Pain Management: Conservative Treatments of Painful Conditions Pain Management: Conservative...
-
Upload
arthur-sparks -
Category
Documents
-
view
215 -
download
1
Transcript of Pain Management: Conservative Treatments of Painful Conditions Pain Management: Conservative...
Pain Management: Pain Management: Conservative Treatments Conservative Treatments
of Painful Conditionsof Painful Conditions
Principles Of Pain ManagementPrinciples Of Pain Management
1. Reduction of Pain Medications, Nerve Blocks, Surgery
2. Rehabilitation Reconditioning and Prevention
3. Coping Management of residual pain with
biofeedback, cognitive therapies
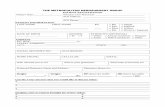
Components of Chronic Pain: Components of Chronic Pain: Stable and Stable and ““BreakthroughBreakthrough”” Pain Pain
Persistent pain
Around-the-clockmedication
Breakthrough pain
Time
Musculoskeletal Pain:Musculoskeletal Pain:The Role of MedicationsThe Role of Medications
• Analgesics are permissive• They allow parallel interventions to succeed
– Physical / occupational therapy– Bracing– Psychological counseling– Surgery
• Adequate analgesia preserves– Function– Quality of life– Psychological well-being
Analgesics and Adjuvants for Analgesics and Adjuvants for Neuropathic PainNeuropathic Pain
• Opioids• Antidepressants• Anticonvulsants• Local anesthetics• Corticosteroids• Alpha agonists
• GABA-ergic• NSAIDs / COX-2s• Cannabinoids• NMDA antagonists• Tramadol
A Place for Opioids?A Place for Opioids?
• Documentation
• The Four “A’s”– Analgesia– ADLs– Adverse events– Abuse issues*
*Passik, SD, Weinreb, HJ. Adv Ther. 2000;17(2):70-83.
Opioid MythsOpioid Myths
• “I’ll get hooked” or “You’ll get hooked”
• Studies show addiction to be problematic only in a small % of patients
• Some patients are tolerant to opioids, different than addiction
Opioid RealitiesOpioid Realities
• Patients don’t like to take them (if they have an effective alternative)
• They cause constipation/mental clouding/nausea (all manageable)
• Costs associated with Opioid side effects• Diversion/Bad Behavior• Endocrine suppression
A Place for Opioids?A Place for Opioids?
• Dependent upon opioid trial– Diminution of pain intensity– Increase in functioning for ADLs– Minimal adverse events which adversely
affect psychological and/or physical functioning• Documented pain / function diary • Documented physical examination• Documented discussion regarding trial,
results, and plan
What is the Risk of Addiction?What is the Risk of Addiction?
• 7% of population uses/abuses illegal drugs1
• Random surveillance urine toxicology screen 400 patients in Ky pain practice receiving prescription opioids2:
• 17% + screen (Comm. Ins)• 10% + screen (Medicare)• 39% + screen (Medicaid)
1. Lussier D, Pappagallo M. The Neurologist 2004;10:221-42. Manchakanti L, et al. J Ky Med Assoc 2005;103(2):55-62
Opioid RealitiesOpioid Realities• Many patients don’t like to take them (if they
have an effective alternative)• They cause constipation/mental clouding/nausea
(all manageable)• Costs associated with opioid side effects• Diversion/bad behavior• Societal/regulatory pressure • Prosecution! (DEA/DPS/Etc.)• Long Term Adverse Outcomes? Endocrine
issues
Opioid AnalgesicsOpioid Analgesics
• Mainstay of cancer pain management1
• Guidelines published by– World Health Organization, 1996– United States Agency for Health Care Policy
and Research, 1994– American Pain Society, 1992
• Adoption into chronic non-cancer pain past decade…not really evidence based…
1 Foley KM. Cancer. 1989;63(11 Suppl):2257-2265.
Increasing use of opioids in Increasing use of opioids in chronic painchronic pain
• Consensus APS-AAPM statements;more pain education; meetings;new opioids
• 1980-2000 use of strong opioids to Rx chronic musculoskeletal pain 2% to 9% in primary care*
• Cause for celebration or alarm? “Flying blind”**
*Caudill-Slosberg MA, et al. Pain 2004**Von Korff M, Deyo RA. Editorial Pain 2004.
