Milestones in Dystonia - residents.lsuhsc.edu milestones.pdfMilestones in Dystonia Laurie J....
Transcript of Milestones in Dystonia - residents.lsuhsc.edu milestones.pdfMilestones in Dystonia Laurie J....
-
Milestones in Dystonia
Laurie J. Ozelius, PhD,1 Naomi Lubarr, MD,2
and Susan B. Bressman, MD2,3*
1Departments of Genetics and Genomic Sciences and Neurology, Mount Sinai School of Medicine, New York, New York, USA2Department of Neurology, Beth Israel Medical Center, New York, New York, USA
3Department of Neurology, Albert Einstein College of Medicine, Bronx, New York, USA
ABSTRACT: The last 25 years have seen remark-able advances in our understanding of the genetic etiol-ogies of dystonia, new approaches into dissectingunderlying pathophysiology, and independent progressin identifying effective treatments. In this review wehighlight some of these advances, especially thegenetic findings that have taken us from phenomeno-logical to molecular-based diagnoses. Twenty DYT locihave been designated and 10 genes identified, allbased on linkage analyses in families. Hand in handwith these genetic findings, neurophysiological andimaging techniques have been employed that havehelped illuminate the similarities and differences amongthe various etiological dystonia subtypes. This knowl-edge is just beginning to yield new approaches to treat-
ment including those based on DYT1 animal models.Despite the lag in identifying genetically based thera-pies, effective treatments, including impressive benefitsfrom deep brain stimulation and botulinum toxin chemo-denervation, have marked the last 25 years. The chal-lenge ahead includes continued advancement intounderstanding dystonia’s many underlying causes andassociated pathology and using this knowledge toadvance treatment including preventing genetic diseaseexpression. VC 2011 Movement Disorder Society
Key Words: dystonia; genetics; neurophysiology; imag-ing; treatments
The last 25 years have seen remarkable advances inour understanding of the genetic etiologies of dysto-nia, new approaches into dissecting underlying patho-physiology, and independent progress in identifyingeffective treatments. These advances take advantage ofthe many new techniques that have revolutionizedmedical scientific research. They also build on a criti-cal base of clinical and pathological studies from priordecades, particularly the rich observations and classifi-cation schema proposed by David Marsden and Stan-ley Fahn through the 1970s and ’80s.
Twenty-five years ago, the Second International Dys-tonia Symposium was held in Harriman, New York.That fully international 3-day event allowed for state-of-knowledge presentations and lively discussion meantto generate ideas on pathophysiology, treatment, andfuture study. The content of that meeting is summar-ized in volume 50 of Advances of Neurology, a longbook of almost 700 pages.1 In that volume are the inti-mations and foundations of the advances to come,including pilot family and genetic linkage studies, neu-rophysiological analyses, PET and MRI reports, anddiscussions of botulinum toxin for focal dystonias.This review will briefly discuss the advances madesince that meeting in defining genetic etiologies and theramifications of gene identification both in terms ofclinical applications and basic investigation, neuro-physiological and imaging studies that have helpedtease apart underlying brain mechanisms in dystonia,and progress in treatment. Despite these advances,many questions remain. Indeed the progress of the last25 years has served to raise many new questions andopened up new avenues of research. These will bementioned as well; hopefully, they will help to
------------------------------------------------------------*Correspondence to: Prof. Susan B. Bressman, Beth Israel MedicalCenter, Neurology, 10 Union Square East, Suite 2Q, New York, NY10003, USA; [email protected]
Funding agencies: This work was supported by National Institute ofNeurological Disorders and Stroke research grant P50NS037409 (toL.J.O.) and the Bachmann Strauss Dystonia and Parkinson Foundation(to L.J.O. and S.B.B.).Relevant conflicts of interest/financial disclosures: Nothing to report.Full financial disclosures and author roles may be found in the onlineversion of this article.
Received: 7 April 2011; Accepted: 7 April 2011Published online in Wiley Online Library (wileyonlinelibrary.com).DOI: 10.1002/mds.23775
R E V I E W
1106 Movement Disorders, Vol. 26, No. 6, 2011
-
engender interest and novel approaches, especiallyamong those newly entering this most exciting field.
Genetics
Coupling the major advances in human geneticsincluding linkage mapping of Mendelian traits, theadvent of polymerase chain reaction for amplificationof specific DNA regions, and the completion of thehuman genome sequence with careful phenotypic stud-ies in families, 20 monogenic dystonia loci have beendefined in the last 25 years.2,3 The DYT loci have beendesignated historically based on phenotype or chromo-somal location and thus represent a clinically heteroge-neous group of disorders including primary dystoniawhere dystonia is the only phenotype (DYT1, DYT2,DYT4, DYT6, DYT7, DYT13, DYT17, and DYT21),dystonia plus loci where other phenotypes in addition
to dystonia such as parkinsonism or myoclonus areseen (DYT3, DYT5/14, DYT11, DYT12, DYT15, andDYT16), and paroxysmal forms of dystonia/dyskinesia(DYT8, DYT9, DYT10, DYT18, DYT19, andDYT20).3 Among these loci, 10 genes have been identi-fied, all using the genetic technique of linkage analysisin families. See Table 1 for dystonia genetic highlights.
Primary Torsion Dystonia (PTD)
The phenotypic spectrum associated with PTD isbroad, ranging from early-onset generalized to adult-onset focal. The prevalence of PTD has been estimatedat between 3304 and 1525 per million, with focal casesconstituting the majority. However, these studies arelikely to underestimate the true frequency of PTDbecause a significant proportion of disease is not diag-nosed.6,7 Loci have been defined for both types includ-ing DYT1, DYT2, DYT4, DYT6, DYT13, andDYT17 for early-onset forms and DYT7 and DYT21
TABLE 1. Dystonia Genetics Highlights
1985–1989Family studies determine that most early limb onset ‘‘idiopathic’’ torsion dystonia, (including in Ashkenazi Jews) is inherited as an autosomal dominanttrait with reduced penetranceThe DYT1 locus for early-onset ‘‘idiopathic’’ or primary dystonia is mapped to chromosome 9q32-34There are family, clinical and biochemical studies of dopa responsive dystonia (DRD) establishing a distinct autosomal dominant subtype
1990–1994The phenotype of DYT1 is characterized using a 9q associated haplotype of alleles identified in Ashkenazi Jewish familiesThe locus for Lubag (X-linked dystonia parkinsonism) is mapped to the pericentromeric region of the X chromosome (DYT3)A locus for DRD (DYT5) is mapped to 14qThe DRD gene at DYT5, GCH1, coding for GTP cyclohydrolase 1, identifiedThe clinical features of rapid onset dystonia-parkinsonism are describedLocus for Wilson’s disease is mapped and gene, coding for ATP7B, identified
1995–1999Mutations in tyrosine hydroxylase are identified as a cause of DRDThe locus for ‘‘Hallervorden-Spatz’’ disease is mapped to chromosome 20p12.3-p13The DYT6 locus for a ‘‘mixed’’ primary dystonia phenotype is mapped to chromosome 8q22-q23The DYT7 locus for adult-onset focal primary dystonia phenotype is mapped to 18pThe DYT8 locus for paroxysmal non-kinesigenic dyskinesia, (PNKD) is mapped to chromosome 2q33-q36Gene for DYT1 (TOR1A), coding torsinA, is identifiedThe DYT9 locus for paroxysmal dyskinesia with spasticity, is mapped to 1p21-p13.3The DYT10 locus for paroxysmal kinesigenic dyskinesia (PKD) is mapped to chromosome 16 p11.2-q12.1The DYT11 locus for myoclonus-dystonia (M-D) is mapped to chromosome 7q21-31The DYT12 locus for rapid-onset dystonia-parkinsonism (RDP) is mapped to chromosome 19q13
2000–2004The gene for ‘‘Hallervorden–Spatz’’ syndrome, (renamed pantothenate kinase associated neurodegeneration or PKAN), PANK2, which codes for panthenatekinase 2, is identifiedThe M-D gene at DYT11, SGCE, coding for epsilon sarcoglycan, is identifiedThe gene for Lubag is reported to involve a multiple transcript system including TAF1The RDP gene at DYT12, ATP1A3, coding for Naþ/Kþ ATPase a3 subunit, is identifiedThe DYT13 locus for cranial-cervical-brachial dystonia is mapped to 1p36.13-p36.32The DYT15 locus, a second locus for M-D is mapped to 18p35-p31.3
2005–2011The gene for infantile neuroaxonal dystrophy, PLA2G6, is identifiedThe DYT16 gene for early-onset dystonia parkinsonism, PRKRA is identifiedThe DYT17 locus for early-onset cervical-cranial dystonia is mapped to chromosome 20p11.22-q13.12The gene for Kufor-Rakeb, ATP13A2, is identifiedDYT18 is designated for the SLC2A1 gene, which causes a deficiency in glucose transport protein type 1 and dystonia, especially exercise inducedThe ‘‘mixed’’ phenotype gene at DYT6, THAP1, is identifiedA second locus, DYT19, for paroxysmal kinesigenic dyskinesia is located to 16q13-q22.1 very near DYT10A second locus, DYT20, for paroxysmal non-kinesigenic dyskinesia is located to 2q31The DYT21 locus for late-onset generalized dystonia is mapped to chromosome 2q14.3-q21.3
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1107
-
for later-onset forms,8,9 but only 2 genes, DYT1 andDYT6, have been identified.10,11
Early-Onset PTD
Two features of early-onset PTD were recognizedearly on: its occurrence was familial,12 and it wasmore frequent among Ashkenazi Jews (AJs).13 How-ever, the mode of inheritance was thought to be domi-nant for non-Jewish (NJ) families and recessive in AJfamilies.14 Studies in the United States, Israel, andBritain showed that the disease was inherited as anautosomal dominant trait with reduced penetrance inboth the AJ and NJ populations.15–20
DYT1. Linkage analysis in a large NJ family withearly-onset disease identified the first locus for early-onset PTD, DYT1, on chromosome 9q34,21 whichwas subsequently confirmed in other AJ and NJ fami-lies.20,22,23 Strong linkage disequilibrium was observedbetween the disease gene and a particular haplotype inthe AJ population,24 indicative of a founder mutation.The haplotype was used to estimate that the mutationwas introduced into the AJ population about 350years ago and probably originated in Lithuania orByelorussia6 and also to define the disease gene withina 150-kb region. Screening of the genes in this regionresulted in the identification of a 3-bp deletion in theTOR1A gene causing the removal of a single in-frameamino acid in the encoded protein, torsinA, in bothAJ and NJ cases.10 The deletion mutation in TOR1Ahas been found in patients with diverse ethnic originsand accounts for about 80% of early-onset PTD in theAJ population because of the founder mutation,25,26
but fewer than 50% in the NJ population,27–32 suggest-ing a significant proportion of early-onset NJ PTD maybe a result of other genes.11,33 Two other missensemutations in the TOR1A gene have been described,each in a single case.34,35 A third missense variant,D216H, found to have functional significance in cellculture studies,36 was subsequently shown to be associ-ated with reduced penetrance37,38 and functionally con-firmed by imaging studies that correlated alteredmetabolism in specific brain regions in DYT1-nonmani-festing carriers with the D216H SNP.39
Although the clinical phenotype associated withDYT1 dystonia can vary from severe dystonic storm40
to mild writer’s cramp,41 a typical phenotype has beendescribed across ethnic groups characterized by early(mean age at onset, 13 years; with the majority before26 years) limb (arm or leg is affected first in 90% ofcases) onset, progressing to generalized/multifocal(65%) involvement, with spread to cranial muscles lesscommon (15%–20%).27,31,42–45 Genetic testing for thedeletion mutation is readily available and relativelyinexpensive and should be considered for any non-dopa-responsive case with onset before age 26 years.
