Message from the new editor 2008 JMS final.pdf · 2015-08-07 · 1Kh.Sulochana Devi, 2Y.Gunabati...
Transcript of Message from the new editor 2008 JMS final.pdf · 2015-08-07 · 1Kh.Sulochana Devi, 2Y.Gunabati...

JMS * Vol 22* No. 1 * January, 2008 1
EDITORIAL
Dear Members,
I, on behalf of the Journal of Medical Society(JMS), RIMS, Imphal wish you all a “Happyand Prosperous New Year 2008”.
First of all, I express my heartfelt thanks to allof you for giving me the responsibility as theeditor for our esteemed journal.
The journal has earned credibility amongst allthe readers and institution during a short periodof time. It is my great pleasure to lead ourjournal as a first editor by an anesthesiologist.I will sincerely try my level best to make it asone of the reputed journals in the country.Besides having a few publications and paperpresentation in various journals, conferencesand my long association with the JMS andwhole hearted willingness to serve as Editorof JMS, it will be a great opportunity for me toguide the journal as a part of continuingresearch in various specialities of medicalsciences.
It is my intension that all manuscripts will also
Message from the new editor
Dr. L. Deban Singh,Editor, JMS.
be subjected to peer reviewer who is an expertin the field. The identity of the author andinstitution will also be concealed so that thereviewer has no bias on the paper concerned.Once more, I request all the authors to followstrictly the “ Instructions to authors” insertedin every January issue.
The first issue under my Editorship as 22nd
volume of the journal is coming up in the monthof January 2008. I believe that the members ofthe society, authors, peer reviewers, editorialboard members and advertisers will continueto help the editor with constructive advice touplift the journal.
My thanks are due to outgoing editorial teamled by Dr. Y. Indibor Singh who has worked sohard for the past 2 years.
Once again, I agree that I will work upto yourexpectations with honesty and transparency.

JMS * Vol 22 * No. 1 * January, 20082
ORIGINAL ARTICLE
AbstractObjective: To detect infections withToxoplasma, Rubella, CMV, HSV (TORCH)among women with still birth by demonstratingIgM & IgG antibodies against TORCH complex.Methods: 43 women with still birth werescreened for IgM and IgG antibodies by usingELISA test (Equipar Diagnostica, Italy).Results: IgM antibodies for Toxoplasma,Rubella, CMV & HSV were found in 4 (9.3%),3(6.9%), 10(23.26%) and 9(20.93%) of thecases respectively indicating primary infection/relapse (CMV, HSV) during pregnancy. IgGantibodies for Toxoplasma, Rubella, CMV &HSV were found in 25 (58.14%), 29 (67.44%),31 (72.09%) and 29(67.44%) respectively.Conclusion: Routine antenatal screening forTORCH antibodies for women with badobstetric for early diagnosis and propermanagement is suggested.
Key words : TORCH, Rubella, CMV, HSV,Toxoplasma, Still birth.
IntroductionFetal demise is a traumatic experience for boththe parents and the obstetrician. Despite theadvances in the field of perinatal medicine,significant number of stillbirths continue tooccur. Primary infection with Toxoplasma
Seroprevalence of TORCH in women with still birth in RIMS hospital
gondii, Rubella, Cytomegalovirus and Herpessimplex virus (TORCH complex) duringpregnancy at various stages can lead tocongenital infections with unfavourable fetaloutcome in the form of spontaneous abortions,intra uterine death, intra uterine growthretardation, still birth, early neonatal death andcongenital malformations.1 Unfortunately thematernal infections are initially asymptomaticor mild so much so that most women areuncertain about whether they have ever hadit.2 Therefore diagnosis of acute TORCHinfection in pregnant women is usuallyestablished by detection of specific IgMantibodies against TORCH complex. Thepresent study aims at the detection of TORCHinfection in women with still birth by detectingIg M and IgG antibodies.
Material and methodsThe present study was carried out in theDepartment of Microbiology, Regional Instituteof Medical Sciences (RIMS), Imphal, duringJanuary 2002 to September 2003.Serum samples from 43 women with still birthwere screened for TORCH IgM and IgG anti-bodies by using ELISA test ( EquiparDiagnostica, Italy) following manufacturer’s in-structions. Absorbance reading was taken at450 nm filter ( referencing at 650 nm ). Theactivity index (A1) values of the controls andserum samples were read from the standardcurve prepared for each run.
ResultsIn the present study, the women with still birthwere between 20 to 40 years. Table 1 showsthe distribution of TORCH antibodies in women
1. Department of Microbiology, 2. Deptt. of Obst. &Gynaecology, 3. Deptt. of Pathology, RegionalInstitute of Medical Sciences (RIMS), Lamphelpat,Imphal-79504, Manipur, India.
Corresponding author:Dr. Kh. Sulochana Devi, Professor, Department ofMicrobiolgy, RIMS, Imphal - 795004, Manipur, IndiaPhone : 9436037996. e-mail:[email protected]
1Kh.Sulochana Devi, 2Y.Gunabati Devi, 2N.Saratkumar Singh, 3A.Meina Singh, 2I.Dorendra Singh

JMS * Vol 22* No. 1 * January, 2008 3
ORIGINAL ARTICLE
with still births. Out of 43 women 4 (9.3%) werepositive for IgM Toxoplasma antibody, 10(23.26%) were positive for CMV Ig M antibody,3 (6.9%) women were positive for Rubella IgMantibody and 9 (20.93%) were positive forHSV IgM antibodies. IgG antibody alone waspositive in 25 (58.14%) cases for Toxoplasma,29 (67.44%) cases for Rubella, 31 (72.09%)cases for CMV and 29 (67.44%) cases for HSVindicating past infection.
Among 26 women who were positive forTORCH IgM antibody mixed infection of all fourTORCH was found in 1, Rubella and HSV in1, Rubella, CMV, HSV in 1 and CMV & HSV in 4.
Most of the women belonged to low socio-economic status (71%) and were illiterate(62%). Congenital malformation was found in3 cases.
occur within 2 to 3 months of gestation. Theprevalence of Toxoplasma varies from placeto place depending upon the food habits andassociation with pets like dogs and cats. Inour present study Toxoplasma IgM antibodywas found in 9.3% of the mothers having stillbirth which is comparable with the study ofTurbadkar D et al1 who reported 10.5%positivity among women with bad obstetrichistory. Bhatia VN et al3 and Rajendra B et al4reported the prevalence of antibodies ofToxoplasma in 12% and 14.66% respectively.The greatest risk of congenital Toxoplasmosisoccurs during the first trimester of pregnancy.However it is during the third trimester that thehighest level of transmission occurs. This isthought to be related to the much larger sizeof the uterus. The transmission rate from amaternal infection is about 45%. Of this 60%are subclinical infections, 9% result in deathof fetus and 30% have severe damage suchas hydrocephalus, intracranial calcification,retinochoroidittis and mental retardation.5
Rubella infection during pregnancy can leadto congenital infections like cardiovasculardefects, eye defects, deafness and it maycause preterm delivery and still birth. In India10 to 20 % of women in the reproductive groupare susceptible to Rubella.6 In our study 6.9%of women were positive for Rubella IgMantibody sugessting acute infection and 67.4%of women were positive for IgG antibodyindicating past infection. In a retrospectivestudy of 7484 blood samples for Rubellaantibody over a period of 15 years (1988-2002)at NICD, Delhi, the immunity status amongchild bearing women was as low as 49% in1988 and there was steady rise over the periodwhere it was 87% in 2002. However 10 to 15%of women reached childbearing age groupwithout developing immunity.7
Seropositivity rate for CMV Ig M in our studywas 23.26% which is much higher than 8.4%of Turbadkar D et al1 in women with badobstetric history but comparable with 26.7%of another study8. Primary infection with HSVII and I acquired by women during pregnancyaccounts for half of the morbidity and mortalityamong neonates. The other half results fromreactivation of old infection.1 Sero positivityrate for HSV IgM among women with stillbirth
DiscussionPrimary infection with TORCH complex leadsto spontaneous abortions in about 20% ofpregnant women and about 80% of these
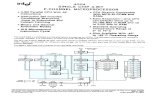
Table 1. Serological analysis for TORCH antibodies in women with still births.
Serological analysis No.of positive Percentage
Toxoplasma Gondii
IgM alone 1
IgM & IgG 39.3
IgG alone 25 58.14
Rubella
IgM alone 1
IgM & IgG 26.98
IgG alone 29 67.44
CMV
IgM alone 2
IgM & IgG 8 23.26
IgG alone 31 72.09
HSV I & II
IgM alone 1
IgM & IgG 820.93
IgG alone 29 67.44
\
\
\
\

JMS * Vol 22 * No. 1 * January, 20084
was 20.93% which was comparable with 26.7%reported by Naveen Thapliyal et al8 but muchhigher than the rate of 3.6% among BOH1.Mixed infections were noted in 6 out of 26women with primary TORCH infection(IgM+ve). One patient had all 4 TORCH IgMantibodies, one with Rubella and HSV, one withHSV, Rubella and CMV and two with CMVand HSV. Similar observation of mixedinfections has been made by other authors.1,8
Among the 43 women studied for TORCH IgMantibodies it is revealed that many women are
still negative for TORCH antibodies indicatingthat there is chance of primary infection withTORCH in further pregnancies and therebychance of fetal morbidity and mortality cannotbe ruled out.
ConclusionIn order to prevent these morbidity andmortality, routine screening for TORCH complexfor antenatal cases with bad obstetric historyshould be carried out for early diagnosis andappropriate management.
ORIGINAL ARTICLE
References1. Turbadkar D, Mathur M, Pele M. Seroprevelance of
TORCH infection in bad obstetric history. Indian JMed Microbiol. 2003; 21(2):108-10.
2. Daftary SN, Chakravarti S. Obstetric disorder in preg-nancy In : Manual of Obstetrics 1st. ed. New Delhi:B1 Churchill Livingstone; 1906.p.138.
3. Bhatia VN, Meenakshi K, Agarwal SC. Toxoplasmo-sis in South India, a serological study. Indian J MedRes. 1974; 62:1818.
4. Rajendra B, Usha S, Kanlakor P, Khadse RK, QaziMS, Jalgaonkar SV. Serological study for TORCHinfections in women with bad obstetric history. J.Obstet. Gynecol. India 2006; 56(1): 41-43.
5. Singh S. Mother to child transmission and diagnosisof Toxoplasma gondii infection during pregnancy. In-dian J. Med. Microbiol. 2003; 21 (2) : 69-76.
6. Seth P. Manjunath N, Balaya S. Rubella infection theIndian scene. Rev Infect Dis .1985; 7 (Suppl 1 ) : S 64.
7. Gandhoke I, Aggarwal R, Lal S, Khare S.Seroprevalence and incidence of Rubella in andaround Delhi. Indian J. Med. Microbiol. 2005; 23 (3) :164-167.
8. Thapliyal N, Sukla P K, Kumar B, Upadhay S,Jain G. TORCH infection in women with bad obstet-ric history - a pilot study in Kumoam region. Indian J.Pathol Microbiol. 2005; 48(4): 551-553.

JMS * Vol 22* No. 1 * January, 2008 5
ORIGINAL ARTICLE
AbstractObjective: Empyema thoracis remains acommon thoracic problem with challengingmanagement strategies. We reviewed ourexperience to outline key aspects of thepresentation, management and outcome of thiscondition in our hospital. Methods: Weanalysed 81 consecutive adult patients, aged18 to 71 years, treated for empyema thoracisover a period of 3 years at Regional Instituteof Medical Sciences (RIMS), Hospital, Imphal.Results: Most of the patients had symptomsattributable to their empyema, with dyspnoeaon exertion being the most common symptoms(95.1%). Broncho-pulmonary infection was themost common aetiological factor, in which65.4% had been treated for pulmonarytuberculosis. Therapeutic thoracentasis wasperformed in six patients, tube thoracostomyin 76 patients and decortication in 52 patients.Decortication was the most successful modeof treatment. Conclusion: Early adequatesurgical drainage and full lung expansion arethe aim of the treatment in empyema thoracis.Success of the operative procedures dependson the stage of disease.
Key words: Empyema thoracis, chestdrainage, decortication, pneumonia.
IntroductionEmpyema thoracis represents a continuum of
Study of empyema thoracis in RIMS hospital
1Th. Chito Singh, 2Ksh. Kala Singh, 2M. Birkumar Sharma, 2Th. Sudhir Chandra
1. Registrar ; 2. Associate Professor, Department ofSurgery, Regional Institute of Medical Sciences (RIMS),Imphal.
Corresponding author:Dr. Th. Chito Singh, Department of Surgery, RIMS, Imphal.Email: [email protected]
disease ranging from thin pleural fluidmicroscopically contaminated by organisms togross purulence with dense deposition of fibrinand scar within the pleural cavity entrappingthe lung. Hippocrates in 600 B.C. definedempyema thoracis as a collection of pus in thepleural cavity and advocated open drainageas its treatment.1 Since then the managementof this condition has posed a challenge to theclinicians.
Different well established therapeuticmodalities - aspiration, lavage, debridement viavideo assisted thoracoscopic surgery,intrapleural fibrinolytic therapy, decortication,thoracoplasty and open window thoracotomyare to be considered in the light of the triphasicnature of the disease. These procedures haveall been used with varying success ratesranging from 10% to 90%.2,3 The success ofthe procedure involved depends on the stageof the disease at presentation, age of thepatient, associated comorbidity and generalcondition of the patient. No single-stageprocedure is suitable for treatment of thoracicempyema.
We reviewed our experience in empyemathoracis with special attention to the clinicalprofile, procedure used and success rate ofeach procedure.
Material and methodsEighty one patients of empyema thoracistreated in RIMS Hospital, Imphal were studiedover a period of three years (Jan 2004 to Dec2006). All the patients were between the age

