Oh no! Intracranial Events While on VAD Support...7 Challenges to Rapid Stroke Management in...
Transcript of Oh no! Intracranial Events While on VAD Support...7 Challenges to Rapid Stroke Management in...

Oh no! Intracranial Events While on VAD Support
Kate Ryan, MD

Oh @#$%! Intracranial Events While on VAD Support
Kate Ryan, MD

3
Financial Disclosures
• No disclosures

4
Outline
• Background
• Scope of the problem using a case example
• Incidence
• Risk factors
• Interventions
• Pathways

5
Background
Congenital/acquired heart disease is the leading cause of stroke in children, and ventricular assist devices (VADs) are the leading cause of stroke in congenital/acquired heart disease
Current adult and pediatric stroke management guidelines are not applicable to children on VAD support because MRI is contraindicated, stopping/reversing anticoagulation may be life-threatening, and patients are often fragile or critically ill

6
AIS: Case presentation
• A 15 m/o boy with DCM who had been on the Berlin Heart EXCOR Pediatric VAD for 6 months stopped using his left arm while playing.
• While awaiting the stat head CT and neurology, questions began to emerge: – should the head CT be portable or not?– Who and how should we page neurology– Is the child eligible for a thrombectomy or thrombolysis if there is
an ischemic stroke, or craniotomy if there is a bleed?
• Although an initial plan was developed on the day of the stroke, the plan tended to change almost daily, especially as the mix of attendings (ICU, heart failure, neurology and neurosurgery) rotated on and off the primary service.

7
Challenges to Rapid Stroke Management in Pediatric VAD Patients
1. Index of suspicion for stroke is low in children so providers often attribute signs to other causes (less arm mobility to hurt arm, HA to migraines, or change in mental status to sedation)
2. Unable to perform gold-standard imaging for stroke guidelines (i.e. MRI)
3. Lack of clarity regarding who to page: neurology resident, neurology attending, stroke attending, ”rapid response”, “stroke code”, stat CT……leads to delays
4. No consensus on what to do with anticoagulation (stop, or actively reverse with vitamin K, FFP, or even prothrombin concentrate?)
5. Tendency for non-cardiology providers to assume that anticoagulation cannot be reversed, leading to important delays in management

8
Challenges to Rapid Stroke Management in Pediatric VAD Patients
8. Platelet inhibitors may be as important if not more important than anticoagulants in potentiating the risk of bleeding
9. Consensus on indications for craniotomy or thrombectomy not well-defined in children (on VAD support), and may vary by attending
10. Different stroke types require presence of different specialists (e.g. neuroradiology for acute ischemic stroke vs neurosurgery for intracranial hemorrhage)
11. No consensus on what to do with antithrombotic therapy prior to imaging
12. No consensus on how frequently to repeat head CTs as anticoagulants are restarted after a stroke
13. No consensus on when to re-activate on transplant list (i.e. bleeding risk on CPB)

9
Pulsatile Devices
• Of children treated with the Berlin Heart EXCOR® device as a bridge to transplant, 29% experienced at least 1 neurological event
• The majority of neurological events were ischemic strokes, and many of those occurred early in the course of support.
• Neurological injury was the leading cause of death after implantation of the Berlin Heart EXCOR® device
Neurological Complications and Outcomes in the Berlin Heart EXCOR® Pediatric Investigational Device Exemption Trial Lori C. Jordan, MD, PhD; Rebecca N. Ichord, MD; Olaf Reinhartz, MD; Tilman Humpl, MD; Sumit Pruthi, MD; Christine Tjossem, BS; David N. Rosenthal, MD

10
Continuous Flow Devices
• VanderPluym et al looked at 194 children (less than 19 years) and 247 young adults (age 19-30) patients supported with CF VAD
• 9.9% of children who were noted to have clinical strokes– 64% were ischemic– 32% were hemorrhagic– 4% were defined as other
• 12% of young adults were noted to have clinical strokes
• 56% were hemorrhagic
• 41% were ischemic
• 3% were defined as other
• No extra-axial bleeding was reported in adults, whereas 11 children (23%) with neurologic dysfunction were classified as having extra-axial bleeding on neuroimaging
Outcomes of children supported with an intracorporeal continuous-flow left ventricular assist system Christina J. VanderPluym, MD,a Iki Adachi, MD,b Robert Niebler, MD, Eric Griffiths, MD,d Francis Fynn-Thompson, MD,e Sharon Chen, MD, MPH,f Matthew J. O’Connor, MD,g Desiree Machado, MD,h Beth Hawkins, FNP,a Mark S. Bleiweis, MD,i Devin A. Koehl, BSc,jRyan S. Cantor, MSPH,j,k David Morales, MD,l and Angela Lorts, MD, MBAl

