Multidrug Resistant Pseudomonas (P) aeruginosa: Medical ... · Multidrug Resistant Pseudomonas (P)...
Transcript of Multidrug Resistant Pseudomonas (P) aeruginosa: Medical ... · Multidrug Resistant Pseudomonas (P)...

CentralBringing Excellence in Open Access
JSM Microbiology
Cite this article: Alnour TMS, Ahmed-Abakur EH (2017) Multidrug Resistant Pseudomonas (P) aeruginosa: Medical Impact, Pathogenicity, Resistance Mecha-nisms and Epidemiology. JSM Microbiology 5(3): 1046.
*Corresponding authorTarig MS Alnour, Department of Medical Laboratory Technology – University of Tabuk (Tabuk – KSA), Saudi Arabia, Tel: 96-6535782141; Email:
Submitted: 01 June 2017
Accepted: 20 October 2017
Published: 23 October 2017
Copyright© 2017 Alnour et al.
OPEN ACCESS
Keywords•Pseudomonasaeruginosa•Multidrug resistant•Intrinsic mechanisms of resistance•Effluxmechanism•MDRPA•Acquired mechanisms of resistance
Review Article
Multidrug Resistant Pseudomonas (P) aeruginosa: Medical Impact, Pathogenicity, Resistance Mechanisms and EpidemiologyTarig MS Alnour1* and Eltayib Hassan Ahmed-Abakur2
1Department of Medical Laboratory Technology, University of Tabuk, Saudi Arabia2Department of Medical Laboratory Science, Alzeaim Alazhari University, Sudan
Abstract
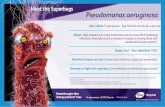
Drug resistant bacteria which are known as super bugs are challenging worldwide problems as they increase the costs of hospitalization, uses of highly toxic drugs and may associated with high mortality rate. Multidrug resistant Pseudomonas aeruginosa (MDRPA) is one of the most important drug resistant strains. This review handling the frequency of MDRPA, risk factors and resistance mechanisms associated with MDRPA. It’s naturally known that P. aeruginosa express a high resistant manner, this attributed to loss of membrane permeability, efflux pumping of the antimicrobial agents and acquired resistant through acquisition of resistance genes in addition to its virulence factors which contribute to the resistance mechanisms. The frequency of MDRPA ranged from 12-36% of isolated P. aeruginosa from different location of the world. It’s highly recommended to focus on drug resistance mechanisms for all microorganisms especially MDR P. aeruginosa to avoid having untreatable infection and superbugs.
INTRODUCTIONPseudomonas (P) aeruginosa has been recognized as a
ubiquitous organism because of its extraordinary survival and adaptation abilities in a wide range of environments such as soil, water, sewage and hospitals [1-3].The organism is able to multiply in various water sources such as seawater, rivers water, and even bottled water [4]. In addition to, it’s highly resistance to several antibiotics and disinfectants [1].
P. aeruginosa is a Gram-negative aerobic bacillus belongs to the Pseudomonadaceae family. It is a small microorganism, straight or slightly curved non-fermenting glucose and not sporulated. It has motility due to a single polar flagellum and twitching [5]. Its identification in the laboratory is simple, because the organism grows easily in a wide variety of media and the requirements for its identification are scarce. Most cultures of this bacterium produce a blue-green pigment pyocyanin; it is useful for identification of the microorganism, and because of the characteristic color of copper oxide, the bacteria are named aeruginosa [5]. Because of its ubiquitous nature, ability to survive in moist environments which makes the wards encouraging bacterial growth, and innate resistance to many antimicrobial agents and antiseptics, P. aeruginosa is a leading cause of nosocomial infections [2,3,6] ranking second among the gram-negative pathogens reported to the National Nosocomial Infection Surveillance System [2,6].
Among all gram-negative bacteria, P. aeruginosa has been considered a predominant opportunistic pathogen, which usually infects persons having some underlying diseases and compromised immune status [1,2].
This study aimed to review the pathogenicity, mechanisms of resistance, risk factors of having multi-drug resistance, medical impact and epidemiology of P. aeruginosa.
PATHOGENICITYP. aeruginosa possesses several virulence factors which aid
in its pathogenicity and resistance to antimicrobial agents. These include:
Flagellum and type IV pili
Each P. aeruginosa cell possesses a single polar flagellum and several much shorter type IV pili also localized at a cell pole. Flagellins in P. aeruginosa perform several functions during host infection. Apart from enabling motility, the flagellum of P. aeruginosa plays an indirect role in membrane permeabilization and surfactant protein mediated bacterial clearance. Flagellins are classified into two types: Type-a (polymorphic glycosylated) and type-b (non-glycosylated). Similarly, pili are involved during inflammation due to glycosylation in the interface between pili and host cells. [2]. Type 4 pili are arguably the most important adhesions of P. aeruginosa and are also involved in twitching motility and the formation of biofilms, it extend and retract like

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 2/8
grappling hooks to pull the cell along solid surfaces by a process termed ‘twitching motility’. Pili can also lead to aggregation, causing the bacteria to form micro-colonies on target tissues, effectively concentrating the bacteria in one location and potentially offering protection from the host immune system and from antibiotics. Pilin-deficient mutants or those impaired in twitching motility demonstrate reduced virulence in various models [7].
