onlay grafting in mandible
-
Upload
arindom-changmai -
Category
Documents
-
view
27 -
download
5
description
Transcript of onlay grafting in mandible
-
Lower border bone onlays A. Soehardi, G. J. Meijer,
Keywords: preimplant surgery; atrophic mand-ible; lower border bone augmentation; dentalimplants.
Int. J. Oral Maxillofac. Surg. 2014; 43: 14931499http://dx.doi.org/10.1016/j.ijom.2014.06.005, available online at http://www.sciencedirect.comDespite the advances made in the treat-ment of patients with severely atrophicmandibles (Cawood and Howell, classVI),1 the thin mandible remains a chal-lenge for which no definitive solution hasyet been found. Several authors recom-mend ultra-short implants,2,3 whilst othersadvocate augmentation before implantsare to be inserted37 or combined withimplant placement.8,9 All options havetheir specific advantages and disadvan-tages.
Although with decreasing height, mea-sured at the mandibular symphysis, thebody of the mandible becomes wider,10
a recent study based on an inventoryamong Dutch oral and maxillofacial sur-geons showed that mandibles with a heightof less than 10 mm are at risk of fracturewhen short implants are used. These frac-tures do not necessarily occur immediatelyafter insertion, but may take place yearslater.11 Short implants may be unfavour-ably loaded because of the increased le-
verage caused by the increasedintermaxillary distance.Augmentation by building up an alve-
olar process via an intraoral route also hasits shortcomings, in that neurosensory dis-turbance in the area of the mental nerve isnot always avoidable. This happens bothwhen onlay grafting is used and in casesof sandwich osteotomies.4,5,12 It is notuncommon when dealing with thinmandibles to find that the inferior alveolarnerve is located on top of the mandible,
0901-5027/01201493 + 07 # 2014 International Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.to augment the severelyatrophic (class VI) mandiblein preparation for implants:a preliminary reportA. Soehardi, G. J. Meijer, S. J. Berge, P. J. W. Stoelinga: Lower border bone onlaysto augment the severely atrophic (class VI) mandible in preparation for implants:a preliminary report. Int. J. Oral Maxillofac. Surg. 2014; 43: 14931499. # 2014International Association of Oral and Maxillofacial Surgeons. Published by ElsevierLtd. All rights reserved.
Abstract. We present the preliminary results of a study involving a group ofconsecutive patients who underwent lower border onlay grafting, limited to thesymphyseal area, in preparation for implant insertion. This technique allows formaximum-sized implants, followed by prosthetic rehabilitation. The mainadvantage of this method is the minimal risk of damage to the mental nerve. Sixteenpatients were followed for a period of 6 months to 4 years and all were free ofneurosensory disturbances. Eight had a removable overdenture placed and weresatisfied with the result. This surgical approach allows the patient to wear theirdentures during the healing period. A further advantage of lower border graftingover intraoral upper border grafting is that mucosal dehiscences are not seen.Accepted for publication 10 June 2014Available online 11 July 2014S. J. Berge, P. J. W. StoelingaDepartment of Oral and Maxillofacial Surgery,Radboud University, Nijmegen MedicalCentre, Nijmegen, The NetherlandsClinical Paper
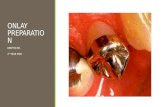
Pre-Implant Surgery
-
completely embedded in connective tis-sue. Dissecting this nerve free may itselfcause a nerve neurosensory disturbance.Distraction might be another option, but incommon with surgery to the upper bor-der, nerve neurosensory disturbance mayoccur for the same reason as mentionedpreviously because the same sandwichcut has to be made. This comes on topof the possible complications that mayoccur when the vector of the verticaldistraction does not coincide with theplanned vector, or when other complica-tions occur, such as fracturing of the man-dible.1317
A somewhat forgotten technique thatwas proposed at the time when pre-pros-thetic surgery was evolving is inferiorborder grafting.1827 Although graftingof the lower border will circumvent theabove-mentioned problems, a visible scaris the main disadvantage of this tech-nique. It is thought that in the older popu-lation, the resulting submental scar mightnot be too much of a problem, particularlywhen weighed against the chances of
the symphyseal area, in preparation forimplant insertion.