TorsinA is a member of the AAAþ superfamily(ATPases associated with a variety of cellular activ-ities) of molecular chaperones.46 It is widely distrib-uted in the brain but restricted to neurons. Within thecell, most of the wild-type protein is in the endoplas-mic reticulum (ER), whereas the mutant protein ismore often associated with the nuclear envelope(NE).47–49 TorsinA disrupts ER/NE and cytoskeletaldynamics, which may be important for neurite exten-sion during brain development49–53 and has also beenimplicated in synaptic vesicle recycling, includingimpaired dopamine release54–57 and alter tyrosinehydroxylase activity.58 Exactly how torsinA functionis compromised to produce disease is unknown, butboth animal and cellular studies indicate that mutanttorsinA results in a loss of function.49,54,59–61
DYT6. This locus was initially mapped to the centro-mere of chromosome 8 in 3 Amish–Mennonite fami-lies that shared a haplotype and were related via acommon ancestor.62,63 In these families, the diseaseshowed autosomal dominant inheritance with a pene-trance of about 60%. Using the Amish–Mennonitefamilies, a complex insertion/deletion mutation thatresults in a truncated protein was identified in theTHAP1 (thanatos-associated protein domain-contain-ing apoptosis-associated protein 1) gene.11 Unlike theTOR1A gene, where a single mutation accounts formost cases, more than 45 heterozygous mutationshave been reported in THAP1, mainly in patients ofEuropean ancestry,11,64–73 but also in Chinese74 andBrazilian75 cases. Interestingly, 2 homozygous mis-sense mutations have been reported.70,76 In addition,heterozygous synonymous amino acid substitu-tions67,68,72 as well as variants in the 50 untranslatedregion72 and within introns70,72 have been found inPTD cases but are of unknown significance. Finally,because almost every individual/family has a uniquemutation, molecular diagnosis requires sequencing ofthe 3 exons of the THAP1 gene.Comparing clinical symptoms in mutation carriers, a
typical DYT6 phenotype emerges characterized byearly onset (mean, 16 years; range, 5–62 years); onsetmost often in an arm (50%), followed by cranialmuscles (about 25%) or the neck (about 25%) but incontrast with DYT1, rarely the leg (4%); with spreadto a generalized or multifocal distribution in morethan half and prominent speech involvement in morethan two thirds of cases.11,65–75 However, about 10%of cases have only focal dystonia and in screens ofadult-onset focal cases, low frequency (>1%) ofTHAP1 mutations has been reported.70–72
THAP1 is a transcription factor with a conservedDNA binding domain at its N-terminus, and a coiled-coil domain and nuclear localization signal (NLS) atits C-terminus.77,78 THAP1 function in the brain is
O Z E L I U S E T A L .
1108 Movement Disorders, Vol. 26, No. 6, 2011
-
unknown, but it regulates endothelial cell proliferationby pRb/E2F cell-cycle target genes,79 is a proapoptoticfactor,78 and through its C-terminus, interacts withprostate apoptosis response 4 protein (Par-4),78 aneffector of cell death linked to prostate cancer andneurodegenerative diseases, including Parkinson’s dis-eases.80 Recently, Thap1 protein has been shown tobind to the TOR1A promoter and repress its expres-sion. DNA binding is disrupted and repressiondecreased by pathogenic THAP1 mutations.81,82 Thesedata link the molecular pathways underlying DYT1and DYT6 dystonia and highlights transcriptional dys-regulation as a cause of PTD. In addition, THAP1 hasbeen shown to be physically linked to OGT, a genethat is next to TAF1 on Xq13.1 in the DYT3 criticalregion (see below).83
At present, there are no genotype:phenotype correla-tions noted in THAP1. Most of the mutations occur inthe DNA binding domain or around the NLS and arethought to eliminate the DNA binding function of theprotein.11,65–75,81 A few mutations occur in the coiled-coil domain,64,69–72 a region important for dimerizationthat could indirectly disrupt DNA binding if, as pro-posed, THAP1 binds DNA as a homodimer.84–86
DYT2 and DYT4. DYT2 and DYT4 are loci thathave been assigned based on phenotype alone with nochromosomal location or gene identified to date.DYT2 is an autosomal recessive form of PTD reportedin consanguineous families of Spanish gypsy (1988),87
Sephardic Jewish,88 and Arab33 descent. All the caseshave a similar phenotype to DYT1 dystonia, withearly limb onset followed by rapid generalization.DYT4 is an autosomal dominant form of PTDreported in a single large Australian family with prom-inent whispering dysphonia that begins in the seconddecade in most family members (range, 13–37years).89,90 The THAP1 gene was excluded as a causein this family.66
DYT13 and DYT17. These 2 loci are each describedin a single family that was used to map their chromo-somal positions. Both show adolescent onset, butDYT13 is inherited as a dominant disorder withreduced penetrance, whereas DYT17 is inherited as anautosomal recessive trait. DYT13 was mapped tochromosome 1p3691 in an Italian family with mainlysegmental dystonia, prominent craniocervical involve-ment, but less speech than in DYT6 dystonia.92 A con-sanguineous Lebanese family with 3 siblings was usedto map DYT17 to chromosome 20. Onset was in theneck in all sibs but progressed to segmental dystoniain 2 and to generalized dystonia in the third and fea-tured severe dysphonia and dysarthria.93 It is possiblethat some of the families currently designated asDYT2 could be linked to the DYT17 gene region.
Late-Onset PTD
Late-onset PTD is more complex genetically thanearly-onset PTD, and the role of genes in the etiologyof the various adult clinical subtypes (torticollis, writ-er’s cramp, blepharospasm, and spasmodic dysphonia)is not fully elucidated. However, the forms arethought to be related complex diseases that share com-mon susceptibility genes as well as additional individ-ual genetic and environmental risk factors that occurin different combinations resulting in specific dis-ease.94 Segregation analyses concluded that focal dys-tonia is inherited as an autosomal dominant trait butwith very low penetrance (about 12%–15% comparedwith 30% for early onset)95,96; alternatively, pene-trance may be higher in a subset, with the remaindernongenetic. Descriptions of several large families withhighly penetrant autosomal dominant late-onsetPTD97–99 are consistent with this latter idea and haveresulted in the mapping of 2 genes for late-onset PTD:DYT7100 and DYT21.9
DYT7 and DYT21. DYT7 and DYT21 are both auto-somal dominant disorders each described in a singlepedigree. DYT7 was assigned to chromosome 18p in afamily from northwestern Germany with 7 affectedmembers, all with adult-onset cervical dystonia (mean,43 years; range, 28–70 years), although some also hadbrachial and cranial involvement.100 Several pheno-typically similar families were excluded from thisregion,101 suggesting the existence of other late-onsetloci. A family with 16 affected members from north-ern Sweden was linked to a region on chromosome2q14.3–q21.3 and designated as DYT21.9 The pheno-type in this family is characterized by later onset(mean, 27 years; range, 13–50 years) and mainly gen-eralized/multifocal PTD, with onset in the cranial/cer-vical muscles in most and the hands in about 25%.Because the majority of late-onset PTD cases do not
have many affected relatives, linkage mapping is not anoption, and instead, association studies using cases andcontrols have been employed to find genetic risk factorsin candidate genes. A polymorphism in the dopamineD5 receptor (DRD5) gene is associated with torticollisand blepharospasm in 3 studies102–104 but could not bereplicated in 2 other studies.105,106 Contradictory find-ings have been reported for the functional V66M SNPin brain-derived neurotrophic factor (BDNF), with 1group finding no association among cranial and cervi-cal PTD patients107 and a second team finding a two-fold increase in the V66M heterozygotes among a smallsample of cervical cases.108 Studies examining theinvolvement of the THAP1 and TOR1A genes in late-onset dystonia have also been performed. Several ofthese have suggested that variants in THAP1 mightcontribute to the risk of focal dystonia,66,70,72 but theassociated variants were not consistent. Associations
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1109
-
with variations in TOR1A are also confusing. TheD216H SNP has been associated with increased risk inpatients with a positive family history,109 whereasSNPs in the 30 untranslated region have been associatedwith risk in some sporadic cases,106,110 risk of spreadof blepharospasm in other cohorts,111 and protectionfrom risk,112 particularly in sporadic cervical cases.113
Finally, 2 studies failed to show any association withSNPs in the TOR1A gene.105,114
The contradictory data reported for these candidategenes is a result of several factors including clinicalheterogeneity (different subtypes of PTD, with andwithout family history, etc.), limited sample size, smallnumber of SNPs tested, and different ethnic groups.To overcome these issues, the use of new genetic tech-niques including genome-wide association studies(GWASs) and next-generation exome or whole-ge-nome sequencing approaches is critical for identifyingthe genetic risk factors contributing to late-onset PTD.However, especially for GWASs, a large number ofuniformly phenotyped late-onset cases will be neededand can only be achieved through a worldwide collab-orative effort.
