Migraine Diagnosis and Treatment · with migraine have headache on ≥4 days per month, and 6% have...
Transcript of Migraine Diagnosis and Treatment · with migraine have headache on ≥4 days per month, and 6% have...


Migraine Diagnosis and Treatment
Merle Diamond, MDPresident, Managing Director,
Diamond Headache ClinicChicago, Illinois

Disclosure: Merle L. Diamond, MD
3
Consultant
• Alder BioPharmaceuticals• Allergan• Amgen• Depomed• Lilly• Supernus Pharmaceuticals
Advisory Boards• Avanir Pharmaceuticals• Lilly• Pernix Therapeutics
Speaker Bureau
• Avanir Pharmaceuticals• Depomed• Pernix Therapeutics• Teva Pharmaceutical Industries

Treatment guidelines recommend preventive treatments for people with frequent and
disabling headaches
Only one-third of people with migraine
who meet guidelines for preventive treatments
receive them1
Of those who start preventive treatment, 80% lapse over the
course of 1 year2
• Why aren’t preventive treatments being more widely utilized?
• How can we optimize the appropriate use of preventive treatments?
1. Blumenfeld AM, et al. Cephalalgia. 2011;31(3):301-315. 2. Hepp Z, et al. Cephalalgia. 2015;35(6):478-488.4
Background

1. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Lancet. 2016;388(10053):1545-1602. 2. GBD Results Tool. GBD 2015 Data Resources.
http://ghdx.healthdata.org/gbd-results-tool?params=querytool-permalink/7c3dc4972502afe131c6794349a8c39b. Accessed March 28, 2017. 3. Lipton RB, et al. Neurology.
2007;68(5):343-349. 4. Russo AF. Annu Rev Pharmacol Toxicol. 2015;55:533-552. 5. Gasparini CF, et al. Curr Genomics. 2013;14(5):300-315. 6. Marketscan data on file;
March 24, 2017. 7. Silberstein SD. Continuum (Minneap Minn). 2015;21(4 Headache):973-989.5
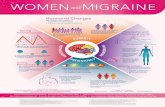
2 to 3x more common in women vs men5-7
Lifetime prevalence4
Global prevalence4 15-25%
43%
6-8%
18%
>44 million individuals affected in the United States2
Affects >10% of population(959 million globally)1
~20% to 35% of people with migraine have ≥4 days per month3
30 to 39 years3
Prevalence peaks in middle life during prime years3
Migraine Is a Global Problem

23.7
41.4
14.7
8.9
4.11.6 1.9 1.4 0.6 0.7 1.0
0
10
20
30
40
50
60
0-1 2-3 4-6 7-9 10-11 12-14 15-18 19-21 22-24 25-27 28-31
1. Blumenfeld AM, et al. Cephalalgia. 2011;31(3):301-315. 2. Headache Classification Committee of the International Headache Society. Cephalalgia. 2013;33(9):629-808.
Migraine Frequency Exists on a Spectrum
6
<15 headache days per month
can be classified as episodic migraine2
≥15 headache days per month for >3 months can be
classified as chronic migraine2
• One-third of people with migraine have headache on ≥4 days per month, and 6% have headache on 15 or more days per month1
• Traditional criteria for preventive treatment are defined in part by headache days
ChronicEpisodic
Headache Days per Month
Frequency of Headache Days in Migraine (N=8281)1
% o
f P
ati
en
ts

23.7
41.4
14.7
8.9
4.11.6 1.9 1.4 0.6 0.7 1.0
0
10
20
30
40
50
60
0-1 2-3 4-6 7-9 10-11 12-14 15-18 19-21 22-24 25-27 28-31
1. Blumenfeld AM, et al. Cephalalgia. 2011;31(3):301-315. 2. Bigal ME, Lipton RB. Headache. 2008;48(1):7-15. 3. Manack A, et al. Neurology. 2011;76(8):711-718.
Migraine Frequency Is Dynamic
7
26% over 2 years3
3% over 1 year2
• Migraine frequency can increase over time and may transition from episodic to chronic, a process termed “chronification”2
• Migraine can also transition from chronic to episodic2 %
of
Pa
tie
nts
Frequency of Headache Days in Migraine (N=8281)1
ChronicEpisodic
Headache Days per Month

