Andrew Whitaker, Marianne Shaw, and Steven D. Gribble Presented By Steve Rizor.
Paul D. Brown, Michael D. Chan, Edward G. Shaw, and Martin J. … · 2015-10-07 · Paul D. Brown,...
Transcript of Paul D. Brown, Michael D. Chan, Edward G. Shaw, and Martin J. … · 2015-10-07 · Paul D. Brown,...

452
C H A P T E R
EPIDEMIOLOGIC AND ETIOLOGIC FINDINGSThe estimated annual incidence of low-grade gliomas in the United States is 2000 cases. Etiologic factors are unknown. These tumors are seen with increased frequency in patients with types 1 and 2 neurofibromatosis.
PATHOLOGIC FINDINGSThe most common pathologic types include pilocytic astrocy-toma (World Health Organization [WHO] grade I), diffuse fibrillary astrocytoma, oligoastrocytoma, and oligodendrogli-oma (WHO grade II).
BIOLOGIC CHARACTERISTICSCombined 1p and 19q deletions are associated with a superior outcome and are most common in oligodendrogliomas. TP53 mutations are more common in diffuse astrocytomas and are mutually exclusive from 1p/19q co-deletions. IDH1 mutations occur in the vast majority of low-grade gliomas and are found both in tumors with TP53 mutations and in tumors with 1p/19q codeletions.
CLINICAL MANIFESTATIONS AND PATIENT EVALUATIONThe mean age at presentation is 37 years. Most patients do not have any signs of their disease (i.e., they are neurologically “intact”). The most common symptom is seizure.
Age is the most powerful clinical prognostic factor for survival. Children have a significantly better outcome than adults. Other prognostic factors associated with better overall or progression-free survival (PFS) rates include oligodendro-glioma histology, normal mental status, and smaller tumor size.
The imaging features vary by pathologic type. Pilocytic astrocytomas are well circumscribed and contrast enhancing. Diffuse fibrillary astrocytomas are poorly circumscribed and typically nonenhancing, best seen on a T2-weighted or fluid attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) scan.
Low-Grade Gliomas
Paul D. Brown, Michael D. Chan, Edward G. Shaw, and Martin J. van den Bent
26
PRIMARY THERAPYMaximum surgical resection is associated with a more favor-able outcome.
In pediatric low-grade gliomas, observation is recom-mended after gross total resection. After subtotal resection or biopsy, treatment (radiation therapy, chemotherapy) is usually deferred until symptomatic or imaging progression.
In adults, after gross total resection of a pilocytic astrocy-toma, observation is recommended. After gross total or subto-tal resection (or biopsy) of a low-grade glioma, irradiation may be given postoperatively or deferred until progression occurs.
The recommended radiotherapy (RT) dose is 45 Gy to 54 Gy in 25 fractions to 30 fractions, treating the MRI-defined tumor volume with a 2-cm margin.
Early results from one large randomized clinical trial suggest disease and outcomes are similar for either temozolo-mide or RT for 1p/19q-deleted tumors although RT may have a superior PFS for 1p-intact tumors; however, the period of follow-up in this trial is immature and not yet adequate to make definitive treatment recommendations.
Long-term follow-up of a large randomized clinical trial of 251 patients with less than gross total tumor resection or older than 40 found significantly better PFS and overall survival (OS) for those treated with RT followed by procarbazine, CCNU, and vincristine (PCV) compared to those treated with RT alone (RTOG 98-02). These results confirm a benefit for RT followed by chemotherapy for select low-grade glioma populations.
RECURRENT DISEASESeveral challenges constrain recommendations in this setting. It is difficult to differentiate recurrence from radionecrosis by clinical symptoms or signs alone or by conventional MRI or positron emission tomography (PET). Further, at recurrence, consideration must be given to the possibility that these tumors could have transformed to malignant gliomas, which are treated differently.
Low-grade gliomas are a pathologically and clinically diverse group of uncommon central nervous system (CNS) tumors that occur primarily in children and young adults. The prognosis is principally affected by patient age and pathologic type of tumor. Studies assessing proliferation and molecular genetics may provide additional insight into prognostic groups that are at higher risk for developing recurrence and therefore may benefit from adjunctive treatments such as radiation therapy and chemotherapy. In general, more extensive resection is asso-ciated with better prognosis. The optimal timing of irradiation
is best determined by weighing all prognostic factors, favoring “early” (or postoperative) irradiation for high-risk patients and delaying irradiation for lower-risk patients. The importance of chemotherapy in the treatment of low-grade glioma is growing based on a number of clinical trials.1
In this chapter, a comprehensive overview of low-grade glioma is provided with an emphasis on adults. Topics covered include epidemiology, etiology, pathology, biology, clinical manifestations, patient evaluation, management (including surgery, radiation therapy, and chemotherapy), and toxicity.

CHAPTER 26 l Low-Grade Gliomas 453D
ISE
AS
E S
ITES
Grading SystemsThe concept of dividing astrocytomas into discrete grades asso-ciated with a distinct clinical prognosis dates back to the mid-1920s and early 1930s to the work of Bailey and Cushing, who recognized a subset of astrocytomas that had a more favorable outcome than glioblastoma.10 There have been many grading systems (e.g., Kernohan, St. Anne-Mayo, and Ringertz systems) in the past, which assess nuclear abnormalities, mitoses, endo-thelial proliferation, and necrosis. Currently, the most widely used and accepted grading system is the WHO system.7 WHO grade I lesions are well circumscribed and have low prolifera-tive potential, with the possibility of cure following surgery alone. Grade II neoplasms are infiltrative, as a rule recur, and tend to progress to higher grades of malignancy (e.g., grade II astrocytoma transforms to grade III anaplastic astrocytoma) despite initial low-level proliferative activity. All histopatho-logical grading schemes are limited by their need to separate gliomas artificially into three or four groups, when in actuality they exist along a biologic continuum and the diagnoses are subject to considerable interobserver variation.11 For the present, this somewhat outdated method is still used in both therapeutic decision making and prognostication, but it is fully anticipated that in the near future reiterations of the WHO grading system will incorporate imaging and genetic testing.
BIOLOGIC CHARACTERISTICS AND MOLECULAR BIOLOGY
Since the 1990s, our understanding of the biology of low-grade gliomas has increased. This has included studies of tumor proliferation, and both cytogenetic and molecular genetic studies.
Studies of ProliferationTumor proliferation can be assessed with Ki-67 labeling. A large review on Ki-67 labeling revealed increasing values of Ki-67/MIB-1 labeling index with increasing grade of malig-nancy.12 The MIB-1 labeling index differentiates diffuse astro-cytomas (WHO grade II) from anaplastic astrocytomas (WHO grade III) and glioblastoma (GM) tumors. Similar findings have been reported in oligodendrogliomas.13 Although the MIB-1 labeling index is a clear prognostic factor in low-grade glioma, the absence of agreed-on low versus high cut-off values and interobserver variation between various institu-tions prevents its routine use.
Genetic and Other Molecular StudiesAbout 50% to 60% of astrocytomas have TP53 mutations, and this figure may be even higher in gemistocytic astrocytoma.14,15 In contrast, low-grade oligodendrogliomas typically have combined loss of 1p/19q, and the genotype is actually an unbalanced t(1;19)(p10;q10) peri-centromeric translocation.16 TP53 mutations and 1p/19q codeletions are mutually exclu-sive, and most mixed oligoastrocytomas carry either the typical oligodendroglial 1p/19q codeletion or a TP53 muta-tion, suggestive of an astrocytic lineage.17 Therefore, at the molecular level, mixed oligoastrocytomas are not true mixed tumors but are of either astrocytic or oligodendroglial lineage.
The recently identified IDH1 mutations (an enzyme that participates in the citric acid cycle) occur in 70% to 80% of low-grade gliomas, both in tumors with TP53 mutations and in tumors with the 1p/19q loss.15,18 The current data and the absence of the acquisition of IDH1 mutations over time suggest that the IDH1 mutation is an early event in the tumorigenesis
EPIDEMIOLOGY AND ETIOLOGY
Annually in the United States, it is estimated that 23,130 CNS tumors will be diagnosed,2 of which approximately 20,000 will arise in the brain.3 Of these, approximately 2000 will be low-grade gliomas.4
Etiologic factors for low-grade gliomas are largely unknown. Low-grade astrocytomas have been associated with von Recklinghausen disease (type 1 neurofibromatosis) and type 2 neurofibromatosis.3 In addition, a direct link has been made between subependymal giant cell astrocytoma, an uncommon pathologic type of low-grade astrocytoma, and tuberous sclerosis.5
PATHOLOGY
Pathologic ClassificationHistorically, low-grade gliomas have been considered a homo-geneous group of neoplasms associated with a more favorable natural history.6 In reality, they are a diverse group of tumors found throughout the CNS, the outcome of which depends on a number of anatomic, pathologic, biologic, host, and treat-ment factors.
Table 26-1 summarizes the current World Health Organiza-tion (WHO) classification of primary CNS tumors as it applies to low-grade gliomas.7 Grade I tumors must be separated from grade II tumors because they have a different molecular back-ground. These tumors are well circumscribed, are considered benign, and if completely resected, they are typically cured. The pilocytic astrocytomas, which comprise nearly all of the grade I cerebral astrocytomas, tend to be better circumscribed and rarely transform.8 Although pilocytic astrocytomas occur more commonly in the cerebellum of children (juvenile pilo-cytic astrocytoma), they also occur in the cerebral hemispheres and in particular near the optic pathway.
The diffusely infiltrative low-grade astrocytomas (WHO grade II) are the most common and include astrocytoma, oligodendroglioma, and mixed oligoastrocytoma.7 Grade II gliomas are diffusely infiltrating tumors and are capable of undergoing anaplastic transformation with an incidence as high as 80%.8,9 Remaining are the uncommon low-grade glioma variants, including the pleomorphic xanthoastrocyto-mas, subependymal giant cell astrocytomas, and others, which are briefly discussed later in the chapter.
TABLE 26-1 Low-Grade Gliomas* Included in World Health Organization (WHO) Classification of Gliomas
Type WHO Grade
ASTROCYTIC TUMORSSubependymal giant cell astrocytomas I
Pilocytic astrocytomas I
Pleomorphic xanthoastrocytomas II
Pilomyxoid astrocytoma II
Diffuse astrocytoma IIOLIGODENDROGLIAL TUMORSOligodendrogliomas IIOLIGOASTROCYTIC TUMORSOligoastrocytomas II
Louis DN, Ohgaki H, Wiestler OD, et al: The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol 114(2):97-109, 2007.*Exclusive of ependymal and glioneuronal neoplasms.