Type 3 secretion system (T3SS)
P. aeruginosa synthesizes a secretory apparatus (Type III) that allows it to inject toxins from their cytoplasm into the target cell; T3SS are shared among many pathogenic Gram-negative bacteria. The latter mechanism allows mucoid bacteria to lyse the host’s macrophages and overcome various defense such as in the case of cystic fibrosis lung infection [2]. P. aeruginosa T3SS is a major determinant of virulence, and its expression is frequently associated with acute invasive infections and has been linked to increased mortality in infected patients. The needle-like appendage of the T3SS, evolutionarily related to flagella, permits the translocation of effector proteins from the bacterium into the host cell through a pore formed in the host cell membrane. The exact contribution of each of the toxins to pathogenesis is unclear, but it is thought that the T3SS may allow Pseudomonas to exploit breaches in the epithelial barrier by antagonizing wound healing during colonization and to promote cell injury [7].
Hemolytic activities and pigmentation
P. aeruginosa are hemolytic on blood agar plates, and several different hemolysins have been described. A heat-stable hemolytic glycolipid has been purified; it is toxic to alveolar macrophages. Moreover, P. aeruginosa strains isolated from respiratory tract infections yield more hemolysin than do environmental strains, indicating that this glycolipid hemolysin may play a role in P. aeruginosa pulmonary infections [8].Several heat-labile protein hemolysins also have been described. One of these hemolysins may be identical to phospholipase C which hydrolyzes lecithin. Some strains of P. aeruginosa produce a thermolabile protein (leukocidin), which lyses leukocytes [8,9]. Most strains of P. aeruginosa also produce one or more pigments, the most common being pyocyanin (a phenazine pigment) and fluorescein. These pigments are nontoxic in animals. Pyocyanin, however, retards the growth of some other bacteria and thus may facilitate colonization by P. aeruginosa [8].
Lipopolysaccharide (LPS)
The LPS is a predominant component of the outer membrane of P. aeruginosa. LPS plays a prominent role in activation the host’s innate and adaptive immune responses; and, eventually causes dysregulated inflammation responses that contribute to morbidity and mortality [9].
Some strains of P. aeruginosa produce a mucoid exopolysaccharide capsule, comprised of alginate, an acetylated random co-polymer of β 1-4 linked D-mannuronic acid and L-guluronic acid. These mucoid strains usually are isolated from patients with cystic fibrosis (CF). The overproduction of alginate is believed to play a role in cell adherence within the CF
lung and is thought to be involved in resistance to host defense by reducing susceptibility to phagocytosis, also impair diffusion of antibiotics and thus facilitate colonization and persistence. Interestingly, mucoid strains are frequently deficient in production of elastase, toxin A, and flagella, and their LPS lacks long polysaccharide side chains [8]. The small minorities of CF patients, who are carrying only non-mucoid P. aeruginosa, have significantly better lung function over time compared to those patients infected with mucoid P. aeruginosa. The tendency of P. aeruginosa to conversion to a mucoid phenotype is one of the most striking and clinically relevant features of infection by this bacterium [8]. Mucoidness phenomenon plays an important role in drug resistance patterns. The strains that showed mucoid colonies were more susceptible to antimicrobial agents than non mucoid strains [10,11]. This might be attributed to the adhesion of some antimicrobial agents to the outer membrane capsule and losing of several other virulence factors which might interfere with resistance. In general transition from non mucoid strains to mucoid ones is correlated to chronic infection [10,11].
Extracellular proteases and toxin A
P. aeruginosa strains produce extracellular protease. Three separate proteases have been purified; all are capable of digesting casein, whereas protease II, also digests elastin. They also possibly contribute to the tissue destruction that accompanies P. aeruginosa eye or lung infections and may support bacteria in tissue invasion. However, their effects appear to be localized, and they are not highly toxic to animals [8].
The most toxic known extracellular protein of P. aeruginosa is Toxin A which produced by 90 percent of all strains. Its toxicity has been attributed to its ability to inhibit protein synthesis in susceptible cells [8].
Quorum sensing
It is a mechanism of bacterial “cell-to-cell” communication via diffusible chemical compounds. A critical number of bacteria (the quorum) are required to produce a sufficient amount of a secreted signal molecule (termed an autoinducer) to trigger expression of a large regulon. Quorum sensing is known to control a number of bacterial genes. More than 300genes are regulated during quorum sensing in P. aeruginosa. Increase in bacterial density during infection leads to an increase in autoinducer concentration. When autoinducer reaches a particular threshold, it subsequently binds to transcriptional activator (LasR/RhlR) forming a complex that activates genes involved in biofilm formation and coding virulence factors. Quorum sensing has been shown to determine the tolerance of P. aeruginosa biofilms to antibiotic therapy [7,9].
Biofilm formation
P. aeruginosa is has ability to form complex structures called biofilms. Resistance to antimicrobial agents is the most important features of biofilm infections. Biofilm development is a complex process and partly controlled by quorum sensing signals. P. aeruginosa has been demonstrated to form biofilms on a variety of indwelling medical devices. It is particularly problematic for patients requiring mechanical ventilation and catheterization, as

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 3/8
the surfaces of medical devices can readily develop P. aeruginosa biofilms that are difficult to remove. Also, P. aeruginosa has been demonstrated to grow as a biofilm within the body particularly at the site of burn wounds. In addition to evasion of the host immune system, the highly antibiotic resistant nature of biofilms to killing by bactericidal antibiotics contributes to bacterial persistence in chronic infections. It has been demonstrated that cells growing in a biofilm can be up to thousand fold more resistant to antibiotics than free-swimming, planktonic cells [7,9].