1. Lipton RB, et al. Neurology. 2007;68(5):343-349. 2. Buse DC, et al. Headache. 2013;53(8):1278-1299.
Migraine Is Usually Associated With Severe Impairment or Need for Bed Rest
Migraine-related impairment was common in the American Migraine Prevalence and Prevention (AMPP) study of >18,000 individuals with migraine.1
Respondents were asked how they are “usually affected by severe headaches” with the following response options:2
• Able to work/function normally
• Working ability or activity impaired to some degree
• Working ability or activity severely impaired
• Bed rest required
8
SevereImpairmentor Bed RestRequired
54%FunctionNormally
7%
SomeImpairment
39%

100
80
90
70
60
50
40
30
20
10
015-18 28-3125-2722-2419-2112-1410-114-62-30-1 7-9
<15 headache days/month (n=7812)
≥15 headache days/month (n=469)
Headache Frequency (Days per Month)
% o
f P
ati
en
ts
Blumenfeld AM, et al. Cephalalgia. 2011;31(3):301-315.
Disability Increases Progressively With Increasing Number of Headache Days
9
Little or no disability (score 0-5)
Mild disability (score 6-10)
Moderate disability (score 11-20)
Severe disability (score 21-40)
Very severe disability (score 41-270)
Level of disability based on Migraine Disability Assessment (MIDAS) score
International Burden of Migraine Study (N=8281)

What Can We Offer This Patient?Abortive Medical Toolbox
Real case.

1899(introduced in)
NSAIDs (nonsteroidal anti-inflammatory drugs)• Block cyclooxygenase (COX) enzymes• Reduce prostaglandins

1926(introduced in)
Ergots• 5-HT1B/1D agonist• Prolonged interaction with 5-HT1A,
5-HT5, 5-HT2, 5-HT7, α-adrenoceptors, and dopamine (DA) D2 receptors

Triptans• 5-HT1B/1D agonist • 5-HT2A receptors in peripheral arteries
1992(FDA approval)

Triptan/NSAID• 5-HT1B/1D agonist + NSAID
2008(FDA approval)

Neuromodulatory devices
Recent(FDA approval)
• Transcranial magnetic stimulation (sTMS, eNeura)
• Supraorbital external trigeminal nerve stimulation (TENS, Cefaly)
• Noninvasive vagus nerve stimulator (nVNS, gammaCore)

Consider Prevention When…
16
Significant InterferenceWith routine activities—
despite use of acute treatment
Attack Frequency> 1/week
Elevated RiskMedication overuse
PatientPreference
IneffectiveContraindicated Troublesome AEsOverused
Acute Medications
HemiplegicBrainstem Prolonged auraMigrainous infarction
Uncommon Subtypes Present

1. Lipton RB, et al. Neurology. 2007;68(5):343-349. 2. Diamond S, et al. Headache. 2007;47(3):355-363.
Migraine Prevention Is Underused
17
~39%
were candidates for or should be considered for prophylactic treatment1
Data from the AMPP study suggest that approximately two-thirds ofindividuals with migraine who qualify for prophylaxis do not receive it2
The AMPP study surveyed 18,968 individuals with migraine and found that
~29%
had received prophylactic medication for migraine in the
past but discontinued treatment2
~12%
were current users of prophylactic medication for the treatment of migraine1

