Pathology Review-Term1
-
Upload
shashidhar-venkatesh-murthy -
Category
Education
-
view
13 -
download
3
description
Transcript of Pathology Review-Term1

“Find the key to yourself and every door in the world
is open to you”Mother..
Know your Strengths, Weakness, Interests etc..

2013 Term 1 CPC 1 Title: Cardiovascular System 1/3 – Valvular Heart DiseaseSystem: Cardiovascular System
Aim: To train students in:Pathology, Clinical & population study of patients with valvular heart disease.
Objectives: 1. History taking & clinical examination of patient with valvular heart disease.
2. Physical examination - heart sounds both normal & abnormal.
3. Pathophysiology of common valve disorders (congenital & acquired) immune and developmental.
4. Review of basic sciences relating to embryogenesis of CVS system, immune system & autoimmunity.
5. Study of population & community/rural issues in rheumatic heart disease.
6. Understanding of cardiomyopathy (pathogenesis, common presentations)
7. Understanding of cyanotic and non-cyanotic congenital heart disease
Week learning overview:

2013 CPC-1.1
– Indigenous family from Cape York– one of seven children. Love sports.
• ‘Short winded’ since 6 months, worse since weeks, ‘heart pounding’, cough – no blood– Smokes 5 cigarettes/day, ‘gunja’ - occasional– Lives in a 4 bedroom house with 17 people *– fever & arthritis at 9y age*, off school for a month.– Brother gets injection every month since years *. – FH: Brother and mother have heart problems *...– Tall*, young*, JVP 4cm*.
Ms JM, 19-year-old woman living in a remote community who drops out of the local basketball team

Summary: ARF
Pancarditis + systemic(skin, joints, CNS)
Chronic RHD

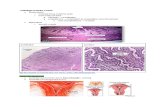
ARF Microscopy: Aschoff body.
Aschoff Body
ARF- MicroscopyAschoff body
1. Necrosis2. Macrophages3. T Lymphocytes4. Giant cells(Near a BV)
ARF- GrossPancarditis
1. Fibrinous Pericarditis2. Myocarditis3. Endocarditis4. Valve Vegetations.

RHD: Clinical Correlations:
?
?
?

AT BIRTH (%)• Ventricular Septal Defect 42*• Atrial Septal Defect 10• Pulmonary Stenosis 8• Patent Ductus Arteriosus 7• Fallot’s Tetralogy 5• Coarctation Of Aorta 5
Adults % *ASD 47VSD 34FT 11COA 10
Congenital Heart Disease:
Classification:LR Shunts: ASD, VSD & PDA.RL Shunts: Fallot’s, Trans.GA.Obstructions: COA, PS.
Etiology: Toxic, Gen, infecPathogenesis: EmbryogenesisMorphology: Clinical:

Infective Endocarditis:
NON INFECTIVE VALVE DISORDERS:• Non bacterial thrombotic..NBTE – marantic.• Libman-Sacks endocarditis – autoimmune – APL sy.• Endocardial myofibrosis in Carcinoid syndrome.
Prosthetic valves – Mech/Bio, infec, thromb, hemolysis.
Intro: ABE- Staph, SBE- StrepEtiology: Abnormal valve, infecPathogenesis: EmbryogenesisMorphology: Valve destruction, bacterial growth.Clinical: Fever, flu, murmur, petechiae.

Aortic valve calcification:• most common cause of aortic
stenosis.• Etiology: calcification from
progressive age-associated "wear and tear".
• More in Congenital bicuspid aortic valve, Rheumatic (10%).
• Pathology:• Thick, irregular, fibrosed, with
nodules of calcification.• LVH & Failure. LVH

Cardiomyopathy:
• Intrinsic myocardial dysfunction, Primary structural abnorm.
• Congenital / Acquired.• Types:
– Dilated 90%– Hypertrophic– Restrictive.
10

“Some people grumble that roses have thorns; I am grateful
that thorns have roses.”-- Alphonse Karr
Look for good in others, no one is without faults & every one has some good quality!