Oxidant generation in the airspace
The oxidative stress refers to an imbalance in the redox status of the cell preferring an oxidizing environment. Extensive reactive oxygen species (ROS) production leads to the depletion of antioxidants and results in cellular damage. Without the protection of antioxidants, ROS can also initiate lipid peroxidation of polyunsaturated fatty acid components of cell membrane phospholipids, affecting cellular integrity, amino acids can also be damaged by ROS, leading to protein denaturation and enzyme deactivation. During the infectious process, P. aeruginosa induces ROS production within epithelial cells in a few ways. Recognition of P. aeruginosa LPS by the epithelial cells leads to ROS production other potential sources of ROS are derived from the activated epithelium. In the case of mechanical ventilation, the introduction of excess oxygen can also fuel the production of ROS. Overwhelming oxidant injury may lead to alveolar collapse and extensive fibrotic scarring, impairing gas exchange between the affected airways and the capillary system [9].
P. aeruginosa isolated from acute infections differ substantially in phenotype from those isolated from chronic infections. Isolates from acute infections express a wealth of virulence factors, while in contrast, many isolates from chronic CF lung infections lack some of the most inflammatory bacterial features, such as flagella and pili, and downregulate other virulence mechanisms such as the type 3 secretion system [7]. However during the process of infection, a number of adaptations happen leading to the characteristic persistence and antibiotic resistance of isolates found from chronic infection. Amongst the most common adaptations of P. aeruginosa found in CF isolates, is the conversion to mucoid phenotype due to overexpression of alginate. Environmental isolates usually present a non-mucoid phenotype, as P. aeruginosa penetrates the thickened mucus lining of the airways, travelling down the oxygen gradient, increased expression of alginate and a switch to a mucoid phenotype occur. This phenotype often occurs coincidently with the establishment of chronic infection and becomes stabilized by regulatory mutations. The mucoid form of P. aeruginosa is associated with 90% of P. aeruginosa CF infections compared to only 2% of P. aeruginosa non-CF infections. This phenotype is often coordinately regulated with a loss of flagella by the alternative sigma factor AlgT. The loss of flagella causes not only loss of motility, but also decreased activation of host inflammatory mediators, other easily identified morphological adaptations of P. aeruginosa include the switch from smooth to rough colony morphology and the appearance of small colony variants. The rough colony morphology is representative of strains that have lost the LPS O-antigen [9].
MULTIDRUG RESISTANCE P. AERUGINOSADefinition
Multidrug resistant pathogen was defined as a pathogen that develops resistance to at least one agent in 3 or more antimicrobial categories. Another terms which extensively used are extensive drug resistance (XDR) which defined as a pathogen resistant to one agent in all categories except 2 or less; and Pan drugresistant (PDR) which defined as a pathogen resistant to one agent in all categories[12-14].The categories which classify the anti- Pseudomonas aeruginosa antimicrobial agents include: Aminoglycoside (gentamicin, tobramycin, amikacin and netilmicin); Carbapenems (imipenem, meropenem and doripenem); Cephalosporins (ceftazidime and cefepime); Fluoroquinolones (ciprofloxacin and levofloxacin); Penicillins β-lactamase inhibitors (Ticarcillin-clavulanic acid and Piperacillin-tazobactam); Monobactams (aztreonam); Phosphonic acids (fosfomycin); Polymyxins (colistin and polymyxin B) [14].
P. aeruginosa multidrug resistance was defined as combined resistance or intermediate susceptibility to piperacillin, ceftazidime, imipenem, and ciprofloxacin. Resistance to aminoglycosides was not included in the definition, because these agents are not used as first-line single-drug therapy for P. aeruginosa infection, but, rather, in combination with 1 of the 4 antibiotics listed above [15]. Other classification involved the aminoglycosides defined multidrug resistant (MDR) P. aeruginosa phenotype as a bacterium which is resistant to three or more anti-Pseudomonal anti-microbial classes; carbapenems, fluoroquinolones, penicillins /cephalosporins and aminoglycosides [2,15,16]. Whereas the French National Technical Committee for Nosocomial Infections defined MDR-PA as a P. aeruginosa with an intermediate susceptibility or resistance to at least one of the three following antibiotics: ticarcillin, ceftazidime and imipenem [17].
Risk factors of having MDRPA
In addition to being intrinsically resistant to several antimicrobial agents, P. aeruginosa often acquires mechanisms of resistance to other antibiotics. Previous treatment with antibiotics that are characterized by high anti-pseudomonal activity and prolonged antibiotic treatment are both recognized risk factors for the emergence of drugresistant P. aeruginosa. Acquisition of strains resistant to ceftazidime, imipenem, piperacillin, or ciprofloxacin is associated with significantly longer hospital stays and an increased rate of secondary bacteremia in patients with P. aeruginosa infection [15].The increasing use of antibiotics and growing numbers of invasive procedures, together with the development of intrinsic and acquired resistance mechanisms of P. aeruginosa, cause the evolution of numerous multidrug-resistant (MDR) P. aeruginosa outbreaks in clinical settings [18].
The risk for acquiring MDR organisms may be related to the number of carriers in the same ward as well as to individual risk factors, such as patient characteristics and in-hospital events (invasive devices and antibiotic treatment).
Resistant mechanisms
Resistance to antimicrobial agents is an increasing clinical

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 4/8
problem and is a recognized public health threat. P. aeruginosa is one of the main organisms responsible for drug-resistant nosocomial infections and is a leading cause of bacteremia and nosocomial pneumonia [2,6,15,16,18]. Multidrug Resistance P. aeruginosa is naturally resistant to a significant number of antimicrobials (Ampicillin, Amoxicillin, amoxicillin/clavulanate, first-generation cephalosporins, second-generation, cefotaxime, ceftriaxone, nalidixic acid). Furthermore, they easily acquire resistance to new antibacterial agents by mutational changes or acquisition of genetic material. Emergence of MDR strains is often due to selective pressure of antimicrobial therapy. Genetic studies confirm the selection of resistant mutants and their subsequent spread. The frequent use of antibiotics has contributed to the emergence of drug resistance and the production of a variety of β-lactamases (BLs) amongst P. aeruginosa strains, which considered an important resistance mechanism observed in many bacteria [12]. Using several classes of antibiotics to treat infections caused by this bacterium might complicate the situation and lead to the emergence of new mutant strains, which have a high level of resistance to many antibiotics [5].