Materials and methods
Patient selection
Seventeen edentulous patients (11 femalesand 6 males) aged 5084 years (mean 66.7years) with class VI mandibles, treated atthe study medical centre from 2007 to2010, were included in this study. Allmandibles had a height of 9 mm or lessin the bilateral canine region, as measuredon cone beam computed tomography(CBCT) scans (i-Cat; Imaging SciencesInternational, Hatfield, PA, USA). Patientdetails are given in Table 1. All patientswere informed about the procedure and theadvantages and disadvantages wereexplained; alternative options were of-fered. The final choice of treatment wasleft to the patient.Patients, who had undergone radiation
therapy or who had received chemothera-py or intravenous bisphosphonates were
tion. All patients received one doseof 1000 mg cefazolin and 500 mg metro-nidazole 30 min before the operationbegan. A corticocancellous bone graftwith dimensions of approximately3 cm 3 cm was harvested from the an-terior iliac crest. The donor site was thenclosed in layers using 30 Vicryl (Ethicon)and 50 Prolene (Ethicon) sutures.Subsequently, a 2.5-cm long, curved
incision was made just behind the sub-mental fold, following the curvature of thesymphysis. The periosteum was then in-cised and dissected. The region of themental nerves was not explored. Afterthe lower border was completely exposedover an area of about 3 cm, the bone graftwas modelled to fit the contour of theexposed bone. Via a submental approach,the graft was first temporarily fixed withone 11-mm long, 2.0-mm screw (KLSMartin) at the midline of the symphysis.When the position of the graft was judgedto be satisfactory, the graft was perma-nently fixed using two 13- to 15-mm long,2.0-mm screws (KLS Martin) via an
1494 Soehardi et al.
oa(m en
1 3
2 1 2 2 3 1 1 1 4 5 4 2 2 2
la ,permanent neurosensory disturbance ofthe lower lip or chin. The fact that thedenture to be made will be supported bytwo implants of maximum length is rea-son to believe that sufficient retention andstability can be achieved without risk ofearly implant loss because of unfavour-able loading.In this report, we present the prelimi-
nary results of a study involving a group of17 consecutive patients who underwentlower border onlay grafting, limited to
Table 1. Relevant patient data.
PatientAge,years Gender
Fafter
1 57 F 2 69 F 3b 75 F 4 50 F 5 64 F 6 68 M 7 64 F 8 73 F 9 79 M 10 69 M 11 69 M 12 84 M 13 71 M 14 75 F 15 61 F 16 60 F 17 51 F
F, female; M, male; NA, not applicable.a Branemark Mk III Groovy: NP = narrow pb Patient died of natural causes.excluded from the study. One patient al-ready suffered from dysesthesia of his leftchinlip area as a result of a previousdistraction procedure that had failed. Thisside was not included in the current study.One patient in the study group sufferedfrom type II diabetes and two smoked 1015 cigarettes per day.
Surgical technique
The operation was carried out under gen-eral anaesthesia with nasotracheal intuba-
llow-upugmentationonths)
Neurosensorydisturbance Dehisc
2 Normal 8 Normal 4 NA 0 Normal 8 Normal 0 Normal 9 Normal 3 Normal 6 Normal 5 Normal 5 Normal 1 Normal 8 Normal 6 Normal 4 Normal 2 Normal 5 Normal
tform, diameter 3.3 mm; RP = regular platformintraoral approach, after which the extrao-rally placed screw was taken out.The previously harvested corticocancel-
lous bone chips were carefully placedalong the inferior and lateral aspects ofthe grafted part of the mandible extendingas far as the canine region. The woundswere then closed in layers using 30Vicryl (Ethicon) and 50 Prolene(Ethicon) sutures.The patients were discharged from
hospital 1 or 2 days after surgery and were
ce
Implantsin place(months)
Types of implanta
and lengths, mm,right/left
10 RP 11.5/11.528 RP 15/NP 15NA NA12 RP 15/1513 RP 11.5/11.519 RP 15/1522 NP 13/1327 RP 11.5/11.522 RP 13/136 RP 13/1335 RP 13/1338 NP 13/1338 NP 11.5/11.534 NP 13/1319 RP 13/1313 RP 13/1517 RP 13/13
diameter 3.75 mm.
-
allowed to wear their dentures during thehealing period.
