NEJMe1012071 Genetica Epigenetica y Leucemia
-
Upload
erickmattos -
Category
Documents
-
view
217 -
download
3
description
Transcript of NEJMe1012071 Genetica Epigenetica y Leucemia
-
T h e n e w e ngl a nd j o u r na l o f m e dic i n e
n engl j med 363;25 nejm.org december 16, 20102460
Genetics, Epigenetics, and LeukemiaKevin Shannon, M.D., and Scott A. Armstrong, M.D., Ph.D.
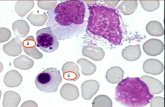
In this issue of the Journal, Ley and colleagues1 report that somatic mutations in a gene encoding a DNA methyltransferase, DNMT3A, are common in adults with acute myeloid leukemia (AML). They also report that these mutations are associ-ated with discrete molecular and cytogenetic features that have prognostic significance. These findings have implications for clinical investiga-tors, for researchers working to characterize the molecular mechanisms that contribute to leuke-mic growth, and, more broadly, for illuminating mechanisms of epigenetic reprogramming in cancer cells.
Ley et al. sequenced the genome of leukemia cells from a patient with AML and observed a DNMT3A mutation. They went on to analyze a large and well-annotated panel of adult AML samples, of which 22% turned out to carry a somatic DNMT3A mutation. Most patients with AML with DNMT3A mutations were classified as having an intermediate risk of treatment failure on the basis of cytogenetic features at diagnosis. Often, their leukemias also carried mutations in other genes that are commonly altered in AML (IDH1, IDH2, FLT3, and NPM1). The authors did not detect DNMT3A mutations in leukemias with a PML-RARA translocation or other transloca-tions associated with a relatively favorable clini-cal outcome. Most important for clinicians who care for patients with AML, the authors showed that mutations in DNMT3A are a strong and in-dependent predictor of relapse.
These new data and a previous investigation of AML2 underscore the power of whole-genome sequencing studies to uncover new molecular le-sions in cancer. The findings also support the sequencing of AML genomes of patients with high-risk disease, for which there is a paucity of molecular data.
Because Ley et al. analyzed archival specimens from patients who received similar anticancer therapies, they were able to perform statistical analyses to determine whether the mutation sta-tus affected the outcome. However, more research is required before these results can be directly translated into clinical practice. The prevalence and prognostic significance of DNMT3A muta-
tions with AML must now be determined in ad-ditional patients; the prevalence reported by Ley et al. is higher than that observed in a smaller series, albeit with the use of a different ap-proach.3 Analyzing pediatric AML samples will also be important, since it is conceivable that the presence of a DNMT3A mutation in this con-text could inform the decision of when to per-form allogeneic hematopoietic stem-cell trans-plantation (HSCT) during first remission. Ley et al. found that patients with DNMT3A mutations who underwent HSCT had better outcomes. Fi-nally, as inhibitors of mutant proteins such as FLT3 and other new therapies are tested in pa-tients with AML, it will be essential to continu-ally reassess the effect of DNMT3A mutations on response and resistance.
The DNMT3A protein is a member of a fam-ily of methyltransferase enzymes that catalyze the addition of methyl groups to DNA in which the sequence contains CpG dinucleotides. DNA methylation at CpG islands that are located near genes regulates gene expression. DNMT3A and DNMT3B initiate most DNA methylation, where-as DNMT1 maintains a stable methylation pat-tern. The DNMT3A mutations found in AML fall into two classes: those likely to abrogate protein function and those that effect an amino acid substitution of arginine at position 882 of the protein (R882). The clinical and biologic features of patients with both types of mutation are sim-ilar, with the exception that patients with R882 mutations have higher blood leukocyte counts at diagnosis. Amino acid substitutions at R882 impair, but do not eliminate, DNMT3A methyl-transferase activity.3 In the vast majority of pa-tients, a single DNMT3A allele is mutated, consis-tent with the observation of residual DNMT3A expression in every AML sample examined by Ley et al.
What are the probable functional conse-quences of these somatic DNMT3A mutations? The most plausible model is that DNMT3A is a tumor-suppressor gene and that its mutation contributes to leukemogenesis, drug resistance, or both by reducing global DNMT3A methyl-transferase activity. This, in turn, could result in
The New England Journal of Medicine Downloaded from nejm.org on December 25, 2010. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
-
editorials
n engl j med 363;25 nejm.org december 16, 2010 2461
reduced repression of one or more genes critical to the normal balance of self-renewal, prolifera-tion, and differentiation of hematopoietic stem cells (HSCs). Consistent with this idea are recent studies showing that DNA methylation profiles change as blood cells develop from HSCs and that the ablation of Dnmt1 in mice perturbs HSC self-renewal and hematopoietic cell-fate deci-sions.4-6 Ley et al. did not observe DNMT3A muta-tions in AML samples with translocations in-volving genes (such as MLL and RARA) that regulate HSC fate by modulating gene expres-sion. Perhaps each of these alterations impairs differentiation and leads to unregulated self-renewal or proliferation through mechanisms that impinge on overlapping pathways. The ab-sence of global changes in DNA methylation in DNMT3A-mutated AML samples indicates that establishing how these mutations contribute to leukemogenesis will require much work.
