Nephrotic syndrome
-
Upload
tosif-ahmad -
Category
Health & Medicine
-
view
149 -
download
4
Transcript of Nephrotic syndrome

By
Dr.Tosif Ahmad
TMO-Pediatrics

Case PresentationA 3-year-old boy who presents to the
pediatric unit with a 2- day history of
puffy eyes. He was initially prescribed
antihistamines by some one but these
have not helped. He is otherwise well.
He is on no other medication. There
is no family history of renal problems.

ExaminationHe looks well and is apyrexial. He has puffy
eyes and pitting pedal oedema. Pulse is 112 beats/min, blood pressure is 103/70 mmHg and capillary refill is 2 s. There is no abdominal distension, tenderness or organomegaly. However, his scrotum appears oedematous. Respiratory rate is 28 breaths/min and there are no respiratory signs.

INVESTIGATIONS Haemoglobin 13.2 g/dL
White cell count 11.7 109/L
Platelets 372 109/L
Sodium 142 mmol/L
Potassium 4.2 mmol/L
Urea 6.3 mmol/L
Creatinine 59 μmol
Alkaline phosphatase 372 U/L
Bilirubin 17 μmol/L (1 mg%)
Alanine aminotransferase (ALT) 37 U/L

INVESTIGATIONS Urine dipstick
Blood - nil
Protein - 4+
Leucocytes - nil

Diagnosis

Nephrotic syndromeNephrotic syndrome, a manifestation of
Glomerular disease, is characterized by nephrotic range proteinuria and the triad of clinical findings associated with large urinary losses of protein: hypoalbuminemia, edema, and hyperlipidemia.

Nephrotic syndromeNephrotic range proteinuria is defined as
protein excretion of > 40mg/m2/hr or a first morning protein : creatinine ratio of > 2:1.
The underlying abnormality in nephroticsyndrome is an increased permeability of the glomerular capillary wall, which leads to massive proteinuria and hypoalbuminemia.

Nephrotic syndromeThe annual incidence is 2-3 cases per
100,000 children per year in most western countries and higher in under developed countries.

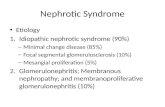
EtiologyMost children with nephrotic syndrome
have a form of primary or idiopathic nephrotic syndrome. Glomerular lesions associated with idiopathic nephroticsyndrome include minimal change disease, focal segmental glomerulosclerosis, and membranoproliferative glomerulonephritis.

EtiologyNephrotic syndrome may also be secondary
to systemic disease such as SLE, HSP, leukemia, lymphoma, hepatitis, HIV, malaria and drugs.

Idiopathic Nephrotic Syndrome
Approximately 90% of children with nephrotic syndrome have idiopathic nephrotic syndrome. Idiopathic nephroticsyndrome is associated with primary glomerular disease without evidence of a specific systemic cause.

Idiopathic nephrotic syndrome includes multiple histologic types: minimal change disease, mesangial proliferation, focal segmental glomerulosclerosis, membranous nephropathy, and membranoproliferativeglomerulonephritis.

CLINICAL MANIFESTATIONSThe idiopathic nephrotic syndrome is more
common in boys than in girls (2 : 1) and most commonly appears between the ages of 2 and 6 yr. However, it has been reported as early as 6 mo of age and throughout adulthood.

Children usually present with mild edema, which is initially noted around the eyes and in the lower extremities.
With time, the edema becomes generalized, with the development of ascites, pleural effusions, and genital edema. Anorexia, irritability, abdominal pain, and diarrhea are common

Important features of minimal change idiopathic nephrotic syndrome are the absence of hypertension and gross hematuria.

Differential diagnosisProtein-losing enteropathy
Hepatic failure
Heart failure
Acute or chronic glomerulonephritis
Protein malnutrition

DIAGNOSIS Urinalysis reveals 3 + or 4 + proteinuria.
A spot urine protein:creatinine ratio exceeds 2.0.
Urinary protein excretion exceeds 40 mg/m 2 /hr.
Serum albumin level is < 2.5 g/dL.
Serum cholesterol and triglyceride levels are elevated. Serum complement levels are normal.

DIAGNOSISChildren with features that make MCNS less
likely (gross hematuria, hypertension, renal insufficiency, hypocomplementemia, or age < 1 yr or > 8 yr) should be considered for renal biopsy.

TREATMENTSupportive
Prednisolone
Cyclophosphamide
Cyclosporine
Tacrolimus
Mycophenolate

TREATMENT A subset of patients relapse while on alternate-day
steroid therapy or within 28 days of completing a successful course of prednisone therapy. Such patients are termed steroid dependent. Patients who respond well to prednisone therapy but relapse ≥ 4 times in a 12-mo period are termed frequent relapsers. Children who fail to respond to prednisone therapy within 8 wk of therapy are termed steroid resistant

TREATMENTSteroid-dependent patients, frequent
relapsers, and steroid resistant patients are candidates for alternative therapies, particularly if the child has severe corticosteroid toxicity.

COMPLICATIONS Spontaneous bacterial peritonitis
Sepsis
Pneumonia
Cellulitis
Urinary tract infections
Thromboembolic events.
Pleural effusion, Pericardial effusion.
Complications of treatment.

PROGNOSISChild with steroid responsive nephrotic
syndrome is unlikely to develop chronic kidney disease.
Most children with steroid-responsive nephrotic syndrome have repeated relapses, which generally decrease in frequency as the child grows older.

PROGNOSISChildren with steroid-resistant nephrotic
syndrome, most often caused by FSGS, generally have a much poorer prognosis. These children develop progressive renal insufficiency, ultimately leading to end-stage renal disease requiring dialysis or kidney transplantation.

PROGNOSISNephrotic syndrome (massive proteinuria,
hypoalbuminemia, edema, and hypercholesterolemia) has a poorer prognosis when it occurs in the 1st yr of life, when compared to nephrotic syndrome manifesting in childhood.