JMS * Vol 22 * No. 1 * January, 20086
ORIGINAL ARTICLE
group of 18 to 73 years. 58 patients were maleand 23 female.
Empyema thoracis was confirmed in all thepatients by (1) pleural fluid culture or Gram'sstain showing organisms, or (2) documentationof grossly purulent fluid at thoracentasis orthoracostomy. Empyema thoracis resultingfrom oesophageal operation or perforationwere excluded.
Multiloculated empyema thoracis was definedby the presence of two or more collections ofpleural fluid observed on chest X-ray,ultrasonography and/or CT scan. Successfulprocedures were defined by empyemaresolution with complete re-expansion oftrapped lung and no further surgicalintervention was required.
Treatment included multiple therapeuticthoracocentasis, closed tube drainage ordecortication. Selection of appropriatetreatment was dependent on the duration andextent of disease, age and fitness of the patient.Closed tube thoracostomy was carried out witha chest tube connected to underwater sealdrainage bag. Suction was not applied. Chesttube was removed when the daily chest drainoutput was below 50 ml and improvement inthe chest radiograph was noted. Decorticationwas performed in the organization phase ofthe empyema thoracis, post-traumaticempyema thoracis, multiloculated or failure toresolve after tube thoracostomy. This operationwas carried out through a standardposterolateral thoracotomy with or without ribresection.
ResultsEighty one patients were included in thispresent study comprising 58 males and 23females within the age group of 18 to 73 years.
Most of the patients had symptoms attributableto their empyema, with dyspnoea on exertionbeing the most common symptoms (95.1%),followed by fever (84.0%). Presentingsymptoms of the patients is shown in Fig.1.
The aetio-pathogenesis of the patients in thepresent study is shown in table 1. Sixty nine
for pulmonary tuberculosis. The antituberculartherapy was started by primary physicianbefore being referred to us. 9 patients hadhistory of firearm injury in the chest and 2patients had history of stab injury in the chest.One patient who had undergonepneumonectomy in a centre outside the statepresented to us with post-pneumonectomyempyema thoracis.
Therapeutic thoracentasis was performed insix patients, of which 4 patients had to undergotube thoracostomy because of inadequatedrainage. Altogether 76 patients underwenttube thoracostomy as primary procedure in 72cases, and as secondary procedure in 4patients who was not benifitted bythoracentasis. Of these 76 patients (93.8%),52 had to undergo decortication. However, 3other patients who presented with calcifiedloculated empyema on chest X-ray haddecortication as initial mode of treatment. Theprocedure employed and their success rate aregiven in table 2.
patients (85.2%) had broncho-pulmonaryinfection, of which 53 patients had been treated
Fig 1. Presenting symptoms of the patients.
Table 1. Aetiology of empyema thoracis.
Aetiology No. of patients (%)
Inflammatory 69(85.2)
(a) Non tubercular 16
(b) Tubercular 53
Post traumatic 11(13.6)
Post-pneumonectomy 1(1.2)

JMS * Vol 22* No. 1 * January, 2008 7
ORIGINAL ARTICLE
Postoperative complications were listed intable 3, which includes air leak, surgicalemphysema, wound infection and frozenshoulder. All the complicated cases weremanaged conservatively and improved withtime before sending home except frozenshoulder which was subjected tophysiotherapy.
Length of hospital stay varied from 8 days to46 days. One patient with the air leak afterdecortication took 39 days to subside.
DiscussionTreatment for thoracic empyema requiresappropriate antibiotics, prompt drainage of theinfected pleural space and lung re-expansion.However, there is no clear consensus on thebest way to obtain these objectives.4 Thevariable success rates of the procedures canbe attributed, in part, to the stage of theempyema at presentation.
Empyema thoracis may be classified based onthe chronicity of the disease process.5 In theinitial exudative stage, pleural fluid is freeflowing and usually amenable to multiplethoracentasis or by tube thoracostomy.Progression to the fibrinopurulent stage, whichbegins after 48 hours, results in the formation
of fibrin strands throughout the pleural fluidcreating a multiloculated pleural space. At thispoint, closed drainage with chest tube isunlikely to be successful. Progression to theorganizational stage which may occur after aslittle as 1 to 2 weeks virtually requiresdecortication because of the extensive pleuralpeel that restricts lung expansion even if thefluid can be successfully drained.
Since many of the infections that causeempyema are indolent, patients are oftentreated by physicians after theirparapneumonic empyema has alreadyreached the fibrinopurulent or organizationalstage. Majority of our patients presented in thelater stage of the disease with multiloculation,thick-walled uniloculated empyema or withtrapped lung.
Tube thoracostomy is usually the initialtreatment of acute empyema thoracis.LeMense GP et al6 reported a success rate of70% - 85% with tube thoracostomy, which isonly 35.6% in our study. This discrepancy isbecause of the late presentation of our patients.Although about half of the successful patientsin tube thoracostomy had some form of pleuralthickening radiographically, the natural historyand significance of these findings are notknown. However, at least some of the patientsshowed continued radiographic improvementafter removal of tubes in limited follow up.
Bilgin M et al7 reported that video assistedthoracoscopic evacuation and chest tubedrainage in situ reduces the necessity of opendecortication. However, this is effective onlyin the fibrinopurulent phase of the disease.Basic elements of intervention - pleuraldrainage, different evacuation techniques,decortication, thoracoplasty and open windowthoracostomy - are well established technicalmodalities.8 Majority of our patients presentedin the chronic stage of the disease.
Length of hospital stay for empyema thoracisis long because of multiple procedures andcoexistent diseases.ConclusionThe lack of a single ideal treatment modalityreflects the complexity of the diagnosis and
Table 2. Procedures employed in the treatment.
Procedure No. of patients Success rate (%) (%)
Aspiration 6 (7.4%) 2 (33.3%)
Tube thoracostomy76 (93.8%) 27 (35.6%)
Decortication 52 (64.2%) 50 (96.2%)
Table 3. Postoperative complications after decortication
Complications No. of patients (%)
Air leak 2
Surgical emphysema 2
Wound infection 1
Frozen shoulder 3

JMS * Vol 22 * No. 1 * January, 20088
ORIGINAL ARTICLE
staging of empyema thoracis. Intrapleuraldrainage remains to be the initial treatmentmodality in acute stage of the disease.Organized pleural callus requires formal
decortication. Decision-making involves a triadconsisting of the aetiology of empyema,general condition of the patient and stage ofdisease, while considering the triphasic natureof development of thoracic empyema.
References1. Adams F. The genuine works of Hippocrates. 1st ed,
Baltimore: William and Wilkins Company;1939.p.51-52.
2. VanSonnenberg F, Nakamoto SK, Mueller PR, et al.CT and ultrasound-guided catheter drainage ofempyemas after chest tube failure. Radiology 1984;151:349-53.
3. Lee KS, Im JG, Kim YH, Hwang SH, Bae WK, LeeBH. Treatment of thoracic multiloculated empyemaswith intracavitary urokinase: a prospective study.Radiology. 1991;179:771-5.
4. Strange C, Sahn SA. The clinician's perspective onparapneumonic effusions and empyema. Chest1993; 103:259-61.
5. Lukanich JM, Sugarbaker DJ. Chest wall and Pleura.In: Townsend CM, Beauchamp RD, Evers BM, MattoxKL, editors. Sabiston textbook of Surgery, 17th ed,Philadelphia: Saunders; 2004.p.1711-1733.
6. LeMense GP, Strange C, Sahn SA. Empyemathoracis - therapeutic management and outcome.Chest 1995;107:1532-7.
7. Bilgin M, Akcali Y, Oguzkaya F. Benefits of earlyaggressive management of empyema thoracis. ANZJ Surg 2006;76(3):120-2.
8. Molnar TF. Current surgical treatment of thoracicempyema in adults. Eur J Cardiothorac Surg 2007;32(3):422-30.

JMS * Vol 22* No. 1 * January, 2008 9
AbstractObjective: To study the various clinico-morphological pattern of beetle dermatitis inManipur and to identify the causative beetlein this region. Methods: 362 cases ofsuspected beetle dermatitis attending the SkinOPD, Regional Institute of Medical SciencesHospital, Imphal between the period March2001 and April 2003 were taken up for thedescriptive study. Results: There were 204males (56.35%) and 158(43.65%) females.Maximum number of patients were in the agegroup 21-30 years (n= 124; 34.25%). Twohundred twentynine (63.25%) and133(36.74%) patients belonged to urban andrural areas respectively. The exposed areasnamely the neck (n=140; 38.67%), face(n=135; 37.29%) and arms (n= 50; 13.8%)were commonly affected. In15 patients(4.14%) there were generalized lesions.Morphology of the lesions varied from theclassical linear lesions with necrotic centre andpustules in the periphery to ovoid and irregularpatches. Small non- descript lesions were alsoseen in some cases. Main presentingsymptoms included burning sensation, pain,tightness and limitation of movement at theaffected site. Constitutional features were alsonoted in those cases with very necrotic and
Beetle dermatitis in Manipur
1Th. Nandakishore, 2 Roslin L, 3Romita B, 2Kalkambe KA
1. Assistant Professor; 2. Registrar ; 3. Junior Resident,Department of Dermatology, Regional Institute ofMedical Sciences (RIMS), Imphal.
Corresponding author:Dr. Th.Nandakishore, Department of Dermatology, RIMS,Imphal, ManipurE-mail: [email protected]
extensive lesions. Maximum cases (56.35%,n=203) presented on the 2nd or 3rd day. Thecaptured beetle belonged to Coleoptera class,Staphylinid family, Paederus genus andsemipurpureous species. Conclusion: Blisterdermatitis is a common easily treatableseasonal dermatitis with little symptoms andcomplications. However a proper diagnosis isessential to allay anxiety among the victimsand proper recognition of such commondisorders is also necessary for medicalpersonnel to avoid inappropriate treatment.
Key words: Beetle, paederus, dermatitis.
IntroductionBeetle dermatoses have been recognized asa common seasonally occurring dermatitis.Although there are more than 2, 80,000species, common beetles which aredermatologically relevant belong to two familiesnamely Meloidae (Blister beetle) andStaphylinidae (Rove beetles). They causeeither a vesicant ( irritant ) reaction frompowerful irritants contained in their body fluidsor allergic contact dermatitis the former beingmore commoner.1
Blister beetles are found in Europe, Unitedstates and Africa whereas rove beetles has aworldwide distribution and has been foundfrequently in tropical areas of the Orient, Africa,South America and Australia.2 Blister beetlescause acute dermatitis which are not properlyrecognized or misunderstood though thisdermatitis is quite common and known to occurseasonally affecting all populations alike.
ORIGINAL ARTICLE

JMS * Vol 22 * No. 1 * January, 200810
Though there are many reports of suchdermatitis both in India3-8 and abroad9-11 no suchstudies has been undertaken in North-EastIndia including Manipur. This study wasconducted to investigate the incidence, extentand clinical patterns of beetle dermatitis andto identify the causative beetle in this region.
Material and methodsThe study was carried out on 362 patients withsuspected beetle dermatitis attending the SkinOPD, Regional Institute of Medical Sciences,Imphal during the period of March 2001-April2003. A medical history was recorded andclinical examination was performed. Skinbiopsies were taken in a few cases. Suspectedbeetles were caught and species identified inconsultation with the Department of LifeSciences, Manipur University.
ResultsOut of the 362 cases included in the study, therewere 204 males (56.35%) and 158(43.65%)females. The youngest patient was 1-1/2 yrand the oldest 68 yr. Most of the cases belongedto the age group of 21-30 years comprising of
contact with any insects. Table 2 shows the siteof lesions affected in patients with Paederusdermatitis. The exposed areas of face, neck andarms were commonly affected. The mostcommon site was the neck seen in 140 (38.67%)patients and 135 (37.29%) patients had lesionson the face. Involvement of the scalp was rare,seen in only 6 patients (1.65%). Fifteen (4.14%)patients had generalized lesions involving morethan 3 sites (face, trunk, and upper thighs).Involvement of the flexural areas like cubital andpopliteal fossa showing kissing lesions was alsocommon. Morphology of the lesions varied fromthe classical linear lesions with necrotic centre
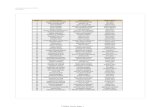
Table 1. Age by sex distribution of affectedcases
124 (34.25%) patients (Table1). Children wereleast affected. Two hundred twentynine(63.25%) and 133(36.74%) patients belongedto urban and rural areas respectively. Most ofthe patients gave history of sleeping in the nightwith lights on. Two hundred thirtyfive (64.4%)patients noticed the lesions in the morning afterwaking up while washing the face. However,many of them were unaware of any direct
Fig 1. Classical Paederusdermatitis lesions on the neck.
Main presenting symptoms included burningsensation, pain, tightness and limitation ofmovement at the affected site. Itching wasminimal to absent. Constitutional features likefever were also noted in a few cases when thelesions were very necrotic and extensive.Maximum number of patients 203(56.35%)presented on the 2nd or 3rd day. Only 31 (8.5%)
Table 2. Distribution of skin lesions inpatients with Paederus Dermatis
Sites Number* Percentage
Neck 140 38.67Face 135 37.29Arms 50 13.8Chest 10 2.7Shoulder 15 4.14Axilla 8 2.2Scalp 6 1.65Generalised 15 4.14
*The number of lesion sites affected is more thanthe actual number of patients (n=362) as in manypatients more than one site was involved.
ORIGINAL ARTICLE
and pustules in theperiphery (Fig 1)to ovoid andirregular patches.Small non-descript lesionswere also seen insome cases.Lympha-denitiswas not seen inour cases.
Age group Male Female Total(%)(years)0-10 18 19 37(10%)
11-20 64 52 116(32%)
21-30 71 53 124(34%)
31-40 37 16 53(15%)
>40 14 18 32(9%)
Total 204 158 362(100%)

JMS * Vol 22* No. 1 * January, 2008 11
Fig 4. Paederus semi-purpureus
Fig 3. Seasonal distribution of Paederus dermatitis from March 2001 to April 2003
ORIGINAL ARTICLE
Fig 2. Photomicroph showingsubcorneal pustules, acan-tholytic cells and mixedinflammatory infiltrate in thedermis (HE Stain, x 100).
Biopsy of the lesions showed mostly necrosisof the epidermis with inflammatory cellinfiltration in the early phase(day 2/3) whereassubcorneal pustules with heavypolymorphonuclear cell infiltration in thosepresenting late (day 4/5) (Fig 2).
Incidence of the disease was very high duringhot and wet weather. In the year 2001, therewere double peaks in the incidence of thedermatitis during the months of May andSeptember coinciding with heavy rainsincluding flood during these months (Fig 3). Inthe year 2003 maximum cases occurred duringthe month of April.
The captured beetle measured about 3-8mmin length with red thorax, greenish black body,dark brown antenna and was identified asbelonging to Coleoptera class, Staphylinidfamily, Paederus genus and semipurpureousspecies (Fig 4).
DiscussionDa Silva from Brazil first described Paederus asa cause of dermatitis in 1912 12, and Lehman etal 13 in 1955 described blister beetle dermatitis.Subsequently many reports came from SriLanka9, Australia10 and America11 and in Indiareports have come from Punjab3,4, Rajasthan5,South India 6,7 and Eastern India.8 Different
geographical areas may report the incidence atdifferent times of the year. In Manipur rainyseason generally occurs during May toSeptember but pre monsoon showers alsooccurs quite frequently during February to April.Though most Indian studies have recordedbeetle dermatitis in the post monsoon periodparticularly, during April-September, our findingsalso support the eastern Indian report that in thesub-Himalayan region, incidence of beetledermatitis occurs perennially as rains occur inprotracted period during the year. Humidenvironment seems to be fertile for thepropagation of the beetle as even during rainyseason no dermatitis is reported if droughtoccurs as seen in June –July 2001. Clusteringof cases which were noticed at the time of heavyrain and flood seen in May and Sept 2001 andlow incidence in cooler months November toFebruary in our study corroborated findings ofother studies.11
There was no predilection of age, sex, rural orurban in the occurrence of the disease as thedermatitis depended on the patient’s activitiesand insect habitat.
In our series 235 patients (64.5%) noticed thelesions in the morning further corroboratingthe nocturnal habit of the insects3. As reportedin other studies6 where exposed partsparticularly face and neck of the bodycontributed for most number of lesions whenthe insects easily come into contact with.However covered parts can also be involved.Other than producing local irritant dermatitis-like picture as reported by other workers 3, 6,our study also revealed that the dermatitis canbecome generalized involving face, trunk,covered parts even masquerading aseczema-tous dermatitis. Complica-tions included post inflam-matory
hyperpigmentation inmost of the cases.
Biopsy of the lesionsrevealed initial toxic effectcharacterized bynecrosis, inflammatorycell infiltration andpolymorphonuclear cellinfiltration as the lesionprogressed.

