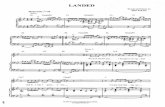
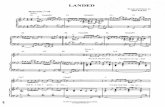
Uncovering Your True Landed Costs – What you don't know could ...
NOTE: Should you have landed here as a result of a search ... · copies to hand out. To ensure that...
Transcript of NOTE: Should you have landed here as a result of a search ... · copies to hand out. To ensure that...

NOTE: Should you have landed here as a result of a search engine (or other) link, be advised that these files contain material that is copyrighted by the American Medical Association. You are forbidden to download the files unless you read, agree to, and abide by the provisions of the copyright statement. Read the copyright statement now and you will be linked back to here.

JM Part a Medicare advisoryLatest Medicare News for JM Part A
palmettogba.com/jma
November 2018Volume 2018, Issue 11
The JM Part A Medicare Advisory contains coverage, billing and other information for Jurisdiction M Part A. This information is not intended to constitute legal advice. It is our official notice to those we serve concerning their responsibilities and obligations as mandated by Medicare regulations and guidelines. This information is readily available at no cost on the Palmetto GBA website. It is the responsibility of each facility to obtain this information and to follow the guidelines. The JM Part A Medicare Advisory includes information provided by the Centers for Medicare & Medicaid Services (CMS) and is current at the time of publication. The information is subject to change at any time. This bulletin should be shared with all health care practitioners and managerial members of the provider staff. Bulletins are available at no-cost from our website at http://www.PalmettoGBA.com/Medicare.
CPT only copyright 2017 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.The Code on Dental Procedures and Nomenclature is published in Current Dental Terminology (CDT), Copyright © 2012 American Dental Association (ADA). All rights reserved.
What’s Inside...MLN Connects ..............................................................................................................3
Weekly Articles .......................................................................................................3Special Edition Articles ..........................................................................................4Hurricane Michael and Medicare Disaster Related Florida and Georgia Claims MLN Matters Article – Revised ...............................................................................4Important New Medicare Card Mailing Update — Wave 7 Begins, Wave 5 Ends ..4
Hurricane Florence and Michael Information ...........................................................5Hurricane Michael and Medicare Disaster Related Florida and Georgia Claims ....5Hurricane Florence and Medicare Disaster Related North Carolina, South Carolina, and the Commonwealth of Virginia Claims .................................10
Multiple Provider Information ..................................................................................152019 Annual Update for the Health Professional Shortage Area (HPSA) Bonus Payments ................................................................................................................15Medicare Beneficiary Identifier (MBI) Look-up Tool ............................................16Help Us Improve/Enhance Our Website ................................................................18Get Your Medicare News Electronically ................................................................20Medicare Learning Network® (MLN) ...................................................................20
Hospital Information ..................................................................................................22Activation of Systematic Validation Edits for OPPS Providers with Multiple Service Locations ............................................................................22Fiscal Year (FY) 2019 Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital (LTCH) PPS Changes ............................................26
Influenza Vaccine Information...................................................................................392018-2019 Influenza (Flu) Resources for Health Care Professionals ....................39
Learning and Education Information .......................................................................43Home Health Referrals and Clinical Documentation Requirements Webinar: November 28, 2018 ................................................................................................43Quarterly Updates Webcast: December 12, 2018 ...................................................44 Educational Events Where You Can Ask Questions and Get Answers from Palmetto GBA ................................................................................................44

2 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Medical Policy Information ......................................................................................45Changes to the Laboratory National Coverage Determination (NCD) Edit Software for January 2019 ..............................................................................45Local Coverage Determinations (LCDs) ................................................................46Part A Local Coverage Determinations (LCDs) Updates .......................................52Part A Local Coverage Determinations (LCDs) Article Updates ...........................53Part A/B Medicare Administrative Contractor (MAC) Local Coverage Determinations (LCDs) Updates ............................................................................53Response to Comments for the Supervised Exercise Therapy for the Treatment of Peripheral Arterial Disease with Symptomatic Lower Extremity Intermittent Claudication Local Coverage Determination (LCD) – LCD Number: DL37774 ..55MolDX Local Coverage Determinations (LCDs) Updates ....................................60MolDX Local Coverage Determinations (LCDs) Article Updates ........................61Response to Comments for the MolDX: the MolDX: Corus® CAD Assay Local Coverage Determination (LCD) Article – LCD Number: DL37612 ....................61
Skilled Nursing Facility (SNF) Informaton .............................................................99Ensuring Occurrence Code 22 is Billed Correctly on Skilled Nursing Facility Inpatient Claims .....................................................................................................992019 Annual Update of Healthcare Common Procedure Coding System (HCPCS) Codes for Skilled Nursing Facility (SNF) Consolidated Billing (CB) Update ..................................................................................................................100
Tools You Can Use .....................................................................................................102Top 10 Inpatient Hospital Medical Review Denials Module ...............................102Top 10 Outpatient Medical Review Denials Module ...........................................103Top 10 Skilled Nursing Facility (SNF) Medical Review Denials Module ..........104New Medicare Card Information .........................................................................105
Helpful Information ..................................................................................................107Contact Information for Palmetto GBA Part A ....................................................107
Upcoming Part A Educational Events
Home Health Referrals and Clinical Documentation Requirements Webinar: November 28, 2018Your Part A/B, Home Health Railroad MACs are excited to announce this webinar collaboration. If you order home health services, this webinar is a great way to assure you are aware of physician roles and Medicare’s coverage criteria!
Quarterly Updates Webcast: December 12, 2018Palmetto GBA will host the Medicare Administrative Contractor Part A Quarterly Updates, Changes and Reminders Webcast at 10 a.m. to 11 a.m. ET on Wednesday, December 12, 2018.
For more information and registration instructions to attend these education sessions, please go to Page 43 of this issue.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
3 11/2018
MLN CONNECTS
MLN Connects will contain Medicare-related messages from the Centers of Medicare & Medicaid Services (CMS). These messages ensure planned, coordinated messages are delivered timely about Medicare-related topics. Please share with appropriate staff. To view the most recent issues, please copy and paste the following links into your Web browser:
Weekly Articles
October 18, 2018https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Downloads/2018-10-18-eNews.pdf
October 11, 2018https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Downloads/2018-10-11-eNews.pdf
October 4, 2018https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Downloads/2018-10-04-eNews.pdf
September 27, 2018https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Downloads/2018-09-27-eNews.pdf

4 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Special Edition Articles
October 12, 2018
Hurricane Michael and Medicare Disaster Related Florida and Georgia Claims MLN Matters Article – Revised
The President declared a state of emergency for the states of Florida and Georgia, and the HHS Secretary declared a Public Health Emergency, which allows for CMS programmatic waivers based on Section 1135 of the Social Security Act. A revised MLN Matters Special Edition Article on Hurricane Michael and Medicare Disaster Related Florida and Georgia Claims (https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/SE18021.pdf) is available. Learn about blanket waivers CMS issued for the impacted geographical areas. These waivers will prevent gaps in access to care for beneficiaries impacted by the emergency. This article was revised to add information regarding the emergency declared for the state of Georgia.
October 15, 2018
Important New Medicare Card Mailing Update — Wave 7 Begins, Wave 5 Ends
CMS has started mailing (https://www.cms.gov/Medicare/New-Medicare-Card/NMC-Mailing-Strategy.pdf) new Medicare cards to people with Medicare who live in Wave 7 states and territories including: Kentucky, Louisiana, Michigan, Mississippi, Missouri, Ohio, Puerto Rico, Tennessee, and the Virgin Islands.
We are finished mailing cards to people with Medicare who live in states within Waves 1 through 4 and now Wave 5. If someone with Medicare who lives in one of these states says they did not get a card, you should instruct them to:
∗ Sign into MyMedicare.gov (https://www.mymedicare.gov/) to see if we mailed their card. If so, they can print an official card. They will need to create an account if they do not already have one.
∗ Call 1-800-MEDICARE (1-800-633-4227) where we can verify their identity, check their address, and help them get their new card.
You can also print out and give them a copy of Still Waiting for Your New Card? (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Tear-Off-for-After-Card-Mailing-Ends.pdf), or you can order (https://productordering.cms.hhs.gov/) copies to hand out.
To ensure that people with Medicare continue to get care, you can use either the former Social Security number-based Health Insurance Claim Number (HICN) or the new alpha-numeric Medicare Beneficiary Identifier (MBI) for all Medicare transactions through December 31, 2019.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
5 11/2018
People with Medicare should continue to protect their new number to prevent medical identity theft and health care fraud, especially during Medicare Open Enrollment. View and share our new Guard your Medicare card (https://www.youtube.com/watch?v=D_-dHiln4bg&feature=youtu.be) video, which reminds people with Medicare to beware of scams. There are also new fraud prevention products on our new Medicare card Outreach & Education (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Products-to-share-with-beneficiaries.html) webpage for you to share with people with Medicare:
∗ Drop-in article (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Drop-in-Article-on-NMC-Scams.pdf) (also in Spanish (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Spanish-Drop-in-NMC-Medicare-Scams.pdf)) and Public Service Announcement script (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/PSA-NMC-Scams.pdf) reminding people to be wary of scams
∗ Flyer (https://www.cms.gov/Outreach-and-Education/Outreach/Partnerships/Downloads/2017-fightfraud-guardmcare.pdf) (also in Spanish (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Spanish-Drop-in-Article-on-NMC-Scams.pdf)) with fraud prevention tips during Open Enrollment
Continue to direct people with Medicare to Medicare.gov/NewCard (https://www.medicare.gov/NewCard) for information about the mailings and to sign up to get emails about the status of card mailings in their state.
HURRICANE FLORENCE AND MICHAEL INFORMATION
Hurricane Michael and Medicare Disaster Related Florida and Georgia Claims MLN Matters Number: SE18021 Revised Article Release Date: October 12, 2018 Related CR Transmittal Number: N/A Related Change Request (CR) Number: N/A Effective Date: N/A Implementation Date: N/A
Note: This article was revised on October 12, 2018, to add information regarding the emergency declared for the State of Georgia as a result of Hurricane Michael.
Provider Types Affected This MLN Matters® Special Edition Article is intended for providers and suppliers who submit claims to Medicare Administrative Contractors (MACs) for services provided to Medicare beneficiaries in the states of Florida and Georgia who were affected by Hurricane Michael.

6 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Provider Information Available On October 9, 2018, pursuant to the Robert T. Stafford Disaster Relief and Emergency Assistance Act, President Trump declared that, as a result of the effects of Hurricane Michael, an emergency exists in the State of Florida. On October 10, 2018, President Trump declared a similar emergency for the State of Georgia as a result of Hurricane Michael. Also, on October 9, 2018, Secretary Azar of the Department of Health & Human Services declared that a public health emergency exists in Florida and authorized waivers and modifications under Section 1135 of the Social Security Act (the Act), retroactive to October 7, 2018, for Florida. Also, on October 11, 2018, Secretary Azar declared that a public health emergency exists in the State of Georgia, retroactive to October 9, 2018, and authorized the same waivers and modifications for Georgia.
On October 9, 2018, the Administrator of the Centers for Medicare & Medicaid Services (CMS) authorized waivers under Section 1812(f) of the Social Security Act for the state of Florida for those people who are evacuated, transferred, or otherwise dislocated as a result of the effect of Hurricane Michael in 2018, retroactive to October 7, 2018. On October 11, 2018, the CMS Administrator authorized the same waivers for the state of Georgia, retroactive to October 9, 2018.
Under Section 1135 or 1812(f) of the Social Security Act, CMS has issued several blanket waivers in the impacted geographical areas of the states of Florida and Georgia. These waivers will prevent gaps in access to care for beneficiaries impacted by the emergency. Providers do not need to apply for an individual waiver if a blanket waiver has been issued. Providers can request an individual Section 1135 waiver, if there is no blanket waiver, by following the instructions available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Requesting-an-1135-Waiver-Updated-11-16-2016.pdf. The most current waiver information is available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page.html. See the Background section of this article for more details. Background Section 1135 and Section 1812(f) Waivers As a result of the aforementioned declaration, CMS has instructed the MACs as follows: 1. Change Request (CR) 6451 (Transmittal 1784, Publication 100-04) issued on July 31, 2009, applies to items and services furnished to Medicare beneficiaries within the State of Florida from October 7, 2018, for the duration of the emergency and for the State of Georgia from October 9, 2018, for the duration of the emergency. In accordance with CR6451, use of the “DR” condition code and the “CR” modifier are mandatory on claims for items and services for which Medicare payment is conditioned on the presence of a “formal waiver” including, but not necessarily limited to, waivers granted under either Section 1135 or Section 1812(f) of the Act.
2. The most current information is available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page.html. Medicare FFS Questions & Answers (Q&As) posted on the waivers and flexibilities page at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Resources/Waivers-and-flexibilities.html, and also referenced below are applicable for items and services furnished to Medicare beneficiaries within the States of Florida and Georgia.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
7 11/2018
These Q&As are displayed in two files:
• One file addresses policies and procedures that are applicable without any Section 1135 or other formal waiver. These policies are always applicable in any kind of emergency or disaster, including the current emergency in Florida and Georgia.
• Another file addresses policies and procedures that are applicable only with approved Section 1135 waivers or, when applicable, approved Section 1812(f) waivers. These Q&As are applicable for approved Section 1135 blanket waivers and approved individual 1135 waivers requested by providers and are effective October 7, 2018, for Florida and October 9, 2018, for Georgia.
In both cases, the links below will open the most current document. The date included in the document filename will change as new information is added, or existing information is revised.
a) Q&As applicable without any Section 1135 or other formal waiver are available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Consolidated_Medicare_FFS_Emergency_QsAs.pdf.
b) Q&As applicable only with a Section 1135 waiver or, when applicable, a Section 1812(f) waiver, are available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/MedicareFFS-EmergencyQsAs1135Waiver.pdf.
Blanket Waivers Issued by CMS Under the authority of Section 1135 (or, as noted below, Section 1812(f)), CMS has issued blanket waivers in the affected areas of Florida and Georgia. Individual facilities do not need to apply for the following approved blanket waivers:
Skilled Nursing Facilities (SNFs)
• Section 1812(f): This waiver of the requirement for a 3-day prior hospitalization for coverage of a SNF stay provides temporary emergency coverage of SNF services without a qualifying hospital stay, for those people who are evacuated, transferred, or otherwise dislocated as a result of the effect of Hurricane Michael in the States of Florida and Georgia. In addition, for certain beneficiaries who recently exhausted their SNF benefits, it authorizes renewed SNF coverage without first having to start a new benefit period (Blanket waiver for all impacted facilities).
• 42 CFR 483.20: Waiver provides relief to SNFs on the timeframe requirements for Minimum Data Set assessments and transmission (Blanket waiver for all impacted facilities).
Home Health Agencies
• 42 CFR 484.20(c)(1): This waiver provides relief to Home Health Agencies on the timeframes related to OASIS Transmission (Blanket waiver for all impacted agencies).
• To ensure the correct processing of home health disaster related claims, Medicare Administrative Contractors (MACs) are allowed to extend the auto-cancellation date of Requests for Anticipated Payment (RAPs).

8 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Critical Access Hospitals This action waives the requirements that Critical Access Hospitals limit the number of beds to 25, and that the length of stay be limited to 96 hours. (Blanket waiver for all impacted hospitals)
Housing Acute Care Patients In Excluded Distinct Part Units
CMS has determined it is appropriate to issue a blanket waiver to IPPS hospitals that, as a result of Hurricane Michael, need to house acute care inpatients in excluded distinct part units, where the distinct part unit’s beds are appropriate for acute care inpatient. The IPPS hospital should bill for the care and annotate the patient’s medical record to indicate the patient is an acute care inpatient being housed in the excluded unit because of capacity issues related to Hurricane Michael. (Blanket waiver for all IPPS hospitals located in the affected areas that need to use distinct part beds for acute care patients as a result of the hurricane.)
Care for Excluded Inpatient Psychiatric Unit Patients in the Acute Care Unit of a Hospital CMS has determined it is appropriate to issue a blanket waiver to IPPS and other acute care hospitals with excluded distinct part inpatient psychiatric units that, as a result of Hurricane Michael, need to relocate inpatients from the excluded distinct part psychiatric unit to an acute care bed and unit. The hospital should continue to bill for inpatient psychiatric services under the inpatient psychiatric facility prospective payment system for such patients and annotate the medical record to indicate the patient is a psychiatric inpatient being cared for in an acute care bed because of capacity or other exigent circumstances related to the hurricane. This waiver may be utilized where the hospital’s acute care beds are appropriate for psychiatric patients and the staff and environment are conducive to safe care. For psychiatric patients, this includes assessment of the acute care bed and unit location to ensure those patients at risk of harm to self and others are safely cared for.
Care for Excluded Inpatient Rehabilitation Unit Patients in the Acute Care Unit of a Hospital CMS has determined it is appropriate to issue a blanket waiver to IPPS and other acute care hospitals with excluded distinct part inpatient rehabilitation units that, as a result of Hurricane Michael, need to relocate inpatients from the excluded distinct part rehabilitation unit to an acute care bed and unit. The hospital should continue to bill for inpatient rehabilitation services under the inpatient rehabilitation facility prospective payment system for such patients and annotate the medical record to indicate the patient is a rehabilitation inpatient being cared for in an acute care bed because of capacity or other exigent circumstances related to the hurricane. This waiver may be utilized where the hospital’s acute care beds are appropriate for providing care to rehabilitation patients, and such patients continue to receive intensive rehabilitation services.
Emergency Durable Medical Equipment, Prosthetics, Orthotics, and Supplies for Medicare Beneficiaries Impacted by an Emergency or Disaster
As a result of Hurricane Michael, CMS has determined it is appropriate to issue a blanket waiver to suppliers of Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) where DMEPOS are lost, destroyed, irreparably damaged, or otherwise rendered unusable. Under this waiver, the face-to-face requirement, a new physician’s order, and new medical necessity documentation are not required for replacement. Suppliers must still include a narrative description on the claim explaining the

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
9 11/2018
reason why the equipment must be replaced and are reminded to maintain documentation indicating that the DMEPOS were lost, destroyed, irreparably damaged or otherwise rendered unusable as a result of the hurricane.
For more information refer to the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies for Medicare Beneficiaries Impacted by an Emergency or Disaster fact sheet at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Emergency-DME-Beneficiaries-Hurricanes.pdf. Medicare Advantage Plan or other Medicare Health Plan Beneficiaries
CMS reminds suppliers that Medicare beneficiaries enrolled in a Medicare Advantage or other Medicare Health Plans should contact their plan directly to find out how it replaces DMEPOS damaged or lost in an emergency or disaster. Beneficiaries who do not have their plan’s contact information can contact 1-800-MEDICARE (1-800-633-4227) for assistance.
Replacement Prescription Fills Medicare payment may be permitted for replacement prescription fills (for a quantity up to the amount originally dispensed) of covered Part B drugs in circumstances where dispensed medication has been lost or otherwise rendered unusable by damage due to the disaster or emergency.
Requesting an 1135 Waiver Information for requesting an 1135 waiver, when a blanket waiver hasn’t been approved, can be found at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Requesting-an-1135-Waiver-Updated-11-16-2016.pdf.
Additional Information If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
The Centers for Disease Control and Prevention released ICD-10-CM coding advice to report healthcare encounters in the hurricane aftermath.
Providers may also want to review the CMS Emergency and Preparedness webpage at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/EPRO-Home.html.
Providers may also want to view the Survey and Certification Frequently Asked Questions at https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/index.html. Document History
Date of Change Description October 12, 2018 The article was revised to add information regarding the emergency
declared for the State of Georgia as a result of Hurricane Michael. October 11, 2018 Initial article released.

10 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Hurricane Florence and Medicare Disaster Related North Carolina, South Carolina, and the Commonwealth of Virginia Claims
MLN Matters Number: SE18014 Revised Article Release Date: October 10, 2018 Related CR Transmittal Number: N/A Related Change Request (CR) Number: N/A Effective Date: N/A Implementation Date: N/A
Note: This article was revised on October 10, 2018, to add the section on Accountable Care Organizations (ACOs) on page 5. All other information is unchanged.
Provider Types Affected This MLN Matters® Special Edition Article is intended for providers and suppliers who submit claims to Medicare Administrative Contractors (MACs) for services provided to Medicare beneficiaries in the States of North Carolina, South Carolina, and the Commonwealth of Virginia who were affected by Hurricane Florence.
Provider Information Available On September 10, 2018, pursuant to the Robert T. Stafford Disaster Relief and Emergency Assistance Act, President Trump declared that, as a result of the effects of Hurricane Florence, an emergency exists in North Carolina and South Carolina. On September 11, 2018, President Trump declared an emergency exists in the Commonwealth of Virginia as a result of Hurricane Florence. Also, on September 11, 2018, Secretary Azar of the Department of Health & Human Services declared that a public health emergency exists in North Carolina and South Carolina and authorized waivers and modifications under Section 1135 of the Social Security Act (the Act), retroactive to September 7, 2018, for the State of North Carolina and retroactive to September 8, 2018, for the State of South Carolina. On September 12, Secretary Azar declared a public health emergency exists in the Commonwealth of Virginia, retroactive to September 8, 2018.
On September 13, 2018, the Administrator of the Centers for Medicare & Medicaid Services (CMS) authorized waivers under Section 1812(f) of the Social Security Act for the States of North Carolina, South Carolina, and the Commonwealth of Virginia for those people who are evacuated, transferred, or otherwise dislocated as a result of the effect of Hurricane Florence in 2018.
Under Section 1135 or 1812(f) of the Social Security Act, the CMS has issued several blanket waivers in the impacted geographical areas of the States of North Carolina, South Carolina, and the Commonwealth of Virginia. These waivers will prevent gaps in access to care for beneficiaries impacted by the emergency. Providers do not need to apply for an individual waiver if a blanket waiver has been issued. Providers can request an individual Section 1135 waiver, if there is no blanket waiver, by following the instructions available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Requesting-an-1135-Waiver-Updated-11-16-2016.pdf.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
11 11/2018
The most current waiver information is available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page.html. See the Background section of this article for more details.
Background
Section 1135 and Section 1812(f) Waivers As a result of the aforementioned declaration, CMS has instructed the MACs as follows:
1. Change Request (CR) 6451 (Transmittal 1784, Publication 100-04) issued on July 31, 2009, applies to items and services furnished to Medicare beneficiaries within the State of North Carolina from September 7, 2018, and the States of South Carolina and the Commonwealth of Virginia from September 8, 2018, for the duration of the emergency. In accordance with CR6451, use of the “DR” condition code and the “CR” modifier are mandatory on claims for items and services for which Medicare payment is conditioned on the presence of a “formal waiver” including, but not necessarily limited to, waivers granted under either Section 1135 or Section 1812(f) of the Act.
2. The most current information is available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page.html. Medicare FFS Questions & Answers (Q&As) posted on the waivers and flexibilities page at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Resources/Waivers-and-flexibilities.html , and also referenced below are applicable for items and services furnished to Medicare beneficiaries within the States of North Carolina, South Carolina, and the Commonwealth of Virginia. These Q&As are displayed in two files:
• One file addresses policies and procedures that are applicable without any Section 1135 or other formal waiver. These policies are always applicable in any kind of emergency or disaster, including the current emergency in North Carolina, South Carolina and the Commonwealth of Virginia.
• Another file addresses policies and procedures that are applicable only with approved Section 1135 waivers or, when applicable, approved Section 1812(f) waivers. These Q&As are applicable for approved Section 1135 blanket waivers and approved individual 1135 waivers requested by providers and are effective September 7, 2018, for North Carolina and September 8, 2018, for South Carolina and the Commonwealth of Virginia.
In both cases, the links below will open the most current document. The date included in the document filename will change as new information is added, or existing information is revised.
a) Q&As applicable without any Section 1135 or other formal waiver are available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Consolidated_Medicare_FFS_Emergency_QsAs.pdf.
b) Q&As applicable only with a Section 1135 waiver or, when applicable, a Section 1812(f) waiver, are available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/MedicareFFS-EmergencyQsAs1135Waiver.pdf.

