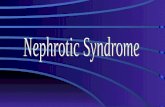
Nephrotic syndrome
-
Upload
amaka-okeukwu -
Category
Documents
-
view
86 -
download
3
Transcript of Nephrotic syndrome
Is secondary phenomena that occur when substantial amts of protein are lost in the urine
Characterised by• Proteinuria >3.5g/24hrs(urine may be
frothy)• Hypoalbuminaemia < 30g/L• Oedema & Generalised fluid retention• Hyperlipidaemia• Intravascular volume depletion with
hypotension/expansion with HTN, may occur
Pathogenesis
Excessive permeability of plasma proteins - >> heavy proteinuria
Depletion of plasma proteins , mainly albumin – hypoalbuminaemia
Liver compensates but not successful - >> reversed A:G ratio
Reduced albumin -> decreased colloid oncotic pressure of the blood -> oedema
Increased Lipoprotein synthesis and decreased catabolism by liver ->> Hyperlipidaemia (mainly VLDL and /or LDL)
HDL is also lost in urine when heavy proteinuria occurs
Loss of body proteins (immunoglobulins /complement) -> frequent infection
Loss of anticoagulants antithrombin III , antiplasmin - > thrombotic and embolic phenomenon
Causes
PRIMARY• Minimal change disease• Membranous glomerulonephritis
• Mesangial proliferative glomerulonephritis• Focal & segmental glomerulosclerosis• Mesangiocapillary glomerulonephritis
Causes
Secondary• Infection: Bacteria
endocarditis,Malaria,Syphilis,Hepatitis B,HIV
• Connective tissue diseases: SLE,Rheumatoid arthritis
• Neoplasms: Hodgkin’s lymphoma,Carcinomas,Leukaemias
• Metabolic: DM,Amyloidsis• Drugs & toxins: Captopril,gold,Mercury
The diseases the cause Nephrotic syndrome all affect the glomerulus
Mechanism:
• injury to podocytes
• Changed architecture
Scarring
Deposition of matrix or other elements
Clinical Presentationsfluid retention ->abdominal distention,ascites,edema,puffy eyelids ,scrotal swelling,weight gain,shortness of breath
Anorexia
Hypertension
Oliguria
Orthostatic hypertension
Foamy urine
Periorbital edema
Pitting edema of lower limbs
Investigations
1.Urine analysis:
Protein : creatinine ratio in a spot sample of urine (PCR>100mg/mL - substantial)
proteinuria > 3.5g/L
Estimate 24 hour albumin excretion (ACR>70 mg/ml)
RBC casts and WBC in glomerulonephritis
Urea and creatinine may be elevated <- renal failure
2.Estimate serum cholesterol concentrations
3.Total cholesterol & LDL- cholesterol elevated in most patients. HDL- cholesterol is normal or decreased.
4. Blood sugar & glycosylated hemoglobin tests for diabetes.
5. Hepatitis B and C serology, HIV serology
6. Renal biopsy if cause is not clear especially in an adult patient.
Management
• Treatment of nephrotic syndrome involves three steps:
1.Measures to reduce proteinuria
2.Measures to control complications of nephrotic syndrome
3.Treatment of underlying cause
Measures to reduce proteinuria
• If immunosuppressive drugs and other measures against the underlying cause do not benefit the patient
1.ACE inhibitors -> proteinuria, intraglomerular pressure -> slows rate of progression of renal failure. Prevents development of haemodynamically mediated FSG
2.NSAIDs -> proteinuria
Measures to control complications of nephrotic syndrome
• Oedema -> salt restriction, rest, judicious use of diuretics
• In severe cases -> I.V. salt-poor albumin• Dietary proteins 0.8-1.0g/kg• Vitamin D supplementation• Hyperlipidaemia -> dietary restrictions,
lipid-lowering drugs• Anticoagulants in patients with DVT or
arterial thrombosis
Measures to treat the underlying disease
Minimal Change Disease•Children – corticosteroids (prednisolone 60mg/m2 x 4wks, followed by alternate day prednisolone 35mg/m2 for 4 additional wks)Children responding to steroid treatment in 1st 4 wks – “steroid responsive”, those who relapse on withrawal –” steroid dependent”•Patients with frequent relapses -> cyclophosphamide 2mg/kg/day x 6 wks
Focal and segmental glomerulosclerosis
•Steroids (20-30% cases)
•Cylophosphamide, cyclosporin
Membranous glomerulonephritis
•Spontaneous remission (40%)
•30-40% cases remit and relapse repeatedly
•Rest 10-20% patients develop progressive renal failure -> cyclophosphamide, cyclosporin and chlorambucil in combination with steroids may retard progression