JMS * Vol 22 * No. 1 * January, 200812
presented beyond 5th day.
Paederus beetles are nocturnal and areattracted by incandescent and fluorescentlights and as a result inadvertently come intocontact with humans. However, daytimecontact may also occur as revealed bysignificant number of patients affected inoutdoor also. Hemolymph of the beetlecontains paederine which is released oncrushing of the insect onto the skin due to reflexof brushing away the insect. Paederin, analkaloid is largely produced by adult femalebeetles. Blisters are the result of activation orrelease of neutral serine proteases which acton the desmosomal region resulting inintraepidermal separation with little scarring butsignificant post inflammatory pigmentation.There are more than 30 species of Paederuswhich can cause dermatitis. Indian reports havementioned Paederus melampus as thecommonest14, P.fuscipes, P.irritants,P.sabaeus, P.himalayicus being other speciesidentified1. Paederus semipurpureus is thespecies identified in our region. Clinically,
paederus dermatitis should be differentiatedfrom herpes simplex, herpes zoster, liquidburns, and acute allergic or irritant contactdermatitis from other causes. Linearappearance of the lesions, their predilectionfor exposed areas, and the presence of kissinglesions are very characteristic. Histopatho-logical and epidemiological features also helpin making definite diagnosis.14
ConclusionBlister dermatitis is not an uncommon seasonaldermatitis with little symptoms but can be asource of apprehension for the patient for moreserious conditions which look morphologicallysimilar and is noteworthy for cosmeticconsideration. A proper diagnosis andtreatment is therefore essential to allay anxietyamong the victims which requires awarenessof such common disorders amongst the medicalpersonnel.
AcknowledgementThe authors wish to express their gratitude to Prof.T. Kameshwar Singh, Dept of Life Sciences,Manipur University for his valuable expertise in theidentification of the beetle involved in the present
study.
References1. Nair BKH, Nair TVG .Diseases caused by
arthropods. In: Valia R.G., Valia A.R. editors.IADVL Textbook and Atlas of Dermatology.2nd
edition. Mumbai, India: Bhalani publishinghouse ; 2001. p . 340-41.
2. Shatin H. Dermatoses caused by Arthropods.In: Canizares O. ed. Clinical TropicalDermatology. Oxford : Blackwell ScientificPublications ; 1975. p. 252-253.
3. Handa F, Pradeep S, Sudarshan G. Beetledermatitis in Punjab. Indian J DermatolVenereol Leprol 1985; 51:208-12.
4. Kalla G, Ashish B. Blister beetle dermatitis.Indian J Dermatol Venereol Leprol. 1997;62:267-8.
5. Bhargava RK, Gupta B. Seasonal blisteringdermatitis. JIMA 1982; 99: 98-9.
6. Ravi Vadrevu. Book of abstracts, IADVL,Dermavision ; 2000 . p .141.
7. Apratim Goel, Shenoi SD. Book of Abstracts,
IADVL, Dermatech ; 2001 . p . 156.8. Sujit SR, Kaushik L. Blister beetle dermatitis
in West Bengal. Indian J Dermatol VenereolLeprol. 1997 ; 63 : 69-70.
9. Kamaladasa SD, Perera WD, Weeratunge L.An outbreak of Paederus dermatitis in asuburban hospital in Sri Lanka. Int J Dermatol.1997 ; 36 (1):34-6.
10. Banny LA, Wood DJ, Francis GD. Whiplashrove beetle dermatitis in central Queensland.Aust J Dermatol. 2000 ; 41 : 162- 7.
11. Claborn DM, Pola JM, Olsa PE, Earhart KC,Sherman SS. Staphylinid (rove) beetledermatitis outbreak in the American Southwest?Mil Med. 1999 ; 164 : 209-13.
12. Skin eruptions caused by Beetles(Coleoptera). In: John O’Donel Alexander.Arthropods and Human Skin. 1st ed. Berlin/New York : Springer–Verlag ; 1984.p.75-85.
13. Lehmann CF, Pipkin JL, Ressman AC. Blisterbeetle dermatosis. Arch Dermatol. 1955 ; 71 :36-8.
14. Singh G, Yousuf Ali S. Paederus dermatitis.Indian J Dermatol Venereol Leprol. 2007 ; 73:13-15.
ORIGINAL ARTICLE

JMS * Vol 22* No. 1 * January, 2008 13
Effect of Azadirachta indica Linn. aqueous leaf extract on blood glucose inadrenaline induced hyperglycemia in albino rats.
ORIGINAL ARTICLE
1Lakshman Das, 2Ng. Gunindro, 3S. Rita, 4R.K. Bharati
AbstractObjective: To evaluate the effect ofAzadirachta indica aqueous leaf extract (ALE)on blood glucose in normal as well asadrenaline induced hyperglycemic albino rats.Methods: Effects of ALE (500 and 1000 mg/kg p.o.) on blood glucose levels wereevaluated in normal and adrenaline (0.5 mg/kg i.p.) induced hyperglycemic albino rats.Blood glucose levels were measured just priorto and after 30, 60 and 120 min of ALEadministration. The control and standard drugsused were 5% gum acacia suspension (5ml/kg p.o.) and glibenclamide (0.5 mg/kg p.o.) in5% gum acacia suspension respectively.Results: Blood glucose levels of normal rats,treated with ALE (500 and 1000 mg/kg p.o.)showed significant reduction (p<0.05) ascompared to control. The maximum reductionof blood glucose was observed at 60 min. Thehyperglycemic response to adrenaline (0.5 mg/kg i.p.) was not reduced by ALE (500 and 1000mg/kg p.o.) treatment. Conclusion: ALEproduces fall in the blood glucose level innormal albino rats. However, ALE fails toreduce adrenaline induced hyperglycemiasuggesting that it does not have inhibitory effecton glycogenolysis.
1.Post graduate student; 2.Senior demonstrator;3.Professor; 4.Professor and Head,Department ofpharmacology, Regional Institute of Medical Sciences(RIMS), Imphal, Manipur.
Corresponding author :Dr. Lakshman Das, Department of Pharmacology, RIMS,Imphal. E- mail :[email protected]
Key words: Azadirachta indica, blood glucose,adrenaline induced hyperglycemia,
IntroductionDiabetes mellitus is a metabolic disorder inwhich the body does not produce or properlyuse insulin. It causes disturbances incarbohydrate, protein and lipid metabolismleading to complications such as retinopathy,microangiopathy and nephropathy.1 Currentlyavailable antihyperglycemic agents for clinicaluse have characteristic profile of side effects.2
In accordance with the WHO expert committeeon diabetes mellitus, investigation ofantihyperglycemic agents of plant origin usedin traditional medicine is considered important.Many herbs and plant products have beenshown to have antihyperglycemic action.3
Azadirachta indica Linn. has been mentionedto possess a number of pharmacological effectslike hypoglycemic, hypotensive, antiserotonin,anti-inflammatory and hepatoprotective.4
The objective of the present study was toevaluate effect of Azadirachta indica Linn.aqueous leaf extract on blood glucose innormal as well as adrenaline inducedhyperglycemic albino rats.
Material and methodsAnimals: Albino rats of Wistar strain (150 -200g) of either sex were used. Animals wereobtained from the RIMS central animal houseand kept in polypropylene cages in thedepartmental animal house. They wereacclimatized for 10 days and fed on standard

JMS * Vol 22 * No. 1 * January, 200814
ORIGINAL ARTICLE
laboratory diet with water ad libitum. 12 hourslight and dark cycle was maintained.
Laboratory practice:The Institutional Ethics Committee of RIMS,Imphal approved the protocol of the study.
Preparation of the extract:Fresh leaves of Azadirachta indica (family -Meliaceae), a tree known as Neem werecollected during the month of June and July,and authenticated. The aqueous extract of theleaves was obtained by the procedure asdescribed by Khosla et al.5 One kg of freshlycollected, shade dried, powdered leaves of A.indica were ground and soaked in 4 litres ofdistilled water overnight. The suspension wascentrifuged at 5000 rpm for 20 min and filteredthrough Whatman No.1 filter paper. Thesupernatant fluid was allowed to evaporate insterile petridishes. After drying, the extract wascollected by scrapping and stored. The yieldwas 12.5%. The extract was found to be safeup to 2g/kg p.o. in albino mice.
The effect of A.indica aqueous leaf extract wasstudied both in normal and adrenaline inducedhyperglycemic rats.
1. Effect of A. indica aqueous leaf extract (ALE)on blood glucose in normal albino rats.
24 albino rats weighing 150 -200 g were usedfor the experiment. They were divided into 4groups of 6 animals in each group and keptfast for 18 h with free access to water. Carewas taken to prevent corpophagy. Bloodsamples were collected from orbital sinus forglucose estimation. Then the animals weretreated as follows:Group - I (control) Aqueous 5% gum acacia
(5 ml/kg, p.o.).Group - II (test -1) ALE (500 mg/kg p.o.)Group - III (test - 2) ALE (1000 mg/kg p.o.)Group - IV (standard) Glibenclamide (0.5 mg/kgp.o.)
Test and standard drugs were given using 5%aqueous gum acacia suspension as vehicle.Blood samples were collected from orbitalsinus at 30, 60, and 120 min after drugadministration. Blood glucose was estimatedby glucose oxidase method.6 Results were
analysed by One-way ANOVA followed byDunnett's't' test. P<0.05 was considered to bestatistically significant.
1. Effect of A. indica aqueous leaf extract (ALE)on blood glucose in adrenaline inducedhyperglycemia.
Effect of A.indica aqueous leaf extract onadrenaline induced hyperglycemia was studiedby the method of Gupta et al7 and Anturlikar etal.8 24 Wistar albino rats of either sex weighing150 - 200g were divided into 4 groups of 6animals in each group. After 18 h fasting withfree access to water, the rats were treated asfollows:
Group - I (control) : Aqueous 5% gum acacia (5 ml/kg,p.o.) + Inj. Adrenaline hydrochloride(0.5 mg/kg i.p.).
Group - II (test -1) : ALE (500 mg/kg p.o.) + Inj.Adrenaline hydrochloride (0.5 mg/kg i.p.).
Group - III (test - 2) : ALE (1000 mg/kg p.o.) + Inj.Adrenaline hydrochloride (0.5 mg/kg i.p.).
Group - IV (standard) : Glibenclamide (0.5 mg/kg p.o.) + Inj.Adrenaline hydrochloride (0.5 mg/kgi.p.).
Blood samples were collected for glucoseestimation just prior to and at 30, 60 and 120min after drug administration. The results wereanalysed by One-way ANOVA followed byDunnett's 't' test. P<0.05 was considered tobe statistically significant.
Results1. Effect of A.indica aqueous leaf extract (ALE)on blood glucose in normal albino rats.
ALE at the dose of 500 mg/kg p.o. reducedblood glucose significantly (p<0.01) at 60 minas compared to control. The dose of 1000 mg/kg p.o. of the extract produced significantreduction of blood glucose at 30 min (p<0.01)as compared to control and the hypoglycemiacontinued to persist significantly (p<0.001) atthe 60 and 120 min. The maximum reductionof blood sugar was seen at 60 min. Thereduction of blood glucose levels byglibenclamide (0.5 mg/kg p.o) at 60 and 120min were highly significant (p<0.001) as