Dystonia Plus
Within the dystonia plus classification there are 4forms that include parkinsonism as part of their phe-notype (DYT3, DYT5/14, DYT12, and DYT16), and2 that have myoclonus in addition to dystonia(DYT11 and DYT15). Genes have been identified forall these forms except DYT15.3
DYT3
DYT3 is the only form of dystonia that is inheritedas an X-linked trait. The disease originated on theisland of Panay in the Philippines due to a foundermutation and primarily affects males,115 although afew females have been reported with the disease.116,117
The DYT3 locus was mapped to Xq,118,119 with furtherlinkage and linkage disequilibrium analyses narrowingthe locus to Xq13.1.120,121 Several disease-specificchanges were identified in a 300-kb region including a48-bp deletion in an exon of a novel transcript, 5 singlebase-pair changes in the TATA-binding protein–associ-ated factor (TAF1) gene, and a retrotransposon inser-tion in an intron of TAF1.122,123 Although the region iscomplex and contains multiple transcripts,124 the retro-transposon insertion appears to reduce neuron-specificexpression of TAF1 and the dopamine receptor D2gene in the caudate nucleus, suggesting this gene playsa role in the disease.123 In addition, a physical associa-tion between the OGT gene, adjacent to TAF1 andwithin the 300-kb DYT3 multiple transcript region,and THAP1/DYT6 has been identified.83
Disease onset of DYT3 dystonia typically occurs inthe mid-thirties (range, 12–52 years), with complete pen-etrance by the end of the fifth decade. The symptomsstart as focal dystonia in almost any part of the bodyand progress to multifocal or generalized dystoniawithin 5 years in most cases. Parkinsonism evolves laterin the disease in about 50% of the patients and canbecome the predominant symptom.125,126 DYT3 dysto-nia is unique among the DYT loci in that neuronaldegeneration has been noted on postmortem analysis.Neuronal loss and astrocytosis have been reported in thecaudate and lateral putamen in 2 patients’ brains127,128
with dramatic depletion of striatosomes and relativesparing of the matrix, suggesting that imbalancebetween the striosomal and matrix-based pathwayscould contribute to the neurologic symptoms.129
DYT5
The disease that would eventually be designated asthe DYT5 locus was initially described by Segawa in1976 under the name hereditary progressive dystoniawith marked diurnal fluctuation (HSP)130 and later byNygaard and colleagues as dopa-responsive dystonia(DRD) because of the dramatic and sustained responseto low-dose levodopa seen in patients.131 The disease isinherited as an autosomal dominant trait with reducedpenetrance that appears to be sex dependent, withfemales expressing symptoms more frequently.132–134 In3 DRD families, the gene was mapped to chromosome14q13135 and subsequently confirmed in an HSP family(Tanaka, 1995). At about the same time, the gene forGTP cyclohydrolase 1 (GCH1) was mapped into theDRD/HSP-linked region of chromosome 14.136 GTPcyclohydrolase 1 is the rate limiting enzyme in the syn-thesis of tetrahydrobiopterin, an essential cofactor fortyrosine hydroxylase, which, in turn, is needed to syn-thesize dopamine. This gene was immediately tested asa positional candidate and mutations identified in HSPpatients.136 More than 100 mutations of all types (non-sense, missense, splicing, promoter region, and largegenomic deletions) have been described in the GCH1gene (for a complete listing, go to http://www.bh4.org),with most arising as new mutations. Comprehensivescreening (including exon deletions) of the GCH1 geneidentifies about 80% of mutations in ‘‘typical’’ DRDpatients,136–139 and comprehensive molecular testing isavailable.The typical phenotype associated with GCH1 muta-
tions includes childhood (average, 6 years) limb-onsetdystonia with worsening symptoms as the day pro-gresses, improvement after sleep, and dramaticresponse to L-dopa therapy. Additional features caninclude arm and axial dystonia, hyperreflexia, andparkinsonism (bradykinesia, hypomimia, posturalinstability),140 and occasionally cranial muscles (upper
O Z E L I U S E T A L .
1110 Movement Disorders, Vol. 26, No. 6, 2011
-
face, oromandibular, laryngeal) may be affected.141
With the identification of the disease gene, the clinicalspectrum of DRD has expanded to include oroman-dibular dystonia,142 spasticity with developmentaldelay mimicking cerebral palsy,143 scoliosis,144 psychi-atric abnormalities,145 and generalized hypotonia withproximal weakness.146
In a minority of cases, DRD can also be inherited as anautosomal recessive disorder with mutations in otherenzymes involved in dopamine synthesis including tyro-sine hydroxylase,147–150 6-pyruvoyltetrahydropterin syn-thase,151 and sepiapterin reductase.139,152,153 Becausethese conditions include deficiencies of serotonin andnorepinephrine as well as dopamine, the clinical manifes-tations are often more severe and can include mental re-tardation, oculogyria, hypotonia, severe bradykinesia,drooling, ptosis, and seizures. However, in 1 family aheterozygous mutation in sepiapterin reductase underliesa typical DRD phenotype.153
Formerly DYT14
Genetic heterogeneity was suggested when a singleSwiss family with autosomal dominant DRD wasmapped to a distinct albeit nearby region on chromo-some 14q13 and designated DYT14.154 Subsequently,an exonic deletion was found in GCH1 and the mis-taken linkage result explained by the finding that 1 ofthe affected members was actually a phenocopy.155
The DYT14 designation has been withdrawn by thehuman genome nomenclature committee.
DYT12
The DYT12 locus was mapped to chromosome19q13 in 2 families156 and confirmed in 2 others.157,158
In these families, the disease is inherited as an autoso-mal dominant trait with reduced penetrance. Usingpositional cloning, 6 heterozygous missense mutationswere identified in the Naþ,Kþ-ATPase alpha 3 subunitgene (ATP1A3), and all were shown to impair cell via-bility in cell culture experiments.159 Currently, a totalof 10 novel mutations (8 missense mutations, a 3-bpin-frame deletion, and a 3-bp in-frame insertion) havebeen reported in 17 families, including 8 de novocases.38,159–166 ATP1A3 encodes the catalytic subunitof the sodium pump that uses ATP hydrolysis toexchange Naþ and Kþ across the cell membrane tomaintain ionic gradients. Functional biochemical studieswith several pathogenic mutations all showed reducedNaþ affinity, suggesting that defects in the handling ofNaþ may be a general feature of the disease.164,167,168
The disease phenotype was first described in1993169 and designated rapid-onset dystonia–parkin-sonism because of key clinical features including ab-rupt onset of dystonia, within hours to weeks, withsigns of parkinsonism (bradykinesia and postural
instability) usually triggered by physical or emotionstress (fever, child birth, running, alcohol binging).The dystonia typically follows a rostrocaudal gradient(face > arm > leg) with prominent bulbar involve-ment.160 The age of onset varies from 4 to 58 yearsbut typically presents in the teens or early twenties.Patients with the typical phenotype can undergo com-mercially available genetic testing; however, becauseof the number of de novo mutations that have beenidentified, a positive family history is not a prerequi-site. One family with an rapid-onset dystonia–parkin-sonism (RDP)-like phenotype but with more cranial-cervical involvement is not linked to chromosome 19qand does not have a mutation in the ATP1A3 gene,thus implicating a second locus for RDP.170
DYT16
An autosomal recessive form of dystonia-parkinson-ism, DYT16, was assigned to chromosome 2q31 usinghomozygosity mapping in 2 consanguineous familiesand a sporadic case, all from Brazil. The same homozy-gous missense mutation (P222L) was identified in theprotein kinase, interferon-inducible double-strandedRNA-dependent activator (PRKRA) gene in the 6affected family members as well as in the 1 sporadiccase.171 The phenotype in these patients is characterizedby early (2–18 years) limb onset (6 of the 7 cases) withprogression to generalized dystonia including promi-nent bulbar involvement with spasmodic dysphonia,dysarthria, and even dysphagia. Four of the affectedmembers in the 2 families also have parkinsonism lim-ited to bradykinesia. A heterozygous frameshift muta-tion leading to a protein truncation was identified in asporadic German case with early-onset dystonia.172
Further screening of early-onset cases will be needed todetermine the overall contribution of this gene to early-onset dystonia and to understand the significance ofheterozygous mutations in this gene. The PRKRA geneis involved in cellular stress response, but exactly howthis may lead to disease is unknown. Possible mecha-nisms of action were reviewed by Bragg et al (2011).173
DYT11
The DYT11 locus was mapped to chromosome 7q21in a large North American family with 10 affected mem-bers174 and subsequently confirmed and narrowed in sev-eral other myoclonus dystonia (M-D) families.175–177
Using classical positional cloning, 5 heterozygous muta-tions were identified in the epsilon sarcoglycan (SGCE)gene in 6 M-D families from Germany.178 Worldwide,more than 50 mutations of all types have been found inthe SGCE gene in more than 100 probands (reviewed inKinugawa et al, 2009179). Genotype/phenotype studieshave not shown any difference in phenotype associatedwith the different types of mutations in SGCE, which is
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1111
-
most likely because all the mutations are thought toresult in loss of function of the protein. Most mutationsare localized to the extracellular domain of the protein,suggesting functional importance. Several nonsense andsmall-deletion mutations have been reported independ-ently and thus appear to be recurrent mutations.179 Inaddition, exonic deletion mutations180,181 and otherlarger deletions have also been reported.182–184 These lat-ter deletions do correlate with phenotype, as they alsoremove other nearby genes and result in more complexmanifestations including skeletal abnormalities, facialdysmorphism, developmental delay, or cavernous cere-bral malformations.182–184 Finally, maternal uniparentaldisomy can also cause M-D because of imprinting (inac-tivation) of both maternal genes.185
M-D linked to the DYT11 locus is inherited as anautosomal dominant trait with reduced penetrancerelated to maternal imprinting.178 Imprinting is an epige-netic phenomenon that results in the selective silencingof 1 of the 2 parental alleles, in the case of SGCE, bypromoter methylation.186,187 Consequently, diseaseexpression is dependent on the sex of the transmittingparent, with almost all individuals who inherit an SGCEmutation from their father showing symptoms. Imprint-ing of SGCE is supported by RNA expression studiesthat revealed expression of only the mutant allele inaffected individuals and expression of the normal allelein unaffected mutation carriers.186,187 Maternal imprint-ing has also been reported for the mouse Sgce gene,188
whereas in heterozygous Sgce-knockout mice, exclusiveexpression of the paternal allele was found in mousebrains.189 However, up to 5% of M-D cases inherit theirmutated allele from their mothers178,187 and presumablyalso express the wild-type allele from their fathers. Thereason for reversal of the maternal imprint in these casesis not known.SGCE is a member of a gene family that also includes
alpha, beta, gamma, delta, and zeta sarcoglycans. Muta-tions in the genes encoding these other sarcoglycans,which are mainly expressed in muscle, cause autosomalrecessive limb-girdle muscular dystrophies.190 The sarco-glycans encode transmembrane components of the dys-trophin-glycoprotein complex that links the cytoskeletonto the extracellular matrix.191 SGCE is 68% homologousto alpha-sarcoglycan and can functionally replace it inskeletal muscle.192 It is widely expressed in embryonicand adult tissues including the brain,193–195 and a brain-specific transcript results from an alternatively splicedmessage with a unique C-terminus.189,196 However,SGCE function in the brain is largely unknown. In thecell, the protein is located at the plasma membrane. Stud-ies expressing pathogenic M-D missense mutations showimpair trafficking of the mutant protein to the plasmamembrane and degradation by the proteasome that isenhanced by an interaction with torsinA (the proteinencoded by TOR1A/DYT1).56
M-D is characterized by a combination of brieflightning-like myoclonic jerks and dystonia that usu-ally begins in childhood. Onset occurs earlier in girlsthan in boys regardless of mutation type.197 Myoclo-nus is usually the presenting symptom and most oftenaffects the neck, trunk, and upper limbs, with legsaffected less prominently. About two thirds of patientswith M–D show dystonia, mostly cervical dystonia orwriter’s cramp,41,198,199 which tends to remain mild.The myoclonic jerks typically show a dramaticresponse to alcohol in many patients.200,201 In addi-tion, prominent psychiatric manifestations includingdepression, anxiety, panic attacks, and obsessive-compulsive disorder (OCD) have been reported,202,203
and in particular, OCD has been found in those notaffected with motor signs,204–206 suggesting it isrelated to the genetic defect. The proportion of M-Dand clinically related phenotypes from SGCE muta-tions is debated and depends on the clinical criteriaused to select subjects for screening as well as thescreening method.207 Up to 50% of ‘‘typical’’ M-Dcases will have a mutation in the SGCE gene; how-ever, this percentage increases in familial cases withpaternal inheritance. Therefore, these factors shouldbe considered when deciding on which M-D patientsto test.
