis and Spine Issues
2
Lordosis Kyphosis Scoliosis
22
23
24

2020‐04‐03
9
Anterior Tilt
Pelvic Tilt: Goal is NeutralNeutral Posterior Tilt
Neutral Posterior tilt
• Sacral sitting, increases pressures
• Pelvic floor muscles off
• Respiratory compromise
• Increases kyphosis, decreases lordosis
• Decreases visual field
• Neck hyperextension
• Swallow difficulty
• Upper extremity function compromise
2
Posterior Pelvic Tilt: Problems
Factors Changing Pelvic Tilt
If the seat is too deepIf the child has limited hip flexionIf spasticity is very strong
If abduction/external rotation of the hip
If hyper lordosis with tight hamstringsIf the foot plate is mounted too high
25
26
27

2020‐04‐03
10
Posterior Pelvic Tilt
• Undercut seat• Front rigging angleLimited ROM hamstrings
• Head placement in space• Tilt in Space frame• Support/stabilize pelvis and torso
Abnormal Reflexes: TLRLow tone
Muscle weakness/paralysis
• Reduce seat depth
Seat depth too long
• Small child ½” webbing• Below ASIS 45-60 angle 2pt., 4pt beltPelvic belt location or web size
Causes Possible Solutions
Posterior Pelvic Tilt
• Pelvic Harness• 4 point pelvic belt• Anti-thrust seat• Dynamic back
Extensor thrust
• Open seat to back angle• Custom cut seat
Limited hip flexion
• Caution with tight hamstrings• Change to non-elevating leg rests• Lumbar support, check seat depthElevating leg rests
Causes Possible Solutions
2
• The seat depth must be from the back of the pelvis to about 2 fingers width from the hollow of the knee sitting on a flat or backward tilted seat
• If the seat is tilted forward, the seat depth must be shorter, because the feet then will be pulled a little backwards
Seat Depth & Support Through Thighs
28
29
30

2020‐04‐03
11
• Hip belt always a must for stable positioning (2 point or 4 point)
• Strap mounting
o One in front of the greater trochantero One behind the greater trochanter
• Important to mount the straps as close to the child's body as possible
Pelvic Positioning
2
Pelvic Positioning• Pelvic (sit on) harness
• The child sits on the harness
• Comes up between the legs and is mounted with the straps ~45˚to the back of the seat
• Good alternative to the 4 point belt for the smaller children
33
Case Study
• Posterior Pelvic Tilt/Kyphosis
• Promote neutral pelvis
o Pelvic belto Anti thrust seat
• Trunk 2 point control
o Thoracic cue: Convaid R82 butterfly vest
o Chest support
• Wheel placement
• Tray
Photos courtesy of Missy Ball, PT
31
32
33

2020‐04‐03
12
Anterior Pelvic Tilt
• Effective placement of pelvic belt
• Capture pelvis with seat shape
• Belly binder• UE & Chest support
Flexible
• Custom molded or shaped back
Structural
Possible Solutions
Client with ArthrogryposisPhoto courtesy of Missy Ball, PT
Pelvic Positioning
4
Pelvic Rotation Pelvic Normal Pelvic Obliquity
Pelvic Positioning: Solutions
The anti thrust seat is designed to prevent the pelvis from sliding forward
An anti-thrust seat gives space for the ischial tuberosities as they are about 1 inch deeper into the cushion than the thighs
Laterals for the pelvis and thighs give stability and symmetryAbduction supports keep the knees in neutral alignment and can reduce tone
34
35
36

2020‐04‐03
13
Pelvic Positioning: Anti-thrust
Pressure mapping of a 3cm cushion on a flat surface
Pressure mapping of the same 3 cm cushion, but with wedges to build up the front of the seat
• Causes
o Imbalance of spinal musculature
o Asymmetrical tone
o ATNR
o Pelvic obliquity
o Muscle paresis/paralysis
2
Scoliosis
• Flexible:
o 3 point lateral trunk & hip support system
o Subtle curved back with lateral supports
• Structural:
o For mild/moderate- severe
o Grid back, foam in place, custom molded back
Scoliosis Solutions
Holmes, et al. Management of scoliosis with special seating for the non-ambulant spastic CP population- a biomechanical study. Clin Biomech, Jul 2003 18(6):480-487.
37
38
39