Implants
Two endosteal implants were placed ineach patient, 46 months after grafting,under local anaesthesia. Via an intraoralapproach, the two screws were removed.Implant placement was carried out usingthe Nobel Guide procedure. BranemarkMk III Groovy implants with a regularplatform (RP, diameter 3.75 mm) or nar-row platform (NP, diameter 3.3 mm) wereselected (Table 1).After integration of the implants in the
bone, approximately 6 months later, theimplants were exposed and prosthetic re-habilitation was completed with remov-able, implant-supported dentures, made bya specialist dentist (Fig. 1).
Follow-up
All patients were seen at regular intervalsto ensure that the healing was uneventful.
They were asked to complete a question-naire at the last follow-up, in which theygraded the whole procedure includingbone grafting and denture function, usinga visual analogue scale (VAS).CBCT scans were made of each patient
preoperatively, immediately postopera-tively, after 6 months, and at the lastfollow-up, which varied from 2 to 4 years.Bone height was assessed preoperatively,immediately postoperatively, at the time
of implant placement (46 months aftergrafting), and again at 24 months afterbone grafting, when applicable (Fig. 2).After identifying the midline, the cross-sections were measured at a distance of12 mm (i-CAT Vision Software; ImagingSciences International, Hatfield, PA,USA). Subsequently, the measured valuesfor the left and right side were averaged.The percentage of height increase was
calculated as follows: (height of originalmandible plus bone graft in mm heightof original mandible in mm)/height oforiginal mandible in mm 100% = gainin height %. Resorption was calculated ina similar manner: (postoperative height inmm final height in mm)/postoperativeheight in mm 100% = height loss %.
Assessment of nerve function
In addition to the light touch test evaluat-ing the patients subjective perception ofnormal sensation versus neurosensorydisturbance, SemmesWeinstein monofi-laments were used with index numbers
Lower border bone onlays for the class VI mandible 1495
Fig. 1. Implants with locators in situ.
bone onlay and (b) after implant placement.Fig. 2. (a) 3D CBCT scan after lower border
-
1496 Soehardi et al.1.65, 2.83, and 3.22, corresponding to0.008 g, 0.07 g, and 0.16 g of force, re-spectively (Fig. 3). Since the actual forcevalue might differ, all filaments were cali-
Fig. 3. The three types of SemmesWeinstein mand 3.22.
Fig. 2. (Continued ).brated using a top-loading balance and bycalculating the mean of 10 force measure-ments per filament. Force values areexpressed in millinewtons (mN; 1 mN =
onofilaments with index numbers 1.65, 2.83,100 mg). Force rather than pressure wasappropriate for defining the stimulus mag-nitude of the monofilaments. A filamentwas gently moved perpendicular to andfrom a test site. The contact time wasapproximately 1.5 s (the examinercounted silently 21, 22 at the correctpace). The upper lip was used as a control.
Results
Healing was uneventful in all patients andno dehiscence occurred, either intraorallyor submentally. All scars were well hiddenposterior to the submental fold. None ofthe patients thought this to be a drawbackof the procedure.One patient died after the augmentation
but before implant placement and mentalnerve function testing, thus implants wereplaced in 16 patients. The whole treatmentwas completed, including the prostheticrehabilitation, in nine patients. A total of32 Branemark Mk III Groovy implantswere inserted, 9 NP and 23 RP. Implantlength varied from 11.5 to 15 mm(Table 1).
-
in the lipchin area. One has to keep inmind that the method of testing used isvery sensitive, as filaments of 1.65 mNwere also not felt in the upper lip of fivetested persons. These findings regardingthe sensitivity of the method of testing arein accordance with those of earlierreports.2830 The method used seems tobe the most simple and reliable method toshow the seriousness of nerve damage,such as paresthesia or anaesthesia, and
Lower border bone onlays for the class VI mandible 1497
Table 2. Gain in height and resorption of the augmented bone on the lower border of themandible at four different times-points.