JMS * Vol 22* No. 1 * January, 2008 15
ORIGINAL ARTICLE
compared to control group (Table 1).
2. Effect of A. indica aqueous leaf extract (ALE)on blood glucose in adrenaline inducedhyperglycemia.
The hyperglycemic response after adrenaline(0.5 mg/kg i.p.) was seen maximum at 60 min.ALE at the doses of 500 and 1000 mg/kg p.o.failed to reduce adrenaline inducedhyperglycemia, but there was significantincrease (p<0.05) in the blood glucose levelas compared to control group. Thehyperglycemic responses of adrenaline at 60and 120 min were reduced significantly(p<0.05) by glibenclamide (0.5 mg/kg p.o)(Table 2).
Table 1. Effect of A.indica aqueous leaf extract (ALE) on blood glucose in normal albino rats.
Blood sugar level (mg %)
Group Fasting 30 min 60 min 120 minControl 89.5 ± 6.18 88 ± 6 90.5 ± 5.47 91 ± 8.97Test - 1 92 ± 5.79 86.5 ± 6.5 80.5 ± 5.89* 84.5 ± 8.02Test - 2 90 ± 6.83 75.5 ± 7.58* 64 ± 5.76** 72 ± 8.46**Standard 91 ± 5.55 79.5 ± 8.34 69.5 ± 6.69** 68 ± 8.53**
One - way ANOVA F 0.21 4.05 23.33 9.22df 3,20 3,20 3,20 3,20p >0.1 <0.025 <0.01 <0.01
Values are mean ± SD; n = 6 in each group, *p <0.01, **p <0.001 as compared to control (Dunnett's 't' test).
DiscussionIn the present study, the two doses of 500 and1000 mg/kg p.o. of Azadirachta indica aqueousleaf extract (ALE) produce hypoglycemic effectin normal rats. This finding is in agreementwith the reports of other workers.5,9 Maximumreduction of blood sugar is observed at 60 minafter administration of the extract. ALE at
the dose of 1000 mg/kg p.o. produces morehypoglycemic effect as compared to 500 mg/kg dose.
Adrenaline is the most potent stimulant ofhepatic glycogenolysis and gives rise toglucose 6-phosphate, which readily enters thecirculation and increases the blood glucoselevel.10 In our study, hyperglycemia is seenat 30, 60 and 120 min after adrenalineadministration. Both the doses of 500 and1000 mg/kg p.o. of ALE fail to reduce thishyperglycemic response as compared tocontrol. This finding is in variance with Murtyet al.6 Failure to reduce adrenaline inducedhyperglycemia shows that Azadirachta indicaaqueous leaf extract is devoid of inhibitory
effect on glycogenolysis. The hypoglycemiceffect of the extract in normal rats will be dueto its effects on other metabolic processesother than inhibition of glycogenolysis.
ConclusionThe present study shows that Azadirachtaindica aqueous leaf extract produces fall in
Table 2. Effect of A.indica aqueous leaf extract (ALE) on adrenaline induced hyperglycemia.
Blood sugar level (mg %)
Group Fasting 30 min 60 min 120 minControl 89 ± 3.32 103.5 ± 6.31 159 ± 6.28 150 ± 6Test - 1 91.5 ± 3.06 113.5 ± 4.08 186.5 ± 10.15 * 180 ± 6.35*Test - 2 88 ± 4.24 136 ± 6.51 178 ± 5.54* 161 ± 6.98*Standard 92 ± 3.89 114.5 ± 11.0 140 ± 6.26* 116 ± 5.54*
One - way ANOVA F 0.725 20.72 48.26 111.01df 3, 20 3, 20 3, 20 3, 20P >0.05 <0.001 <0.001 <0.001
Values are mean ± SD; n = 6 in each group, * p<0.05 as compared to control (Dunnett's't'test).

JMS * Vol 22 * No. 1 * January, 200816
ORIGINAL ARTICLE
blood glucose level in normal rats. It does notreduce elevated blood glucose level afteradrenaline administration. The failure to reduce
adrenaline induced hyperglycemia signifies thatthe extract does not have inhibitory effect onglycogenolysis.
References1. Rameshkumar K, Shah SN, Goswami BD, Mohan V,
Bodhankar SL. Efficacy and Toxicity of Vanadiumnicotinate in diabetic rats. Toxicol Int. 2004; 11: 75 - 80.
2. Rao KB, Kesavulu MM, Giri R, Apparao CH. HerbalMedicines. Manphar Vaidya Patrika 1997; 1: 33 - 35.
3. Bailey CJ, Dav C. Traditional plant medicines astreatment of diabetes. Diabetic care 1989; 12: 553 - 564.
4. Chopra RN, Nayer SL, Chopra IC. Azadirachtaindica, Glossary of Indian medicinal plants. 1st Edn.Council of Scientific and Industrial Research, NewDelhi 1956; 31.
5. Khosla P, Bhanwara S, Singh J, Seth S, SrivastvaRK. A study of hypoglycemic effect of Azadirachtaindica (Neem) in normal and diabetic rabbits. IndianJ Physiol Pharmacol 2000; 44(1): 69 - 74.
6. Barham D, Trinder P. An improved colour reagentfor determination of blood glucose by oxidase
system. Analyst 1972; 97: 142 - 145.
7. Gupta SS, Verma SCL, Garg VP, Rai M. Antidiabeticeffects of Tinospora cardifolia (part-I): effect onfasting blood sugar level, glucose tolerance andadrenaline induced hyperglycemia. Indian J Med Res1976; 55: 733 - 745.
8. Anturlikar SD, Gopumadhavan S, Chauhan BL, MitraSK. Effect of D - 400, a herbal formulation, on bloodsugar of normal and alloxan induced diabetic rats.Indian J Physiol pharmacol 1995; 39(2): 95 - 100.
9. Murty KS, Rao DN, Rao DK, Murty LBG. Apreliminary study on hypoglycemic andantihyglycemic effects of Azadirachta indica. IndianJ Pharmacol 1978; 10(3): 247 - 250.
10. Lee TJ, Stitzel RE. Adrenomimetic drugs. In: Craig CR,Stitzel RE, editors. Modern Pharmacology. 2nd ed. NewYork: Little brown Company; 1994. p. 115-128.

JMS * Vol 22* No. 1 * January, 2008 17
ORIGINAL ARTICLE
AbstractObjective: To study the spectrum of bonemarrow metastasis of solid tumours in RegionalInstitute of Medical Sciences (RIMS) Hospital,Imphal. Methods: Retrospective analyses of905 bone marrow aspirates conducted duringthe period from June 2000 to May 2005 in thedepartment of Pathology, RIMS, Imphal,Manipur, was done. Detailed clinical data,investigation results including completehaemogram were collected from the medicalrecord section. Bone marrow smears were re-examined independently by twohaematopathologist. Results: Out of the 905cases analyzed, metastatic infiltration in bonemarrow was encountered in 22 cases (2.43%).In 8 cases (36.36%), the primary sites couldnot be ascertained because of theundifferentiated morphology. Among children,all the 4 cases (18.18%) were Neuroblastoma.In adults, the primary sites were breast(13.63%) and GIT (13.63%). There were 2cases (9.09%) each from carcinoma prostateand lung. The age group ranged from 10months to 75 years with mean age of 55 years.Male to female ratio was 1.3:1. Majority of thepatients were more than 45 years.Conclusion: Bone marrow examination is an
Bone marrow metastasis of solid tumours
1Laishram Rajesh Singh, 1Sushma Khuraijam, 2R.K.Tamphasana Devi, 3A. Meina Singh, 3D.C Sharma,3Y. Mohen Singh.
1.Demonstrator; 2.Asst. Professor; 3.Professor,Department of Pathology, Regional Institute of MedicalSciences(RIMS), Imphal-795004 Manipur, India.
Corresponding author:Dr.Laishram Rajesh Singh, Department of Pathology,RIMS,Lamphelpat, Imphal-795004 India.Phone:91-0385-2427280 Fax: 91-385-2400727E-mail: [email protected].
effective, economical and easy procedure indetecting solid tumour metastasis. It may,therefore be considered to be included in theroutine investigation panel for cancer patients.
Key words: Bone marrow, metastatictumours.
IntroductionBone marrow (BM) is one of the most commonsites of tumour metastasis via blood streamand signifies poor prognosis. It is thereforeconsidered imperative to rule out BMinvolvement in malignancies likeneuroblastoma, carcinoma breast, lungs andprostate where curative treatment isenvisaged.1 BM examination has been foundto be increasingly useful in documentingmetastatic deposits of tumours havingpredilection for haematogenous spread.2
In adults, carcinomas of breast, lung andprostate account for majority of metastasis inbone marrow specimens.3,4 Less commonsources of malignancies are gastrointestinaltract, kidneys and skin. In childrenneuroblastoma, rhabdomyosarcoma andEwing's sarcoma constitute the majority of BMmetastasis.5 BM evaluation is also done forstaging of lymphomas and other malignanttumours.
BM infiltration is suspected on the basis of bonepains, pathological fractures, lytic or scleroticlesions on X-ray, hypercalcaemia, elevatedserum alkaline phosphatase or unexplainedhaematogical abnormalities such as

JMS * Vol 22 * No. 1 * January, 200818
ORIGINAL ARTICLE
leukoerythroblastic picture etc. However,metastasis missed by bone scans andradiographic pictures, may be detected inrandom marrow aspirates.6
We reviewed BM aspirates with metastaticinvolvement during the last five years andevaluated haematological findings andassociated changes in haemopoietic andstromal elements of BM.
Material and methodsThe retrospective study was carried out atRIMS Hospital, Imphal, Manipur. Detailedclinical and investigation data were collectedfrom medical record section. A total of 905 bonemarrow aspirations was performed during theperiod June 2000 to May 2005. BM smearscollected were re-examined by twohaematopathologist independently. Smearswere routinely stained by Leishman's stain.Special stains such as Periodic Acid Schiff's(PAS) stain, Myeloperoxidase and Iron stainswere also used for some selective cases.
Cases subjected to BM examinations were asa part of tumour staging (13 cases) or due todevelopment of severe anaemia (4 cases) orbone pains (2 cases) or for investigatingpyrexia of unknown origin (3 cases).
ResultsA diagnosis of metastatic infiltration in BM wasencountered in 22 cases (2.43%) of which 18(81.81%) were in adults and 4 (18.18%) inchildren. The age group ranged from 10months to 75 years with mean age of 55 years.(Table.1) Male to female ratio was 1.3:1. Mostof the patients were more than 45 years. In 8cases (36.36%), the findings were incidental
and primary sites could not be ascertained.Among children, all the 4 cases (18.18%) weremetastatic neuroblastomas(Fig 1). In adults,the primary sites were breast (3 cases,13.63%) (all females) and GIT (3 cases,13.63%) (1 male and 2 females). There were2 cases (9.09%) each from carcinoma prostate(Fig 2) and lung (1 male and 1 female)(Table 2).
Fig 1. Photomicrograph ofBM aspirates showing bloodmixed aspirates and roundcell tumour metastasis.(Leishman’s stain, X400)
Fig 2. Photomicrograph ofBM aspirates showingmetastasis of adeno-carcinoma in a hypocellularbackground. (Leishman’sstain, X400)
From the records of peripheral bloodexamination, all the patients were found to beanaemic with hemoglobin ranging from 5.6 to9.0 g %. Thrombocytopenia was recorded in11 (50%) cases while leucopenia was presentin 2 (9.09%) cases. Leucoerythroblastic picturewas documented in 9 (40.9%) cases.BM smears in 18 cases (81.81%) werehypocellular, 3 cases (13.64%) normocellularand one case (4.55%) was hypercellular. In 4cases of neuroblastomas, BM aspirations weredone as a part of staging. Diagnosis of adeno-carcinomas was made in 8 cases on the basis ofglandular pattern, presence of signet ring cell andmucin detected by PAS. In the remaining cases,the cell clusters were undifferentiated malignantcells and it was not possible to identify theirtissue of origin from marrow aspirate.
Table 2. Primary sites of bone marrow metastasis
Sl. Primary Sites No. of Cases Percen-No. (Total = 22) tage (%)
1. Neuroblastoma 4 18.182. Breast 3 13.633. GIT 3 13.634. Lungs 2 9.095. Prostate 2 9.096. Others (undifferentiated) 8 36.36
Age No. of cases.(22) %
< 10 4 18.18
11-20 0 0
21-30 1 4.54
31-40 2 9.09
41-50 2 9.09
51-60 5 22.73
Above 60 8 36.36
Table 1. Age distribution

JMS * Vol 22* No. 1 * January, 2008 19
References1. Sharma S, Murari M. Bone marrow involvement by
metastatic Solid tumours. Indian J Pathol Microbiol.Jul 2003; 46 (3):382-84.
2. Mohanty SK, Dash S. Bone marrow metastasis inSolid tumours. Indian J Pathol Microbiol. Oct 2003;46 (4):613-16.
3. Anner RM, Drewinko B. Frequency and Significanceof Bone marrow involvement by Solid metastatictumours. Cancer 1977; 39:1337-44.
4. Singh G, Krause JR, Breitfeld V. Bone marrowexamination for metastatic tumour. Cancer 1977;40:2317-32.
5. Finkelstein JZ, Ekert H, Isaacs H, Higgins G. Bone
ORIGINAL ARTICLE
FNAC slides from primary sites were availablein 14 cases. In 8 cases primary could not beascertained as either results of roentge-nographic studies were negative or patientswere lost to follow-up.
DiscussionBM aspirations are now employed in theinvestigation of many disorders in haematology,oncology and internal medicine.7 Detection ofmetastatic tumours in BM is of great importancefor the clinical staging of tumour spread becauseit influences the response to treatment and theoverall survival.1 Patients with metastatic tumourcells in BM usually have a normochromic,normocytic anaemia and less commonly,thrombocytopenia or neutropenia. In less thanhalf the patients with bone marrow metastasis,the blood films contain some erythroblast andneutrophil precursors (leukoerythroblasticanaemia).8 In our study, leucoerythroblasticpicture was seen in 40.9% cases similar to thestudy conducted by Sharma S et al 1 where theleucoerythroblastic picture was seen in 50%cases. In adults, the tumors that most commonlymetastasize to marrow are carcinomas ofprostate, breast, lung, thyroid and kidney. Inchildren they are neuroblastoma,rhabdomyosarcoma, Ewing's sarcoma andretinoblastoma.
In a study conducted by Sharma S et al1,neuroblastoma (12%) and breast tumors (12%)
predominated. These results are comparableto our study where neuroblastoma (18.18%)predominated among all the metastatic solidtumours in BM, followed by breast andgastrointestinal tract tumours (13.63%) each.Mohanty SK et al2 in their study of 73 casesreported neuroblastoma in 27 (36.98%) casesfollowed by 22 (30.13%) cases of cacinomaprostate and 13 (17.81%) cases of breastcancer. In our study, carcinoma prostate wasfound in 2 cases (9.09%).
Often, it is not possible to identify the primarytumour on the basis of the morphologic featuresof metastatic cells in marrow smears.Information on the nature of malignant cellsmay be obtained by immunocytochemistry andimmunohistochemistry which are available inselected centres only.
ConclusionBM aspiration is an important part of routineinvestigation of cancer patients. It may identifymetastasis where radiography and bone scanshave failed. It is effective, practical andeconomical in detecting solid tumoursmetastasis to BM in selected group of patientsand rightly considered mandatory for stagingof solid malignant tumours.
marrow metastasis in Children with Solid tumours.Am J Dis Child. 1970; 119:49-52.
6. Hansen HH, Muggia FH, Selawry OS. Bone marrowexamination in 100 consecutive patients withbronchogenic carcinoma. Lancet 1971; 2:443-45.
7. Sar R, Aydogdu I, Ozen S, Sevinc A, BuyukberberS. Metastatic bone marrow tumour: a report of sixcases and review of literature. Haematologica(Budap). 2001; 31(3):215-23.
8. Smitha NW, Jeffrey MC. Blood and Bone marrowpathology. In: S.N.W and BJ Bain, editors. Pathologyof marrow: general considerations.1st ed.Philadelphia: Churchill Livingston; 2003.p.112.

