OR Smoothing The Value of Analytics - IHI Home...
Transcript of OR Smoothing The Value of Analytics - IHI Home...
OR SmoothingThe Value of
AnalyticsFrederick C. Ryckman, MDProfessor of Surgery / TransplantationSr. Vice President – Medical Operations
Cincinnati Children’s HospitalCincinnati, Ohio
James Anderson Center for Health Systems Excellence
I have nothing to disclose
Hospital Flow Seminar
April 2016
James M. Anderson Center
For
Health Systems Excellence
Key Drivers for Capacity Management
Management of
Variability
Predictable Care
Delivery
Capacity
Prediction
Capacity
Management
Optimization of
Flow Delivery
Flow:Safety
Matching
Identify Patient Streams – Inpatient/Outpatient/OR
Manage System Variation
Evidence Based Best Practices, Analysis of ALOS and outliers,
Standardize then Customize, Eliminate unnecessary care
Integration of simulation modeling and planning
“Environmental Impact” Reports for growth programs
Simulation for design and patient placement
“Environments Impact” Planning
Placement initiatives – D:C Matching plans
Discharge prediction and planning,
Home Care, Parent Initiatives
Flow Failure Analysis, GARDiANS
IHI Drivers CCHMC Initiative Operations Possibilities
D/C
Match
System
Re-Design
Shape /
Reduce
Demand
James M. Anderson Center
For
Health Systems Excellence
Surgical Streams of Care
• Urgent / Emergent Surgery
• Predictable and Measurable – Natural Variation
• Possible to Model
• Can be managed within the System with resource allocation
• Delay Increased risk and worse outcomes
• Elective Surgery
• Unpredictable – Whim of Surgical Schedule
• High variability over time
• Delay Case specific risk
• Initial Design around Urgent Needs
• Goal – No urgent cases in Block Time
• Allocate “Block” for Urgent Needs
James M. Anderson Center
For
Health Systems Excellence
Traditional Block
• Reactive System
• Urgent Emergent Cases
placed within Block Time as
needed
• Elective Case Plan disrupted,
prolonged waiting time for
elective patients
• Inefficient (Unsafe) Access for
Urgent Cases
• Push complex Elective Cases
into the late hours
• Overtime
• Wrong Team in OR
Not
Ideal
James M. Anderson Center
For
Health Systems Excellence
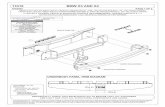
Scheduling Guidelines – A to EGUIDELINES FOR SURGICAL CASE GROUPING DIAGNOSES/PROCEDURES
(guideline only: medical judgment required)
Acute Life and Death Emergencies
A < 30 MinutesAirway emergency(upper airway obstruction)
Cardiac surgery postop bleeding with tamponade
Cardiorespiratory decompensation (severe)
Liver transplant postoperative emergency
Malrotation with volvulus
Massive bleeding
Mediastinal injury
Multiple Trauma-unstable or O.R. resuscitation
Neurosurgical condition w/imminent herniation
Urgent C < 4 HoursAbscess with sepsis
Airway (non-urgent diagnostic L&B, flex bronch, non-symptomatic foreign
body)
Appendicitis-with sepsis/rapid progression