*Oral prophylactic medications analyzed in this retrospective study were limited to specific antidepressants, β-blockers, and anticonvulsants.
Adherence rates were reported as the proportion of patients with a proportion of days covered ≥80%.
Hepp Z, et al. Cephalalgia. 2015;35(6):478-488.
Adherence to Current Migraine Preventives Is Poor
18
26
17
0
10
20
30
40
50
60
70
80
90
100
6 Months 12 Months
83% of people withmigraine discontinuepreventive treatment
over 1 year
% o
f P
ati
en
ts A
dh
ere
nt
to O
ral
Pro
ph
yla
xis
Retrospective Claims Database Analysis: Insured Patients With Migraine and ≥15 Headache Days/Month (N=8688)*

Blumenfeld AM, et al. Headache. 2013;53(4):644-655.
Reasons Patients Discontinue Oral Prophylactic Medication
19
0
5
10
15
20
25
30
35
40
45
50
SatisfactoryResolution
Lack of Efficacy Side Effects Cost Other
Antidepressants (n=205)Antiepileptics (n=125)
Beta blockers (n=120)
Calcium channel blockers (n=59)
% o
f P
ati
en
ts
Lack of efficacy and medication side effects are the most common reasons for discontinuation of prophylactic medications
International Burden of Migraine Study-II Assessed Prophylactic Therapy Patterns in 1165 Patients With Migraine
Patient-Reported Reasons for Discontinuation of Prophylactic Medication

4. High discontinuation rates on current therapies may reflect unmet and inadequately managed patient expectations.
Defining Success in Migraine Prevention
20
1. Standard definition of success is a 50% headache response rate (50% reduction in migraine days from baseline to weeks 9 to 12 or later).
2. This definition is predicated on the art of the possible or on what available treatments deliver.
3. Patients would prefer greater reductions in migraine days that would be achieved more quickly.

What Can We
Offer This Patient?Preventive Medical Toolbox
Real case.

Tricyclic antidepressants • Increase levels of norepinephrine
(NE) and 5-HT• Block histaminic, cholinergic,
and α1-adrenergic receptor sites
(FDA approval)
mid-
1960s(case reports
showing benefit)

Beta blockers • Noradrenergic receptor antagonists
1979(FDA approval)

Antiepileptics• Enhance gamma-aminobutyric
acid (GABAergic) inhibitory neurotransmission
• Decrease glutamatergic excitatory neurotransmission
1996(FDA approval)

OnabotulinumtoxinA• Block acetylcholine release• May act in part through blocking
CGRP release
2010(FDA approval)

Recent(FDA approval)
Neuromodulatorydevices• Supraorbital external trigeminal nerve
stimulation (TENS, Cefaly)• Transcranial magnetic stimulation
(sTMS, eNeura)• Caloric vestibular stimulation (CVS,
Scion NeuroStim)

2018(FDA approval)
Anti-CGRP MAB therapy • Targets the CGRP receptor or ligand• 3 compounds have FDA-approval

1. Hepp Z, et al. Cephalalgia. 2015;35(6):478-488. 2. Lipton RB, et al. Headache. 2013;53(8):1300-1311.
3. Bonafede M, et al. J Manag Care Spec Pharm. 2015;21(suppl10):S48-S49.
Addressing the Unmet Need in Preventive Treatment
28
40%
More than 40% of patients receiving therapy still experience at least one migraine-related issue, including headache-related disability, treatment dissatisfaction, and/or excessive opioid use2
13%
Up to 13% of patients with migraine receiving acute or preventive therapy still have at least 1 emergency department visit a year3
80%Approximately 80% of patients discontinue oral preventive therapy after 1 year of treatment1

RCTs=randomized, controlled trials.
Shamliyan T. J Gen Int Med. 2013;28(9):1225-1237.
All Approved Oral Drugs Share Similar Efficacy to Prevent Migraine
29
• Topiramate and antidepressants result in more adverse events
• No significant differences in treatment discontinuation due to adverse events between labeled drugs
• Angiotensin-converting enzyme inhibitors and beta blockers most tolerable and effective
• Long-term evidence is lacking (>3-month duration)
215 publications of RCTs provided mostly low-strength evidence because of the risk of bias and imprecision
• Metoprolol (4 RCTs)
• Atenolol (1 RCT)
• Nadolol (1 RCT)
• Captopril (1 RCT)
• Lisinopril (1 RCT)
• Candesartan (2 RCTs)
Off-Label Drugs
• Topiramate (9 RCTs)
• Divalproex (3 RCTs)
• Timolol (3 RCTs)
• Propranolol (4 RCTs)
Approved Drugs