11
Adult Endovascular Intervention
• Prospectively collected data of LVAD patient registry from a single, tertiary center from October 2004 to November 2016
• 477 persons with LVAD, 49 (10.3%) AIS occurred time of AIS
• Of 25 (51%) persons who underwent CT angiography (CTA), 33% (16/49) had acute LVOs
• Thirty-one percent (5/16) of persons with acute LVOs underwent intra-arterial endovascular therapy.
• All of 5 cases presented with middle cerebral artery syndrome with a median pre-procedural National Institutes of Health Stroke Scale of 13 (Quick NIHSS primer: high score bad, low score good)
• Successful recanalization was achieved in all 5 cases.
Cory J. Ricea Sung-Min Chob Lucy Q. Zhanga Catherine Hassetta Randall C. Starlingc Ken Uchinoa The Management of Acute Ischemic Strokes and the Prevalence of Large Vessel Occlusion in Left Ventricular Assist Device. Cerebrovasc Dis 2018;46:213–217

12
Pediatric Endovascular Intervention
• Window for intervention is longer than for adults
• Intervention can be limited by patient size
• Stowe et al present a case of a 9-year-old boy with a ventricular assist device who presented with acute onset of dense right hemiparesis, global aphasia, and a pediatric NIHSS score of 23
Robert Clinton Stowe a,⇑, Peter Kan b, Day Burruss Breen a, Sonika Agarwal. Mechanical thrombectomy for pediatric acute stroke and ventricular assist device. Brain & Development 40 (2018) 81–84

13

14
Neurosurgical Interventions
• 11 yo 40 kg girl presented in May 2018 with acute decompensated heart failure and was cannulated to VA ECMO
• 3 Days later she was transitioned to CF-VAD
• 1 Month later was somnolent on exam and found to have a large left subdural hematoma

15
Neurosurgical Interventions

16
Outcomes
• Lack of data regarding outcomes following neurosurgical interventions for children on VAD support
• Can be difficult to appropriately counsel families given the risks inherent in interventions

17
Anticoagulation in the acute and subacute period
• In ischemic stroke, large size > 1/3 MCA territory and high NIHSS is considered to be a particular risk for impending bleed or malignant swelling
• For hemorrhage, imaging predictors of bleed expansion in adults have not been validated in children, and are typically based on a fixed volume, which is not appropriate for pediatric brains that grow over time
• Decisions surrounding reversal of anticoagulation, resumption of therapy and pace of escalation are often varied and arbitrary.

18
Neurocritical Care Management
• Permissive hypertension?
• Choice of antihypertensive agent?
• Expansion or a reduction in inotropic agents?
• Stop or reverse anticoagulation?
• Higher serum sodium levels?
• Sedation?

19
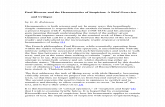
Pediatric VAD Stroke Summit
• The primary purpose of the meeting was:– To review the challenges of developing acute stroke
management guidelines for children on VAD support– To develop acute stroke management guidelines for each of
the common stroke types: acute ischemic stroke (IAS), intracranial hemorrhage (ICH) and subdural hematoma (SDH).
– To develop quality metrics to foster accountability to the guidelines

20
VAD Stroke Summit
• The multidisciplinary summit was held with representatives from the Pediatric VAD Team, Cardiac ICU, Neurology (including a national pediatric stroke expert from Vanderbilt), Neurosurgery, Neuroradiology, Interventional Radiology, Cardiac Anesthesia, Pharmacy, Adult Neurocritical Care, and the Adult VAD Team at Stanford
• Four stroke pathways were created: – (1) management prior to image confirmation of stroke;
– (2) management of arterial ischemic stroke;
– (3) management of intracranial hemorrhage
– (4) management of subdural hematoma