Biliary obstruction non-drainable
Cardiac ventricular assist device placement
Cerebral angiogram for intracranial hemorrhage
Chest tube placement in patient w/unstable vital signs, increased work of
breathing and decreased O2 saturation
Contaminated Wounds-Multiple Trauma
Diagnostic/therapeutic airway intervention
Hepatic angiogram w/suspected vascular thrombus
Hip Dislocation
Intestinal Obstruction-no suspected vascular compromise
Kidney transplant (ORGAN AVAILABLE)
Liver laparotomy
Massive soft tissue injury
Nephrostomy tube placement in patient w/sepsis
Obstructed kidney (stones) with sepsis
Older child with bowel obstruction
PICC placement where patient has no access but needs
fluids/medications urgently
Progressive shunt malfunction
Traumatic dislocation-hip
Unstable neurosurgical condition
Add-on case to elective schedule
E < 24 HoursNeeds to be done that day, but does not require the
manipulation of the elective schedule,
pyloromyotomy
Broviac
Closed reduction
Eyelid/canalicular lacerations
Facial nerve decompression
Femoral neck fracture
Liver biopsy
Mastoidectomy
Open fracture grade I/II
Open reduction of fracture
PICC placement-has other IV access
Retinopathy of prematurity treatment
Unstable slipped capital femoral epiphysis
Emergent, but not immediately life threatening
B < 2 HoursAcute shunt malfunction
Acute spinal cord compression
Bladder rupture
Bowel perforation, traumatic
Cardiac congenital emergencies w/hemodynamic or pulmonary
instabilities
Compartment syndrome
Donor harvest
ECMO cannulation
Ectopic pregnancy
Embolization for acute hemorrhage
Esophageal atresia with tracheoesophageal fistula
Gastroschisis/omphalocele
Heart, heart/lung, lung, liver and intestinal transplants
Incarcerated hernias
Intestinal obstruction with suspected vascular compromise
Intussusception-irreducible
Ischemic limb/cold extremity (compromised arterial flow)
Liver/Multivisceral/SI Transplant (when organ available)
Liver transplant with suspected thrombosis
Newborn bowel obstruction
Open globe
Orbital abscess
Pacemaker insertion for complete heart block
Replant fingers
Replant hand or arm
Spontaneous abortion
Semi-Urgent D < 8 HoursAbscess drainage
Appendicitis-stable/elective
Caustic ingestion
Chest tube in patient w/stable vital signs
Chronic airway foreign bodies
Closure abdomen-liver transplant
Coarctation repair in newborn
Esophageal foreign body without airway symptoms
GJ tube/NJ tube placement with no other nutrition access
Hematuria with clot retention
I & D abscess without septicemia
Joint aspiration or bone biopsy prior to starting antibiotic therapy
Kidney transplant (ORGAN NOT YET AVAILABLE)
James M. Anderson Center
For
Health Systems Excellence
Options from Simulation
# Cases Included # Rooms Average Waiting
Times (minutes)
Probability 1 Or
More Rooms
Will Be Available
Utilization
Rate
Recommendations/Considerations
1 A, B, C, D, “missing”