2013 Term 1 CPC 2 Title: Cardiovascular System 2/4 – IHDSystem: Cardiovascular System
Aim: To train students in:Basic Pathology, clinical skills & population study of patients with ischaemic heart disease.
Objectives: 1. History taking & clinical examination of patient with Acute Coronary Syndrome (ACS).
2. Pathophysiology of ischaemic heart disease.3. Review of Basic sciences relating to CVS –
Anatomy, Physiology.4. Study of Population & community/rural issues
in life style associated diseases.
CPC12: Week overview:

CPC13-1.2 – Chest pain.
• While climbing steps* 15-20min, Pale, unwell, no pain now. Burning sensation in her neck.
• Similar episodes - 2y, more frequent now. Centre of sternum, no radiation*
• ↑Exertion, stress - ↓rest*• HPTN 15y, Dyslipidemia 8y, GORD 7y, • P/H: Chest pain, weak heart, no blocks.• F/H: Smoker, 1pack/day 25y, IHD, DM2,
Mrs. J.B 45 year old Aboriginal woman Presents for an urgent visit complaining of SOB, ‘oppressive feeling’ in her chest

Pathogenesis:1. intimal injury (at bifurcations)2. Inflammatory cells & macrophages.3. Lipid deposition, Central Necrosis,
more inflammation (soft plaque)4. Fibrosis, smooth muscle proliferation
(hard plaque)5. Complications – activaton, Thrombosis,
embolism, aneurism, dissection & rupture.

DANGER FACTORS• Low SMC.• Thin cap.• High Inflammation.• Large lipid core.
Plaque Biology:

Morphologic types:
Dots/streaks Soft Plaques Complicated Pl.

Atheroma types:

IHD Pathogenesis:
Stable
Unstable
Coronary block:
• <70% - Asymptomatic.
• >70-75% - Stable Angina
(exersion)
• 90% - Fixed stenosis (rest)
Chronic IHD
• Plaque change: (ACS)– Rupture, fissure, ulcer,
thromb/embolism.
– Unstable angina, MI / SCD

Common Sites:• Large BV : Aorta, Carotid & Iliac.
(large vessels) – Bruit.• Medium BV : Coronary,
Cerebral, Limbs, viscera – ischemia.
Why?
* AS never affects veins or small arteries.
* Microangiopathy is not due to AS
* AS is not a risk factor for DVT
* Alcohol is not a risk factor for AS.
* LDL is not bad type of cholesterol*

No Q wave - Q wave
Why spared?

What is important in this world is not where we are, but in which direction we are moving.
-- Oliver Wendell Holmes, Jr.

Location of MI & Involved Coronary A.

Morphology - Gross & Microscopic
Time (approx) GROSS MICROSCOPY
Up to 4 hour None None (loss of glycogen/LDH)
4 - 24 hours Gradually deepening dark area surrounded by erythema. Oedema.
Beginning coagulation necrosis contraction bands. Pyknotic nuclei, Oedema, few acute inflammatory cells.
3-7 days Pale / Yellow centre with haemorrhagic border
Obvious necrosis of muscle and plenty of Neutrophils hemorrhage (more if reperfusion injury) few macrophages.
1-3 weeks Pale, thin (loss of tissue mass) pale grey area with red border.
No muscle, Granulation tissue, macrophages prominent capillaries, fibroblasts.
3-6 weeks(permanent)
Small Silvery white scar . Replacement of granulation tissue by dense fibrosis

Myocardial Infarction: duration
Old & Recent

MI – stages.
Normal <1day Coagulative necrosis <7 days Acute inflam.
1-3 wk Granulation 3-6 wk Scar 3-6wk scar.

Complications of MI:
A Anterior myocardial rupture . B Rupture ventricular septum C Rupture papillary muscle. D Fibrinous pericarditis (dark, rough) E Thinning and mural thrombus. F aneurysm

“Be like a postage stamp”Stick to one thing until you get there...!
- Josh Billings…

2013 Term 1 CPC 3
Title: Cardiovascular 3/4 - PVD
System: Cardiovascular System, SkinAim: To train students in :
Clinical, Pathology & population study of patients with arterial + venous disorders + skin lesions.
Objectives: 1. History taking & clinical examination of patients with peripheral vascular disease
2. Clinical examination of peripheral circulation.3. Clinical examination of skin & skin lesions.4. Pathophysiology of common arterial and venous disorders.
Atherosclerosis & Deep vein thrombosis.5. Pathophysiology of common skin disorders Infection,
inflammation & malignancy. (Review MB3-TIN)6. Pathophysiology of Ischemia, infarction, and necrosis. (Review
MB3-TIN)7. Review of Basic sciences relating to structure and function of
blood vessels. Fluid balance and dynamics of micro capillary circulation & Pathophysiology of oedema formation.
8. Epidemiology of lifestyle diseases, population & community/rural issues in life style disorders specifically atherosclerosis.