21
Acute Stroke Management Pathway
Head CT positive for
stroke
Get rid of the bleedy/clotty bit
Everything is awesome!

Page 211 “Peds Stroke Code”• Pediatric Neurology to
respond STAT (< 30 min)• HOLD antithrombotic
therapy• Attempt PIV but do not
delay CT• Send labs: CBC, Glucose,
BUN/Cr, PT/PTT/INR, blood cx x 2 (if concern for infection)
• Consider ordering reversal agents but DO NOT GIVE prior to discussion after imaging
LPCH Ventricular Assist Device (VAD) Stroke Diagnosis Pathway
Child on VAD with suspected
stroke symptoms
IF:✓ Concern for ischemic stroke with large vessel occlusion; and✓ PIV in place; and✓ Creatinine normal
IF✓ Concern for hemorrhage; or✓ Not safe to administer contrast; or✓ Unable to place PIV
✓ Acute-onset focal neurologic deficit (at least 1):• Weakness or numbness on one side
of the body• Inability to speak or understand• Vision loss in one or both eyes or
double vision• Gait instability, extreme dizziness or
incoordination• New onset seizure
OR
✓ NEW acute headache with at least 1 RED FLAG: • Altered mental status• Encephalopathy• Vomiting
OR
✓ Acute-onset altered mental status/obtundation
STAT Head CT/CTA
STAT Non-contrast Head CT (NCT)
Order STAT HEAD CT (Goal: First image < 30 minutes)
*If during off hours ADULT CT can be utilized
• Call peds neurology• Call peds neuroradiology
fellow on call
✓ New or old headache WITHOUT RED FLAGS (NO altered mental status,
encephalopathy, vomiting)
✓ No focal neurologic deficits
• Pos CT: continue to appropriate pathway (ischemic, hemorrhagic, or subdural)
• Neg CT AND persistent neuroconcerns: see ischemic pathway
• Neg CT AND no further neuroconcerns: resume usual care
• Consider increased frequency of neuroand device checks

VAD Ischemic Stroke Management Pathway
NCT/CTA: Pos ischemic
stroke OR
Neg but with persistent neurologic
deficit
✓ Transfer or Admit to
CVICU
• Start neuroprotectivemeasures for ischemic stroke*
• Re-examine patient to confirm deficit
• Call Neuro IR STAT• Call Cardiac Anesthesia• Consider IV tPA if INR < 1.5 and
last seen normal < 4.5 hours• Berlin: Consider pump change
• Resume Aspirin ASAP (<24h), consider restarting full antithrombotic therapy if no cortical signs (gaze preference, aphasia, neglect) in addition to weakness
• If on Berlin: Consider pump change
• Q1 hour pump checks x 24 hrs• Start neuroprotective
measures for ischemic stroke*• Repeat NCT scan @ 48 hrs
(sooner if concerns)
• Call neurosurgery for possible decompression
• Start neuroprotectivemeasures for increased ICP**
• Consider antithrombotic reversal
• If on Berlin: Consider pump change
• Repeat NCT scan @ 12-24 hrs
✓ Hypodensity >1/3 MCA territory; OR✓ Significant edema; OR✓ Bilateral cerebellar infarctions
✓ Negative or hypodensity <1/3 MCA territory; AND✓ No large vessel occlusion; AND✓ No hemorrhage; AND✓ Persistent neurologic deficit
Ensure full antithrombotic regimen is restarted if not alreadyRemain active on transplant list
• Refer to subdural or hemorrhagic pathways
• Timing of restarting antithrombotic therapy dependent on size/characteristics of hemorrhage after discussion with neurology/NSG
NCT stable &no
hemorrhage
NCT w/ hemorrha
gic conversio
n
✓ CTA: + vessel occlusion consistent w/ symptoms; AND ✓ NCT: normal or hypodensity <1/3 MCA territory or ASPECTS > 71
• Post-thrombectomy BP management based on discussion between Neuro IR, neuro, CVICU, and VAD teams
• Restart aspirin • Consider restarting other
antithrombotic therapy• Repeat NCT @ 48 hrs (sooner
if concerns)• Inactivate on transplant list
for 2 weeks
Cath lab for
thrombectomy
No thrombectom
y
• If antithrombotic therapy held, timing of restarting based on full team discussion with neurosurgery, neurology, CVICU, and VAD teams
• Repeat NCT based on team discussion
• Inactivate on transplant list for 2 weeks
Refer to the Appendix for neuroprotective measures for ischemic stroke (*) or for increased ICP (**)
1 ASPECT score = 10-pt score based on CT findings for MCA stroke