PatientMandibular height, mm
Preoperative Postoperativea6 months
postoperativeb24 years
postoperativec
1 8.2 13.8 13.0 2 6.9 16.4 15.8 15.13d 8.5 16.4 NA NA4 8.2 15.9 15.6 5 6.5 12.7 12.5 The measurements of the height of thegrafted mandibles are presented in Table2. The height of the mandible varied be-tween 5.4 and 8.9 mm (mean 7.6 mm)preoperatively, and between 12.2 and16.7 mm (mean 14.9 mm) immediately
6 8.7 16.7 7 7.4 15.7 8 5.4 12.2 9 8.8 16.1 10 8.4 15.0 11 6.2 14.7 12 5.6 14.4 13 7.4 12.7 14 8.9 15.7 15 7.2 13.5 16 8.3 16.2 17 8.2 14.8 Mean, mm 7.6 14.9
NA, not applicable.aMean height gain postoperatively 98%.bMean height loss at 6 months 4.7%.cMean height loss at 24 years 9.3%.d Patient died of natural causes.after augmentation. The calculated meanheight gain was 98%.Initial resorption after 6 months varied
from 0.2 to 1.0 mm (mean 0.7 mm; 4.7%);resorption of 0.10.7 mm (mean 0.4 mm;9.3%) was observed between 6 and 24months. The last measurements were notcomplete, because the follow-up wasshorter than 2 years for eight patients.Sixteen patients underwent mental
nerve function tests (Table 3); howeveronly one side was tested for one of thesepatients (see Materials and methods sec-tion). The light touch test expressing dif-ferences in threshold of neurosensorytactile perception was within the normallimits in this patient group. Monofilament1.65 was not felt by seven of the 15
Table 3. Results of mental nerve function tests
1.
Left
Normal sensitivity (n patients) 12 Neurosensory disturbance (n patients) 3 patients, but numbers 2.83 and 3.22 werefelt by all 15 patients.The average VAS score for patient
appreciation was 7.9 on a scale from 0to 10, varying between 7 and 9. All 16 ofthe patients treated were satisfied with the
16.0 15.0 14.311.7 11.615.1 14.4 14.0 13.5 13.112.4 12.215.3 14.613.1 13.015.8 14.4 14.114.2 (13.5)result and would do it again.
Discussion
Augmentation of the lower borderappeared to be reasonably stable, but someresorption occurred in the first 6 months(Table 2), which continued at a lower ratein most cases for up to 2 years afteraugmentation. It appeared that the mea-sured resorption took place at the periph-ery of the bone transplant. Long-termfollow-up will be necessary to confirmthis trend. The height gained allowed forinsertion of implants, often of maximumsize.Most importantly the results of the men-
tal nerve testing showed normal sensitivity
for the three types of monofilament.
Upper lipMonofilament index number
65 2.83 3.22
Right Left Right Left Right Le
13 15 15 15 15 82 0 0 0 0 7to follow the recovery process over time.30
Ideally, the sensitivity of the mental regionwould be tested preoperatively, instead ofusing the upper lip as control.The VAS score revealed a high degree
of satisfaction for the whole treatmentprocess, despite the presence of a visiblescar. As compared to the conventionalaugmentation (onlay technique) of theedentulous mandible, using the techniquepresented does not reduce the intermax-illary distance. Another disadvantage isthe lack of improvement of the facialprofile, because the augmentation doesnot provide support for the muscles ofthe lower lip. Compensation, of course,is provided by the prosthesis. Also, theprocedure does not provide an opportunityto correct bony irregularities of the upperborder, nor can the mental nerve be repo-sitioned at the same time. When theseprocedures need to be done because ofpressure pain, they need to be performedseparately.One of the advantages of the method
described is certainly the opportunity forthe patient to wear their dentures duringthe healing period. A further advantage oflower border grafting over intraoral upperborder grafting is that mucosal dehis-cences are not seen.7,31
To the best of our knowledge there arethree publications that have followed asimilar pattern, with inferior border graft-ing of the mandible being carried out priorto implant placement. Quinn et al.21 used acadaver cortical tray, filled with an autog-enous bone marrow graft, also fixed withcircum-mandibular sutures. This way theyaugmented not only the submental areabut included the whole horizontal part ofthe mandible. Implant placement took
Lower lipMonofilament index number
1.65 2.83 3.22
ft Right Left Right Left Right
9 15 15 15 15 6 0 0 0 0
-
1498 Soehardi et al.
or h
ps
ne
ne
ne
ne
ne
neTable 4. Review of augmentation techniques fwere taken from the iliac crest.