Communication
Calendar/diary
30
Establish goals Headache toolbox Check in

Q & A
31

New and Emerging Headache Therapies
Robert Kaniecki, MDDirector, UPMC Headache Center Assistant Professor of Neurology,
University of Pittsburgh School of MedicinePittsburgh, Pennsylvania

Disclosures 2017-2018 Robert Kaniecki, MD
33
Consultant/Advisory Boards Alder Biopharmaceuticals

34
New Horizons in Headache Treatment!

Overview
• New formulations of existing medications
• New medications and devices
• New classes of acute medication in development
• Gepants, serotonin (5-HT1F) agonists [ditans]
• New classes of preventive medication released or in development
• Anti-calcitonin gene-related peptide (CGRP) or anti-CGRP receptor monoclonal antibodies (MABs)
• Neuromodulation
• Noninvasive, FDA approved: Transcutaneous supraorbital neurostimulation (tSNS), single pulse transcranial magnetic stimulation (sTMS), non-invasive vagal nerve stimulation (nVNS), and caloric vestibular stimulation (CVS)
• Noninvasive in development: Remote nonpainful electrical upper arm skin stimulation and combined occipital and supraorbital transcutaneous nerve stimulation (OS-TNS)
• Minimally invasive in development: Sphenopalatine ganglion stimulation (SPG)
35

36
Pathophysiology and Neurotransmitter
Targets

Dura
Cutaneous allodynia
Throbbing pain
Neck muscle tenderness
Activated central neuron (thalamus)
Sensitized peripheral neuron(trigeminal ganglion)
Meningealblood vessel
Pain processing: Sensitized central neuron(trigeminal cervical complex)
Peripheral pain mechanisms: CGRP, pituitary adenylate cyclase-activating polypeptide (PACAP)
Central generator?
Pain perception
Pathophysiology
Tepper SJ. Adapted from C79, Comprehensive Migraine
Education Program 1 presented at AAN 2017; Boston. 37

Adapted from Hargreaves RJ, Shepheard SL. Can J Neurol Sci. 1999;26(suppl3):S12-S19.
Serotonin (5-HT) Mechanisms in Migraine
• Anti-migraine targets: 5-HT1B/1D receptors
5-HT1F receptors
38
5-HT1D
5-HT1F
5-HT1D
5-HT1B
(CGRP)

cAMP=cyclic adenosine monophosphate. CLR=calcitonin receptor-like receptor. NS=nervous system. RAMP=receptor activity modifying protein. RCP=receptor component protein.
1. Naot D, Cornish J. Bone. 2008;43(5):813-818. 2. Benarroch EE. Neurology. 2011;77:281-287.
CGRP Mechanisms in Migraine
• Neuropeptide belonging to calcitonin family• Calcitonin• Amylin• Adrenomedullin• Intermedin
• Present at all migraine pathogenesis sites
• Increases in migraine, decreases with treatment
39
adenylylcyclase
Gs
RCP
CGRP
RA
MP
1
CLR
cAMP
Cortex
CGRP receptors

Adapted from Edvinsson L, et al. Nat Rev Neurol. 2018;14(6):338-350.
CGRP Signaling and Blockade
40

41
New Devices for Delivering Medications

New Acute Treatment Classes
RCT=randomized, controlled trial. ADAM=Adhesive Dermally Applied Microarray.
1. www.fda.gov/Drugs/. Accessed June 11, 2018. 2. www.clinicaltrials.gov. Accessed June 11, 2018.
Devices for Delivering Medications
FDA-approved and available1
• Sumatriptan autoinjectors
• Sumatriptan breath-powered dry nasal powder
In development2
• Phase 3 RCTs completed
• Zolmitriptan skin patch (ADAM)
• DFN-02 sumatriptan nasal spray
• In development
• Oxytocin nasal spray, T1-001
• Sumatriptan skin patch, KC5010
• Zolmitriptan oral inhalation, CVT-427
• Sumatriptan oral spray, SUD-001
• DHE HFA nasal spray, powder nasal spray, novel autoinjectors
42