454 PART A l Central Nervous System Tumors
Clinical PresentationLow-grade gliomas are generally a disease of patients in their 20s, 30s, or 40s, with a mean age at presentation of 37 years. Cases have been reported in patients as young as 7 months and as old as 78 years. Low-grade gliomas are more common in men than in women by a ratio of 1.4 : 1.
The symptoms of low-grade gliomas are shown in Table 26-2. The most common symptom is seizure, occurring in two thirds of patients. Focal seizures are more common than gen-eralized ones. Generalized tonic-clonic, simple partial, and complex partial seizures occur in 43%, 23%, and 34% of patients, respectively. Seizures are particularly common in patients with tumors located in the temporal and frontal lobes, insula, and perirolandic cortex.30 Headache and weakness occur in approximately one third of patients. The remaining symptoms occur in 15% or fewer patients. The median dura-tion from onset of symptoms to diagnosis is between 6 and 17 months, with a range of 1 day to 17 years.
Neurologic signs associated with low-grade gliomas have not been as rigorously reported in the literature. Focal neuro-logic deficits are related to the tumor location. About 50% of affected patients have a normal neurologic examination. The frequency of other signs at presentation is as follows: sensory or motor deficit, 42%; altered mental status, 23%; papilledema, 22%; aphasia, dysphasia, or decreased memory, 20%; focal deficit, 15%; altered consciousness, 8%; and motor deficit, 8%. Neurologic function is considered normal or mildly symptom-atic or impaired in 63% of patients, moderately symptomatic or impaired in 25% of patients, and severely symptomatic or impaired in the remaining 12%. Less than 5% of low-grade gliomas are discovered incidentally (generally because of work-up of head trauma). These tumors appear to have improved outcomes compared to symptomatic tumors.31
Prognosis by Clinical PresentationAge, gender, symptoms, signs, and neurologic function have all been significantly associated with survival in univariate and multivariate analyses from a number of retrospective studies in the literature. Both preoperative and postoperative neurologic function and performance status are correlated with outcome.32 Brown et al conducted an analysis of baseline (before radiation therapy) Mini-Mental State Examination (MMSE) scores collected in patients with low-grade glioma on a prospective, intergroup clinical trial and found that the
of IDH1-mutated tumors19 and distinguishes primary from secondary glioblastoma.18
Methyl-guanine methyl transferase (MGMT) is a DNA-repair enzyme that removes alkyl groups from the O6 position of guanine in DNA and therefore repairs damage induced by alkylating agents (e.g., temozolomide). MGMT promoter methylation in IDH-mutated tumors is highly associated with the CpG Island methylated phenotype (CIMP) that is induced by the metabolic alterations induced by IDH mutations.20 It is currently unclear if MGMT promoter methylation can be used for treatment decisions in low-grade gliomas; recent data suggest that MGMT promoter methylation may have different significance in IDH-mutated versus IDHwt tumors.21 Lastly, a concept of “triple negative” low-grade glioma is emerging, low-grade astrocytomas without either IDH mutations, TP53 mutation, or 1p/19q co-deletion. Of all grade II diffuse glioma these tumors tend to have the worst survival.22
The PI3K/mTOR pathway is activated in most adult low-grade gliomas, with methylation of the promoter region of the PTEN gene in one third of patients.23 One study observed that p14(ARF) hypermethylation and MGMT hypermethylation constitute distinct molecular pathways of astrocytoma pro-gression, with more frequent progression in p14(ARF) hyper-methylation cases.24
Prognostic and Predictive Molecular FactorsMolecular and cellular biologic characterization of low-grade gliomas may help to predict which patients are more likely to require earlier and more aggressive therapy. Conversely, it may help to determine which patients may be observed ini-tially, withholding treatment until the time of disease progres-sion. To date, molecular findings are still infrequently used for clinical decision making primarily because most lack prospec-tive validation. Today, most of the observed findings are pri-marily prognostic and are not predictive for outcome to specific treatments. For example, the presence of IDH1 muta-tions have a major favorable prognostic impact in low-grade astrocytomas but does not affect outcome with temozolomide treatment.15,25 However, recent studies show that molecular profiling holds more prognostic information in low-grade glioma compared to classical histology.25 Moreover, the upcom-ing molecular analyses of recently completed large Radiation Therapy Oncology Group (RTOG) and European Organisation for Research and Treatment of Cancer (EORTC) Phase III studies on low-grade gliomas are expected to change the prog-nostic nature of these molecular features to predictive factors, similar to the recent developments in anaplastic glioma.
The presence of the 1p/19q codeletion also confers a favor-able prognosis, with slower growth rates, compared with non–codeleted low-grade gliomas.26,27 In a study of patients with low-grade glioma enrolled on two North Central Cancer Treat-ment Group (NCCTG) protocols, the median OS time and 5-year OS were 13 years and 96% in oligodendroglioma patients with 1p/19q codeleted tumors versus 10.8 years and 70% in those without codeletion.16 For oligoastrocytomas, the median OS and 5-year OS were 11 years and 90% for 1p/19q codeleted tumors and 8.3 years and 62% for tumors without the 1p/19q codeletion. Several studies noted improved outcome with chemotherapy of 1p/19q codeleted tumors as opposed to 1p/19q intact (oligodendroglial) tumors.28
CLINICAL MANIFESTATIONS AND PATIENT EVALUATION
In this section, information is reviewed on the clinical presen-tation and imaging of supratentorial low-grade gliomas based on the literature.29
TABLE 26-2 Symptoms of Low-Grade Gliomas
Symptom Frequency (%) Mean Range
Seizure 65 30-92
Headache 36 5-48
Weakness 30 6-53
Visual loss or change 15 4-16
Personality change 14 5-16
Focal symptom, NOS 13 6-20
Language dysfunction 13 4-17
Altered sensation 10 8-11
Nausea and vomiting 10 4-14
Altered mental status 9 7-12
Altered consciousness 8 4-20
Cranial neuropathy, NOS 7 —
Data from Levin VA, Gutin PH, Leibel S: Neoplasms of the central nervous system. In DeVita V, Hellman J, Rosenberg S, editors: Cancer: principles and practice of oncology, ed 4, Philadelphia, 1993, JB Lippincott.NOS, Not otherwise specified; data reported in only one series.

CHAPTER 26 l Low-Grade Gliomas 455D
ISE
AS
E S
ITES
TABLE 26-3 Survival of Children with Low-Grade Astrocytoma
Series No. Age (yr)5-yr OS (%)
10-yr OS (%)
Pollack et al35 71 ≤18 95 93
Youland et al36 351 <20 95 90
Merchant et al33 78 <20 99 96
No., Number; OS, overall survival; yr, year.
TABLE 26-4 Imaging Characteristics of Supratentorial Low-Grade Astrocytoma
Characteristics Frequency (%) Mean Range
LOCATIONLobar 80 50-90
Deep/midline* 20 4-40
Right 50 42-55
Left 50 41-60
Bilateral 5 1-11
Hemispheric† 0.5 —LOBAR SITESSingle 84 —
Multiple 16 13-38
Frontal 44 38-65
Temporal 37 8-61
Parietal 18 5-40
Occipital 3 0-10OTHEREnhancement 34 22-58
Size ≥5 cm 66 21-88
Calcification 10 3-18
Cyst 15 6-29
Mass effect‡ — 12-84
From Shaw EG, Scheithauer BW, Dinapoli PR: Low-grade hemispheric astrocytomas. In Black PM, Loeffler JS, editors: Cancer of the nervous system. Cambridge, UK, 1997, Blackwell Scientific.*Deep/midline sites include thalamus, basal ganglia, hypothalamus, third ventricle, and corpus callosum.†Only one series presented data on hemispheric involvement.42
‡Only two series presented data on mass effect.43,44
presence of an abnormal baseline MMSE score (26 or less) was a strong predictor of worse outcome. Patients with an abnor-mal baseline MMSE score had worse 5-year PFS (27% versus 60%) and OS (31% versus 76%) compared with those with a normal score.
After grade, the most powerful predictor of survival in patients with low-grade glioma is age, with much better sur-vival rates in pediatric patients compared with adults. Table 26-3 shows the survival rate of children with low-grade astro-cytoma. In a Phase II trial of 78 pediatric patients with low-grade glioma treated with RT (54 Gy), the 5- and 10-year OS were 99% and 96%, respectively.33 For adult patients with low-grade astrocytoma, there is also an association between age and survival. Those younger than 40 years of age have a better survival than older patients.34
Of all the neurologic symptoms associated with low-grade astrocytoma, seizures, particularly when preceding the diag-nosis by 6 months or more and in the absence of other neuro-logic symptoms, are associated with a better prognosis. In one series, the 5-year OS was 47% in patients presenting with seizures, 33% in those with headaches, 20% in those with altered mental status, and 0% when stupor was the presenting symptom.37 In another series, the 5-year OS was 64% in patients with low-grade glioma who had seizures versus 14% in those without seizures.38 Recent evidence suggests that low-grade gliomas presenting with seizures as first symptom may correlate with the presence of IDH mutations.39
Patients who present with a history of chronic epilepsy resulting from an underlying cerebral neoplasm are frequently found to have a low-grade astrocytoma. These patients are usually children or young adults (30 years of age or younger) whose seizure disorder and underlying tumor are often cured by a complete resection.40
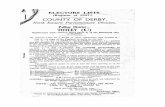
Imaging of Low-Grade GliomasTable 26-4 shows the imaging characteristics of supratentorial low-grade astrocytomas based on multiple series in the litera-ture.41 On computed tomography (CT), the typical low-grade astrocytoma is lobar in location, involves the frontal or tem-poral lobes, is larger than 5 cm in diameter, and is nonenhanc-ing. Because of the infiltrative nature of low-grade astrocytomas, the CT appearance of a typical nonenhancing tumor is a poorly defined area of low attenuation (Figure 26-1, A).
MRI (see Figure 26-1, B) provides superior visualization. FLAIR and both T2- and T1-weighted images (without and with contrast) provide anatomic detail that is useful in defin-ing the extent of the tumor and in planning for surgical and radiation therapy. An understanding of these imaging-based anatomic-histopathologic relationships is important for both the neurosurgeon and the radiation oncologist. Removal of the poorly defined area of low attenuation (increased T2 or FLAIR signal) in a functionally intact area of brain (Figure 26-2) may lead to significant neurologic morbidity.
The radiographic features of low-grade gliomas have been correlated with prognosis in a number of retrospective series.
Although the presence of contrast enhancement on a CT or MRI scan in nonpilocytic low-grade gliomas would seemingly be associated with a worse prognosis because of presumed higher-grade elements or malignant transformation, data from prospective trials have not found the presence of contrast enhancement to be a predictor of outcome.45,46 This may be related to the type of enhancement. Nodular enhancement as opposed to faint, patchy enhancement appears to be related to decreased survival times.47 Other imaging findings, such as tumor size greater than 5 or 6 cm, or tumor crossing the midline (Figure 26-3), have been consistently associated with worse outcome.34,45 Although the relationship between enhancement and prognosis has been controversial in the literature, two series assessing the likelihood of malignant transformation in low-grade gliomas based on the presence of enhancement have demonstrated a statistical association between enhancement and earlier malignant transformation.48,49
Imaging alone cannot reliably distinguish between grade II astrocytomas and oligodendrogliomas, though there are some imaging characteristics that may suggest that a tumor has an oligodendroglial component. Oligodendrogliomas are the most frequent primary brain tumor to calcify and have calci-fications in 70% to 90% of cases.50 They also tend to have corti-cal involvement and heterogeneous signal. There is also emerging evidence that oligodendroglioma and astrocytoma may have distinct signatures on perfusion MRI as the relative cerebral blood volume (rCBV) was found in one study to be significantly higher in low-grade oligodendroglioma than in low-grade astrocytoma.51
Pignatti et al34 developed a prognostic scoring system using imaging, patient, and tumor characteristics derived from the

456 PART A l Central Nervous System Tumors
Figure 26-1 Postcontrast CT (A) and a noncontrast MRI (B) of an adult with a nonenhancing posterior left frontal WHO II astrocytoma.
A B
Figure 26-2 Postgadolinium T1-weighted (A) and T2-weighted (B) MRI scans of an adult with a WHO II astrocytoma of the left parietal lobe.
BA
databases of two large Phase III adult low-grade glioma trials (EORTC trials 22844 and 22845). By means of Cox regression analysis, they identified and validated the following negative risk factors: age 40 years or older, astrocytoma histology subtype, largest diameter of the tumor of 6 cm or more, tumor crossing the midline, and presence of neurologic deficit before surgery. The total number of unfavorable factors present was found to be useful in predicting outcome. The presence of two of these factors or fewer identified a low-risk group (median survival, 7.7 years), whereas three risk factors or more identi-fied a high-risk group (median survival, 3.2 years). A more recent meta-analysis of the four available large Phase III studies using only data on centrally confirmed low-grade astrocytoma found that both PFS and OS were adversely influ-enced by the presence of baseline neurological deficits, a shorter time since first symptoms (<30 wk), an astrocytic
tumor type, and tumors larger than 5 cm in diameter. Age was no longer of prognostic significance.52
PRIMARY THERAPY
ObservationThe decision to observe a patient with low-grade glioma has been justified in the literature for several reasons. These reasons include the relatively favorable natural history of the disease, the lack of proven benefit for invasive interventions such as surgical resection or radiation therapy, and the poten-tial morbidities of treatment. Patients who are observed should be monitored at regular intervals (e.g., every 6 months) to detect radiologic progression before new signs and symp-toms occur.