12 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Blanket Waivers Issued by CMS Under the authority of Section 1135 (or, as noted below, Section 1812(f)), CMS has issued blanket waivers in the affected area of the States of North Carolina, South Carolina, and the Commonwealth of Virginia. Individual facilities do not need to apply for the following approved blanket waivers:
Skilled Nursing Facilities
• Section 1812(f): Waiver of the requirement for a 3-day prior hospitalization for coverage of a Skilled Nursing Facility (SNF) stay provides temporary emergency coverage of SNF services without a qualifying hospital stay, for those people who are evacuated, transferred, or otherwise dislocated as a result of the effect of Hurricane Florence in the States of North Carolina, South Carolina, and the Commonwealth of Virginia in 2018. In addition, for certain beneficiaries who recently exhausted their SNF benefits, it authorizes renewed SNF coverage without first having to start a new benefit period (Blanket waiver for all impacted facilities).
• 42 CFR 483.20: Waiver provides relief to SNFs on the timeframe requirements for Minimum Data Set assessments and transmission (Blanket waiver for all impacted facilities).
Home Health Agencies
• 42 CFR 484.20(c)(1): This waiver provides relief to Home Health Agencies on the timeframes related to OASIS Transmission (Blanket waiver for all impacted agencies).
• To ensure the correct processing of home health disaster related claims, Medicare Administrative Contractors (MACs) are allowed to extend the auto-cancellation date of Requests for Anticipated Payment (RAPs).
Critical Access Hospitals
This action waives the requirements that Critical Access Hospitals limit the number of beds to 25, and that the length of stay be limited to 96 hours. (Blanket waiver for all impacted hospitals)
Housing Acute Care Patients In Excluded Distinct Part Units
CMS has determined it is appropriate to issue a blanket waiver to IPPS hospitals that, as a result of Hurricane Florence, need to house acute care inpatients in excluded distinct part units, where the distinct part unit’s beds are appropriate for acute care inpatient. The IPPS hospital should bill for the care and annotate the patient’s medical record to indicate the patient is an acute care inpatient being housed in the excluded unit because of capacity issues related to Hurricane Florence. (Blanket waiver for all IPPS hospitals located in the affected areas that need to use distinct part beds for acute care patients as a result of the hurricane.)
Care for Excluded Inpatient Psychiatric Unit Patients in the Acute Care Unit of a Hospital
CMS has determined it is appropriate to issue a blanket waiver to IPPS and other acute care hospitals with excluded distinct part inpatient psychiatric units that, as a result of Hurricane Florence, need to relocate inpatients from the excluded distinct part psychiatric unit to an acute care bed and unit. The

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
13 11/2018
hospital should continue to bill for inpatient psychiatric services under the inpatient psychiatric facility prospective payment system for such patients and annotate the medical record to indicate the patient is a psychiatric inpatient being cared for in an acute care bed because of capacity or other exigent circumstances related to the hurricane. This waiver may be utilized where the hospital’s acute care beds are appropriate for psychiatric patients and the staff and environment are conducive to safe care. For psychiatric patients, this includes assessment of the acute care bed and unit location to ensure those patients at risk of harm to self and others are safely cared for.
Care for Excluded Inpatient Rehabilitation Unit Patients in the Acute Care Unit of a Hospital
CMS has determined it is appropriate to issue a blanket waiver to IPPS and other acute care hospitals with excluded distinct part inpatient Rehabilitation units that, as a result of Hurricane Florence, need to relocate inpatients from the excluded distinct part Rehabilitation unit to an acute care bed and unit. The hospital should continue to bill for inpatient rehabilitation services under the inpatient rehabilitation facility prospective payment system for such patients and annotate the medical record to indicate the patient is a rehabilitation inpatient being cared for in an acute care bed because of capacity or other exigent circumstances related to the hurricane. This waiver may be utilized where the hospital’s acute care beds are appropriate for providing care to rehabilitation patients and such patients continue to receive intensive rehabilitation services.
Emergency Durable Medical Equipment, Prosthetics, Orthotics, and Supplies for Medicare Beneficiaries Impacted by an Emergency or Disaster
As a result of Hurricane Florence, CMS has determined it is appropriate to issue a blanket waiver to suppliers of Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) where DMEPOS is lost, destroyed, irreparably damaged, or otherwise rendered unusable. Under this waiver, the face-to-face requirement, a replacement. Suppliers must still include a narrative description on the claim explaining the reason why the equipment must be replaced and are reminded to maintain documentation indicating that the DMEPOS was lost, destroyed, irreparably damaged or otherwise rendered unusable as a result of the hurricane.
For more information refer to the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies for Medicare Beneficiaries Impacted by an Emergency or Disaster fact sheet at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Emergency-DME-Beneficiaries-Hurricanes.pdf.
Medicare Advantage Plan or other Medicare Health Plan Beneficiaries
CMS remind suppliers that Medicare beneficiaries enrolled in a Medicare Advantage or other Medicare Health Plans should contact their plan directly to find out how it replaces DMEPOS damaged or lost in an emergency or disaster. Beneficiaries who do not have their plan’s contact information can contact 1-800-MEDICARE (1-800-633-4227) for assistance.

14 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Performance Year 2019 ACO Participant List and SNF Affiliate List Change Request: Response to Hurricane Florence The Round 3 deadline is extended for ACOs and ACOs with ACO participants and/or SNF affiliates impacted by Hurricane Florence in North Carolina, South Carolina, and the Commonwealth of Virginia. The deadline for these ACOs to submit change request in ACO-Management System (ACO-MS) to add or modify its ACO Participant List and/or SNF Affiliate List is extended until October 26, 2018, at 12:00 p.m. (noon) Eastern Time (ET), for an effective date of January 1, 2019.
Replacement Prescription Fills Medicare payment may be permitted for replacement prescription fills (for a quantity up to the amount originally dispensed) of covered Part B drugs in circumstances where dispensed medication has been lost or otherwise rendered unusable by damage due to the emergency.
Requesting an 1135 Waiver Information for requesting an 1135 waiver, when a blanket waiver hasn’t been approved, can be found at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Requesting-an-1135-Waiver-Updated-11-16-2016.pdf.
Additional Information If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list. The Centers for Disease Control and Prevention released ICD-10-CM coding advice to report healthcare encounters in the hurricane aftermath.
Providers may also want to review the CMS Emergency and Preparedness webpage at https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/EPRO-Home.html.
Providers may also want to view the Survey and Certification Frequently Asked Questions at https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/index.html.
Document History
Date of Change Description October 10, 2018 This article was revised on October 10, 2018, to add the section on ACOs
on page 5. September 14, 2018 Initial article released.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
15 11/2018
MULTIPLE PROVIDER INFORMATION
2019 Annual Update for the Health Professional Shortage Area (HPSA) Bonus Payments
MLN Matters Number: MM10968 Related CR Release Date: September 28, 2018 Related CR Transmittal Number: R4142CP Related Change Request (CR) Number: 10968 Effective Date: January 1, 2019 Implementation Date: January 7, 2019
Provider Types Affected This MLN Matters Article is intended for physicians and providers billing Medicare Administrative Contractors (MACs) for services provided to Medicare beneficiaries.
Provider Action Needed Change Request (CR) 10968 provides files for the automated payments of Health Professional Shortage Area (HPSA) bonuses for dates of service January 1, 2019, through December 31, 2019. Make sure your billing staffs are aware of these changes.
Background Section 413(b) of the Medicare Prescription Drug, Improvement and Modernization Act of 2003 mandated an annual update to the automated HPSA bonus payment file. The Centers for Medicare & Medicaid Services (CMS) automated HPSA ZIP code file are populated using the latest designations as close as possible to November 1st of each year. The HPSA ZIP code file shall be made available to the MACs in early December of each year. MACs shall implement the HPSA ZIP code file and for claims with dates of service January 1st to December 31st of the following year and make automatic HPSA bonus payments to physicians providing eligible services in a ZIP code contained on the file.
You should review the Physician Bonuses webpage at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HPSAPSAPhysicianBonuses/index.html each year to determine whether you need to add modifier AQ to your claim in order to receive the bonus payment, or to see if the ZIP code in which you rendered services will automatically receive the HPSA bonus payment.
Additional Information The official instruction, CR10968, issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4142CP.pdf.

16 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description September 28, 2018 Initial article released.
Medicare Beneficiary Identifier (MBI) Look-up Tool
Palmetto GBA is excited to announce that the Medicare Beneficiary Identifier (MBI) Look-up tool is now available in eServices! This tool allows providers to use our secure online portal to obtain the new MBI number when patients do not present their Medicare card. The MBI Look-up tool will only return an MBI if the new Medicare card has been mailed to avoid potential confusion if the MBI is used before the beneficiary receives their new Medicare card.
As background, the New Medicare Card Project, was established in the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 which mandates the removal of the Social Security Number (SSN)-based Health Insurance Claim Number (HICN) from Medicare cards by April 2019. CMS began mailing new Medicare cards with the MBI on April 2, 2018.
From April 1, 2018 to December 31, 2019, CMS will offer a transition period during which the system will accept both HICNs and MBIs on Medicare transactions (including eligibility requests and claims) for beneficiaries in the Medicare program prior to April 1, 2018 (i.e., those who received a HICN on their Medicare card). Note: Providers should not submit both numbers on the same transaction.
Beginning in January 2020, physicians may only use MBIs, with limited exceptions. When the new Medicare card is mailed to people with Medicare, you will be able to use the eServices MBI Look-Up Tool to obtain a patient’s MBI. To submit an inquiry you must do the following:
• Once logged into eServices, click on the MBI LOOKUP tab located in the header of the portal
• Complete the required* fields:
• Beneficiary’s Last Name
• First Name
• Date of birth and
• Social security number. NOTE: The social security number must be in the XXX-XX-XXXX format
• To meet our CAPTCHA requirements, you must select the I’M NOT A ROBOT checkbox
• Click SUBMIT INQUIRY

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
17 11/2018
Figure 1: MBI Lookup Tab
Look-Up Tool Status ResultsIf the inquiry successfully returns an MBI, the screen will refresh with the data at the bottom.
Figure 2: MBI Lookup Successful Response Screenshot
In the event that your MBI lookup request does not result in a successful response, eServices will display error messages to assist you. If any required fields are left blank or are not in a proper format, a message will appear advising you which fields to correct.

18 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Figure 3: MBI Lookup Unsuccessful Response Screenshot
Check the CMS New Medicare Card Project Outreach & Education webpage (https://www.cms.gov/Medicare/New-Medicare-Card/Outreach-and-Education/Outreach-and-education.html) for additional information.
Help Us Improve/Enhance Our Website
We need your help to enhance the Palmetto GBA website. As a valued website visitor, only you know what information and tools are needed to assist you with your work.
Your input is important! Please complete our short survey that’s sponsored by CMS and conducted by ForeSee Results. It represents your voice and provides us with detailed information on the types of services you like, want, or are dissatisfied with on the website. Please be specific in your evaluation of the website. Your detailed answers help us ‘get it right’!
Palmetto GBA strives to ensure your experience with our website provides accurate, detailed, and current information. With the content changing daily, it’s best to access the website regularly to ensure you have the most current information. We have found that some visitors print old forms and articles that may have become obsolete So it’s important to visit often.
If you have taken the survey in the past, Thank You! We have used those results to add many new features to help you diagnose and fix claim denials, stay in compliance with Medicare regulations, and ultimately, better serve your patients.
We encourage you to complete this survey and appreciate your feedback. Each new idea, self-service tool, and article depends on you, and your participation in our Foresee survey.
Please complete the survey today! https://survey.foreseeresults.com/survey/display?cid=wtsU0tp0khBZxlUgcpcMxA==&sid=link-palmetto-jm

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
19 11/2018

20 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Get Your Medicare News Electronically
The Palmetto GBA Medicare listserv is a wonderful communication tool that offers its members the opportunity to stay informed about:
• Medicare incentive programs • Fee Schedule changes• New legislation concerning Medicare • And so much more!
How to register to receive the Palmetto GBA Medicare Listserv:
Go to http://tinyurl.com/PalmettoGBAListserv and select “Register Now.” Complete and submit the online form. Be sure to select the specialties that interest you so information can be sent.
Note: Once the registration information is entered, you will receive a confirmation/welcome message informing you that you’ve been successfully added to our listserv. You must acknowledge this confirmation within three days of your registration.
Medicare Learning Network® (MLN)
Want to stay informed about the latest changes to the Medicare Program? Get connected with the Medicare Learning Network® (MLN) – the home for education, information, and resources for health care professionals.
The Medicare Learning Network® is a registered trademark of the Centers for Medicare & Medicaid Services (CMS) and the brand name for official CMS education and information for health care professionals. It provides educational products on Medicare-related topics, such as provider enrollment, preventive services, claims processing, provider compliance, and Medicare payment policies. MLN products are offered in a variety of formats, including training guides, articles, educational tools, booklets, fact sheets, web-based training courses (many of which offer continuing education credits) – all available to you free of charge!
The following items may be found on the CMS web page at:
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/index.html
• MLN Catalog: is a free interactive downloadable document that lists all MLN products by media for-mat. To access the catalog, scroll to the “Downloads” section and select “MLN Catalog.” Once you have opened the catalog, you may either click on the title of a product or you can click on the type of “For-mats Available.” This will link you to an online version of the product or the Product Ordering Page.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
21 11/2018
• MLN Product Ordering Page: allows you to order hard copy versions of various products. These prod-ucts are available to you for free. To access the MLN Product Ordering Page, scroll to the “Related Links” and select “MLN Product Ordering Page.”
• MLN Product of the Month: highlights a Medicare provider education product or set of products each month along with some teaching aids, such as crossword puzzles, to help you learn more while having fun!
Other resources:
• MLN Publications List: contains the electronic versions of the downloadable publications. These prod-ucts are available to you for free. To access the MLN Publications go to: https://www.cms.gov/Out-reach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/MLN-Publications.html. You will then be able to use the “Filter On” feature to search by topic or key word or you can sort by date, topic, title, or format.
MLN Educational Products Electronic Mailing ListTo stay up-to-date on the latest news about new and revised MLN products and services, subscribe to the MLN Educational Products electronic mailing list! This service is free of charge. Once you subscribe, you will receive an e-mail when new and revised MLN products are released.
Note: This article was revised on August 8, 2017, to reflect an updated Change Request (CR) 9859. In the article, the CR release date, transmittal numbers, and the Web address of the CR are revised. Also, a clarification was made on page 3 to denote that HBV is not separately payable for ESRD TOB 72X unless reported with modifier AY. Another bullet point was added on page 3 to show that contractor pricing applies to G0499 with dates of service September 28, 2016 through December 31, 2017. All other information is unchanged. To subscribe to the service:
1. Go to https://list.nih.gov/cgi-bin/wa.exe?A0=mln_education_products-l and select the ‘Subscribe or Unsubscribe’ link under the ‘Options’ tab on the right side of the page.
2. Follow the instructions to set up an account and start receiving updates immediately – it’s that easy!
If you would like to contact the MLN, please email CMS at [email protected].

22 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
HOSPITAL INFORMATION
Activation of Systematic Validation Edits for OPPS Providers with Multiple Service Locations
MLN Matters Number: SE18023 Article Release Date: October 12, 2018 Related CR Transmittal Numbers: R1704OTN and R1783OTN Related Change Request (CR) Number: 9613; 9907 Effective Date: N/A Implementation Date: N/A
Provider Types Affected This MLN Matters® Special Edition Article is intended for Outpatient Prospective Payment System (OPPS) providers that have multiple service locations submitting claims to Medicare A/B Medicare Administrative Contractors (MACs).
What You Need To Know This article conveys the activation of systematic validation edits for the enforcement of requirements in the Medicare Claims Processing Manual, Chapter 1, and Section 170 which describes Payment Bases for Institutional Claims. These requirements are not new requirements. Previously, these requirements were discussed in CRs 9613 and 9907, both of which were effective on January 1, 2017. MLN Matters articles for CRs 9613 and 9907 are available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM9613.pdf and https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM9907.pdf, respectively. Make sure your billing staff is aware of these instructions.
Background Increasingly, hospitals operate an off-campus, outpatient, provider-based department of a hospital. In some cases, these additional locations are in a different payment locality than the main provider. In order for Medicare Physician Fee Schedule (MPFS) and OPPS payments to be accurate, the service facility address of the off-campus, outpatient, provider-based department of a hospital facility is used to determine the locality in these cases.
Additionally, in accordance with Section 1833(t)(21) of the Social Security Act (the Act), as added by section 603 of the Bipartisan Budget Act of 2015 (Pub. L. 114-74), non-excepted services provided at an off-campus, outpatient, provider-based department of a hospital were required to be identified; as the payment rate for non-excepted items and services billed on an institutional claim are to be paid under the MPFS and not the OPPS rates.
Claim level information: Medicare outpatient service providers report the service facility location for an off-campus, outpatient, provider-based department of a hospital in the 2310E loop of the 837 institutional claim transaction. Direct Data Entry (DDE) submitters also are required to report the service facility location for an off-campus,

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
23 11/2018
outpatient, provider-based department of a hospital. Paper submitters report the service facility address information in Form Locator (FL) “01” on the paper claim form. For MPFS services, Medicare systems use this service facility information to determine the applicable payment method or locality whenever it is present.
Additionally, Medicare systems will validate service facility location to ensure services are being provided in a Medicare enrolled location. The validation will be exact matching based on the information submitted on the Form CMS-855A submitted by the provider and entered into the Provider Enrollment, Chain and Ownership System (PECOS). Providers need to ensure that the claims data matches their provider enrollment information.
When all the services rendered on the claim are from the billing provider address, providers are:
• To report the billing provider address only in the billing provider loop 2010AA and not to report any service facility location in loop 2310E (or in DDE MAP 171F screen for DDE submitters).
When all the services rendered on the claim are from one campus of a multi-campus provider that report a billing provider address, providers are:
• To report the campus address where the services were rendered in the service facility location in loop 2310E if the service facility address is different from the billing provider address loop 2010AA (or in DDE MAP 171F screen for DDE submitters).
When all the services rendered on the claim are from the same off-campus, outpatient, provider-based department of a hospital, providers are:
• To report the off-campus, outpatient, provider-based department service facility address in the service facility provider loop 2310E (or in DDE MAP 171F screen for DDE submitters).
When there are services rendered on the claim from multiple locations:
• If any services on the claim were rendered at the billing provider address, providers should report the billing provider address only in the billing provider loop 2010AA and do not report the service facility location in loop 2310E (or in DDE MAP 171F screen for DDE submitters).
• If no services on the claim were rendered at the billing provider address, providers should report the service facility address in loop 2310E (or in DDE MAP 171F screen for DDE submitters) from the first registered encounter of the “From” date on the claim.
NM1 - SERVICE FACILITY LOCATION NAME – 60 Characters 837I – 25, UB-04N3 - SERVICE FACILITY LOCATION ADDRESS
N301 – 55 Characters 837I – 25 Characters on the UB-04 N302 – 55 Characters 837I – not on UB-04 paper form

24 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
N4 - SERVICE FACILITY LOCATION CITY, STATE, ZIP CODE
N401 City Name – 30 Characters 837I – 12 Characters on the UB-04 N402 State Code – 2 Characters 837I – 2 Characters on the UB-04 N403 Postal Code – 15 Characters 837I – 9 Characters on the UB-04
DDE Screen MAP 171F:
Line level information: In the CY 2015 OPPS Final Rule (79 FR 66910-66914), the Centers for Medicare & Medicaid Services (CMS) created a HCPCS modifier for hospital claims that is to be reported with each claim line with a HCPCS for outpatient hospital items and services furnished in an off-campus provider-based department (PBD) of a hospital. This 2-digit modifier was added to the HCPCS annual file as of January 1, 2015, with the label ‘‘PO.’’ Reporting of this new modifier was voluntary for CY 2015, with reporting required beginning on January 1, 2016. In accordance with Section 1833(t)(21) of the Act, as added by section 603 of the Bipartisan Budget Act of 2015 (Pub. L. 114-74), CMS established a new modifier “PN” (Non-excepted service provided at an off-campus, outpatient, provider-based department of a hospital) to identify and pay non-excepted items and services billed on an institutional claim. Effective January 1, 2017, non-excepted off-campus provider-based departments of a hospital are required to report this modifier on each claim line with a HCPCS for non-excepted items and services. The use of modifier “PN” will trigger a payment rate under the MPFS. CMS expects the PN modifier to be reported with each non-excepted line item and service including those for which payment will not be adjusted, such as separately payable drugs, clinical laboratory tests, and therapy services; with reporting required beginning on January 1, 2017.
As a result, effective January 1, 2017, excepted off-campus provider-based departments of a hospital must continue to report existing modifier “PO” (Services, procedures and/or surgeries provided at off-campus provider-based outpatient departments) for all excepted items for services reported with a HCPCS furnished.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
25 11/2018
National Testing
Round 1 Testing During the week of July 23 through July 30, 2018, CMS performed a national trial activation of the Fiscal Intermediary Shared System (FISS) Edits 34977 and 34978 in production environments. Reason Codes 34977 (claim service facility address doesn’t match provider practice file address) and 34978 (Off-campus provider claim line that contains a HCPCS must have a PN or PO) were activated. The testing was transparent to providers as most claims impacted by the test were suspended for one (1) billing cycle and then editing was turned off so the claim could continue processing as normal.
This national test brought to light that many providers are not sending the correct exact service facility location on the claim that produces an exact match with the Medicare enrolled location as based on the information entered into the PECOS for their off-campus provider departments.
Most discrepancies had to do with spelling variations. For example, in PECOS the word entered was “Road” as part of their address, but the provider entered “Rd” or “Rd.” as part of their address on the claim submission. Another example, in PECOS the word entered was “STE” as part of their address, but the provider entered “Suite” as part of their address on the claim submission.
Round 2 Testing Providers should also ensure that all practice locations are present in PECOS and if any locations are not in PECOS to submit the 855A to add the location(s). Providers can review their practice locations in PECOS and/or the confirmation letter from PECOS when they last enrolled that was received from their A/B MAC to ensure that their service facility address for their off-campus provider department locations provided on claims is an exact match.
CMS will conduct an additional national testing in November 2018. Providers should use the time before this national testing to correct the off-campus provider department location addresses within their billing systems to match exactly PECOS for their off-campus provider departments.
Full Production After the November national test in November 2018 has been completed, CMS will review the results. One suggestion given during our Round 1 Testing was to have the practice location addresses available in DDE so providers could query their own PECOS practice location addresses. This should greatly reduce uncertainty as to the exact information found in the PECOS file and make claim practice location address comparison more efficient. As a result CMS has issued instructions to the FISS maintainer to make the practice location address screen available to providers in DDE at the April 2019 system quarterly release. Starting in April 2019, the practice location screen will be available in DDE. Full production implementation has been postponed until such time. CMS will continue with additional round(s) of testing to ensure that we have a smooth implementation of the edits.
Once the April 2019 Quarterly release has been implemented, CMS will direct A/B MACs to permanently turn on the edits and set them up to Return-to-Provider (RTP) claims that do not exactly match. Providers can make corrections to their service facility address for a claim submitted in the DDE MAP 171F screen for

26 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
DDE submitters. Providers who need to add a new or correct an existing Practice location address will still need to submit a new 855A enrollment application in PECOS.
CMS expects that the 2 year time frame that the edits have not been active have provided ample time for providers to validate their claims submission system and the PECOS information for their off-campus provider departments are exact matches.
Additional Information If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description October 12, 2018 Initial article released.
Fiscal Year (FY) 2019 Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital (LTCH) PPS Changes
MLN Matters Number: MM10869 Related CR Release Date: October 4, 2018 Related CR Transmittal Number: R4144CP Related Change Request (CR) Number: 10869 Effective Date: October 1, 2018 Implementation Date: October 1, 2018
Provider Types Affected This MLN Matters® Article is intended for hospitals that submit claims to Medicare Administrative Contractors (MACs) for inpatient hospital services provided to Medicare beneficiaries by acute care and Long-Term Care Hospitals (LTCHs).
Provider Action Needed Change Request (CR) 10869 implements Fiscal Year (FY) 2019 policy changes for the Inpatient Prospective Payment System (IPPS) and LTCH PPS. Failure to adhere to these new policies could affect payment of Medicare claims. Make sure that your billing staffs are aware of these changes.
Background The Social Security Amendments of 1983 (P.L. 98-21) provided for establishment of a PPS for Medicare payment of inpatient hospital services. In addition, the Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act of 1999 (BBRA), as amended by the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA), required Medicare to implement a budget neutral, per discharge PPS for LTCHs based on Diagnosis-Related Groups (DRGs) for cost reporting periods beginning on or after October 1, 2002. The Centers for Medicare & Medicaid Services (CMS makes updates to these prospective payment systems annually. CR10869 outlines those changes for FY 2019.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
27 11/2018
IPPS FY 2019 Update The following list of policy changes for FY 2019 were displayed in the Federal Register on August 2, 2018, with a publication date of August 17, 2018, and in the corresponding correction document published on October 3, 2018 in the Federal Register. The Federal Register and CR10869 covers all items in more depth and are effective for hospital discharges occurring on or after October 1, 2018, through September 30, 2019, unless otherwise noted. New IPPS and LTCH PPS Pricer software packages were released prior to October 1, 2018, that include updated rates that are effective for claims with discharges occurring on or after October 1, 2018, through September 30, 2019. The MACs installed the new revised Pricer programs timely to ensure accurate payments for IPPS and LTCH PPS claims.
Files for download listed throughout CR10869 are available on the CMS website. MACs used the following links for files for download and hospitals may find this information helpful:
• FY 2019 Final Rule Tables webpage: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2019-IPPS-Final-Rule-Home-Page-Items/FY2019-IPPS-Final-Rule-Tables.html
• FY 2019 Final Rule Data Files webpage: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2019-IPPS-Final-Rule-Home-Page-Items/FY2019-IPPS-Final-Rule-Data-Files.html
• MAC Implementation Files webpage: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2019-IPPS-Final-Rule-Home-Page-Items/FY-2019-MAC-Implementation-Files.html
Alternatively, the files on the webpages listed above are also available on the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Click on the link on the left side of the screen titled, “FY 2019 IPPS Final Rule Home Page” or the link titled “Acute InpatientFiles for Download” (and select ‘Files for FY 2019 Final Rule and Correction Notice’).
IPPS FY 2019 Update
A. FY 2019 IPPS Rates and Factors For the Operating Rates/Standardized Amounts and the Federal Capital Rate, refer to Tables 1A-C and Table 1D, respectively, of the FY 2019 IPPS/LTCH PPS Final Rule, available on the FY 2019 Final Rule Tables webpage. For other IPPS factors, including applicable percentage increase, budget neutrality factors, High Cost Outlier (HCO) threshold, and Cost-of-Living Adjustment (COLA) factors, refer to MAC Implementation Files 1 available on the FY 2019 MAC Implementation Files webpage.
B. Medicare Severity -Diagnosis Related Group (MS-DRG) Grouper and Medicare Code Editor (MCE) Changes The Grouper Contractor, 3M Health Information Systems (3M-HIS), developed the new International Classification of Diseases Tenth Edition (ICD-10) MS-DRG Grouper, Version 36.0, software package effective for discharges on or after October 1, 2018. The GROUPER assigns each case into a MS-DRG on