43
New Acute MigraineTreatments

1. Kuca B, et al. Presented at Diamond Headache Clinic Research & Educational Foundation Headache Update 2017; Lake Buena Vista, FL. 2. Wietecha LA, et al. Abstract PO-02-
180 presented at IHC 2017; Vancouver.
Lasmiditan - 5-HT1F AgonistPhase 3 Trials for Acute Treatment of Episodic Migraine
• 2-Hour Pain Freedom:
100 mg- 28.2-31.4%
200 mg- 32.4-38.8%
Placebo- 15.3%-21.3%
• Both doses also eliminated the Most Bothersome
Symptom (MBS), chosen by the patient from
nausea, photophobia, or phonophobia at 2 hours
• Adverse events in the Phase 3 RCTs:
Dizziness + vertigo =100 mg average 15.5% 200 mg average 16.8%
Somnolence + fatigue + lethargy =100 mg average 10.4%
200 mg average 12%
• For comparison, rizatriptan 10 mg prescribing information:
Dizziness 20% greater than lasmiditan
Somnolence + fatigue 15% greater than lasmiditan
44
Conclusions for lasmiditan acute treatment:
• Efficacy and side effects similar to rizatriptan
• Central adverse events probably due to central 5-HT1F activity and likely no vasoconstrictive effects

1. Tfelt-Hansen P. Headache. 2011;51:118-123. 2. Tfelt-Hansen P, Do TP. Abstract PO-01-48 presented at IHC 2017; Vancouver. 3. Allergan press release. February 6, 2018. https://www.allergan.com/news/news/thomson-reuters/allergan-announces-positive-top-line-phase-3-resul. Accessed April 26, 2018. 4. Biohaven press release. March 26, 2018. http://biohavenpharma.com/biohaven-announces-successful-achievement-of-both-co-primary-regulatory-endpoints-in-two-pivotal-phase-3-trials-of-rimegepant-an-oral-cgrp-receptor-antagonist-for-the-acute-treatment-of-migraine/. Accessed April 26, 2018. 5. https://www.prnewswire.com/news-releases/allergans-oral-cgrp-receptor-antagonist-atogepant-demonstrates-robust-efficacy-and-safety-in-episodic-migraine-prevention-in-a-phase-2b3-clinical-trial-300663770.html. Accessed June 13, 2018.
Gepants - Small Molecule CGRP Receptor Antagonists
Acute Treatment of Episodic Migraine • 6 gepants effective in acute migraine treatment: olcegepant, BI 44370 TA, telcagepant, MK-3207, rimegepant, and ubrogepant
• BI 44370 TA, telcagepant, and MK-3207 all reportedly liver toxic
• Efficacy: Ubrogepant Phase 3 acute treatment of episodic migraine: • 2-hour pain freedom: 50 mg 19.2%; 100 mg 21.2%; placebo 11.8%; Also relieved 2-hour MBS
• Efficacy: Rimegepant Phase 3 acute treatment of episodic migraine: • 2-hour pain freedom: 75 mg 19.2-19.6%; placebo 12%-14.2%; also relieved 2-hour MBS
• Adverse events1. Liver, Ubrogepant: 6 cases with ALT >3x ULN, one of which was 10X ULN; 1 case with placebo >3x ULN; Rimegepant: one case
each from active and placebo with >3x ULN
2. Tolerability, Ubrogepant: nausea, somnolence, dry mouth in <5% of patients; Rimegepant: nausea in <2% of patients
45
Preventive Treatment of Episodic Migraine
• Telcagepant had liver toxicity when given daily
• Atogepant vs placebo positive phase 2 for migraine prevention, no liver signal; Rimegepant to be tested
Conclusions for gepants acute treatment:
• Efficacy and side effects similar to naratriptan
• Tolerability is excellent
• Liver safety will still need to be explored
• Prevents vasodilation; no expectation of vasoconstriction