JMS * Vol 22 * No. 1 * January, 200820
CME
Laparoscopy is a surgical technique wherebyorgans, vessels and other structures of theabdomen and pelvis are visualized anddissected by developing a small video cameraand surgical instruments through trocarsinserted through small skin incisions in theabdominal wall.
Gynecologists pioneered its widespread usefor surgery of pelvic organs in the 1970s. Mostrecently, general surgeons have takenlaparoscopy for many surgeries (about 11% ofall operations). The first laparoscopiccholecystectomy (LC) was performed byPhillipe Mauret in France in 1987.
Anaesthesiologists caring for patientsundergoing laparoscopic surgeries should beknowledgeable of the specific benifit oflaparoscopy, recognized the unique physiologicchanges caused by insufflation and anticipatethe special hazards (e.g. visceral injuries, bloodloss, capnothorax) associated with this surgicaltechnique.
Physiologic changes : The importantphysiological changes in several organsystems during laparoscopic surgery arebrought about by patient position, insufflatinggas and body's response to increased intra-abdominal pressure (IAP) following
Anaesthesia in laparoscopic surgery
1L. Deban Singh, 2GS Moirangthem
pneumoperitoneum for successful per-formance of the surgery.
Patient position
The changes associated with positioning maybe influenced by the extent of the tilt, patient'sage, intravascular volume status, associateddisease, anesthetic drugs administered andventilation techniques. Patients are usuallypositioned in head down or head up positions.
a) Head down position (Trendelenburg,100- 200)
This position is commonly requested duringinsertion of Verees needle and trocar insertionand in lower abdominal surgery e.g. gynecologicand GIT surgery like abdominal hysterectomy,appendicectomy and herniorhaphy.
i) Haemodynamic changes : There is anincrease in venous return (VR), right atrialpressure (RAP), central blood volume andcardiac output (CO). In contrast, other reportsindicate that MAP and CO usually remainsunchanged or decrease, although theTrendelenburg position increases preload.These seemingly paradoxical responses maybe explained by carotid and aorticbaroreceptor-mediated reflexes. CVPincreases by an average 8 mmHg at IAP of 15mmHg in the supine position. It increases byan additional 6mmHg at similar IAP in theTrendelenburg position.
ii) Respiratory changes: Head down tilt causesa cephalad shift in abdominal viscera anddiaphragm. Functional residual capacity (FRC),
1. Associate Professor of Anaesthesiology, 2. Professor& Head of Surgical Gastroentrology and Minimal AccessSurgery Unit, Department of Surgery, Regional Instituteof Medical Sciences(RIMS), Imphal.
Corresponding author :Dr. L. Deban Singh, Dept. of Anaesthesiology, RIMS,Imphal-795004. e-mail : [email protected]

JMS * Vol 22* No. 1 * January, 2008 21
total lung volume(TLV), pulmonary compliance,VC and diaphragmatic excursion are decreasedthus predisposing to atelectasis. There is anincrease in the likehood of hypoxaemia inpatients with obese and pre-existing lungdisease.
Right mainstem bronchus intubation withinadvertent single-lung ventilation and itsassociated complications like hypercarbia,hypoxemia and bronchial contriction arepossible.1 There is a tendency for the tracheato shift upward so that a tracheal tube anchoredat the mouth may migrate into the rightmainstem bronchus and hypoxemia due tocephalad displacement of the diaphragm andcarina during insufflation of the abdomen.
iii) Other changes: Nerve compression, brachialplexus injury and elevation of ICP and IOP havebeen reported.
b) Head up tilt (Reversed Trendelenburg,rT,200-300)
For upper abdominal surgeries, afterinsufflation the patient's position is usuallychanged to a steep head up position to allowthe viscera to settle down by gravity away fromthe operative site and facilitate surgicaldissection.
i) Haemodynamic changes : The prolongedhead up position in upper abdominal surgeriesresults in decrease in venous return(VR) dueto pooling of blood in lower extremities resultingin reduction in RAP,PCWP, and fall in MAP andCO, and preload, exaggerated by compressionof IVC during pneumoperitoneum. Thesechanges may be deleterious effects in patientswith coronary artery insufficiency.
A steep head up causes venous stasis in thelegs predisposing to deep venousthrombosis and pulmonary thromboembolicmanifestation postoperatively.
ii) Respiratory changes: The changes are theopposite of head down position. FRCincreases and the work of breathingdecreases.
Insufflating gas
The ideal gas for abdominal insufflation would
be physiologically inert, nonflammable,inexpensive, easily acquired, relativelyabsorbable by abdominal tissue and solublein blood so that it allows pulmonary excretionand thereby minimizes potentially life-threatening effects if embolized into the venousvasculature.2 At the initial stages laparoscopistsused only air and met with complications likeair embolism, physiological trespasses likepneumothorax, pneumomediastinum, surgicalemphysema. Various gases like nitrogen(air),O2, N2O, CO2, helium, argon, etc have beentried. Still the ideal agent is yet to bediscovered.
Zollikofer from Switzerland first used CO2insufflation in 1924. CO2 is the insufflating gasof choice because of its high solubility in bloodwith low risk of venous embolism, non-inflammability (safety during electrocautery andlaser surgery), its capability of pulmonaryexcretion, low cost, relatively inert, rapidlybuffered by HCO3 in blood and readilyavailability despite having the risk of producinghypercarbia due to its rapid absorption byabdominal viscera and tissue.
Body's response to increased intraabdominal pressure (IAP) followingpneumoperitoneumPneumoperitoneum is created and maintainedby insufflating gas(Initial flow, 1-1.5L/min, thenhigher flow rate, 2 - 3L/min) through Veressneedle into the peritoneal cavity. A "Hasson"minilaparotomy technique has also beenadvocated for pneumoperitoneum creation toavoid injuries associated with blind Veressneedle and trocar insertion. Once thepneumoperitoneum is established, the gas flowrate is reduced to maintain IAP usually at 10-15mmHg (range 5-20mmHg). About 4L of thetotal gas volume (range 3-5L) is required toachieve IAP of 8-12mmHg. This is necessaryto create the space to visualize the surgicalarea through the laparoscope. The overallpressure on the diaphragm amounts to a forceof approximately 50 kg in the trendelenbergposition. When gas is insufflated into theperitoneal cavity, there are two immediateeffects: IAP is raised to a level depending onthe gas volume and cavity compliance andsecondly gaseous interchange occurs acrossthe peritoneum. Pneumoperitoneum may be
CME

JMS * Vol 22 * No. 1 * January, 200822
avoided by using special surgical retracters orsubcutenous wiring to lift the abdominal wallalthough exposure is inferior to that achievedwith pneumoperitoneum. Cardiovascular, respi-ratory and renal changes are common and varyin degree of severity based on the length andcomplexity of surgery, patient's age and his orher cardiopulmonary status.
1. CVS changesThe mechanism by which laparoscopy causescardiovascular effects is not clearly delineatedbut may depend partly from two main factors:neurohumoral response following increasedIAP, and hypercarbia and the subsequentacidosis.
Neurohumoral response : Neurohumoralresponse increases vasopressin partly from1.5 ± 0.5 to 12.3 ± 47 pmol/L3 and latercatecholamines following increased IAP.Vasopressin (Anti-diurectic hormone, ADH)causes the mascular layer of arterioles (i.e.Tunica media vasorum) to contract. The risein vasopressin tended to parallel temporallyincreases in systemic vascular resistance(SVR) and blood pressure whereas elevatedconcentrations of catecholamines occourredlater in the surgery. IV clonidine given beforeinsufflation significantly attenuate some ofthese hemodynamic changes. However, renin-angiotensin-aldosterone system is alsoinvolved. The most important mechanism ofthe neurohumoral response of the vasopressinand rennin-angiotensin-aldosterone system isthe sympathetic stress response4 includingvagal reflexes. The increased IAP also leadsto a mechanical impairment of the VR leadingto an increase in venous pressure of the lowerextremity while decreasing the cardiac preload.Depending on the extent of above mentionedmechanisms there will be an increase in SVRand pulmonary vascular resistance resultingin an increased afterload. The development ofhemodynamic changes depends on thefunctional reserve of the heart. There may bea decrease in cardiac output and hypotensionwithout an increase in the heart rate.
Other factors includes the positioning of thepatient, preoperative cardiorespiratory status,intravascular volume and anesthetic agentsemployed.
Reflex increase in vagal tone due tooverstretching of the peritoneum may producebradycardia and even asystole and death,aggravated by lighter plane of anesthesia,patient on ß-blocker, stimulation of trachealtube during biplolar electro-cauterization andCO2 embolization. In 0.5% of healthy patients,however, bradycardia and asystole can occurduring CO2 insufflation and pneumo-peritoneum. Although the exact mechanism forthis response and why only certain patientsexperience bradycardia remains topics ofcontinued research, it is believed that directpressure on the vagus nerve causes astimulatory parasympathetic effect that leadsto a drop in heart rate. Hypercarbia can alsoexacerbate arrhythmias. The thresholdpressure that produces minimal effects onhaemodynamic function is 12mmHg.Hypercarbia and Acidosis : CO2 is highlysoluble and therefore is very rapidly absorbedfrom the peritoneal cavity and retroperitonealspace into circulation. Because absorbed CO2can only be excreted through the lungs,hypercarbia can only be avoided by acompensatory hyperventilation by increasingthe tidal volume of ventilation in anesthetizedpatients. Hypercarbia can develop as a resultof a highly increased peritoneal absorption ofCO2 and an insufficiently increased exhaustionof CO2. Absorption of CO2 is increasedparticularly during prolonged surgery usinghigh intra-abdominal pressure. Exhaustion ofCO2 is reduced in patients with compromisedcardiopulmonary function and restricted CO2clearance.5 Also, the compensatoryhyperventilation is impeded by theTrendelenburg position or a high intra-abdominal pressure, which cause a cephaladdisplacement of the diaphragm (resulting inreduction of lung volumes) and a restriction indiaphragmatic mobility. In these conditions,severe hypercarbia can develop despiteaggressive hyperventilation. It should bestressed that intra-abdominal pressure has amajor role in the development of hypercarbiasince it both increases the absorption anddecreases the exhaustion of CO2.
Hypercarbia and acidosis can causehemodynamic changes by direct action on thecardiovascular system and by an indirect action
CME

JMS * Vol 22* No. 1 * January, 2008 23
through sympathoadrenal stimulation.4,5 Thedirect effect of carbon dioxide and acidosis canlead to decreased cardiac contractility,sensibilization of myocardium to thearrhythmogenic effects of catecholamines andsystemic vasodilatation. The centrallymediated, autonomic effects of hypercarbialead to a widespread sympathetic stimulationresulting in tachycardia, hypertesion andvasoconstriction counteracting the directvasodilatatory effect. Attempting to compensateby increasing the TV/RR will increase themean thoracic pressure, further hindering VRand increasing mean pulmonary arterypressure. These effects can prove particularlychallenging in patients with restrictive lungdisease, impaired cardiac function orintravascular volume depletion.
Clinical studies of hemodynamic changes:A biphasic change in CO is produced (COelevated initially,then decreased). Upto10mmHg of IAP, the cardiac filling pressuresare unchanged or elevated and CO improves.Most of these studies reported increased SVRand pulmonary vascular resistance andreduction of cardiac index (CI) whenlaparoscopy was performed at about 15 mmHg and head up tilt 10°. Joris et al6 usinginvasive monitoring, observed a significantincrease in mean arterial pressure (MAP)(35%) after peritoneal insufflations, along withan increase of SVR (65%) and pulmonaryvascular resistance (90%), and a decrease inCI (20%), while the PCWP and CVP increased.The decrease in CI can be partly explained byan increase in SVR. CI can be reduced by 35-40% after induction of anesthesia and rTpositioning, and further reduced to 50% of itspreoperative value 5min after the beginning ofCO2 insufflation. The CI gradually improved10min of CO2 insufflation. This biphasic changein hemodynamic has been supported by manystudies whereas some investigatorscommented an unchanged CI during CO2insufflation. The mechanism by which biphasicchanges in CO has been explained as a) itforces blood out of the abdominal organs(splanchnic venous bed) and IVC into thecentral venous reservoir thereby increasedcentral BV and hence CO, b) with furtherincreased in IAP, there is peripheral pooling of
blood in the lower extremities and pelvic region,thereby tends to decrease the VR and CO.However, higher insufflation pressure(>18mmHg) tends to collapse the majorabdominal vessels (particularly IVC) whichdecreases VR and leads to a drop in preloadand CO in some patients. TransesophagealEchocardiography (TEE) has shown that thereis marked decrease in left ventricular enddiastolic. These hemodynamic changes arewell tolerated by healthy individuals but mayhave deleterious consequences in patientswith cardiovascular disease. TheTrendelenburg position attenuated thisincrease while rT position aggravates it.
Using lower insufflation pressures, CVSchanges were milder and transient. Threeminutes after the onset of pneumoperitoneumat the pressure of 8-12 mm Hg, Branche et al7observed a 25.7% increase in MAP, a 49%increase in left ventricular end-systolic wallstress (a measure of left ventricular afterload)and a 17% decrease in fractional areashortening (a measure of left ventricularfunction-contractility). All measured variablesreturned to preinsufflation values after 30 minof pneumoperitoneum and thereafter were nolonger significantly affected by posturalchanges (10° head-up position) or pneumo-peritoneum exsuflation.
Minimal to no changes in cardiac conductionare usually caused by pneumoperitoneum ifhalothane is avoided for maintenance ofanesthesia. Halothane is associated withventricular arrhythmogenesis if administeredin the presence of hypercarbia,not aninfrequent event during CO2 insufflation.Although rare, traction on peritoneal tissue canenhance efferent vagal traffic to the sinus nodeand slow or abolish spontenous rhythm. Littledata are available regarding the effects ofpneumoperitoneum on other indices of cardiacconduction such as dromotropism andrepolarization.
2. Respiratory changes
The increased IAP following pneumo-peritoneum leads to cephalad displacement ofthe diaphragm which results in reduced lung
CME