28 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
the basis of the reported diagnosis and procedure codes and demographic information (that is age, sex, and discharge status). The ICD-10 MCE Version 36.0, which is also developed by 3M-HIS, uses edits for the ICD-10 codes reported to validate correct coding on claims for discharges on or after October 1, 2018.
For discharges occurring on or after October 1, 2018, the Fiscal Intermediary Shared System (FISS) calls the appropriate GROUPER based on discharge date
For discharges occurring on or after October 1, 2018, the MCE selects the proper internal code edit tables based on discharge date. Note that the MCE version continues to match the Grouper version. CMS increased the number of MS-DRGs from 754 to 761 for FY 2019. CMS is implementing 18 new MSDRGs for FY 2019 and deleting 11 MS-DRGs.
FY 2019 New MS-DRGs
• MS-DRG 783 Cesarean Section with Sterilization with MCC
• MS-DRG 784 Cesarean Section with Sterilization with CC
• MS-DRG 785 Cesarean Section with Sterilization without CC/MCC
• MS-DRG 786 Cesarean Section without Sterilization with MCC
• MS-DRG 787 Cesarean Section without Sterilization with CC
• MS-DRG 788 Cesarean Section without Sterilization without CC/MCC
• MS-DRG 796 Vaginal Delivery with Sterilization/D&C with MCC
• MS-DRG 797 Vaginal Delivery with Sterilization/D&C with CC
• MS-DRG 798 Vaginal Delivery with Sterilization/D&C without CC/MCC
• MS-DRG 805 Vaginal Delivery without Sterilization/D&C with MCC
• MS-DRG 806 Vaginal Delivery without Sterilization/D&C with CC
• MS-DRG 807 Vaginal Delivery without Sterilization/D&C without CC/MCC
• MS-DRG 817 Other Antepartum Diagnoses with O.R. Procedure with MCC
• MS-DRG 818 Other Antepartum Diagnoses with O.R. Procedure with CC
• MS-DRG 819 Other Antepartum Diagnoses with O.R. Procedure without CC/MCC
• MS-DRG 831 Other Antepartum Diagnoses without O.R. Procedure with MCC
• MS-DRG 832 Other Antepartum Diagnoses without O.R. Procedure with CC
• MS-DRG 833 Other Antepartum Diagnoses without O.R. Procedure without CC/MCC

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
29 11/2018
FY 2019 Deleted MS-DRGs
• MS-DRG 685 Admit for Renal Dialysis
• MS-DRG 765 Cesarean Section with CC/MCC
• MS-DRG 766 Cesarean Section without CC/MCC
• MS-DRG 767 Vaginal Delivery with Sterilization and/or D&C
• MS-DRG 774 Vaginal Delivery with Complicating Diagnosis
• MS-DRG 775 Vaginal Delivery without Complicating Diagnosis
• MS-DRG 777 Ectopic Pregnancy
• MS-DRG 778 Threatened Abortion
• MS-DRG 780 False Labor
• MS-DRG 781 Other Antepartum Diagnoses with Medical Complications
• MS-DRG 782 Other Antepartum Diagnoses without Medical Complications
CMS revised the titles to the following MS-DRGs for FY 2019:
MS-DRG Revised Title Descriptions for FY2019
• MS-DRG 11 Tracheostomy For Face, Mouth & Neck Diagnoses Or Laryngectomy With MCC
• MS-DRG 12 Tracheostomy For Face, Mouth & Neck Diagnoses Or Laryngectomy With CC
• MS-DRG 13 Tracheostomy For Face, Mouth & Neck Diagnoses Or Laryngectomy Without CC/MCC
• MS-DRG 16 Autologous Bone Marrow Transplant With CC/MCC Or T-Cell Immunotherapy
• MS-DRG 864 Fever And Inflammatory Conditions
• MS-DRG 207 Respiratory System Diagnosis With Ventilator Support>96 Hours Or Peripheral Extracorporeal Membrane Oxygenation (ECMO)
• MS-DRG 291 Heart Failure & Shock With MCC Or Peripheral Extracorporeal Membrane Oxygenation (ECMO)
• MS-DRG 296 Cardiac arrest, unexplained w MCC Or Peripheral Extracorporeal Membrane Oxygenation (ECMO)
• MS-DRG 870 Septicemia Or Severe Sepsis With MV >96 Hours Or Peripheral Extracorporeal Membrane Oxygenation (ECMO)

30 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
See the ICD-10 MS-DRG V36.0 Definitions Manual Table of Contents and the Definitions of Medicare Code Edits V36 manual at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html for the complete list of FY 2019 ICD-10 MS-DRGs and Medicare Code Edits.
C. Post-acute Transfer and Special Payment Policy The changes to MS-DRGs for FY 2019 have been evaluated against the general post-acute care transfer policy criteria using the FY 2017 MedPAR data according to the regulations under Sec. 412.4(c). As a result of this review no new MS-DRGs will be added to the list of MS-DRGs subject to the post-acute care transfer policy. However, MS-DRGs 023 (Craniotomy with Major Device Implant or Acute CNS Principal Diagnosis with MCC or Chemotherapy Implant or Epilepsy with Neurostimulator) and 024 (Craniotomy with Major Device Implant or Acute Complex CNS Principal Diagnosis without MCC or Chemotherapy Implant or Epilepsy with Neurostimulator) were added to the special payment policy list.
See Table 5 of the FY 2019 IPPS/LTCH PPS Final Rule for a listing of all Post-acute and Special Post-acute MS-DRGs available on the FY 2019 Final Rule Tables.
CMS notes that implementation of the inclusion of discharges to hospice care as a post-acute care transfer subject to the payment adjustments beginning in FY 2019, as required by Section 53109 of the Bipartisan Budget Act of 2018, was addressed in Change Request 10602 (Transmittal 2094; June 20, 2018).
D. New Technology Add-On The following items will continue to be eligible for new-technology add-on payments in FY 2019:
1. Name of Approved New Technology: Defitelio®
• Maximum Add-on Payment: $80,500 (Note, this amount has been updated for FY 2019)
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW03392 or XW04392
2. Name of Approved New Technology: ZINPLAVA™
• Maximum Add-on Payment: $1,900
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW033A3 or XW043A3
3. Name of Approved New Technology: Stelara®
• Maximum Add-on Payment: $2,400
• Identify and make new technology add-on payments with ICD-10-PCS procedure code: XW033F3

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
31 11/2018
The following items are eligible for new-technology add-on payments in FY 2019: 1. Name of Approved New Technology: VYXEOS™
• Maximum Add-on Payment: $36,425
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW033B3 or XW043B3
2. Name of Approved New Technology: Remedē® System
• Maximum Add-on Payment: $17,250
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: 0JH60DZ and 05H33MZ in combination with procedure code: 05H03MZ or 05H43MZ
3. Name of Approved New Technology: GIAPREZA™
• Maximum Add-on Payment: $1,500
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW033H4 or XW043H4
4. Name of Approved New Technology: AndexXa™
• Maximum Add-on Payment: $14,062.50
• Identify and make new technology
5. Name of Approved New Technology: Sentinel® Cerebral Protection System™
• Maximum Add-on Payment: $1,400
• Identify and make new technology add-on payments with ICD-10-PCS procedure code: X2A5312
6. Name of Approved New Technology: Aquabeam®
• Maximum Add-on Payment: $1,250
• Identify and make new technology add-on payments with ICD-10-PCS procedure code: XV508A4
7. Name of Approved New Technology: VABOMERE™
• Maximum Add-on Payment: $5,544
• Identify and make new technology add-on payments with an NDC of 70842012001 or 65293000901 (VABOMERE™ Meropenem-Vaborbactam Vial)

32 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
8. Name of Approved New Technology: ZEMDRI™ (Plazomicin)
• Maximum Add-on Payment: $2,722.50
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW033G4 or XW043G4
9. Name of Approved New Technology: Kymriah®/Yescarta®
• Maximum Add-on Payment: $186,500
• Identify and make new technology add-on payments with ICD-10-PCS procedure codes: XW033C3 or XW043C3
E. Cost of Living Adjustment (COLA) Update for IPPS PPS There are no changes to the COLA factors for FY 2019. For reference, a table showing the applicable COLAs that are effective for discharges occurring on or after October 1, 2018, is available in the FY 2019 IPPS/LTCH PPS final rule and in MAC Implementation File 1 available on the FY 2019 MAC Implementation Files webpage.
F. Wage Index Changes and Issues
1. New CBSA In OMB Bulletin No. 17–01, OMB announced that one Micropolitan Statistical Area now qualifies as a Metropolitan Statistical Area. As discussed in the FY 2019 final rule, effective for FY 2019 new urban CBSA is as follows:
• Twin Falls, Idaho (CBSA 46300). This CBSA is comprised of the principal city of Twin Falls, Idaho in Jerome County, Idaho and Twin Falls County, Idaho.
2. Section 505 Hospitals (Out-Commuting Adjustment) Section 505 of the Medicare Modernization Act of 2003 (MMA), also known as the “outmigration adjustment,” is an adjustment that is based primarily on commuting patterns and is available to hospitals that are not reclassified by the Medicare Geographic Classification Review Board (MGCRB), reclassified as a rural hospital under § 412.103, or redesignated under Section 1886(d)(8)(B) of the Act.
G. Treatment of Certain Providers Redesignated Under Section 1886(d)(8)(B) of the Act and Certain Urban Hospitals Reclassified as Rural Hospitals Under Section 412.103 42 CFR 412.64(b)(3)(ii) implements Section 1886(d)(8)(B) of the Act, which redesignates certain rural counties adjacent to one or more urban areas as urban for the purposes of payment under the IPPS. (These counties are commonly referred to as “Lugar counties”.) Accordingly, hospitals located in Lugar counties are deemed to be located in an urban area and their IPPS payments are determined based upon the urban area to which they are redesignated. A hospital that waives its Lugar status in order to receive the out-migration adjustment has effectively waived its deemed urban status and is considered rural for all IPPS purposes. The list of hospitals that have waived Lugar status for FY 2019 is available on the FY 2019 MAC Implementation File webpage.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
33 11/2018
An urban hospital that reclassifies as a rural hospital under § 412.103 is considered rural for all IPPS purposes. Note, hospitals reclassified as rural under § 412.103 are not eligible for the capital Disproportionate Share Hospitals (DSH) adjustment since these hospitals are considered rural under the capital PPS (see § 412.320(a)(1)).
H. Multicampus Hospitals
1. Wage Index
Beginning with the FY 2008 wage index, CMS instituted a policy that allocates the wages and hours to the CBSA in which a hospital campus is located when a multi-campus hospital has campuses located in different CBSAs. Medicare payment to a hospital is based on the geographic location of the hospital facility at which the discharge occurred. Therefore, if a hospital has a campus or campuses in different CBSAs, the MAC adds a suffix to the CCN of the hospital in the Provider Specific File (PSF), to identify and denote a sub-campus in a different CBSA, so that the appropriate wage index associated with each campus’s geographic location can be assigned and used for payment for Medicare discharges from each respective campus. Also, note that, under certain circumstances, it is permissible for individual campuses to have reclassifications to another CBSA, in which case, the appropriate reclassified CBSA and wage index is noted in the PSF. In general, subordinate campuses are subject to the same rules regarding withdrawals and cancellations of reclassifications as main providers.
2. Qualification for Certain Special Statuses
In the FY 2019 Final rule, CMS codified its current policies regarding how multi-campus hospitals may qualify for special status as a Sole-Community Hospital (SCH), Rural Referral Center (RRC), Medicare-Dependent Hospital (MDH), and rural reclassification under § 412.103.
Specifically, the main campus of a hospital cannot obtain a SCH, RRC, or MDH status or rural reclassification independently or separately from its remote location(s), and vice versa. Rather, the hospital (the main campus and its remote location(s)) are granted the special treatment or rural reclassification as one entity if the criteria are met. To meet the criteria, combined data from the main campus and its remote location(s) are used where the regulations at § 412.92 for SCH, § 412.96 for RRC, § 412.103 for rural reclassification, and § 412.108 for MDH require data, such as bed count, number of discharges, or case-mix index, for example. Where the regulations require data that cannot be combined, specifically qualifying criteria related to location, mileage, travel time, and distance requirements, the hospital needs to demonstrate that the main campus and its remote location(s) each independently satisfy those requirements in order for the entire hospital, including its remote location(s), to be reclassified as rural or obtain a special status.
I. Updating the PSF for Wage Index, Reclassifications and Redesignations MACs will update the PSF by following the steps, in order, in Attachment 1 of CR10869 to determine the appropriate wage index and other payments.

34 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
J. Hospital Specific (HSP) Rate Factors for Sole Community Hospitals (SCHs) and Medicare-Dependent, Small Rural Hospital (MDH) Program For FY 2019, MACs must update the Hospital-Specific (HSP) amount in the PSF for all SCHs and MDHs. The HSP amount must be updated from FY 2012 dollars to FY 2018 dollars by applying an update factor of 1.04058 to the current HSP amount in the PSF before entering this final amount in the PSF with an effective date of 10/1/2018. The factor of 1.04058 represents the product of all of the annual market basket updates (that is, applicable percentage increases), the DRG budget neutrality factors for FYs 2012 through 2018, and the cumulative documentation and coding adjustment factor for FYs 2011 through 2014 of 0.9480. PRICER will apply the update and DRG budget neutrality factor to the HSP amount for FY 2019.
K. Low-Volume Hospitals – Criteria and Payment Adjustments for FY2019 Section 50204 of the Bipartisan Budget Act of 2018 (Pub. L. 115–123) modified the definition of a lowvolume hospital and modified the methodology for determining the payment adjustment for hospitals meeting that definition. Specifically, Section 50204 amended the qualifying criteria for lowvolume hospitals to specify that, for FYs 2019 through 2022, a subsection (d) hospital qualifies as a low-volume hospital if it is more than 15 road miles from another subsection (d) hospital and has less than 3,800 total discharges during the fiscal year. Section 50204 also amended the statute to provides that, for discharges occurring in FYs 2019 through 2022, the Secretary shall determine the applicable percentage increase using a continuous, linear sliding scale ranging from an additional 25 percent payment adjustment for hospitals with 500 or fewer discharges to 0 percent additional payment for hospitals with more than 3,800 total discharges in the fiscal year. A hospital’s total discharges, which includes Medicare and non-Medicare discharges, is based on the hospital’s most recently submitted cost report. The regulations implementing the hospital payment adjustment policy are at section 412.101.
For FY 2019, a hospital must make a written request for low-volume hospital status that is received by its MAC no later than September 1, 2018, in order for the applicable low-volume payment adjustment to be applied to payments for its discharges beginning on or after October 1, 2018 (through September 30, 2019). Under this procedure, a hospital that qualified for the low-volume hospital payment adjustment for FY 2018 may continue to receive a low-volume hospital payment adjustment for FY 2019 without reapplying if it meets both the discharge criterion and the mileage criterion applicable for FY 2019. As in previous years, such a hospital had to send written verification that was received by its MAC no later than September 1, 2018, stating that it meets the mileage criterion applicable for FY 2019. If a hospital’s request for low-volume hospital status for FY 2019 was received after September 1, 2018, and if the MAC determines the hospital meets the criteria to qualify as a low-volume hospital, the MAC will apply the applicable low-volume hospital payment adjustment to determine the payment for the hospital’s FY 2019 discharges, effective prospectively within 30 days of the date of the MAC’s low-volume hospital status determination.
For FY 2019, for each qualifying hospital, MACs must determine the low-volume hospital payment adjustment using the hospital’s total discharges in its most recently submitted cost report as of the time of the MAC’s low-volume hospital status determination as follows:
• For hospitals with 500 or fewer total discharges, the adjustment is an additional 25 percent for each Medicare discharge.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
35 11/2018
• For hospitals with 501 and fewer than 3,800 total discharges, the adjustment for each Medicare discharge is an additional percent calculated using the formula: (95 / 330) – (number of total discharges / 13,200)
As noted above, “number of total discharges” includes Medicare and non-Medicare discharges and based on the hospital’s most recently submitted cost report at the time of the hospital’s low-volume hospital payment adjustment request.
L. Hospital Quality Initiative The hospitals that will receive the quality initiative bonus are listed at the following Web site: www.qualitynet.org. Should a provider later be determined to have met the criteria after publication of this list, they will be added to the Web site. A list of hospitals that will receive the statutory reduction to the annual payment update for FY 2019 under the Hospital IQR Program is available in MAC Implementation File 3 available on the FY 2019 MAC Implementation Files webpage.
M. Hospital Acquired Condition Reduction Program (HAC) The Hospital-Acquired Conditions (HAC) Reduction Program requires the Secretary of Health and Human Services (HHS) to adjust payments to hospitals that rank in the worst-performing 25 percent of all subsection (d) hospitals with respect to HAC quality measures. Hospitals with a Total HAC Score greater than the 75th percentile of all Total HAC Scores (that is, the worst-performing quartile) will be subject to a 1 percent payment reduction. This payment adjustment applies to all Medicare discharges for that fiscal year.
CMS did not make the list of providers subject to the HAC Reduction Program for FY 2019 public in the final rule because hospitals had until August 2018 to notify CMS of any errors in the calculation of their Total HAC Score under the Scoring Calculations Review and Corrections period. Updated hospital level data for the HAC Reduction Program will be made publicly available on the Hospital Compare website following the review and corrections process in January 2019.
N. Hospital Value Based Purchasing (VBP) For FY 2019 CMS will implement the base operating MS-DRG payment amount reduction and the value-based incentive payment adjustments, as a single value-based incentive payment adjustment factor applied to claims for discharges occurring in FY 2019. CMS expects to post the final value-based incentive payment adjustment factors for FY 2019 in the near future in Table 16B of the FY 2019 IPPS/LTCH PPS final rule (which will be available through the Internet on the FY 2019 IPPS/LTCH PPS Final Rule Tables webpage.
O. Hospital Readmissions Reduction Program (HRRP) CMS expects to post the HRRP payment adjustment factors for FY 2019 in Table 15 of the FY 2019 IPPS/LTCH PPS final rule (which are available on the FY 2019 IPPS Final Rule Tables webpage). Hospitals that are not subject to a reduction under the HRRP in FY 2019 (such as Maryland hospitals), have a readmission adjustment factor of 1.0000. For FY 2019, hospitals should only have a readmission adjustment factor between 1.0000 and 0.9700.

36 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
P. Medicare Disproportionate Share Hospitals (DSH) Program Section 3133 of the Affordable Care Act modified the Medicare DSH program beginning in FY 2014. Under current law, hospitals received 25 percent of the amount they previously would have received under the current statutory formula for Medicare DSH. The remainder, equal to 75 percent of what otherwise would have been paid as Medicare DSH, will become an uncompensated care payment after the amount is reduced for changes in the percentage of individuals that are uninsured. Each Medicare DSH hospital will receive a portion of the aggregate amount available for uncompensated care payments based on its share of total uncompensated care reported by Medicare DSH hospitals.
The Medicare DSH payment is reduced to 25 percent of the amount they previously would have received under the current statutory formula in PRICER. The calculation of the Medicare DSH payment adjustment will remain unchanged and the 75 percent reduction to the DSH payment is applied in PRICER.
The total uncompensated care payment amount to be paid to Medicare DSH hospitals was finalized in the FY 2019 IPPS Final Rule, and the uncompensated care payment will continue to be paid on the claim as an estimated per discharge amount to the hospitals that have been projected to receive Medicare DSH for FY 2019. The Uncompensated Care Per Discharge Amount and Projected DSH Eligibility are located in the Medicare DSH Supplemental Data File for FY 2019, which are available on the FY 2019 Final Rule Data Files webpage.
For FY 2019, new hospitals with a CCN established after October 1, 2015 that are eligible for Medicare DSH will have their Factor 3 calculated at cost report settlement using uncompensated care costs reported on Line 30 of Worksheet S-10 as the numerator and a denominator of $30,210,112,106. Factor 3 is then applied to the total uncompensated care payment amount finalized in the FY 2019 IPPS Final Rule to determine the total amount to be paid to the hospital. If a new hospital has a CCR on line 1 of Worksheet S-10 in excess of 0.93, MACs will contact b for further instructions on how to calculate the uncompensated care costs for the numerator. MACs can refer to the Medicare DSH Supplemental Data File on the CMS website to confirm whether a hospital should be treated as new. CMS notes it is possible that there are additional new hospitals during FY 2019 and therefore those would not be listed on the Medicare DSH Supplemental Date File. In the case of a new hospital in Puerto Rico, the hospital’s Factor 3 would need to be calculated by the MAC based on cost report’s Medicaid days, which may need to be annualized, plus 14% for SSI proxy, and then divided by denominator of 37,539,919.
Q. Recalled Devices A hospital’s IPPS payment is reduced, for specified MS-DRGs when the implantation of a device is replaced without cost or with a credit equal to 50 percent or more of the cost of the replacement device. New MS-DRGs are added to the list subject to the policy for payment under the IPPS for replaced devices offered without cost or with a credit when they are formed from procedures previously assigned to MS- DRGs that were already on the list. There are no new MS-DRGs for FY 2019 subject to the policy for replaced devices offered without cost or with a credit.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
37 11/2018
LTCH PPS FY 2019 Update
A. FY 2019 LTCH PPS Rates and Factors The FY 2019 LTCH PPS Standard Federal Rates are located in Table 1E available on the FY 2019 Final Rule Tables webpage. Other FY 2019 LTCH PPS Factors are available in MAC Implementation File 2 on the FY 2019 MAC Implementation File webpage.
The LTCH PPS Pricer is updated with the Version 36.0 MS-LTC-DRG table, weights and factors, effective for discharges occurring on or after October 1, 2018, and on or before September 30, 2019.
B. Application of the Site Neutral Payment Rate Section 1886(m)(6) of the Act establishes patient-level criteria for payments under the LTCH PPS for cost reporting periods beginning on or after October 1, 2015. LTCH discharges that do not meet the patient-level criteria are paid the site neutral payment rate. The application of the site neutral payment rate is codified in the regulations at § 412.522.
The statute originally established a transitional blended payment rate for site neutral payment rate LTCH discharges occurring in cost reporting periods beginning during FY 2016 or FY 2017, which was extended by subsequent legislation to cost reporting periods beginning during FY 2018 and FY 2019. The blended payment rate is comprised of 50 percent of the site neutral payment rate for the discharge and 50 percent of the LTCH PPS standard Federal payment rate that would have applied to the discharge. This transitional blended payment rate for site neutral rate LTCH discharges is included in the Pricer logic.
Under Section 51005 of the Bipartisan Budget Act of 2018 (Pub. L. 115-123), the IPPS comparable amount under the site neutral payment rate is reduced by 4.6 percent for FYs 2018 through 2026. This adjustment is included in the Pricer logic.
The temporary exception to the site neutral payment rate for certain severe wound discharges from certain LTCHs expires for cost reporting periods that begin on or after October 1, 2018.
C. The 25-Percent Threshold Policy CMS eliminated the 25-percent threshold policy in the FY 2019 IPPS/LTCH PPS final rule, effective October 1, 2018. Accordingly, the regulations describing the 25-percent threshold policy at Section 412.538 have been removed and reserved.
D. LTCH Quality Reporting (LTCHQR) Program Under the Long-Term Care Hospital Quality Reporting (LTCHQR) Program, for FY 2019, the annual update to a standard Federal rate will continue to be reduced by 2.0 percentage points if a LTCH does not submit quality-reporting data in accordance with the LTCHQR Program for that year.
E. Provider Specific File (PSF) The PSF required fields for all provider types, which require a PSF are available in Pub. 100-04, Medicare Claims Processing Manual, Chapter 3, §20.2.3.1 and Addendum A.

38 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
In OMB Bulletin No. 17–01, OMB announced that one Micropolitan Statistical Area now qualifies as a Metropolitan Statistical Area. As discussed in the FY 2019 final rule, effective for FY 2019 new urban CBSA is as follows:
• Twin Falls, Idaho (CBSA 46300). This CBSA is comprised of the principal city of Twin Falls, Idaho in Jerome County, Idaho and Twin Falls County, Idaho
Table 8C contains the FY 2019 Statewide average LTCH total Cost-to-Charge Ratios (CCRs) for urban and rural LTCHs. Table 8C is available on the FY 2019 Final Rule Tables webpage. Per the regulations in 42 CFR Sections 412.525(a)(4)(iv)(C) and 412.529(f)(4)(iii), for FY 2019, Statewide average CCRs are used in the following instances:
1. New hospitals that have not yet submitted their first Medicare cost report. (For this purpose, a new hospital is defined as an entity that has not accepted assignment of an existing hospital’s provider agreement in accordance with 42 CFR Section 489.18).
2. LTCHs with a total CCR is in excess of 1.280 (referred to as the total CCR ceiling).
3. Any hospital for which data to calculate a CCR is not available.
NOTE: Hospitals and/or MACs can request an alternative CCR to the statewide average CCR per the instructions in Section 150.24 of Chapter 3 of Pub. 100-04, Medicare Claims Processing Manual.
F. Cost of Living Adjustment (COLA) under the LTCH PPS There are no updates to the COLAs for FY 2019. The COLAs effective for discharges occurring on or after October 1, 2018 are available in the FY 2019 IPPS/LTCH PPS final rule and are also located in MAC Implementation File 2 available on the FY 2019 MAC Implementation Files webpage. (Note that the same COLA factors are used under the IPPS and the LTCH PPS for FY 2019.)
G. Discharge Payment Percentage Beginning with LTCHs’ FY 2016 cost reporting periods, the statute requires LTCHs to be notified of their “Discharge Payment Percentage” (DPP), which is the ratio (expressed as a percentage) of the LTCHs’ FFS discharges which received LTCH PPS standard Federal rate payment to the LTCHs’ total number of LTCH PPS discharges. MACs shall continue to provide notification to the LTCH of its DPP upon final settlement of the cost report.
Hospitals Excluded from the IPPS
The update to extended neoplastic disease care hospital’s target amount is the applicable annual rate-of-increase percentage specified in § 413.40(c)(3), which is equal to the percentage increase projected by the hospital market basket index. In the FY 2019 IPS/LTCH PPS final rule, CMS established an update to an extended neoplastic disease care hospital’s target amount for FY 2018 of 2.9 percent.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
39 11/2018
Additional Information The official instruction, CR10869, issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4144CP.pdf. If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description October 11, 2018 Initial article released.
INFLUENZA VACCINE INFORMATION
2018-2019 Influenza (Flu) Resources for Health Care Professionals
MLN Matters Number: SE18015 Article Release Date: September 24, 2018 Related CR Transmittal Number: N/A Related Change Request (CR) Number: N/A Effective Date: N/A Implementation Date: N/A Provider Types Affected All health care professionals who order, refer, or provide flu vaccines and vaccine administration to Medicare beneficiaries and submit bills for these services to Medicare Administrative Contractors (MACs). Provider Action Needed Special Edition (SE) MLN Matters article SE18015 provides information about influenza (flu) resources for health care professionals and providers relevant to the 2018-2019 flu season. Health care professionals should:
• Keep this article and refer to it throughout the 2018-2019 flu season.
• Take advantage of each office visit as an opportunity to encourage patients to protect themselves from the flu and serious complications by getting a flu shot.
• Continue to provide the flu shot if you have vaccine available, even after the new year.
• Remember to immunize yourself and your staff.