2020‐04‐03
14
Scoliosis Solution: 3-point Principle
Flexible Pelvis in balance
Rigid Pelvis in balance
Head in balance
Photos courtesy of Missy Ball, PT
2
• The back cushion can be built up with wedges or trunk supports to give support and to help the child stay in midline
• A lumbar support for smaller children is not needed (before three years old) because they have not developed a normal lumbar curve. For older children, lumbar support may assist in positioning the child correctly
Scoliosis Solution: Contoured Back Cushion
Scoliosis Solution: Multiple Adjustments
Lateral thoracic supportsWidth adjustment-minimum 6”chest width
Back height adjustment
40
41
42

2020‐04‐03
15
Scoliosis Solution: Lateral Trunk Supports
Swing away supports Fixed supports
• Shoulder straps should always pull from shoulder height or above
• Back pack straps: Static or dynamic; no abdominal contact
• Butterfly: Sternum pull only, clavicle pads slip
• H-strap: Clavicle pull with anterior buckle for alignment
• Full thoracic: Sternum input, anterior chest pull, clavicle pull, g-tube clearance, consider breast relief
• Strap risers: For headrest clearance and proper posterior pull
• Cross Vest:
Solutions: Anterior Chest Supports
• Can facilitate symmetry
• Can create stability for head and trunk alignment
• Angling of the tray may improve the alignment of the upper body and may be used for the visually impaired
Solutions: Tray
43
44
45

2020‐04‐03
16
Solutions: Trunk Control & UE Assistance
Upper Arm Supports
Overarm Supports Chest Vest
Tray Height and Angle Adjustable Armrests
Lower Extremity Range of Motion
• Seat to back angle• Frame choice• Seat options
Hip: Flexion limitations(Hip extensor flexibility)
• Front rigging angle• ClearanceKnee: Popliteal angle (Hamstring
flexibility)
• Overall chair depth• Adjustable foot plate, foot choicesAnkle: ROM/Orthotics (Calf
muscle flexibility)
Joint Issues Chair Considerations
Lower Extremity Issues
• Medial/lateral thigh padsWindswept lower extremities
• Open seat to back angle• Custom split seatPainful hip
• Open seat to back angle• Custom split seatDislocation/subluxation
• Asymmetrical seat depthLeg length discrepancy
• Medial thigh padExcessive adduction
• Lateral thigh pad• Adjustable foot plate, foot choicesExcessive abduction
Problems Solutions
46
47
48

2020‐04‐03
17
Lower Extremity Research• Robb, Hägglund (2013). Hip surveillance and management of the displaced hip in cerebral palsy. J
Child Orthop Nov 7(5): 407–413.
• Hip dislocation may be preventable
• Early surveillance program includes:
• Radiography
• Clinical Examination
• Preventive Positioning
• Reimer’s Migration Percentage (MP)
• MP > 30-33°= hip displacement
• MP > 90-100°= hip dislocation
• MP > 33 consider hip surgery
• Hip displacement is directly related to GMFCS levels
Lower Extremity Research• McLean, et. al. Positioning for Hip Health: A Clinical Resource, Sunny Hill Heath Centre for Children
BC, Canada
• Position in HIP ABDUCTION + HIP EXTENSION for hip health
• Positions: supine, sitting, standing & walking
5 months-2 years
• Sitting:• Hip
Abduction 15-30o
• Hip ER 5-15o
• Per tolerance
2-6 years
• Sitting• Hip
Abduction 15-30o
• Hip ER 5-10o
• Per tolerance up to 6 hr/day
6 years-skeletal maturity
• Sitting• Hip
Abduction 15-30o
• Hip ER 5-10o
• Per feeding, FM, mobility needs
Lower Extremity: Windswept
49
50
51

2020‐04‐03
18
Lower Extremity: Scissoring or Excessive Adduction
Lower Extremity and Hip Alignment Options
Trekker Width Adjustable Pelvic & Lateral Thigh Support With/Without
Armrests
Rodeo Align Cushion Cruiser or Rodeo Position Cushion
EZ Rider Lateral Thigh Support
EZ Rider Medial Thigh Support
Lower Extremity Solution: Cushion
2
52
53
54

2020‐04‐03
19
• Hip abduction/adduction
• Seat depth differences
• Lateral trunk pads
• Lateral and medial thigh pads
• Seat depth and width
• Back height and width
55
Solutions: Multi-Adjustablex:panda
Solutions: Multi-Adjustable
Swing-awaylaterals
Fixed Laterals Hip ABD/ADD Seat depth differences
Foot Position
• Width and depth is important
• Single or parted foot plate
55
56
57