DYT15
Although the SGCE gene appears to be a majorlocus for M-D, sporadic and familial cases withoutmutations in SGCE have been reported,181,208–211 sug-gesting genetic heterogeneity. One of these families,with autosomal dominant inheritance and reducedpenetrance, was used to map a second locus for M-Dto chromosome 18p.211 This Canadian family has 13affected members, with average age at onset of 9.6years (range, 7–15 years) and typical alcohol-respon-sive M-D. Fine-mapping studies in this family hasrefined the locus to a 3.2-Mb region; however, all thegenes in this interval have been sequenced and nomutations identified.212
Paroxysmal Dystonia/Dyskinesia
This is a heterogeneous group of disorders charac-terized by sudden transient attacks of involuntarymovements. They are subdivided into kinesigenic(DYT10 and DYT19), nonkinesigenic (DYT8 andDYT20), and exercise-induced forms (DYT9 andDYT18). The genes for DYT8 and DYT18 have beenidentified.3
DYT8
Paroxysmal nonkinesigenic dyskinesia (PNKD1) isinherited as an autosomal dominant trait with high pen-etrance. The DYT8 locus was localized to chromosome
O Z E L I U S E T A L .
1112 Movement Disorders, Vol. 26, No. 6, 2011
-
2q33–36 in 2 families, a 5-generation Italian family213
and a large Polish-American family214; then subse-quently, the region was narrowed in a third family.215
Two missense mutations (A7V and A9V) were identifiedin the myofribillogenesis regulator (MR-1) gene.216,217
These 2 missense mutations have been found in 14unrelated families on different haplotype backgroundsand appear to be mutation hot spots.216–220 A thirdmissense mutation (A33P) was reported in this gene ina single family.221 The transcript is alternatively spliced,resulting in at least 3 isoforms, 1 of which is specificallyexpressed in the brain.217 The function of the MR-1gene is unknown, but its sequence is closely related tohydroxyacylglutathione hydrolase,217 an enzyme knownto detoxify methylglyoxal, which is produced as a by-product of oxidative stress and found in coffee andalcohol. Lee et al217 proposed that impaired function ofMR-1 might block this pathway, resulting in the accu-mulation of methylglyoxal and explain how alcohol,stress, and caffeine might precipitate attacks. However,a recent study showed that several of the MR-1 iso-forms are targeted to the mitochondria via an N-termi-nal mitochondrial targeting sequence (MTS) that iscleaved off the mature protein. All 3 PNKD-associatedmutations are in the cleaved MTS peptide, suggesting apossible toxic gain-of-function mechanism.221
PNKD is characterized by attacks of dystonia, cho-rea, ballismus, or athetosis, often provoked by alcoholor caffeine. The episodes last from minutes to hours,with a frequency from once per day to 1 or 2 peryear. The age at onset is typically in childhood or ado-lescence but can be as late as 50 years.222 Comparisonof MR-1 mutation–positive and –negative casesrevealed that an earlier age at onset, precipitation ofattacks with alcohol and caffeine but not exercise orfatigue, and lack of seizures distinguished the muta-tion-positive cases223 and that when these strict crite-ria were applied, the MR-1 patients were clinicallysimilar to the original description by Mount andReback (1940).224 Genetic testing for PNKD shouldbe considered for patients who meet these strict crite-ria, with testing for the recurrent mutations done first.PNKD can be distinguished clinically from PKC(DYT10/19), in which attacks are shorter, more fre-quent, and triggered by sudden movement, and fromPED (DYT9/18), which is precipitated by prolongedexercise.
DYT9
This locus was assigned to a 12-cM interval onchromosome 1p21–p13.3 in a large German familywith 18 affected members and clear autosomal domi-nant inheritance.225 Age at onset ranged from 2 to 15years, and symptoms included episodes of involuntarydystonia of the limbs, dysarthria, double vision, par-oxysmal choreoathetosis, episodic ataxia, and dyskine-
sia. In addition, 5 members had constant spasticparaplegia. Episodes usually lasted approximately 20minutes and occurred between twice a day and twicea year. Attacks are precipitated by physical exercise,emotional stress, fatigue, and alcohol. This disorderhas been termed paroxysmal choreoathetosis/spastic-ity. Both the phenotype and the chromosomal locationoverlap with the DYT18 locus (see below), which hasrecently been identified and can now be tested in thisfamily to determine if these are the same disorder.
DYT10
In 8 Japanese families showing autosomal dominantinheritance of paroxysmal kinesigenic dyskinesia(PKD), linkage analysis was used to map the DYT10locus on chromosome 16p11.2–q12.1.226 This wasconfirmed in an African American family227 as well asin 4 new families, in which 157 genes within the criti-cal region were sequenced, with no pathogenic muta-tions identified.228 The disease is characterized byshort (seconds to minutes), frequent (up to 100 timesper day) attacks of dystonic or choreiform movementsprecipitated by sudden unexpected movements. Age atonset is usually during childhood or adolescence, butsymptoms can resolve in adulthood.227 A second locusfor PKD, designated DYT19, maps to an overlappingregion and thus may represent the same locus (seebelow). In addition, another PKD pedigree has beenexcluded from linkage to chromosome 16 and thusmost likely represents a novel PKD locus.229
DYT18
Paroxysmal exercise-induced dyskinesia (PED)shows an autosomal dominant inheritance patternwith slightly reduced penetrance. The locus was identi-fied by candidate gene search in 1 case230 and by link-age analysis in a second.231 Based on several clinicalclues including various CSF glucose parameters andthe co-occurrence of hemolytic anemia with PED in 1family, the SLC2A1 gene encoding glucose transporter1 (GLUT1) was screened and a mutation identified in3 families.230 Around the same time, linkage analysisin a 5-generation Belgian family with PED and epi-lepsy identified a region on chromosome 1p35–p31that included the SLC2A1/GLUT1 gene. Mutationswere identified in this and 3 other PED families.231
Mutations in SLC2A1 have also been found in spo-radic cases of PED232 and in a family with dystonictremor as the presenting feature.233 SLC2A1/GLUT1is the main glucose transporter in the brain. PED isthought to be caused by reduced glucose transportinto the brain, particularly when energy demand ishigh after prolonged exercise.230,231
PED is characterized by exercise-induced attacks ofdystonic, choreoathetotic, and ballistic movementsaffecting the exercised limbs that last from a few
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1113
-
minutes to an hour.234,235 The disease usually has itsonset in childhood and can have other disease mani-festations including epilepsy, migraine, developmentaldelay, and hemolytic anemia.230,231 The DYT9 criticalregion is in an overlapping interval of chromosome1p, and the phenotype resembles that of DYT18;therefore, it is possible these are the same disease.
DYT19
DYT19 is the designation for the second locus forparoxysmal kinesigenic dyskinesia (PKD2). This locuswas mapped to chromosome 16q13–q22.1 in an In-dian family with 13 affected members.236 This regionis in close proximity to the DYT10 locus and overlapsthis locus in 1 family.227 The clinical features in thisfamily mimic those of DYT10-associated PKD1, sug-gesting they may be the same locus; however, until agene is found for either locus, this will remain uncer-tain. In the Indian family, the age at onset rangedfrom 7 to 13 years. Attacks could last up to 2minutes, occurred with a frequency of 1–20 per day,and produced dystonic or choreic movements inresponse to sudden movements. Several affected mem-bers showed spontaneous remission by age 23.229
DYT20
This locus designates a second form of paroxysmalnonkinesigenic dyskinesia (PNKD2), which wasdescribed in a single Canadian family with 10 affectedmembers. Linkage analysis in this family assigned thelocus to chromosome 2q31, just proximal to theDYT8/MR-1 gene.237 No mutations were detected inthe MR-1 gene, and thus a new PNKD locus was des-ignated. The clinical symptoms in this family are verysimilar to those described in the DYT8/MR-1 families.Detection of mutations in a different gene than MR-1will be required to confirm the existence of this secondform of PNKD.
Genetics Summary
The genes involved in monogenic forms of dystoniareflect the clinical heterogeneity of the dystonias.Although the genes identified to date are diverse andat present, the underlying functions of most of thesegenes and how they lead to dystonia remain elusive,their identification has fostered basic research (devel-opment of animal and cellular models) aimed atunderstanding the pathophysiology of dysto-nia.173,238,239 The recent discovery that Thap1 bindsto the TOR1A promoter81,82 and the potential associ-ation of variants in TOR1A and THAP1 with suscep-tibility to focal/segmental PTD suggests that commonpathways may be involved in dystonia, and thus noveltherapeutics targeting these common pathways couldbe effective for the treatment of different forms of dys-
tonia. The definition of genetic subtypes has alsoallowed clinical researchers to compare and contrastthese subtypes to better understand the common andunique pathophysiology that should help direct thera-pies and define endophenotypes240,241 that can eventu-ally be applied back to families with dystonia to helpelucidate more genes. Finally, harnessing the newgenetic technologies, including Chip-seq for genome-wide identification of transcription factor–binding sites(related to downstream targets of TAF1 and THAP1)and next-generation exomic and whole-genomesequencing, should accelerate gene discovery for dysto-nias that in turn should further elucidate the underly-ing pathways.
Neurophysiology and Imaging
Over the last 25 years important advances in ourunderstanding of dystonia pathophysiology have comefrom work using neurophysiologic and imaging techni-ques; they have been applied to clinical and etiologicsubtypes of dystonia, especially genetic PTD subtypesand focal dystonias. See Table 2 for highlights of dys-tonia physiology, imaging, and treatment.
