Pathogenesis of diseases of the Pituitary, Pineal, Thyroid and Parathyroid Glands Trinity Medical...
-
Upload
charlotte-turner -
Category
Documents
-
view
224 -
download
1
Transcript of Pathogenesis of diseases of the Pituitary, Pineal, Thyroid and Parathyroid Glands Trinity Medical...
Pathogenesis of diseases of the Pituitary, Pineal, Thyroid and Parathyroid Glands
Trinity Medical School Dublin
Dr. B. Loftus
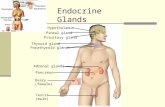
Endocrine System
Highly integrated group of organs that maintains metabolic equilibrium
Hormones act on distant target cells-concept of feedback inhibition
Endocrine disease may be due to underproduction or overproduction of hormones, or mass lesions
Adenohypophysis:cell types
Acidophils secrete growth hormone (GH) and prolactin (PRL)
Basophils secrete corticotrophin (ACTH), thyroid stimulation hormone (TSH), and the gonadotrophins follicle stimulating hormone (FSH) and luteinizing hormone (LH).
Chromophobes have few cytoplasmic granules but may have secretory activity
Cell population of the anterior pituitary
Somatotroph (GH) 50% (acidophils)
Lactotroph (PRL) 20% (acidophils)
Corticotroph (ACTH) 20% (basophils)
Thyrotroph/Gonadotroph 10% (basophils) (TSH/FSH/LH)
Neurohypophysis
Resembles neural tissue with glial cells, nerve fibres, nerve endings and intra-axonal neurosecretory granules
ADH (antidiuretic hormone, vasopressin) and oxytocin made in the hypothalmus are transported into the intra-axonal neurosecretory granules where they are released
Control of Anterior Pituitary Function
The Neuroendocrine Axis Cerebral cortical effects on hypothalamic
nuclei Hypothalamic releasing and release-
inhibiting factors Ambient levels of target-organ hormone
product
Causes of Pituitary Hypofunction
Infarction: Post-partum (Sheehans syn.)DICSickle cell anaemiaTemporal arteritisDM/hypovolaemiaCav. sinus thrombosis
Compression: Non-functional tumourCraniopharyngiomaTeratoma
Infection: TB meningitis
Symptoms and Signs of Pituitary Hypofunction Acute (adult):
Apoplexy failure of lactation secondary amenorrhoea
Chronic (adult): Myxedema Hypoadrenalism hair loss/depigmentation hypothermia hypoglycaemia
Chronic (childhood): proportional dwarfism Frolich’s syndrome
Effects of Pituitary Tumour
Hormone overproductionHormone overproduction (e.g.TSH) with normal production of other hormones
Hormone overproductionHormone overproduction with reduced production of other hormones
Pressure atrophyPressure atrophy of gland with panhypopituitarism (non-functioning)
Space-occupying lesion lesion in the skull
Clinically Significant Pituitary Tumours
Lactotroph 32.0% Somatotroph 21.0% Corticotroph 13.0% Mixed somato/lacto 6.0% Gonadotroph 1.0% Thyrotroph 0.5% Non-functional 26.5%
Syndromes of Common Functional Pituitary Adenomas
Lactotroph (PRL) Galactorrhoea
Amenorrhoea Somatotroph (GH) Acromegaly
Gigantism
Corticotroph (ACTH) Cushing’s disease
Acromegaly: clinical features Median age 30+. Equal male/female incidence.
Characterised by acral enlargement, increased soft tissue mass, arthritis and osteoporosis. Diabetes develops in 30%. Serum GH elevated.
Possible compressive effects of tumour include visual field defects (bitemporal hemianopia), hypogonadism and amenorrhoea.
Tumours often display synthetic infidelity and may cause galactorrhoea, hyperpigmentation, hyperthyroidism, virilisation or adrenal hyperplasia
The condition of gigantism develops if epiphyses are unfused
Secondary Abnormalities of the Pituitary
“Feedback” tumours due to adrenal, thyroid or gonadal failure (Nelson-Salassa syndrome)
“Crooke’s hyaline change” in corticotrophs due to high plasma cortisol
Empty Sella Syndrome
The pituitary undergoes pressure atrophy due to a suprasellar mass compressing the gland in the sella turcica.
The pituitary becomes completely flattened, and clinical hypopituitarism accompanies this.