Opioid Precriptions USOpioid Precriptions USJan Jan ’’04-Dec 04-Dec ‘‘0404
• 200+ m prescriptions
129m NSAIDs 185m 25m C II
Opioids: Cochrane Review Opioids: Cochrane Review Efficacy/Evidence Based MedicineEfficacy/Evidence Based Medicine
• 15 randomized placebo controlled trials• 11/15 po meds, 1-8 weeks trial, 6-24 mos. Open
label f/u; Mean reduction pain 30%
Conclusions:• Short-term efficacy good for musculoskeletal
and neuropathic pain• Cannot make conclusions about long term
efficacy, tolerance, addiction
Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: Systemic review of efficacy and safety. Pain 2004;112:372-80.
Opioid Titration and Opioid Titration and MaintenanceMaintenance
• No analgesic “ceiling” dose
• Drug titration until satisfactory pain relief or unmanageable side effects occur
• Maintenance doses vary considerably according to individual factors and nature of pain
Therapeutic Use of OpioidsTherapeutic Use of Opioids
When given at stable doses for long-term therapy, opioids do not significantly impair cognition, attention, mood, driving ability, or general functioning
Portenoy RK. Ann Acad Med Singapore. 1994;23(2):160-170; Vainio A, et al. Lancet. 1995;346(8976):667-670; Haythornthwaite JA, et al. J Pain Symptom Manage. 1998;15(3):185-194.
Management of Common Management of Common Opioid Side EffectsOpioid Side Effects
• Constipation – Prophylactic use of laxatives and stool softeners
• Nausea and vomiting– Neuroleptics, metoclopramide, cisapride, antivertigenous drugs
• Sedation– Discontinue other CNS depressants – Add psychostimulants
• Respiratory depression– Extremely rare. Monitor if not severe; carefully titrate naloxone
if severe
CNS: Central nervous system
Opioid ConclusionsOpioid Conclusions
• Opioids are broad spectrum analgesics which act at multiple points in the pain pathway– Safety and short term efficacy are established– Appropriate use of opioids should be
established with a controlled opioid trial– Safeguards against diversion/abuse
Chronic Opioids: The downsideChronic Opioids: The downside
• DAWN network reporting noted increased abuse of prescription opioids ’94-’00 123%*
• Some, albeit small percentage of prescription opioids diverted into abuse**
• Trace methadone increase prescribing p oxycodone-CR scare, ’02-’03 methadone prescriptions 1m to 2.6m with 5 fold increase in abuse cases***
*Zacny J 2003; **Hurwitz W Pain Med 2005; ***Cicero TJ JAMA 2005
Long-Term Opioid Side EffectsLong-Term Opioid Side Effects
• Opioid induced hypogonadism• Immune suppression• Hyperalgesia• Hearing Loss
• All probably seen at higher doses over long term (years) administration
Rajagopal A, et al, JCO 2003. Roy S, et al. Neurochem Res 1996; Mao J Pain 2002; Ballantyne J, NEJM 2003; Vrabec J, Burton AW in press
How to safely prescribe How to safely prescribe chronic opioidschronic opioids
• Make a Dx• Psychological assessment including addictive disorders • Informed consent• Treatment agreement• Pre- Post- interventional assessment of pain level and functioning• Trial of “rational polypharmacy”• Regular reassessment• Reassess 4 “A’s”: Analgesia, activity, adverse events, aberrant
behavior• Review Dx and comorbidities periodically• Documentation
Gourlay DL, Heit HA, Almahrezi A, Universal precautions in Pain Medicine: A rational approach to the treatment of chronic pain. Pain Med 2005;6:107-12.
Chronic Pain Treatment StrategyChronic Pain Treatment Strategy
• Multidisciplinary Care• Primary care, pain specialist, physical medicine,
surgeon, psychologist, physical therapist
• Multimodal Care• Adjuvant medications • Opioids• Topicals
• Holistic Approaches• Massage, meditation, etc.