Neurophysiology
Three interrelated neurophysiologic abnormalitieshave been identified: impaired inhibition including sur-round inhibition, increased plasticity, and sensoryprocessing dysfunction.Loss of inhibition was an early finding; both loss of
reciprocal inhibition in patients with arm dysto-nia242,243 and abnormalities in blink reflex recovery inblepharospasm244 were discovered more than 20 yearsago. These findings of inhibitory dysfunction werethought to help explain the cocontraction of antago-nists that marks action-induced dystonia. Both theseabnormalities were thought to be a result of dysfunc-tion in supraspinal control, particularly corticostriato-thalamocortical circuitry and the ability to select awanted movement and inhibit unwanted ‘‘overflow.’’Thus, cortical inhibition was interrogated next, usingtechniques that employed transcranial magnetic stimu-lation (TMS). These studies demonstrated loss ofshort245,246 and long247 intracortical inhibition and ashortened silent period.247 Other work focused ondemonstrating a lack of surround inhibition, assessingMEP amplitudes of antagonist hand muscles in sub-jects with writer’s cramp.248
These studies all point to deficient inhibition as acorrelate of having a dystonic movement. However,the meaning of these neurophysiologic findings vis-à-vis dystonia etiology and brain mechanisms producingdystonic movements is unclear. For example, DYT1gene carriers not manifesting dystonia,249 and subjects
O Z E L I U S E T A L .
1114 Movement Disorders, Vol. 26, No. 6, 2011
-
with psychogenic dystonia246 also have abnormalintracortical inhibition and a shortened silent period.Another feature of dystonia recognized in the past
25 years is increased plasticity. One of the first find-ings invoking enhanced plasticity was the Byl monkeymodel250 of task-specific hand dystonia. That modeldisplays dedifferentiated hand representation in theprimary somatosensory cortex. Similarly, a degradedhomunculus with enlarged receptive fields was identi-fied in subjects with focal hand dystonia.251 Both sug-gest that repeated afferent input from overtraining oroveruse could lead to dystonia by driving improperlyadjusted cortical plasticity. Subsequent support forabnormalities in plasticity has derived from studies ofprimary dystonia patients using indirect measures oflong-term potentiation and depression, includingpaired associative stimulation (PAS) and TMS. Usingtheta bursts of TMS, both DYT1 mutation carrierswith dystonia and torticollis subjects had prolongedresponses compared with controls. Interestingly, incontrast, nonmanifesting carriers had no response,suggesting a hyperregulated state that may protect
these individuals from developing dystonia.252 Severalstudies have assessed PAS in focal dystonia, findingenhanced effects consistent with increased plasticitybut also loss of spatial specificity253–255; the latter isconsistent with loss of surround inhibition. Recurringquestions are whether the presence of increased plas-ticity derives from impaired inhibition and whethermeasures of cortical inhibition and plasticity are neces-sary correlates of dystonia. To help address thesequestions, psychogenic and organic dystonia subjectswere studied using tests of cortical inhibition and plas-ticity. Again, there was evidence of impaired intracort-ical inhibition in both groups of patients, butabnormal plasticity as measured by PAS was observedonly in those with organic dystonia.256
A third focus of neurophysiologic investigation hasbeen the study of sensory function. Although clinicallyovert sensory abnormalities are not a feature of dysto-nia, several lines of evidence stimulated this focus ofresearch including the efficacy of sensory tricks, thepresence of dystonia after trauma or in cases ofchronic regional pain, and sensory abnormalities
TABLE 2. Highlights in Dystonia Physiology, Imaging, and Treatment
1985–1989Dystonic movements characterized as having abnormally long EMG bursts, co-contraction of antagonists, and overflow to unintended musclesFindings of abnormal inhibition in dystonia patients: abnormal blink reflex recovery in blepharospasm, and loss of reciprocal inhibition in patients with writ-er’s cramp.Various task specific dystonias and traumatic dystonias describedDouble blind prospective trial establishes efficacy of high dose trihexyphenidyl in primary generalized dystonia.Intrathecal baclofen found to be most beneficial for patients with secondary dystonia associated with spasticity or pain.BotoxVR receives FDA approval for treatment of blepharospasm and VIIth nerve disorders.First study of BoNT for cervical dystoniaFirst report of BoNT for spasmodic dysphonia
1990–1994FDG PET defines relative metabolic overactivity of the lentiform nucleus and premotor cortices.Loss of intracortical inhibition in PTD describedIntroduction of the hypothesis of dystonia as a disorder of sensory processing.Numerous descriptions of secondary dystonia with pathology involving striatum, cerebellum, parietal lobe, and brainstem.
1995–1999Monkey model of task specific dystonia displaying enlarged sensory receptive fields is described, supporting theory of increased plasticityAbnormal somatosensory cortical representation identified in focal hand dystoniaRodent model of blepharospasm created by partial dopamine depletion and partial weakening of orbicularis oculiPET studies demonstrate a hypermetabolic pattern involving lentiform, cerebellum, and supplementary motor area in DYT1 gene carriers whether or notthey have dystoniaIntra-operative neuronal activity recorded from GP and thalamus of dystonia patients identifies abnormalities in firing patternsStriatal dopamine receptor binding abnormalities detected by PET in focal dystoniaPallidotomy begins to replace thalamotomy as preferred surgical treatment for generalized dystonia.First report of GPi DBS for treatment of generalized dystonia
2000–2004Multiple reports of defects in sensory processing, especially temporal processingFailure of surround inhibition identified using paired associative stimulation (PAS).Animal models of DYT1 dystonia developed
2005–2010Abnormal motor cortex plasticity in different dystonia subtypesBasal ganglia interactions are demonstrated in cerebellar animal models of dystoniaDTI MRI demonstrates that connectivity of cerebellothalamic and thalamocortical pathways regulates penetrance in genetic PTDStudies of DYT1 transgenic mice support D2 receptor dysfunctionTwo double-blind controlled trials of bilateral GPi DBS for treatment of primary generalized dystonia demonstrate significant reduction of dystonia symp-toms and functional disabilityReports of good outcomes after GPi DBS for various forms of secondary dystonia (PKAN, Lubag, tardive dystonia) and dystonic storm
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1115
-
identified in the monkey model. And, indeed, subtlebut significant abnormalities in spatial and temporaldiscrimination have been uncovered,257 as have SEPabnormalities.251 The sensory findings appear to be adystonia endophenotype, in that the dysfunction is notdirectly dependent on the presence of dystonic move-ments per se. For example, temporal discrimination isabnormal in DYT1 gene carriers that do not manifestdystonia,258 and it is also abnormal in the unaffectedlimbs of patients with focal dystonia.259
How these neurophysiological findings come to-gether mechanistically to explain dystonia remainsconjectural; indeed, because dystonia is so etiologicallyand clinically heterogeneous, it may be best to onlyconsider data and hypotheses restricted to one etiologyor phenotype. Nevertheless, one proposed overarchingexplanation240 draws from pathological studies of sec-ondary dystonias as well as deep brain stimulation(DBS) experience in primary dystonia patients260 andDYT1 animal findings.261 These point to dysfunctionin GPi that may in some etiologies be related toabnormal striatal dopaminergic signaling andincreased cholinergic tone262,263; this dysfunction leadsto abnormal synchronization of the basal ganglia out-put to the thalamus and sensory feedback misprocess-ing. Together they have the effect of increasingstriatal, brain stem, and cortical plasticity and overtime producing neural reorganization and overt dysto-nia. The various etiologies may feed into this cycle ofevents in different and multiple ways, including thepresence of trauma or overuse that may be more orless important in driving neural reorganization.
Imaging
Imaging studies have extended the findings of theneurophysiological studies by delineating cerebral met-abolic and microstructural abnormalities in dystoniapatients and gene carriers that point to disturbed con-nectivity in both the cortico-striato-pallido-thalamo-cortical and cerebello-thalamocortical pathways. Inearly studies using FDG-PET imaging, Eidelberg andcolleagues applied a principal-components analysis toidentify disease-specific patterns of covarying meta-bolic activity, first in patients with sporadic dystoniaand then in both manifesting and nonmanifestingDYT1 gene carriers.264 These patients expressed anabnormal metabolic brain network characterized byrelative increases in the posterior putamen/globus pal-lidus, cerebellum, and supplementary motor area(SMA). These changes are often referred to as trait orgenotype specific.264
Nonmanifesting DYT6 gene carriers were found tohave a somewhat different pattern of abnormalities,with regional hypometabolism in the putamen, cere-bellum, and upper brainstem and hypermetabolism inthe temporal cortex.39,265 Although the trait-related
metabolic abnormalities differed across genotypes, allDYT1 and DYT6 patients with dystonia showed rela-tive metabolic increases in the pre-SMA and parietalassociation regions regardless of genotype or heteroge-neous clinical manifestations.265 More recent studieshave identified a distinct metabolic pattern related toclinical penetrance (termed state- or phenotype-associ-ated changes as opposed to trait or genotype), charac-terized by relative increases in the pre-SMA andparietal association cortices and also relative reduc-tions in the cerebellum, brain stem, and ventral thala-mus.39 This pattern distinguished manifesting fromnonmanifesting carriers across genotypes. These find-ings are consistent with an important role of sensori-motor processing dysfunction in the clinicalpenetrance of dystonia.39
Further support for maladaptive sensorimotor proc-essing has been provided by oxygen-labeled H2O PETstudies of DYT1 gene carriers tested in 2 scenarios;one assessed brain activation during a simple motortask and the other tested activation in a nonmotoraudiovisual setting.266 Not surprisingly differenceswere noted between manifesting and nonmanifestingcarriers. Both had a pattern of increased activation inthe nonmotor setting involving the sensorimotor cor-tex, dorsal premotor cortex, supplementary motorarea, and cerebellum. When performing a motor task,however, only the manifesting carriers had increasedactivation. This dissociation between motor and non-motor patterns suggests an underlying genotype-proc-essing abnormality in the sensory integration ofaudiovisual input and then additional motor-activateddysfunction.The pathoanatomic basis for penetrance, the differ-
ence between manifesting and not-manifesting dysto-nia in susceptible individuals, may relate todevelopmental structural defects in the cerebello-thalamo-cortical pathway. Evidence for microstruc-tural abnormalities have been identified in diffusiontensor imaging (DTI) studies of focal and geneticforms of dystonia.267–270 The most recent studies ofboth manifesting and nonmanifesting DYT1 andDYT6 gene carriers point to critical abnormalitiesinvolving cerebellothalamic tracts; nonmanifestingmutation carriers, however, appear to have additionalfiber tract disruption, situated distally along the thala-mocortical segment of the pathway (in tandem withthe proximal cerebellar outflow abnormality). In indi-vidual gene carriers, clinical penetrance appears to bedependent on the difference in connectivity for these 2tracts.39,266,271 The cerebellum has been suggested tohave a prominent role in modulating cortical plastic-ity,272–274 so that basal abnormalities in the cerebel-lum and its outflow pathways may give rise toalterations in cortical activation responses duringmovement and learning, leading to the functionalchanges seen in dystonia.