StudyNumberof patients
Follow-umonth
Stellingsma et al.3
200420 24
Satow et al.5
199732 24
Verhoeven et al.6
199713 29
Verhoeven et al.7
200613 106
McGrath et al.9
199618 17
Bell et al.12
200214 48
Enislidis et al.13
20059 27
Perdijk et al.15
200745 36
Raghoebar 3 6 place 4 months after augmentation. Un-fortunately, their case series does not men-tion the number of patients treated, nor hastheir preliminary report been followed up.Bell et al.12 did the dissection through
skin, subcutaneous tissue, and platysma,and approached both the inferior, superior,anterior, and lateral borders of the mandi-ble. The mental nerves were identified andprotected. If necessary the inferior alveo-lar nerve was freed from its canal andrepositioned laterally into the adjacent softtissue. Previously harvested corticocan-cellous bone was then placed carefullyalong the superior and lateral aspects ofthe mandible extending as far posteriorlyas the retromolar trigone. This method,however, results in a large scar, impairsthe blood supply to the mandible, andcarries a high risk of damage to the mentalnerve.
et al.16 2000Raghoebar et al.17
200846 72
van der Meij et al.31
200517 52
Bianchi et al.32
20086 23
Ettl et al.33
201036 54
Haers et al.34
199181 60
Kent et al.35
198347 48
Stellingsma et al.36
199810 31
Vanassche et al.37
198855 30
Vermeeren et al.38
199631 60
HA, hydroxylapatite. the atrophic mandible for implant placement. W
,Augmentation technique
Type ofaugmentedmaterials
Sandwich osteotomy Autogenous bo
Sandwich osteotomy Autogenous boHA
One-stage upperborder onlay
Autogenous bo
One-stage upperborder onlay
Autogenous bo
One-stage upperborder onlay
Autogenous boHA
Two-stage lowerborder (rib) onlay
Autogenous bo
Distraction osteogenesis
Distraction osteogenesis
Distraction osteogenesis Gutta and Waite18 stressed that aug-mentation of the lower border can belimited to the submental area only. How-ever, these authors not only augmented thelower border but at the same time put bonestrips in the upper part of the mandible,thereby compromising the blood supply tothe atrophic mandible. They also advocat-ed identifying the mental nerves, therebyincreasing the risk of nerve damage.A review of the other augmentation
techniques for severely atrophic mand-ibles in combination with implant place-ment is presented in Table 4.3,57,9,12,13,1517,3138 Unfortunately, the data presentedare difficult to compare because of thedifferent techniques used to measureresorption and to define nerve damage.In conclusion, by limiting the lower
border augmentation to only the submen-tal area, certain advantages to existing
Distraction osteogenesis
One-stage upperborder onlay
Autogenous bone
Sandwich osteotomy Autogenous bone
Distraction osteogenesis
Sandwich osteotomy Autogenous boneHA
Upper border onlay Autogenous boneHA
Sandwich osteotomy Autogenous bone
Sandwich osteotomy Autogenous boneHA
One-stage upperborder onlay
Autogenous boneen not specifically mentioned, the bone grafts
Percentageof boneresorption(in n years)
Nervedamage,
%
Wounddehiscence(number ofpatients)
10% (2) 10%
, 12.7% (2) 16% 1
36% (3)
51% (10) 0% 3
, 20% (2) 11.1%
33% (0.5)
28%
0% Nonetechniques are offered, notably avoidingmental nerve dysesthesia. Whether thelong-term results will be equally satisfyingremains to be seen. The authors plan toreport these results in due course.
Funding
None.
Competing interests
None declared.
Ethical approval
The study was approved by the CMORegio Arnhem-Nijmegen (File numberCMO: 2013/528).
Patient consent
Not required.
8.7%
15% (4) 29.4% 2 (+2)
15.5% (0.5)
21.1% (0.5)
, 23% (4) 23.4%
, 15%
0%
, 30% (2.5) 29%
50% (5)
-
edentulous mandibles. Br J Oral Maxillofac
Surg 2005;43:399403.
omy using a SemmesWeinstein pressure
Lower border bone onlays for the class VI mandible 1499References
1. Cawood JI, Howell RA. A classification of
the edentulous jaws. Int J Oral Maxillofac
Surg 1988;17:2326.
2. Nedir R, Bischof M, Szmukler-Moncler S,
Bernard JP, Samson J. Predicting osseointe-
gration by means of implant primary stabili-
ty: a resonance-frequency analysis study
with delayed and immediately loaded ITI
SLA implants. Clin Oral Implants Res
2004;15:5208.