40 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Background The Centers for Medicare & Medicaid Services (CMS) reminds health care professionals that Medicare Part B reimburses health care providers for flu vaccines and their administration (Medicare provides coverage of the flu vaccine without any out-of-pocket costs to the Medicare patient. No deductible or copayment/coinsurance applies).
You can help your Medicare patients reduce their risk for contracting seasonal flu and serious complications by using every office visit as an opportunity to recommend they take advantage of Medicare’s coverage of the annual flu shot. As a reminder, please help prevent the spread of the flu by immunizing yourself and your staff! Know What to Do About the Flu!
Payment Rates for 2018-2019 Each year, CMS updates the Medicare Healthcare Common Procedure Coding System (HCPCS) and Current Procedure Terminology (CPT) codes and payment rates for personal flu and pneumococcal vaccines. Payment allowance limits for such vaccines are 95 percent of the Average Wholesale Price (AWP), except where the vaccine is furnished in a hospital outpatient department, Rural Health Clinic (RHC), or Federally Qualified Health Center (FQHC). In these cases, the payment for the vaccine is based on reasonable cost. Annual Part B deductible and coinsurance amounts do not apply. All physicians, non-physician practitioners, and suppliers who administer the influenza virus vaccination and the pneumococcal vaccination must take assignment on the claim for the vaccine. The following table contains the applicable Medicare Part B payment allowances for HCPCS and CPT codes:
Code Labeler Name Drug Name Payment Allowance
Effective Date
90653 Seqirus Inc Fluad (2018/2019) $54.673 08/01/2018 – 07/31/2019
90656 Seqirus Inc Afluria (2018/2019) $19.773 08/01/2018 – 07/31/2019
90662 Sanofi Pasteur Fluzone High-Dose (2018/2019)
$53.373 08/01/2018 – 07/31/2019
90674 Seqirus Inc Flucelvax Quadrivalent (2018/2019)
$24.047 08/01/2018 – 07/31/2019
90682 Sanofi Pasteur Flublok Quadrivalent (2018/2019)
$53.373 08/01/2018 – 07/31/2019
90685 Sanofi Pasteur Fluzone Quadrivalent Pediatric (2018/2019)
$21.813 08/01/2018 – 07/31/2019

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
41 11/2018
90686 Seqirus Inc, GlaxoSmithKline, Sanofi Pasteur
Afluria Quadrivalent (2018/2019), Fluarix Quadrivalent (2018/2019), Flulaval Quadrivalent (2018/2019), Fluzone Quadrivalent (2018/2019) [Preservative Free]
$19.032 08/01/2018 – 07/31/2019
90687 Sanofi Pasteur Fluzone Quadrivalent Pediatric (2018/2019)
$9.403 08/01/2018 – 07/31/2019
90688 Seqirus Inc, GlaxoSmithKline, Sanofi Pasteur
Afluria Quadrivalent (2018/2019), Flulaval Quadrivalent (2018/2019), Fluzone Quadrivalent (2018/2019)
$17.835 08/01/2018 – 07/31/2019
90756 Seqirus Inc Flucelvax Quadrivalent (2018/2019)
$22.793 08/01/2018 – 07/31/2019
Q2035 Seqirus Inc Afluria (2018/2019) $18.236 08/01/2018 – 07/31/2019
Payment allowance information is still pending as of the date of this article for other CPT and HCPCS codes. Once payment allowances are available, CMS will post them at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/VaccinesPricing.html. For 2018/2019, there is a new CPT code (90689), for which the applicable Dates of Service (DOS) are January 1, 2019, through July 31, 2019. The payment rate for 90689 is pending. The new influenza virus vaccine code 90689 is not retroactive to August 1, 2018. No claims will be accepted for influenza virus vaccine code 90689 for DOS between August 1, 2018, through December 31, 2018. If MACs receive claims with code 90689 for DOS between August 1, 2018, and December 31, 2018, MACs will follow their normal course of action for codes billed prior to their effective date. Providers are encouraged to review MM10871 (“Quarterly Influenza Virus Vaccine Code Update – January 2019”) for more information about 90689, available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM10871.pdf. Background on influenza vaccine payment allowances is in MM10914, available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM10914.pdf.
Note: MACs will reprocess any previously processed and paid claims for the current flu season that were paid using influenza vaccine payment allowances other than the allowanced published in the influenza vaccine pricing website for the 2018/2019 season that began on August 1, 2018. This reprocessing should occur by November 1, 2018.

42 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Additional Information If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list. Educational Products for Health Care Professionals The Medicare Learning Network® (MLN) has developed a variety of educational resources to help you understand Medicare guidelines for seasonal flu vaccines and their administration.
1. MLN Influenza Related Products for Health Care Professionals
• Medicare Part B Immunization Billing: Seasonal Influenza Virus, Pneumococcal, And Hepatitis B educational tool - http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/qr_immun_bill.pdf
• Medicare Preventive Services educational tool - https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/medicare-preventive-services/MPS-QuickReferenceChart-1.html
• Mass Immunizers And Roster Billing For Influenza Virus And Pneumococcal Vaccinations booklet - https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Mass_Immunize_Roster_Bill_factsheet_ICN907275.pdf
2. Other CMS Resources • Provider Resources webpage - https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/ProviderResources.html
• Immunizations webpage - https://www.cms.gov/Medicare/Prevention/Immunizations/Overview.html
• Prevention Services webpage - http://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/index.html
• Medicare Benefit Policy Manual - Chapter 15, Section 50.4.4.2 – Immunizations http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c15.pdf
• Medicare Claims Processing Manual - Chapter 18, Preventive and Screening Services http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c18.pdf
3. Other Resources The following non-CMS resources are useful information and tools for the 2018 – 2019 flu season: • Advisory Committee on Immunization Practices - http://www.cdc.gov/vaccines/acip/index.html
• Centers for Disease Control and Prevention - http://www.cdc.gov/flu
• Flu.gov - http://www.flu.gov
• Food and Drug Administration - http://www.fda.gov
• Immunization Action Coalition - http://www.immunize.org

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
43 11/2018
• Indian Health Services - http://www.ihs.gov • National Alliance for Hispanic Health - http://www.hispanichealth.org
• National Foundation For Infectious Diseases - http://www.nfid.org/influenza
• National Library of Medicine and NIH Medline Plus - http://www.nlm.nih.gov/medlineplus/immunization.html
• National Vaccine Program - http://www.hhs.gov/nvpo
• Office of Disease Prevention and Health Promotion - http://healthfinder.gov/FindServices/Organizations/Organization/HR2013/office-of-disease-prevention-and-health-promotion-us-department-of-health-and-human-services
• World Health Organization - http://www.who.int/en
Document History
Date of Change Description September 24, 2018 Initial article released.
LEARNING AND EDUCATION INFORMATION
Home Health Referrals and Clinical Documentation Requirements Webinar: November 28, 2018
Your Part A/B, Home Health Railroad MACs are excited to announce this webinar collaboration. If you order home health services, this webinar is a great way to assure you are aware of physician roles and Medicare’s coverage criteria! Topics will include an overview of coverage for home health services, billing opportunities, common documentation errors seen as well as resources. There will be time for questions after the presentation portion of the webinar
For more information about this workshop session and registration instructions select the link below:
https://register.gotowebinar.com/register/7854333118335561729

44 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Quarterly Updates Webcast: December 12, 2018
Palmetto GBA will host the Medicare Administrative Contractor Part A Quarterly Updates, Changes and Reminders Webcast at 10 a.m. to 11 a.m. ET on Wednesday, December 12, 2018.
This 60-minute Webcast is designed to provide pertinent updates, changes and reminders to assist the provider community in staying compliant with Medicare rules and regulations and will include:
• Any new billing regulations
• Hot topics that impact provider billing
To register for this Webcast go to: https://event.on24.com/wcc/r/1561133/AD6B4C240C9A70E4221709E2828FE799
Note: An NPI and PTAN are required to register. You should only enter ‘n/a’ if you do not have an NPI or PTAN.
Educational Events Where You Can Ask Questions and Get Answers from Palmetto GBA
Don’t Miss this Wonderful Opportunity!If you are in search of an opportunity to interact with and get answers to your Medicare billing, coverage and documentation questions from Palmetto GBA’s Provider Outreach and Education (POE) department, please see these educational offerings which have a question and answer session:
To acesss the following information, go to: https://www.palmettogba.com/palmetto/providers.nsf/DocsCat/JM-Part-A~AH2JQQ2870
Quarterly Ask the Contractor Teleconferences (ACTs)
ACTs are intended to open the communication channels between providers and Palmetto GBA, which allows for timely identification of problems and information-sharing in an informal and interactive atmosphere. These teleconferences will be held at least quarterly via teleconference.
Preceding the presentation, providers are given an opportunity to ask questions both on the topics discussed as well as any other question they may have. While we encourage providers to submit questions prior to the call, this is not required. Just fill out the Ask the Contractor Teleconference (ACT): Submit A Question form). Once the form is completed, please fax it to (803) 935-0140, Attention: Ask-the-Contractor Teleconference

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
45 11/2018
Quarterly Updates Webcasts The Quarterly Update Webcasts are intended to provide ongoing, scheduled opportunities for providers to stay up to date on Medicare requirements.
Providers are able to type a question and have it responded to by the POE department throughout the webcast. At the end of the presentation the moderator will also read and respond to questions submitted by attendees in order to share the responses with the group at large.
Event Registration Portal Visit our Event Registration Portal to find information on upcoming educational events and seminars.
This is a complete listing of both our face-to-face outreach opportunities as well as our teleconference and webcast listings. Providers are able to dialogue with POE and get answers to their questions at all of these educational events.
If you have a question that you need an answer to today or a claims specific question which requires the disclosure of PII or PHI for response, please contact the Provider Contact Center (PCC) at 1-855-696-0705.
MEDICAL POLICY INFORMATION
Changes to the Laboratory National Coverage Determination (NCD) Edit Software for January 2019
MLN Matters Number: MM10941 Related CR Release Date: September 28, 2018 Related CR Transmittal Number: R4139CP Related Change Request (CR) Number: 10941 Effective Date: January 1, 2019 Implementation Date: January 7, 2019
Provider Type Affected This MLN Matters Article is intended for physicians, other providers, and suppliers submitting claims to Medicare Administrative Contractors (MACs) for services provided to Medicare beneficiaries.
Provider Action Needed This MLN Matters® Article is based on Change Request (CR) 10941 which informs MACs about the changes that will be included in the January 2019 quarterly release of the edit module for clinical diagnostic laboratory services. Make sure your billing staffs are aware of these changes.
Background CR 10941 announces the changes that will be included in the January 2019 quarterly release of the edit module for clinical diagnostic laboratory services. The National Coverage Determinations (NCDs) for clinical diagnostic laboratory services were developed by the laboratory negotiated rulemaking committee,

46 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
and the final rule was published on November 23, 2001. Nationally uniform software was developed and incorporated in the Medicare shared systems so that laboratory claims subject to one of the 23 NCDs (Publication 100-03, Sections 190.12 - 190.34) were processed uniformly throughout the nation, effective April 1, 2003.
In accordance with Chapter 16, Section 120.2, Publication 100-04, the laboratory edit module is updated quarterly as necessary to reflect ministerial coding updates and substantive changes to the NCDs developed through the NCD process. The changes are a result of coding analysis decisions developed under the procedures for maintenance of codes in the negotiated NCDs and biannual updates of the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes. CR 10941 communicates requirements to MACs notifying them of changes to the laboratory edit module to update it for changes in laboratory NCD code lists for January 2019.
Please access the following link for the NCD spreadsheets included with CR10941 (https://www.cms.gov/medicare/coverage/determinationprocess/downloads/January2019.zip)
Note: MACs will adjust claims brought to their attention, but will not search their files to retract payment for claims already paid or retroactively pay claims.
Additional Information The official instruction, CR10941, issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4139CP.pdf.
If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description September 28, 2018 Initial article released.
Local Coverage Determinations (LCDs)
MLN Matters Number: MM10901 Related CR Release Date: October 3, 2018 Related CR Transmittal Number: R829PI Related Change Request (CR) Number: 10901 Effective Date: October 3, 2018 Implementation Date: January 8, 2019
Provider Types Affected This MLN Matters Article is intended for physicians, providers, and suppliers billing Medicare Administrative Contractors (MACs) for services provided to Medicare beneficiaries.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
47 11/2018
Provider Action Needed Change Request (CR) 10901 notifies MACs that, in accordance with Section 4009 of H.R. 34-21st Century Cures Act (Public Law No: 114-255), the Centers for Medicare & Medicaid Services (CMS) is updating the Medicare Program Integrity Manual with detailed changes to the Local Coverage Determination (LCD) process. You should ensure that your staffs are aware of these changes.
Background Through feedback received in the proposed Calendar Year (CY) 2018 Physician Fee Schedule (PFS) Rule (82 FR 33950), and through meetings and correspondence; stakeholders, including providers and healthcare associations, have provided CMS with valuable insight regarding modernization of the LCD process.
Most stakeholders acknowledged that the local coverage process is an important means to provide decisions related to the items and services that benefit Medicare’s beneficiaries and to ensure beneficiary access to life saving and medically necessary products and procedures. However, there is concern about the lack of local coverage process transparency, including notifying stakeholders of proposed revisions to, and drafting of, new LCDs.
Additional stakeholder concerns include: ineffective MAC processes for soliciting from, and providing to, stakeholders feedback on information provided during open public meetings, a lack of non-physician representation on Contractor Advisory Committees (CACs), and concerns that CAC meetings are not open to the public.
In CR10901, the revisions to the Medicare Program Integrity Manual, Chapter 13, CMS is revising instructions to MACs, reflecting policy process changes in response to the new statutory (21st century Cures Act) requirements and to the stakeholder comments. These changes will help to increase transparency, clarity, consistency, reduce provider burden and enhance public relations while retaining the ability to be responsive to local clinical and coverage policy concerns.
The 2016 21st Century Cures Act included changes to the LCD process, adding language to 1862(l)(5)(D) of the Social Security Act (the Act) to describe the LCD process. Section 1862(l)(5)(D), of the Act requires each MAC that develops an LCD to make available on their Internet website on the Medicare website, at least 45 days before the effective date of such determination, the following information:
• Such determination in its entirety
• Where and when the proposed determination was first made public
• Hyperlinks to the proposed determination and a response to comments submitted to the MAC with respect to such proposed determination
• A summary of evidence that was considered by the contractor during the development of such determination and a list of the sources of such evidence
• An explanation of the rationale that supports such determination

48 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
CMS revamped the format of the manual so that it could be used as a roadmap to understand the steps of the local coverage process, which enable stakeholders to effectively engage in the process. This transparency also carries through to the reconsideration process, which is a process by which stakeholders can request a MAC take a second look at an existing decision using evidence that has developed since its first review.
The manual also sets forth consistent requirements for communication to providers and other stakeholders to occur at predictable milestones so anyone with an interest in the local policy can stay informed as the policy moves through the process.
New LCD Process The key parts of the New LCD Process are summarized as follows:
1. The New LCD Process may begin with informal meetings in which interested parties within the MAC’s jurisdiction can discuss potential LCD requests. These educational meetings, which are not required, can be held either in person, using web-based technologies, or via teleconference, which allow discussions before requestors submit a formal request.
2. New LCD Requests
The New LCD Request Process is a mechanism through which interested parties within a MAC’s jurisdiction can request a new LCD. In this process, MACs will consider all new LCD requests from:
• Beneficiaries residing or receiving care in the MAC’s jurisdiction
• Health care professionals doing business in the MAC’s jurisdiction
• Any interested party doing business in the MAC’s jurisdiction
MACs will consider a New LCD Request to be a complete, formal request if the following requirements are met. The request:
• Is in writing and is sent to the MAC via e-mail, facsimile or written letter
• Clearly identifies the statutorily-defined Medicare benefit category to which the requestor believes the item or service applies
• Identifies the language that the requestor wants in an LCD
• Includes a justification supported by peer-reviewed evidence (full copies of published evidence must be included or the request is not valid) • Addresses relevance, usefulness, clinical health outcomes, or the medical benefits of the item or service
• Fully explains the design, purpose, and/or method, as appropriate, of using the item or service for which the request is made.
Within 60 calendar days of the day they receive the request; MACs will review the materials and determine whether the request is complete or incomplete. If the request is complete, the MAC will follow the New LCD Process, as described in the revised manual. If, however, the process is incomplete, they will respond, in writing, to the requestor explaining why the request was incomplete.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
49 11/2018
3. Clinical Guidelines, Consensus Documents and Consultation
During an LCD’s development, MACs should (when applicable and available) supplement their research with clinical guidelines, consensus documents, or consultation by experts (recognized authorities in the field), medical associations or other health care professionals for an advisory opinion. They will summarize the opinions they receive as a result of this consultation with healthcare professional expert(s), professional societies, and others prior to the drafting of a proposed or final LCD, and include this information in the proposed or final LCD. Note that acceptance by individual health care providers, or even a limited group of health care providers, does not indicate general acceptance of the item or service by the medical community.
4. Publication of the Proposed LCD
The public announcement of a MAC’s proposed determination begins with the date the proposed LCD is published on the Medicare Coverage Database (MCD) at https://www.cms.gov/medicare-coverage-database/overview-and-quick-search.aspx. Once the proposed LCD is published, MACs will provide a minimum of 45 calendar days for public comment, and will contact the CMS if they determine an extension to the comment period is needed.
These processes shall be used for all LCDs except in the following situations:
• Revised LCD Being Issued for Compelling Reasons.
• Revised LCD that Makes a Non-Substantive Correction - For example, typographical or grammatical errors that do not substantially change the LCD.
• Revised LCD that Makes a Non-discretionary Coverage Update - Contractors shall update LCDs to reflect changes in NCDs or when a conflict with national policy occurs, coverage provisions in interpretive manuals, and payment systems.
• Revise LCD to effectuate an Administrative Law Judge’s decision to nullify an existing LCD due to an LCD Challenge.
5. Contractor Advisory Committee (CAC)
The CAC is to be composed of healthcare professionals, beneficiary representatives, and representatives of medical organizations; and is used to supplement the MAC’s internal expertise, and to ensure an unbiased and contemporary consideration of “state of the art” technology and science. Additionally, all CAC meetings will be open to the public to attend and observe.
MACs will establish one CAC per state or one per jurisdiction with representation from each state, ensuring that each state has a full committee and the opportunity to discuss the quality of evidence used to make a determination.
The CAC’s purpose is to provide a formal mechanism for healthcare professionals to be informed of the evidence used in developing the LCD and promote communications between the MACs and the healthcare community. The CAC is advisory in nature, with the final decision on all issues resting with MACs.

50 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
6. Open Meeting
After the proposed LCD is made public, MACs will hold open meetings to discuss the review of the evidence and the rationale for the proposed LCD(s) with stakeholders in their jurisdiction. Interested parties (generally those that would be affected by the LCD, including providers, physicians, vendors, manufacturers, beneficiaries, caregivers, etc.) can make presentations of information related to the proposed LCDs. Members of the CAC may also attend these open meetings. MACs must notify the public about the dates and location for the open meeting. MACs have the option of setting up email listservs to announce this information or may use other education methods to adequately inform the public. The listserv or other method should clearly identify the location, dates and telephone/video/on-line conference information for the open meeting to ensure that this information is clearly distinguished from the information for the CAC meetings.
7. Publication of the Final Determination
After the close of the comment period and the required meetings and consultation, the final LCD and the Response to Comment (RTC) Article will be published on the MCD.
8. Response to Public Comments
MACs will respond to all comments received during the comment period of the proposed LCD by using the RTC article associated with the LCD. The RTC Article is published on the start date of the notice period. The RTC Article will remain publicly available indefinitely on the MCD or the MCD Archive.
9. Notice Period
The date the final LCD is published on the MCD, marks the beginning of the required notice period of at least 45 calendar days before the LCD can take effect. If the notice period is not extended by the MAC, the effective date of the LCD is the 46th calendar day after the notice period began.
Full details of this new process are contained in the updated manual which is an attachment to CR10901. LCD Reconsideration Process The LCD reconsideration process is a mechanism by which a beneficiary or stakeholder (including a medical professional society or physician) in the MAC’s jurisdiction can request a revision to an LCD. The LCD reconsideration process differs from an initial request for an LCD in that it is available only for final effective LCDs. The whole LCD or any provision of the LCD may be reconsidered. In addition, MACs have the discretion to revise or retire their LCDs at any time on their own initiative. This process is summarized as follows:
1. MACs shall consider all LCD reconsideration requests from:
• Beneficiaries residing or receiving care in a contractor’s jurisdiction
• Providers doing business in a contractor’s jurisdiction
• Any interested party doing business in a contractor’s jurisdiction

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
51 11/2018
2. MACs should only accept reconsideration requests for LCDs published as an effective final. Requests shall not be accepted for other documents including:
• National Coverage Determinations (NCDs);
• Coverage provisions in interpretive manuals;
• Proposed LCDs;
• Template LCDs, unless or until they are adopted and in effect by the contractor;
• Retired LCDs;
• Individual claim determinations
• Bulletins, articles, training materials; and
• Any instance in which no LCD exists, i.e., requests for development of an LCD.
3. Process Requirements - The requestor shall submit a valid LCD reconsideration request to the appropriate MAC, following instructions on the MAC’s Web site. Within 60 calendar days of the day the request is received, the MAC shall determine whether the request is valid or invalid. If the request is invalid, the MAC will respond, in writing, to the requestor explaining why the request was invalid. If the request is valid, the MAC will open the LCD and follow the LCD process as outlined in the above for new LCDs or include the LCD on the MAC’s waiting list. The MAC shall respond, in writing, to the requestor notifying the requestor of the acceptance, and if applicable, wait-listing, of the reconsideration request.
Other Important Changes Other key changes to the manual include the following:
• MACs shall finalize or retire all proposed LCDs within one calendar year of publication date on the MCD.
• Upon further notice from CMS, it will no longer be appropriate to routinely include Current Procedure Terminology (CPT) codes or International Classification of Diseases-Tenth Revision-Clinical Modification (ICD-10-CM) codes in the LCDs. All codes will be removed from LCDs and placed in billing & coding articles that are linked to the LCD.
Additional Information The official instruction, CR10901, issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R829PI.pdf. The complete manual revision is included in CR10901.
If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.