JMS * Vol 22 * No. 1 * January, 200824
volumes (TV, FRC, FEV1,VC,TLV), andthoraco-pulmonary compliance (35-40%),increased peak airway pressure and risk ofbarotraumas during IPPV, and an inadvertentright mainstem bronchial intubation particularlyin Trendelenburg position. This decreasedcompliance leads to an increased in the workof breathing. There is chances of opening ofembryonal channels between the peritonealcavity and the pleural and pericardial sacswhich may cause pneumothorax, pneumo-mediastium and pneumopericardium. Thecephalic shift results in early closure of smallairways leading to intraoperative atelectasiswith a decrease in FRC. Uneven distributionof ventilation to non-dependent parts of thelungs (increases in less ventilated alveoli)produces ventilation perfusion mismatch,elevated dead space, intrapulmonary shunting,hypoxia, hypercarbia and atelectasispredispose to PO chest infections. This ismanifested by widening of the alveolar-arterialpartial pressure of O2 difference (A-aDO2).PaCO2/PEtCO2 increases about 15% to 25%usually reflected to capnography. Increased inminute volume (10-25%) is required to maintaina constant PEtCO2 concentration and preventoccurrence of a respiratory acidosis (pH-7.30)that would otherwise occur. Disproportionateincreased of PaCO2/ PEtCO2 (>25%) needsfurther search for various causes likecardiorespiratory compromise, subcutaneousemphysema, endobronchial intubation,pneumothorax and pulmonary embolism.
Depending upon absorption of CO2 fromperitoneal surface, retroperitoneal space,impairment of pulmonary ventilation, abdominaldistension and patient position, an IAP of 15mmHg raises the PaCO2 by 10mmHg ( PEtCO2-10mmHg), the PACO2 by 4mmHg anddecreased lung compliance by 25%. Duringcarboperitoneum, both PEtCO2 and PaCO2increases progressively (time dependent) toreach a plateau 15-20 min (range 10-30 min)after the insufflation (similar to the phasiccardiac response). This occurs both in headup and head down positions in patients withcontrolled ventilation, the correction of theincreased CO2 and respiratory acidosis canbe made by increasing minute ventilation (10-25%) (increasing RR and / or TV 12-15mL/kg)
in order to prevent progressive alveolaratelectasis and hypoxemia and to allow CO2elimination but will inevitably lead to someincreased in airway. Both PEtCO2 andpulmonary CO2 elimination continued toincrease slowly throughout CO2 insufflation.Although ventilation with PEEP significantlyimproves pulmonary gas exchange andpreserves arterial oxygenation duringprolonged pneumoperitoneum, PEEP in thepresence of elevated IAP increases theintrathoracic pressure (ITP) and producesmarked reduction in CO. A modern ventilationtechnique is the 'alveolar recruitment strategy',consisting of manual ventilation to an airwaypressure of 40 cm H2O for 10 breaths over 1min, followed by usual mechanical ventilationwith mild PEEP (5cm H2O) to improves arterialoxygenation intraoperatively duringlaparoscopy, without clinical cardiovascularcompromise or respiratory complications.8
Since up to 120 liters of CO2 can be stored inthe human body during pneumoperitoneum, aprolonged mechanical ventilation is neededpostoperatively in some cases until CO2 iseliminated completely. If the ventilation is notcontrolled, these changes are primarilymitigated by a more frequent RR but PEtCO2concentrations still rise. However, in ASA GradeIII or IV patients, PaCO2 may remain elevated(about 3-fold more than that determined in ASAI patient) despite adjusting minute ventilationto normalize PEtCO2. Preoperative evaluationwith pulmonary function tests demonstratingFEV less than 70% of predicted values, lowVC, high risk ASA and diffusion defects lessthan 80% of predicted values can identifypatients at risk of developing hypercarbia andrespiratory acidosis following pneumo-peritoneum. Significant variations of meangradients of arterial - PEtCO2 is seen in patientswith COPD, morbid obesity and congenitalcardiac disease.
In patients with interstitial pulmonary diseaseor COPD, poor CO2 diffusion and eliminationmay lead to significant and catastrophicincreases of PCO2. PEtCO2 measurements areunreliable and tend to underestimate the truePCO2 in this population because of impairedgas exchange. Periodic arterial blood gas
CME

JMS * Vol 22* No. 1 * January, 2008 25
(ABG) measurements should be obtained andin the event that CO2 can not be quicklyeliminated, pneumoperitoneum or pneumo-retroperitoneum should be relievedimmediately. Once PCO2 has fallen into theacceptable range, CO2 insufflation can beresumed and the laparoscopic procedurecontinued.
3. Embolism
The chance of thromboembolism is more inpatients undergoing long laparoscopicprocedures in the rT position. At least twofactors in Virchows triad are affected (venousstasis and hypercogulability) during increasein IAP. Doppler studies showed decrease infemoral blood flow with increase IAP and thereis no adaptation during prolonged surgery. AtIAP >14mmHg, rT position, obesity, pelvicsurgery and prolonged surgery reduce venousblood flow in the lower extremities therebyincreasing chances of thromboembolism.
4. Renal and splanchnic blood flow
A pneumoperitoneum induces importantchanges in the physiology of the kidneys. Themost common result is oliguria. The maincauses of oliguria during laparoscopy are :i) Direct mechanical compression of renal
arteries, veins and parenchyma.9ii) The vicious cycle of reduced renal perfu-
sion activation of renin-angiotensinaldosterone system renal corticalvasoconstriction10
iii) Increased ADH(Vasopressin)10,11
iv) Elevation of endothelinv) Reduced CO.12
With desufflation, these mediators return tobaseline levels, and a post-desufflation diuresisis generally noted in the following hours. Renalhomeostasis is re-established within 24 hoursafter surgery with normalization of serum andurinary creatinine and electrolytes.
Renal and hepatic blood flow may beinfluenced by IAP (physical pressure ofpneumoperitoneum), humoral mediators suchas renin, hypercarbia and patient position. AnIAP of >20 mmHg reduces renal andmesenteric blood flow. There is an overallreduction of blood supply to all the organsexcept the adrenal glands. The RBF and GFR
decrease because of an increase in renalvascular resistance, reduced glomerularfiltration gradient and reduced CO. The renaleffects are mild to negligible when the IAP isless than 10 mm Hg. Head-up position andIAP from 12 to 15mmHg compromised hepaticand renal blood flow in animal study. Thefunctional consequence of the diminishedblood flow(cortical renal flow decreases by28%, medullar renal flow decreases by 31%,13
GFR decreases to 18-31% of normal values14)to kidneys resulted in a urinary output of only0.01±0.03ml/kg/h (63% to 64%),compared with0.85±0.4ml/kg/h in patients undergoinglaparoscopic surgery using CO2 pneumo-peritoneum or an abdominal wall retractor,respectively. There is also reduction ofcreatinine clearance and sodium excretion.This is a functional (prerenal) acute renalfailure, which is generally reversible after 2 hpostoperatively.9 The greater concern is toavoid over-resuscitation, fluid overload,pulmonary edema, and exacerbation ofcongestive heart failure. Prolonged renalhypoperfusion carries the risk for acute tubularnecrosis and its consequences. One must keepin mind the possibility of renal, hepatic andintestinal failure after laparoscopic procedures.Some prophylactic actions are available andcan easily be taken before acute tubularnecrosis occurs.
Methods for maintaining renal perfusion :i) Intravascular volume loading should bedone before and during pneumoperitoneum.In an effort to maintain renal perfusion andminimize possible deleterious effects on graftfunction, some investigators have suggestedthe use of isotonic and hypertonic intravascularvolume expansion for transplant cases. Analternative to volume expansion is to decreaseIAP as much as visualization will allow.ii) Low dose dopamine 2 µg/kg/min can preventrenal dysfunction usually associated with long-lasting laparoscopic procedures and higherpressures of pneumoperitoneum (~15 mmHg).15
iii) Urine output is significantly higher wheninsufflation of gas at body temperature is usedas compared with room temperature CO2insufflation. Warm insufflation probably causesa local renal vasodilation and may be beneficial
CME

JMS * Vol 22 * No. 1 * January, 200826
to patients with borderline renal function.16
iv) Esmolol inhibits the release of reninand blunts the pressor response to inductionand maintenance of pneumoperitoneum.Therefore, it may protect the kidneys againstrenal ischemia during laparoscopy.17
v) Non-steroidal anti-inflammatory drugs(NSAIDs), widely used for pain management,can cause renal medullary vasoconstrictionthat may induce acute tubular necrosis if addedto the previous vasoconstriction caused bypneumo-peritoneum.18 Therefore, NSAIDs,both the 'older' ones and the new selectiveCOX-2 inhibitors (selective inhibitors of cyclo-oxygenase-2 enzyme) should be avoidedpreoperatively in patients with impaired renalfunction or renal diseases.
High risk of regurgitation and aspiration(acid)of gastric contents has been reported duringlaparoscopic procedures. Several factors thatpredispose to regurgitation are steep headdown tilt, IAP during insufflation ofintraperitoneal gas and mechnical pressureexerted on the abdomen by the surgical team.However, risk of gastric regurgitation from IAPduring insufflation is usually minimized due toincreased lower esophageal sphincter tone.
Studies in rats have shown a decrease insplanchnic macro- and micro-circulationdepending on the amount of intra-abdominalpressure.19 An increase of 5 mm Hg, from 10to 15 mm Hg of the intra-abdominal pressureresulted in a blood flow decrease to thestomach (40-54%), jejunum(32%), colon(44%),liver(39%), and peritoneum (60%).20 The fallin blood flow to these organs may be due torelease of hormones (catecholamines,angiotensin and vasopressin), mechanicalcompression on abdominal organs and rTposition.
Few studies showed increased levels ofaminotransferase (alanine aminotransferase,aspartate aminotransferase) and also ofalcohol dehydrogenase and glutathioneS-transferase but the phenomenon is transientas these enzymes returned to normal valueswithin 1-3 days.21 These changes are clinicallysilent in patients with a normal liver function.Even in selected patients of Child-Pughclasses A and B with compensated cirrhosis
some laparoscopic procedures ( chole-cystectomy, appendectomy, splenectomy )seem to be safe, in any case safer than the'open' procedures.22
5. TemperatureThere is a 0.3C fall in core temperature forevery 50L flow of CO2 due to the continuousflow of dry gases over the peritoneal surfacesunder pressure because of the JouleThompson effect (sudden expansion of gas),higher flow rate and leakage through the ports.If the gas used is dried, the heat expenditureto humidify the dry gas is much more than justwarming dry CO2. Insufflation of gas at bodytemperature is recommended.6. Hormonal effectsLaparoscopy elicits a classic stress responsebut a lessor degree as evidenced by theincreased in the concentrations of plasmaACTH, cortisol, epinephrine, norepinephrine,glucagons, insulin, dopamine and renin.7. CNSLaparoscopy causes increase in ICP. Twomechanisms have been suggested to accountfor this rise in ICP: i) impaired venous return oflumbar venous plexus and head caused byincrease in IAP, ITP and Trendelenburg posi-tioning and ii) increase intracranial flow due toelevated PaCO2 after abdominal insufflation.Safety of laparoscopy in patient with pre-existing elevated ICP has been reported.However, more detailed human studies arerequired.8. IOP
Increase in IAP compresses IVC and increaseslumbar spinal pressure by reducing drainagefrom the lumbar plexus,then increases IOP.
9. Pediatric patientIn pediatric patient PEtCO2 rises more rapidlyand achieves plateau values sooner in younger(11-24 months of age) versus older (5-14 yr ofage) children during CO2 insufflation.23 Tobiasand coauthers24 noted small change in PEtCO2(32±3 to 35±5 mmHg) and peak inflatingpressure (20±3 to 23±3 cm H2O) afterinsufflation during brief laparoscopic inspection(15min) of the peritoneum. Changes in BP,HR, RR and TV are not always consistent but
CME

JMS * Vol 22* No. 1 * January, 2008 27
appear to be at least qualitatively similar tothose in adult patients. In another study, PEtCO2concentration overestimate PaCO2 in longerlaparoscopic procedures.Insufflation of CO2 is limited to a pressure of 8-15 mm Hg (average 10mmHg) in children tominimise diaphragmatic splinting. Gaslesslaparoscopy is achievable by lifting theabdominal wall with special retractors orsubcutaneous wiring.With increases in IAP, the diaphragm is pushedrelatively more cephalad in children, therebydecreasing FRC. Diaphragm mobilitydecreases significantly as does overallrespiratory efficiency. Both respiratory rate andpeak airway pressures will increase, and therespiratory changes appear to be moresignificant with intraperitoneal thanextraperitoneal insufflation.25 From a metabolicstandpoint, CO2 absorption is much moreefficient in children due to a relatively greaterabsorptive surface-to-weight ratio.26 To preventhypercarbia, minute ventilation should beincreased, with close monitoring of PEtCO2 andarterial oxygenation in longer cases.Urologic laparoscopy in the pediatricpopulation is generally well tolerated. From acardiac perspective, a similar IAP-dependentphysiologic response can be anticipated. WhenIAP is maintained at 10 to 12 mm Hg or less,clinically significant hemodynamic compromiseis generally not observed; although increasesin SVR (162%) and decreases in cardiacperformance (67%) have been reported atpressures of 10 mm Hg. As with adults,bradycardia and asystole can occur during gasinsufflation from vagal nerve stimulation.26
Children typically have a higher resting vagaltone. Therefore, it is advisable to minimize IAPif visibility allows because lower IAP isassociated with fewer cardiac effects andinitiating pneumoperitoneum at a lowerinsufflation rate may be warranted.Low complication rate (1-2%) of laparoscopicsurgery in children has been reported.Complications are more or less same as inadults.
Anaesthetic considerationsCareful pre-operative assessment is requiredfocusing on cardiac and respiratory reserve,
liver and renal function because these organsmay be affected by the increase IAP. Medicalillness such as diabetes, hypertension, asthma,and hypothyroiddism need to be optimallycontrolled before surgery.In patients with pulmonary and cardiac disease,specialty consultation is generally necessary.The cardiac and pulmonary, liver and renalfunction should be carefully evaluated andoptimized so that the best preoperativecondition is achieved and the operative risk isacceptable. Concomitant use of cardiotoxic,hepatotoxic and nephrotoxic drugs should beavoided.Although reported safety of laparoscopy in someneurosurgical procedures in patients with pre-existing elevated ICP, there is still the possibilityof laparoscopy causing increase in ICP.Patients with distorted abdominal anatomy(e.g.obesity, prior abdominal surgery withadhesions) are at higher risk for vessel ororgan damage or puncture during insertion ofVeress needle or larger trocar that encasesthe video camera. The experience and the skillof the surgeons must be counted.Conversion to laparotomy is always apossibility and must be taken into accountduring pre-anaesthtic assessment.Laboratory investigation of a patient should bebased on the evaluation of the patient (historyand physical examination). Electrolyte andcreatinine analysis, coagulation studies,chemistry panels including LFT, ECG, andchest radiographic films are advised. A bloodsample should be sent to the blood bank forcross-match. For procedures in which bloodloss is not anticipated, a type and screen issufficient. Autologous blood use should beencouraged if the patient is in good generalhealth.Prophylactic antibiotics should be givenspecially patients with valvular heart disease,a history of endocarditis, a vascular graft, orimplanted devices.PremedicationPremedication needs meticulous preparationkeeping in mind the onset and duration ofaction of drugs since many laparoscopicprocedures are now conducted on day carebasis.
CME