2020‐04‐03
20
• Muscle weakness• Forward flexion
• Capital hyperextension
• Forward flexion with rotation and/or lateral flexion
• ATNR: Rotation & asymmetrical extension
• Extensor Thrust• Head trigger
• Head Banger
• Head Shape/Size Abnormal
Head Issues
Solutions: Head Rests• Provide support
• Create symmetry
• Provide stable base
• Correct and maintain position
• Mount switches
• R82- 18 headrest options
Seating Challenges
58
59
60

2020‐04‐03
21
2
Motor Function• Postural Stability
o Maintains the center of body (COM) over the base of support
• Postural Orientation
o Provides appropriate relationship between body parts to the environment for a task
• Quality of posture
o Determines motor skill capabilityMovement
Posture
Position vs. Posture
Position
Static
Muscle inactive
Absent response to sensory input
Focus: Skeletal alignment & pressure distribution
Function not enhanced
Posture
Dynamic
State of readiness
Sensory responsive; adaptive
Focus: Skeletal mobility & motor function
Function enhanced
Postural Control: Interrelationship
2
61
62
63

2020‐04‐03
22
The Challenge• Seating specialist
o Promote optimal postural alignment without restricting movement potential and the flow of sensory information for postural control
• Manufacturer
o Develop more fluid systems, that interact & are responsive to client’s changing postural needs for movement in functional tasks
Components of Postural Control
Posture
Musculoskeletal
Neuromotor
SensorySystems
SensoryMotor
Strategies
CognitiveInfluence
Internal Maps
3
• Tone Types: Floppy, spastic, rigid, athetoid, ataxic
• Dynamic Joint Stiffness o Force Generationo Grading Force (scaling)
• Balance in Muscle Execution o Co-activationo Reciprocal inhibition
• Muscle Contraction o Initiate, Sustain, Terminate
• Coordinationo Sequencing & Timing
• Muscle Synergyo Coupling muscles for task
Neuromotor Status: Muscle Tone & Coordination
Posture
Musculoskeletal
Neuromotor
SensorySystems
SensoryMotor
Strategies
CognitiveInfluence
Internal Maps
64
65
66

2020‐04‐03
23
Motor types
Neuromotor Status• Muscle Tone= force which a muscle resists being lengthened
• Hypotonic - Floppy• Poor force generation or scaling• Poor sustainability• Limited control of termination• Poor co-activation & reciprocal inhibition• Limited coordination
69
Neuromotor Status• Hypertonic – Spastico Imbalance of muscle activity about jointo Poor ability to grade & scale forceo Coordination limited
67
68
69

2020‐04‐03
24
Sensory Systems Influencing Posture
Visual • Visual reference to space and objects
Auditory • Sound waves identify objects distance to client
Somatosensory-Tactile
• Discriminations shape/texture• Helps body adapt to environmental changes• Deep pressure, touch, vibration, pain
Somatosensory-Proprioception
• Provides info for body schema/position sense• Provides info for timing/speed of movement• Helps plan, learn and remember movement
Vestibular
• Provides info on body orientation to gravity• Provides info on speed, direction of head motion• Influences tone, equilibrium, arousal, bilateral coordination,
directionality
Posture
Musculoskeletal
Neuromotor
SensorySystems
SensoryMotor
Strategies
CognitiveInfluence
Internal Maps
Sensory: Seating Choices• Frame orientation
Visual
• Head support not blocking ears
Auditory
• Back seat shape• Upholstery material/texture• Medium
Somatosensory
• Frame orientation, tilt, recline
Vestibular
Case Study: Kye• 10 years old
• Dravet Syndrome
• Seizure disorder
• Needs
o Low tone, crouched gait, ambulation fatigue
o Sensory-processing issues, easily overstimulated, stress induced seizures
o Post-ictal state, reduced responsiveness, requires oxygen
70
71
72

2020‐04‐03
25
Convaid Rodeo
• Provides for:
o Postural support
o Security, reduced stimulation
- Harness
- Oversized canopy
oMedical needs
- Recline post-ictal
- Medical basket for O2
73
Seating Solution
Sensory Input & Feedback• Critical for motor development
• Feedback: Sensory used to modify motor output to hit mark
• Feed-forward: Postural adjustments made in anticipation of actual task requirements
• Individuals learn movement and postural adjustment through feedback, then perform them with feed-forward for automatic or habitual movements
Seating choices
Allow some movement potential in
system
2
• Typical Development
• Atypical Development
Sensory Motor Strategies = Motor Development
PosturePosture
MusculoskeletalMusculoskeletal
Neuromotor Neuromotor
SensorySystemsSensorySystems
SensoryMotor
Strategies
CognitiveInfluenceCognitiveInfluence
Internal Maps
Internal Maps
73
74
75