Chronic leg ulcers: DD
• Venous : Varicose veins, Thrombophlebitis.
• Arterial : Atherosclerosis, Diabetes*.• Neuropathic : Diabetes*• Malignancy : BCC, SCC, MM• Infections : leprosy, TB, Treponemal, (Yaws)
• Others : Dermatitis, Vasculitis, Lymphedema..
Leg ulcers 1% Venous 80% - Arterial 10% * RACGP

Venous ulcers: (Wet, Bleeding, Dermatitis.
• Cause: Varicose veins.• Location: Gaiter region. • Features:
– large, irregular, shallow.– Wet edematous, oozing.– Moist granulating base – bleeds on
touch.– Surrounding eczematous stasis
dermatitis.– Mild pain, relieved by elevation. – Compression bandage helps.

Arterial Ulcers: (Dry & Painful)
• Cause: AS (PVD, DM2)• Location: distal & dorsal foot or toes.• Features:
– Cold, pale feet, absent or weak pulses. – Dry, Irregular clear border, grey black
necrotic. – Pale granulation, Does not bleed on
touch. – Painful (Nocturnal) partly relieved by
dependency.– Skin: Shiny, loss of hair – atrophy.
* Note: Angiogram, no compression bandage..

Neuropathic ulcers: (Clean, Caving, Callus)
• Cause: Nerve damage.• Location: Distal leg, pressure points.• Features:
– Punched-out ulcers, deep caving. – Frequently painless, loss or weak pulses. – Often with surrounding calluses
(hyperkeratosis)– Probing or debriding leads to brisk bleeding. – May also have Impaired sensation and
diminished positional sense or 2-point discrimination.

Malignant ulcers: (Exposed, tumour)
• Cause: UV-rays, Idiopathic.• Location: Sun exposed*.• Features: (remember ABCDE…!)
– irregular, Punched-out, deep, caving or with tumour.
– Frequently painless.– Lymphnodes, spreading, metastases.– Cancer cachexia – weight loss etc.

Infectious ulcers: multiple,
• Cause: TB, Treponema (Yaws, Pinta), etc.
• Location: not particular, multiple.• Features:
– irregular, non specific. – Lymphadenitis.

DVT: Typical Clinical History:• 34 year male – sudden chest pain and
collapse while recovering 12 days after orthopaedic surgery for comminuted # of femur.
• 68 year male AS, past MI, chest pain following 24 hour flight travel.
• 28 year female, recurrent abortions.• 54 year obese female, tender calf muscles.• Pregnancy, OCP, flight, surgery,

Risk Factors for DVT• Virchow’s triad: (Flow– Blood - Vessel)
– Stasis, Hypercoagulability & BV injury.
• Stasis (flow)– Immobilization, paralysis, in-patients, heart failure.
• Hypercoagulability (Blood):– Congenital: AT III, Protein-C/S deficiency, F V Leiden– Acquired: Lupus & anti cardiolipin anticoagulants, – Drugs, Oral contraceptives, Hyperhomocysteinemia.– Hyperviscosity – Polycythemia, paraproteins.
• Tissue damage (Vessel):– Surgery, Trauma, MI, Stroke, Malignancy, Phlebitis.