Diabetes Insipidus
Failure of ADH release from posterior pituitary due to destruction of hypothalamic-pituitary axons
Causes polyuria of up to 10L daily of low specific gravity urine with concomitant hypovolaemia and hypernatraemia
Urine specific gravity does not alter with fluid deprivation but increases with parenteral ADH
Cushing Disease/Syndrome
Cushing disease: overproduction of adrenal cortical glucocorticoids secondary to overstimulation by ACTH
Cushing syndrome: similar to Cushing disease, but is caused by adrenal cortical adenoma, adrenal cortical hyperplasia or adrenal cortical carcinoma
PINEAL GLAND
Pinecone shaped, minute, 180mg, at base of brain
Stroma and pineocytes (photosensory and neuroendocrine)
TUMOURS: Germinomas, teratomas (sequestered germ
cells)Pinealomas (pineoblastoma, pineocytoma)
Thyroid Hormone SynthesisI- I2 + tyrosine
Mono-iodotyrosine
Di-iodotyrosine
Triiodothyronine (T3) Thyroxine (T4)
Thyroid Hormone Secretion
T3 (triiodothyronine) and T4 (thyroxine) are secreted into the rich vascular supply of the interstitium
The “C” cells of the interstitium secrete calcitonin which lowers serum calcium but has minimal functionality
Metabolic Effects of Thyroid Hormone
1. Uncouples oxidative phosphorylation
a. less effective ATP synthesis
b. greater heat release
2. Increases cardiac output, blood volume and systolic blood pressure
3. Increases gastrointestinal motility
4. Increases O2 consumption by muscle, leading to increased muscular activity with weakness
Thyroid Gland Development
Downward migration of epithelium from foramen caecum of tongue along the thyroglossal duct
Thyroglossal duct cysts develop from remnants of this path
Types of Thyroiditis Lymphocytic (focal) :immunologic basis? Hashimoto (struma lymphomatosa):
antithyroid microsomal antibodies Atrophic (primary myxedema):
antithyroid microsomal antibodies Granulomatous (de Quervain’s):mumps
or adenoviral antibodies Invasive fibrous (Riedel’s): unknown but
associated with fibromatosis
Hashimoto Thyroiditis
Middle aged females. Diffuse rubbery goitre; initially painless, later atrophy
50% hypothyroid at presentation, many euthyroid, minority hyperthyroid
All become hypothyroid eventually Strong assn. with other autoimmune disease including
SLE, RA, pernicious anaemia, Sjogren’s syndrome Antibodies to TSH and thyroid peroxidases Lymphocytic infiltration, Hurthle cell change, follicle
destruction, replacement fibrosis
Hashimoto Thyroiditis-pathogenesis
Abnormal T cell activation and B cell stimulation to secrete a variety of autoantibodies.
Antibodies to TSH and thyroid peroxidases (antimicrosomal)
De Quervain’s Thyroiditis
Subacute granulomatous thyroiditis Self-limited disease, weeks to months Painful enlargement of thyroid Microscopy shows numerous foreign-
body giant cells and destruction of follicles
Primary Hypothyroidism
Low T4, low BMR: Slow mentation,bradycardia,constipation,
muscle weakness, coarse and scanty hair, menorrhagia, cold sensitivity
Increased tissue mucopolysaccharide: non-pitting oedema, hoarseness, cardiomegaly
Hypercholesterolemia: accelerated atherosclerosis
Commonest cause is autoantibodies to TSH
Hypothyroidism in infants
Cretinism goitre in endemic cretinism pale cold skin with myxedema mental retardation stunted growth protruding tongue, round face
Aetiology of Simple Goitre (euthyroid, enlargement without nodularity) Absolute or relative lack of iodine: endemic goitre Inherited enzyme defects (dyshormogenesis):
iodine trapping, organification, coupling, deiodination
Excess dietary goitrogens :cassava, brassica, turnip, cabbage, kale, sprouts- these suppress the synthesis of T3 and T4
Treatment with thiourea Increased physiologic demand on function, e.g.