2020‐04‐03
26
• For the first 3-5 month
oMidline orientation
oHead raising/extension
oRotation within the body
o Extension and abduction of limbs
o Equilibrium reactions in prone and supine
Typical Motor Development
Typical Motor Development• 6-7 months: Ring sit• Sit without UE support• Good head & trunk control• UE free to explore toys & environmento Visual perceptualo Visual spatialo Aids cognitive development o Aids feeding independentlyo Oral motor development precursor to speech acquisition
• Muscles controlling pelvis active:o Hip extensors and oblique abdominalso Control weight shift across pelvis
R82.com
Less experienced sitter More experienced sitter
Typical Motor Development
78
• From 6-10 month
o Active stable base
o Spine in a straight line
o Body and head balanced and hands free
o This posture requires the least amount of effort to maintain the position
76
77
78

2020‐04‐03
27
Motor Development
1m• Cervical extension
3m• Prone on forearms• Midline orientation
4m• Lumbar extension “swimming”
6m• Hip ext/abdominals active• Sitting without UE support• Weight shift across pelvis• LE dissociation
Typical Atypical1m
• Lack effective cervical extension
3m•Neck/head hyperextension & shoulder elevation•Lack thoracic extension
4m•Humeral ext/add/IR used for spinal extension•Prone: lack humeral flex/ER to prop on elbow
6m•Weak oblique abdominals & hip extension•Poor sitting base•Poor weight shift at pelvis•Limited LE dissociation•Rectus abdominus short, rocks pelvis posterior & LE extend•Poor stability in shoulder & pelvis girdles
Capital Hyperextension Shoulder Extension & Internal Rotation/Adduction
80
Atypical Development
Photos courtesy of Missy Ball, PT
81
Solution
Angle adjustable tray with elbow blocks to promote effective weight bearing & shoulder girdle synergy
79
80
81

2020‐04‐03
28
82
Atypical Development
83
• Unable to manage weight shift at pelvis which is key to postural control
• Poor sitting base
• Poor pelvic weight shift
• Weak oblique abdominals
• Weak hip & spinal extension
• RA short, pulls pelvis posterior
• LE react in extension
Atypical Development
• Anterior Tilt
oMuscle re-education and strengthening
o If client cannot actively manage pelvis, then support through seating system options (Myhr von Wndt 1991; Cherng et al. 2009)
84
Atypical Development: Solution
82
83
84

2020‐04‐03
29
Atypical Development: Solution
• Anterior Tilt
o Can be achieved with Trekker, Flyer, Kudu, Wombat
o Promotes:
Functional pelvic synergy/active sitting
Fine motor activities
Feeding
Speech
• Head control
• Trunk control
• Sitting balance
• Fine motor capability
• Transfer capability
• Ambulation capability or limitations
• Pressure relief capability
• Self care skills: feeding, dressing, toileting
2
Motor Capability Assessment
Other Considerations• Physiologic Systems
o Respiratory Status Ventilator needs within life of new chair
o Renal/Bladder
o GI Issues Reflux Bowel (e.g. voiding, constipation, absorption)
o Skin Issues
• Vision
• Cognitive Status
85
86
87

2020‐04‐03
30
Case Study: Madi
88
• 4 years old
• 5q14.3 Microdeletion Syndrome
• Developmental Delays
• Low tone in her trunk and neck with high tone in her UE and LE
• Extensor tone
• G-tube fed
• Visual deficits
89
Case Study: Madi
90
88
89
90