Varicose Veins:• Tortuous superficial veins due
to valve defect in deep veins of lower limb.
• Congenital / Acquired.• Tortuous prominent veins.• Gaiter region.• Thrombosis & ulceration.• Over Medial malleolus.• Note: No DVT* or PE*

Leg Veins & varicosity:

Common Immune Vasculitis:

Raynaud’s Phenomenon:• Vasoconstriction of digital arteries.• Cold/emotional trigger.• Primary: R.disease – genetic 3-5%• Secondary: Vasculitis, SLE, Buergers,
atherosclerosis, cold Ab hemolytic anemia etc.
Pallor Cyanosis

Polyarteritis nodosa:• Rare, Immune, HBs ag.• Systemic vasculitis with
necrotizing inflammation.• Nodules over arteries.• Acute fever, muscle & joint
pain, asymetric polyarthritis • Malaise rash & weight loss.• Neuropathy, kidney failure,.• High ESR, CRP, WBC.• Treat: Immunosuppression. Fibrin
oid NecrosisIn
flam
mato
ry cells

Wegener’s granulomatosis:
Granulomatous inflammation around small vessels with epitheloid cells and giant cells. Lung specimen showing cavitating grey white lesions. (similar to TB)

Buerger’s Disease:• Thromboangiitis
obliterans• Strong association with
smoking.• Common Males, Jews.• Peripheral gangrene• Small artery in limbs
thrombosis & fibrosis. • Also involves veins &
surrounding tissue.

Giant cell arteritis:
Aorta Temporal Art. Nodular segmental thickening, Most common in adults, T-cell Granuloma + Giant cells, Ophthalmic artery blindness

That person who declares that there is always something wrong is
always doing something to make things wrong.
— Christian Larson

CPC14: Week overview:2013 Term 1
CPC 4Title: Respiratory 1/3 - Pneumonia
System: Respiratory SystemAim: To train students in :
Clinical, Pathology & population study of patients with pneumonia COPD, and pneumoconiosis.
Objectives: 1. History taking & clinical examination of patients with a chronic lung disease (COPD, asthma, TB, fungal & other chronic infections) and acute infection (pneumonia).
2. Review of Basic sciences relating to structure and function of lungs. Blood gas physiology, measurement of blood gasses and lung function tests, sputum cytology and serology in lung infection.
3. Pathology of chronic obstructive airway disorders.4. Pathophysiology of acute respiratory infection.5. Pathophysiology of occupational, environmental & smoking related lung disorders. 6. Pathophysiology of common and important rare causes of pneumonia, particularly
tropical illnesses.7. Physical examination of Respiratory system.8. Complications of pneumonia. 9. Interpretation of Chest X-rays.10. Epidemiology of pneumonia in Australia, South East Asia and The Tropics.11. Role of health promotion, screening, public health in acute and chronic pneumonic
conditions.12. Smoking & lung disease. Role of health promotion, Population & community/rural
issues in smoking & work related lung disorders (pneumoconiosis).

Pneumonia
47
Pathogenesis of Pulmonary Infections
Aspiration, Inhalation, Inoculation, Colonization, Hematogenous & Direct spread

Pneumonia
48
Pneumonia Types:
Etiologic Types: Infective
Viral Bacterial Fungal Tuberculosis
Non Infective Toxins chemical Aspiration
Morphologic types: Lobar Broncho InterstitialDuration: Acute ChronicClinical: Primary /
secondary. Typical / Atypical Community a /
hospital a

Pneumonia
49
Types of Pneumonias & Causative agents
Community-Acquired Typical Pneumonia: Strep, H.influenzae, Staph aureus, Klebsiella.
Community-Acquired Atypical Pneumonia: Mycoplasma, Chlamydia, Legionella, SARS*, Q
Fever Nosocomial Pneumonia:
Klebsiella spp., Serratia, E coli, Pseudomonas Aspiration Pneumonia:
Anaerobic oral flora (Bacteroides) Chronic Pneumonia:
Nocardia, Actinomyces, Atyp. Mycob, Fungal (TB) Necrotizing Pneumonia and Lung
Abscess: Anaerobic bacteria
Pneumonia in the Immunocompromised: CMV, Pneumocystis, Atyp. Mycob. Fungal.