52 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
As part of the CMS commitment to continuous improvement, CMS invites interested stakeholders to submit feedback on their experience with the revised LCD process. CMS will collect feedback via submissions to [email protected] and consider additional revisions based on stakeholder feedback.
Document History
Date of Change Description October 3, 2018 Initial article released.
Part A Local Coverage Determinations (LCDs) Updates
Revised ICD-10 LCDsThe table below provides a summary of recent Part A/B MAC ICD-10 LCD revisions/updates. To view these revised LCDs, go to www.PalmettoGBA.com/jja/lcd. Under the Medical Policies section, select Active LCD Policies. Scroll down to the LCDs for Contractor Browser section and make sure the Active LCDs category is selected. Then select the Submit button. The LCDs are listed in alphabetical order.
TitleLCD NumberRevision Number
Changes/Additions/Deletions Effective Date
Nerve Conduction Studies and ElectromyographyLCD Number: L35048Revision Number: 20
Under ICD-10 Codes that Support Medical Necessity Group 1: Codes the following ICD-10 codes have been added: G71.09, M79.11, M79.12, M79.18. Under ICD-10 Codes that Support Medical Necessity Group 2: Codes the following ICD-10 codes have been deleted: G71.09, M79.11, M79.12, M79.18.
10/01/2018
Partial Hospitalization Programs LCD Number: L37633Revision Number: 3
Revisions were made to the Partial Hospitalization Programs Local Coverage Determination (LCD) L37633. Under CPT/HCPCS Codes Group 1: Paragraph added the verbiage “The CPT®/HCPCS codes listed in Group 1: Codes describe covered services when performed in the context of partial hospitalization. It is outside of the scope of this LCD to list all circumstances where the services represented by CPT® codes 96116, 96118 and 96119 may be appropriately performed outside of the context of this LCD. Absence of a diagnosis code in this LCD for other conditions for which these evaluations may be medically necessary does not imply non-coverage in those circumstances.”
At this time 21st Century Cures Act will apply to new and revised LCDs that restrict coverage which requires comment and notice. This revision is not a restriction to the coverage determination; and, therefore not all the fields included on the LCD are applicable as noted in this policy.
10/08/2018

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
53 11/2018
Part A Local Coverage Determinations (LCDs) Article Updates
Revised ICD-10 LCD Article UpdatesThe table below provides a summary of a recent Part A MAC ICD-10 LCD article revision/updates. To view these revised LCD articles, go to www.PalmettoGBA.com/jma/lcd. In the Articles section select Coverage Articles. Under the Articles for Contractor Browser section, make sure the Active Articles category is selected and the click on the Submit button. The LCD articles are listed in alphabetical order.
TitleLCD Article ID NumberRevision Number
Changes/Additions/Deletions Effective Date
Billing Requirements for PET Scan Claims to Identify Bone Metastasis of CancerLCD Article Number: A54735Revision Number: 4
Under Article Text formatting was corrected throughout the Article. 10/11/2018
Part A/B Medicare Administrative Contractor (MAC) Local Coverage Determinations (LCDs) Updates
Revised ICD-10 LCDsThe table below provides a summary of recent Part A/B MAC ICD-10 LCD revisions/updates. To view these revised LCDs, go to www.PalmettoGBA.com/jja/lcd. Under the Medical Policies section, select Active LCD Policies. Scroll down to the LCDs for Contractor Browser section and make sure the Active LCDs category is selected. Then select the Submit button. The LCDs are listed in alphabetical order.
TitleLCD NumberRevision Number
Changes/Additions/Deletions Effective Date
Health and Behavior Assessment-InterventionLCD Number: L37638Revision Number: 4
ICD-10 codes referenced in Revision #3 were not added as new codes; they were broken out from the range F01.50 - F99. All ICD-10 codes that are no longer listed in the LCD under ICD-10 Codes that DO NOT Support Medical Necessity may be considered covered as of 9/13/18.
09/13/2018
Non-Covered Category III CPT CodesLCD Number: L34555Revision Number: 27
Under CPT/HCPCS Codes Group 1: Codes CPT code 0474T has been added. On August 29, 2018, the manufacturer of the CyPass device (0474T) announced an immediate, voluntary market withdrawal from the global market for patient safety reasons. Therefore, CPT code 0474T is non-covered.
Note: The revised LCD is being issued for compelling reasons; therefore, CMS has approved the expedited revision process.
09/27/2018

54 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Supervised Exercise Therapy for the Treatment of Peripheral Arterial Disease with Symptomatic Lower Extremity Intermittent ClaudicationLCD Number: L37774NEW
Under Coverage Indications, Limitations and/or Medical Necessity changed verbiage from “plan of care” to “medical record” in the fourth paragraph. Under Certifying medical necessity and referral to SET added the verbiage “The physician who signs the referral for PAD treatment may also be the physician supervising the treatment sessions” after the first sentence in the second paragraph. Under Assessing benefits and harms of each SET session changed the verbiage at the end of the sentence from “plan of care” to “SET protocol”, and added verbiage that reads “This assessment must reflect that the patient’s primary physician does not believe that the patient has an absolute contraindication to exercise. It should also reflect a consideration of how the plan will accommodate any contraindications to specific exercises the patient’s primary physician identifies. A non-exhaustive list of examples includes plans to mitigate risks to a beneficiary’s skin, heart rate parameters, or plans to protect the beneficiary’s bones and joints.” Under Frequency of treatment sessions changed verbiage from “unless there is compelling rational for different schedule” to “but the frequency of treatment may be tailored to the needs of the beneficiary so as to maintain or improve the risk to benefit profile of the treatment course for the beneficiary” at the end of the sentence. Under Components of treatment added the verbiage “Relevant evidence includes sources upon which a beneficiary’s treatment plan is based. Examples are not limited to but may include peer-reviewed studies or professional society recommendations” at the end of the third paragraph. Under Summary of Evidence added the verbiage “the Agency for Healthcare Research and Quality” in front of the acronym AHRQ in the third paragraph. Under Associated Information – Documentation Requirements changed the word “documentation” to the verbiage “referral, additional orders if present, and modifications to the treatment protocol if present” in the second sentence of the fourth statement. Under Bibliography changes were made to citations to reflect AMA citation guidelines. The citation date was changed from 2001 to 2011in the first reference. The verbiage “a collaborative report from the american association for vascular surgery/society for vascular surgery, society for cardiovascular angiography and interventions, society for vascular medicine and biology, society of interventional radiology, and the ACC/AHA task force on practice guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease: endorsed by the american association of cardiovascular and pulmonary rehabilitation; national heart, lung, and blood institute; society for vascular nursing; transatlantic inter-society consensus; and vascular disease foundation.“ was added to the title in the third reference. Formatting,
11/19/2018

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
55 11/2018
Supervised Exercise Therapy for the Treatment of Peripheral Arterial Disease with Symptomatic Lower Extremity Intermittent ClaudicationLCD Number: L37774NEWcontinued
dpunctuation and typographical errors were corrected throughout the policy. Acronyms were inserted where appropriate throughout the policy.
11/19/2018
Total Joint ArtroplastyLCD Number: L33456Revision Number:16
Under ICD-10 Codes that Support Medical Necessity Group: 2 Paragraph added CPT® code 27132.
09/13/2018
Response to Comments for the Supervised Exercise Therapy for the Treatment of Peripheral Arterial Disease with Symptomatic Lower Extremity Intermittent Claudication Local Coverage Determination (LCD) – LCD Number: DL37774
The comment period for the Supervised Exercise Therapy for the Treatment of Peripheral Arterial Disease with Symptomatic Lower Extremity Intermittent Claudication Local Coverage Determination (LCD) DL37774 began on June 4, 2018 and ended on July 19, 2018. The comments below were received from the provider community. The notice period for L37774 begins on October 4, 2018 and will become effective on November 19, 2018.
Comment 1: A number of commenters addressed the LCD text below: “Class I level of evidence A recommendations by the ACC/AHA are that SET be given at least 3 times per week to achieve maximal effectiveness (Hirsch 2006). As such SET sessions should generally be at least 3 times per week unless there is compelling rational for different schedules.”
They requested that the text of this statement be changed to recommend SET sessions 3 days per week but allow the frequency to be tailored to the needs of each beneficiary with some commenters raising the possibility of altering the treatment schedule based on matters of convenience to the beneficiary or to the treatment center.
Response 1: We agree with the commenters that the frequency should be tailored to meet the needs of the beneficiary. However, any tailoring of the treatment schedule must not come at the cost of providing a meaningful benefit to the patient.
For any particular course of supervised exercise therapy to be coverable by Medicare under law, it must be reasonable and necessary. For supervised exercise therapy in the treatment of symptomatic peripheral arterial disease, the evidence shows efficacy for a three times weekly or higher frequency treatment schedule, which has led to the ACC / AHA recommendation. It has been found that supervised exercise is an effective treatment for symptomatic peripheral arterial disease, whereas unsupervised exercise is not. A potential mechanism for supervised exercise therapy’s efficacy is thought to be related to compliance with a regular exercise program that is not found in unsupervised exercise therapy. Therefore, modification of

56 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
the schedule to a reduced frequency based on matters of convenience to the beneficiary or provider would not be expected to be equivalent to the three times weekly treatments that have been established to be reasonable and necessary.
As such these sessions should generally be at least three times per week, as the LCD text states, to have efficacy. Notably, the LCD’s current wording does not make at least three times per week sessions mandatory and does allow providers to modify the treatment schedule for compelling reasons.
To clarify the LCD, we will change the LCD text as follows:Class I level of evidence A recommendations by the ACC/AHA are that SET be given at least 3 times per week to achieve maximal effectiveness (Hirsch 2006). As such SET sessions should generally be at least 3 times per week, but the frequency of treatment may be tailored to the needs of the beneficiary so as to maintain or improve the risk to benefit profile of the treatment course for the beneficiary.
Comment 2: A number of commenters commented on the following text:“Every page of the record must be legible and include appropriate patient identification information (complete name, dates of service). The documentation must include the legible signature of the physician or non-physician practitioner responsible for and providing the care of the patient.”
Commenters agreed that daily documentation for each date of service needs to be legible and contain patient identification information as well as the name of the supervising physician. However, commenters raised concern regarding whether the LCD text indicates that the physician or the non-physician practitioner managing and caring for the patient needed to sign each daily treatment note.
Response 2: The LCD was not intended to require a physician or non-physician practitioner signature on each daily treatment note. Due to the confusion that the current LCD text may cause, we will modify the text to be clearer:
Every page of the record must be legible and include appropriate patient identification information (complete name, dates of service). The referral, additional orders if present, and modifications to the treatment protocol if present must include the legible signature of the physician or non-physician practitioner responsible for and providing the care of the patient.
Comment 3: One commenter raised a concern about the requirement for the supervising physician, PA, or NP to be trained in advanced life support and provide direct supervision, since these requirements will likely exclude many family practice physicians from referring a beneficiary to a qualified auxiliary provider for supervised exercise therapy.
Response 3: The requirements for coverage addressed by the commenter are requirements of NCD 20.35 regarding supervised exercise therapy for symptomatic peripheral arterial disease. The LCD indicates that this is the case in the following quote form the draft LCD text:
The NCD indicates that the beneficiary must be under the direct supervision of a physician, physician assistant, or nurse practitioner/clinical nurse specialist who must be trained in both basic and advanced life support techniques.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
57 11/2018
The specific wording in NCD 20.35 is:Effective for services performed on or after May 25, 2017, the Centers for Medicare & Medicaid Services has determined that the evidence is sufficient to cover SET for beneficiaries with IC for the treatment of symptomatic PAD. Up to 36 sessions over a 12-week period are covered if all of the following components of a SET program are met. The SET program must:…•be under the direct supervision of a physician (as defined in 1861(r)(1)), physician assistant, or nurse practitioner/clinical nurse specialist (as identified in 1861(aa)(5)) who must be trained in both basic and advanced life support techniques.
In summary, removal of this text from the LCD would not change the coverage requirements, since they would still be present in the NCD, and this text will be left in the LCD to remind providers of the requirement in the NCD.
Comment 4: One commenter questioned the requirements for the physician who is referring the patient to the supervised exercise therapy as noted in the following draft LCD text:
Beneficiaries must have a face-to-face visit with the physician responsible for PAD treatment to obtain the referral for SET.
The commenter recommended changing the wording to allow that the beneficiary’s face to face may also be with the physician supervising the exercise therapy itself
Response 4: The LCD is intended only to require that the treating physician with knowledge of the patient’s peripheral arterial disease and health conditions make the referral. We can understand how the current wording of the draft LCD may be interpreted as precluding a single physician from managing the patient’s peripheral arterial disease and overseeing the exercise. In acknowledgement of the fact that in certain instances the treating (referring) physician may in fact also be the supervising physician overseeing the patient’s exercise program, we will modify the LCD text as follows:
Beneficiaries must have a face-to-face visit with a physician who is responsible for PAD treatment to obtain the referral for SET. The physician who signs the referral for PAD treatment may also be the physician supervising the treatment sessions.
Comment 5: The LCD is intended only to require that the treating physician with knowledge of the patient’s peripheral arterial disease and health conditions make the referral. We can understand how the current wording of the draft LCD may be interpreted as precluding a single physician from managing the patient’s peripheral arterial disease and overseeing the exercise. In acknowledgement of the fact that in certain instances the treating (referring) physician may in fact also be the supervising physician overseeing the patient’s exercise program, we will modify the LCD text as follows:
Beneficiaries must have a face-to-face visit with a physician who is responsible for PAD treatment to obtain the referral for SET. The physician who signs the referral for PAD treatment may also be the physician supervising the treatment sessions.

58 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Response 5: While NCD does not mention a specific document referred to as a “plan of care,” the record must still reflect that the elements of the NCD required for coverage were met in order for the service to be reimbursable under Medicare. Since coverage under the NCD is contingent upon the delivery of supervised exercise therapy, the record must reflect that this service was indeed delivered as intended by the NCD.
The NCD’s publication followed from a national coverage analysis in which studies were reviewed to reach a coverage conclusion. The studies reviewed contained protocols, in some cases using this specific term, for the delivery of supervised exercise therapy. These protocols described a method for planning the course of exercise therapy spread over many sessions, with a common theme of advancing time and / or intensity of exercise as the subject progressed through the exercise therapy program. As such, Palmetto interprets the NCD to specifically refer to a planned course of exercise treatment in its use of the term “supervised exercise therapy.” The documentation must reflect that supervised exercise therapy is indeed the treatment that a beneficiary is receiving if Medicare is being billed for the service as supervised exercise therapy, and this would require that the record demonstrate the presence of a plan for exercise time and intensity over the anticipated course of therapy. The demonstration of this plan is what Palmetto GBA is referring to as a “plan of care.” This plan of care need not be a single document, but the record must reflect its presence, so as to establish that supervised exercise therapy within the scope of the NCD is the service being delivered.
Comment 6: One comment expressed appreciation that Palmetto GBA was addressing this issue with an LCD.
Response 6: We appreciate comments reflecting opinions both agreeing and disagreeing with our proposed coverage determination.
Comment 7: One comment did not object to or request a modification of the coverage conditions set forth in the LCD, but it expressed concern that reimbursement for this service may not be authorized for the necessary length of time.
Response 7: As per our LCD, treatment for a beneficiary may continue as long as there is a reasonable expectation that benefits will continue to exceed risks
Comment 8: One comment encouraged Palmetto GBA to include physical therapists as providers of supervised exercise for PAD.
Response 8: The NCD requires that supervised exercise therapy “be delivered by qualified auxiliary personnel necessary to ensure benefits exceed harms, and who are trained in exercise therapy for PAD.” Professional titles are neither necessary nor sufficient to meet the requirements of the NCD, though Palmetto GBA would expect that many physical therapists would meet these requirements.
Comment 9: One comment expressed a request that Palmetto GBA clarify in its LCD the criteria for determining whether a beneficiary had absolute contraindications to exercise.
Response 9: Per the NCD “SET is non-covered for beneficiaries with absolute contraindications to exercise as determined by their primary physician.” We do not see a meaningful way to clarify the NCD’s language further.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
59 11/2018
Comment 10: One comment requested that Palmetto GBA clarify the documentation requirements to meet the requirement that there be an assessment of benefits and harms.
Response 10: We appreciate the comment pointing out possible ambiguity, and we have clarified the draft LCD text to indicate what is meant by this statement. We have added the following text:
This assessment must reflect that the patient’s primary physician does not believe that the patient has an absolute contraindication to exercise. It should also reflect a consideration of how the plan will accommodate any contraindications to specific exercises the patient’s primary physician identifies. A non-exhaustive list of examples includes plans to mitigate risks to a beneficiary’s skin, heart rate parameters, or plans to protect the beneficiary’s bones and joints.
Comment 11: One comment requested that we remove the following text from the LCD since it is an additional requirement not given in the NCD and is vague and replace it with clearer language:
The auxiliary personnel delivering SET to a given beneficiary must be those providers whose scope of practice, keeping in mind all relevant national and local laws and regulations, includes making the assessments of benefit and risk included in the plan of care for that particular beneficiary.
Response 11: We are not certain where the commenter is concerned that confusion may arise, which hinders us from clarifying it in a meaningful way. Following LCD publication, if the commenter still has concerns about clarity, further information may be submitted to request reconsideration of this statement to make it clearer.
Comment 12: One comment expressed a disagreement with the NCD’s requirement that physical therapists have direct supervision from physicians, nurse practitioners, or physician assistants when providing supervised exercise therapy.
Comment 12: The disagreement is understood.
Comment 13: One comment noted appreciation that the LCD allows flexibility for the type of exercises being delivered but requested clarification of what would be deemed “relevant evidence.”
Response 13: We have modified the LCD text to further clarify what is expected of the evidence as follows:
Relevant evidence includes sources upon which a beneficiary’s treatment plan is based. Examples are not limited to but may include peer-reviewed studies or professional society recommendations.
Comment 14: One comment expressed disagreement with accepted places of service in which supervised exercise therapy may be delivered.
Response 14: The disagreement is understood.
Comment 15: One commenter noted a concern that the section of the LCD describing discharge from the supervised exercise therapy program is subject to provider misinterpretation and requested a clarification.

60 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Response 15: It is not clear to us specifically why this may be misinterpreted, which hinders us from revising the text to be clearer. Revisions to the LCD will be possible through the reconsideration process following publication if it appears that there is a misinterpretation hindering access to care.
MolDX Local Coverage Determinations (LCDs) Updates
Revised ICD-10 LCDsThe table below provides a summary of recent Part A MolDX ICD-10 LCD revisions/updates. To view these revised LCDs, go to www.palmettogba.com/moldx. Select MolDX LCDs under the Topics section. Go to your state and select Active. Scroll down to the Final LCDs for Contractor Results section and make sure the Active LCDs category is selected. Then select the Submit button. The LCDs are listed in alphabetical order.
TitleLCD NumberRevision Number
Changes/Additions/Deletions Effective Date
MolDX: Biomarkers in Cardiovascular Risk AssessmentLCD Number: L36129Revision Number: 12
The following ICD-10 codes were added to the ICD-10 Codes that Support Medical Necessity field: E78.41, E78.49, I63.81, I63.89, I67.858. These codes were inadvertently left out of the initial 2018 Annual ICD-10 Code Update revision (#11). This revision becomes effective 10/01/18.
10/01/2018
MolDX: Corus® CAD AssayLCD Number: L37612, Notice
The comment period for the MolDX: Corus® CAD Assay DL37612 began on 03/26/2018 and ended on 05/10/2018. Comments were received from the provider community. The notice period begins on 09/20/2018 and ends 11/04/2018. The LCD becomes final on 11/05/2018.
11/04/2018
MolDX: Genomic Health™ Oncotype DX® Prostate Cancer AssayLCD Number: L36153Revision Number: 13
Updated the NCCN reference in the LCD under Table 1 and in the Bibliography with the 2018 version.
10/01/2018
MolDX: NSCLC, Comprehensive Genomic Profile TestingLCD Number L36143Revision Number: 13
The release of a National Coverage Determination regarding the use of next generation sequencing in cancer has obviated the coverage decisions set forth in this LCD.
09/24/2018

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
61 11/2018
MolDX Local Coverage Determinations (LCDs) Article Updates Revised ICD-10 LCD Article UpdatesThe table below provides a summary of recent Part A MolDX ICD-10 LCD article revisions/updates. To view these revised LCD articles, go to www.palmettogba.com/moldx. Select MolDX LCDs under the Topics section. Go to your state and select Active. Scroll down to the Final LCDs for Contractor Results section and make sure the Active LCDs category is selected. Scroll down to the Associated Documents section and access the link. Then select the Submit button. The LCDs are listed in alphabetical order.
TitleLCD Article ID NumberRevision Number
Changes/Additions/Deletions Effective Date
MolDX: Afirma™ Assay by Veracyte UpdateLCD Number: A53098, Revision Number: 13
Added clarifying language to reimbursement conditions. 09/20/2018
Response to Comments for the MolDX: the MolDX: Corus® CAD Assay Local Coverage Determination (LCD) Article – LCD Number: DL37612
The comment period for the MolDX: Corus® CAD Assay DL37612 began on 03/26/2018 and ended on 05/10/2018. Comments were received from the provider community. The notice period begins on 09/20/2018 and ends 11/04/2018. The LCD becomes final on 11/05/2018.
Comment 1:A large number of comments that were received described a single clinician’s or a single institution’s anecdotal success with the Corus CAD test without providing specific utilization or outcome data or without an indication that these sources of experience were systematically tracking utilization and outcomes of patients who were or were not tested with the Corus CAD test. Commenters included practicing physicians, some of whom are speakers for CardioDX, and advanced practice nurses.
Response 1:This non-coverage policy is specifically based on the lack of evidence supporting clinical utility in the Medicare population.

62 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
While anecdotes of success may be the observable effect of meaningful clinical utility, such cases may also be isolated coincidences. Systematic tracking of patient characteristics, test results, and patient outcomes are the minimum necessary information to ascertain meaningful information regarding the clinical utility of a test.
Comment 2:Numerous providers reported an opinion that the Corus CAD test has good performance characteristics that allow them to confidently use it to stratify a patient’s risk of having coronary artery disease to either reassure the patient or recommend further diagnosis or treatment options. Some of these comments specifically cited research, which is also reviewed in the draft LCD.
Response 2:The draft LCD is non-covering the Corus CAD test specifically due to a lack of clinical utility of the test in the Medicare population. None of these commenters presented new data regarding clinical utility in the Medicare population or referenced a study demonstrating this. Clinical utility relates to changing the management of a patient in a way that is beneficial to the patient. While the commenters did discuss evidence supporting the diagnostic accuracy of the Corus CAD test, they did not bring to our attention any high quality research suggesting that the Corus CAD test could be used as an alternative to an existing test or that it identified high risk patients who were missed and led to a better long term outcome for stable coronary artery disease.
Comment 3:One physician raised the possibility of this test being used in the emergency room.
Response 3:The test has a turnaround time of a couple of days at least and therefore does not provide a timely result in patients with possible acute cardiac ischemia.
Comment 4:A representative from CardioDX sent the following comment:
Executive SummaryThe Corus CAD blood test incorporates age, sex, and gene expression to calculate a score reflecting a given symptomatic patient’s current likelihood of obstructive coronary artery disease (oCAD). The score ranges from 1-40, with higher scores associated with higher likelihood of obstructive disease. We believe that the Corus CAD test had demonstrated clinical utility and is medically necessary for the following reasons:
• Corus CAD provides an accurate measure of the current likelihood of CAD and has higher accuracy than other commonly used test modalities
• Corus CAD changes the pre-test probability for patients and provides incrementally actionable information that is not available from other sources
• Corus CAD is used by physicians to change diagnostic management, leading to fewer unnecessary procedures

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
63 11/2018
• Corus CAD is associated with lipid lowering agent initiation and adherence
• Corus CAD reduces the number of downstream procedures, which drives improved patient outcomes
As in indication of the growing acceptance of Corus CAD as a valuable tool in evaluation of symptomatic patients, the American Heart Association Scientific Statement on the Expressed Human Genome in July 2017 referred to Corus CAD as “valid and useful.” CardioDx has, under separate cover, submitted comments directly on the draft policy posted by Palmetto. We appreciate that the level of evidence expected today is different than it was when Corus CAD was launched in 2009. We have attempted to continually update our published evidence with 30 peer reviewed published articles and 70+ abstracts and presentations. As an organization, we strive to take a leadership position in the development and commercialization of clinically validated molecular diagnostics. As such, our organization is in the planning phases of a randomized control trial to further support the clinical utility of Corus CAD.
Conclusion: We have demonstrated clinical utility in the targeted patient population by showing that use of Corus CAD can reduce unnecessary cardiac testing without a negative impact on patient safety. We have demonstrated that low score Corus CAD patients are at low likelihood of experiencing a major adverse cardiac event or revascularization in long-term follow-up. The Corus CAD test changes the pre-test probability for patients compared to clinical factors. We believe this data is adequate to maintain Medicare coverage of Corus CAD.
Section 1. Clinical Utility of Corus CAD
• Target population: Patients with symptoms suggestive of obstructive coronary artery disease (oCAD) where the physician is considering wha action to take
• Clinical utility of Corus CAD is driven by:
• Corus CAD provides an accurate measure of the current likelihood o oCAD (data from: PREDICT, COMPASS, PROMISE)
• Corus CAD changes the pre-test probability for patients and provides information that is not available from other sources (PREDICT, COMPASS, PROMISE)
• Physicians use the likelihood from Corus CAD to change their further diagnostic management leading to fewer unnecessary procedures (IMPACT-CARD, IMPACT-PCP, PRESET) with benefit in vulnerabl population (PRESET ELDERLY)
• Corus CAD decreases the use of unnecessary downstream testin (COMPASS, IMPACT-PCP, PROMISE, IMPACT-CARD, PRESET)
• Corus CAD is associated with higher rates of starting lipid lowering agents and adherence on therapy

64 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Outlined below is a description of the published evidence to support the test performance and clinical utility of Corus CAD:
a. Corus CAD provides an accurate measure of the current likelihood of oCAD
In the COMPASS study, we demonstrated that Corus CAD has an AUC of 0.79, sensitivity of 89%, and negative predictive value of 96% when determining the current likelihood of obstructive coronary disease at a threshold of 15. Obstructive CAD was defined prospectively as ≥1 stenosis ≥50% in a major vessel based on a centralized reading quantitative coronary angiography or coronary computed tomography angiography. This level of stenosis was chosen as indication of oCAD in the COMPASS study because this level of stenosis represents a clinical finding in which either coronary artery stents or coronary artery bypass graft surgery would be clinically indicated.1
• The likelihood readout that is provided by Corus CAD outperforms existing methods of evaluating obstructive coronary artery disease likelihood
All Patients (n=431) Corus CAD MPI** P Value
Sensitivity 89% 36% P<0.001NPV 96% 88% P>0.001AUC 0.79 0.59 P>0.001Elderly Patients ≥ 65 Corus
CAD MPI P Value
Sensitivity 88% 21% P<0.05NPV 80% 74% P<0.05AUC 0.65 0.55 P=0.253
• Conclusion: Corus CAD provides an accurate measure of the likelihood of oCAD and has higher accuracy than myocardial perfusion imaging (MPI), the most commonly used test modality in the United States.
• Corus CAD changes the pre-test probability for patients and provides information that is not available from other sources
o In the COMPASS study, we calculated the pre-test probability of a patient having coronary artery disease using the clinical factors included in the Diamond-Forrester (D-F) score (Diamond and Forrester, N Engl J Med 1979) We are able to compare the pre-test probability from the D-F score to the Corus CAD probability and measure whether Corus CAD improves the pre-test probability of disease among symptomatic patients suspected of having oCAD.
We used the definition of obstructive coronary artery disease of a ≥50% stenosis in at least one major vessel from a centralized reading. In our previous work, we had seen that local readings of stenosis tended to be higher by approximately 15-20. We have three graphical representations of the improvement in pre-test probability that Corus CAD provides over the Diamond-Forrester. In the first figure, the mean probabilities and 95% confidence intervals are shown as an interval plot for all COMPASS patients and for elderly male COMPASS patients.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
65 11/2018
The referenced graphic could not be displayed in this report format.
• From the above, in patients without obstructive coronary artery disease, Corus CAD outperforms D-F by providing a lower estimate of disease probability compared to D-F.
• In the next set of figures, we highlight that Corus CAD provides a more accurate probability in the assessment of oCAD compared to D-F. For each patient in the COMPASS study without oCAD, we graphed for which patients Corus CAD was more accurate (lower probability) and for which patients D-F was more accurate and the magnitude of the difference in the pre-test probabilities. In the graphs below, we show that Corus CAD correctly lowered the pre-test probability in 275 patients, while Diamond-Forrester correctly lowered the pre-test probability in just 93 patients. For the elderly male population, Corus CAD correctly adjusted the pre-test probability in almost twice as many patients (17 v 9). In addition to the direction of change, one can see from the data that the Corus CAD test correctly shifted the pre-test probability at a greater magnitude than the shift from the Diamond-Forrester assessment.
The referenced graphics could not be displayed in this report format.Key to above graphs:
• The horizontal axis represents the individual patients in the analysis. Blue dots are male patients and red dots are female patients. All patients were clear of obstructive coronary artery disease as determined by invasive coronary angiography (ICA) or cardiac computed tomography angiography (CCTA)
• All patients above the horizontal dotted red line are patients that Corus CAD more accurately characterized (lower probability) than Diamond-Forester and all patients below the horizontal line are patients where Diamond-Forester had a more accurate (lower probability) than Corus CAD.
• The vertical distance from the horizontal red zero line represents the difference in probability between the Corus CAD score and the Diamond-Forrester score. The further away from the horizontal line, the greater the difference between the Corus CAD and Diamond-Forester scores.
• The improvement in pre-test probability that Corus CAD provides over D-F can also be seen in the graphs below. In this analysis we show the D-F and Corus CAD probabilities for all COMPASS patients and COMPASS elderly male patients with a given Corus CAD score. One can see that D-F more often overestimates the probability of disease when compared to Corus CAD. Overestimation of disease likelihood is associated with potentially unnecessary cardiac testing with its associated risks and costs. One can also see that there is wide variation in the D-F score for these patients without CAD.
The referenced graphics could not be displayed in this report format.Key to above graphs:
• The horizontal axis represents the Corus CAD score. Blue dots are Corus CAD probabilities and red dots are Diamond-Forrester probabilities. All patients were clear of obstructive coronary artery disease as determined by ICA or CCTA.
• The vertical access [sic] represents the probability of obstructive coronary disease