treated as B
1 A: 45
B + missing: 53
C: 72
D: 101
60% 40% NOT RECOMMENDED
Mean wait for A cases would exceed stated limit
2 A, B, C, “missing”
treated as B
1 A: 21
B + missing: 24
C: 30
76% 24% NOT RECOMMENDED
Low utilization rate
3 A, B, C (No “missing”) 1 A: 17
B: 19
C: 22
81% 19% NOT RECOMMENDED
Low utilization rate
Ignores “missing” cases
4 A – E, divided;
“missing” treated as D
2 rooms:
1 room for A- C,
1 room for D,E, &
missing
A: 18
B: 19
C: 24
D + missing: 70
E: 162
A – C room: 80%
D – E room: 43%
A – C room:
20%
D – E room:
57%
NOT RECOMMENDED
Low utilization rate in A – C room
Some cases with missing urgency codes may be more urgent than D
5 A – E together;
“missing” treated as
B
2 rooms that would
take any A – E case
A: 7
B + missing: 8
C + D: 9
E: 17
83% 42%, each
room
RECOMMENDED
Very good waiting times (Wait for A cases would exceed stated limit about
1X/112 weekdays (21.4 weeks ))
Treats missing cases conservatively
Highest utilization rate
Not very sensitive to small increases in case duration or case volume
James M. Anderson Center
For
Health Systems Excellence
Block with Urgent Access Assured
Predictive system
Urgent Cases in
Defined Rooms
with Scheduled
Teams
Resources needed
can be modeled
Care based on
Urgency / Medical
Need
James M. Anderson Center
For
Health Systems Excellence
B-E Case Access - % Successful
60%
65%
70%
75%
80%
85%
90%
95%
100%
Ju
l 20
06 (
n=
278)
Sep 2
006 (
n=
290
)
Nov 2
006 (
n=
239
)
Ja
n 2
00
7 (
n=
217)
Ma
r 2
007 (
n=
263
)
Ma
y 2
00
7 (
n=
262)
Ju
l 20
07 (
n=
285)
Sep 2
007 (
n=
282
)
Nov 2
007 (
n=
227
)
Ja
n 2
00
8 (
n=
242)
Ma
r 2
008 (
n=
231
)
Ma
y 2
00
8 (
n=
244)
Ju
l 20
08 (
n=
42)
Sep 2
008 (
n=
104
)
Nov 2
008 (
n=
102
)
Ja
n 2
00
9 (
n=
191)
Ma
r 2
009 (
n=
227
)
Ma
y 2
00
9 (
n=
227)
Ju
l 20
09 (
n=
216)
Sep 2
009 (
n=
236
)
Nov 2
009 (
n=
206
)
Ja
n 2
01
0 (
n=
245)
Ma
r 2
010 (
n=
183
)
Ma
y 2
01
0 (
n=
262)
Ju
l 20
10 (
n=
275)
Sep 2
010 (
n=
277
)
Nov 2
010 (
n=
229
)
Ja
n 2
01
1 (
n=
142)
Ma
r 2
011 (
n=
192
)
Ma
y 2
01
1 (
n=
194)
Ju
l 20
11 (
n=
276)
Sep 2
011 (
n=
275
)
Nov 2
011 (
n=
173
)
Ja
n 2
01
2 (
n=
228)
Ma
r 2
012 (
n=
199
)
Ma
y 2
01
2 (
n=
319)
Ju
l 20
12 (
n=
205)
Sep 2
012 (
n=
281
)
Nov 2
012 (
n=
212
)
Ja
n 2
01
3 (
n=
169)
Ma
r 2
013 (
n=
221
)
Ma
y 2
01
3 (
n=
244)
Ju
l 20
13 (
n=
216)
Sep 2
013 (
n=
184
)
Nov 2
013 (
n=
196
)
Ja
n 2
01
4 (
n=
147)
Ma
r 2
014 (
n=
184
)
Ma
y 2
01
4 (
n=
263)
Ju
l 20
14 (
n=
284)
Sep 2
014 (
n=
116
)
Nov 2
014 (
n=
75)
Ja
n 2
01
5 (
n=
40)
Ma
r 2
015 (
n=
73)
Ma
y 2
01
5 (
n=
77)
Ju
l 20
15 (
n=
342)
Sep 2
015 (
n=
208
)
Nov 2
015 (
n=
185
)
% o
f "B
-E" C
as
es
pe
rfo
rme
d w
ith
in 1
5%
of
the
ir
ac
ce
pta
ble
tim
efr
am
e
Month
Add on Access to OR within Accepted Timeframe
"B-E" CasesPopulation: Base Hospital Add-on Cases
% Cases Center Line Control Limits
*NOTE: Current Control Limits set from 1/2011 - 8/2012.