CongestionRed Hepatisation
Grey HepatizationResolution
Pathogenesis of Pneumonia

Pneumonia
51
Stages of pneunomia:

Pneumonia
52
Broncho – Pneumonia - Lobar
Extremes of age. Secondary, in sick. Both genders. Staph, Strep, H.infl. Patchy consolidation Around Small Bronchi Not limited by anatomic
boundaries. Usually bilateral.
Middle age – 20-50 Primary in a healthy adult. males common. 95% pneumococcus
(Klebs.) Entire lobe consolidation Diffuse Limited by anatomic
boundaries. Usually unilateral

Pneumonia
53
Chronic Pneumonia Chronic, lymphoid infiltrate, No classic stages. Lung destruction. Organisms
TB, Fungal etc.
Interstitial pneumonia
Viral
NON INFECTIVE PNEUMONIA:• Aspiration pneumonia
• Lower lobe, sec infection, abscess.
• Lipid pneumonia• Airway obstruction,
atelectasis.• Eosinophilic pneumonia
• Asthma, Löffler's syndrome.

The ability to concentrate and to use your time well is everything if you want to succeed in business, or anywhere else for that matter!-- Lee Iacocca

CPC15: Week overview:2013 Term 1 CPC 5 Title: Respiratory 2/2 - Asthma & COPD
System: Respiratory SystemAim: To train students in :
Clinical, Pathology and Population studies of patients with Upper Airway Disease Processes. Asthma, Chronic Cough, Emphysema, COPD, Chronic Bronchitis and Acute Bronchitis. [Epiglottitis, Croup]
Objectives:
1. History taking & clinical examination of patients with obstructive airway disease, upper airway disease.
2. Physical examination of Respiratory system.3. Review of Basic sciences relating to structure and
function of lungs. Blood gas physiology, measurement of blood gasses and lung function tests,
4. Pathophysiology of acute upper airway injury.

Pathogenesis of COPD
1. Smoke, irritants, carcinogens.
2. Tissue irritation & destruction
3. Inflam Mucous production.
4. Airway thickening narrowing.
5. Alveolar damage widening.• Increase in
– Alveolar marcrophages– CD8 Lymphocytes– Neutrophils– Proteases.
• Airway damage Bronchitis• Alveoli damage Emphysema.• Both COPD.
α1AT def.. Emphysema
Bronchitis Emphysema

Both affected commonly COPD

COPD: Overlap of Clinical syndromes
COPD

Normal - COPD
CB
Emphysema

Restrictive lung disorders:Definition: Reduced expansion.
A. Intrinsic Lung Disorders:– Sarcoidosis, pneumoconiosis.– TB, Interstitial Pneumonia
B. Extrinsic Dis. (chest wall):– Scoliosis, Kyphosis, Obesity,– Pleurisy, rib fracture etc.
C. Neuromuscular Disorders:– Paralysis of the diaphragm,
Myasthenia Gravis, Poliomyelitis.
Pathogenesis

Silicosis:• Inorganic – sand & stone
dust.• Toxic to macrophages –
destruction fibrosis.• Scattered multiple small,
fibrotic Nodules• Surrounding Irregular
emphysema.• Restrictive pattern of
PFT.

Asbestosis:• Asbestos bodies in sputum.
– (Protein & Hemosiderin)
• “Inconsumable”, Beaded 5-100mm x 0.25mm.
• Within alveoli at lung bases.• Dyspnoea, dry cough• Clubbing is common.• Diffuse effusion consolidation*,
fibrosis Honey comb lung.

Coal Miner’s Lung:• Athraco-Silicosis:• Dense cardon
pigmentation – Anthracosis and nodules of silicosis.
• Commonly seen in coal miners.
• Only anthracosis no fibrosis or damage.

Sarcoidosis:• Granulomatous, immune,
multisystem disorder. • Unknown Etiology.• Multiple fine nodules.• Like TB (no caseation).• Smokers – Uncommon• SOB, Erythema nodosum,
lymphadenopathy, hypercalcemia, nephrocalcinosis, occular, skin & nerve damage.. Etc.
• Stage I asymptomatic to Stage IV – Pulm fibrosis.