JMS * Vol 22 * No. 1 * January, 200828
Preoperative visits are clearly helpful toalleviating anxiety. In addition to psychologicalpreparation, patients also benefit frompremedication. A short acting anxiolytic,benzodiazepine like midazolam allays anxietyand ensures a rapid recovery.An antiemetic like ondansetron (4-8mg IV),granisetron (40µg/kg BW IV), dexamethasone(8mgIV) reduces postoperative nausea andvomiting (PONV). A gastrokinetic such asmetoclo-pramide (10mg IV,1-3min prior toinduction of anesthesia) hastens gastricemptying and increased lower esophagealtone. An H2 antagonist (ranitidine 50mg IV 1-2h before induction of anesthesia) reduces thevolume and raised pH of gastric secretions.Premedication with oral omeprazole, 40mg atnight and in the morning also appears to behighly effective in patients with laparoscopicsurgeries. Anticholinergic like glycolpyrrolate0.1-0.2mg IM 1h prior to induction helps toreduce airway secretion. Pre-emptic analgesia(multimodal analgesic) is achieved withparenteral NSAIDS and opiods. Deep veinthrombosis (DVT) prophylaxis may berecommended.MonitoringMinimum mandatory monitoring like HR, ECG,NIBP, pulse-oximetry (SPO2), continuouscapnography/capnometry (PEtCO2) andtemperature probe should be used. PEtCO2 ismost commonly used as a noninvasivesubstitute for PaCO2 in the evaluation of theadequacy of ventilation during LC. Whenpneumoperitoneum occurs, the PaCO2increases and may require an increasedminute ventilation (12-16%) to maintain normalPaCO2 close to preinduction levels. However,PEtCO2 may not be a satisfactory noninvasiveindex of PaCO2 if it exceeded 41 mmHg and iflarge volumes of CO2 insufflated. But PEtCO2proved to be a reasonable approximation ofPaCO2 in those patients free from cardio-pulmonary disease. In contrast, patients withpreoperative cardio-pulmonary disease maydemonstrate significant increases in PaCO2 notreflected by similar increases in PEtCO2 duringinsufflation. PaCO2 may be underestimated byPEtCO2 if there is a reduction in CO or anincreased in V/Q mismatch, and occasionallyPEtCO2 may overestimate PaCO2. In patients
with cardiopulmonary disease, it would seemprudent to monitor PaCO2 levels at times duringthe procedure to avoid problems withhypercarbia and acidosis.Patients with reduced cardiaorespiratoryreserve (ASA grade III / IV) will require invasivehemodynamic techniques such as arterial line,BP, TEE, periodic ABG measurement, PCWP,CVP and estimation of perfusion via centralvenous oxygenation in order to monitor thecardiovascular response to insufflation andinstitute therapy. Because the CO is inverselyproportional to the insufflation pressure in theabdomen, gradual insufflation should bemonitored by the anesthesiologists and a limitof 8-12 mmHg set as maximal inflationarypressure. Limiting the rT tilt may attenuatethe reduction in CO during peumoperitoneum.Significant hemodynamic compromise,refractory persistent hypercarbia, acidosis,and/or a reduction in SvO2 may necessitateexsufflation of the pneumoperitoneum orlowering of the insufflation pressure orconversion to open procedure. CO can bemonitored with pulmonary artery catheters orthe less invasive technique such esophagealDoppler.Anaesthetic techniqueDepending on the duration and type ofsurgeries, laparoscopic procedures can beperformed under general, regional (epidural orspinal anesthesia or combined spinal-epidural,CSE) or local anesthesia (infiltration of localanesthetic with IV sedative).General anaesthesia:General anesthesia (IV induction followed bymuscle relaxant, cuff endotracheal intubationand controlled ventilation - gold standardtechnique) is usually perferred because ofpatient discomfort associated with creation ofthe pneumoperitoneum and the extent ofposition changes associated with theprocedure. During pneumoperitoneum,controlled ventilation must be adjusted tomaintain PEtCO2 at approximately 35mmHg byincreasing minute ventilation by 10-25%.Tracheal intubation with positive pressureventilation under GA is usually favored formany reasons 1) it protect airway and preventthe risk of regurgitation and acid aspiration
CME

JMS * Vol 22* No. 1 * January, 2008 29
from increase IAP during insufflation. Althoughoperations like laparoscopic gastrostomy,jejunostomy, herniorrhaphy, gynecological andpelvic surgeries and other minimal procedureshave been performed using local or RAcombined with IV sedative, chances ofaspiration of gastric contents is very high withthese patients than GA 2) Increase in IAP andTrendelenburg positioning hindersspontaneous breathing and may compromiserespiratory exchange. There lies the necessityfor controlled ventilation at high TV which areused to prevent hypercarbia and to reduceatelectasis including depression of ventilationby anesthetic agents, absorption of CO2 fromthe peritoneal cavity and mechanicalimpairment of ventilation by pneumo-peritoneum and the initial steep Trendelenburgposition. The obese patient would also benefitfrom intubation to decrease the likehood ofhypoxemia, hypercarbia and aspiration. PEEPmay be applied to reduce basal atelectasis.Airway pressure should be carefully monitoredand vigilance for pneumothorax maintained.The relatively high peak inspiratory pressurerequired because of the pneumoperitoneum 3)the need for neuromuscular blockade(muscular relaxation and immobile operativefields) during surgery to allow lower insufflationpressure provide better visualization and aidssurgeons to performed a rapid safe procedurewithout coughing, retching and unexpectedpatient movement 4) CO2 insufflates the entireabdomen including the inferior aspect of thediaphragm and may cause significantdiscomfort or pain as the phrenic nervesoriginate from the nerve roots of 3rd,4th and5th cervical vertebrae, diaphragmatic pain isdifficult to treat with local or RA. Likewise,anesthesia for manipulation of abdominalorgans and peritoneal traction may be difficultto achieve using local or RA. 5) skill andefficiency of the surgeon may be necessary tocomplete a laparoscopic procedure in thetimely manner necessary for patientsexperiencing laparoscopy under LA or RA.6) the placement of an orogastric or nasogastrictube and urinary catheters to empty thestomach or bladder is an additional discomfortthat may be avoided by GA and minimize therisk of visceral perforation during trocarintroduction and optimizise visualization.
Preloading with crystalloid solution is recom-mended to prevent the haemodynamicchanges during pneumoperitoneum. Atropinemay be administered at induction to preventbradycardia.Any modern IV or volatile anesthetics (such aspropofol, isoflurane, sevoflurane anddesflurane) may be used to maintainanesthesia, with the exceptions of halothaneand N2O. Practically, balanced anesthetictechnique with O2, N2O, volatile anestheticagents, relaxants, NSAIDs and opiods (e.g.tramadol, butorphanol, fentanyl, remi-fentanil,sufentanil etc.) is still applied. Inhalationalanesthetics like isoflurane, sevoflurane anddesflurane show least sensitivity to arrhythmiasin the presence of increased catecholaminesdue to hypercarbia and maintain hemodynamicstability throughout the perioperative period,ensure rapid recovery with minimal PONV andtherefore may be suitable agents to use duringCO2 insufflation. These agents are favouredfor patients with compromised cardiac function.Because the CO2 may increase duringlaparoscopy especially if the patient breathesspontaneously, cardiac arrhythmias may occurif halothane used. However, in our experiencelow concentration of halothane and controlledventilation, the incidence is less. If ventilationis controlled, laparoscopy does not precludeuse of halothane. Currently, spontaneousrespiration is only recommended for shortlaparoscopic procedures. Propofol infusion isalso an excellent choice for general anestheticin the presence of raised catecholaminesduring insufflation. So, it can be used analternative to volatile anesthetics. But propofolshould perhaps be avoided when anesthetizingwomen for pronunuclear-stage transfer ofembryos because this anesthetic results in alower ongoing pregnancy rate (29%) whencompared with isoflurane use (54%). N20 hasbeen blamed to contribute to PONV and boweldistention, intra-abdominal fire (N2O act as anoxidizing agent to fuel sources) and mayexpand any CO2 emboli into the venousvasculature. N2O may be replaced bysevoflurane and desflurane which are havingblood gas solubility constant similar to N2O andare useful alternative agents. The omission ofN2O reduced the risk of PONV by 28%.However, there is no conclusive evidence
CME

JMS * Vol 22 * No. 1 * January, 200830
demonstrating a clinically significant effect ofN2O on surgical conditions during LC or onthe incidence of PO emesis. Therefore, N2Omay still be a useful adjuvant during GA forthis procedure. Its omission in laparoscopicsurgery might also increase awareness duringsurgery. The advent of parenteral perioperativeNAIDs and the tendency for less PO painassociated with the laparoscopic approachmay obviate perioperative narcoticadministeration.Following induction of anesthesia the urinarybladder is decompressed and a nasogastrictube inserted to empty the stomach therebyreduces trauma to intra-abdominal contentsat the time of trocar insertion and may improvelaparoscopic visualization and facilitatesretraction of right upper quadrants.Patient positioning should be done graduallyto avoid haemodynamic changes. The positionof the endotracheal tube (ETT) should bechecked after any change in position and afterinsufflation to prevent displacement of ETT intomainstem bronchus with subsequentinadvertent single-lung ventilation. To lessenthe possiblility of mainstem bronchial intubation,the depth of endotracheal intubation may bereduced by 1.5cm, the approximate cephaladdisplacement of the carina duringpneumoperitoneum.Use of LMA during laparoscopic surgeriesremains controversial for two reasons. a)Aspiration of gastric contents has beenobserved during control ventilation. Becausethe LMA does not partition the trachea fromthe esophagus as cuff ETT does, gastriccontents may be more likely to be aspirated.Moreover, peritoneal insufflation andTrendelenburg positioning may compress thestomach and thereby cause gastric contentsto be expelled in the esophagus, with migrationinto the trachea. However, the possibility oftracheal aspiration is mitigated by placementin the Trendelenburg position that allowsdependent drainage of gastric contents andb) If spontenous ventilation is required, theLMA limits the maximum positive pressure tothat pressure created by the seal in theposterior pharynx, about 20mmHg. Given thedisplacement of the diaphragm caused by theIAP, 8 to 12mmHg, positive pressure ventilation
may be compromised. Report of safe use ofLMA in laparoscopic surgeries has beenidentified except less than 0.14% of patientsuffered airway regurgitation, vomiting andaspiration of gastric contents. So, use of anLMA may not be precluded by abdominalinsufflation in the absence of othercontraindication to LMA insertion.The pressure points should be padded withcare to prevent nerve compression injuries.Post-operative pain reliefi. Local anesthetics infiltration of the port sites andlocal anesthetics applied directly to the operative site.ii. Pain can be quickly controlled by a systemicmultimodal approach (opiods for central painmodulation, and wound infiltration with LA andNSAIDs to attenuate peripheral pain). Shouldertip pain is reduced by setting the patient upearly in recovery. Intraperitoneal (IP)administration of LA (10ml of 0.5% bupivacaine)has been reported to reduce PO shoulder painafter minor or gynecologic laparoscopicprocedures. Experiences with IP localanesthetic administration after LC have rangedfrom significant reduction in PO pain duringthe first 48h with 10ml of 0.5% bupivacaine27
to no effect in reducing PO pain, improvinglung function or attenuating metabolicendocrine responses with 20ml of 0.25%bupivacaine28.RecoveryHaemodynamic monitoring should becontinued into the PO period. Decreased PaO2and increased O2 demand observed afterlaparoscopy necessitates O2 administrationpostoperatively, even to healthy patients.Local anaesthesiaLaparoscopy under local anesthesia(LA) withIV sedation has been reported to be successful.Although PO recovery is rapid, increased inthe patients discomfort, diaphragmatic pain, therisk of aspiration of gastric contents anddifficulty in breathing due to CO2 insufflation,and difficulty in manipulation and suboptimalvisualization of abdominal organs andperitoneal traction, preclude the use of thislocal anesthesia technique for LC. Success withlocal anesthesia requires a relaxed and co-operative patient, and an experienced surgeon.IAP should be as low as possible to reduce
CME