• Continue to hold antithrombotic therapy3
• Reverse heparin with protamine• Reverse anticoagulation with 4F-
PCC + Vit K for goal INR <=1.4• Transfuse platelets • Neurosurgical intervention if
indicated• Repeat NCT per NSG• Avoid factor VIIa (increased risk of
thrombosis)
VAD Hemorrhagic Stroke Management Pathway
• Hold antithrombotic therapy for 1-2 weeks3, then resume at low dose
• Titrate to goal antithrombotic therapy over 1-2 weeks
• Repeat NCT 12hrs after resuming antithrombotic therapy and again at full therapy (sooner if clinically indicated)
• If unable to obtain neuro exam, repeat NCT prior to resuming antithrombotic therapy
• Inactivate on transplant list until repeat NCT at full antithrombotic therapy
NCT: pos acute
hemorrhage (not subdural)
✓ Call neurosurgery✓ Start neuroprotectivemeasures for increased ICP** & hemorrhagic stroke***✓ Transfer or admit to CVICU
NO, and meets following:Tiny/small bleed1
AND no neurologic
deficits
Bleed expansion
1 Size of bleed as agreed upon by neurosurgical, neurology, and cardiology2 Minor or major neurologic deficit as agreed upon by neurosurgical, neurology, and cardiology3 When holding antithrombotic therapy, monitor for pump thrombosis: Berlin – Q1hr pump checks; CF-VADs – daily LDH
• Continue to hold antithrombotic therapy3
• Consider reversal of heparin with protamine
• Reverse anticoagulation with FFP+ Vit K for goal INR <=1.4
• Transfuse platelets • Q1h neurochecks (with
pupillometer) x 24 hrs• Repeat NCT @ 4-6 hrs• Avoid factor VIIa (increased risk of
thrombosis)
NO, and meets 1 of following:
• Moderate-sized bleed1
• Minor focal neurologic deficit2
• Continue to hold antithrombotic therapy3
• Q1hr neurochecks (with pupillometer) x 24 hrs
• Repeat NCT @ 4-6 hrs
Meets 1 of following:
• Urgent neurosurgical intervention planned
• Mass effect with >5mm midline shift
• Infratentoriallocation (posterior fossa)
• Significant hydrocephalus
• Clinical signs of herniation
• Major neurologic deficit2
Neuroimaging signs of active bleeding (CT black hole sign, CTA spot sign, fluid-fluid level)
Bleed expansion
YES
NCT stable
NCT stable
• Resume antithrombotic therapy at prior dose
• Remain active on transplant list
• Resume low dose antithrombotic therapy 24-48 hrs from initial scan and titrate to goal over 1-2 weeks
• If unable to obtain neuro exam, repeat NCT prior to resuming antithrombotic therapy
• Repeat NCT once at full anticoagulation
• Inactivate on transplant list until repeat NCT at full anticoagulation
Refer to the Appendix for neuroprotective measures for increased ICP (**) and hemorrhagic stroke (***)

• Transfer to CVICU (if on floor)• Continue to hold antithrombotic
therapy2
• Repeat NCT @ 12-24 hrs
VAD Subdural Hemorrhage Management Pathway
• Restart antithrombotic therapy at prior dose
NCT:pos subdural hemorrhage
✓ Call neurosurgery
• Transfer to CVICU (if on floor) • Start neuroprotective measures
for hemorrhagic stroke***• Continue to hold
antithrombotic therapy2
• Reverse heparin with protamine• Reverse anticoagulation with
4F-PCC + Vit K for a goal INR <=1.4
• Transfuse platelets • Repeat NCT @ 4-6 hours
Small subdural1
without neurologic deficit
Large size subdural1 + one of the following:• Significant
mass effect (including impending herniation)
• Neurologic deficit
Bleed expansion
CT stable
CT stable
• Resume full antithrombotic therapy
• Remain active on waitlist
• Consider repeat NCT @ 24 hrs if concern for acute bleedTiny
bleed/inciden
tal finding
1
• Transfer to CVICU (if on floor)• Start neuroprotective measures
for hemorrhagic stroke***• Continue to hold antithrombotic
therapy2
• Consider reversal with protamine/FFP+ Vit K
• Repeat NCT @ 4-6 hours
Small subdural1+ neuro deficit; ORmoderate subdural1 +/- neuro
deficit; ORlarge subdural1 without neuro
deficit
• Repeat NCT scan @ 48 hrs; if stable restart low-dose antithrombotic therapy
• Titrate to goal antithrombotic therapy over 4-7 days
• Repeat NCT once at full anticoagulation
• Inactivate on transplant list until repeat NCT at full anticoagulation
Bleed expansion
• Repeat NCT @ 48 hrs• Hold antithrombotic therapy for 4-7
days, then restart at low-dose• If unable to obtain neuro exam, repeat
NCT prior to resuming antithrombotic therapy
• Titrate to goal antithrombotic therapy over 1-2 weeks
• Repeat NCT once at full antithrombotic therapy
• Inactivate on transplant list until repeat NCT at full antithrombotic therapy
• Repeat NCT per neurosurgery• Hold antithrombotic therapy for 1-2
weeks, then restart at low-dose• If unable to obtain neuro exam, repeat
NCT prior to resuming antithrombotic therapy
• Titrate to goal antithrombotic therapy over 2 weeks
• Repeat NCT once at full antithrombotic therapy
• Inactivate on transplant list until repeat NCT at full antithrombotic therapy
No neurosur
gical interventi
on
Neurosurgical
intervention
1 Size of bleed as agreed upon by neurosurgical, neurology, and cardiology
For ***hemorrhagic neuroprotective measures, please refer to the Appendix