Restrictive vs Obstructive• Interstitial - (stiff lung)• Increased tissue •Relatively normal FEV1:FVC ratio
•Normal PEFR. •Types:•Acute – ARDS,Viral.•Chronic - pneumoconioses & sarcoidosis, Int. fibrosis.
•Obstructive (soft lung)•Destruction of tissue.•Low FEV1:VC ratio
•Low PEFR.•Types:
–Localised & Diffuse–Reversible & progressive.–COPD –Asthma–Bronchiectasis,

Asthma : Pathogenesis
Early phase (immediate) and late phase reactions

Asthma Morphology:
Asthma Microscopy1.Mucous Plugs +eosinophils2.Goblet cell hyperplasia3.Inflammation + Eosinophils4.Smooth muscle hyperplasia5.Mucous gl. Hyperplasia.

Lung Function Tests:

Whether you think that you can or that you can't,
you are usually right…!
– Henry Ford

CPC16: Week overview:2013 Term 1 CPC 6 Respiratory 3/3 – Lung cancer
System: Respiratory SystemAim: To train students in:
Clinical, pathological & population study of patients with lung cancer & smoking related lung diseases.
Objectives: 1. History taking & clinical examination of patients for chronic lung disease & smoking (COPD, cancer etc)
2. Physical examination of patient with respiratory symptoms.3. Pathophysiology of smoking related lung diseases.4. Pathophysiology of lung cancers.5. Review of basic sciences relating to structure and function of
lungs. Blood gas physiology, measurement of blood gases and lung function tests.
6. Pathophysiology of environmental & smoking related cancer development (carcinogenesis, chemical, radiation, viral etc.)
7. Epidemiology of smoking related disorders in Australia.8. Role of health promotion, population & community/rural issues
in smoking & work related lung disorders (pneumoconiosis).

Pathogenesis – Lung Cancer.
3pK-RasC-myc
p53
Irritation Carcinogens Initiation Promotion Ca.
Pathogenesis:1. Smoking – carcinogens2. 3p – tumor suppressor gene loss3. Mutations (p53, KRAS, EGFR..)4. Dysplasia5. Infiltration6. Spread7. Metastases.

Biology of Cancer:• Grading Differentiation Microscopic• Staging Progression Clinical - TNM
Low Grade high
• T – Tumor (T1-4)
• N – Node (N1-3)
• M – Metastasis (M0-1)
Stage

Lung tumors Classification:
• Bronchogenic Carcinoma: (95%)– Small cell carcinoma SCC 20%– Non Small Cell Carcinoma NSCC 80%
• Adeno carcinoma ~40%*• Squamous carcinoma ~35%• Large cell anaplastic ~5%
• Other Tumours (5%)– Bronchial Carcinoid Tumor– Lung Hamartoma
• Metastatis (more common)• Tumors of Pleura - Mesothelioma• Mediastinal Tumours
– Thymic & other Lymphoma, Teratoma.
SCCSq
Big 3
Ad
SCC NSCC

SCC Sq. Ca Ad. Ca

Common types of Lung Ca: Biopsy
Adeno carcinoma Squamous Ca. Small Cell CaPeripheral Central CentralLocalised Localised DiffuseFemale Males MalesNon smokers Smokers SmokersGlands Keratin Oat cellPale Blue Pink Dark Blue

Lung Ca – Cytology
Adeno carcinoma Squamous Ca. Small Cell CaGland formation Pink Cytoplasm little cytoplasmMucin Keratin nil
EGFR (bevacizumab) Epithelial marker NeuroendocrineALK, KRAS PTH-rp, ACTH, ADH, Calcitonin

Clinical features & complications.• Local:
– Obstruction– Effusion– Pneumonia* lipid, other.– Bronchiectasis– Atelectasis– Haemoptysis– COPD (risk)
• Systemic:– Cachexia– Paraneoplastic sy– Clubbing– Pulm. Osteoarthropathy.– Bone pain– CNS dysfunction

Carcinoid Tumour:
• Young <40y, • No relation to smoking. • Bronchus, Small polypoid submucosal (<4cm)• Neuroendocrine cells, secrete seratonin carcinoid
syndrome (intermittent attacks of diarrhea, flushing and cyanosis).
• behave benign even with nodal spread (no distant metastases).
• Uniform clusters with capillaries (endocrine pattern)

Mesothelioma:• 50% history of asbestos exposure.• Latent period of 25-40 years.• Preceded by pleural fibrous plaques.• Encases lungs from pleura.• Biphasic: (Carcinoma+Sarcoma)
Epithelial and fibrous components.