P. aeruginosa resistance mechanisms classified into intrinsic or acquired resistance. The intrinsic resistance includes decreases in membrane permeability, efflux mechanism pumping the antimicrobial agents outside the cell wall and production of inactivation enzymes [19].
Intrinsic pathway of resistance:
a. Membrane permeability: The outer membrane of Gram-negative bacteria including Pseudomonas is less permeable to hydrophobic agents due to the presence of lipopolysaccharide. The influx and uptake of antibiotics are slowed by Gram-negative outer membrane (OM) [20]. This membrane is an asymmetric bilayer of lipopolysaccharides (LPS) and phospholipids, into which nonspecific porins and specific uptake channels are embedded [20]. The LPS-containing bilayers are more rigid than normal bilayers, slowing passive diffusion of hydrophobic compounds, whereas narrow pores limit by size the penetration of hydrophilic drugs [20]. Aminoglycoside and colistin interact with lipopolysaccharide leading to increases in the permeability while beta-lactams and quinolones need to diffuse through certain porin channels, P. aeruginosa expresses few specific porins which allow hydrophilic molecules to pass in [19, 20]. Other Resistance Mechanisms present in P. aeruginosa is the formation of permeability barriers (OM). Impaired penetration of different substances through the membrane (e.g. imipenem) is due to diminished expression of specific OM protein. It has been shown that OM permeabilizers such as EDTA increase susceptibility to antibiotics, indicating that the lack of OprD protein leads to a reduction of active antibiotic molecules capable of reaching the target penicillin-binding-proteins [2].
b. Efflux mechanism: P. aeruginosa express several efflux pumps that expel drugs together with other substances outside the bacterial cells. Pumps may be specific for one substrate or may transport a range of structurally dissimilar compounds (including antibiotics of multiple classes); such pumps can be associated with multiple drug resistance (MDR) [20,21]. Six resistance nodulation division (RND) family efflux pumps have been described for P. aeruginosa.These efflux pumps can eject
a wide range of antibiotics; for example, MexAB–OprM and MexXY–OprM can collectively efflux b-lactams, chloramphenicol, fluoroquinolones, macrolides, novobiocin, sulfonamides, tetracycline, and trimethoprim and aminoglycosides. The b-lactamase, AmpC, is located in the periplasm and can efficiently hydrolyze several b-lactam antibiotics such as penicillins and cephalosporins. It is expressed at low levels but can be induced by sub-inhibitory concentrations of certain b-lactams. The resistance imparted by efflux pumps and AmpC is intricately connected to restricted outer membrane permeability, because the concentration of b-lactams in the periplasm is dependent on the efficiency and rate by which they are transported through the porins of the outer membrane [7]. All of these systems efflux fluoroquinolones and the RND pumps (CmeB, AcrB and the Mex pumps) also export multiple antibiotics. Cross-resistance is also a problem; exposure to any one agent that belongs to the substrate profile of a pump would favor over-expression of that pump and consequent cross-resistance to all other substrates of the pump. These may include clinically relevant antibiotics. An example of this is seen with the mexAB system of P. aeruginosa; mutants that over-produce MexAB are less susceptible, if not fully resistant to a range of antibiotics (fluoroquinolones, β-lactams, chloramphenicol and trimethoprim) but also triclosan, a commonly used household biocide [21]. The P. aeruginosa genome contains at least 10 distinct tripartite (3-protein) efflux pump system gene operons, which are energy dependent [22].
c. Antimicrobial inactivating enzymes: Hydrolysis of β-lactam antibiotics by β-lactamases is the most common mechanism of resistance for this class of antibacterial agents in clinically important Gram-negative bacteria. Because penicillins, cephalosporins, and carbapenems are included in the preferred treatment regimens for many infectious diseases. the presence and characteristics of these enzymes play a critical role in the selection of appropriate therapy [23]. All P. aeruginosa strains possess the ampC gene for the inducible chromosomal b-lactamase [24]. The β-lactams induce synthesis of a new penicillin-binding protein, PBP2a, which does not bind any β-lactam [8]. Due to more sophisticated molecular approaches than were previously available, it has become increasingly easy to obtain nucleotide sequences, with their deduced amino acid sequences, for the genes encoding these enzymes in β-lactam-resistant clinical isolates. Classification of β-lactamases has traditionally been based on either the functional characteristics of the enzymes or their primary structure. The simplest classification is by protein sequence, whereby the β-lactamases are classified into four molecular classes, A, B, C, and D, based on conserved and distinguishing amino acid motifs. Classes A, C, and D include enzymes that hydrolyze their substrates by forming an acyl enzyme through an active site serine, whereas class B β-lactamases are metalloenzymes that utilize at least one active-site zinc ion to facilitate β-lactam hydrolysis [23].Over-expression of the enzyme results from spontaneous mutation in the regulatory gene, ampR. Over-production of the ampC b-lactamase poses a particular threat to cephalosporins. Other b-lactamases produced by P. aeruginosa include extended-spectrum plasmid-mediated enzymes (ESBLs) active against penicillins and cephalosporin [24,25]. Use of b-lactamase inhibitors (clavulanic acid with ticarillin and tazobactam with

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 5/8
piperacillin) provides protection of these antibiotics against some of the plasmid-mediated enzymes, but not the ampC enzyme [24].