2020‐04‐03
31
91
The Seating Process
Referral
Client Interview
Physical Assessment
Determination of Equipment
Measurement and Translation to Equipment Choices
Simulation
Prescription with Letter of Medical Necessity
Follow-Up
Ordering and Assembling
Delivery, Check Out, Training
Product Application• Identify Major Client Problems
• Structural or flexible issues• ROM limitationsSkeletal
• Abnormal muscle tone, muscle weakness• Abnormal movement strategies• Sensory issues
Posture/Movement
• Bowel/bladder management• TransfersADL or Self Care
• Respiratory (vent)• Gastrointestinal (g-tube)• Skin
Other
• Home, school, work• TransportationClient Environment
Seating Goals Specific to Client Needs
• Promote normal skeletal alignment & accommodate structural issues
• Promote functional posture & movement
• Facilitate balance in muscle tone
• Promote healthy skin
• Consider comfort & future growth/changes of client
• Promote healthy physiological functioning (RS, CV, GI)
• Promote greatest independence in ADL/mobility
• Accessibility in client environments & easy transport
91
92
93

2020‐04‐03
32
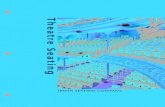
Measurements Critical for Equipment Choices
A. Shoulder
B. Chest Width
C. Hip Width
D. Width at Knee
E. Seat to Top of Head
F. Seat to Top of Shoulder (L,R)
G. Seat to Axilla (L,R) Armpit
H. Chests Dept (L,R) Back to Tip of Chest
I. Seat Dept (L,R) Actual- 2-3 Fingers
J. Seat to Footplate (L, R)
95
96
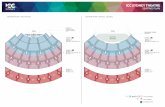
• Frame Choice:
• Power Wheelchair
• Manual Wheelchair
o Dependento Self propelling
• Tilt-in Space
• Recline
• Combination
• Dynamic
Translate Client Measurements & Goals Into Equipment
94
95
96

2020‐04‐03
33
Early Mobility: Why?• Immobility associated with learned helplessness
• Established by age 4yr in children without functional mobility (Butler, 1991; Safford & Arbitman, 1975; Lewis & Goldberg, 1969)
• Decreased curiosity & initiative
• Poor academic achievement
• Poor social interaction skills (Kohn, 1977)
• Passive, dependent behavior
• Lack object permanence
• Dependent on vision to control posture (Bai & Berenthal, 1992)
• Poor visual spatial skills and memory (map testing difficult)
Independent Mobility: Why?
A child usually explores the environment through crawling about 9-10 months of age
This experience increases sensory input of vestibular, visual & somatosensory systems as body moves
Increases trial & error: coupling of motor output to specific task
Increases cognition through problem solving for barriers & visual spatial issues
For the child needing assistance - walkers, gait trainers and wheeled standers need to be used as soon as developmentally appropriate
For the non-mobile or non-ambulatory child, self propulsion with manual WC or power WC should be considered as early as 10-15 months if they have potential to be independent
Dependent Mobility: When?
99
Client is unable to self propel a manual WC
Family does not have vehicle to transport a power chair or financial means to purchase appropriate vehicle
Family not interested in power WC presently
Environmental limitations: Home layout
2nd floor apartment
Daycare does not allow power mobility in center
97
98
99

2020‐04‐03
34
Tilt and/or Recline: Rationale• Realign posture and enhance function
• Enhance visual orientation, speech, alertness, and arousal
• Improve physiological processes orthostatic hypotension, respiration, bowel/ bladder function
• Improve transfer biomechanics
• Regulate spasticity / muscle tone by changing joint angles
• Accommodate/prevent contractures and orthopedic deformity
• Manage edema
• Pressure management
• Increase seating tolerance /comfort
• Independently change position to allow dynamic movement
Tilt In Space
• Allows change in orientation to gravity
• No change in Seat to Back angle
• No change in relationship of client to seating components
Orientation of Seating System in Space
Standard Recline
• Allows change in orientation to gravity
• Change in Seat to Back angle
• Linear and Angular change in relationship between seating components and client
102
Orientation of Seating System in Space
100
101
102

2020‐04‐03
35
Tilt in Space: Posterior • Pressure relief
• Assist with skeletal alignment
• Promote functional posture
• Promote effective physiological function
o Orthostatic hypotension, GE reflux, respiration, digestion
• Aid feeding/swallow (Tilt 5-30°)
• Assist with venous return insufficiency or edema
• Aid in transfers
• Provide comfort
Pressure Relief• TS and Recline affect pressure/perfusion of skin and muscle tissue at ischial tuberosity, less at
sacrum.
• Tilt used alone, >25° to achieve pressure relief and/or tissue perfusion at ischial tuberosity
• Recline 120o + ELR significantly reduced pressure
• Greatest reductions in pressure with combination
o Tilt of 35° with recline 100°
o Tilt of 25° with recline of 120°
• Greater angles = greater pressure relief
Tilt in Space: Posterior• 45o posterior tilt
• Rodeo without seating can accommodate third party seating
103
104
105