66 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Conclusion: Corus CAD improves the pre-test probability over clinical factors in both the overall population and the elderly male population.
• In the PROMISE study, we examined Corus CAD’s ability to provide information incremental to the standard of care of imaging (MPI or CCTA) in identifying patients likely to suffer a major cardiac event or revascularization. A common metric to show the incremental value of a new testing modality is the Net Reclassification Index (NRI)
o As both a dichotomous score and continuous score, Corus CAD provides significant reclassification benefit when compared to noninvasive imaging testing of MPI and CCTA in PROMISE
Net Reclassification Index in the PROMISEa Trial2
Overall NRI (95% Bootstrap CI)
Event NRI
Nonevent NRI
Corus CAD ( ≥ 15, >15) 43.2%(23.5% - 59.9%) 50.4% -7.3%
Corus CAD Continuous 41.1%(20.5% - 59.4%) 32.7% 8.4%
aVoora et al. PROMISE
We have not included the Net Reclassification data for elderly patients (65+ years old.), as the data is held by the PROMISE investigators.
• From the above table, one can see that Corus CAD correctly reclassified a meaningful percentage of the patients compared to MPI or CCTA imaging. This is significant because it again demonstrates that Corus CAD provides accurate information that is not available from other sources – in this case standard of care cardiac imaging. Corus CAD was able to provide a net reclassification (correct reclassifications minus incorrect reclassifications) in over 40% of the study participants, when used as either a dichotomous or continuous score.
• Another well-established methodology to determine if a diagnostic strategy is providing independent information is to conduct a multivariate analysis
o In PRESET, using multivariate analysis to isolate the independent effect of the Corus CAD score on the outcome of referral (to cardiology or to advanced cardiac testing), the Corus CAD score was significantly associated with this endpoint, both as a binary score as well as a continuous score. In the table below, patients with scores < 15 have an 82% decreased odds of referral than patients with scores > 15.
Low ASGES Score (>15)0.180.070.20<0.000Low ASGES Score (>15)0.180.070.070.20

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
67 11/2018
Referral to Cardiology or Advanced Cardiac Testing Multivariate AnalysisPredictor (or score) OR 95% CI p-value
Low ASGES Score (>15) 0.18 0.07 0.20 <0.000
Age > 65 years 2.02 1.20 3.39 0.008
Male 1.61 0.91 2.87 0.103
White Race 0.34 0.18 0.64 0.001
BMI >30 1.20 0.78 1.83 0.401
Current Smoker 1.53 0.89 2.61 0.120Hypertension 0.81 0.53 1.25 0.343Dyslipidemia 0.90 0.58 1.38 0.620Ladapo, et. al PRESET CardioDx understands Palmetto’s concern over referral rates as a metric of clinical utility. We will address that issue later in this response. Our intention in the analysis above is to show that the Corus CAD score has a larger impact on a physician’s decision to send a patient for further testing and evaluation than any of the typical clinical measures or risk factors.
Conclusion: Corus CAD provides incrementally actionable information that is not available from other sources
• Corus CAD is used by physicians to change diagnostic management, leading to fewer unnecessary procedures
o In the two IMPACT studies, we designed the studies to show change in physician behavior when the Corus CAD score was the one piece of additional clinical information added3. The IMPACT studies represent an additional way to demonstrate that the Corus CAD changed the pre-test probability of oCAD, as measured by change in the intensity of the diagnostic workup pre and post Corus CAD testing.
o In both studies, IMPACT-Card and IMPACT-PCP, the physicians changed behavior for more than 55% of the patients after these physicians had access to the Corus CAD score
o In addition to the level of behavior change, we also measured the direction of that change. We demonstrated in IMPACT-PCP that when the physicians changed their treatment plans, the physicians reduced the intensity of their treatment plan in 60% of the patients with scores ≤15 and increased the intensity in 39% of patients with scores >15. Similar results were seen in the IMPACT-CARD study.

68 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Score ClassTesting Intensity ≤ 15 >15 AllIMPACT-PCP Decreased 76 (60%>) 17 (14%) 93No Change 48 (38%) 58 (47%) 106Increased 3 (2%) 49 (39%) 52All 127 (100%) 124 (100%) 251 IMPACT-CARD Decreased 29 (56%) 3 (10%) 32No Change 23 (44%) 12 (39%) 35Inreased 0 (0%) 16 (51%) 16All 52 31 83
Change on testing Intensity: This change was prospectively defined as either a downgrade or upgrade in the intensity of the diagnostic plan based on the following categories (in hierarchical order): (1) no further cardiac testing or treatment, (2) lifestyle changes or medical therapy, (3) stress testing (with or without imaging) or computed tomography/coronary angiography, or (4) invasive coronary angiography. Data are n (%). P <.00001, exact test Herman, et. al IMPACT – PCP, McPherson, et. al IMPACT-CARD
• Both IMPACT studies asked physicians to document their intended treatment pathway both before and after receiving the Corus CAD score. We recorded those choices and analyzed both how often the pre and post Corus CAD pathways were different, and analyzed whether the change in patient management was more or less intensive.
o CardioDx understands that Palmetto has questioned the study design for both IMPACT studies. (Please see CardioDx’s comments to the draft policy provided under separate cover) Both IMPACT studies were designed to assess whether the use of the Corus CAD altered the clinicians’ decision-making, as defined by a change in patient management before and after receiving the Corus CAD score, while keeping all other diagnostic information constant. Both studies show that physicians change their behavior after receiving the Corus CAD score in over 55% of patients: generally a change of > 20% in an outcome is considered clinically relevant. (Cohen J. et. Al. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. Pp. 19–27.) The patient benefits from the fact that the physicians altered the intensity of their decision to better reflect the risk profile of that patient after learning of the Corus CAD score. In the IMPACT – PCP study, 76 patients (30% of all patients in the study) received less intensive follow-up because of the Corus CAD test. Thus the Corus CAD test decreased unnecessary testing by helping to identify patients unlikely to benefit from further non-invasive or invasive testing.
• In the most recent of our real world registry studies, PRESET, we show a consistent relationship between Corus CAD score and the decision to send the patient for further cardiac testing or evaluation. (Later in this document we discuss the use of referral rates as a proxy for patient outcomes.) Graphed below is the relationship between Corus CAD score and decision to send the patient to the either advanced testing or to cardiology for all patients and for elderly patients in the PRESET registry

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
69 11/2018
o It is important to note that the referral rate increases with Corus CAD score in a continuous fashion, in both the overall and elderly patient population.
The referenced graphic could not be displayed in this report format.
• The continuous relationship between Corus CAD score and referral rates is consistent when we look separately at elderly males and females
The referenced graphic could not be displayed in this report format.
• Furthermore, it is clear that there is a strong correlation between referral rate and increasing probability of obstructive CAD, including patients with higher scores such as elderly males. Patients at low current likelihood of disease as identified by the Corus CAD score were referred to the cardiologist or advanced testing at a low rate, as such patients were ruled out by the primary care physicians as they were unlikely to benefit from further testing.
The referenced graphic could not be displayed in this report format.Conclusion: Physicians use the likelihood from Corus CAD to change their further diagnostic management. That change is consistent with their revised post-test probability which leads to fewer unnecessary procedures. In the next section, we further demonstrate the reduction in testing from the use of Corus CAD.
• Corus CAD decreases the use of unnecessary downstream testing
• We have shown in two studies that Corus CAD reduces the use of downstream testing
o We In the IMPACT-CARD study, we included a historical control group to determine baseline referral rates demonstrated that the Corus CAD test can significantly reduce the amount of advanced testing performed, saving 45 patients (69-24) from further testing. Those 45 patients represent more than 50% of the patients in the study.
o Of the patients that were referred to the cardiac catheterization lab for an invasive coronary angiography, the yield of finding coronary artery disease was 3x higher (79% vs 25%) in the Corus CAD arm than in the historical control arm
o In IMPACT-CARD, when compared to a historical control group, the patients that received Corus CAD had less downstream testing (29% vs 83%)
‘ Sent for Additional
Testing4Yield at ICA (patients with detectable CAD)5
Corus CAD arm 29% (24/83) 79%(11/14)
Historical Control Arm 83% (69/83) 25% (4/16)

70 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
New analysis not previously seen by Palmetto – Reduction of testing in the COMPASS Study
• In the correspondence with Palmetto, CardioDx recognizes Palmetto’s assumption that clinical usage of Corus CAD was as a dichotomous score, such that all patients with scores ≤ 15 would not be sent for further evaluation given the low risk of oCAD. Similarly, we believe Palmetto’s assumptions was that all patients with scores > 15 would be sent for further testing and/or evaluation given their higher risk profile. We have provided data from multiple studies showing that actual clinical usage does not follow that binary pattern around a specific threshold, but rather clinicians use the test as a continuous score, with the rates of further testing and evaluation rising with higher Corus CAD scores. (See section below for a further discussion of Corus CAD as a continuous score.)
• In appreciation to Palmetto’s original understanding of Corus CAD and in an effort to be responsive to Palmetto’s desire to see additional analysis, we reviewed the COMPASS data, where we had performed either a CCTA or ICA on every evaluable patient. This new analysis allowed us to determine the number of procedures that would be performed on patients if physicians followed the dichotomous pathway assumed by Palmetto (Corus CAD and then advanced testing for all patients with scores >15) and compare it to use of MPI alone, which would be the likely pathway if access to Corus CAD is not available. Since the dichotomous pathway would be the “worst case” for the number of downstream procedures compared to the use as a continuous score, we believe this analysis represents the floor for the clinical utility of Corus CAD in this data set.
All patients (n=431) Corus MPI CCTA & ICA
MPI Alone 0 431 481
Corus then MPI 431 2322 343
aAssumptions
All patients wi
All patients with Corus CAD ≥ 15 go on to MPI
BThomas et. al. COMPASS
1 = number of patients with positive MPI; 2 = us CAD score; 3= number of patients with elevated score and positive MPI
• Based on the analysis above, the clinical strategy of Corus CAD followed by MPI results in a 46% (n=199) reduction in MPI tests and a 29% (n=14) reduction in cardiac catheterization procedures. Given the procedural risks, radiation exposure, and patient burden for both MPI and cardiac catheterization procedures, the use of Corus CAD provides patient outcome benefit when compared to MPI alone.
• To evaluate that the reduction in downstream testing does not negatively impact patient safety, we have also published data that shows low score patients are unlikely to have major adverse cardiac events or cardiac revascularization, at rates equivalent to negative imaging tests
• In the large, NHLBI sponsored PROMISE study, a subset of the patients (N=2,370) had the Corus CAD test drawn for analysis and followed for a minimum of two years

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
71 11/2018
• PROMISE showed that Corus CAD scores was equally predictive of the composite endpoint (death, myocardial infarction, unstable angina, or revascularization) when compared with a negative noninvasive test (functional test or CTA)
o Patient with Corus CAD ≤15 (N=1,058) had an event rate of 3.21% which was no different (P=.29) to the event rate for negative noninvasive tests (N=1,963)
o In summary, the authors of the PROMISE study stated “the Corus CAD is associated with oCAD, can improve risk stratification, and identifies individuals at low risk for cardiac revascularization procedures in the short term”
Conclusion: Corus CAD reduces the number of downstream procedures which drives improved patient outcomes with no negative impact on patient safety
o We have published and presented other examples of clinical utility and the effect of the Corus CAD score on clinical decision making, particularly as the Corus CAD score relates to medication initiation and adherence
• In the PRESET Lipids study (presented at SGIM 2018 Meeting), the purpose of the study was to examine prescriptions of lipidlowering agents in relation to Corus CAD scores. Prospective exploratory endpoints were collected from the PRESET registry of 566 patients from 21 sites.
• PRESET Lipids – patients with higher Corus CAD scores were more likely to initiate lipid lowering therapy. This finding is important, as higher score patients are more likely to have coronary artery disease and are more likely to benefit from use of this drug class.
Corus CAD Impact of New Lipid Lowering Prescriptions
Corus CAD Score New Prescriptions for Lipid Lowering Medication< 15 6% (16/252)> 15 19% (59/314)
P<0.0001Pokrywka et al, presented at the 2018 SGIM Meeting
In this sub-group analysis of a community-based registry, the Corus CAD test was adopted into clinical practice and associated with a statistically significant and clinically relevant change in the rate of new prescription for lipid-lowering medication.
o PICNICC - patients with higher scores were more likely to start on lipid lowering therapy and were more likely to be adherent with this therapy. This finding is very consistent with the Medicare HEDIS/Five Star program. (Medicare members with a prescription for a cholesterol medication filled that prescription greater than or equal to 80% of the time they are supposed to be taking the medication.)

72 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
In the PICNICC study (Parsons et al, Circulation 2012;126:A17332), the purpose of the study was to explore the relationship between Corus CAD scores and effect on patient utilization and adherence to lipid lowering therapy. In this retrospective study on 767 patients, researchers examined medication adherence by reviewing medication dispensing data. Assessment of medication adherence relied on the proportion of days covered methodology, quantified by the medication possession ratio (MPR) after 365 days of follow-up. We determined the quantity of medication dispensed and the number of days supplied data on each prescription for each patient.
Medication Adherence in PICNICC
Corus CAD Score Adherence with Lipid Lowering Medication
<15 64%
>15 75%P<0.001
Parsons et al, Circulation. 2012;126:A17332
Conclusion: The analyses above provide other examples of clinical utility. Patients with higher Corus CAD scores were more likely to start lipid-lowering lipid therapy and more likely to continue such therapy, and lipid-lowering therapy has been associated with improved cardiovascular outcomes.
Summary of Section 1: Clinical Utility of Corus CAD
We have demonstrated clinical utility in the overall and elderly population by showing that the use of Corus CAD:
• Provides an improved pre-test probability over clinical factors
• Provides incrementally actionable information that is not available from other sources
• Changes physician clinical decision making
• Is associated with medication adherence
• Decreases the use of downstream cardiac testing
Section 2: Clarifications
In the correspondence with Palmetto and in the draft coverage policy, there were a number of topics that CardioDx believes were not adequately clarified for Palmetto.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
73 11/2018
Those topics include:
1. Corus CAD as a continuous score
2. Corus CAD as a rule out test
We wanted to include those topics here in order to more directly address Palmetto’s concerns.
• The use of Corus as a dichotomous score versus a continuous score
o The Corus CAD test was always intended to be used as a continuous score. CardioDx has always reported the Corus CAD test as a continuous score. Every patient report form since product launch in 2009 includes the following graphic:
The referenced graphic could not be displayed in this report format.
• We have included the entire Patient Report Form as Exhibit C
• We believe that confusion on the clinical value of Corus CAD may stem from the conflating of two issues 1) the use of Corus CAD as a dichotomous score or a continuous score and 2) whether the measurement of “referral rates” based on the Corus CAD test provides a meaningful metric to assess clinical utility.
• On the first point of the clinical use of Corus CAD as a dichotomous or continuous score, we have demonstrated with strong published evidence that the test – in the hands of practicing physicians – is consistently and correctly used as a continuous score.
• The score of 15 is used to perform statistical analysis on the sensitivity, specificity, negative predictive value, and positive predictive value.
• We recognize that there were multiple references in the 2012 submission to Palmetto about the threshold of 15, including a patient flow diagram excerpted from the pre-publication COMPASS trial data. The references to a threshold of 15 can lead one to think of the test as a dichotomous yes/no result around one and only one threshold. We would note, however, that also included in the 2012 submission were several references (page 18 of the submission) to data that showed the clinicians were not using the test solely as a dichotomous score, but were using it as a continuous score consistent with their understanding of the progression of coronary artery disease and the Corus CAD patient report form.
• As referenced in Exhibit A, a Corus CAD score of 15 represents an 8% probability (in the COMPASS study) of a patient currently having oCAD. That 8% probability is true for patients of all ages and both sexes. Physicians are aware that elderly male patients have a higher risk of oCAD, so they understand that elderly male patients will have higher scores. Given the known higher risk for males patients as well as the fact that not every elderly male has obstructive CAD as the cause of the patients’ symptoms, physicians use the probability associated with the Corus CAD score for a particular patient to determine whether it is appropriate to rule out furthe cardiac testing.

74 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
• For reference, we have included in Exhibit A in the Appendix a listing that shows for each Corus CAD score, the probability of having obstructive CAD, the cumulative percentage of all patients receiving a specific score, the cumulative percentage of elderly receiving a specific score, and the cumulative percentage of all elderly male patients receiving a specific score. CardioDx believes this information can helpful in understanding the clinical use of Corus CAD.
• Conclusion: We appreciate that Palmetto’s previous understanding of Corus CAD’s usage may have been primarily informed by our original dossier submission to MolDX in 2012. The evidence published since that date demonstrates that the test has consistently been used as a continuous score. We believe that, as we continue the discussion with Palmetto, it will be useful to view the test as a continuous score, which is consistent with its use in clinical practice and supported physician users of Corus CAD.
• On the second point, CardioDx understands that Palmetto is not persuaded that referral rates are an adequate measure of improved patient outcomes. In the analysis above (1.a. – 1.d.) we have strived to go beyond referral rates and demonstrate more direct patient outcome benefit, including the actual reduction in unnecessary testing procedures. Given the high correlation between referrals rates and actual downstream testing, CardioDx believes that referral rates are an appropriate proxy for downstream patient outcomes. We acknowledge, however, that Palmetto is interested in seeing “harder” patient outcome endpoints. As an organization, we have committed to conducting a randomized controlled trial to extend our knowledge of Corus CAD and its impact on patient outcomes, including endpoints of unnecessary testing, resources utilization, and patient satisfaction. We are happy to share those plans with Palmetto.
• Conclusion: We acknowledge Palmetto’s concern about the use of referral rates as less than a direct measure of improved patient outcomes. We believe that the data presented above on the change in pre-test probability and the reduction of downstream testing, coupled with CardioDx’s commitment to conduct a randomized controlled trial for a diagnostic test provides additional support for the continuation of Medicare coverage.
Clarifying the use of Corus CAD as a “rule out” test
• In an effort to clearly and simply communicate the clinical value of Corus CAD, CardioDx has used the term “rule out” to describe its primary function
• A more precise description of the test’s value is “to help clinicians determine if given the patient’s current risk, they can be ruled out of having oCAD so that further cardiac testing would be unnecessary”
• A less than optimal reading and potentially a mis-interpretation of the published literature is to believe that the test absolutely “rules out” the presence of coronary artery disease in scores below 15 and “rules in” the presence of disease at scores above 15

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
75 11/2018
• In the original MolDX submission in 2012, we noted (page 18) that Corus CAD is used as a continuous score by showing the relationship between Corus CAD score and physicians decision to order advanced testing and/or cardiac evaluation. We have extended that early work by publishing several additional studies (PRESET, IMPACT-PCP) demonstrating the physicians use the test as a continuous score in making clinical management decisions.
• It was our intention in that original submission as well as our supplemental publications to show that the physician’s decision to pursue or not pursue additional testing and evaluation is impacted by the Corus CAD score. That decision by the physician will also include other relevant clinical information about the patient. Ultimately it is the physician who determines if he or she can rule out oCAD as the cause of the patient’s symptoms. CardioDx believes this model is consistent with other tests that provide probabilities (e.g. breast cancer recurrence scores), which also give guidance to the physician but do not dictate clinical decision making.
Conclusion: The Corus CAD helps clinicians determine if given the patient’s current risk, they can be ruled out of having oCAD so that further cardiac testing would be unnecessary.
3. Section 3: Other Information
o We believe that there is additional information that is supportive of continued coverage for Corus CAD by Palmetto:
o American Heart Association Scientific Statement
o The AHA issued their first genome focused Scientific Statement titled “The Expressed Human Genome in Cardiovascular Disease and Stroke: Refinement, Diagnosis, and Prediction” in July 2017
Only two diagnostic products, Corus CAD and AlloMap, were included in that publication
Corus CAD was referred to as “valid and useful” in the report
Comment: We were gratified by the inclusion of Corus CAD in the recent American Heart Association Scientific Statement. While different than the inclusion in guidelines, we believe that the recent AHA Statement validates the quality and quantity of the published data on Corus CAD and constitutes a strong argument for continued Medicare coverage.
o No financial incentive driving usage of Corus CAD
Unlike stress echo, nuclear imaging, and coronary angiography, in which the physician is financially compensated for performing those tests under a fee-for-service system, there is no financia incentive for physicians to use Corus CAD
Since the product’s launch in 2009, the Corus CAD test has been ordered over 250,000 times, with many physicians using the tes consistently for multiple years

76 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Given the challenges with managing patients in today’s complicated health care environment, physicians do not have the time to order tests or complete procedures that do not add to their clinical decision making
Comment: We believe that physicians consistently use the Corus CAD test because they find it to have clinical utility in their patient populations
• Providing Additional Information to Elderly Patientso In our effort to continually add more value to clinicians in their use of our test, we sent a letter to
MolDX on April 1, 2015 expressing our desire to add additional information to the Corus CAD Test Report Form. That letter stated that elderly patients receive few scores below 15, and that CardioDx was proposing to add information to the test report form. We believe that providing the percentile information will add a “relative risk” component to the absolute risk provided by the Corus CAD score.
Comment: We have endeavored to be thoughtful and pro-active about the specific needs of patients in the Medicare population. We are always willing to engage with Palmetto in an effort to provide additional information and to address any questions that may arise.
• In the draft policy, Palmetto inquired as to the number of elderly patients included in the published clinical trials. The chart below highlights the number and percentages of patients over the age of 65 in our referenced studies.
Study All (n) Elderly (n) Elderly Mailes (n) Elderly Females (n)
PREDICT 526 192 (37%) 109 (21%) 83 (16%)
COMPASS 433 83 (19%) 44 (10%) 39 (9%)
IMPACT-CARD 83 16 (19%) 4 (5%) 12 (14%)IMPACT-PCP 251 73 (29%) 23 (9%) 50 (20%)PROMISE substudy 2,370 638 (27%) 231 (10%) 407 (17%)
PRESET 566 176 (31%) 68 (12%) 108 (19%) In addition to our extensive list of previously published studies, CardioDx continues to invest in additional data sets. The company is currently enrolling patients in trials with both the Veterans Administration and the Allegheny Health Network. Both of these trials are designed to look at health care resource utilization and health outcomes in patients that receive the Corus CAD test compared to patients with similar symptoms that do not receive the Corus CAD test.
• Access to quality cardiovascular care
o One of the key benefits of the Corus CAD test is the ease of use in multiple settings.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
77 11/2018
o The simple blood draw is significantly less complicated, less time consuming, and more patient friendly than any of the competing imaging modalities
o The test can be administered in the same patient visit that the patient describes the symptoms. No additional appointments, fasting, or special preparations are necessary.
o That ease of use makes Corus CAD an ideal solution for practices with any of the following characteristics:
Within in a rural setting, where access to a cardiologist or advanced testing equipment can require long travel time
With a large population of elderly patients, where limited mobility makes coming back for additional appointments difficult
With a population that is at risk for additional radiation exposure and complications from imaging studies
o We have also provided (in a separate document) to Palmetto a marked up version of the draft policy, which responds to questions and concerns raised.
Summary
a. Corus CAD has been extensively studied with 30 publications in peer reviewed journals
b. Corus CAD was noted in the American Heart Association Scientific Statement as “valid and useful”
c. Corus CAD has been shown to provide actionable information that is not available from other sources. Corus CAD drives change in physician behavior
d. Corus CAD changes the pre-test probability of having oCAD
e. Corus CAD decreases the number of advanced cardiac tests performed without a negative impact on patient safety
f. Therefore, we request a change to the draft policy that would maintain coverage for Corus CAD
CardioDx appreciates the time and effort that Palmetto has devoted to reviewing the Corus CAD test.
Conclusion:CardioDx believes it has demonstrated Corus CAD’s analytical and clinical validity in the intended use population and that the test has clinical utility in directing diagnostic and therapeutic management in patients with suspected oCAD, including Medicare beneficiaries. Therefore, we urge Palmetto/MolDx to retain limited coverage for the test in the intended use population. Given the extensive nature of our comments/submission and previous discussions with the MolDX team regarding the evidence, we request an opportunity to meet to discuss the evidence provided.