3. Stellingsma C, Raghoebar GM, Meijer HJ,
Stegenga B. The extremely resorbed mandi-
ble: a comparative prospective study of 2-
year results with three treatment strategies.
Int J Oral Maxillofac Implants 2004;19:563
77.
4. Moon JW, Choi BJ, Lee WH, An KM, Sohn
DS. Reconstruction of atrophic anterior
mandible using piezoelectric sandwich
osteotomy: a case report. Implant Dent
2009;18:195202.
5. Satow S, Slagter AP, Stoelinga PJ, Habets
LL. Interposed bone grafts to accommodate
endosteal implants for retaining mandibular
overdentures. A 17 year follow-up study.
Int J Oral Maxillofac Surg 1997;26:35864.
6. Verhoeven JW, Cune MS, Terlou M, Zoon
MA, de Putter C. The combined use of
endosteal implants and iliac crest onlay
grafts in the severely atrophic mandible: a
longitudinal study. Int J Oral Maxillofac
Surg 1997;26:3517.
7. Verhoeven JW, Cune MS, Ruijter J. Permu-
cosal implants combined with iliac crest
onlay grafts used in extreme atrophy of
the mandible: long-term results of a prospec-
tive study. Clin Oral Implants Res
2006;17:5866.
8. Lew D, Hinkle RM, Unhold GP, Shroyer JV,
Stutes RD. Reconstruction of the severely
atrophic edentulous mandible by means of
autogenous bone grafts and simultaneous
placement of osseointegrated implants. J
Oral Maxillofac Surg 1991;49:22833.
9. McGrath CJ, Schepers SH, Blijdorp PA,
Hoppenreijs TJ, Erbe M. Simultaneous
placement of endosteal implants and man-
dibular onlay grafting for treatment of the
atrophic mandible. A preliminary report. Int
J Oral Maxillofac Surg 1996;25:1848.
10. Enlow DH, Bianco HJ, Eklund S. The remo-
deling of the edentulous mandible. J Pros-
thet Dent 1976;36:68593.
11. Eyrich GK, Gratz KW, Sailer HF. Surgical
treatment of fractures of the edentulous man-
dible. J Oral Maxillofac Surg 1997;55:
10811087.
12. Bell RB, Blakey GH, White RP, Hillebrand
DG, Molina A. Staged reconstruction of the
severely atrophic mandible with autogenous
bone graft and endosteal implants. J Oral
Maxillofac Surg 2002;60:113541.
13. Enislidis G, Fock N, Ewers R. Distraction
osteogenesis with subperiosteal devices in14. Krenkel C, Grunert I. The Endo-Distractor
for preimplant mandibular regeneration. Rev
Stomatol Chir Maxillofac 2009;110:1726.
15. Perdijk FB, Meijer GJ, Strijen PJ, Koole R.
Complications in alveolar distraction osteo-
genesis of the atrophic mandible. Int J Oral
Maxillofac Surg 2007;36:91621.
16. Raghoebar GM, Heydenrijk K, Vissink A.
Vertical distraction of the severely resorbed
mandible. The Groningen distraction device.
Int J Oral Maxillofac Surg 2000;29:41620.
17. Raghoebar GM, Stellingsma C, Meijer HJ,
Vissink A. Vertical distraction of the severe-
ly resorbed edentulous mandible: an assess-
ment of treatment outcome. Int J Oral
Maxillofac Implants 2008;23:299307.
18. Gutta R, Waite PD. Cranial bone grafting and
simultaneous implants: a submental tech-
nique to reconstruct the atrophic mandible.
Br J Oral Maxillofac Surg 2008;46:4779.
19. Lekkas K, Wes BJ. Absolute augmentation
of the extremely atrophic mandible: a modi-
fied technique. J Maxillofac Surg 1981;9:
103107.
20. Pogrel MA. The lower border rib graft for
mandibular atrophy. J Oral Maxillofac Surg
1988;46:959.
21. Quinn PD, Kent K, MacAfee KA. Recon-
structing the atrophic mandible with inferior
border grafting and implants: a preliminary
report. Int J Oral Maxillofac Implants
1992;7:8793.
22. Reitman MJ, Brekke JH, Bresner M. Aug-
mentation of the deficient mandible by bone
grafting to the inferior border. J Oral Surg
1976;34:9168.