Acquired resistance: Acquired resistance is a consequence of mutational changes or the acquisition of resistance mechanisms via horizontal gene transfer and can occur during chemotherapy [26]. The main way of acquiring drug resistance in MDRPA is through acquiring plasmid. Plasmid mediated resistance has been documented by several authors [26-30]for the genetic transfer of several drug resistance genes.
It has become increasingly clear that resistance development in P. aeruginosa is multifactorial, with mutations in genes encoding porins, efflux pumps, penicillinbinding proteins, chromosomal β-lactamase and aminoglycoside modifying enzymes all contributing to resistance to β-lactams, carbapenems, aminoglycosides, and fluoroquinolones [2,3].
Falagas and kopterides 2006 carried out a systemic review, and searched in pubmed for 20 years they found that the carbapenems and fluoroquinolones are implicated MDR of P.aeruginosa [17]. Moreover, such drug as ampicillin makes the individuals more susceptible to Pseudomonas gastrointestinal infection probably results from suppression of normal intestinal flora, which would allow Pseudomonas to colonize [30,31].The increased use of carbapenems in hospitalized patients contributes to an increased selective pressure on nosocomial microorganisms, which favors the selection of bacterial subpopulations with reduced sensitivity or resistance to these antimicrobial agents [12].
Extended-spectrum beta-lactamases (ESBLs) that can confer resistance to cephalosporins are common in Enterobacteriaceae and have spread worldwide. Various class A ESBLs, such as TEM-, SHV-, VEB-, and PER-type ESBLs, and class D ESBLs such as OXA-type ESBLs have been identified in P. aeruginosa [3,18]. Antibiotic resistance is on the rise due to gene dissemination via horizontal transfer. Horizontal gene transfer via integrons, is responsible for multi-drug resistance in many gram-negative bacteria particularly P. aeruginosa [32].
Integrons are genetic elements encoding the components of a site specific recombination system that recognizes mobile gene cassettes, mostly resistance determinants [5]. It is potentially a major agent in the dissemination of multidrug resistance among gram-negative bacteria and Pseudomonas [32-34]. Class I integrons are predominant among integrons that carry resistance cassettes [32,35] and have a threatening potential for the development of antimicrobial resistance and the emergence of MDR profiles in clinical bacteria. Several resistance gene cassettes are associated with class I integrons in P. aeruginosa that confer resistance to antimicrobial agents. Typically, a class I integron is composed of a 5’-conserved segment (5’CS) including the integrase gene (intI), and a 3’-conserved segment (3’CS) encoding resistance to sulfonamides and disinfectants [32,35]. Previous studies of P. aeruginosa clinical isolates reported that acquired resistance to carbapenems resulted from the complex interaction of several mechanisms, including loss of the OprD porin, overexpression of efflux systems (MexAB-OprM, MexEF-OprN), and production of carbapenemase activity. The most frequent causes of OprD mutational inactivation were frameshift mutations produced by insertion, deletions, and point mutations,
leading to the creation of premature stop codons occurring in numerous isolates. These genetic events were located on the whole OprD gene [19]. The capability of P. aeruginosa to generate resistance against commonly-used broad-spectrum antibiotics contributes greatly in its notorious fame. This organism can combat against these drugs because of its ability to acquire multiple mechanisms of resistance as mentioned elsewhere [1].
Genomic Profile of P. aeruginosa complete sequencing of the P. aeruginosa PA01 strain revealed a complex organism. Low gene replication across the genome indicates that such a comparatively large genome has vast potential of functional diversity, which may support rich mechanisms responsible for multidrug resistance. Available genome data supports the hypothesis of the existence of evolutionary paths where resistance to naturally available antibiotics was acquired [2].
MEDICAL IMPACT AND EPIDEMIOLOGY OF MDR P. AERUGINOSA
Pseudomonas species cause a variety of infections, mainly urinary tract infections, respiratory infections, ocular infections, endocarditis, bone and joint infections, burn infections and other skin infections, such as ecthyma gangrenosum or cellulitis [5]. These infections among others include: bacteriaemia, endocarditis, meningitis, otitis media, osteomyelitis, diarrheal disease or enterocolitis and green nail syndrome of skin, which is usually hospital acquired [1]. In hospitalized patients, this organism colonizes with higher rates, particularly when the patient is under administration of broad-spectrum antibiotics which affects normal flora. Similarly, the disruption of natural barriers because of insertion of intravascular medical devices, endotracheal tubes and urinary catheters also predispose patients to acquire nosocomial infection by this pathogen [1].
In hospitalized patients, P. aeruginosa usually attacks patients with burns and wounds where they further complicate the primary condition and sometimes lead to bacteremia. In this connection, 40-60% mortality has been attributed to ventilator-associated pneumonia caused by P. aeruginosa. It is also the major causes of morbidity and mortality in patients suffering from cystic fibrosis (CF) which is an autosomal recessive disorder [12]. CF is multi-system disease, which affects mainly lung and digestive system. Mortality in this afflicted population is mainly attributed to chronic respiratory infections and the associated gradual deterioration of lung function. There are several pathogens known to play a role in CF lung infection, with Staphylococcus aureus and Haemophilus influenzae being the predominant pathogens colonizing in infancy and early childhood, and eventual replacement by P. aeruginosa. However, P. aeruginosa is often isolated from patients less than 2 years of age and is the most predominant concern in adults. Up to 90% of individuals suffering from CF become infected with P.aeruginosa during their lifetime. In the majority of cases, colonization of the CF airway by P. aeruginosa leads to a chronic infection that is resistant to antimicrobial therapy. Chronic colonization and infection with P. aeruginosa is an inevitable reality for the majority of adults with CF, as over 80% of adults over the age of 18 years return positive cultures for P. aeruginosa[9].