CHAPTER 26 l Low-Grade Gliomas 457D
ISE
AS
E S
ITES
Figure 26-4 Survival curves for patients with the various subtypes of low-grade glioma compared with curves for an age- and sex-matched control population. A, WHO I (pilocytic) astrocytoma. B, WHO II (diffuse fibrillary) astrocytoma. C, WHO II (mixed) oligoastrocytoma, D, WHO II oligodendroglioma. A to D, Adapted from Shaw EG: The low-grade glioma debate. Evidence defending the position of early radiation therapy. Clin Neurosurg 42:488-494, 1995.
Control populationPilocytic astrocytoma
00
20
40
60
80
100
1 2 3 4 5 6 7 8 9 10
Pilocytic Astrocytoma
Per
cen
tag
eP
erce
nta
ge
Per
cen
tag
eP
erce
nta
ge
p = .031
Years
Control populationLow-grade diffusefibrillary astrocytoma
Control populationLow-grade mixedoligoastrocytoma
00
20
40
60
80
100
1 2 3 4 5 6 7 8 9 10
Diffuse Fibrillary Astrocytoma
00
20
40
60
80
100
1 2 3 4 5 6 7 8 9 10
Mixed Oligoastrocytoma
p �.0001
Years
p �.0001
Years
Control populationLow-grade oligodendroglioma
00
20
40
60
80
100
1 2 3 4 5 6 7 8 9 10
Oligodendroglioma
p �.0001
Years
A B
C D
Figure 26-3 Postgadolinium T1-weighted (A) and FLAIR (B) MRI scans of an adult with a WHO II oligoastrocytoma of the left frontal lobe with midline involvement.
BA
Despite the favorable survival rates observed in certain subsets of patients with low-grade gliomas, the natural history of all pathologic types of supratentorial low-grade gliomas, including the pilocytic astrocytomas (WHO grade I), diffuse astrocytomas, oligoastrocytomas, and oligodendrogliomas
(WHO grade II), is significantly worse than that of an age- and sex-matched control population, for which the expected sur-vival rate is greater than 95% (Figure 26-4).53 Based on this observation, some have argued that all such patients should undergo maximal safe surgical resection followed by

458 PART A l Central Nervous System Tumors
inappropriate management in up to 50% of cases56 diagnosed by imaging underscores the need for histologic verification if a therapeutic intervention is planned. For instance, patients with higher-grade astrocytomas typically receive high-dose external beam radiation therapy in addition to alkylating agents (e.g., temozolomide), whereas GTR without adjuvant radiation therapy constitutes curative treatment for a ganglioglioma.
Extent of ResectionA number of retrospective studies have suggested a benefit for greater extent of resection recognizing the inherent bias associ-ated with extent of resection and tumor location (e.g., more favorable “lobar” lesions are resectable and unfavorable brain-stem lesions are unresectable) that makes any definitive con-clusions about extent of resection dubious.57 Nonetheless, some retrospective trials have attempted to further assess this issue.
Investigators from the University of California San Fran-cisco (UCSF) measured tumor volumes based on FLAIR imaging in 216 patients with low-grade gliomas.58 Patients with at least 90% extent of resection had an 8-year OS of 91% whereas patients with less than 90% extent of resection had an 8-year OS of 60%. After adjusting for age, Karnofsky perfor-mance status (KPS) score, tumor location, and tumor subtype, OS and PFS outcomes were both predicted by postoperative tumor volume. One limitation of this study was the relatively short follow-up (median, 4.4 years).
A long-term follow-up (median, 13.6 years) study from the Mayo Clinic reviewed 314 adult patients with low-grade gliomas and found on multivariate analyses significantly improved OS and PFS rates with GTR or nearly GTR. Almost 50% of patients after GTR or nearly GTR were free of recur-rence 10 years after diagnosis.59
Prospective trials have also found a benefit for greater extent of resection. The Phase II portion of RTOG 9802 (see Figure 26-5) prospectively observed 111 low-risk cases after neurosurgically defined GTR.46 Review of the postoperative MRI emphasized the importance of postoperative imaging to confirm the extent of resection because a substantial minority of patients had residual disease (32% with 1 cm to 2 cm of residual disease and 9% with more than 2 cm of residual tumor). The crude incidence of tumor recurrence was 26% with a residual tumor of less than 1 cm, 68% with a residual tumor of 1 to 2 cm, and 89% with a residual tumor of more than 2 cm.
Although there are no randomized trials that directly assess the impact of maximal tumor resection in low-grade gliomas, a review of the literature suggests a benefit for maximal safe tumor resection, recognizing the importance of achieving this with as little morbidity as possible.60-62
External Beam IrradiationThe key external beam irradiation (EBRT) issues in the man-agement of supratentorial low-grade gliomas are timing of radiation (postoperative versus at time of recurrence) and the appropriate dose and treatment volume. The timing of radia-tion therapy has best been addressed by the Phase III random-ized trial EORTC 2284554 and the RTOG intergroup trial 98-02,46 as previously reviewed.
Radiation, however, has several other beneficial effects besides the potential delay in tumor recurrence. In a small series of 25 patients with medically intractable epilepsy result-ing from an underlying cerebral low-grade glioma, 19 (76%) achieved a significant reduction (>50% decrease) in seizure frequency after RT.63 In the EORTC Phase III randomized trial 22845, there were no differences in seizure control at baseline,
postoperative radiation therapy or chemotherapy, although a survival benefit for treatment, with either aggressive surgery, chemotherapy, or radiation therapy has not been demon-strated in prospective clinical trials.
The RTOG Phase II portion of protocol 9802 (Figure 26-5) prospectively observed 111 patients with low-risk (age younger than 40 years and neurosurgically defined gross total resec-tion) low-grade gliomas.46 In this “low-risk” population, the 5-year OS was 93%. Astrocytoma histology, residual tumor of 1 cm or more according to MR imaging, and preoperative tumor diameter of 4 cm or more were found to be predictive of a poorer PFS. In patients with all three unfavorable prog-nostic factors, the 2- and 5-year rates of PFS were 60% and 13%, respectively. In patients with none of the three unfavor-able prognostic factors, the 2- and 5-year rates of PFS were 100% and 70%, respectively. These data suggest that observa-tion is a reasonable strategy for the most favorable subset (<1 cm residual tumor, preoperative tumor diameter <4 cm, and oligodendroglioma histology) of younger patients after a gross total resection (GTR).
An EORTC Phase III trial (22845) of 311 adults with supra-tentorial low-grade gliomas randomized patients to either observation with radiation therapy at progression (which should be considered a delayed RT arm because two thirds of the patients in the observation group received RT at the time of progression) or initial radiation therapy using 54 Gy to localized treatment fields.54 The 5-year rate of PFS was signifi-cantly better for patients receiving initial radiation therapy (55% versus 35%). However, the median OS was not affected (7.4 years versus 7.2 years). In patients who were progression free at 2 years, there were no differences with respect to cogni-tive deficits, performance status, and headache. These data suggest that observation is a reasonable strategy in adults with asymptomatic supratentorial low-grade glioma.
SurgeryThe key surgical issues in the management of supratentorial low-grade gliomas are twofold. The first issue is whether to perform a biopsy on a patient whose clinical presentation and imaging studies suggest a low-grade glioma, and the second is extent of resection.
Although one series in the literature suggests that the sur-vival rate of patients irradiated for presumed low-grade glioma is comparable to that of patients irradiated for histo-logically verified low-grade astrocytoma,55 the possibility of
Figure 26-5 Schema of the Radiation Therapy Oncology Group Intergroup Low-Grade Glioma Trial 98-02. PCV, procarbazine, CCNU, and vincristine.

CHAPTER 26 l Low-Grade Gliomas 459D
ISE
AS
E S
ITES
Other Radiation ModalitiesSeveral other radiation modalities (e.g., stereotactic radiosur-gery, proton therapy) have been used selectively in patients with low-grade gliomas with growing interest especially in proton RT. Because proton RT reduces the amount of radiation to the normal surrounding brain it is hoped this will decrease late toxicity. To date only small studies have been conducted and more clinical trials are needed to evaluate the efficacy and safety of protons in this setting.66
ChemotherapySeveral Phase II chemotherapy studies have shown efficacy of both temozolomide and PCV chemotherapy in both newly diagnosed and in progressing low-grade gliomas67-73 (Figure 26-6). The studies on newly diagnosed tumors show that the response assessment may be difficult, and that most cases have radiologically stable disease or a minor response as their best response to chemotherapy (at times, even despite clinical improvement and improved seizure control).67 As a result, the PFS appears to be a more informative endpoint than objective response rate in unenhancing tumors.74
Trials that investigated recurrent tumors with enhancing disease report high response rates both in relapsing oligoden-drogliomas and astrocytomas even in the absence of 1p/19q deletion.72,73 For example a study of 58 patients with dedif-ferentiated low-grade astrocytomas treated with temozolo-mide found a response rate of 50% and 6- and 12-month rates of PFS in 67% and 25% of patients, respectively.75
The potential role of chemotherapy in newly diagnosed low-grade glioma is better defined based on the results of two large Phase III chemotherapy studies. RTOG intergroup trial 98-02 (see Figure 26-5) randomized patients with low-grade gliomas at high risk for recurrence (age of 40 years or older or subtotal resection/biopsy) between radiation therapy alone or radiation therapy followed by six cycles of PCV.1,76 With a median follow up of 12 years the patients in the RT and PCV arm had significantly longer median PFS (10.4 years versus 4.0 years, p = 0.002) and OS (13.3 years versus 7.8 years, p = 0.03) compared with the radiotherapy alone arm. These
but at 1 year there were significantly fewer seizures in the irradiated group (25%) than in the observation group (41%).54
It has been suggested that radiation therapy may either increase or decrease the likelihood of malignant transforma-tion or may delay its onset. However, in the EORTC Phase III randomized trial 22845, there were no differences in the malig-nant transformation rate (observation group, 66% versus 72% in the irradiated group) between the study arms at the time of progression.54 These data imply that irradiation neither increases nor decreases the likelihood of malignant transfor-mation, suggesting that dedifferentiation is a biologic phe-nomenon observed in low-grade gliomas independent of the treatment.
EBRT Dose-Volume ConsiderationsRegarding the potential benefit of higher doses of radiation therapy compared with lower doses, two prospective random-ized clinical trials (EORTC 22844 and NCCTG 86-72-51) failed to show improved outcome with higher radiation therapy doses.45,64 The EORTC trial randomized 379 patients to receive moderate-dose (45 Gy) or higher-dose (59.4 Gy) radiation therapy and found no difference in survival rates between the two doses but did find worse quality of life in the higher-dose arm with lower levels of functioning (i.e., emotional and leisure time functioning) and a more extensive symptom burden, including fatigue, malaise, and insomnia.65 The NCCTG trial compared 50.4 Gy with 64.8 Gy and also failed to demonstrate a difference in survival rates between the two doses. Taken together these trials (along with EORTC 22845) support moderate doses in the range of 45 Gy to 54 Gy using localized fields.54
Several series analyzing failure patterns in irradiated patients with low-grade hemispheric gliomas suggest that when tumor progression occurs, it almost always is at the site of the primary tumor within the treatment volume, which implies that partial brain irradiation is appropriate. This was confirmed in the prospective dose-response trial NCCTG 86-72-51 with 92% of failures occurring in the treatment field, 3% within 2 cm of the treatment field, and 5% more than 2 cm beyond the treatment field.45 These data support the appropri-ateness of partial brain irradiation.
Figure 26-6 Prechemotherapy (A) and postchemotherapy (B) T2-weighted MRI of a young adult with a WHO II oligodendroglioma of the left frontal lobe.
A B