26
Neuroprotective Measures for Ischemic Stroke
Airway, Breathing, Circulation• Continuous cardiorespiratory monitoring• NPO, Head of bed FLAT• BP goals based on clinical scenario:
• If pulsatile pump, aim for systolic blood pressure 50-95%ile for age but can accept unsustained SBP 15% above 95%ile for age unless tPA candidate.
• If continuous-flow, Doppler pressures as high as tolerable (10mm Hg above baseline systolic Doppler goals, but no higher than 85)
• Target euvolemia and avoid hypovolemia: Isotonic fluids without dextrose unless hypoglycemic (0.9% NS at maintenance)
• Treat sustained severe hypertension with short acting, easily titratable agents (i.e. hydralazine, nicardipine, clevidipine; avoid nitroprusside and esmolol)
• Normoglycemia• Normothermia: Acetaminophen or cooling blanket for T>37.5; monitor for shivering• Seizure control with antiepileptic drugs if suspected seizure activity (i.e. 20mg/kg
fosphenytoin or Keppra 40mg/kg unless contraindications)
• If intubated, maintain pCO2 > 40

27
Neuroprotective Measures for Increased ICP
Airway, Breathing, Circulation• Continuous cardiorespiratory monitoring• NPO, Head of bed 30 degrees, midline• BP goals based on clinical scenario: • If pulsatile pump, aim for Systolic blood pressure 25-50%ile for age; avoid hypertension
and hypotension • If continuous-flow, aggressively maintain systemic Doppler pressure goal (hyper- and
hypotension may both be detrimental)
• Target euvolemia (general CVP 5-8)
• Target higher sodium goals in discussion with neurology• Treat hypertension with short acting, easily titratable agents (i.e. hydralazine,
nicardipine, clevidipine; avoid nitroprusside and esmolol)• Euglycemia; aggressively control hyperglycemia• Euthermia: Acetaminophen or cooling blanket for T>37.5; monitor for shivering• Seizure control with antiepileptic drugs if suspected seizure activity (i.e. 20mg/kg
fosphenytoin or Keppra 40mg/kg unless contraindications)
• If intubated, maintain pCO2 > 40

28
Neuroprotective measures for hemorrhagic/subdural stroke
*
• Airway, Breathing, Circulation• Continuous cardiorespiratory monitoring• NPO, Head of bed 30 degrees, midline• BP goals based on clinical scenario:
• If pulsatile pump, aim for systolic blood pressure 25-50%ile for age; avoid hypertension and hypotension
• If continuous-flow, aggressively maintain systemic Doppler pressure goal (hyper- and hypotension may both be detrimental)
• Target euvolemia (general CVP 5-8); hypotension and dehydration has potential to cause traction on bridging veins and expanding subdural bleed
• Target higher sodium goals in discussion with neurology
• Treat hypertension with short acting, easily titratable agents (i.e. hydralazine, nicardipine, clevidipine; avoid nitroprusside and esmolol)
• Euglycemia; aggressively control hyperglycemia• Euthermia: Acetaminophen or cooling blanket for T>37.5; monitor for shivering• Seizure control with antiepileptic drugs if suspected seizure activity (i.e. 20mg/kg fosphenytoin or Keppra unless
contraindications)
• If intubated, maintain pCO2 > 40

29
Take Home Points
• ANY neurologic change in a patient with a VAD should prompt you to think of stroke
• Timely diagnosis CAN make a difference
• The guideline outlined is consistent with existing stroke guidelines for non-VAD patients that emphasizes– Urgent detection
– Diagnosis
– Treatment