Advances in our understanding of the molecu-lar pathogenesis of AML have yet to be translated into more effective and less toxic treatments, and the therapeutic backbone of intensive cytarabine and anthracycline chemotherapy has not changed during the past 30 years. It is unclear how the finding of DNMT3A mutations in AML might lead to novel therapeutic approaches. Like other loss-of-function mutations in cancer, DNMT3A mutations do not result in the production of a protein that lends itself to direct chemical inter-vention. These mutations probably contribute to leukemic growth by modulating a highly inter-dependent network of epigenetic processes, such as DNA methylation, histone methylation, and histone acetylation. As we learn more about how such mutations deregulate cell fates, it may be feasible to develop drugs that reverse the aber-rant epigenetic programs in AML and other can-cers. Clinical trials of DNA methyltransferase inhibitors and histone deacetylase inhibitors are under way in patients with AML, and it now be-comes critical to assess whether the presence of a DNMT3A mutation influences the clinical re-sponse to these agents.
The discovery of DNMT3A mutations in AML and recent reports of mutations in genes encod-ing histone-modifying enzymes in cancers7-10
suggest that the global patterns of aberrant epi-genetic modifications that are seen in some can-cers may result from acquired mutations in genes that control this process. These mutations are found in primary cancer cells, implying that ab-errant methylation contributes directly to tumor growth rather than reflecting the maturation state of the tumor-initiating cell. Extended screen-ing of cancers for mutations in DNMT3A and other genes that encode enzymes involved in re-versibly modifying chromatin will probably pro-vide new insights into mechanisms of epigenetic reprogramming in cancer and may inform inno-vative therapeutic approaches to reverse the un-derlying aberrant gene-expression programs.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
From the Department of Pediatrics and Comprehensive Cancer Center, University of California at San Francisco, San Francisco (K.S.); and the Department of Pediatric Oncology, DanaFar-ber Cancer Institute; the Department of Medicine, Childrens Hospital Boston; and Harvard Medical School all in Boston (S.A.A.).
This article (10.1056/NEJMe1012071) was published on Novem-ber 10, 2010, at NEJM.org.
1. Ley TJ, Ding L, Walter MJ, et al. DNMT3A mutations in acute myeloid leukemia. N Engl J Med 2010;363:2424-33.2. Mardis ER, Ding L, Dooling DJ, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med 2009;361:1058-66.3. Yamashita Y, Yuan J, Suetake I, et al. Array-based genomic resequencing of human leukemia. Oncogene 2010;29:3723-31.4. Ji H, Ehrlich LI, Seita J, et al. Comprehensive methylome map of lineage commitment from haematopoietic progenitors. Nature 2010;467:338-42.5. Trowbridge JJ, Snow JW, Kim J, Orkin SH. DNA methyltrans-ferase 1 is essential for and uniquely regulates hematopoietic stem and progenitor cells. Cell Stem Cell 2009;5:442-9.6. Brske AM, Vockentanz L, Kharazi S, et al. DNA methylation protects hematopoietic stem cell multipotency from myeloery-throid restriction. Nat Genet 2009;41:1207-15.7. Nikoloski G, Langemeijer SM, Kuiper RP, et al. Somatic mu-tations of the histone methyltransferase gene EZH2 in myelodys-plastic syndromes. Nat Genet 2010;42:665-7.8. van Haaften G, Dalgliesh GL, Davies H, et al. Somatic muta-tions of the histone H3K27 demethylase gene UTX in human cancer. Nat Genet 2009;41:521-3.9. Morin RD, Johnson NA, Severson TM, et al. Somatic muta-tions altering EZH2 (Tyr641) in follicular and diffuse large B-cell lymphomas of germinal-center origin. Nat Genet 2010;42: 181-5.10. Ernst T, Chase AJ, Score J, et al. Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nat Genet 2010;42:722-6.Copyright 2010 Massachusetts Medical Society.
The New England Journal of Medicine Downloaded from nejm.org on December 25, 2010. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.