460 PART A l Central Nervous System Tumors
For patients who have subtotal resection, particularly chil-dren, a reasonable strategy is observation with close follow-up because there is no apparent survival benefit for routine post-operative radiation therapy, and a second surgical procedure accomplishing GTR appears curative.81 Radiation therapy is usually reserved for symptomatic subtotally resected or unre-sectable tumors, usually in the setting of tumor recurrence. This paradigm was tested and proved to be successful in an NCCTG prospective clinical trial of 20 adults with supratento-rial pilocytic astrocytomas observed after gross or subtotal resection or treated with irradiation after biopsy.8 The 10-year rate of PFS and OS was 95%. When pilocytic astrocytomas require irradiation, the recommendation is to treat localized fields (enhancing tumor with a 4-mm to 5-mm margin using image-guided radiotherapy [IGRT]) with moderate doses (45 Gy to 54 Gy). Radiosurgery (e.g., 13 Gy or 15 Gy marginal dose) has also been used in the treatment of pilocytic astrocy-toma, although it is most frequently used in the salvage setting after prior fractionated RT.82,83 The recurrence rate seems to be higher with radiosurgery when compared to fractionated RT, which may be as a result of patient selection, dose inadequacy, or margin inadequacy.
Pleomorphic XanthoastrocytomasPleomorphic xanthoastrocytomas occur in children and young adults, usually presenting with seizures caused by an underly-ing tumor in the cerebral cortex (temporal lobes), sometimes with adjacent meningeal and, rarely, craniospinal leptomenin-geal involvement. Despite their pleomorphism, these tumors often behave in an indolent manner.7 An analysis of BRAF V600E mutation in 1320 CNS tumors found BRAF mutations in several tumor types (e.g., pilocytic astrocytoma, ganglio-glioma) with an especially high frequency (66%) in pleomor-phic xanthoastrocytoma, possibly providing a new therapeutic window for BRAF-targeted therapies although this will require future clinical trials.84 Treatment recommendations depend on the grade of the astrocytic component. When GTR has been achieved of a pleomorphic xanthoastrocytoma that contains a low-grade diffuse astrocytoma (WHO grade II), observation is appropriate, although local tumor recurrence, sometimes with malignant transformation, can occur. Indica-tions for radiation therapy (doses and treatment fields are similar to those of the more common forms of WHO grade II low-grade gliomas) include pleomorphic xanthoastrocytomas that contain an anaplastic astrocytoma or glioblastoma (WHO grades III/IV), symptomatic subtotally resected or unresect-able tumors, or recurrent tumors, particularly if their astro-cytic component dedifferentiates.85
Central NeurocytomasCentral neurocytomas contain neuronal elements that are usually mature. They are classified as WHO grade II tumors. By definition, they arise in the ventricular system (although an extraventricular neurocytoma with similar clinical behavior
results confirm a benefit for RT followed by PCV for selected low-grade glioma populations.
An EORTC trial addressed the role of temozolomide in newly diagnosed patients with high-risk low-grade gliomas.77 This trial, with PFS as the primary endpoint, randomized patients with progressive disease, uncontrolled seizures despite anticonvulsants, or neurologic symptoms to either standard radiation therapy or daily low-dose temozolomide. Initial results suggest that in 1p-intact tumors RT may confer an improved PFS (p = 0.06), whereas in 1p-deleted tumors temozolomide may be equivalent to RT. At the time of the first report, OS data were still immature. Further follow-up reports of this study must confirm whether a strategy to treat with early chemotherapy and delay administration of RT will trans-late into better long-term cognitive functioning. An intergroup Phase III trial (Figure 26-7) with similar eligibility criteria and stratification factors investigated the efficacy of combined chemoradiation with temozolomide compared with RT alone although the results of this trial are not yet available. Of note a RTOG Phase II study of RT plus concurrent and adjuvant temozolomide for high-risk low-grade gliomas did find improved OS compared to a historical control of RT alone.78
FAVORABLE LOW-GRADE GLIOMA VARIANTS
One group of primary CNS tumors with a distinctly more favorable prognosis than WHO grade II low-grade gliomas includes the pilocytic astrocytomas (WHO grade I) and the other low-grade glioma variants, such as pleomorphic xantho-astrocytomas, subependymal giant cell astrocytomas, and sub-ependymomas. Three other primary CNS tumors of neuronal or mixed neuronal-glial origin are often grouped with the low-grade glioma variants because of their similar presentation and favorable prognosis, including the gangliogliomas, central neurocytomas, and dysembryoplastic neuroepithelial tumors. Other than the pilocytic astrocytomas, which make up approx-imately 20% of supratentorial low-grade gliomas and 80% of cerebellar gliomas,41 the other six variants are uncommon, accounting for approximately 1% or less of primary CNS tumors. From an imaging standpoint, they are typically well circumscribed, enhancing, and sometimes cystic or calcified, or both.7
Pilocytic AstrocytomasPilocytic astrocytomas typically occur in children and young adults, with common locations being the cerebellum, optic pathways, hypothalamus/third ventricle, and cerebral hemi-spheres. They are the most common primary brain tumor occurring in patients with type 1 neurofibromatosis.79,80 The 10-year OS rate is 80% or greater, independent of location in the brain, although rarely, they behave more aggressively.8 In patients undergoing GTR, the 10-year disease-free survival and OS approach 100%.8
Figure 26-7 Schema of the Eastern Cooperative Oncology Group Intergroup Phase III trial E3F05 of radiation therapy with or without temozolomide for symptomatic or progressive low-grade gliomas. fx, Fraction; KPS, Karnofsky performance scale; RT, radiotherapy; TMZ, temozolomide.
Centralpath
review
Stratify by: Arm A (standard arm)RT (50.4 Gy/28 fx)
Arm B (experimental arm)RT � TMZ daily TMZ � 12 cycles
• Age �/� 40• 1p19q status• Pre-op tumor size• KPS �/� 70• Contrast enhancement
REGISTER
RANDOMIZE

CHAPTER 26 l Low-Grade Gliomas 461D
ISE
AS
E S
ITES
Prospective placebo-controlled trials91 have shown the efficacy and safety of mTOR inhibitors (e.g., everolimus) in the treat-ment of SEGA, even in the long term.92
Subependymomas are also classified as WHO grade I epen-dymal tumors. They contain both low-grade astrocytic and ependymal-like cells, and they usually arise in an intraven-tricular location (lateral or fourth ventricles, particularly in and around the foramen of Monro) in adults near the age of 50 years. Treatment recommendations parallel those of pilo-cytic astrocytomas, both surgically and radiotherapeutically. Subtotally resected and recurrent tumors have been reported to respond to radiation therapy.93
RECURRENT DISEASE AND PALLIATIONThe vast majority of patients with a low-grade diffuse glioma die of their disease. As such, at some point in his or her illness, the typical patient with a low-grade glioma likely has the combination of progressive neurologic symptoms and signs in the face of neuroimaging evidence of tumor recurrence. Most of the time the lesion progresses at the original site, but uncommon patterns of treatment failure can occur in patients with recurrent low-grade gliomas such as infiltra-tion across the deep, dense white matter tracts of the brain. Leptomeningeal failure has also been reported, though this is more likely to occur in the pediatric low-grade glioma population.
At the time of progression, often (in up to 70% of patients) the lesion has dedifferentiated to a higher grade of malig-nancy.54 This is revealed on the MRI scan by areas of enhance-ment, which can be preceded for 6 months to 12 months by a local increase in regional cerebral blood volume (e.g., Figure 26-8). The clinical and radiographic features of a high-grade tumor recurrence can be difficult to distinguish from radiation necrosis by conventional MRI. Advanced imaging techniques such as PET,94 single-photon emission CT,95 MRI spectros-copy,96 perfusion and diffusion-weighted MRI97 may prove to be more useful in this regard (Figure 26-9), though there is not yet a consensus as to the most accurate imaging technique for distinguishing transformation from treatment-related imaging changes. As such, tissue must be obtained, although even pathologic findings can be difficult to interpret.
In Forsyth et al,98 51 previously irradiated patients (40 of whom had Kernohan grade 1 or grade 2 astrocytoma, oligoas-trocytoma, or oligodendroglioma) underwent stereotactic biopsy for suspected recurrence. Pathologic examination revealed the presence of tumor only in 30 biopsies (59%), tumor plus necrosis in 17 biopsies (33%), radionecrosis in three instances (6%), and one case of a radiation-induced sarcoma (3%). In patients in whom tumor was found, it was of a high grade in 63%. Median survival time after biopsy was 10 months in patients with tumor only, a finding significantly worse than the 22-month median survival time in those with tumor plus necrosis. No deaths occurred among the patients whose biopsies showed radionecrosis alone.
In general, survival after tumor recurrence is poor. In one series, patients with recurrent low-grade astrocytoma after treatment with surgery and postoperative irradiation were treated with temozolomide and had a 1-year OS of 60%.75 Typically, survival in patients with recurrent oligodendrogli-oma showing a 1p/19q codeletion will be better. In the series Leighton et al99 conducted before the 1p/19q era, the median survival time after recurrence was 39 months for all patients, 16 months for those with recurrent low-grade diffuse astrocy-tomas, and 60 months for those with recurrent low-grade oligodendrogliomas.
Treatment options for recurrence include surgery, re-irradiation (e.g., EBRT, brachytherapy, stereotactic radiation
is described in the fourth edition of the WHO classification), usually as large tumors in the lateral ventricular system, and they rarely have been reported to disseminate craniospi-nally. The typical age at presentation is the late 20s, although these tumors can occur in children or adults.7 Subtotally resected tumors have been reported to respond to radiation therapy.86
A review of 45 patients with central neurocytoma treated with various combinations of surgery, radiation therapy (median dose, 55.8 Gy), and chemotherapy found a 10-year OS of 83%.86 The 5-year local control rate was 100% for patients who received radiation therapy compared with 51% for those who did not (p = 0.045); however, there was no difference in 5-year OS, likely because of the effectiveness of salvage irra-diation. Therefore, patients are observed after GTR with con-sideration of observation after subtotal resection of typical neurocytomas. Patients with unresectable tumors, recurrent tumors, or select patients with subtotally resected tumors (especially, “atypical neurocytomas”) are usually offered radi-ation therapy postoperatively. A systematic review of radio-surgery identified 64 central neurocytomas with a tumor control of 91% at a mean follow-up of 59 months after radio-surgery (median marginal dose 12 Gy to 16 Gy).87 Although this review was limited by small patient numbers, radiosur-gery appears to be an effective treatment for highly selected patients with recurrent or residual disease.
Other Favorable VariantsGangliogliomas consist of neoplastic ganglion (neuronal) cells and neoplastic glial (astrocytic) cells. They can occur in chil-dren and adults, although most are present in the first two to three decades of life. Gangliogliomas can develop anywhere in the CNS, but they tend to occur in the supratentorial brain, most often in a temporal location, and enhance on MR images with contrast medium. Like pleomorphic xanthoastrocytomas, the glial component can be a low-grade tumor (WHO grade I) or a higher-grade tumor (WHO grade III).7 A review of 402 patients found no local control or survival benefit with post-operative RT after GTR but did find improved local control (but not survival) after subtotal resection for both low and high-grade tumors.88 Treatment principles are similar to those of pleomorphic xanthoastrocytoma from both a surgical and radiotherapeutic standpoint.89
Dysembryoplastic neuroepithelial tumors, like gangliogliomas, also contain a mixture of neuronal and glial elements, although the neuronal component is mature and the glial component is well differentiated and has astrocytic or oligodendroglial tissue. As such, the tumors are classified as WHO grade I tumors. Typically, these tumors occur in a temporal location, are characteristically multinodular, and arise during the first two decades of life. Treatment principles are similar to those of pilocytic astrocytomas from both a surgical and radiotherapeutic standpoint, although irradiation is rarely necessary.7
Subependymal giant cell astrocytomas (SEGA) occur in patients with tuberous sclerosis, often during the first two decades of life but sometimes later.5 Characterized by large astrocyte-like cells, they are classified as WHO grade I tumors, like the pilocytic astrocytomas. Typically, they arise in an intraven-tricular or periventricular location (e.g., lateral ventricles, foramen of Monro) and on MR images appear as intraven-tricular enhancing masses. Treatment recommendations paral-lel the pilocytic astrocytomas; that is, GTR is considered curative.90 However the role of RT for symptomatic progres-sion or relapse has been diminished even more with the rec-ognition that tuberous sclerosis is associated with constitutive activation of mammalian target of rapamycin (mTOR).