46
New Preventive Migraine
Treatments

MABs to CGRP or the CGRP Receptor
• Physiological differences from presently available options
• MABs are big molecules that do not cross the blood brain barrier
• Peripheral, not central, mechanism of action
• MABs are eliminated by the reticuloendothelial system
• No hepatic, renal toxicity
• Clinical differences from presently available options
• Work to prevent episodic and chronic migraine, and medication-overuse headache
• Have quick onset, separating from placebo within 1 week
• Clinically meaningful response by 1 month
• Have favorable responder rates for ≥50%, 75%, and 100%
• Have safety and tolerability similar to placebo
471. Yu YJ, Watts RJ. Neurotherapeutics. 2013;10(3):459-472. 2. Lipton RB, et al. US Neurology. 2018;14(suppl 4):S3-S10. 3. Tepper SJ. Headache. 2018;58:in press.

cCH=chronic cluster headache. CM=chronic migraine. eCH=episodic cluster headache. EM=episodic migraine. SC=subcutaneous. RCT=randomized controlled trial.
Tepper SJ. Headache. 2018;58:in press.
4 Injectable MABs to CGRP or Its Receptor
48
Erenumab-aooe(fully human)
Galcanezumab-gnlm(90% humanized)
Fremanezumab-vgrm(95% humanized)
Eptinezumab(90% humanized)
Studied for EM, CM EM, CM, eCH, cCH EM, CM, eCH, cCH EM, CM
Dosing Monthly SC Monthly SCMonthly or quarterly SC;
IV load for CHQuarterly IV
Target CGRP receptor CGRP ligand CGRP ligand CGRP ligand
Regulatory status
FDA approved May 17, 2018;
EM & CM registration
FDA approved September 28, 2018; EM & CM registration
FDA approved September 14, 2018; EM & CM registration
Presented (+) phase 3 EM & CM RCTs
Terms: n=neurologic; umab=fully human; zumab=humanized, 90-95% human

1. Tepper SJ, et al. Lancet Neurol. 2017;16:425-434. 2. Oakes TM, et al. Abstract PS-19 presented at AHS 2017; Boston. 3. Alder press release. Jan 8, 2018.
https://globenewswire.com/news-release/2018/01/08/1284947/0/en/Alder-Announces-Eptinezumab-Significantly-Reduces-Migraine-Risk-Meets-Primary-and-All-Key-Secondary-
Endpoints-in-Pivotal-PROMISE-2-Phase-3-Trial-for-Chronic-Migraine-Prevention.html. Accessed April 27,2018. 4. Goadsby P et al. Poster IOR08. Headache 2018;;58(Supplement
2):77 (presented at American Headache Society 60th Scientific meeting 2018 ;San Francisco.
Clinical Utility of the 4 MABs
• All data announced to date for EM and CM have shown a reduction in mean monthly migraine days (MMDs) with a magnitude of 1-3 days drop over placebo
• Using MMDs is necessary from a regulatory standpoint, but not clinically useful endpoint• More useful are certain secondary endpoints, such as responder rates
• Erenumab in CM prevention showed a 6.7-day reduction in MMDs in the pivotal trial, which would represent 79 fewer migraine days/year1; for eptinezumab, an 8-day reduction from baseline would be 96 fewer migraine days per year
• The ≥50% responder rates (secondary endpoints) in the galcanezumab EM registration studies were ≥50%,in the eptinezumab CM study 61%, and the ≥75% responder rates for both were about 1/3 of patients2,3
• Erenumab 140 mg worked in patients who had failed 2-4 preventive medications in a prospective randomized placebo-controlled trial4
49