“A good scare is worth more to a man than good advice."
- Edgar Watson Howe - Country Town Sayings (1911)
That’s why we have…. Exams!

CPC17: Week overview:
2013 Term 1 CPC 7 Title: Cardiovascular System 4/4 – Hypertension & CCFSystem: Cardiovascular System
Aim: Clinical presentation, pathology and population studies of patients with Hypertension and Cardiac Failure.
Objectives: 1. History taking and Clinical examination of patients with hypertension.
2. Clinical examination of patients with Heart Failure.3. Pathophysiology of HT and CCF4. Anatomy of CVS5. Complications of Hypertension---CCF, AF, CVA, Renal
Failure, Retinal changes, Central vein thrombosis, Aortic Aneurysm and Aortic Dissection.

Blood Pressure:
82
(Aorta)
Cerebral / Coronary arteries
Resistant chamber
• Pressure = Pump + Resistance.• BP = Cardiac Output + BV. Res.• BP = CO + PR• Heart function, Blood volume, BV
elasticity control BP.• Kidney function important control.• Water*, Sodium* & BV tone*• Renin & Angiotensin system.
Measurements
BP
mmHg
• Pulse Pressure: 120-80 = 40 mmHg• Central Venous Pressure: 6 mmHg• Mean Arterial Pressure: DP+1/3PP = 93• Pulmonary Pressure: 20/10 mmHg• Cardiac Output: 4-8 L/min

Control of Blood Pressure:
83
Kidney BP Control:• Heart• Kidney• Hormones• Nerves

Complications: • BV thickening – Ischemia – Claudication.• Chronic, end organ & vascular damage.• Infarction(MI), Hemorrhage, Stroke & Aneurysm.

Heart Failure- PathophysiologyRenin Angiotensin Aldosterone BP & Fluid retention.
85
12
3
Low BloodLow GFR
High Fluid & High PR = High BP

Neurohormonal Mechanisms in HF
86
Inciting event

Hypertension
87

Ventricular Hypertrophy
88
LVH RVH
Systemic Hypertension Pulmonary Hypertension
>2 cm

Microangiopathy in Hypertension:• Hyaline arteriolosclerosis:
– Pink, hyaline thickening of vessel walls – narrowing of lumen
• Hyperplastic arteriolosclerosis:
– malignant hypertension : definition?– concentric laminated thickening of walls (“onion skin”) – Narrowing of lumen - smooth muscle proliferation
89
“onion skin”

Benign Nephrosclerosis
“Grain-leather kidney”
Hyaline arteriolosclerosis

Subarachnoid HaemorrhageIntracerebral haemorrhage (Stroke)
Hypertensive Intracranial haemorrhage

Hypertensive Retinopathy
• Grade I – Thickening of arterioles.
• Grade II – Focal Arteriolar spasms. Vein constriction. (AV nipping)
• Grade III – Hemorrhages (Flame shape), dot-blot and Cotton wool (ischemia) and hard waxy exudates (lipid deposition).
• Grade IV - Papilloedema

“Intelligence plus character, that is the goal of true education”
- Martin Luther King Jr.

Terminal cancer vs CHF
94
Worsening & compensatory mechanisms.

Compensatory Mechanisms:• Frank-Starling mechanism:
– More stretch – more contraction.• Neurohumoral activation:
– Vaso constrictors – norepinephrine– Renin-Angiotensin system.– Atrial Natriuretic Peptide – (opposite effect)
• Compensatory Hypertrophy of Heart:– Pathologic Hypertrophy:
• concentric, pressure, high mortality.
– Physiologic Hypertrophy• Eccentric, Volume, more BV, e.g. exercise.
95

LVF: Pulmonary odema, Brown induration
96“Heart-failure cells”
Brown induration of lung.

“To educate a person in the mind but not in morals is to educate a menace to society.”
-Theodore Roosevelt

“Identifying your Goal is like identifying the North Star, you fix your compass on it and then
use it as the means of getting back on track when you tend to stray”
-- Marshall Dimock
What am I doing? - Where am I going?(Where I want to be in 5 years?)

Wish you all Success, Health,
& Happiness in life.
Need help for exams? You can still contact me..