462 PART A l Central Nervous System Tumors
Figure 26-8 A, Axial T1-weighted MRI of diagnostic imaging of WHO grade II diffuse astrocytoma demonstrating nonenhancing mass in the left medial temporal lobe. B, Axial arterial spin labeling MRI of the same patient acquired simultaneously with image A and showing increased perfusion in the left temporal lobe mass. C, Axial T1-weighted MRI performed at 6-month interval showing increased enhancement in the left temporal lobe. Subsequent biopsy demonstrated malignant transformation to WHO grade IV glioblastoma.
A B C
Figure 26-9 Postgadolinium T1-weighted MRI of a young adult with a WHO grade II oligoastrocytoma after subtotal resection, 50.4-Gy external beam radiation therapy, and 18 Gy given in a single fraction in stereotactic radiosurgery for recurrent disease at the medial edge of the resection cavity. A, An area of increased contrast enhancement at the site of the stereotactic radiosurgery. B, Positron emission tomography using fluorodeoxyglucose showed increased uptake at the site of the contrast enhancement (arrow). However, MRI spectroscopy (C) was more suggestive of radiation necrosis because the choline-to-creatine ratio was less than 2 and the lactate peak was elevated. Subsequent biopsy demonstrated radiation necrosis.
A B
C

CHAPTER 26 l Low-Grade Gliomas 463D
ISE
AS
E S
ITES
therapy, radiosurgery) and chemotherapy (or second-line che-motherapy). Patients must be managed on an individual basis, depending on the timing of the relapse, previous treatments, and accessibility for clinically significant surgery. In one series, 63 patients with recurrent low-grade gliomas were treated with a second course of conventionally fractionated RT (median dose 36 Gy in 2 Gy fractions) in which the enhancing and FLAIR abnormality was encompassed within the RT volume.100 From time of reirradiation, median survival and PFS were 23 and 12 months, respectively. Hypofractionated reirradiation has also been reported for recurrent low-grade gliomas.101
A concern for stereotactic radiosurgery (SRS) as a treatment option for recurrent low-grade glioma is the likely infiltrative nature of these tumors and the limitations of SRS to a smaller treatment volume. There have been several reported series of salvage SRS, and although durable local control is not the rule, there likely exists a population of patients that may benefit from this modality. In a University of Pittsburgh SRS series, PFS was 81.5% at 5 years after SRS for patients with recurrent grade II oligodendroglioma.83 In a separate SRS series from the same institution in patients with recurrent grade II astrocy-toma, only 54.1% remained progression free at 5 years.102 Figure 26-10 depicts a patient treated with SRS for a nodular resection cavity recurrence of grade II oligodendroglioma along with a 10 year follow-up MRI documenting continued local control.
Salvage chemotherapy appears to have a modest effect after failure of low-grade glioma that has progressed beyond either prior RT or prior first-line chemotherapy. Retrospective series appear to suggest that neither PCV nor temozolomide have significant activity after a low-grade glioma has failed the other regimen as first-line therapy.103,104 The EORTC is cur-rently assessing the efficacy of adding bevacizumab to temo-zolomide in a randomized Phase II study in progressive non 1p/19q codeleted grade II and grade III tumors.
Figure 26-10 A, Axial T1-weighted MRI depicting treatment plan for single fraction radiosurgery of multiply recurrent WHO grade II oligodendroglioma treated with 18 Gy to the 50%. B, Axial T1-weighted MRI depicting 10-year follow-up imaging confirming long-term local control of previously treated lesion.
A B
IRRADIATION TECHNIQUES AND TOXICITIES
EBRT Volume ConsiderationsBecause the vast majority of treatment failures after partial brain irradiation occur in the field, treatment of the tumor plus a margin of normal tissue is considered the standard of care. With the identification of tumor cells up to several centimeters beyond the margin of the tumor identified by T2-weighted MRI,105 the appropriate irradiation volume should include the MRI extent of tumor as defined by T2-weighted or FLAIR MR images with a 2-cm to 3-cm margin. A 2-cm margin may be acceptable if some form of IGRT is used (Figure 26-11).
EBRT Dose and Technique IssuesAs previously outlined, three prospective randomized clinical trials (EORTC 22844, EORTC 22845, and NCCTG 86-72-51) support moderate RT doses in the range of 45 Gy to 54 Gy.45,54,64 In an effort to improve conformality and possibly better spare normal structures, many centers use intensity-modulated radiation therapy (IMRT), especially in select situ-ations such as tumors involving the inferior temporal lobes or tumors with irregular or complex shapes. However, a disad-vantage of IMRT is the increased dose heterogeneity because in low-grade gliomas, much of the target is an admixture of tumor cells and normal brain tissue.106 As an example, if IMRT is used with a prescription of 54 Gy in 30 fractions, this may result in heterogeneity of 10% or more in the target. This increased heterogeneity results in an increased daily dose per fraction and an increased total dose such that the biologically equivalent dose approaches that of the high-dose arm in NCCTG 86-72-51 (e.g., 64.8 Gy) and therefore increases the risk of radiation necrosis.45 Selecting a slightly lower dose (e.g., 50.4 Gy) is a reasonable strategy because even with

464 PART A l Central Nervous System Tumors
supratentorial low-grade gliomas. To assess the toxicity of irradiation, it is also important to understand the neurologic and cognitive dysfunction that results from having a cerebral low-grade glioma.109 To assess the impact of early intervention on quality of life (QOL), investigators from the University Medical Center Utrecht matched 24 patients with suspected low-grade gliomas (based on imaging and clinical history) to 24 patients with proven low-grade gliomas, who had under-gone early surgery, and 24 healthy controls.110 Both patient groups scored worse on QOL and cognitive function scales than healthy control subjects. Unoperated patients with sus-pected low-grade gliomas scored better on most items than patients who had undergone surgery and had tissue with proven low-grade gliomas. This study suggests that observa-tion is a reasonable option for a select population. In addition, this study emphasizes the need for baseline (i.e., before surgery or RT) cognitive testing because the tumor itself causes cogni-tive deficits.
Because there is no convincing evidence that early radia-tion therapy improves OS, deferring irradiation until there is evidence of symptomatic tumor growth is an acceptable prac-tice. The primary rationale for delaying irradiation is to reduce the risk of radiation-induced neurocognitive damage. Some retrospective studies have found increased neurocognitive dif-ficulties after cranial radiation therapy. However, these studies have several deficiencies109 although the most serious is the lack of baseline neurocognitive testing because the brain tumor itself is often the primary cause of cognitive difficulties. In contrast, a number of studies have prospectively performed extensive neuropsychological testing on adult patients with low-grade neoplasms before (baseline) and after radiation therapy (up to 6 years after radiation therapy) and have not found significant neurocognitive deficits when compared with either baseline111,112 or a cohort of patients with low-grade brain neoplasms not treated with irradiation113,114 (Table 26-5). For example, in NCCTG 86-72-51, a subset of 20 of the 203 adult study patients who received either 50.4 Gy or 64.8 Gy underwent psychometric testing before and up to 5 years after localized radiation therapy.112 No significant loss in general intellectual function, new learning, or memory was seen. However, four patients, all in the 64.8-Gy arm, had a mild decline in one or more of the domains (immediate verbal memory, learning, and spatial problem solving) assessed. Therefore the weight of evidence indicates a low incidence of neurocognitive difficulties after focal, conventionally fraction-ated (1.8 Gy to 2 Gy) radiation therapy using modern tech-niques to deliver moderate doses in adults.109
In children, the risk of cognitive injury after irradiation appears to be most closely associated with younger age (i.e., developing brain) at the time of treatment and secondarily with the volume of brain irradiated.115 The effects of surgery and other therapies for these tumors are also associated with a risk of cognitive injury, which can make assessments after RT difficult.116,117 To better assess the cognitive impact of RT in children St Jude Children’s Hospital evaluated late effects in 78 patients with low-grade gliomas after treatment with more modern techniques (54-Gy conformal EBRT with a 10-mm clinical target volume margin).115 Through 5 years of follow-up for the entire group (baseline testing after surgery and serial evaluations), only a decline in spelling scores was clinically significant. Thirteen of the patients had neurofibro-matosis 1 (NF-1) and were found to have worse function at baseline compared with other pediatric patients with low-grade gliomas. In addition, the patients with NF-1 had wors-ening function over time whereas patients without NF-1 had stable function over time. Age had a significant impact on cognitive function over time, such that a 10-point decline in IQ 5 years after irradiation would be expected for a child age
heterogeneity of 10% the hot spots are within the range of what is considered to be a low risk of radiation necrosis. Accordingly, a dose of 50.4 Gy was chosen for the current intergroup low-grade glioma trial (E3F05) (see Figure 26-7). Because modern IMRT techniques tend not to have this degree of dose heterogeneity, the issue will likely become less significant with better treatment planning techniques.
Toxicities of Radiation TherapyA spectrum of radiation-induced toxicities can occur in patients receiving therapeutic brain irradiation. These range from cognitive sequelae, the pathogenesis of which is likely white matter injury, to overt radiation necrosis, which is prob-ably a consequence of vascular injury.107 The incidence of overt radiation necrosis after irradiation for a cerebral low-grade glioma is approximately 3% based on data from surgical series in which reoperation data were reported.43,108 This is consistent with findings from NCCTG 86-72-51 (50.4 Gy versus 64.8 Gy), in which the 2-year actuarial incidence of severe, life-threatening, or fatal radionecrosis was 1% at 50.4 Gy and 5% at 64.8 Gy.45 Examples of the clinical presentation, imaging changes, time course, management, and outcome of the spec-trum of severe or worse radiation toxicities seen in patients with cerebral low-grade gliomas are shown in Figures 26-12 to 26-14.
Prospective Quality-of-Life and Neurocognitive AnalysesSeveral studies have focused on the neurocognitive effects of radiation therapy in patients who are long-term recurrence-free survivors, most of whom were irradiated for
Figure 26-11 Fractionated stereotactic radiotherapy (50.4 Gy in 28 fractions), using daily image-guided radiotherapy (IGRT), in the treatment of a WHO grade II oligoastrocytoma involving the posterior insular cortex and superior temporal gyrus.

CHAPTER 26 l Low-Grade Gliomas 465D
ISE
AS
E S
ITES
Figure 26-12 Preirradiation, postgadolinium T1-weighted (A) and T2-weighted (B) MR images of an adult with a WHO grade II oligodendroglioma of the right frontotemporal lobes. Seven months after 64.8-Gy external beam radiation therapy, the patient developed headaches. Postgadolinium T1-weighted (C) and T2-weighted (D) MR images are shown. The differential diagnosis considered recurrent tumor and radiation necrosis. After a brief course of oral corticosteroid medications, the imaging abnormalities resolved, a finding supporting the diagnosis of transient radiation necrosis. Postgadolinium T1-weighted (E) and T2-weighted (F) magnetic resonant images are shown. Adapted from Daumas-Duport C, Scheithauer BW, Kelly PJ: A histologic and cytologic method for spatial definition of gliomas. Mayo Clin Proc 62:435-449, 1987; and Kelly PJ, Daumas-Duport C, Scheithauer BW, et al: Stereotactic histologic correlations of computed tomography and magnetic resonance imaging-defined abnormalities in patients with glial neoplasms. Mayo Clin Proc 62:450-459, 1987.
A B C
D E F

466 PART A l Central Nervous System Tumors
Figure 26-13 Contrast-enhanced CT demonstrates the progress of a left frontal WHO grade II astrocytoma in an adult patient. A, Before 64.8-Gy external beam radiation therapy. B, After irradiation, the patient had headaches. C, Eighteen months after gross total resection of what proved to be a combination of radiation necrosis and persistent low-grade astrocytoma, the patient had no evidence of further radiation necrosis or tumor.
A B C
Figure 26-14 A, T2-weighted MRI scan of an older adult with an infiltrative, poorly defined WHO grade II astrocytoma the epicenter of which was in the left temporal lobe. Six months after completing 64.8-Gy external beam radiation therapy, the patient developed a significant decline in cognitive function and overall performance status. B, Repeat MRI showed dramatic white matter changes. The patient subsequently died, and an autopsy showed radiation necrosis with a persistent low-grade astrocytoma.
A B
TABLE 26-5 Prospective Trials with Baseline and Serial Cognitive Testing in Adults with Low-Grade Neoplasms
Author Histology (No. with RT)RT: Total Dose/Fraction (Gy) Mean FU (yr) Neurotoxicity after RT
Vigliani et al114 LGG, AA (17) Focal RT 54/1.8 4 No; transient decline in RcT
Armstrong et al111 LGG, pituitary, pineal, meningioma (26)
Focal RT mean 54.6/1.8-2
3 No; mild decline in visual memory after 5 yr
Torres et al113 Meningioma, LGG, GBM, ependymoma, adenoma (15)
Focal RT mean 54/1.8
2 No; decline in memory and attention only if tumor progression
Laack et al112 LGG (20) Focal RT 50.4/1.8 or 64.8/1.8
3 No; mild decline in 64.8-Gy arm in immediate verbal memory, learning, and spatial problem solving
AA, Anaplastic astrocytoma; CGE, cobalt Gray equivalent; FU, follow-up; GBM, glioblastoma multiforme; LGG, low-grade glioma; NFS, neurologic function scores; RcT, reaction time; RT, radiation therapy.