Moreover, this organism plays a significant role in the

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 6/8
enhancement of complications in chronic obstructive pulmonary diseases (COPD) [1]. P. aeruginosa bacteremia, in particular, is associated with high mortality. Reported mortality rates exceed 50% in some series and are even higher within certain populations, such as in patients with severe underlying comorbid conditions or those with immunosuppression [12], P. aeruginosa was the third most frequently isolated species from blood in an intensive care unit (ICU) and the predominant isolate in central venous catheters among the species included in the ESKAPE group of multidrug-resistant microorganisms (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [12].
Infections caused by P. aeruginosa are particularly problematic because the organism is inherently resistant to many drug classes and is able to acquire resistance to all effective antimicrobial drugs [8]. However, multidrug-resistant P. aeruginosa (MDRPA) strains were first reported in patients with cystic fibrosis. Out breaks due to single strains have been reported; however, in other instances, outbreaks due to multiple strains have been reported [2, 15].
The incidence rate of infections produces by MDR P. aeruginosa strains may vary from 5.5 to 14 cases per 10,000 patients admitted per year. A study developed in a hospital in Rome, Italy revealed the first case of MDR P. aeruginosa infection in a haematologic patient in 1992. After that, the prevalence of MDR P. aeruginosa increased from 8% in 1993 to 17% in 1999, related to that hospital [5]. Of 358 cases of bloodstream infections due to P. aeruginosa, 14% (51 cases) were caused by strains of MDR P. aeruginosa. In these cases, 96% (46 infections) were nosocomial. The overall mortality rate due to P. aeruginosa infection is greater than 20%, which increases when the infection is due to MDR P. aeruginosa strains [5].As a frequency, MDR P. aeruginosa account for 12.3% to 36.5% of the isolated P. aeruginosa from different health care units in different countries. In a retrospective study covered 18 hospitals in Brazil the frequency of MDR P. aeruginosa was 23.1% [36], in Keratchi - Pakistan tertiary Hospital the prevalence was 36.5% [37], in another study conducted in a Military Hospital in Islam Abad- Pakistan the frequency was 22.7% [38], in study conducted in India covered burns patients the frequency of MDR P. aeruginosa was 36.45% [39], another study covered burns patients and environmental sources estimated the frequency of MDR P. aeruginosa as 36.2% [40], low frequency rate of MDR P. aeruginosa (12.3% and 19%) was reported in Egypt in two different studies [3,41]. The isolated P. aeruginosa from pneumonic patients during 10 years in Germany resulting in 24.4% frequency of MDRPA [42].
TREATMENT OF P. AERUGINOSA INFECTION AND MDR-PA
Because of the unavailability of the successful therapeutic option, the treatment of severe infections with pseudomonas is now becoming more difficult. Only few anti-pseudomonal drugs such as some beta-lactams, aminoglycosides and fluoroquinolones can be considered good therapeutic options due to the emergence of resistance to most of the antibiotics giving rise to multiple drug resistant P. aeruginosa strains [1]. The most
important anti-pseudomonal agents include some b-lactams (ticarcillin, ureidopenicillins, piperacillin, cefoperazone, ceftazidime, cefepime, aztreonam, imipenem and meropenem), aminoglycosides (gentamicin, tobramycin, netilmicin and amikacin) and fluoroquinolones (of which ciprofloxacin remains the most active compound]. [43].
The use of antimicrobials can enhance the incidence of resistant strains [44]. Treatment of MDRPA is a challenging issue worldwide. The treatment is facilitated by rapid detection of resistance and characterization of the isolates. Doripenem is a new drug of choice for treatment of MDRPA [5]. Doripenem (DPM) is the new β-lactamic from the carbapenems family. It has a four membered β-lactamics in one ring, which connect with a second ring in the structure[5]. Polymyxins (polymyxin B and colistin) are also active but, due to their higher toxicity, are usually considered only for multidrug-resistant Multidrug-resistant Pseudomonas aeruginosa is a major threat in healthcare settings. Mono therapy is highly recommended for uncomplicated infection such as UTI, while combined therapy is recommended in severe infection such as bacteremia and pneumonia or in severely ill patient [45]. The most common combination is colisitin with one of beta lactams drugs, cephalsporins, rifampicin, amikacin or carbapenem. The second choice for combination is aminoglycoside with carbapenems or tigecycline. Polymexin B with tigecycline was also been studied as a choice of combination [45,46].
CONCLUSIONDrug resistance in P. aeruginosa is multifactorial increasing
phenomenon. Estimated frequencies were between 12-36%. Mechanisms of resistance either through membrane permeability and efflux system or through its virulence factors or acquired genetically by plasmid. Combination of these mechanisms leads to a super bugs, which are very difficult to be treated.
REFERENCES1. Ali Z, Mumtaz N, Naz SA, Jabeen N, Shafique M. Multi-drug resistant
Pseudomonas aeruginosa: a threat of nosocomial infections in tertiary care hospitals. J Pak Med Assoc. 2015; 65: 12-16.
2. Porras-Gómez M, Vega-Baudrit J, SNúñez-Corrales S. Overview of Multidrug-Resistant Pseudomonas aeruginosa and Novel Therapeutic Approaches. J Biomater Nanobiotechnol. 2012; 519-527.