Practical dosing
• Erenumab – 70 mg or 140 mg SQ monthly
• Fremanezumab – 225 mg SQ monthly or 775 mg SQ quarterly
• Galcanezumab – 240 mg SQ month 1, then 120 mg SQ monthly
• Eptinezumab – Dosing TBA, IV infusion every 3 months
50
Fremanezumab Prefilled Syringe
Erenumab Galcanezumab

Q & A
51

Neuromodulation
52
Single Pulse Transcranial Magnetic Stimulator (sTMS, SpringTMS)
2
Transcutaneous supraorbital neurostimulation(tSNS, e-TNS, Cefaly)
1
Noninvasive vagal nerve stimulator (nVNS, gammaCore)3
Noninvasive caloric vestibular stimulation (CVS, Scion NeuroStim)4
Remote, nonpainful stimulation for acute treatment of migraine (Nerivio Migra)5
Combined occipital and supraorbital transcutaneous nerve stimulation
(OS-TNS, Relievion)
6
Sphenopalatine ganglion stimulation (SPGs, Pulsante)7
FDA-approved In development

-2.1
0.3
-2.5
-2
-1.5
-1
-0.5
0
0.5
Active Sham
38.2
12.2
0
5
10
15
20
25
30
35
40
45
Active Sham
HA=headache. NS=non-significant
1. Schoenen J, et al. Neurology. 2013;80;697-704. 2. Tepper D. Headache. 2014;54(8):1415-1416. 3. Chou DE, et al. Abstract OC-LB-005 presented at IHC 2017; Vancouver.
Transcutaneous Supraorbital Neurostimulation(tSNS, e-TNS, Cefaly)
• FDA approved in 2017 for preventive and acute treatment of migraine as nonsignificant risk device
• Preventive RCT: Turn it on and wear it 20 minutes/day; N=67
• ≥50% reduction in migraine days/month
• Acute RCT: turn on in different setting for acute attack for 1 hour; N=57
• Mean change in visual analog (VAS) 1-hour pain score reported as statistically significant in active vs placebo
• Cost: $550 (initial)
• Cost: $25 (3 electrodes every 3 months)
53
Change in
HA days (NS)
P=0.054
50%
Responder
Rates
P=0.023

1. Andreou AP, et al. Brain. 2016;139:2002-2014. 2. Lipton RB, et al. Lancet Neurol. 2010;9:373-380.
3. Bhola R, et al. J Headache and Pain. 2015;16:535. 4. Starling A, et al. Abstract S52.004 presented at AAN 2017; Boston.
Single Pulse Transcranial Magnetic Stimulation (sTMS, SpringTMS)
• Magnetic pulses disrupt cortical spreading depression (CSD), the basis for aura, and down-regulate thalamocorticalpain pathways
• 1 RCT for acute treatment of migraine with aura, N=167
• 2 hours pain-free: 39% sTMS vs 22% sham (P=0.0179)
• 2 studies for prevention of migraine with prn extra pulses, N=249
• 4-25 headache days for inclusion; 4 pulses BID with extra prn up to 17 pulses per day
• FDA-approved in 2017 as nonsignificant risk device for preventive and acute treatment of migraine
• Rental cost $225/month
54

1. Mourdoukoutas AP, et al. Neuromodulation. 2018;21(3):261-268. 2. Chen SP, et al. Pain. 2016;157:797-805. 3. Hawkins JL, et al. Presented AAN 2016; Vancouver. 4. Akerman
S, et al. Neurobiol Dis. 2017;102:96-104. 5. Silberstein SD, et al. Headache. 2016;56:1317-1332. 6. Goadsby PJ, et al. Presented at Clinical Trials Plenary Session, AAN 2017;
Boston. 7. Silberstein SD, et al. Neurology. 2016;87:529-538. 8. Tassorelli C, et al. Abstract OC-LB-002 presented at IHS 2017; Vancouver.
Noninvasive Vagal Nerve Stimulator (nVNS, gammaCore)
• Handheld, patient-controlled device, which preferentially activates afferent A and large B fibers, not C or efferent pathways that mediate bradycardia and bronchoconstriction1
• Inhibits CSD2 and central trigeminovascular and thalamocortical pathways3,4
• 2 RCTs showed effectiveness in terminating attacks of episodic cluster headache, but not chronic cluster headache5,6
• 2 RCTs failed primary endpoints in prevention and acute treatment of migraine, but showed suggestive secondary endpoints7,8
• FDA-approved as nonsignificant risk device for acute treatment of episodic cluster headache attacks and acute treatment of migraine
• $575/month for loaded stimulation package
55