78 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Response 4:The company representative’s comments indicate that the test is intended to be interpreted based on the continuous score. The Corus CAD result was not intended to be interpreted in a dichotomous fashion using a threshold of 15. However, a significant limitation to the use of the Corus CAD test is the lack of clarity from the company or the existing evidence as to how the test result should be interpreted. As the company points out in the comments above, the reported result from the test is a continuous score and has been used that way by clinicians. However, the company also points out that they have selected a threshold score of 15 to perform statistical analysis on the sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV). Notably, the company had to dichotomize the score to do sensitivity, specificity, NPV, and PPV analyses, because such analyses can only be done for a dichotomous outcome. If the test is intended to be used as a continuous outcome, such analyses are meaningless. However, the company makes the information on the sensitivity and specificity for the score threshold of 15 available on the report, and it has included analyses on how the results of the Corus CAD test affected clinical decision making based on such dichotomized test result in its comments above.
In summary, much of the evidence surrounding the diagnostic capability of the test focuses on this dichotomization, and treating the test result as a continuous variable in clinical applications rather than a dichotomous variable means that applicability of studies focusing on dichotomized results is quite limited.
Additionally, the company points out that the test has been studied in individuals who are likely to represent the Medicare beneficiary population, specifically the population who is Medicare eligible on the basis of age. However, whether studies on Corus CAD included subjects who are likely to represent the Medicare population is less relevant to the justification for coverage than the matter of what the Corus CAD test showed in such subjects. The draft LCD is non-covering the Corus CAD test specifically due to a lack of clinical utility, which relates to changing the management of a patient in a way that is beneficial to the patient. As such, for the Corus CAD test to be covered by Medicare, it is important to have evidence indicating not only that the test was studied in a population representative of the Medicare population but also that test changes management in this population in a way that benefits the patient. There remains a lack of sufficient evidence demonstrating this point.
Comment 5:A representative for CardioDX sent the following comment:The developer of test recently completed data analysis determining if the reduction in referral rates to cardiologists and cardiac procedures we had seen in our previous published studies would be reflected in lower utilization rates in medical claims data in a comparative analysis. The developer also believed that through the analysis of a large, medical claims database, we could provide an extensive comparative effectiveness analysis of the real world, current impact of the Corus CAD test. We were especially interested in comparing the rates of clinical utilization in patients that received the Corus CAD test to propensity-matched patients that did not receive the Corus CAD test. They wanted to share additional information that has recently become available concerning the use of the Corus CAD test and are in the process of completing a manuscript on the study.The developer also sent in additional information concerning the intended use for the test, physician education and training, and laboratory information system requirements. Information was also provided concerning the requirements on test requisition form.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
79 11/2018
They wish to see continued coverage for the Corus CAD test and not the proposed non-coverage as listed in the draft policy based on the following criteria listed in the comments received.Corus CAD has been extensively studied with 30 publications in peer reviewed journals
• Including being highlighted in a recent American Heart Association Scientific Statement as “valid and useful”
• CardioDx limits use of Corus CAD to symptomatic patients compared with the pre-test probability based upon clinical factors
• Corus CAD score leads to physician changes in obstructive CAD probability assessment
• Corus CAD has been shown to provide actionable information that is not available from other sources
• NEW DATA - Corus CAD decreases the number of advanced cardiac procedures performed compared to controls in the Medicare population
Response 5:We look forward to receiving any additional data that could potentially show how the lives and health of Medicare beneficiaries can be improved, and we will review all such data.
Comment 6:The full text of a manuscript for a study evaluating utilization of healthcare services following the Corus CAD test is provided below. This was sponsored by the test developer. It has not been peer-reviewed to our knowledge.
Corus CAD
Medical Claims Data Analysis Now Available
IntroductionCardioDx had previously submitted comments on the draft LCD for Corus CAD to Palmetto on May 4, 2018. Since that time, the company has been able to analyze additional data and is including these data in this public comment to CGS.
Several months ago, CardioDx undertook a project to analyze medical claims data to help identify and quantify the clinical impact of the Corus CAD test. The company was interested in determining if the reduction in referral rates to cardiologists and cardiac procedures we had seen in our previous published studies would be reflected in lower utilization rates in medical claims data in a comparative analysis. The company also believed that through the analysis of a large, medical claims database, we could provide an extensive comparative effectiveness analysis of the real world, current impact of the Corus CAD test. We were especially interested in comparing the rates of clinical utilization in patients that received the Corus CAD test to propensity-matched patients that did not receive the Corus CAD test.

80 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
CardioDx collaborated with Baker Tilly Virchow Kraus, LLP on this analysis. Baker Tilly provided access to data from Optum, which contains primarily commercial and Medicare Advantage data from United Healthcare. Baker Tilly was also responsible for the data analytics work from a statistical analysis plan that was jointly developed between CardioDx and Baker Tilly, with input from several industry experts.
While we initiated this study several months ago, the analysis was not available until mid-June 2018. Therefore these data were not able to be included in our submission during the public comment period for Palmetto, but we are pleased to provide these data during the public comment period for CGS. Baker Tilly is currently drafting a manuscript that will include results from the study.
MethodologyBaker Tilly examined the medical claims available from Optum for the period January 1, 2015 through October 31, 2017. In those data, they identified 1,431 patients with claims for the Corus CAD test between July 1, 2015 and April 30, 2017. Baker Tilly also identified 127,268 control patients that both a) met the inclusion and exclusion criteria for the study and b) had at least one claim for one of the four functional / anatomical tests.
Those four functional / anatomical tests are:
1. Nuclear perfusion imaging or MPI
2. Stress ECG
3. Stress echocardiogram
4. Coronary Computer Tomography Angiography (CCTA)
The inclusion and exclusion criteria are noted below:
Inclusion criteria:
• Typical or atypical symptom with risk factor consistent with potential coronary artery disease (intended use criteria for Corus CAD)
• Received Corus CAD (index event for the Corus CAD arm) between July 2015 and April 2017, inclusive OR Received an MPI, stress echo, stress ECG, or coronary CT Angiography (index event for the control arm) between July 2015 and April 2017, inclusive
• Continuously enrolled in the health plan for 6 months prior and 6 months post the index event
• Age 21 or older at the data of the index event
Exclusion criteria:
• History of Myocardial Infarction (MI)
• Current MI or acute coronary syndrome
• Any previous coronary artery revascularization

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
81 11/2018
• Diabetes mellitus
• Suspected unstable angina
• Systemic infection
• Systemic inflammatory or auto-immune conditions
• Oncological conditions
• Any major surgery within four months
Baker Tilly then performed an outlier analysis that removed 0.06% of the patients (n=71) based on the effect of extreme observations on overall data in an exponential (Gamma) distribution.
Once Baker Tilly determined the available patients that met the inclusion and exclusion criteria, they completed a propensity matching process that equalized the following criteria between the two groups in a 4:1 ratio of controls to cases:
• Gender
• Age
• Geographic region
• Typical symptom or atypical symptom with risk factor
• Minority population of patient’s zip code
• Comorbidities (obesity, hypertension, smoking, dyslipidemia)
• Insurance type (commercial, Medicare Advantage)
For the analysis we included:
• 4,079 patients with commercial insurance (2,125 females, 1,954 males)
o 794 patients in the Corus CAD arm (412 females, 382 males)
o 3,285 patients in the control arm (1,713 females, 1,572 males)
• 1,421 patients with Medicare Advantage insurance (892 females, 529 males)
o 306 patients in the Corus CAD arm (194 females, 112 males)
o 1,115 patients in the control arm (698 females, 417 males)

82 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
The endpoints that were analyzed included:
• Comparison of the two arms at 60 and 180 days
• Frequency of invasive coronary angiography or cardiac catheterization
• Frequency of coronary artery revascularization and CABG (coronary artery bypass graft)
• Frequency of functional and anatomical tests
• Major adverse cardiac events (MACE), including myocardial infarction, hospitalization due to unstable angina, or transient ischemic attack/stroke
• Frequency of other coronary artery disease (CAD) related resource utilization (office visits, emergency department (ED) visits and inpatient admissions)
The 60-day endpoint allowed for measurement of the episode of care around the evaluation of the symptomatic patient. The 180-day endpoint allowed for confirmation of the shorter term finding as well as validation of the robustness of such findings at a longer time interval. We are conducting an analysis looking at the effect of the Corus CAD score in 5-point increments: these results will be reported separately in the future.
Results
Results SummaryThe analysis of the large medical claims database found that patients who received the Corus CAD test had less cardiac related medical care after their index event than patients in the control arm. Specifically, the Corus CAD patients had fewer tests and procedures as compared to usual care control patients, specifically:
• Corus CAD care patients had fewer functional and anatomical tests
• Corus CAD care patients had fewer invasive coronary angiographies
• Corus CAD care patients had fewer coronary artery revascularizations
• Corus CAD care patients had fewer office, emergency, and inpatient admissions
The reduction in downstream tests and procedures had no negative impact on patient outcomes, as Corus CAD care patients had lower or similar MACE rates.
We looked separately at the results for patients with commercial insurance and Medicare Advantage and found similar results:
• In the commercial insurance population
• Corus CAD patients had fewer functional and anatomical tests than usual care control patients
• Corus CAD patients had fewer invasive coronary angiographies than control patients

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
83 11/2018
• Corus CAD patients had fewer cardiac related encounters (office visits, ED visits, in patient admission) than control patients
• In the Medicare population
• Corus CAD patients had fewer invasive coronary angiographies than control patients
• Corus CAD patients had fewer revascularizations than control patients
• Corus CAD patients had fewer cardiac related encounters (office visits, ED visits, in patient admission) than control patients
• Male patients that did not receive the Corus CAD are 3x more likely to be sent for an invasive coronary angiography procedure at 180 days
• Male patients that did not receive the Corus CAD are 4x more likely to be sent for an invasive coronary angiography procedure at 180 days
• Medicare patients had a higher yield (percentage of patients who received revascularization procedures after an invasive coronary angiography) in the cardiac catheterization lab than control patients at 60 days
• Corus CAD patients had lower rates of MACE than control patients
Results for All Patients When we evaluated the endpoints at 60 DAYS post the index event for ALL patients in the study, we found the following results:
Functional and Anatomical Tests1
• For the Corus CAD patients, 16.4% (n=180) received a test
• For the control patients, 27.9% (n=1,229) received a test
• The rate of functional and anatomical testing in the Corus CAD population was significantly lower than the control arm (p<0.0001)
Invasive Coronary Angiography (ICA)
• For the Corus CAD patients, 1.3% (n=14) underwent an ICA procedure
• For the control patients, 5.6% (n=246) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p<0.0001)

84 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.5% (n=6) underwent a coronary artery revascularization procedure
• For the control patients, 1.8% (n=80) underwent a coronary artery revascularization procedure
• The rate of coronary artery revascularization in the Corus CAD population was significantly lower than the control arm (p=0.0005)
CAD Related Utilization2
• For the Corus CAD patients, 1.7% (n=19) had at least one CAD related utilization event
• For the control patients, 4.0% (n=176) had at least one CAD related utilization event
• The rate of CAD related utilization in the Corus CAD population was significantly lower than the control arm (p<0.0001)
When we evaluated the endpoints at 180 DAYS post the index event for ALL PATIENTS in the study, we found the following results:
Functional and Anatomical Tests
• For the Corus CAD patients, 21.6% (n=238) received a test
• For the control patients, 30.9% (n=1,359) received a test1Includes myocardial perfusion imaging (MPI), stress ECG, stress echo, or coronary CTA 2Includes office visits, emergency room visits, and in patient admissions
• The rate of testing in the Corus CAD population was significantly lower than the control arm (p<0.0001)
Invasive Coronary Angiography
• For the Corus CAD patients, 2.6% (n=29) underwent an ICA procedure
• For the control patients, 6.5% (n=286) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p<0.0001)
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.8% (n=9) underwent a coronary artery revascularization procedure
• For the control patients, 2.1% (n=92) underwent a coronary artery revascularization procedure
• The rate of coronary artery revascularization in the Corus CAD population was significantly lower than the control arm (p=0.0017)

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
85 11/2018
CAD Related Utilization
• For the Corus CAD patients, 2.6% (n=29) had at least one CAD related utilization event
• For the control patients, 5.0% (n=221) had at least one CAD related utilization event
• The rate of CAD related utilization in the Corus CAD population was significantly lower than the control arm (p=0.0002)
Summary of Analysis for All Patients: In the overall population, patients that received the Corus CAD test received fewer advanced cardiac tests, had fewer invasive coronary angiographies, had fewer revascularization procedures, and had fewer CAD related utilizations than patients that did not receive the Corus CAD test.
Results for Medicare Advantage PatientsWhen we evaluated the endpoints at 60 DAYS post the index event for Medicare Advantage patients (n=1,421) in the study, we found the following results:
Functional and Anatomical Tests
• For the Corus CAD patients, 15.7% (n=48) received a test
• For the control patients, 14.2% (n=158) received a test
• The rate of testing in the Corus CAD population was not significantly higher than the control arm (p=0.4520)[1]
• Note the functional and anatomical tests for this endpoint represent the second such tests received by these patients, as the first such test was the index event
Invasive Coronary Angiography
• For the Corus CAD patients, 0.7% (n=2) underwent an ICA procedure
• For the control patients, 7.1% (n=79) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p<0.0001)
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.3% (n=1) underwent a coronary artery revascularization procedure
• For the control patients, 2.5% (n=28) underwent a coronary artery revascularization procedure
• The rate of coronary artery revascularization in the Corus CAD population was significantly lower than the control arm (p=0.0053)

86 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
CAD Related Utilization
• For the Corus CAD patients, 2.0% (n=6) had at least one CAD related utilization event
• For the control patients, 5.7% (n=63) had at least one CAD related utilization event
• The rate of CAD related utilization in the Corus CAD population was significantly lower than the control arm (p=0.0054)
When we evaluated the endpoints at 180 DAYS post the index event for Medicare Advantage patients (n=1,421) in the study, we found the following results:Functional and Anatomical Tests
• For the Corus CAD patients, 21.6% (n=66) received a test
3In the control group with Medicare Advantage coverage, a larger percentage of the index events was an MPI test (69%) compared to the control patients with commercial insurance (45%). When the index event is an MPI test, the physician may be less likely to order a functional and anatomical test (stress echo, stress ECG, coronary CTA) that he or she may consider less informative than an MPI, explaining the difference between the Medicare Advantage and commercial patients.
• For the control patients, 19.2% (n=214) received a test
• The rate of testing in the Corus CAD population was slightly higher than the control patients, but the difference was not statistically significant (p=0.2851)
Invasive Coronary Angiography
• For the Corus CAD patients, 2.6% (n=8) underwent an ICA procedure
• For the control patients, 8.6% (n=96) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p<0.0001)
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.3% (n=1) underwent a coronary artery revascularization procedure
• For the control patients, 2.8% (n=31) underwent a coronary artery revascularization procedure
• The rate of coronary artery revascularization in the Corus CAD population was significantly lower than the control arm (p=0.0029)
CAD Related Utilization
• For the Corus CAD patients, 3.6% (n=11) had at least one CAD related utilization event
• For the control patients, 7.4% (n=82) received at least one CAD related utilization event
• The rate of CAD related utilization in the Corus CAD population was significantly lower than the control arm (p=0.0257)

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
87 11/2018
MACE
• For the Corus CAD patients, 0.0% (n=0) had a MACE event within 180 days
• For the control patients, 0.6% (n=7) had a MACE event within 180 days
• The rate of MACE events in the Corus CAD population was lower than the control arm but the difference was not statistically significant (p=0.3573)
Summary of Analysis for Medicare Advantage Patients: In the Medicare Advantage population, patients that received the Corus CAD test had fewer invasive coronary angiographies, had fewer revascularization procedures, and lower rates of CAD related utilization than patients that did not receive the Corus CAD test.In the Medicare Advantage population, patients that received the Corus CAD test had no statistical difference of MACE events than those who did not receive the Corus CAD test. Therefore, the reduction of tests and procedures seen in patients that receive the Corus CAD test does not increase the patient’s risk, as seen in the rate of MACE.
Results for Medicare Advantage Male PatientsWhen we evaluated the endpoints at 60 DAYS post the index event for Medicare Advantage male patients (n=529) in the study, we found the following results:
Functional and Anatomical Tests
• For the Corus CAD patients, 16.1% (n=18) received a test
• For the control patients, 13.2% (n=55) received a test
• The rate of testing in the Corus CAD population was slightly higher than the control patients but the difference was not statistically significant (p=0.4196)
• Note that the functional and anatomical tests for this endpoint represent the second functional and anatomical tests received by these patients, as the first such test was the index event
Invasive Coronary Angiography
• For the Corus CAD patients, 1.8% (n=2) underwent an ICA procedure
• For the control patients, 9.8% (n=41) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p=0.0014)
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.9% (n=1) underwent a coronary artery revascularization procedure
• For the control patients, 3.6% (n=15) underwent a coronary artery revascularization procedure

88 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
• The rate of coronary artery revascularization in the Corus CAD population was lower than the control arm, but the difference was not statistically significant (p=0.1056)
When we evaluated the endpoints at 180 DAYS post the index event for Medicare Advantage male patients (n=529) in the study, we found the following results.
Functional and Anatomical Tests
• For the Corus CAD patients, 24.1% (n=27) received a test
• For the control patients, 19.2% (n=80) received a test
• The rate of testing in the Corus CAD population was higher than the control patients. but the difference was not statistically significant (p=0.2027)
• The functional and anatomical tests for this endpoint represent the second such tests received by these patients, as the first such test was the index event
Invasive Coronary Angiography
• For the Corus CAD patients, 3.6% (n=4) underwent an ICA procedure
• For the control patients, 12.2% (n=51) underwent an ICA procedure
• The rate of ICA procedures in the Corus CAD population was significantly lower than the control arm (p=0.0015)
Coronary Artery Revascularization and CABG
• For the Corus CAD patients, 0.9% (n=1) underwent a coronary artery revascularization procedure
• For the control patients, 3.8% (n=16) underwent a coronary artery revascularization procedure
• The rate of coronary artery revascularization in the Corus CAD population was lower than the control arm, but the difference was not statistically significant (p=0.0848)
CAD Related Utilization
• For the Corus CAD patients, 5.4% (n=6) had at least one CAD related utilization event
• For the control patients, 10.8% (n=45) had at least one CAD utilization related event
• The rate of CAD related utilization in the Corus CAD population was lower than the control arm, but the difference was not statistically significant (p=0.0935)

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
89 11/2018
Summary of Analysis for Medicare Advantage Male Patients: In the Medicare Advantage male population, patients that received the Corus CAD test were sent to the cardiac catheterization lab less than 1/3 as often as patients that did not have the Corus CAD test. Male Corus CAD patients also were sent to other CAD related visits less than 1/2 as frequently as non-Corus CAD patients, although that difference was non-significant given the small sample size.
ConclusionsConclusions for the Medicare Advantage PopulationIn a large, claims analysis reflecting actual clinical care utilization and outcomes, Medicare Advantage patients that received the Corus CAD test had reduced invasive procedures
1. Patients that received the Corus CAD test had fewer invasive coronary angiography procedures
2. Patients that received the Corus CAD test had fewer coronary artery revascularization procedures
3. Patients that received the Corus CAD test had fewer CAD related office visits, ED visits, and inpatient admissions
4. The rate of testing and procedures in the Corus CAD arm did not negatively impact patient health, as seen in MACE rates
Corus CAD provides clinical utility and patient benefit by showing reduced rates of invasive procedures and CAD related encounters for the Medicare Advantage populati
Conclusions for Medicare Advantage MalesIn a large, claims analysis reflecting actual clinical care utilization and outcomes, male Medicare Advantage patients that received the Corus CAD test had reduced invasive coronary procedures
1. Patients that received the Corus CAD test had fewer invasive coronary angiography procedures
2. Patients that received the Corus CAD test had fewer CAD related office visits, ED visits, and inpatient admissions
o Males that received the Corus CAD test had 50% fewer cardiac related office visits, ED visits, and hospital admissions, but the difference was not statistically significant given the sample size
3. The reduction in tests and procedures in the Corus CAD arm did not negatively impact patient health, as seen in MACE rates
Corus CAD provides clinical utility and patient benefit by showing reduced rates of invasive procedures and CAD related encounters for the Medicare Advantage male population

90 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Limitations of the AnalysisAs with any data analysis, there are limitations of this approach. Those limitations include:
• Billing and diagnosis codes submitted on medical claims may not accurately reflect actual diagnoses
o Comment: The ability to study large number of patients with verified follow-up as well as the inclusion of large, demographically diverse, and multicenter cohorts represent advantages of this claims-based approach over other study methodologies and may thus mitigate any inaccuracies in the coding information. Furthermore, since it is likely that any coding inaccuracies occurred among both the Corus CAD and control patients, these accuracies would be more likely to lead to a finding or no difference between the groups.
• Causation is difficult to show in all retrospective analysis
o Comment: There was a strong association noted, with robust findings across different populations and scenarios.
• The Corus CAD cohort may be different than the control cohort
o Comment: To address this concern, patients in the groups were selected from a large claims based database and were well matched on several demographic and clinical factors. Propensity matching allows one to design and analyze an observational (nonrandomized) study in order to mimic some of the particular characteristics of a randomized controlled trial. In this manner, the distribution of observed baseline covariates will be similar between treated and untreated subjects. (Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behavioral Research. 2011;46(3):399-424. doi:10.1080/00273171.2011.568786)
• The follow up period of 60 and 180 days may not be long enough
o Comment: An episode of care is variable, depending on multiple factors, including but not limited to the patient’s symptoms, access to resources, previous tests, and procedures. The results at 60 and 180 days were very similar, with greater than 75% of the clinical care utilization occurring within the first 60 days. We believe that time frame of 60 and 180 days is appropriate for showing the impact of Corus CAD testing on clinician decision-making.
Intended Use of Corus CAD Palmetto asked about the intended use of the Corus CAD test. We are pleased to provide a description of the intended use and the procedures the CardioDx uses to safeguard that patients fit the intended use criteria.
Intended Use of Corus CAD
• The Medicare Local Coverage Determination (LCD) established in 2012 reads as follows:
o “The CORUS® CAD test will be considered reasonable and necessary for patients with stable symptoms that have a history of chest pain, suspected anginal equivalent to chest pain, or a high risk of CAD, but no known prior myocardial infarction or revascularization procedures”

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
91 11/2018
• CardioDx reinforces the intended use in multiple ways, including
o Physician education and training
o Lab information system requirements
o Physician verification
• CardioDx lab rejects samples that are not within intended use
• Based on an inquiry from Palmetto, the next several pages will focus on how CardioDx ensures that patients have appropriate symptoms
Physician Education and Training
• CardioDx consistently educates and trains physicians on the intended use of Corus CAD using multiple approaches, such as
• Our marketing material
• Our sales representative training
• Regional Medical Director interactions
• Our website
Laboratory Information System Requirements
• Corus CAD test requisition form requires listing of symptoms
o Typical or atypical with a risk factor
• Laboratory Information Management System (LIMS) will not accept a sample for processing that does not have a typical or atypical/risk factor marked on the test requisition form
• The vast majority of test requisition designate that the patient has the appropriate symptoms
o A small number (0.89%) of TRFs were rejected because the patient was asymptomatic (June 2017- June 2018)
Test Requisition Form (TRF)
• Our Test Requisition Form requires an indication that each patient has either 1) typical symptom(s) or 2) or atypical symptom(s) and cardiac risk factor(s)
• CardioDx personnel review the TRF when the sample arrives in the lab to ensure that the TRF has contains the required information

92 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
• Physician signatures are required on all TRF forms
• TRF also includes a highlighted box listing the patient characteristics that would not be appropriate for Corus CAD testing
Analysis of Symptoms for Corus CAD Patients
• Historically the mix of symptoms has been approximately 50/50 between typical and atypical
o In April 2018, 45% of all samples received had typical symptoms
o In April 2018, 42% of Medicare samples received had typical symptoms
• The most common symptoms in the Medicare population are
o Typical – chest pain, shortness of breath
o Atypical – malaise, heartburn
o Patients with atypical symptoms are also required to also have a cardiac risk factor
• Multiple symptoms in the overall population
o Typical symptom – 60% of patients have more than 1 typical symptom
o Atypical symptom – 34% of the patients have more than 1 atypical symptom / risk factor
Physician Signature on the Test Requisition Form
• Every Test Requisition Form requires a signature to confirm that the test ordering meets intended use and follows exclusion criteria
o If a requisition form arrives without a signature, we contact the physician office and attempt to receive that signature
o Approximately 2% of all samples arrived without signatures in Q1 2018
o If we are not able to acquire the signature, the sample result is not reported to the physician
• To reinforce the physicians understanding of the Corus CAD intended use, we had physicians acknowledge and sign a separate document listing the intended use
o We collect > 650 completed acknowledgements May – August 2016
Summary of Intended Use Information
CardioDx strives to educate and inform the physician on the intended use of Corus CAD and diligently monitors incoming samples to insure they are appropriate for testing

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
93 11/2018
Concluding Remarks
• Corus CAD has been extensively studied with 30 publications in peer reviewed journals
• Including being highlighted in a recent American Heart Association Scientific Statement as “valid and useful”
• CardioDx limits use of Corus CAD to symptomatic patients compared with the pre-test probability based upon clinical factors
• Corus CAD score leads to physician changes in obstructive CAD probability assessment
• Corus CAD has been shown to provide actionable information that is not available from other sources
• NEW DATA - Corus CAD decreases the number of advanced cardiac procedures performed compared to controls in the Medicare population
Corus CAD had demonstrated clinical utility and provides patient benefit; therefore, we recommend continued coverage as a Medicare benefit
Response 6:The test sponsor provided us with an unpublished manuscript that has not been peer-reviewed from claims data as a comment to the draft LCD. The sponsor was made aware prior to submission that such information when provided as a comment to the draft LCD may be publicly shared as necessary to allow for a public response to comments as is required of Palmetto GBA and MolDX.
In summary, this was a retrospective observational study that examined health care service utilization in two cohorts using claims data from a large data set including commercial insurance beneficiaries and beneficiaries enrolled in Medicare Advantage plans. One cohort included patients in whom the CardioDX study was used. A control group was created using propensity-matching to obtain a 4:1 ratio of controls to CardioDX tested subjects in the study. Patients excluded from the study included those with diabetes and known obstructive coronary disease. The dependent variables examined in the study were utilization of healthcare services including diagnostic cardiac imagining, diagnostic catheterization, and cardiac revascularization interventions. Patient outcomes for survival, functional status, or quality of life were not reported.
Summary of the methods:Claims data from commercial and Medicare advantage plans was used including claims submitted between January 1, 2015 and October 31, 2017. Patients were considered for inclusion if they were enrolled in a plan submitting data to the data set for at least 6 months prior to and 6 months following an index event, which is further described below. The group of patients tested using the Corus CAD test was identified by the presence of a claim for this test in the beneficiary, and the use of the Corus CAD test was the index event for this group. A potential set of patients from whom the control group would ultimately be selected was identified if they did not have the Corus CAD test and had at least one of the following cardiac diagnostic tests: 1. Nuclear perfusion imaging or MPI 2. Stress ECG 3. Stress Echocardiogram 4. Coronary Computer Tomography Angiography (CCTA).