3. Mahmoud AB, Zahran WA, Hindawi GR, Labib AZ, Galal R. Prevalence of Multidrug-Resistant Pseudomonas aeruginosa in Patients with Nosocomial Infections at a University Hospital in Egypt, with Special Reference to Typing Methods. J Virol Microbiol. 2013; 2013: 290047.
4. Tirodimos I, Arvanitidou M, Dardavessis T, Bisiklis A, Alexiou-Daniil S. Prevalence and antibiotic resistance of Pseudomonas aeruginosa isolated from swimming pools in northern Greece. East Mediterr Health J. 2010; 6: 783-787.
5. Barrios CC, Ciancotti-Oliver L, Bautista-Rentero D, Adán-Tomás C, and Zanón-Viguer V. A New Treatment Choice against MultiDrug Resistant Pseudomonas aeruginosa: Doripenem. J Bacteriol Parasitol. 2014; 5: 199.
6. Carmeli Y, Troillet N, Eliopoulos G M, and Samore M H. Emergence of Antibiotic-Resistant Pseudomonas aeruginosa: Comparison of Risks Associated with Different Antipseudomonal Agents. Antimicrobial Agents and Chemotherapy. 1999; 43: 1379-1382.

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 7/8
7. Gellatly SL, Hancock RE. Pseudomonas aeruginosa: new insights into pathogenesis and host defenses. Pathog Dis. 2013; 159-173.
8. Iglewski BH. Pseudomonas. In: Baron S, editor. Medical Microbiology. 4thed. University of Texas Medical Branch at Galveston. 1996.
9. Alhazmi A. Pseudomonas aeruginosa Pathogenesis and Pathogenic Mechanisms. Int J Biol. 2015; 7: 44-67.
10. Owlia P, Nosrati R, Alaghehbandan R, Lari AR. Antimicrobial susceptibility differences among mucoid and non-mucoid Pseudomonas aeruginosa isolates. GMS Hyg Infect Control. 2014; 9.
11. Srifuengfung S, Tiensasitorn C, Yungyuen T, Dhiraputra C. Prevalence and Antimicrobial susceptibility of Pseudomonas aeruginosa mucoid and non-mucoid type. Southeast Asian J Trop Med Public Health. 2004; 35: 893-896.
12. Inacio HSM, Bomfim MRQ, França RO, Farias LM, Carvalho MAR, Serufo JC, et al. Phenotypic and Genotypic Diversity of Multidrug-Resistant Pseudomonas aeruginosa Isolates from Bloodstream Infections Recovered in the Hospitals of Belo Horizonte, Brazil. Chemotherapy. 2014; 60: 54-62.
13. Jombo GT, Jonah P, Ayeni JA. Multidrug Resistant Pseudomonas aeruginosa in Contemporary Medical Practice: Findings from Urinary Isolates at a Nigerian University Teaching Hospital. Niger J Physiol Sci. 2008; 23: 105-109.
14. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18: 268-281.
15. Paramythiotou E, Lucet JC, Timsit JF, Vanjak D, Paugam-Burtz C, Trouillet JL, et al. Acquisition of Multidrug-Resistant Pseudomonas aeruginosa in Patients in Intensive Care Units: Role of Antibiotics with Antipseudomonal Activity. Clin Infect Dis. 2004; 38: 670-677.
16. Hassuna N, Mohamed AHI, Abo-Eleuoon SM, Rizk HA. High Prevalence of Multidrug Resistant Pseudomonas aeruginosa Recovered from Infected Burn Wounds in Children. Arch Clin Microbiol. 2015; 6.
17. Falagas ME, Kopterides P. Risk factors for the isolation of multi-drug-resistant Acinetobacter baumannii and Pseudommonas aeruginosa: a systemic review of the literature. J Hosp Infect. 2006; 64: 7-15.
18. Defeza C, Fabbro-Peraya P, Bouzigesc N, Goubyc A, Mahamata A, Daure`sa JP, et al. Risk factors for multidrug-resistant Pseudomonas aeruginosa nosocomial infection. J Hosp Infect. 2004; 57: 209-216.
19. Hancock RE. Resistance Mechanisms in Pseudomonas aeruginosa and Other Nonfermentative Gram-Negative Bacteria. Clin Infect Dis. 1998; 93-99.
20. Zgurskaya HI, Löpez CA, Gnanakaran S. Permeability Barrier of Gram-Negative Cell Envelopes and Approaches to Bypass It. ACS Infect Dis. 2015; 1: 512-522.
21. Webber MA. Piddock LJV. The importance of efflux pumps in bacterial antibiotic resistance. J Antimicrob Chemother. 2003; 51: 9-11.
22. Aeschlimann JR. The Role of Multidrug Efflux Pumps in the Antibiotic Resistance of Pseudomonas aeruginosa and Other Gram-Negative Bacteria. Pharmacotherapy. 2003; 23: 916-924.
23. Bush K, Jacoby GA. Updated Functional Classification of β-Lactamases. Antimicrob Agents Chemother. 2010; 54(3): 969–976.
24. Lambert PA. Mechanisms of antibiotic resistance in Pseudomonas aeruginosa. J R Soc Med. 2002; 95 (41):22–26.
25. Jacoby GA. AmpC – Lactamases. CMR. 2009; 22(1): 161–182.
26. Poole K. Pseudomonas Aeruginosa: Resistance to the Max. Front
Microbiol. 2011; 2: 65.