O Z E L I U S E T A L .
1116 Movement Disorders, Vol. 26, No. 6, 2011
-
Hand in hand with findings pointing to the importof the cerebellum and thalamus and their outflow isthe more traditional focus on the basal ganglia anddopaminergic mechanisms. Dopaminergic deficits areknown to be etiologic in secondary dystonias such asdystonia in Parkinson’s disease and dopa-responsivedystonia and also in primary inherited dystonia, whereDYT1 animal models displayed D2 receptor dysfunc-tion.263,275 In this setting, early PET and SPECT stud-ies in primary dystonia subjects tested striatal D2receptor binding, and moderate reductions were iden-tified.276,277 More recently, reduced D2 receptor avail-ability has been identified in DYT1 and DYT6mutation carriers regardless of whether dystonic signswere manifest.278 These findings of dopaminergic dys-function are consistent with neurophysiologic and ani-mal studies in supporting abnormalities in dopaminesignaling and consequent GPi firing. How they relateto the microstructural abnormalities of cerebellothala-mic and thalamocortical tracts detected by MRI DTIin the same cohort of DYT1 and DYT6 mutation car-riers still needs to be worked out. Determining thetemporal–causal relationships of microstructural neu-rodevelopmental defects verses functional and possiblysecondary/downstream changes remains a challengefor future studies of PTD.
Therapy
The landscape of treatment options for dystonia hasdramatically changed over the last 25 years, first withthe introduction of botulinum toxin injections for thetreatment of focal dystonias and then with the adventof DBS surgery for generalized dystonia. For decades,treatment for many forms of dystonia relied on oralmedications, which were often only modestly effectiveand frequently caused significant adverse effects. How-ever, with the widespread application of these 2 thera-peutic options over the last 2 decades, thearmamentarium for clinicians treating patients withdystonia has been radically expanded and improved.
Oral Medications
The efficacy of high-dose trihexyphenidyl for treat-ment of primary generalized dystonia was establishedin a double-blind prospective trial by Burke and col-leagues in 1986.279 Since then, there has been little inthe way of major progress in identifying oral medicaltherapies for primary dystonia, although medical treat-ments for the nonprimary dystonias have advanced;these latter include levodopa for DRD, tetrabenazineand clozapine for tardive syndromes, and therapies formetabolic syndromes such as glutaric acidemia. In cur-rent practice, options for oral medications for primarydystonia remain essentially the same as in prior deca-
des and consist of anticholinergics (particularly trihex-yphenidyl), baclofen, benzodiazepines, and levodopa.Although trihexyphenidyl is an established first-line
oral medication for primary generalized dystonia, it canalso be used for symptomatic treatment of secondarydystonia, although there is a paucity of data regardingthis use. Two recent small studies have addressed thequestion of the efficacy of trihexyphenidyl for treatmentof children with dystonic cerebral palsy, with inconclu-sive results.280,281 Data are similarly lacking regardingthe question of efficacy of levodopa for treatment ofnon-DRD forms of dystonia. Levodopa has beenreported to provide benefit in some patients withDYT1 dystonia,282,283 and isolated case reports havedescribed good responses to levodopa in various formsof secondary dystonia284–287; its use in these forms ofdystonia thus warrants further investigation.
Intrathecal and Intraventricular Baclofen
Intrathecal baclofen infusion has also been used fortreatment of generalized dystonia refractory to oralmedications, but it has been found to be most benefi-cial for patients with secondary dystonia, when dysto-nia occurs in association with spasticity or pain, suchas in patients with dystonia from cerebral palsy.288–290
More recently, the use of intraventricular baclofen,with intraventricular catheters placed endoscopicallyin the third ventricle, has been explored for the treat-ment of severe secondary generalized dystonia refrac-tory to oral medications. Results of a small studyshowed good response in 8 of 10 patients.291
Botulinum Toxin
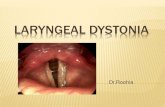
Treatment of various forms of focal dystonia, previ-ously limited to oral medications that had limited effi-cacy and frequent systemic side effects, has beentransformed by the introduction of botulinum toxin(BoNT) treatment. BoNT is a highly effective localtreatment that causes minimal side effects. The toxinblocks the vesicular release of acetylcholine into theneuromuscular junction, causing temporary local che-modenervation and resultant muscle weakness, reduc-ing the excessive activity of dystonic muscles.Blepharospasm was one of the first studied indicationsfor BoNT treatment, and Botox received FDA approvalfor blepharospasm or cranial nerve VII disorders in1989. Since the early reports and studies in the 1980sand ’90s, BoNT injections have become a crucial treat-ment option for various forms of focal dystonia. BoNTis currently the first-line treatment for blepharospasm,cervical dystonia, laryngeal dystonia (spasmodic dys-phonia), and focal upper extremity dystonia and is alsofrequently used for hemifacial spasm, oromandibulardystonia, and focal lower limb dystonia.292
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1117
-
Cervical dystonia (CD) is a frequent dystonia, witha prevalence of approximately 20–200 per million293
and is typically a lifelong disorder causing significantdisability because of dystonic posture and pain. Treat-ment options prior to the introduction of BoNT con-sisted primarily of oral medications that had limitedoverall efficacy at tolerated dosages and selective pe-ripheral denervation. The first study evaluating BoNT-A for CD was published in 1985294 and was a single-blind study of 12 patients with cervical dystonia andshowed improvement in head posture and pain in92%, with the only adverse event being transient neckweakness in 3 patients. Since that time there havebeen approximately 80 studies evaluating BoNT forCD, including 8 prospective, double-blind, random-ized, controlled clinical trials meeting the criteria forclass I evidence.292,295
Prior to BoNT, treatment options for patients withspasmodic dysphonia (SD) were limited to speech ther-apy and psychotherapy, both with poor results. Otherforms of denervation procedures of the recurrent la-ryngeal nerve were also explored that had initiallygood results but many long-term failures.295 Blitzeret al gave the first laryngeal injection of BoNT for SDin 1984,296 and experience in 1300 patients over sub-sequent years has shown BoNT to be a safe and effec-tive treatment for laryngeal dystonia.295
BoNt is also currently the treatment of choice forfocal upper extremity dystonia, including task-specificdystonias such as writer’s cramp and musician’s dysto-nia. Oral medications for treatment of these forms ofdystonia can provide some benefit but only in somepatients, and their use is often limited by side effects.
DBS Surgery for Dystonia
In the mid-20th century, surgical treatment for gen-eralized dystonia consisted of lesional surgeries, classi-cally targeting the thalamus. Although bilateralthalamotomy provided significant benefit to dystonicsymptoms in some patients, it also frequently causedpermanent, disabling neurological side effects, particu-larly dysarthria. Subsequently, the observation thatpallidotomy in patients with Parkinson’s disease allevi-ated off-dystonia symptoms led to interest in theglobus pallidus as the optimal surgical target in treat-ment of dystonia. After the introduction of DBS forthe treatment of essential tremor and Parkinson’s dis-ease in the mid-1990s established DBS as an alterna-tive to ablative procedures for treatment of movementdisorders, bilateral pallidal stimulation began to beused for treatment of generalized dystonia.The first report of DBS for dystonia was by Mun-
dinger in 1977, who reported benefit of unilateral,intermittent, low-frequency thalamic stimulation in 7patients with cervical dystonia.297 Reports of DBS fordystonia next appeared in 1999 and the early 2000s
and suggested that the GPi was the preferred target.Further, in some patients with primary generalizeddystonia, especially those with DYT1 dystonia, theresponse was dramatic.298 Two double-blind, con-trolled trials of bilateral GPi DBS for treatment of pri-mary generalized dystonia were reported, and bothfound significant reduction in dystonic symptoms andfunctional disability.299,300 Subsequently, bilateral GPiDBS has become a crucial treatment option forpatients with medically refractory primary generalizeddystonia. With DBS, patients who in the past wouldhave been restricted to a life of severe motor disabilityfrom a young age can now lead lives with only mini-mal symptoms. In addition, studies of long-term fol-low-up of DBS in dystonia patients have foundsustained clinical improvement in patients followedfor up to 8 and 10 years.301,302
However, important questions remain regarding theuse of DBS for dystonia. Although some dystoniapatients respond dramatically to DBS, there has beensignificant variability in the response across all thepublished reports, pointing to the crucial question ofpatient selection and factors predictive of response toDBS. Alhtough no predictive factors have been defini-tively established, several studies including meta-analy-ses point to lower preoperative severity score, youngerage at surgery, positive DYT1 mutation status, shorterduration of disease, and the lack of fixed skeletal de-formity as possible predictive factors.303–307 The ques-tion of whether DBS is as effective for treatment ofnon-DYT1 forms of primary generalized dystoniaremains unclear. Recent reports of DBS in a smallnumber of patients with DYT6 dystonia have shownless robust results than in DYT1 patients.69,73
Further, although the use of DBS for the treatmentof primary generalized dystonia, and especially DYT1dystonia, has become widely accepted, the question ofwhether DBS may be effective in various forms of sec-ondary dystonia remains unresolved. Data regardingthe efficacy of DBS for secondary dystonia consists,with one recent exception, of individual case reportsor small case series with heterogeneous forms of sec-ondary dystonia, with results ranging from no benefitto dramatic improvement. In 2009, Vidailhet et alreported a multicenter prospective pilot study of bilat-eral pallidal DBS in 13 adults with dystonia-choreoa-thetotic cerebral palsy.308,309 The response in thesepatients was again heterogeneous; therefore, the ques-tion of DBS for secondary generalized dystonia fromcerebral palsy requires further investigation. Casereports of good outcomes of DBS in patients with cer-tain forms of secondary dystonia, such as dystonia dueto the heredo-degenerative diseases PKAN (pantothe-nate kinase deficiency) and Lubag syndrome (X-linkeddystonia parkinsonism), suggest a potential role forDBS.309–313 In addition, recent reports of small series
O Z E L I U S E T A L .