94 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
In addition to having a claim for an index event in the specified time window, specific inclusion criteria for the study was as follows: Typical or atypical symptom with risk factor consistent with potential coronary artery disease (intended use criteria for Corus CAD) and age 21 or older at the date of the index event. Exclusion criteria were as follows: History of Myocardial Infarction (MI), current MI or acute coronary syndrome, any previous coronary artery revascularization, diabetes mellitus, suspected unstable angina, systemic infection, systemic inflammatory or auto-immune conditions, oncological conditions, any major surgery within four months. The investigators identified 1,431 patients with claims for the Corus CAD test between July 1, 2015 and April 30, 2017, and they identified 127,268 control patients with a claim for one of the 4 tests in this time window. From the 127,268 control patients, a control group was created by propensity matching control patients to patients who received Corus CAD using the following matching variables: gender, age, geographic region, typical symptom or atypical symptom with risk factor, minority population of patient’s zip code, comorbidities (obesity, hypertension, smoking, dyslipidemia), insurance type (commercial, Medicare Advantage).
A final set of 2 cohorts of patients were selected for the study: 1,100 patients in the Corus CAD arm and 4,400 patients control arm.
The study sought to compare care utilization and outcomes in these two cohorts of patients at 60 and 180 days. Specific endpoints that were examined were:
• Frequency of invasive coronary angiography or cardiac catheterization
• Frequency of coronary artery revascularization and CABG (coronary artery bypass graft)
• Frequency of functional and anatomical tests
• Major adverse cardiac events (MACE), including myocardial infarction, hospitalization due to unstable angina, or transient ischemic attack/stroke
• Frequency of other coronary artery disease (CAD) related resource utilization (office visits, emergency department (ED) visits and inpatient admissions)
Methodological details for how the typical or atypical symptoms of a patient were identified in claims data are not explained in the manuscript. Additionally, the specific details of how specific diagnoses and comorbidities were abstracted from the claims data (e.g. comorbidity classification method) were not explained in the manuscript.
Brief response by MolDX to the methods:This study design, has the ability to show suggestive results, but not results that would establish clinical utility of the Corus CAD. This is not only because it is a retrospective observational study in which causation cannot be asserted, but also because of both the shallow nature of claims-based research and because of the relatively short window for observation of the study endpoints. Moreover, a clear study design was not provided up front, so it is unclear how much of the analysis was based on a-priori analytical decisions with intent to have the most informative study versus how much the study reflects selectively chosen results from an exploration of the data.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
95 11/2018
In summary, the nature of this study is such that it has the potential to hint at the clinical utility of the Corus CAD test and may be able to help create good hypothesis for future investigation, but this study the nature of its design, regardless of the results, does not allow conclusions to be drawn with a level of confidence that would support Medicare coverage.
Summary of the results:Results are reported stratified by payer as well as by gender. Here we summarize the most important results for making a coverage determination in the Medicare population, results for all patients as well as for the Medicare Advantage population.
As regards care utilization 60 days following the index event in all of the patients:
Results for endpoints following index event in all patients (combined payers)
Corus CAD % (n) Control % (n) Reported p-value
Care utilization
Functional or anatomic tests 16.4% (180 27.9%60 days 21.6% (1,229) <0.0001180 days (n=238) 30.9% <0.0001
Invasive coronary angiography <0.0001
60 days 1.3% (14) 5.6% (246) <0.0001
180 days 2.6% (29) 6.5% (286)
Coronary artery revascularization (and CABG) 0.000560 days 0.5% (6) 1.8% (80) 0.0017 180 days 0.8% (9) 2.1% (92)
Use of at least one CAD-related utilization <0.0001
60 days 1.7% (19) 4.0% (176) 0.0002
180 days 2.6% (29) 5.0% (221)
Major adverse cardiac events
60 days Not Reported Not Reported
180 days Not Reported Not reported

96 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Results for endpoints following index event in Medicare Advantage patients
Care utilization
Functional or anatomic tests 15.7% (48) 14.2% (158)
60 days 21.6% (66)
180 days
Invasive coronary angiography
60 days 0.7% (2) 7.1% (79) 0.0053
180 days 2.6% (8) 8.6% (96) 0.0029
Coronary artery revascularization (and CABG)
60 days 0.3% (1) 0.0054
180 days 0.3% (1) 0.0257
Use of at least one CAD-related utilization
60 days 2.0% (6) 5.7% (63)180 days 3.6% (11) 7.4% (82) 0.3573
Major adverse cardiac events
60 days Not Reported Not reported
180 days 0% (0) 0.6% (7)
In summary, the data shows less utilization of invasive coronary angiography, coronary artery revascularization, and CAD-related utilization for the combined payer (all patients) analysis and for the analysis restricted to Medicare Advantage patients. In the combined payer analysis, the Corus CAD cohort had less use of functional or anatomic tests than controls, but in the Medicare Advantage analysis the Corus CAD and control cohorts had numerically similar use of functional or anatomic testing. Major adverse cardiac events were only reported at 180 days for the analysis restricted to Medicare Advantage patients, and there was no significant difference between the groups.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
97 11/2018
MolDX assessment of study results: This study clearly shows a difference between the Corus CAD cohort and the control Cohort in terms of utilization of cardiac services when the analysis is performed for all patients as well as when it is restricted to Medicare Advantage patients only, with the latter group likely better representing the Medicare Fee for Service population. However, it did not show that there was any difference in patient outcome in terms of major adverse cardiac events at 180 days. There are two unanswered questions that this research leaves. 1. What exactly what defined the study population? And 2. Was the observed difference in utilization between groups due to the use of Corus CAD in one of the cohorts?
As regards the defined study population, this may become clear in further research that the company suggests that they may pursue. An important aspect of claims-based research is that clinical concepts and disease processes are not necessarily captured in claims data in the way that they must be clinically treated. For example, diagnosis capture, and assessment of medical comorbidities in a claim is done by ICD-9 or ICD-10 code. However, multiple ICD codes may reflect similar diagnostic concepts. (e.g. multiple codes for diabetes with different manifestations and complications), so grouping patients by specific ICD codes is often not practical or even feasible, and comorbidity grouping methods, of which a number have been developed, are used. Additionally, the few numbers of diagnosis fields on physician claims may mean that multimorbid patients have medical conditions not captured on each claim, but that are more likely to be captured when the longitudinal medical record is searched for that diagnosis. For Medicare’s hospital compare risk adjustment methodology, for example, the prior year of claims data is searched to find the presence of a particular comorbid condition for inclusion. Additionally, characteristics of the cohorts created for this study such as age, gender, and comorbid disease burden are not given. These are all important analytical details that help figure out how to translate patient features in claims data into clinical characteristics of human beings a physician encounters at the bedside. As such, though inclusion and exclusion criteria are given, the vagueness of both the methods and the cohorts of patients mean that it is unclear what the patient population of this study is. This question, while unclear in the current manuscript, is potentially answerable with a more detailed explanation of the methods without further research.
The second question related to the cause of the observed differences between groups in the endpoints does not seem easily addressed by the existing data set. It is also worth noting that propensity matching accounts for observed variables to make groups similar. The possibility of an important baseline difference between groups that is not captured in the observed variables used for propensity matching is quite possible, and if present may explain part or all of the observed differences in endpoints between the two cohorts. The intended role of Corus CAD test is to obviate the need for other coronary artery disease testing, and as such it would be natural to consider the reduced use of cardiac testing services in patients who received the Corus CAD test in a matched study to be significantly attributable the use of the Corus CAD test. This is a possibility, but a between group difference in the use of CAD care may also be the effect of a selection bias due to clinicians selecting various diagnostic modalities for different kinds of patients. While it can never be known with certainty that the two cohorts were similar at baseline, it is possible to test the possibility that the cohorts were likely different at baseline in a meaningful way not captured by the propensity matching, which is intended to make the two groups similar. If such a difference were found then it would strongly suggest that observed differences between the cohorts in the endpoints were related to baseline differences between the cohorts other than choice of index test to include a patient in the study.

98 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
In this study, such a test was done, though not explicitly described in this way by the study authors. Specifically, they studied the use of cardiac revascularization procedures, such as coronary artery bypass grafting surgery, in individuals who did and did not receive the Corus CAD test. They found that those who received the Corus CAD test were less likely to get a revascularization procedure. The importance of this is that while Corus CAD could plausibly be a substitute for diagnostic cardiac tests, it would not be a plausible replacement for therapeutic procedures; it is a test rather than an intervention. It is, therefore, implausible that laboratory in vitro measurement of blood compounds would affect coronary blood flow in the heart of a patient in vivo.
Another unlikely explanation of the observed association between Corus CAD use and lower utilization of revascularization services is that the use of Corus CAD in the cohort who had it used was informative in a way that accepted cardiac testing used in the control group was not. This explanation would require that Corus CAD’s use prevented unnecessary revascularization procedures. This explanation is unlikely if the data on Corus CAD’s test performance highlighted by the company in a prior comment is to true. The Corus CAD test has a sensitivity of 88%, a significantly greater sensitivity than myocardial perfusion imagining’s sensitivity of 21% in patients 65 years of age and older. As such, Corus CAD would tend not to catch obstructive coronary artery disease that conventional diagnostic approaches would not, which would not likely have the effect of reducing the use of revascularization procedures.
Additionally, revascularization procedures require an identification of the specific cardiac vasculature in need of revascularization. Even if the Corus CAD test is more accurate than conventional diagnostic techniques it still lacks anatomic specificity that may be needed to make a treatment decision. The conventional diagnostic approaches (i.e. those recognized in ACC guidelines) can provide the necessary anatomic information either by showing a specific poorly perfused region of the heart corresponding to a vascular territory, or by directly showing arterial obstruction, as may happen with angiography. The Corus CAD test does not provide anatomy specific-information and therefore cannot serve as a substitute for conventional cardiac diagnostic techniques. As such, in patients with a higher need for revascularization, there is necessarily a higher need for conventional cardiac diagnostic techniques for CAD, limiting the possible clinical utility of this test.
The observed difference in use of coronary artery revascularization procedures in the group who was tested with Corus CAD compared with the control group indicates that the Corus CAD group was a lower risk group for the need for cardiac intervention than the control group eve at baseline, or restated – the propensity matching was not successful in creating truly similar groups. It is a methodological strength of the study that they assessed the robustness of the propensity matching by looking at endpoints that would not be different in presence of successful propensity matching. However, it is a weakness of the study’s results that the study did find that propensity matching likely created dissimilar groups.
In summary, an unpublished manuscript of a claims-based study sponsored by the test sponsor provides evidence regarding the particular patients studied, but generalizing these findings to patients in clinical care cannot be meaningfully done both because the population studied was not clearly described, and more importantly, because differences in endpoints between the two studied cohorts were likely caused to an unknown degree by latent differences in the baseline cardiac risk of the two groups. Finally, even if these limitations did not exist, and we felt confident generalizing the findings to a well-defined population, the retrospective claims-based data with a relatively short follow-up does not allow for any meaningful

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
99 11/2018
conclusions that the Corus CAD test is associated with better or worse patient outcomes. As such, while this study may be suggestive, it does not provide evidence of clinical utility that would justify coverage by the Medicare program.
SKILLED NURSING FACILITY (SNF) INFORMATION
Ensuring Occurrence Code 22 is Billed Correctly on Skilled Nursing Facility Inpatient Claims MLN Matters Number: MM10922 Related CR Release Date: October 5, 2018 Related CR Transmittal Number: R2146OTN Related Change Request (CR) Number: 10922 Effective Date: April 1, 2019 Implementation Date: April 1, 2019
Provider Types Affected This MLN Matters Article is intended for Skilled Nursing Facilities (SNFs) billing Medicare Administrative Contractors (MACs) for SNF inpatient services provided to Medicare beneficiaries.
Provider Action Needed This article is based on Change Request (CR) 10922 which describes systems changes necessary to ensure SNFs bill Occurrence Code (OC) 22 correctly. Please make sure your billing staffs are aware of these changes. Background Medicare’s Common Working File (CWF) Maintainer recently discovered that an incoming inpatient claim was applied to the wrong benefit period when OC ‘22’ was submitted incorrectly on a SNF claim in history.
CR10922 will ensure OC ‘22’ is billed correctly so that the CWF can apply the appropriate benefit period.
Note that CR10922 contains no policy changes or new policies, and it improves the implementation of the existing policy in the Medicare Claims Processing Manual, Chapter 6 (https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c06.pdf). As a result of CR10922, your MAC will Return to Provider (RTP) an inpatient SNF claim (Type of Bill (TOB) 21X or swing bed claim with TOB 18X) when all of the following are present on the claim:
• OC ‘22’ and
• OC ‘22’ date is equal to the through date of the claim and
• Patient discharge status code is other than ‘30’.

100 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Additional Information The official instruction, CR10922 issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R2146OTN.pdf.
If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description October 5, 2018 Initial article released.
2019 Annual Update of Healthcare Common Procedure Coding System (HCPCS) Codes for Skilled Nursing Facility (SNF) Consolidated Billing (CB) Update
MLN Matters Number: MM10981 Related CR Release Date: October 5, 2018 Related CR Transmittal Number: R4143CP Related Change Request (CR) Number: 10981 Effective Date: January 1, 2019 Implementation Date: January 7, 2019
Provider Types Affected This MLN Matters® Article is intended for physicians, other providers, and suppliers submitting claims to Medicare Administrative Contractors (MACs), including Home Health & Hospice (HH&H) MACs and Durable Medical Equipment (DME) MACs, for services provided to Medicare beneficiaries who are in a Part A covered Skilled Nursing Facility (SNF) stay.
Provider Action Needed CR 10981 makes changes to HCPCS codes and Medicare Physician Fee Schedule (MPFS) designations that will be used to revise Common Working File (CWF) edits to allow MACs to make appropriate payments in accordance with policy for SNF CB in Chapter 6, Section 110.4.1 and Chapter 6, Section 20.6 in the Medicare Claims Processing Manual (https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c06.pdf). Make sure your billing staff are aware of these changes. Background The CWF currently has edits in place for claims received for beneficiaries in a Part A covered SNF stay, as well as for beneficiaries in a non-covered stay. These edits allow only those services that are excluded from SNF CB to be paid separately. Barring any delay in the MPFS, Medicare will provide the new code files CWF by November 1, 2018.
By the first week in December 2018, Medicare will post the new code files at https://www.cms.gov/Medicare/Billing/SNFConsolidatedBilling/index.html. The files will be applicable to claims with dates of service on or after January 1, 2019, through December 31, 2019. It is important and necessary for the

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
101 11/2018
provider community to view the “General Explanation of the Major Categories” file located at the bottom of each year’s update in order to understand the Major Categories including additional exclusions not driven by HCPCS codes. Additional Information The official instruction, CR10981, issued to your MAC regarding this change is available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4143CP.pdf. If you have questions, your MACs may have more information. Find their website at http://go.cms.gov/MAC-website-list.
Document History
Date of Change Description October 5, 2018 Initial article released.
This advisory should be shared with all health care practitioners and managerial members of the provider/supplier staff. Medicare Advisories are available at no cost from the Palmetto GBA website at www.PalmettoGBA.com/jma.
Address Changes
Have you changed your address or other significant information recently? To update this information, please complete and submit a CMS 855A form. The most efficient way to submit your information is by Internet-based Provider Enrollment, Chain and Ownership System (PECOS). To make a change in your Medicare enrollment information via the Internet-based PECOS, go to https://pecos.cms.hhs.gov on the CMS website. To obtain the hard copy form plus information on how to complete and submit it – visit the Palmetto GBA website (www.PalmettoGBA.com/jma).

102 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
TOOLS THAT YOU CAN USE
Top 10 Inpatient Hospital Medical Review Denials Module
To access this module and other online training courses, please go to the Self-Paced Learning Section (https://www.palmettogba.com/palmetto/providers.nsf/docscat/Providers~JM%20Part%20A~Learning%20Education~Self-Paced%20Learning) of the JM Part A website.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
103 11/2018
Top 10 Outpatient Medical Review Denials Module
To access this module and other online training courses, please go to the Self-Paced Learning Section (https://www.palmettogba.com/palmetto/providers.nsf/docscat/Providers~JM%20Part%20A~Learning%20Education~Self-Paced%20Learning) of the JM Part A website.

104 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Top 10 Skilled Nursing Facility (SNF) Medical Review Denials Module
To access this module and other online training courses, please go to the Self-Paced Learning Section (https://www.palmettogba.com/palmetto/providers.nsf/docscat/Providers~JM%20Part%20A~Learning%20Education~Self-Paced%20Learning) of the JM Part A website.

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
105 11/2018
New Medicare Card Information
For more information about the new Medicare card, please go to the New Medicare card Web Page on the CMS Website.
To access this page, copy and paste the following link in your browser:
https://www.cms.gov/Medicare/New-Medicare-Card/index.html

106 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
NOTES

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
107 11/2018
HELPFUL INFORMATION
Contact Information for Palmetto GBA Part A
Department Contact Information Type of InquiryAppeals Palmetto GBA
Part A AppealsMail Code: AG-630P.O. Box 100238Columbia, SC 29202-3238Fax: (803) 699-2425
For Fed Ex/UPS/Certified MailPalmetto GBAPart A Appeals Mail Code: AG-630Building One2300 Springdale DriveCamden, SC 29020
• Request for Redeterminations
• Redetermination Form
Contact Center (Provider)
Palmetto GBAPart A PCCMail Code: AG-840P.O. Box 100238Columbia, SC 29202-3238 Provider Contact Center: 855-696-0705
Our PCC Representatives are ready to answer your questions about billing problems and other issues. Please see the following links for more guidance about the Part A Interactive Voice Response (IVR) and contacting the Call Center.
IVR Flowchart (PDF, 74 KB) Call Flowchart (PDF, 95 KB) IVR Conversion Tool
Part A PCC Hours: 8 a.m. to 4:30 p.m. ET
EmailEmail Part A to have your inquiry answered. Please do not include any Protected Health Information.
• General coverage and Medicare-related questions
• Crossover questions
• Questions regarding claim filing requirements
• Explanation of denial reasons
• IVR resources
• MSP resources
• Modifier guidelines
• Medical record documentation questions
• Written Inquiries

108 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Checks For Overpayments
Palmetto GBAMedicare Part A Overpayments Mail Code: AG-340P.O. Box 100277Columbia, SC 29202-3277
Provider Inquiries:For inquiries regarding overpayments, please call the Provider Contact Center at 855-696-0705.
Fax Numbers:
• To send any financial correspondence to the overpayment department by fax, please fax this information to (803) 419-3275.
• To request an immediate offset, fax your request to (803) 462-2574.
• Overpayments
• Checks for cost report and credit balances
Cost Report Cost Report Filing
Mailing AddressPalmetto GBAAttn: Cost Report AcceptanceMail Code: AG-330P.O. Box 100144Columbia, SC 29202-3144
Fed Ex/UPS/Certified Mail AddressPalmetto GBAAttn: Cost Report AcceptanceMail Code: AG-3302300 Springdale DriveBuilding OneCamden, SC 29020-1728
Cost Report Overpayment Address (checks only)Palmetto GBAMedicare FinanceMail Code: AG-260P.O. Box 100277Columbia, SC 29202-3277
• Cost Reports
• Checks

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
109 11/2018
Credit Balance Reporting
Regular and Certified MailPalmetto GBAAttn: Credit Balance ReportingMail Code: AG-340P.O. Box 100109Columbia, SC 29202-3109
Fed Ex/UPS/Overnight CourierPalmetto GBAAttn: Credit Balance ReportingMail Code: AG-3402300 Springdale DriveBuilding OneCamden, SC 29020-1728
Credit Balance Overpayment Address(checks only):Palmetto GBAMedicare FinanceMail Code: AG-260P.O.Box 100277Columbia, SC 29202-3277
Reports may be faxed to:MCBR ReceiptsAttn: Credit Balance Reporting (803) 419-3277
If you have questions about your Credit Balance Report, please call the Provider Contact Center at: 855-696-0705.
• Questions or concerns regarding credit balance reports
Customer Service Center (Beneficiary)
1-800-Medicare (1-800-633-4227)
TTY: 877-486-2048
Visit the Medicare website at www.medicare.gov
All questions related to the Medicare program

110 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Electronic Data Interchange (EDI) for NC and SC
Email: [email protected]
Provider Contact Center: 855-696-0705
• EDI enrollment
• Administrative Simplification and Compliance Act (ASCA)
• Electronic Remittance Advice (ERA)
• PC-ACE Pro 32 (billing software)
• Direct Data Entry (billing software)
• Other EDI-related issues DDE Hours of Availability • Monday to Friday 6 am - 8 pm ET
• Saturday 6 am - 4 pm ET
• Sunday: Not AvailableElectronic Data Interchange (EDI) for VA and WV
NGS EDI Help Desk: 855-696-0705 • EDI enrollment
• Electronic Remittance Advice (ERA)
• PC-ACE Pro 32 (billing software)
• Direct Data Entry (billing software)
• Other EDI-related issues Financial correspondencewith/without checks
Palmetto GBAPO Box 100277Columbia, SC 29202
Freedom of Information Act (FOIA) Requests
Palmetto GBA – Part AFOIA CoordinatorMail Code: AG-840P.O. Box 100190Columbia, SC 29202-3190
Email: [email protected]
• FOIA requests
Medical Affairs Palmetto GBAMedical AffairsMail Code: AG-275P.O. Box 100238Columbia, SC 29202-3238
Send emails to [email protected].
• Local coverage determinations (LCDs)

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
111 11/2018
Medical Review Palmetto GBAPart A Medical ReviewMail Code: AG-230P.O. Box 100238Columbia, SC 29202-3238
Please call the Provider Contact Center (PCC) at 855-696-0705 for Medical Review questions.
Fed Ex/UPS/Overnight CourierPalmetto GBA Mail Code: AG-2302300 Springdale Drive, Building OneCamden, SC 29020Fax: (803) 699-2436
• Responding to Additional Documentation Requests (ADRs)
• Responses to our requests for medical records
Medicare Secondary Payer (MSP)
For questions/concerns related to MSP records, contact the Benefits Coordination & Recovery Center (BCRC) at: 855-798-2627 (TTY/TDD at 855-797-2627 for the hearing and speech impaired). Customer Service Representatives are available to provide you with quality service Monday through Friday from 8 a.m. to 8 p.m. ET, except holidays.
Mailing addresses are available on the CMS website.
• MSP questions
• Questions regarding beneficiary’s primary or secondary records
Provider Audit Palmetto GBAProvider AuditMail Code: AG-320P.O. Box 100144Columbia, SC 29202-3144
Palmetto GBACost Report Appeals and ReopeningsMail Code: AG-380P.O. Box 100144Columbia, SC 29202-3144
Email:Filing of Cost Report [email protected]
Filing of Cost Report [email protected]
• Issues related to cost reports, desk reviews, audits and settlements
• Issues related to the filing of cost report appeals and reopenings

112 11/2018
CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
Provider Enrollment
Palmetto GBAPart A Provider EnrollmentMail Code: AG-331P.O. Box 100144Columbia, SC 29202-3144
For inquiries regarding provider enrollment, please call the PCC at 855-696-0705.
• Enrollment (credentialing) questions
• Request CMS-855 B, I or R forms
• Change address, add a location or add a new member to a provider group
• Independent Diagnostic Testing Facility (IDTF) enrollment
• Electronic Funds Transfer (EFT) CMS 588 form
• Medicare Participating Physician or Supplier Agreement (PAR) CMS 460 form
• How to obtain a National Provider Identifier (NPI)
• Participation corrections
• IRS 1099 tax form corrections
• Consent forms Provider Outreach and Education (POE)
Palmetto GBAPart A POEMail Code: AG-830P.O. Box 100238Columbia, SC 29202-3238
For education, please complete the Education Request Form. To access this document, go to the Forms Web page at www.PalmettoGBA.com/jma/forms
• Educational training requests
• Request a speaker for association meetings in your state
Provider Reimbursement
Palmetto GBAProvider ReimbursementMail Code: AG-330P.O. Box 100144Columbia, SC 29202-3144
Phone Number: (803) 382-6104
Fax updated certificates for diabetes education, mammography and PET scan to the reimbursement department at (803) 935-0262.
• Submission of interim rate information
• Reimbursement issues
• Reimbursement specialist
• Submission of certificates
Southeastern Unified Program Integrity Contractor (SE UPIC)
Safeguard Services (SGS)-A CMS Unified Program Integrity Contractor 3450 Lakeside Drive, Suite 201 Miramar, FL 33027 Phone Number: (954) 988-2851 Website: www.safeguard-servicesllc.com
• Fraud
• Abuse
• Questionable billing practices

CPT codes, descriptors and other data only are copyright 2017 American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable FARS/DFARS apply. Current Dental Terminology, fourth edition (CDT) (including procedure codes, nomenclature, descriptors and other data con-tained therein) is copyright by the American Dental Association. ©2002, 2004 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
113 11/2018
NOTES