Last Updated 2/1/2016 by E. McDaniel, James M. Anderson Center for Health Systems Excellence
OR Renovation
1 Add-On Room Closed
James M. Anderson Center
For
Health Systems Excellence
“A” Case Access Times – Target 30 Minutes
0
30
60
90
120
150
180
210
240
270
Jul 2006 (
n=
3)
Se
p 2
006
(n=
6)
Nov 2
006 (
n=
16)
Jan
2007 (
n=
6)
Ma
r 20
07 (
n=
7)
Ma
y 2
007 (
n=
6)
Jul 2007 (
n=
7)
Se
p 2
007
(n=
3)
Nov 2
007 (
n=
1)
Jan
2008 (
n=
3)
Ma
r 20
08 (
n=
3)
Ma
y 2
008 (
n=
7)
Jul 2008 (
n=
0)
Se
p 2
008
(n=
0)
Nov 2
008 (
n=
2)
Jan
2009 (
n=
2)
Ma
r 20
09 (
n=
2)
Ma
y 2
009 (
n=
4)
Jul 2009 (
n=
2)
Se
p 2
009
(n=
5)
Nov 2
009 (
n=
1)
Jan
2010 (
n=
2)
Ma
r 20
10 (
n=
0)
Ma
y 2
010 (
n=
1)
Jul 2010 (
n=
2)
Se
p 2
010
(n=
4)
Nov 2
010 (
n=
2)
Jan
2011 (
n=
1)
Ma
r 20
11 (
n=
2)
Ma
y 2
011 (
n=
1)
Jul 2011 (
n=
0)
Se
p 2
011
(n=
0)
Nov 2
011 (
n=
3)
Jan
2012 (
n=
2)
Ma
r 20
12 (
n=
2)
Ma
y 2
012 (
n=
2)
Jul 2012 (
n=
3)
Se
p 2
012
(n=
4)
Nov 2
012 (
n=
3)
Jan
2013 (
n=
4)
Ma
r 20
13 (
n=
4)
Ma
y 2
013 (
n=
1)
Jul 2013 (
n=
2)
Se
p 2
013
(n=
3)
Nov 2
013 (
n=
2)
Jan
2014 (
n=
3)
Ma
r 20
14 (
n=
3)
Ma
y 2
014 (
n=
2)
Jul 2014 (
n=
0)
Se
p 2
014
(n=
0)
Nov 2
014 (
n=
0)
Jan
2015 (
n=
0)
Ma
r 20
15 (
n=
3)
Ma
y 2
015 (
n=
1)
Jul 2015 (
n=
6)
Se
p 2
015
(n=
7)
Nov 2
015 (
n=
0)
Ave
rag
e W
ait
Tim
e (
Min
ute
s)
Month
Add on Access to OR within Accepted Timeframe
Wait Time for "A" Cases Population: Base Hospital Add-on Cases
Wait Time (Minutes) Center Line Goal Control Limits
Source: CPM/EPICLast Updated 2/1/2016 by E. McDaniel, James M. Anderson Center for Health Systems Excellence
James M. Anderson Center
For
Health Systems Excellence
Resources
• Nursing and Anesthesia allocated by system
• “We know they are coming, we don’t know their names”
• Surgeon Availability
• SOD – Surgeon of the Day
• DOOD – Doctor of Orthopaedics of the Day
• ENT – Available resources
• PLA, URO, OPH, Dental, NSg, GYN – Herd Immunity
• Cardiac – Special Resources
P















![L29 Presentation.ppt [Read-Only] - IHI Home Pageapp.ihi.org/FacultyDocuments/Events/Event-2491/Presentation-10640/...management from data systems and sustaining relationships ... Data](https://static.fdocuments.us/doc/165x107/5b3430f37f8b9aa0238da72c/l29-read-only-ihi-home-pageappihiorgfacultydocumentseventsevent-2491presentation-10640management.jpg)

![IMPORTANCIA DE DETERMINAR LAS LECCIONES …repository.unimilitar.edu.co/bitstream/10654/13316/1/Articulo MLG... · del proyecto” PMBOK [1]. ... un cuestionario enviado a 200 pequeñas](https://static.fdocuments.us/doc/165x107/5a7a82927f8b9a8d558c48e2/importancia-de-determinar-las-lecciones-mlgdel-proyecto-pmbok-1-.jpg)











![L5 High Five Lachman.pptx [Read-Only] - IHI Home Pageapp.ihi.org/.../Document-11517/Presentation_L5_High_Five_Lachman.pdf · 11/29/2016 2 Key content of The High Five Improving Access](https://static.fdocuments.us/doc/165x107/5e19beb513040b6db9117d64/l5-high-five-read-only-ihi-home-pageappihiorgdocument-11517presentationl5highfivelachmanpdf.jpg)