Nongenital pelvic leiomyosarcoma metastatic to the heart
-
Upload
diane-mitchell -
Category
Documents
-
view
214 -
download
2
Transcript of Nongenital pelvic leiomyosarcoma metastatic to the heart
GYNECOLOGIC ONCOLOGY 43, 84-87 (1991)
CASE REPORT Nongenital Pelvic Leiomyosarcoma Metastatic to the Heart’
DIANE MITCHELL, M.D. ,* DOUGLAS MITCHELL, M.D.,? MARTIN DAVIDSON, M.D.,* MARINA VERNALIS, D.O.,§ FRED EDWARDS, M.D.,11 ROBERT PARK, M.D.,* AND DANNY BARNHILL, M.D.*
Gynecologic Oncology Service, *Department of Obstetrics and Gynecology, TDepartment of Medicine, $Department of Pathology, BEchocardiography Laboratory, and I(Thoracic Surgery Service, Walter Reed Army Medical Center, Washington, D. C. 20307
Received January 15, 1991
A patient who had a S-year history of a low-grade nongenital pelvic leiomyosarcoma was evaluated for worsening dyspnea, hy- pertension, and jugular venous distension. An echocardiogram revealed a large right atria1 mass. At surgical exploration, met- astatic leiomyosarcoma was found within the inferior vena cava extending from below the renal veins up into the right atrium. Using cardiopulmonary bypass with profound hypothermia and circulatory arrest, the inferior vena cava was opened below the renal veins, and the tumor was transected. That portion of the tumor above this transection was then extracted through a right atriotomy. Resection of the pelvic tumor was not thought to be feasible. The patient remains asymptomatic with stable pelvic tumor 1 year after the procedure. o 1~1 Academic PISS, IIIC.
Soft tissue sarcomas are rare malignancies comprising 0.7% of all cancers in adults [l-3]. Only 15% of soft tissue sarcomas originate in the retroperitoneal space, and few of these will be detected as a pelvic mass on routine examination in the female patient [1,3]. The treatment for soft tissue sarcomas is generally accepted to be com- plete surgical exeision, including the performance of rad- ical procedures if necessary, to obtain clear margins [1,3]. Metastases may occur at a variety of distant sites; how- ever, metastasis of a retroperitoneal soft tissue sarcoma to the heart has not previously been reported. An ag- gressive approach to the diagnosis and treatment of these lesions may produce long-term survivors. This report pre- sents a patient with a pelvic low-grade leiomyosarcoma metastatic to the vena cava and heart that was surgically treated with satisfactory results.
’ The opinions and assertions contained herein are those of the au- thors and are not to be construed as official or as representing the views of the Department of the Army, the Department of Defense, or the United States Public Health Service.
CASE REPORT
The patient was a 48-year-old White female, when she underwent an exploratory laparotomy for a pelvic mass. She had previously had a total abdominal hysterectomy at age 42 for a symptomatic fibroid uterus. At the ex- ploratory surgery, she was found to have a solid retro- peritoneal mass extending from the right pelvic sidewall anteriorly to the bladder. The mass was completely re- sected. The visibly normal ovaries were not removed. Histologically, with zero to one mitosis per 10 high power fields, this tumor was identified as a low-grade leiomy- osarcoma. One month later, the patient was referred to Walter Reed Army Medical Center, where her exami- nation revealed an 8 x lo-cm solid right-sided pelvic mass. Fine-needle aspiration confirmed the diagnosis of persistent leiomyosarcoma. The patient’s earlier hyster- ectomy specimen was reviewed, and only benign leio- myomata were identified. She was treated with 4500 rad whole pelvis irradiation, and the mass decreased in size to 4 x 6 cm. Because of the apparent adherence to the bladder and since she had failed one operation and ra- diation therapy, a pelvic exenteration was recommended. At exploration, the frozen section evaluation of an en- larged para-aortic lymph node was thought to be con- sistent with metastatic tumor, so the planned exenteration was aborted. On later review of the permanent sections of that lymph node, only benign nodal angiomatosis was identified. The patient declined reoperation or other ad- juvant therapy. Over the next 5 years, the mass slowly increased in size to 8 x 10 cm, but the patient remained asymptomatic on no treatment.
At age 53, the patient presented with a lo-month his- tory of a pounding sensation in her neck and with what
84 0090-8258/91 $1.50 Copyright 0 1991 by Academic Press, Inc. All rights of reproduction in any form reserved.
CASE REPORT 85
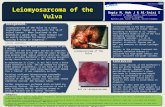
FIG. 1. Two-dimensional echocardiogram showing the tumor (T) within the right atrium. The left atrium (LA), right ventricle (RV), and left ventricle (LV) are clearly seen.
appeared to be visible carotid artery pulsations. Five gressive dyspnea on exertion accompanied by a 14-pound months prior to admission, she had developed new onset weight gain. On admission, she was found to have a blood hypertension that required medical management, and, 6 pressure of 160/110 and a grade III/VI pansystolic cardiac weeks prior to evaluation, she began experiencing pre murmur at the left sternal border radiating to the axilla
FIG. 2. The tumor after excision from the heart and vena cava.
MITCHELL ET AL.