2020‐04‐03
36
• Stingray
o Tilt in space 0-45o
o Full recline
o 180o turn-able seat
Tilt in Space: Posterior
• Increase muscle strength in spine/ hip extensors for functional pelvic synergy
• 95% functional tasks occur here
• Speech production, intelligibility, & feeding (Costigan & Light, 2011)
• Improvement in respiration (FVC) spastic CP (Shin, Byeon, & Kim 2015)
• Improvement in vital capacity & forced expiratory volume (Mac Neela, 1987; Nwaobi & Smith, 1986)
• Assists in transfers
Tilt in Space: Anterior
TrekkerTilt in Space (-10 to 45o)
Recline (170o)
Central Gravity Axis Tilt • Greater stability in full tilt
• Aligns center of gravity with center of rotationo Maintains client’s mass within the center of the frame
• Greater environmental accessibility - smaller footprinto Access to tabletop activities
• Less weight transferred to casters when upright o Reduces energy to push chair & caster repair issues
• Excellent frame for clients with sensory processing issues, extensor thrust, LE spasms, obesity
106
107
108

2020‐04‐03
37
Central Gravity Axis Tilt
Convaid FLYER Extremely lightweight WC19 tested
110
• Lightness of a stroller with growth & seating of a WC
• 5° Anterior Tilt- 40° Posterior Tilt
• Growth through Seat Pano 4” seat widtho 4” seat depth
• Accepts Convaid or After Market Seating
• Multiple wheel choices
• WC 19 crash tested
• Extremely lightweight; Portable base frame under 14 lbs.
• Seating without front rigging under 18 lbs.
Central Gravity Axis Tilt
Case Study: Justine• 5 years old
• Ehlers-Danlos, Hypotonia and Coordination Disturbance
• Frequent falls, skin breakdown and hypersensitivity of her integumentary system
• Decreased balance and strength after 15 minutes of ambulation without a device
• Current equipment:
o Scallop chair
o Carrot car seat for assistance in the car due to low back pain
o Rodeo
• Chokes with thin liquids unless environmental supports are in place
• Mom has same syndrome
109
110
111

2020‐04‐03
38
Convaid Rodeo Convaid Flyer
Case Study: Solutions
Case Study- Justine• Homeschooled- anterior tilt for table top activities
113
Crocodile Gait Trainer
Case Study: SolutionsCarrot Car Seat
112
113
114

2020‐04‐03
39
Uses for Recline• Management of bladder to avoid urinary retention
• Pressure management
• Postural hypotension/blood pressure (SCI)
• Respiratory compromise
• Limited hip flexion
• Increase sitting tolerances (CP, SMA, SCI)
• Comfort
• Daily needs: sleep, G-tube feedings, diapering, trach care
• Assist with transfers
• Manage edema or venous return insufficiency
Medicare and Medicaid Reimbursement Criteria
Tilt
Client at risk for developing pressure injury and unable to
perform functional weight shift
Increased or excessive muscle tone /spasticity related to a
medical condition that will not change for at least one year
Recline
Client at risk for developing pressure injury and unable to
perform functional weight shift
Client uses intermittent catheterization for bladder
management
Unable to transfer independently from W/C to bed
Used to manage increased tone or spasticity
Seating Challenges
117
115
116
117

2020‐04‐03
40
118
119
120
118
119
120

2020‐04‐03
41
Case Study: Hamza
Goals• Feeding goals/Visual scanning
Convaid R82 Chairs with Recline
123
Rodeo
Convaid
Trekker
Convaid
Flyer
Convaid
Stingray
R82
x:panda on Stingray base
R82
x:panda on Multi-Frame
R82
121
122
123

2020‐04‐03
42
Convaid R82 Tilt in Space & Recline
Posterior TS•Rodeo•Trekker•Flyer•Kudu•Stingray,•x:panda/multi-frame
Anterior TS•Trekker•Kudu•Flyer
Central Axis TS•Flyer•Kudu
Adjustable TS Full Recline
•Trekker•Flyer•Stingray
Partial Recline•Rodeo•Kudu•x:panda
Adjustable TS &
Recline
2
• Frame or seating components
• Possible uses:
o Extensor thrust /spasms
o Sensory processing issues
o Allow dynamic movement
o Reduce WC breakage
Dynamic Seating
Extensor Thrust
Hong, et al. (2006) Indentification of human-generated forces during extensor thrust. International Journal of Precision Engineering and Manufacturing. 7(3): 66-71.
124
125
126