1118 Movement Disorders, Vol. 26, No. 6, 2011
-
of patients with DBS for treatment of severe tardivedystonia have also been promising.314–316 Patientswith myoclonus-dystonia have also been found tohave good responses to DBS.317–319 Bilateral GPi DBShas also been reported to be effective as a treatmentfor status dystonicus because of various underlyingcauses and should therefore be considered in the acutemanagement of this life-threatening condition.320–322
Future Directions in Treatment
Although the last 25 years have seen dramaticadvances in treatment options for dystonia, there havebeen no significant advances in oral medications forprimary dystonia, and all existing treatments includingBoNT and DBS remain essentially symptomatic. Tar-geted treatments aimed at etiologic mechanisms ofdystonia remain the ultimate goal of treatment.Possibilities for potential novel therapies for dysto-
nia have emerged out of recent basic science advancesrelated to underlying molecular and neurochemicalpathophysiologic mechanisms of dystonia. A study byNapolitano and colleagues investigating dopamine D2receptor (D2R) transmission in a transgenic mousemodel of DYT1 dystonia demonstrated a link betweenthe torsinA mutation and D2R dysfunction and foundthat pharmacological blockade of adenosine A2Areceptors restored the abnormal plasticity seen in theDYT1 mice. This suggests that antagonism of A2Areceptors can counteract the abnormal D2 receptor–mediated transmission in the mutant mice and, as theauthors note, opens new perspectives for treatment ofDYT1 dystonia.263
Along another line of inquiry related to DYT1 dys-tonia, Cao et al reported results of the first screen forcandidate small-molecule therapeutics for dystonia inwhich they searched for compounds that couldenhance wild-type torsinA activity. They found 2classes of antibiotics, quinolones and aminopenicillins,that enhance wild-type torsinA activity and furtherfound that a behavioral defect associated with aDYT1 mouse knock-in model was rescued followingadministration of ampicillin.323
Ultimately, continued further investigation into thegenetic, molecular, neurochemical, and functional–anatomical mechanisms of dystonia will lead to better,more rational targeted therapies for all forms ofdystonia.
References1. Fahn S, Marsden CD, Caine DB, eds. Dystonia 2. Advances in
Neurology.1988.
2. de Carvalho Aguiar PM, Ozelius LJ. Classification and genetics ofdystonia. Lancet Neurol. 2002;1:316–325.
3. Muller U. The monogenic primary dystonias. Brain. 2009;132:2005–2025.
4. Nutt JG, Muenter MD, Aronson A, Kurland LT, Melton LJ 3rd.Epidemiology of focal and generalized dystonia in Rochester,Minnesota. Mov Disord. 1988;3:188–194.
5. Epidemiological Study of Dystonia in Europe (ESDE) Collabora-tive Group. A prevalence study of primary dystonia in eight Euro-pean countries. J Neurol. 2000;247:787–92.
6. Risch N, de Leon D, Ozelius L, et al. Genetic analysis of idio-pathic torsion dystonia in Ashkenazi Jews and their recent descentfrom a small founder population. Nat Genet. 1995;9:152–159.
7. Muller J, Kiechl S, Wenning GK, et al. The prevalence of primary dys-tonia in the general community. Neurology. 2002 Sep 24;59:941–943.
8. Ozelius LJ, Bressman SB. Genetic and clinical features of primarytorsion dystonia. Neurobiol Dis. 2011;42:127–135.
9. Norgren N, Mattson E, Forsgren L, Holmberg M. A high-pene-trance form of late-onset torsion dystonia maps to a novel locus(DYT21) on chromosome 2q14.3-q21.3. Neurogenetics. 2011[Epub ahead of print].
10. Ozelius LJ, Hewett JW, Page CE, et al. The early-onset torsiondystonia gene (DYT1) encodes an ATP-binding protein. NatGenet. 1997;17:40–48.
11. Fuchs T, Gavarini S, Saunders-Pullman R, et al. Mutations in theTHAP1 gene are responsible for DYT6 primary torsion dystonia.Nat Genet. 2009;41:286–288.
12. Schwalbe W. Eine eigentumliche tonische Krampform mit hyster-iscehn Symptomen. Medicin and chirurgie. 1908.
13. Zeman W, Dyken P. Dystonia musculorum deformans. clinical,genetic and pathoanatomical studies. Psychiatr Neurol Neurochir.1967;70:77–121.
14. Eldridge R. The torsion dystonias: literature review and geneticand clinical studies. Neurology. 1970;20:1–78.
15. Zilber N, Korczyn AD, Kahana E, Fried K, Alter M. Inheritanceof idiopathic torsion dystonia among Jews. J Med Genet. 1984;21:13–20.
16. Bressman SB, de Leon D, Brin MF, et al. Idiopathic dystoniaamong Ashkenazi Jews: evidence for autosomal dominant inheri-tance. Ann Neurol. 1989;26:612–620.
17. Risch NJ, Bressman SB, deLeon D, et al. Segregation analysis ofidiopathic torsion dystonia in Ashkenazi Jews suggests autosomaldominant inheritance. Am J Hum Genet. 1990;46:533–538.
18. Fletcher NA. The genetics of idiopathic torsion dystonia. J MedGenet. 1990;27:409–412.
19. Pauls DL, Korczyn AD. Complex segregation analysis of dystoniapedigrees suggests autosomal dominant inheritance. Neurology.1990;40:1107–1110.
20. Kramer PL, Heiman GA, Gasser T, et al. The DYT1 gene on9q34 is responsible for most cases of early limb-onset idiopathictorsion dystonia in non-Jews. Am J Hum Genet. 1994;55:468–475.
21. Ozelius L, Kramer PL, Moskowitz CB, et al. Human gene for tor-sion dystonia located on chromosome 9q32-q34. Neuron. 1989;2:1427–1434.
22. Kramer PL, de Leon D, Ozelius L, et al. Dystonia gene in Ashke-nazi Jewish population is located on chromosome 9q32–34. AnnNeurol. 1990;27:114–120.
23. Warner TT, Fletcher NA, Davis MB, et al. Linkage analysis inBritish and French families with idiopathic torsion dystonia.Brain. 1993;116:739–744.
24. Ozelius LJ, Kramer PL, de Leon D, et al. Strong allelic associa-tion between the torsion dystonia gene (DYT1) and loci on chro-mosome 9q34 in Ashkenazi Jews. Am J Hum Genet. 1992;50:619–628.
25. Bressman SB, de Leon D, Kramer PL, et al. Dystonia in Ashke-nazi Jews: clinical characterization of a founder mutation. AnnNeurol. 1994;36:771–777.
26. Bressman SB, Sabatti C, Raymond D, et al. The DYT1 phenotypeand guidelines for diagnostic testing. Neurology. 2000;54:1746–1752.
27. Valente EM, Warner TT, Jarman PR, et al. The role of DYT1 inprimary torsion dystonia in Europe. Brain. 1998;121:2335–2339.
28. Lebre AS, Durr A, Jedynak P, et al. DYT1 mutation in Frenchfamilies with idiopathic torsion dystonia. Brain. 1999;122:41–45.
M I L E S T O N E S I N D Y S T O N I A
Movement Disorders, Vol. 26, No. 6, 2011 1119
-
29. Slominsky PA, Markova ED, Shadrina MI, et al. A common 3-bpdeletion in the DYT1 gene in Russian families with early-onsettorsion dystonia. Hum Mutat. 1999;14:269.
30. Brassat D, Camuzat A, Vidailhet M, et al. Frequency of theDYT1 mutation in primary torsion dystonia without family his-tory. Arch Neurol. 2000;57:333–335.
31. Bressman SB, Sabatti C, Raymond D, et al. The DYT1 phenotypeand guidelines for diagnostic testing. Neurology. 2000;54:1746–1752.
32. Zorzi G, Garavaglia B, Invernizzi F, et al. Frequency of DYT1mutation in early onset primary dystonia in Italian patients. MovDisord. 2002;17:407–408.
33. Moretti P, Hedera P, Wald J, Fink J. Autosomal recessive primarygeneralized dystonia in two siblings from a consanguineous fam-ily. Mov Disord. 2005;20:245–247.
34. Zirn B, Grundmann K, Huppke P, et al. Novel TOR1A mutationp.Arg288Gln in early-onset dystonia (DYT1). J Neurol NeurosurgPsychiatry. 2008;79:1327–1330.
35. Calakos N, Patel VD, Gottron M, et al. Functional evidenceimplicating a novel TOR1A mutation in idiopathic, late-onsetfocal dystonia. J Med Genet. 2010;47:646–650.
36. Kock N, Naismith TV, Boston HE, et al. Effects of genetic varia-tions in the dystonia protein torsinA: identification of polymor-phism at residue 216 as protein modifier. Hum Mol Genet. 2006;15:1355–1364.
37. Risch NJ, Bressman SB, Senthil G, Ozelius LJ. Intragenic cis andtrans modification of genetic susceptibility in DYT1 torsion dysto-nia. Am J Hum Genet. 2007;80:1188–1193.
38. Kamm C, Fischer H, Garavaglia B, et al. Susceptibility to DYT1dystonia in European patients is modified by the D216H poly-morphism. Neurology. 2008;70:2261–2262.
39. Carbon M, Eidelberg D. Abnormal structure-function relation-ships in hereditary dystonia. Neuroscience. 2009;164:220–229.
40. Opal P, Tintner R, Jankovic J, et al. Intrafamilial phenotypicvariability of the DYT1 dystonia: from asymptomatic TOR1Agene carrier status to dystonic storm. Mov Disord. 2002;17:339–345.
41. Gasser T, Windgassen K, Bereznai B, Kabus C, Ludolph AC. Phe-notypic expression of the DYT1 mutation: a family with writer’scramp of juvenile onset. Ann Neurol. 1998;44:126–128.
42. Im JH, Ahn TB, Kim KB, Ko SB, Jeon BS. DYT1 mutation in ko-rean primary dystonia patients. Parkinsonism Relat Disord. 2004;10:421–423.
43. Yeung WL, Lam CW, Cheng WT, et al. Early-onset primary tor-sional dystonia in a 4-generation Chinese family with a mutationin the DYT1 gene. Chin Med J (Engl). 2005;118:873–876.
44. Gambarin M, Valente EM, Liberini P, et al. Atypical phe-notypes and clinical variability in a large Italian familywith DYT1-primary torsion dystonia. Mov Disord. 2006;21:1782–1784.
45. Lin YW, Chang HC, Chou YH, et al. DYT1 mutation in a cohortof Taiwanese primary dystonias. Parkinsonism Relat Disord.2006;12:15–19.
46. Neuwald AF, Aravind L, Spouge JL, Koonin EV. AAAþ: a classof chaperone-like ATPases associated with the assembly, opera-tion, and disassembly of protein complexes. Genome Res. 1999;9:27–43.
47. Naismith TV, Heuser JE, Breakefield XO, Hanson PI. TorsinA inthe nuclear envelope. Proc Natl Acad Sci U S A. 2004;101:7612–7617.
48. Goodchild RE, Dauer WT. Mislocalization to the nuclear enve-lope: an effect of the dystonia-causing torsinA mutation. ProcNatl Acad Sci U S A. 2004;101:847–852.
49. Hewett JW, Zeng J, Niland BP, Bragg DC, Breakefield XO. Dys-tonia-causing mutant torsinA inhibits cell adhesion and neuriteextension through interference with cytoskeletal dynamics. Neu-robiol Dis. 2006;22:98–111.