FIG. 3. Photomicrograph of the retroperitoneal leiomyosarcoma metastatic to the heart (x300).
and increasing with inspiration. There was a midsystolic “plop” and prominent jugular venous distension with ac- centuated “a” waves. No hepatomegaly was detected. The pelvic tumor was noted to be 8 x 10 cm. There was trace ankle edema. The chest X ray and the routine lab- oratory values were normal. The electrocardiogram was unremarkable. A transthoracic two-dimensional echocar- diogram demonstrated an 8 x lo-cm right atria1 mass extending distally into the inferior vena cava (Fig. 1). The mass prolapsed through the tricuspid valve into the right ventricle during diastole. The patient was taken to surgery for removal of the cardiac mass under total circulatory arrest. At that operation, the tumor was found to extend up the inferior vena cava, from below the level of the bifurcation of the common iliac veins, into the right atrium, and through the tricuspid valve into the right ventricle, The inferior vena cava was opened below the level of the renal veins, and the tumor was transected. The vena cava itself was cross-clamped at that level with a vena cava clip to retard subsequent propagation of the tumor into the inferior vena cava. Although intravascular tumor was left below the clip, all of the remaining tumor mass was extracted from the inferior vena cava and heart
through a right atriotomy (Fig. 2). Resection of the pelvic tumor was not thought to be feasible. The patient had an uneventful postoperative recovery. One year after this surgery, and six years after the original diagnosis, she remains asymptomatic on no therapy and has stable pelvic disease.
Histologically, the tumor was identical to the previously diagnosed leiomyosarcoma of the retroperitoneum. It was composed of interlacing bundles of spindle-shaped cells with abundant eosinophilic, often fibrillar, cytoplasm (Fig. 3). The nuclei were elongated and had blunt ends. Focal epithelioid features, as well as tumor necrosis, were found. Atypia and nuclear pleomorphism were not con- sistently noted, although they could be found focally. There was less than one mitotic figure per 10 high power fields.
DISCUSSION
The initial treatment for retroperitoneal leiomyosar- comas is complete excision [l-3]. Radical or ultraradical operations may be necessary to obtain clear surgical mar-
CASE REPORT 87
gins. In addition to surgery, patients may also be treated with radiation and chemotherapy, although the efficacy of these modalities is somewhat uncertain [4]. The patient in this report had only a partial response to radiation therapy after excision of the primary tumor. She later declined an exenterative procedure.
Metastasis from a retroperitoneal leiomyosarcoma to the heart has not previously been published; however, cases of cardiac metastases from uterine leiomyosarcomas have been reported [5-111. Forty percent of those patients died as a result of their cardiac disease. In the successfully treated patients, two-dimensional echocardiography was highly effective in detecting tumor within the chambers of the heart [6,8-lo]. The patients who survived were treated by surgically removing the tumor from the heart.
The prognosis of patients with a soft tissue sarcoma is related to tumor grade, site, and size and lymph node involvement [l-3]. Mitotic activity seems to be the best predictor of behavior. Higher mitotic rates generally por- tend a more aggressive course; however, even tumors with less than one mitotic figure per 10 high power fields may metastasize.
Patients with a slowly growing, low-grade retroperi- toneal leiomyosarcoma who also have maintained a high performance status over a prolonged period of time should have prompt evaluation of cardiovascular symp- toms since they may be related to resectable cardiac me- tastases. The two-dimensional echocardiogram is the cur- rently recommended study to identify intracardiac tumor.
These patients should have surgical therapy aimed at re- section of all intravascular and cardiac disease if possible.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
REFERENCES
Adam, Y., Oland, J., Halvey, A., and Reif, R. Primary retroper- itoneal soft-tissue sarcomas, J. Surg. Oncol. 25, 8-11 (1984). DeVita, V., Hellman, S., and Rosenberg, S. Cancer, principles and practice of oncology, Lippincott, Philadelphia (1989). Zhang, G., Chen, K., Manivel, C., and Fraley, E. Sarcomas of the retroperitoneum and genitourinary tract, J. Ural. 141, 1107-1110 (1989). Hashimoto, H., Tsuneyoshi, M., and Enojoji, M. Malignant smooth muscle tumors of the retroperitoneum and mesentery: A clinico- pathologic analysis of 44 cases, J. Surg. Oncol. 28, 177-186 (1985). Rosenblatt, W., and Featherston, W. Metastatic leiomyosarcoma of the heart, Am. J. Cardiol. 6, 672-677 (1960). Keir, P., and Keen, G. Secondary leiomyosarcoma of the right ventricle: A surgical report, Br. Heart J. 40, 328-330 (1978).
Martin, J., and Boak, J. Cardiac metastasis from uterine leiomy- osarcoma, J. Am. Coil. Cardiol. 2, 383-386 (1983). Lang, R., Borow, K., and Neumann, B. Metastatic carcinoma in- volving the left atrium, Am. Heart 1. 11, 884-886 (1986).
Moreno-Cabral, R., Fukuyama, O., Powell, W., Gold, S., and McNamara, J. Surgical resection of giant metastatic leiomyosarcoma of the heart, J. Thorac. Cardiovusc. Surg. 94, 447-448 (1987). Hoy, G., Boucher, R., and Brody, A. Uterine leiomyosarcoma with cardiac metastases, Canad. J. Surg. 31, 418-420 (1988).
Tominga, K., Shinkai, T., Eguchi, K., Saijop, N., Sasaki, Y., Beppu, Y., and Nishikawa, K. The value of two-dimensional ech- ocardiography in detecting malignant tumors in the heart, Cancer 58, 164-1647 (1986).