27. Kato T, Sato Y, Iyobe S, and Mitsuhashi S. Plasmid-mediated gentamicin resistance of Pseudomonas aeruginosa and its lack of expression in Escherichia coli. Antimicrob Agents Chemother 1982; 22(3):358-363.
28. Fahimeh Beige F, Salehi MB, Bahador N, and Mobasherzadeh S. Plasmid Mediated Antibiotic Resistance in Isolated Bacteria From Burned Patients Jundishapur. J Microbiol. 2015; 8(1): 13567.
29. Saleh MA and Balboula MM. Plasmid Mediated Quinolone Resistance Determinants among Nosocomial Clinical Pseudomonas aeruginosa Isolates. IJCMAS. 2017; 6(1): 42-50.
30. Shahid M, Malik A, and Sheeba. Multidrug-resistant Pseudomonas aeruginosa strains harboring R-plasmids and AmpC L-lactamases isolated from hospitalized burn patients in a tertiary care hospital of North India. FEMS Microbiology Letters. 2003; 228(2):181-186.
31. Campos C, Gabarrus A, Liapikou A, Martinez D, Niederman M, and Torres A. Community-acquired pneumonia due to multidrug and non-multidrug resistant Pseudomonas aeruginosa. ERJ. 2016; 48(supp60).
32. Budak F, Kasap M, Kolayli F, Karadenizli A, Vahaboğlu M H. Integron-associated resistance genes among multidrug-resistant Pseudomonas aeruginosa isolated from clinical specimens. Turk J Med Sci. 2012; 42 (1): 149-156.
33. Fuste’ E, Lo’pez-Jime’nez L, Segura C, Gainza E, Vinuesa T and Viñas M. Carbapenem-resistance mechanisms of multidrug-resistant Pseudomonas aeruginosa. JMed Microbiol. 2013; 62: 1317–1325.
34. Suarez C, Pena C, Tubau F, Gavalda L, Manzur A, Dominguez M A, Pujol M, Gudiol F, Ariza J. Clinical impact of imipenem resistant Pseudomonas aeruginosa blood stream infections. J Infect. 2009; 285-290.
35. Nathwani D, Raman G, Sulham K, Gavaghan M, Menon V. clinical and economic consequences of hospital acquired resistant multi-drug resistant Pseudomonas aeroginosa: a systemic review and meta-analysis. Antimicrobial resistant and infection control. 2014; 3: 32.
36. das Neves MT , de Lorenzo MEP, Almeida RAMB and Fortaleza CMCB. Antimicrobial use and incidence of multidrug-resistant Pseudomonas aeruginosa in a teaching hospital: an ecological approach. Revista da Sociedade Brasileira de Medicina Tropical 2010;43(6):629-632.
37. Mansoor K, Tanvir SB, Shariq A, Hussain A, Farooqi BJ, Ahmed S, Tanvir R. Frequency and susceptibility pattern of Multidrug Resistant Pseudomonas aeruginosa in isolates of patients from a tertiary care hospital of Karachi, Pakistan. Eur J Biotechnol Bio Sci. 2015;3(5):33-36.
38. Gill MM, Usman J, Fatima Kaleem, Hassan A, Khalid A, Anjum R and Fahim Q. Frequency and Antibiogram of Multi-drug Resistant Pseudomonas aeruginosa. J Coll Physicians Surg Pak. 2011; 21 (9): 531-534.
39. Kamaria PA, Aring BJ, and Sinha M. Incidence of Multidrug Resistant Pseudomonas Aeruginosa Isolated From Burn Patients Tertiary Care Hospital, Jamnagar, Gujarat, India. IOSR-JDMS. 2016; 15(7):31-34.
40. Biswal I, Arora BS, Kasana D, and Neetushree. Incidence of Multidrug Resistant Pseudomonas aeruginosa Isolated from Burn Patients and Environment of Teaching Institution. J Clin and Diagn Res. 2014;8(5): 26-29.
41. Wassef M, El Mahallawy H, Zafer MM, Ghaith D and Abd Elhamid R. Lab Based Surveillance of Multidrug Resistant Pseudomonas aeruginosa in Cairo University Hospitals, Egypt J Microbiol Exp. 2015, 2(2): 00039.
42. Yayan J, Ghebremedhin B, and Rasche K. Antibiotic Resistance of Pseudomonas aeruginosa in Pneumonia at a Single University Hospital Center in Germany over a 10-Year Period. PLoS One.2015; 10(10).
43. Rossolini GM. and Mantengoli E. Treatment and control of severe

CentralBringing Excellence in Open Access
Alnour et al. (2017)Email:
JSM Microbiology 5(3): 1046 (2017) 8/8
Alnour TMS, Ahmed-Abakur EH (2017) Multidrug Resistant Pseudomonas (P) aeruginosa: Medical Impact, Pathogenicity, Resistance Mechanisms and Epidemiol-ogy. JSM Microbiology 5(3): 1046.
Cite this article
infections caused by multiresistant Pseudomonas aeruginosa. Clin Microbiol Infect. 2015; 11 (Suppl. 4), 17–32.
44. Pogue JM, Kaye KS, Cohen DA. and Marchaim D. Appropriate antimicrobial therapy in the era of multidrug-resistant human pathogens. Clin Microbiol Infect.2015; 21(4):302–312.
45. Tamma PD, Cosgrove SE, and Maragakis LL. Combination Therapy for Treatment of Infections with Gram-Negative Bacteria. CMR 2012;3(25):450-470.
46. Tängdén T. Combination antibiotic therapy for multidrug-resistant Gram-negative bacteria. Ups J Med Sci. 2014; 119: 149–153.