CHAPTER 26 l Low-Grade Gliomas 467D
ISE
AS
E S
ITES
Figure 26-15 Treatment algorithm for low-grade glioma. *Treatment is deferred until the time of symptomatic or imaging progression. Appropriate treatment at the time of progression may include surgery, chemotherapy, or radiation therapy. ** For patients with less than gross total tumor resection or older than 40 consider radiotherapy followed by procarbazine, CCNU, and vincristine. A, Astrocytoma; CT, chemotherapy; O, oligodendroglioma; OA, oligoastrocytoma; PA, pilocytic astrocytoma; RT, radiation therapy.
Child
Gross Total Resection(any pathology)
Subtotal Resection/Biopsy(any pathology)
Asymptomatic Symptomatic
Prepub Pubertal
Adult
Gross TotalResection
PA A,OA,O
SubtotalResection/Biopsy
Asymptomatic Symptomatic
Pathologically Proven Low-Grade Glioma
Observe*
Observe*
Observe*
Observe*or
RT** or CTCT(or RT) RT(or CT)
Observe*or
RT** or CT
RT** (or CT)
5 years at the time of irradiation. Each year of increasing age significantly reduced the decline in IQ. The authors noted that cognitive function was largely preserved after conformal RT using modern techniques, but RT should be delayed if possi-ble for younger patients.
CONCLUSIONS, TREATMENT ALGORITHM, AND FUTURE POSSIBILITIES
Low-grade gliomas are a heterogeneous group of CNS neo-plasms, and their natural history depends primarily on patho-logic type and tumor size. A treatment algorithm for low-grade gliomas is provided in Figure 26-15. Despite having been con-sidered “benign,” most of these tumors behave in an aggres-sive manner, even after surgery and radiation therapy.
Prospective trials confirm the role of chemotherapy for select low-grade glioma populations. Long-term follow-up of RTOG 98-02 (high-risk patients with less than gross total tumor resection or older than 40) found significantly better PFS (10.4 years versus 4.0 years, p = 0.002) and OS (13.3 years versus 7.8 years, p = 0.02) for those treated with RT followed by PCV chemotherapy compared to those treated with RT alone.
Translational research, including studies of proliferation, cytogenetics, and molecular genetics, will provide much needed insight for the next generation of biologically based therapies.
CRITICAL REFERENCESA full list of cited references is published online at www.expertconsult.com.
1. Buckner JC, Pugh S, Shaw EG, et al: Phase III study of radiation therapy (RT) with or without procarbazine, CCNU, and vincristine (PCV) in low-grade glioma. RTOG 9802 with NCCTG, ECOG and SWOG Paper pre-sented at ASCO, 2014.
3. Mehta MP, Buckner JC, Sawaya R, et al: Neoplasms of the central nervous system. In DeVita V, Lawrence TS, Rosenberg S, editors: Cancer: principles and practice of oncology, ed 8, Philadelphia, 2008, Lippincott Williams & Wilkins.
4. Schiff D, Brown PD, Giannini C: Outcome in adult low-grade glioma: The impact of prognostic factors and treatment. Neurology 69(13):1366–1373, 2007.
7. Louis DN, Ohgaki H, Wiestler OD, et al: The 2007 WHO classification of tumours of the central nervous system. [erratum appears in Acta Neuro-pathol. 2007 Nov;114(5):547]. Acta Neuropathol 114(2):97–109, 2007.
8. Brown PD, Buckner JC, O’Fallon JR, et al: Adult patients with supratento-rial pilocytic astrocytomas: A prospective multicenter clinical trial. Int J Radiat Oncol Biol Phys 58(4):1153–1160, 2004.
11. van den Bent MJ: Interobserver variation of the histopathological diagnosis in clinical trials on glioma: A clinician’s perspective. Acta Neuropathol 120(3):297–304, 2010.
15. Dubbink HJ, Taal W, van Marion R, et al: IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurol-ogy 73:1792–1795, 2009.
16. Jenkins RB, Blair H, Ballman KV, et al: A t(1;19)(q10;p10) mediates the combined deletions of 1p and 19q and predicts a better prognosis of patients with oligodendroglioma. Cancer Res 66(20):9852–9861, 2006.
18. Ichimura K, Pearson DM, Kocialkowski S, et al: IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro-Oncol 11(4):341–347, 2009.
19. Watanabe T, Nobusawa S, Kleihues P, et al: IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174(4):1149–1153, 2009.
20. Turcan S, Rohle D, Goenka A, et al: IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature 483(7390):479–483, 2012.
21. Wick W, Meisner C, Hentschel B, et al: Prognostic or predictive value of MGMT promoter methylation in gliomas depends on IDH1 mutation. Neu-rology 81(17):1515–1522, 2013.
27. van den Bent MJ, Looijenga LH, Langenberg K, et al: Chromosomal anoma-lies in oligodendroglial tumors are correlated with clinical features. Cancer 97(5):1276–1284, 2003.
28. Kaloshi G, Benouaich-Amiel A, Diakite F, et al: Temozolomide for low-grade gliomas: Predictive impact of 1p/19q loss on response and outcome.[see comment]. Neurology 68(21):1831–1836, 2007.
32. Brown PD, Buckner JC, O’Fallon JR, et al: Importance of baseline mini-mental state examination as a prognostic factor for patients with low-grade glioma. Int J Radiat Oncol Biol Phys 59(1):117–125, 2004.
33. Merchant TE, Kun LE, Wu S, et al: Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol 27(22):3598–3604, 2009.
34. Pignatti F, van den Bent M, Curran D, et al: Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20(8):2076–2084, 2002.
36. Youland RS, Khwaja SS, Schomas DA, et al: Prognostic factors and survival patterns in pediatric low-grade gliomas over 4 decades. J Pediatr Hematol Oncol 35(3):197–205, 2013.
41. Shaw EG, Scheithauer BW, Dinapoli RP: Low-grade hemispheric astrocy-tomas, Cambridge, 1997, Blackwell Scientific Publications.
45. Shaw E, Arusell R, Scheithauer B, et al: Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: Initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study. J Clin Oncol 20(9):2267–2276, 2002.
54. van den Bent MJ, Afra D, de Witte O, et al: Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendro-glioma in adults: The EORTC 22845 randomised trial. [see comment][erratum appears in Lancet. 2006 Jun 3;367(9525):1818]. Lancet 366 (9490):985–990, 2005.
58. Smith JS, Chang EF, Lamborn KR, et al: Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol 26(8):1338–1345, 2008.
64. Karim AB, Maat B, Hatlevoll R, et al: A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys 36(3):549–556, 1996.

468 PART A l Central Nervous System Tumors
65. Kiebert GM, Curran D, Aaronson NK, et al: Quality of life after radiation therapy of cerebral low-grade gliomas of the adult: Results of a randomised phase III trial on dose response (EORTC trial 22844). EORTC Radiotherapy Co-operative Group. Eur J Cancer 34(12):1902–1909, 1998.
68. Hoang-Xuan K, Capelle L, Kujas M, et al: Temozolomide as initial treat-ment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol 22(15):3133–3138, 2004.
70. Buckner JC, Gesme D, O’Fallon JR, et al: Phase II trial of procarbazine, lomustine, and vincristine as initial therapy for patients with low-grade oligodendroglioma or oligoastrocytoma: Efficacy and associations with chromosomal abnormalities. J Clin Oncol 21(2):251–255, 2003.
71. Levin N, Lavon I, Zelikovitsh B, et al: Progressive low-grade oligodendro-gliomas: Response to temozolomide and correlation between genetic profile and O6-methylguanine DNA methyltransferase protein expression. Cancer 106(8):1759–1765, 2006.
73. Quinn JA, Reardon DA, Friedman AH, et al: Phase II trial of temozolomide in patients with progressive low-grade glioma. [see comment]. J Clin Oncol 21(4):646–651, 2003.
74. van den Bent MJ, Wefel JS, Schiff D, et al: Response assessment in neuro-oncology (a report of the RANO group): Assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12(6):583–593, 2011.
75. Taal W, Zonnenberg CBL, Bromberg JE, et al: MGMT assessed with methylation-specific (MS-) multiplex ligation-dependent probe amplifica-tion (MLPA) predicts response to temozolomide in progressive low-grade astrocytoma after radiotherapy. Neuro Oncol 10(5):868, 2008.
76. Shaw EG, Wang M, Coons SW, et al: Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: Initial results of RTOG 9802. J Clin Oncol 30(25):3065–3070, 2012.
77. Baumert BG, Mason WP, Ryan G, et al: Temozolomide chemotherapy versus radiotherapy in molecularly characterized (1p loss) low-grade glioma: A randomized phase III intergroup study by the EORTC/NCIC-CTG/TROG/MRC-CTU (EORTC 22033–26033). J Clin Oncol 31(Suppl), 2013. abstr 2007.
91. Franz DN, Belousova E, Sparagana S, et al: Efficacy and safety of everoli-mus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): A multicentre, randomised, placebo-controlled phase 3 trial. Lancet 381(9861):125–132, 2013.
104. van den Bent MJ, Chinot O, Boogerd W, et al: Second-line chemotherapy with temozolomide in recurrent oligodendroglioma after PCV (procarba-zine, lomustine and vincristine) chemotherapy: EORTC Brain Tumor Group phase II study 26972. Ann Oncol 14(4):599–602, 2003.
105. Kelly PJ, Daumas-Duport C, Scheithauer BW: Stereotactic histologic cor-relations of computed tomography and magnetic resonance imaging-defined abnormalities in patients with glial neoplasms. Mayo Clin Proc 62:450–459, 1987.
107. Laack NN, Brown PD: Cognitive sequelae of brain radiation in adults. Semin Oncol 31(5):702–713, 2004.
109. Brown PD, Buckner JC, Uhm JH, et al: The neurocognitive effects of radiation in adult low-grade glioma patients. Neuro Oncol 5(3):161–167, 2003.
111. Armstrong CL, Hunter JV, Ledakis GE, et al: Late cognitive and radio-graphic changes related to radiotherapy: Initial prospective findings. [see comments.]. Neurology 59(1):40–48, 2002.
112. Laack NN, Brown PD, Ivnik RJ, et al: Cognitive function after radiotherapy for supratentorial low-grade glioma: A North Central Cancer Treatment Group prospective study. Int J Radiat Oncol Biol Phys 63(4):1175–1183, 2005.
113. Torres IJ, Mundt AJ, Sweeney PJ, et al: A longitudinal neuropsychological study of partial brain radiation in adults with brain tumors. Neurology 60(7):1113–1118, 2003.
114. Vigliani MC, Sichez N, Poisson M, et al: A prospective study of cognitive functions following conventional radiotherapy for supratentorial gliomas in young adults: 4-year results. Int J Radiat Oncol Biol Phys 35(3):527–533, 1996.
115. Merchant TE, Conklin HM, Wu S, et al: Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: Prospective evalua-tion of cognitive, endocrine, and hearing deficits. J Clin Oncol 27(22):3691–3697, 2009.

