Paediatric Sepsis Kills: The (missing)
-
Upload
truongduong -
Category
Documents
-
view
219 -
download
0
Transcript of Paediatric Sepsis Kills: The (missing)
Paediatric Sepsis Kills
The (Missed) Golden Hour
Leanne Crittenden, Rhonda Winskill, Helen Stevens, Sandra Babekuhl, Tomas Ratoni, Louise Caire, K Howard, Oct 2016
NSW Deteriorating Patient Committee,Clinical Excellence Commission
Joshua’s story
• Day1.
• 6m boy presents level 2 hospital – District Hospital, mixed ED, no paediatric in-patients.
• “Flu-like” 1 week, fever 1 day, SOB
• Triage T 37.4, HR 168, RR 52
• ED JMO T 39 “Not sick”
• PD viral RTI, allowed home
Day 3
• Represents to same hospital.
• Carer concern, SOB, fever
• Triage, T 40.1, RR 64, No HR recorded “crying”, mild recession and head bobbing
• Paracetamol supositary
• ED MO “Happy, active, chest clear, eczema”
• PD viral RTI, allowed home
Day 4
• Saw GP
• CXR: Bilateral increase in peri-hilar markings
• PD Bronchopneumonia
• Referred to level 6 hospital ED for admission.
Day 4, level 6 ED
• Arrived 14.31, Unwell, RR 80, increased WOB
• Transferred to Resus bay
• T 38.1, HR 190, RR 79, Sats 98 in air
• Severe WOB, bilateral crackles
• For WHO, iv Antibiotics
• DW Respiratory Paediatrician, for Gentamycin as well as Penicillin and Azithromycin
Day 4 time-line
• 14.31 Arrives at hospital
• 16.05 Given N/Saline 70ml i.v. (10 ml/kg), WHO increased, NPA performed
• 17.40 Decision documented for admission to ICU
• 18.00 1st dose of Penicillin documented on routine medication chart
• 18.50 Arrives ICU, Gentamycin yet to be given
• 20.00 1st dose of Genta and Azithromycin documented
Results
• Total wbc 30.1, neutrophils 16.4
• Lactate 1.7
• CRP 153
• B Culture Pneumococcus
• PNA Picornavirus
• Transferred from ICU to ward the following day, 5 days iv Penicillin. Made a good recovery.
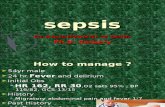
Sepsis Kills
Sepsis is a leading cause of death in paediatric patients, with mortality as high as 10%. Almost 5000 children die from sepsis pa in US.In ANZ Sepsis accounted for 26% of deaths in ICU in 2012.Mortality around 25% for adults with septic shock. increasing by 7.6% for every hour of delay after onset of hypotension, in starting antibioticsCEC Clinical Focus Report (2009) found deficits in a range of NSW healthcare settings.
Sepsis Kills and Paediatric Sepsis Kills, Introduced 2012
• RECOGNISE risk factors, signs and symptoms of sepsis.
• RESUSCITATE with rapid IV fluids and antibiotics, within the first hour of recognition of Sepsis.
• REFER to senior clinicians and specialty teams, including escalation as required.
SEPSIS KILLS: Early intervention saves lives. MJA Jan 2016 Burrell et al
Database 13,567 (adult) patients.
2009-11 2013 2015Patients who received Antibiotics <60min 29.3% 52.2%Patients who received1L IV <60 min 10.6% 27.5%
Mortality 19.3% 14.3% 13.7%
i.e. 29% improvement in mortality
Time to 1st antibiotic
• Median time (in minutes) from presentation to completion of first dose of IV antibiotics:
• 2009-11 2013 2016
• Adult 150 60 54
Paediatric 191 86
(Benchmark 60 minutes)
• Paediatric patients represent only 4.2% of Sepsis Kills data base.
• Correlation is uncertain between;
• recognition of likely sepsis, with management according to an appropriate pathway and
• subsequently confirmed sepsis by significant culture from a “usually sterile” site.
Audit
• Chart Review was undertaken of all patients in HNE LHD, Term - 16th birthday with significant positive cultures from blood or CSF, July –December 2015.
• Chart Review was conducted for the same population with a sepsis data collection tool completed and submitted to CEC.
Parameters
• Time from presentation to completion of first dose of IV antibiotic.
• Time from presentation to completion of first resuscitation bolus of 20ml/kg 0.9% Normal Saline.
• Observations in red or yellow zone on SPOC• Clinical comments relating to severity of illness• WBC, Neutrophil count and serum Lactate• Organism and site of culture• Final diagnosis and outcome
Results
• Total Paediatric population of HNE (0-16y-old) around 180,000 (ABS census 2011).
• 95,000 presentations to ED p.a.
• 40 patients with positive blood or CSF cultures
• 12 Ex-prems, still in NICU
• 12 Immuno-supressed children including 11 on chemotherapy for malignant disease.
• 16 previously well children, 17.8/100,000 pa
16 Previously well children
• 5 did not fulfil clinical criteria for sepsis at presentation. Of the 11 who did;
• 2 Beta Haem Strep sepsis• 3 Pneumococcus, including 1 meningitis• 1 E coli UTI and sepsis• 1 S aureus UTI and sepsis• 1 Proteus otitis media and sepsis• 1 Enterococcus• 1 Salmonella• 1 H flu/Aerococcus/Pseudomonas osteomyelitis
• 5/11 aged 3 months or younger
Management
• 3/11 registered on sepsis pathway.
• Time to completion of 1st dose of one antibiotic;• 23 minutes• 54 minutes• 1 hour 25 minutes• 2-3 hours; 2 patients• 3-4 hours; 3 patients• 4 hours 10• 7 hours 30• 5 days
• 2/11 administered within 60 minutes
Management
• No child received complete recommended dose of antibiotic doses within 60 minutes.
• 1/11 received appropriate fluid bolus (Normal Saline 20ml/kg) within 60 minutes.
• 6/11 had serum lactate measured.
• 10/11 had wbc measured.
Sepsis Pathway use
• 39 children entered on a sepsis pathway• 3 had positive cultures (Salmonella, Proteus, E
coli)• 17 had Entero/Parecho/Picornavirus• 4 had UTI• 9 had no defined cause• 9/34 (26%) had 1st dose of antibiotic within 60
minutes (52% for adults in NSW)• 8/14 potentially septic children presenting to
JHCH were aged 3/12 or less.
Serum Lactate
• Prolonged stay in ICU & Increased mortality from sepsis when lactate >3.
• Khan et al. Arch Dis Child April 2016 vol 101 p 297-8
• All EDs in NSW have POC testing.
Improving Paediatric Sepsis Outcomes
• Paediatric Sepsis Collaborative of Children’s Hospitals Association (US)
• Comprises 4 bundles of care;• Recognition;Fever, tachycardia + 1 other clinical sign or risk factor, Continuous monitoring, Structured assessment, investigation.
Resuscitation; timely intervention.Stabilisation Performance.
• Mortality from severe sepsis improved from 11% to 3%
Take home messages
• Bacterial Sepsis is uncommon in the paediatric age group, • Our current tools seem poor at distinguishing between
bacterial and viral sepsis, especially in infants, BUT• A septic work-up alone is not enough and the importance
of appropriate management of sepsis in infants and children is under-recognised in comparison with adults.
• A lumbar puncture won’t save your life,• Waiting for a wbc result won’t save your life,• Paracetamol won’t save your life,• But prompt treatment with antibiotics just might!