puberty, pregnancy, stress
Colloid Cysts
Appear as “cold” nodules on scanning, do not take up radioactive iodine
Usually an incidental finding
Multinodular Goitre
Also known as colloid goitre End result of long-standing ‘simple’ goitre The gland is enlarged and weighs over
30g Majority of patients are euthyroid Presents as swelling in the neck Commonest cause of enlarged thyroid
Clinical features of Primary Hyperthyroidism
SYMPTOMS Weight loss Nervousness Heat intolerance Palpitation Diarrhoea Amenorrhoea
SIGNS Tachycardia Warm, moist palms Lid-lag Diffuse Goitre +/- bruit Tremor High T4, low TSH
Causes of Hyperthyroidism
Grave’s Disease (diffuse hyperplasia) Ingested exogenous hormone Hyperfunctional adenoma Hyperfunctional multinodular goitre Thyroiditis
Features unique to Grave’s Hyperthyroidism
Exophthalmos Lymphoid hyperplasia Pretibial Myxedema Pathogenesis is autoantibodies that bind
and activate TSH receptors on follicular cells Strong association with other autoimmune
diseases e.g. PA and myasthenia gravis
Thyroid Storm
Severe hyperthyroid symptoms Hyperpyrexia Dehydration Hypertension Tachycardia, arrthymias Shock May be fatal
Thyroid Adenoma
Uncommon benign tumours of thyroid follicular epithelium which occur at any age but with female preponderance (6F:1M)
Solitary Encapsulated Uniform internal pattern Expansile growth compresses surrounding
thyroid Usually non- or hypofunctional (cold nodule);
rarely hyperfunctional
Thyroid Carcinoma
Accounts for 0.4% of all deaths from malignancy but forms a higher proportion of those under 30 years (up to 15%)
More frequent in females (3:1) Types of cancer in descending order of
incidence are:
Papillary, Follicular, Medullary, Anaplastic
Papillary Thyroid Cancer
Over 80% of all thyroid malignancies Up to 10% radiation-induced Unencapsulated tumour with papillary structures and
focal calcifications (psammoma bodies) Uniform age distribution (6 months to 104 years) Early rapid spread to cervical lymph nodes- 60% have
metastases at presentation but long survival common- 25 years or more
Only 5% have spread outside the head and neck at autopsy
Follicular Thyroid Cancer
About 10% of thyroid Cancers Peak incidence 5th to 6th decade Female preponderance, but less than PTC Blood borne metastases to lung and bone 5 yr. Survival 30% Follicular/solid growth pattern, often
encapsulated- invasion of capsule and blood vessels distinguishes it from follicular adenoma
Medullary Thyroid Cancer
Rare. Less than 5% of thyroid malignancies Familial (under 30) or sporadic (over 30) Equal male:female incidence Solid C-cell tumour with amyloid stroma Like PTC shows early spread to nodes 10 year survival 42% Secretes calcitonin(+/- 5HT, ACTH, Pge) which
lowers serum calcium
Normal Parathyroid Gland
Parenchyma consists of chief cells that secrete parathyroid hormone (parathormone, PTH) under the influence of decreasing serum calcium.
There are also variable numbers of oxyphil cells in small nodules which have pink cytoplasm
Parathyroid Glands
Normal number 4 (but can be 2 or 6) Normal combined weight 120 mg Normal maximum dimension 6mm Derived from epithelium and 3rd and 4th
branchial clefts
Actions of Parathormone PTH Kidney: a.increased Ca resorbtion by tubule
b.decreased phosphate resorbtion
c. stimulate 1,25-OH2D3 synthesis by the kidney, thus promoting Ca absorbtion from the gut
Bone: increased calcium and phosphate resorbtion by osteoclasts
Bowel: increased calcium and phosphate absorbtion by enterocytes
Net effect:raises serum calcium, lowers serum phosphate
Normal Ca2+
Ca2+
PO43–
ReleaseBone
Kidneys
Ca2+ reabsorptionPO4
3– excretion
PTH
Normal mineral metabolism
Brown EM. In: The Parathyroids – Basic and Clinical Concepts 2nd ed. 2001. Bilezikian JP et al. (eds)PTH, parathyroid hormone
Ca2+
Parathyroidglands
Calcitriol
Causes and Types of Hyperparathyroidism
Primary: found in 1:1000 adults. Usually female, 30+. Adenoma 70%, hyperplasia 30%.
Secondary: less common. Chronic renal disease, Vit D deficiency, malabsorbtion, ectopic hormone production
Tertiary: rare. Autonomous adenoma developing in secondary hyperplasia.
Features of Hyperparathyroidism
Malaise, constipation, muscle weakness, neuropsychiatric disorders
renal colic due to stones (60%) bone pain due to generalised Ca loss peptic ulcer (10%) acute pancreatitis nephrocalcinosis raised serum calcium and PTH raised urinary PO4 and serum alk phos raised urinary hydroxyproline
Osteitis Fibrosa Cystica
Classic localised bone lesion of hyperparathyroidism. Bone is lysed by osteoclasts driven by elevated PTH. Marrow replace by highly vascularised fibrous tissue. Stress on weakened bone causes haemorrhage and cyst formation.
Old term for this lesion was “brown tumour”. Colour due to massive haemosiderin deposition
Typically found in jaw and long bones and may cause pathological fractures
Can be distinguished from other giant cell tumours of bone by estimation of serum Ca.