50. Kamm C, Boston H, Hewett J, et al. The early onset dystoniaprotein torsinA interacts with kinesin light chain 1. J Biol Chem.2004;279:19882–19892.
51. Hewett JW, Tannous B, Niland BP, et al. Mutant torsinA inter-feres with protein processing through the secretory pathway inDYT1 dystonia cells. Proc Natl Acad Sci U S A. 2007;104:7271–7276.
52. Nery FC, Zeng J, Niland BP, et al. TorsinA binds the KASH do-main of nesprins and participates in linkage between nuclear en-velope and cytoskeleton. J Cell Sci. 2008;121:3476–3486.
53. Naismith TV, Dalal S, Hanson PI. Interaction of torsinA with itsmajor binding partners is impaired by the dystonia-associatedDeltaGAG deletion. J Biol Chem. 2009;284:27866–27874.
54. Torres GE, Sweeney AL, Beaulieu JM, Shashidharan P, CaronMG. Effect of torsinA on membrane proteins reveals a loss offunction and a dominant-negative phenotype of the dystonia-asso-ciated DeltaE-torsinA mutant. Proc Natl Acad Sci U S A. 2004;101:15650–15655.
55. Misbahuddin A, Placzek MR, Taanman JW, et al. Mutant tor-sinA, which causes early-onset primary torsion dystonia, is redis-tributed to membranous structures enriched in vesicularmonoamine transporter in cultured human SH-SY5Y cells. MovDisord. 2005;20:432–440.
56. Esapa CT, Waite A, Locke M, et al. SGCE missense mutationsthat cause myoclonus-dystonia syndrome impair epsilon-sarcogly-can trafficking to the plasma membrane: modulation by ubiquiti-nation and torsinA. Hum Mol Genet. 2007;16:327–342.
57. Granata A, Watson R, Collinson LM, Schiavo G, Warner TT.The dystonia-associated protein torsinA modulates synaptic vesi-cle recycling. J Biol Chem. 2008;283:7568–7579.
58. O’Farrell CA, Martin KL, Hutton M, Delatycki MB, CooksonMR, Lockhart PJ. Mutant torsinA interacts with tyrosine hydrox-ylase in cultured cells. Neuroscience. 2009;164:1127–1137.
59. Giles LM, Chen J, Li L, Chin LS. Dystonia-associated mutationscause premature degradation of torsinA protein and cell-type-spe-cific mislocalization to the nuclear envelope. Hum Mol Genet.2008;17:2712–2722.
60. Goodchild RE, Dauer WT. The AAAþ protein torsinA interactswith a conserved domain present in LAP1 and a novel ER pro-tein. J Cell Biol. 2005;168:855–862.
61. Giles LM, Li L, Chin LS. TorsinA protein degradation andautophagy in DYT1 dystonia. Autophagy. 2009;5:82–84.
62. Almasy L, Bressman SB, Raymond D, et al. Idiopathic torsiondystonia linked to chromosome 8 in two Mennonite families.Ann Neurol. 1997;42:670–673.
63. Saunders-Pullman R, Raymond D, Senthil G, et al. Narrowingthe DYT6 dystonia region and evidence for locus heterogeneity inthe Amish-Mennonites. Am J Med Genet A. 2007;143A:2098–2105.
64. Bonetti M, Barzaghi C, Brancati F, et al. Mutation screening ofthe DYT6/THAP1 gene in Italy. Mov Disord. 2009;24:2424–2427.
65. Bressman SB, Raymond D, Fuchs T, Heiman GA, Ozelius LJ,Saunders-Pullman R. Mutations in THAP1 (DYT6) in early-onsetdystonia: a genetic screening study. Lancet Neurol. 2009;8:441–446.
66. Djarmati A, Schneider SA, Lohmann K, et al. Mutations inTHAP1 (DYT6) and generalised dystonia with prominent spas-modic dysphonia: a genetic screening study. Lancet Neurol. 2009;8:447–452.
67. Paisan-Ruiz C, Ruiz-Martinez J, Ruibal M, et al. Identification ofa novel THAP1 mutation at R29 amino-acid residue in sporadicpatients with early-onset dystonia. Mov Disord. 2009;24:2428–2429.
68. Clot F, Grabli D, Burbaud P, et al. Screening of the THAP1 genein patients with early-onset dystonia: myoclonic jerks are part ofthe dystonia 6 phenotype. Neurogenetics. 2011;12:87–89.
69. Groen JL, Ritz K, Contarino MF, et al. DYT6 dystonia: mutationscreening, phenotype, and response to deep brain stimulation.Mov Disord. 2010;25:2420–2427.
70. Houlden H, Schneider SA, Paudel R, et al. THAP1 mutations(DYT6) are an additional cause of early-onset dystonia. Neurol-ogy. 2010;74:846–850.
71. Sohn AS, Glockle N, Doetzer AD, et al. Prevalence of THAP1sequence variants in German patients with primary dystonia.Mov Disord. 2010;25:1982–1986.
72. Xiao J, Zhao Y, Bastian RW, et al. Novel THAP1 sequence var-iants in primary dystonia. Neurology. 2010;74:229–238.
73. Zittel S, Moll CK, Bruggemann N, et al. Clinical neuroimagingand electrophysiological assessment of three DYT6 dystonia fami-lies. Mov Disord. 2010;25:2405–2412.
O Z E L I U S E T A L .
1120 Movement Disorders, Vol. 26, No. 6, 2011
-
74. Cheng FB, Wan XH, Feng JC, Wang L, Yang YM, Cui LY. Clini-cal and genetic evaluation of DYT1 and DYT6 primary dystoniain china. Eur J Neurol. 2011;18:497–503.
75. De Carvalho Aguiar P, Fuchs T, Borges V, et al. Screening of bra-zilian families with primary dystonia reveals a novel THAP1mutation and a de novo TOR1A GAG deletion. Mov Disord.2010;25:2854–2857.
76. Schneider SA, Ramirez A, Shafiee K, et al. Homozygous THAP1mutations as cause of early-onset generalized dystonia. Mov Dis-ord. 2011 [Epub ahead of print].
77. Clouaire T, Roussigne M, Ecochard V, Mathe C, Amalric F, Gi-rard JP. The THAP domain of THAP1 is a large C2CH modulewith zinc-dependent sequence-specific DNA-binding activity. ProcNatl Acad Sci U S A. 2005 May 10;102:6907–6912.
78. Roussigne M, Cayrol C, Clouaire T, Amalric F, Girard JP.THAP1 is a nuclear proapoptotic factor that links prostate-apo-ptosis-response-4 (par-4) to PML nuclear bodies. Oncogene.2003;22:2432–2442.
79. Cayrol C, Lacroix C, Mathe C, et al. The THAP-zinc finger pro-tein THAP1 regulates endothelial cell proliferation through mod-ulation of pRB/E2F cell-cycle target genes. Blood. 2007;109:584–594.
80. Duan W, Zhang Z, Gash DM, Mattson MP. Participation ofprostate apoptosis response-4 in degeneration of dopaminergicneurons in models of Parkinson’s disease. Ann Neurol. 1999;46:587–597.
81. Gavarini S, Cayrol C, Fuchs T, et al. Direct interaction betweencausative genes of DYT1 and DYT6 primary dystonia. Ann Neu-rol. 2010;68:549–553.
82. Kaiser FJ, Osmanoric A, Rakovic A, et al. The dystonia geneDYT1 is repressed by the transcription factor THAP1 (DYT6).Ann Neurol. 2010;68:554–559.
83. Mazars R, Gonzalez-de-Peredo A, Cayrol C, et al. The THAP-zinc finger protein THAP1 associates with coactivator HCF-1 andO-GlcNAc transferase: a link between DYT6 and DYT3 dysto-nias. J Biol Chem. 2010;285:13364–13371.
84. Sabogal A, Lyubimov AY, Corn JE, Berger JM, Rio DC. THAPproteins target specific DNA sites through bipartite recognition ofadjacent major and minor grooves. Nat Struct Mol Biol. 2010;17:117–123.
85. Campagne S, Saurel O, Gervais V, Milon A. Structural determi-nants of specific DNA-recognition by the THAP zinc finger.Nucleic Acids Res. 2010;38:3466–3476.
86. Lanati S, Dunn DB, Roussigne M, et al. Chemotrap-1: an engi-neered soluble receptor that blocks chemokine-induced migrationof metastatic cancer cells in vivo. Cancer Res. 2010;70:8138–8148.
87. Gimenez-Roldan S, Delgado G, Marin M, Villanueva JA, Mateo D.Hereditary torsion dystonia in gypsies. Adv Neurol. 1988;50:73–81.
88. Khan NL, Wood NW, Bhatia KP. Autosomal recessive, DYT2-like primary torsion dystonia: a new family. Neurology. 2003;61:1801–1803.
89. Parker N. Hereditary whispering dysphonia. J Neurol NeurosurgPsychiatry. 1985;48:218–224.
90. Ahmad F, Davis MB, Waddy HM, Oley CA, Marsden CD, Har-ding AE. Evidence for locus heterogeneity in autosomal dominanttorsion dystonia. Genomics. 1993;15:9–12.
91. Valente EM, Bentivoglio AR, Cassetta E, et al. Identification of anovel primary torsion dystonia locus (DYT13) on chromosome1p36 in an Italian family with cranial-cervical or upper limbonset. Neurol Sci. 2001;22:95–96.
92. Bentivoglio AR, Ialongo T, Contarino MF, Valente EM, AlbaneseA. Phenotypic characterization of DYT13 primary torsion dysto-nia. Mov Disord. 2004;19:200–206.
93. Chouery E, Kfoury J, Delague V, et al. A novel locus for autoso-mal recessive primary torsion dystonia (DYT17) maps to20p11.22-q13.12. Neurogenetics. 2008;9:287–293.
94. Defazio G, Berardelli A, Hallett M. Do primary adult-onset focaldystonias share aetiological factors? Brain. 2007;130:1183–1193.
95. Waddy HM, Fletcher NA, Harding AE, Marsden CD. A geneticstudy of idiopathic focal dystonias. Ann Neurol. 1991;29:320–324.
96. Defazio G, Livrea P, Guanti G, Lepore V, Ferrari E. Genetic con-tribution to idiopathic adult-onset blepharospasm and cranial-cer-vical dystonia. Eur Neurol. 1993;33:345–350.
97. Uitti RJ, Maraganore DM. Adult onset familial cervical dystonia:report of a family including monozygotic twins. Mov Disord.1993;8:489–494.
98. Bressman SB, Warner TT, Almasy L, et al. Exclusion of theDYT1 locus in familial torticollis. Ann Neurol. 1996;40:681–684.
99. Munchau A, Valente EM, Davis MB, et al. A yorkshire family