2020‐04‐03
43
Extensor Thrust Effects
Patrangenaru, V. (2006) Development of Dynamic Seating System for High-tone Extensor Thrust. Georgia Institute of Technology.
• Materials and Method:
• 10 children
o 6-12 years old
o GMCFS Level V
• Seating system x:panda
• Evaluated o with a dynamic back
o with a static back
Research
Cimolin, et al. (2009) 3-D Quantitative evaluation of a rigid seating system and dynamic seating system using 3D movement analysis in individuals with dystonic tetra paresis. Disability and Rehabilitation: Assistive Technology: 4(4): 422-428.
x:panda Dynamic Back
Clients with extensor thrust or sensory processing issues
Dynamic Back:Can open or lock out
Recline: Pivot point near hip joint Less
Shear/Skin Deformation
127
128
129

2020‐04‐03
44
Data collection
Optoelectronic system
Passive markers
Pressure mapping
DynamicSession
5 sec pause
Clap
10 sec pause
Clap
10 sec pause
Clap
10 sec pause
StaticSession
5 sec pause
Clap
10 sec pause
Clap
10 sec pause
Clap
10 sec pause
• Head
• Torso
• Upper extremities
• Lower extremities
• 6 markers on the seat to represent the movement of the back
Position of Markers
Dynamic Static
2
Pressure Distribution Results
130
131
132

2020‐04‐03
45
Results & Impressions
• Greater ROM of head and trunk in the forward backward direction in dynamic configuration
• Greater ROM of trunk in vertical direction in static configuration meaning greater sliding of patient in static configuration
• Movements in UE’s larger in static versus dynamic configuration
Discussion
134
Demonstrates that the seating system in dynamic configuration improves the stability and the comfort of the users during the extensor thrust
The forward slide of the pelvis is limited significantly with the use of the dynamic system
In some subjects the movements of the upper limbs are more contained and more smooth while in the dynamic system
Case Study: Taylor• 8 years old with Cerebral Palsy
• Fluctuating muscle tone and has no independent sitting balance
• Tends to push through the backrest as part of his extensor pattern
• Mom has really struggled to position him well due to his high tone
• Mom struggled to hold his pelvis in previous seating like she had been shown by her OT
• Mom found getting harness and belt on was very difficult. She never had enough hands
133
134
135

2020‐04‐03
46
Postural Solutions
136
Dynamic Seating Solution
• Dynamic back provided Taylor with enough resistance while giving some ability for him to push back with his extensor tone
• Tilt and recline functions are specially designed to articulate around the hip and allows gravity to assist positioning.
• Taylor’s pelvic position was maintained and his spine was supported in neutral alignment.
• The lateral and head supports stayed in the desired position without any shear effect.
• Taylor was content and able to sit for longer periods and his Mom found it much easier to position him in his new seat.
Once Equipment Decision Made
2
Simulation with equipment if needed
Letter of Medical Necessity (LMN)•All parts specifically justified for client’s issues
LMN and prescription sent by Equipment Specialist to third party payer•Upon approval, re-measure as needed, equipment ordered and assembled
Delivery/Checkout with original seating team•To ensure all items are correct
Follow-Up
136
137
138

2020‐04‐03
47
Letter of Medical Necessity
139
Written by Professional
Paint a picture of the client
Detail present equipment problems and reasons it can no longer be used
Describe therapeutic goals for new equipment
Describe trials/use with this equipment and others if necessary
Include pictures if possible (videos for appeal)
Provide clinical reasoning for each line item of equipment that is being requested specific to client’s issues
Clearly state problems that will occur without the procurement of this equipment
Delivery/Checkout• Delivery occurs with original team present
• Check that all parts as per prescription are on the chair
• Ensure proper fit of client in new seating system
• Determine if seating goals have been met
• If problems arise, specify what will be done and timeline for its accomplishment
• If practice is needed (e.g. power mobility), set up therapy sessions
141
1. Go to: www.brainsbuilder.com
2. Select “Take an assessment”
3. Enter Your Assessment ID:
4. Enter Your Login: Convaid
5. Complete evaluation
6. Certificate of Completion will be sent to the email you provide in evaluation
Contact: Annette Hodges, [email protected]
Course Evaluation and
Certificate Instructions
139
140
141