23. Ridley MT, Mason KG. Resorption of rib
graft to inferior border of the mandible. J
Oral Surg 1978;36:5468.
24. Sanders B, Cox R. Inferior-border rib grafting
for augmentation of the atrophic edentulous
mandible. J Oral Surg 1976;34:897900.
25. Sanders B. Rib grafting to the inferior border
of the mandible. J Oral Surg 1978;36:669.
26. Sanders B, Beumer J. Augmentation rib
grafting to the inferior border of the atrophic
edentulous mandible: a 5-year experience. J
Prosthet Dent 1982;47:1622.
27. Sanders B. Augmentation rib grafting to the
inferior border of the mandible: current con-
cepts. Head Neck Surg 1982;4:3249.
28. Kabasawa Y, Harada K, Jinno S, Satoh Y,
Maruoka Y, Omura K. A new evaluation
method for neurosensory disturbance in
the chin of patients undergoing mandibular
sagittal split ramus osteotomy: an applica-
tion of the heat flux technique. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod
2006;102:71924.
29. Takasaki Y, Noma H, Masaki H, Fujikawa
M, Alberdas JL, Tamura H, et al. A clinical
analysis of the recovery from sensory distur-
bance after sagittal splitting ramus osteot-aesthesiometer. Bull Tokyo Dent Coll
1998;39:18997.
30. Vriens JP, van der Glas HW. Extension of
normal values on sensory function for facial
areas using clinical tests on touch and two-
point discrimination. Int J Oral Maxillofac
Surg 2009;38:11548.
31. van der Meij EH, Blankestijn J, Berns RM,
Bun RJ, Jovanovic A, Onland JM, et al. The
combined use of two endosteal implants and
iliac crest onlay grafts in the severely atrophic
mandible by a modified surgical approach.
IntJ Oral Maxillofac Surg 2005;34:1527.
32. Bianchi A, Felice P, Lizio G, Marchetti C.
Alveolar distraction osteogenesis versus in-
lay bone grafting in posterior mandibular
atrophy: a prospective study. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod
2008;105:28292.
33. Ettl T, Gerlach T, Schusselbauer T, Gosau M,
Reichert TE, Driemel O. Bone resorption
and complications in alveolar distraction
osteogenesis. Clin Oral Investig 2010;14:
481489.
34. Haers PE, van Straaten W, Stoelinga PJ, de
Koomen HA, Blydorp PA. Reconstruction of
the severely resorbed mandible prior to ves-
tibuloplasty or placement of endosseous
implants. A 2 to 5 year follow-up. Int J Oral
Maxillofac Surg 1991;20:14954.
35. Kent JN, Quinn JH, Zide MF, Guerra LR,
Boyne PJ. Alveolar ridge augmentation
using nonresorbable hydroxylapatite with
or without autogenous cancellous bone.
J Oral Maxillofac Surg 1983;41:62942.
36. Stellingsma C, Raghoebar GM, Meijer HJ,
Batenburg RH. Reconstruction of the ex-
tremely resorbed mandible with interposed
bone grafts and placement of endosseous
implants. A preliminary report on outcome
of treatment and patients satisfaction. Br J
Oral Maxillofac Surg 1998;36:2905.
37. Vanassche BJ, Stoelinga PJ, de Koomen HA,
Blijdorp PA, Schoenaers JH. Reconstruction
of the severely resorbed mandible with in-
terposed bone grafts and hydroxylapatite. A
23 year follow-up. Int J Oral Maxillofac
Surg 1988;17:15760.
38. Vermeeren JI, Wismeijer D, van Waas MA.
One-step reconstruction of the severely
resorbed mandible with onlay bone grafts
and endosteal implants. A 5-year follow-up.
Int J Oral Maxillofac Surg 1996;25:1125.
Address:Antariksa SoehardiDepartment of Oral and MaxillofacialSurgery
Radboud UniversityNijmegen Medical CentreNijmegenThe NetherlandsTel.: +31 655355253E-mail: [email protected]
Lower border bone onlays toaugment the severely atrophic (class VI) mandible inpreparation for implants: apreliminary reportMaterials and methodsPatient selectionSurgical techniqueImplantsFollow-upAssessment of nerve function
ResultsDiscussionFundingCompeting interestsEthical approvalPatient consentReferences