Wilkinson D, et al. Headache. 2017; 57: 1065-1087.
Caloric Vestibular Stimulation
(CVS, Scion NeuroStim)
• 6-site, placebo-controlled, blinded
• 4-14 HA days/month
• 1° endpoint: migraine days, 3rd month
• Active: -3.6 HA days vs baseline(P <0.0001), -2.7 HA days vs sham (P=0.012)
• 2° endpoints also positive
• Approved by FDA in March 2018 for prevention of EM ages 12 and above; not commercially available yet
56
ITT
No
rma
lize
d m
on
thly
mig
rain
e
da
ys (
%)
of
ba
se
lin
e
Trigeminocervical
complex
VIII,
Vestibulo-cochlear inputV,
Neck
AEs >1 patient: nausea,
dizziness, ear sx, tinnitus.
Placebo dizziness=
Active dizziness (4 in each).

1. Yarnitsky D, et al. Neurology. 2017; 88(13): 1250-1255. 2. Nir RR, et al. Eur J Pain. 2011;15: 491-497. 3. Goadsby PJ. Ann Indian Acad Neurol. 2012;15(suppl1):S15-S22.
Remote Nonpainful Electrical Upper Arm Stimulation(Nerivio Migra)
• Prospective, double-blinded, randomized, crossover, sham-controlled trial in acute migraine
• Participants with migraine applied electrical patch to upper arm soon after attack onset for 20 minutes, at various pulse widths, for up to 20 attacks
• 50% pain reduction for 64% of participants based on best of 3-pulse width stimuli per individual vs 26% sham, N=71 patients, 299 treatments
• Second study underway in US
57

Hering-Hanit. Cephalalgia. 2017;37(suppl1):73.
Combined Occipital and Supraorbital Transcutaneous Nerve Stimulation (OS-TNS, Relievion)
• Randomized, sham-controlled trial for acute treatment of migraine attack, N=30, treatment duration 45 minutes
• Decreased pain VAS score in the treatment group vs increased pain VAS score in the control group (-79.2% vs + 14.9%, P=0.0002)
• 2-hour pain-free: active OS-TNS vs sham (P=0.0031)
58

1. Edvinsson L, Goadsby PJ. Cephalalgia. 1994;14:320-327. 2. Burstein R, Jakubowski M. J Comp Neurol. 2005;493:9-14. 3. Schoenen J, et al. Cephalalgia. 2013;33: 816–830.
4. Jurgens TP, et al. Cephalalgia. 2017;37:423-434. 5. Late Breaking Abstract, 60th Scientific American Headache Society meeting, San Francisco, June 2018
Sphenopalatine Ganglion Stimulation (SPGs, Pulsante)
• Wireless device with programmable remote control
• Inserted via a minimally invasive oral procedure
• 1 RCT showed efficacy for acute and preventive treatment of chronic cluster headache
• Around 2/3 of cluster patients have relief after stimulation within 15 minutes and/or at least a 50% reduction in cluster attack frequency
• The US randomized controlled trial for acute treatment ofchronic cluster headache was announced as positive in 6/18
59

Summary Of Migraine Management Advances
• New devices delivering existing medications
• New acute and preventive migraine medications
• New neuromodulatory devices for migraine
60

Q & A Session
For valuable resources related to this activity, please visit
forefrontcollabactivities.com/Diamond2018
61