CHAPTER 26 l Low-Grade Gliomas 468.e1D
ISE
AS
E S
ITES
REFERENCES1. Buckner JC, Pugh S, Shaw EG, et al: Phase III study of radiation therapy
(RT) with or without procarbazine, CCNU, and vincristine (PCV) in low-grade glioma. RTOG 9802 with NCCTG, ECOG and SWOG Paper pre-sented at ASCO, 2014.
2. Siegel R, Naishadham D, Jemal A: Cancer statistics, 2013. CA Cancer J Clin 63(1):11–30, 2013.
3. Mehta MP, Buckner JC, Sawaya R, et al: Neoplasms of the central nervous system. In DeVita V, Lawrence TS, Rosenberg S, editors: Cancer: principles and practice of oncology, ed 8, Philadelphia, 2008, Lippincott Williams & Wilkins.
4. Schiff D, Brown PD, Giannini C: Outcome in adult low-grade glioma: The impact of prognostic factors and treatment. Neurology 69(13):1366–1373, 2007.
5. Nabbout R, Santos M, Rolland Y, et al: Early diagnosis of subependymal giant cell astrocytoma in children with tuberous sclerosis. [see comment]. J Neurol Neurosurg Psychiatry 66(3):370–375, 1999.
6. Horrax G: Benign (favorable) types of brain tumor: The end results (up to twenty years), with statistics of mortality and useful survival. N Engl J Med 250:981–984, 1954.
7. Louis DN, Ohgaki H, Wiestler OD, et al: The 2007 WHO classification of tumours of the central nervous system. [erratum appears in Acta Neuro-pathol. 2007 Nov;114(5):547]. Acta Neuropathol 114(2):97–109, 2007.
8. Brown PD, Buckner JC, O’Fallon JR, et al: Adult patients with supratento-rial pilocytic astrocytomas: A prospective multicenter clinical trial. Int J Radiat Oncol Biol Phys 58(4):1153–1160, 2004.
9. Sofietti R, Chio A, Giordana MT: Prognostic factors in well-differentiated cerebral astrocytomas in the adult. Neurosurgery 24:686–692, 1989.
10. Bailey P, Cushing H: A classification of the tumors of the glioma group on a histogenetic basis with a correlated study of prognosis, Philadelphia, 1926, JB Lippincott.
11. van den Bent MJ: Interobserver variation of the histopathological diagnosis in clinical trials on glioma: A clinician’s perspective. Acta Neuropathol 120(3):297–304, 2010.
12. Johannessen AL, Torp SH: The clinical value of Ki-67/MIB-1 labeling index in human astrocytomas. Pathol Oncol Res 12(3):143–147, 2006.
13. Kros JM, Hop WC, Godschalk JJ, et al: Prognostic value of the proliferation-related antigen Ki-67 in oligodendrogliomas. Cancer 78(5):1107–1113, 1996.
14. Stander M, Peraud A, Leroch B, et al: Prognostic impact of TP53 mutation status for adult patients with supratentorial World Health Organization Grade II astrocytoma or oligoastrocytoma: A long-term analysis. Cancer 101(5):1028–1035, 2004.
15. Dubbink HJ, Taal W, van Marion R, et al: IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurol-ogy 73:1792–1795, 2009.
16. Jenkins RB, Blair H, Ballman KV, et al: A t(1;19)(q10;p10) mediates the combined deletions of 1p and 19q and predicts a better prognosis of patients with oligodendroglioma. Cancer Res 66(20):9852–9861, 2006.
17. Maintz D, Fiedler K, Koopmann J, et al: Molecular genetic evidence for subtypes of oligoastrocytomas. J Neuropathol Exp Neurol 56(10):1098–1104, 1997.
18. Ichimura K, Pearson DM, Kocialkowski S, et al: IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro-Oncol 11(4):341–347, 2009.
19. Watanabe T, Nobusawa S, Kleihues P, et al: IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174(4):1149–1153, 2009.
20. Turcan S, Rohle D, Goenka A, et al: IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature 483(7390):479–483, 2012.
21. Wick W, Meisner C, Hentschel B, et al: Prognostic or predictive value of MGMT promoter methylation in gliomas depends on IDH1 mutation. Neu-rology 81(17):1515–1522, 2013.
22. Figarella-Branger D, Bouvier C, de Paula AM, et al: Molecular genetics of adult grade II gliomas: Towards a comprehensive tumor classification system. J Neurooncol 110(2):205–213, 2012.
23. McBride SM, Perez DA, Polley MY, et al: Activation of PI3K/mTOR pathway occurs in most adult low-grade gliomas and predicts patient survival. J Neurooncol 97(1):33–40, 2010. 2009:published online.
24. Watanabe T, Katayama Y, Yoshino A, et al: Aberrant hypermethylation of p14ARF and O6-methylguanine-DNA methyltransferase genes in astrocy-toma progression. Brain Pathol 17(1):5–10, 2007.
25. Leu S, von Felten S, Frank S, et al: IDH/MGMT-driven molecular classifica-tion of low-grade glioma is a strong predictor for long-term survival. Neuro Oncol 15(4):469–479, 2013.
26. Laigle-Donadey F, Martin-Duverneuil N, Lejeune J, et al: Correlations between molecular profile and radiologic pattern in oligodendroglial tumors. Neurology 63(12):2360–2362, 2004.
27. van den Bent MJ, Looijenga LH, Langenberg K, et al: Chromosomal anoma-lies in oligodendroglial tumors are correlated with clinical features. Cancer 97(5):1276–1284, 2003.
28. Kaloshi G, Benouaich-Amiel A, Diakite F, et al: Temozolomide for low-grade gliomas: Predictive impact of 1p/19q loss on response and outcome.[see comment]. Neurology 68(21):1831–1836, 2007.
29. Shaw EG, Scheithauer BW, O’Fallon JR: Supratentorial gliomas: A compara-tive study by grade and histologic type. J Neurooncol 31(3):273–278, 1997.
30. Whittle IR: The dilemma of low grade glioma. J Neurol Neurosurg Psychia-try 75(Suppl 2):ii31–ii36, 2004.
31. Potts MB, Smith JS, Molinaro AM, et al: Natural history and surgical man-agement of incidentally discovered low-grade gliomas. J Neurosurg 116(2):365–372, 2012.
32. Brown PD, Buckner JC, O’Fallon JR, et al: Importance of baseline mini-mental state examination as a prognostic factor for patients with low-grade glioma. Int J Radiat Oncol Biol Phys 59(1):117–125, 2004.
33. Merchant TE, Kun LE, Wu S, et al: Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol 27(22):3598–3604, 2009.
34. Pignatti F, van den Bent M, Curran D, et al: Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20(8):2076–2084, 2002.
35. Pollack IF, Claassen D, al-Shboul Q, et al: Low-grade gliomas of the cerebral hemispheres in children: An analysis of 71 cases. J Neurosurg 82(4):536–547, 1995.
36. Youland RS, Khwaja SS, Schomas DA, et al: Prognostic factors and survival patterns in pediatric low-grade gliomas over 4 decades. J Pediatr Hematol Oncol 35(3):197–205, 2013.
37. Reichenthal E, Feldman Z, Cohen ML: Hemispheric supratentorial low-grade astrocytomas. Neurochirurgia (Stuttg) 35:18–22, 1992.
38. Rudoler S, Corn BW, Werner-Wasik M: Patterns of tumor progression after radiotherapy for low-grade gliomas. Am J Clin Oncol 21:23–27, 1998.
39. Stockhammer F, Misch M, Helms HJ, et al: IDH1/2 mutations in WHO grade II astrocytomas associated with localization and seizure as the initial symptom. Seizure 21(3):194–197, 2012.
40. Fried I, Kim JH, Spencer DD: Limbic and neocortical gliomas associated with intractable seizures: A distinct clinicopathological group. Neurosur-gery 34:815–824, 1994.
41. Shaw EG, Scheithauer BW, Dinapoli RP: Low-grade hemispheric astrocy-tomas, Cambridge, 1997, Blackwell Scientific Publications.
42. Philippon JH, Clemenceau SH, Fauchon FH, et al: Supratentorial low-grade astrocytomas in adults. Neurosurgery 32(4):554–559, 1993.
43. Janny P, Cure H, Mohr M, et al: Low grade supratentorial astrocytomas. Management and prognostic factors [see comments]. Cancer 73(7):1937–1945, 1994.
44. Vertosick FT, Selker RG, Arena VC: Survival of patients with well-differentiated astrocytomas diagnosed in the era of computed tomography. Neurosurgery 28:496–501, 1991.
45. Shaw E, Arusell R, Scheithauer B, et al: Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: Initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study. J Clin Oncol 20(9):2267–2276, 2002.
46. Shaw EG, Berkey B, Coons SW, et al: Recurrence following neurosurgeon-determined gross-total resection of adult supratentorial low-grade glioma: Results of a prospective clinical trial. J Neurosurg 109(5):835–841, 2008.
47. Pallud J, Capelle L, Taillandier L, et al: Prognostic significance of imaging contrast enhancement for WHO grade II gliomas. Neuro-Oncol 11:176–182, 2009.
48. Chaichana KL, McGirt MJ, Niranjan A, et al: Prognostic significance of contrast-enhancing low-grade gliomas in adults and a review of the litera-ture. Neurol Res 31(9):931–939, 2009.
49. Kreth FW, Faist M, Rossner R, et al: Supratentorial World Health Organiza-tion Grade 2 astrocytomas and oligoastrocytomas. A new pattern of prog-nostic factors. Cancer 79(2):370–379, 1997.
50. Jenkinson MD, du Plessis DG, Smith TS, et al: Histological growth patterns and genotype in oligodendroglial tumours: Correlation with MRI features. Brain 129(Pt 7):1884–1891, 2006.
51. Saito T, Yamasaki F, Kajiwara Y, et al: Role of perfusion-weighted imaging at 3T in the histopathological differentiation between astrocytic and oligo-dendroglial tumors. Eur J Radiol 81(8):1863–1869, 2012.
52. Gorlia T, Wu W, Wang M, et al: New validated prognostic models and prognostic calculators in patients with low-grade gliomas diagnosed by central pathology review: A pooled analysis of EORTC/RTOG/NCCTG phase III clinical trials. Neuro-Oncol 15(11):1568–1579, 2013.
53. Shaw E: The low-grade glioma debate: Evidence defending the position of early radiation therapy. Clin Neurosurg 42:488–494, 1995.
54. van den Bent MJ, Afra D, de Witte O, et al: Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendro-glioma in adults: The EORTC 22845 randomised trial. [see comment][erratum appears in Lancet. 2006 Jun 3;367(9525):1818]. Lancet 366 (9490):985–990, 2005.
55. Rajan B, Pickuth D, Ashley S: The management of histologically unverified presumed cerebral gliomas with radiotherapy. Int J Radiat Oncol Biol Phys 28:405–413, 1993.
56. Kondziolka D, Lunsford LID, Martinez AJ: Unreliability of contemporary neurodiagnostic imaging in evaluating suspected adult supratentorial (low-grade) astrocytoma. J Neurosurg 79:533–536, 1993.
57. Florell RC, Macdonald DR, Irish WD, et al: Selection bias, survival, and brachytherapy for glioma. [erratum appears in J Neurosurg 1992 Sep;77(3):489]. J Neurosurg 76(2):179–183, 1992.

468.e2 PART A l Central Nervous System Tumors
58. Smith JS, Chang EF, Lamborn KR, et al: Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol 26(8):1338–1345, 2008.
59. Schomas DA, Laack NN, Rao RD, et al: Intracranial low-grade gliomas in adults: 30-year experience with long-term follow-up at Mayo Clinic. Neuro-Oncol 11(4):437–445, 2009.
60. Duffau H: A new philosophy in surgery for diffuse low-grade glioma (DLGG): Oncological and functional outcomes. Neurochirurgie 59(1):2–8, 2013.
61. Pallud J, Capelle L, Taillandier L, et al: The silent phase of diffuse low-grade gliomas. Is it when we missed the action? Acta Neurochir (Wien) 155(12):2237–2242, 2013.
62. Soffietti R, Baumert BG, Bello L, et al: Guidelines on management of low-grade gliomas: Report of an EFNS-EANO Task Force. Eur J Neurol 17(9):1124–1133, 2010.
63. Soffietti R, Borgognone M, Ducati A, et al: Efficacy of radiation therapy on seizures in low-grade astrocytomas. Neuro-Oncol 7(3):389, 2005.
64. Karim AB, Maat B, Hatlevoll R, et al: A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys 36(3):549–556, 1996.
65. Kiebert GM, Curran D, Aaronson NK, et al: Quality of life after radiation therapy of cerebral low-grade gliomas of the adult: Results of a randomised phase III trial on dose response (EORTC trial 22844). EORTC Radiotherapy Co-operative Group. Eur J Cancer 34(12):1902–1909, 1998.
66. Hauswald H, Rieken S, Ecker S, et al: First experiences in treatment of low-grade glioma grade I and II with proton therapy. Radiat Oncol 7:189, 2012.
67. Stege EM, Kros JM, de Bruin HG, et al: Successful treatment of low-grade oligodendroglial tumors with a chemotherapy regimen of procarbazine, lomustine, and vincristine. Cancer 103(4):802–809, 2005.
68. Hoang-Xuan K, Capelle L, Kujas M, et al: Temozolomide as initial treat-ment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol 22(15):3133–3138, 2004.
69. Brada M, Viviers L, Abson C, et al: Phase II study of primary temozolomide chemotherapy in patients with WHO grade II gliomas. [see comment]. Ann Oncol 14(12):1715–1721, 2003.
70. Buckner JC, Gesme D, O’Fallon JR, et al: Phase II trial of procarbazine, lomustine, and vincristine as initial therapy for patients with low-grade oligodendroglioma or oligoastrocytoma: Efficacy and associations with chromosomal abnormalities. J Clin Oncol 21(2):251–255, 2003.
71. Levin N, Lavon I, Zelikovitsh B, et al: Progressive low-grade oligodendro-gliomas: Response to temozolomide and correlation between genetic profile and O6-methylguanine DNA methyltransferase protein expression. Cancer 106(8):1759–1765, 2006.
72. Pace A, Vidiri A, Galie E, et al: Temozolomide chemotherapy for progres-sive low-grade glioma: Clinical benefits and radiological response.[see comment]. Ann Oncol 14(12):1722–1726, 2003.
73. Quinn JA, Reardon DA, Friedman AH, et al: Phase II trial of temozolomide in patients with progressive low-grade glioma. [see comment]. J Clin Oncol 21(4):646–651, 2003.
74. van den Bent MJ, Wefel JS, Schiff D, et al: Response assessment in neuro-oncology (a report of the RANO group): Assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12(6):583–593, 2011.
75. Taal W, Zonnenberg CBL, Bromberg JE, et al: MGMT assessed with methylation-specific (MS-) multiplex ligation-dependent probe amplifica-tion (MLPA) predicts response to temozolomide in progressive low-grade astrocytoma after radiotherapy. Neuro Oncol 10(5):868, 2008.
76. Shaw EG, Wang M, Coons SW, et al: Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supraten-torial adult low-grade glioma: Initial results of RTOG 9802. J Clin Oncol 30(25):3065–3070, 2012.
77. Baumert BG, Mason WP, Ryan G, et al: Temozolomide chemotherapy versus radiotherapy in molecularly characterized (1p loss) low-grade glioma: A randomized phase III intergroup study by the EORTC/NCIC-CTG/TROG/MRC-CTU (EORTC 22033–26033). J Clin Oncol 31(Suppl), 2013. abstr 2007.
78. Fisher BJ, Lui J, Macdonald DR, et al: A phase II study of a temozolomide-based chemoradiotherapy regimen for high-risk low-grade gliomas: Pre-liminary results of RTOG 0424. J Clin Oncol 31, 2013. abstr 2008.
79. Kleihues P, Ohgaki H: Genetics of glioma progression and the definition of primary and secondary glioblastoma. Brain Pathol 7:1131, 1997.
80. Blatt J, Jaffe R, Deutsch M: Neurofibromatosis and childhood tumors. Cancer 57:1225–1229, 1986.
81. Morreale VM, Ebersold MJ, Quast LM, et al: Cerebellar astrocytoma: Expe-rience with 54 cases surgically treated at the Mayo Clinic, Rochester, Minnesota, from 1978 to 1990. J Neurosurg 87:257–261, 1997.
82. Hallemeier CL, Pollock BE, Schomberg PJ, et al: Stereotactic radiosurgery for recurrent or unresectable pilocytic astrocytoma. Int J Radiat Oncol Biol Phys 83(1):107–112, 2012.
83. Kano H, Kondziolka D, Niranjan A, et al: Stereotactic radiosurgery for pilocytic astrocytomas part 1: Outcomes in adult patients. J Neurooncol 95:211–218, 2009.
84. Schindler G, Capper D, Meyer J, et al: Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in
pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilo-cytic astrocytoma. Acta Neuropathol 121(3):397–405, 2011.
85. Marton E, Feletti A, Orvieto E, et al: Malignant progression in pleomorphic xanthoastrocytoma: Personal experience and review of the literature. J Neurol Sci 252(2):144–153, 2007.
86. Leenstra JL, Rodriguez FJ, Frechette CM, et al: Central neurocytoma: Man-agement recommendations based on a 35-year experience. Int J Radiat Oncol Biol Phys 67(4):1145–1154, 2007.
87. Park HK, Steven DC: Stereotactic radiosurgery for central neurocytoma: A quantitative systematic review. J Neurooncol 108(1):115–121, 2012.
88. Rades D, Zwick L, Leppert J, et al: The role of postoperative radiotherapy for the treatment of gangliogliomas. Cancer 116(2):432–442, 2010.
89. Krouwer HGJ, Davis RL, McDermott MW: Gangliogliomas: A clinicopatho-logical study of 25 cases and review of the literature. J Neurooncol 17:139–154, 1993.
90. Shepherd CW, Scheithauer BW, Gomez MR: Subependymal giant-cell astro-cytomas: A clinical pathologic and flow cytometric study. Neurosurgery 28:864–868, 1991.
91. Franz DN, Belousova E, Sparagana S, et al: Efficacy and safety of everoli-mus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): A multicentre, randomised, placebo-controlled phase 3 trial. Lancet 381(9861):125–132, 2013.
92. Krueger DA, Care MM, Agricola K, et al: Everolimus long-term safety and efficacy in subependymal giant cell astrocytoma. Neurology 80(6):574–580, 2013.
93. Lombardi D, Scheithauer BW, Meyer FB: Symptomatic subependymoma: A clinicopathologic and flow cytometric study. J Neurosurg 75:583–588, 1991.
94. Francavilla TL, Miletich RS, De Chiro G: Positron emission tomography in the detection of malignant degeneration of low-grade gliomas. Neurosur-gery 24:1–5, 1989.
95. Henze M, Mohammed A, Schlemmer HP, et al: PET and SPECT for detec-tion of tumor progression in irradiated low-grade astrocytoma: A receiver-operating-characteristic analysis. J Nucl Med 45(4):579–586, 2004.
96. Hlaihel C, Guilloton L, Guyotat J, et al: Predictive value of multimodality MRI using conventional, perfusion, and spectroscopy MR in anaplastic transformation of low-grade oligodendrogliomas. J Neurooncol 97(1):73–80, 2010.
97. Liu X, Tian W, Kolar B, et al: MR diffusion tensor and perfusion-weighted imaging in preoperative grading of supratentorial nonenhancing gliomas. Neuro Oncol 13(4):447–455, 2011.
98. Forsyth PA, Kelly PJ, Cascino TI: Radiation necrosis or glioma recurrence: Is computer assisted stereotactic biopsy useful? J Neurosurg 82:436–444, 1995.
99. Leighton C, Fisher B, Bauman G, et al: Supratentorial low-grade glioma in adults: An analysis of prognostic factors and timing of radiation [see com-ments]. J Clin Oncol 15(4):1294–1301, 1997.
100. Combs SE, Ahmadi R, Schulz-Ertner D, et al: Recurrent low-grade gliomas: The role of fractionated stereotactic re-irradiation. J Neurooncol 71(3):319–323, 2005.
101. Fogh S, Glass C, Carry B, et al: Hypofractionated stereotactic radiotherapy as salvage therapy for recurrent low-grade glioma. Cancer Ther 7:423–428, 2009.
102. Danysz W, Parsons CG, Karcz-Kubicha M, et al: GlycineB antagonists as potential therapeutic agents. Previous hopes and present reality. Amino Acids 14(1–3):235–239, 1998.
103. Kaloshi G, Sierra del Rio M, Ducray F, et al: Nitrosourea-based chemo-therapy for low grade gliomas failing initial treatment with temozolomide. J Neurooncol 100(3):439–441, 2010.
104. van den Bent MJ, Chinot O, Boogerd W, et al: Second-line chemotherapy with temozolomide in recurrent oligodendroglioma after PCV (procarba-zine, lomustine and vincristine) chemotherapy: EORTC Brain Tumor Group phase II study 26972. Ann Oncol 14(4):599–602, 2003.
105. Kelly PJ, Daumas-Duport C, Scheithauer BW: Stereotactic histologic cor-relations of computed tomography and magnetic resonance imaging-defined abnormalities in patients with glial neoplasms. Mayo Clin Proc 62:450–459, 1987.
106. Bauman GS, Shaw EG, Cha S, et al: Some like it hot . . . and others not! Int J Radiat Oncol Biol Phys 74(5):1319–1322, 2009.
107. Laack NN, Brown PD: Cognitive sequelae of brain radiation in adults. Semin Oncol 31(5):702–713, 2004.
108. Shaw EG, Daumas-Duport C, Scheithauer BW, et al: Radiation therapy in the management of low-grade supratentorial astrocytomas. J Neurosurg 70(6):853–861, 1989.
109. Brown PD, Buckner JC, Uhm JH, et al: The neurocognitive effects of radiation in adult low-grade glioma patients. Neuro Oncol 5(3):161–167, 2003.
110. Reijneveld JC, Sitskoorn MM, Klein M, et al: Cognitive status and quality of life in patients with suspected versus proven low-grade gliomas. Neurol-ogy 56(5):618–623, 2001.
111. Armstrong CL, Hunter JV, Ledakis GE, et al: Late cognitive and radio-graphic changes related to radiotherapy: Initial prospective findings. [see comments.]. Neurology 59(1):40–48, 2002.
112. Laack NN, Brown PD, Ivnik RJ, et al: Cognitive function after radiotherapy for supratentorial low-grade glioma: A North Central Cancer Treatment

CHAPTER 26 l Low-Grade Gliomas 468.e3D
ISE
AS
E S
ITES
Group prospective study. Int J Radiat Oncol Biol Phys 63(4):1175–1183, 2005.
113. Torres IJ, Mundt AJ, Sweeney PJ, et al: A longitudinal neuropsychological study of partial brain radiation in adults with brain tumors. Neurology 60(7):1113–1118, 2003.
114. Vigliani MC, Sichez N, Poisson M, et al: A prospective study of cognitive functions following conventional radiotherapy for supratentorial gliomas in young adults: 4-year results. Int J Radiat Oncol Biol Phys 35(3):527–533, 1996.
115. Merchant TE, Conklin HM, Wu S, et al: Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: Prospective evalua-tion of cognitive, endocrine, and hearing deficits. J Clin Oncol 27(22):3691–3697, 2009.
116. Hirsch J-F, Sainte Rose C, Pierre-Kahn A: Benign astrocytic and oligoden-drocytic tumors of the cerebral hemispheres in children. J Neurosurg 70:568–572, 1989.
117. Dewit L, Van Der Schueren E, Ang KK: Low-grade astrocytoma in children treated by surgery and radiation therapy. Acta Radiol 23:1–8, 1984.