JMS * Vol 22* No. 1 * January, 2008 31
pain and ventilatory disturbances. Thetechnique is largely limited to briefgynecological procedures (e.g. laparoscopictubal sterilization) in young, healthy andmotivated patients.
Regional anaesthesiaSpinal and epidural or CSE techniquespresents another alternative for laparacopicsurgeries. The same disadvantages thatassociate with LA may also be faced in regionalanesthesia (RA). Laparoscopy under RA is bestsuited for lower abdominal procedures.However, procedures in the upper abdomenhave been managed effectively. A high level(Sensory block upto T4-T5) is necessary forupper abdominal surgical laparoscopy forcomplete muscle. General anesthesia wouldtherefore be the preferred technique for thispatient.
In general, local or regional anesthetictechniques have not been advocated for LCor other upper abdominal laparoscopicprocedures.
Complications
Complications of laparoscopic surgeries candevelop depending on IAP, the amount of CO2absorption, the circulatory volume of thepatient, the ventilation technique used, theunderlying pathologic conditions and the typeof anesthesia. Anesthesiologists caring forpatients in intra-operative period and PACUshould maintain high degree of suspicion forinadvertent unrecognized injuries/complications with these laparoscopicprocedures. Therefore, adequate monitoringand correct management are important toprevent the development of complications.
Incidence of laparoscopy complications:a) Overall complication rate : 4.0 to 5.7 per
1000 laparoscopic procedures.b) Complication rate according to type of
surgery:i. 12.6 per 1000 cases in operative cases,
ii.0.6 per 1000 cases in diagnosticlaparoscopy
c) Death rate : 0.1 to 1 per 1000 cases(approximately)
1. Hemorrhage:
Lacerated injuries of major vessels (e.g. aorta,epigastric, iliac, hypogastric, mesentericvessels, portal vien and other vessels) maybe unrecognized because of limitation oflaparoscopic visualization and is usually dueto the veress needle or trocars insertion,subsequent use of scissors, probes,electrocautery, ultrasonically activated(ultracision, harmonic) scalpel and lasers.Other causes of hypotention and shock (e.g.pneumothorax, gas embolism, rT position,anesthetic overdose etc.) during laparoscopymust be considered.
Management :i. Require early recognization and
management,ii. Usually presented as unexplained
profound hypotension unresponsive tofluid and mild vasopressor therapy (e.g.ephedrine) is especially concerning duringlaparoscopy and may be an indication fortermination of the procedure or conversionto laparotomy and repair of vessels ifrequired.
iii. Use of open technique (Hassonmini-laparotomy) with a blunt needle toreduce the incidence of perforation,
iv. To restore vascular volume withfluids,blood and blood product andestablishment of additional IV lines, andto decrease depth of anesthesia.
2. Hypotension (upto 13% of laparoscopies)Hypotention is due to IV anesthetics likethiopentone, propofol, inhalational anestheticslike halothane, isoflurane, sevoflurane,decrease volume status of the patient, suddeninflation of abdomen (> 20mmHg) with CO2compressing IVC, high ITP during IPPV/PEEP,vagal response, injuries to major vessels,venous embolism and hypercarbia which mayinduce dysrhythmias. 12.9% of patientundergoing LC developed intra-operativehypotension.
Treatment:i. Preoperative fluid loading (10ml/kg),
vasopressor therapy and vagolytic agents.ii. Gradual induction with IV anesthetics and
CME

JMS * Vol 22 * No. 1 * January, 200832
supplementation of inhalationalanesthetics.
iii. Slow insufflation and low IAP should beused as far as possible. Some procedurescan be done at 5-7 mm Hg, but the requiredabdominal distension varies with surgicalprocedure, anatomical conditions andmyorelaxation. The recommendation is toapply the lowest possible pressure levelfor each particular case.
iv. Intermittent pneumatic compressionincreases VR and cardiac preload.
v. Extreme position should be avoidedsince it may have an influence both oncardiac and ventilation.
vi. Explore and repair the injuries vessels asrequired and treatment of gas embolism.
3. Hypertension:The risk of hemorrhagic stroke, pulmonaryedema and cardiac decompensation is highfollowing hypertensive episodes. Because ofthe pharmacological interventions, incidenceof hypertensive episodes is rare. But itsincidence seems to be higher at the beginningof insufflations, when the increasing (but stillbelow 10 mm Hg) IAP increases the VR byreducing the BV in the splanchnic vasculature.This increased preload augments CO andarterial pressure. The situation commonlyoccurs in patients having sufficientintravascular volume loading, i.e. ~10 ml/kgprior to CO2 insufflation, a loading which isnowadays standard for the prevention ofhypotension.Causes are due to light plane of anesthesiaand CO2 insufflation and hypercabia. Othercauses of hypertension must be explored.Treatment :a) To increase depth of anesthesia with
propofol, inhalational agents, opiods-tramadol, butorphanol, fentanyl,remifentanil etc,
b) Antihypertensive agents like calciumchannel blocker, ß- blocker like esmololand vasodilator like nitroglycerine arealso selectively used.
c) Slow insufflation with low IAP as far aspossible and correction of hypercarbia.
4. Arrhythmias(14-27% of laparoscopies):
Cardiac arrhythmias may occur duringlaparoscopy with CO2.
i) Bradyarrhythmias (sinus bradycardia, nodalrhythm, atrio-ventricular dissociation andasystole) :
The causes are due to increased vagus-mediated cardiovascular reflex by rapid andexcessive stretching of the peritoneum at thebeginning of peritoneal insufflation, duringtrocar insertion, or manipulation of the viscera,aggravated by lighter plane of anesthesia,patient on ß-blocker, stimulation of trachealtube during biplolar electrocauterization andCO2 embolization. Cardiac arrest (2-20 of1,00,000 laparoscopies) could be araised.Among the causes of cardiac arrest, profoundvasovagal response to rapid peritonealdistension and gas embolism are particularlyassociated with laparoscopy.
ii) Tachyarrythmias (Sinus tachycardia andventricular extrasystoles) are also possible.There should be a distinction between sinustachycardia and ventricular extrasystoles whichare due to the release of catecholaminesfollowing CO2 insufflation (respiratory acidosisand increased sympathetic outflow) andhypercarbia specially in the presence ofhalogenated anesthetic agents.
Treatment:i. Usually transient and spontaneously
resolve with the reduction of IAP.ii. 100% O2 hyperventilation.iii. Elimination of stimulation(e.g. slow
insuflation if possible defflation ofperitoneum, avoidance of halothane inpresence of hypercarbia).
iv. Pharmalogical therapy of arrhythmias(e.g.use of vagolytic drug like atropine, ß-blocker - esmolol) should be available.
v. To deepen plane of anesthesia, keep CO2in the normal range, correct hypoxia as itmay contribute the occurrence ofarrhythmias and treat CO2 embolization.
5. Injuries:Injuries to bile duct, stomach, liver, spleenuterus, urinary bladder, bowel burns and bowelgas explosions, and vessels are associatedduring insertion of needle and trocars.
CME

JMS * Vol 22* No. 1 * January, 2008 33
Fulguration (thermal) and also peritonitis arepossible if a viscus is perforated during trocarintroduction.Diagnosis of injury to stomach and bowel :a) Visualization of mucosal lining after the
insertion of laparoscopic,b) Increase IAP at the beginning of
pneumoperitoneum,c) Asymtomatic distention of peritoneal
cavity,d) Aspiration of gastric particulate matter
through the lumen of the needle,e) Feculent odour if trocar enters into
the large bowel,f) Occur usually in patients with previous
abdominal surgeries,Decompression of the urinary bladder and oral/nasogastric tube insertion before surgery mayreduce injuries to intra-abdominal organs. Useof "Hasson" minilaparotomy technique hasalso been advised for pneumoperitoneumcreation to avoid injuries associated with blindVeress needle and trocar insertion.6. Pulmonary dysfunction (persist for at least24 h PO) :FRC, FEV1, TLC, PEFR and VC are reducedby approximately 25%(30-38%) following LCas opposed to a 50% reduction following opencholecytectomy. Diaphragmatic dysfunctionafter laparoscopic cholecystectomy may berelated to diaphragmatic tension during thepneumoperitoneum through somatic afferentsarising from the abdominal wall which exert aninhibitory action on phrenic nerve dischargeor visceral afferents originating in GB area orresidual pnemoperitoneum. Laparoscopicsurgery may reduce PO pulmonarycomplications by avoiding the restrictivepattern of breathing that usually follows upperabdominal surgery.Pulmonary complications are represented byhypoxemia, barotraumas, pulmonary edemaand atelectasis.Only patients with compromised cardio-pulmonary function such emphysema, COPDand cardiac disease are at risk for thedevelopment of hypoxemia. If appropriateventilation and oxygen administration are notable to reverse hypoxemia, conversion to opensurgery may be required. Most of the patientswith normal cardiopulmonary function will
surpass these pathophysiological changeswithout developing hypoxemia or severehypercapnia. Elevated airway pressures anddecreased compliance could be associatedwith pulmonary barotrauma, which may occuras an immediate pneumothorax. Although thereis chance of impairment of pulmonary functionand gas exchange during laparoscopy, therecovery of pulmonary function is more rapidand the rate of pulmonary sequelae(atelectasis) or complications (pneumonia) islower than after open surgical procedures,irrespective to the magnitude of the proceduresor age of the patient.
7. Mainstem bronchial intubation:This can be prevented if position of the ETT ischecked regularly after CO2 insufflation andevery change of patient's position.8.Subcutaneous emphysema (sc) (0.3-3.0%laparoscopic procedures):Usually, the gas passes through any disruptionof the peritoneum into the sc tissue and intothe retroperitoneal tissue. Rarely, it is theconsequence of inadvertent placement oftrocars and direct insufflation into the sc tissue.Further extension of sc emphysema may occuron larger areas (extremities, neck) and evento the mediastinum and pleura thereby causingpneumomediastinum and pneumothorax. Thereverse situation is also possible, i.e. theextension of a pneumomediastinum into the sctissue. If there is an involvement of the neck itis also important to monitor the upper airwayfor obstruction. As the sc emphysemaconstitutes an important reservoir of CO2 intothe body, it leads to an increase in end-tidalCO2 concentrations and therefore increasedventilation is required.
Diagnosis :i) Crepitus in the abdominal wall and other
parts of the body if generalised.ii) Abrupt increase in EtCO2
iii) Upper airway for obstruction if there isinvolment of the neck.
Treatment :a) Spontaneuos resolution possible,b) Discontinuance of N2O administration,
increase in ventilation, continuation ofmechanical positive pressure ventilationin the immediate PO period and ABGanalysis.
CME

JMS * Vol 22 * No. 1 * January, 200834
9. Capnothorax (pneumothorax, pneumome-diastinum and pneumopericardium) :Pneumothorax could be developed from pleuraltears during laparoscopic surgical proceduresat the level of the gastroesophageal junction(Fundoplication,15%), adrenalectomy andaccidental diaphragmmatic injuries. Otherpossible routes for gas to enter the thoraciccavity during pneumoperitoneum via anycongenital diaphragmatic defects (e.g. foramenof Morgagni or foramen of Bochdalek) aroundthe esophageal and aortic hiatus and via anyprocedure that can damage the falciformligament (e.g. during insertion of a Veressneedle), opening of embryonic channelsbetween the peritoneal cavity and the pleuraland pericardial sacs, rupture of pre-existingcongenital pulmonary bullae as a result ofincrease alveolar inflation from increase minuteventilation, as a result of CO2 dissecting andspreading through retroperitoneum or by theextension of a sc emphysema up to pleura,resulting in pneumothorax and pneumo-mediastinum (e.g. after laparoscopic extraperi-toneal inguinal hernia repair).Diagnosis :i. Increase EtCO2,ii. Oxygen desaturation,increased airway
pressure and reduced air entry, andshould be confirmed by radiography,
iii. Decrease thoracopulmonary compliance,iv. Abdominal movement of one
hemidiaphragm on laparoscopic view.Treatment :i. Avoid thoracentesis unless necessary as
spontenous resolution occurs within30-60 min after insufflation.
ii. Discontinuance of N2O administration,decrease in insufflation pressure and IAPand continuation of mechanical ventila-tion (PEEP if necessary) and adjustmentof its setting.
iii. Pneumomeidastineum and pneumo-pericardium are manisfested as the abovepicture mostly. Usually desufflation ofabdomen is adequate to relieve suchcomplications.
10. Venous CO2 embolism (0.0014-0.6% oflaparoscopies) :Embolism occurs from unintentionalinsufflations of gas into an open vein/tear in a
vessel in the abdominal wall or peritoneumduring introduction of the pneumoperitoneumneedle, subsequently trocar placement or laterduring sharp dissection or electrocautery,ultra-sonically activated (ultracision,harmonic) scalpel or lasers at the operativesite and presence of pressure gradient to drivethe gas from the intra-abdominal cavity intothe venous vasculature.CO2 > 1 L/min may enter the vessels beforesignificant embolism.Emboli may lodge in the right atrium/ventricleto form a gas lock which may impair VR andobstruct right ventricular outflow resulting insudden CV collapse.Emboli may also enter pulmonary circulationresulting in hypoxemia, acute pulmonaryhypertension, pulmonary edema and rightheart failure and CV collapse and death.60% of symptomatic cases occur during initialinsufflation.Diagnosis :i. Transient increase EtCO2 in early stage
and decrease later due to moredecreases pulmonary dead space andcardiovascular collapse.
ii. Increase pulmonary artery pressure,profound hypotension, dyspnea, hypoxia(cynosis), Mill wheel murmur onauscultation, arrhythmias or asystole anddeath.
iii. TEE is an extremely sensitive monitor todetect material embolized into the rightheart and can identify all CO2, even thosewith volumes as small as 0.1mL/kg. 68%of asymptomatic patients have CO2bubbling in the right chamber of the heartduring laparoscopic cholecystectomy.
iv. Doppler techniques are the most sensitiveindicators of embolic phenomena.Transcranial Doppler experiments haveshown that CO2 bubbles may even reachthe cerebral circulation.
Treatment:i. Immediate cessation of CO2 insufflations,
defflation of pneumoperitonium anddiscontinuation of N2O.
ii. Patient turned to left lateral decubitus withhead down position (Durant's
CME

JMS * Vol 22* No. 1 * January, 2008 35
position) to allow the gas to rise into theapex of the right ventricle and prevent intothe pulmonary. The Trendelenburgposition is also sufficient as it has thesame effect.
iii. Hyperventilation of patient andadministration of 100% O2 helps rapidCO2 elimination. Use of PEEP to preventparadoxical emboli remains controversialfor gas emboli.
iv. Removal of air through central venouscatheter, aggressive cardiopulmonaryresuscitation, administration of IV fluidsand catecholamine, management ofarrhythmias, hyperbaric O2 therapy andcardiopulmonary bypass.
Use of Hasson technique is recommendedinstead of the Veress needle becauseincidence of gas embolism is less with Hassontechnique (0%) than the Veress needletechnique (0.001%).29
11. Hypercarbia :Causes of hypercarbia are incresased IAP andTrendelenburg position. Other causes ofhypercarbia must be sought.Treatment :
Hyperventilating the patient bycomparatively less TV to preventpulmonary barotraumas and greaterventilatory frequencies, and use of lowerinsufflation pressure as far as possible.
12. Positioning of patients :Nerve injuries are usually due to inappropriatepositioning of the patient or pressure exertedby surgical teams, hyperabduction of shoulderjoint (brachial plexus injury) and duringlithotomy position (perineal, femoral andexternal cutaneous nerves injuries). Usuallyspontanous recovery but preventable ifhyperabduction is avoided at the shoulder jointand placement of arms by the side of thepatient in adducted position.
13. Retention of foreign bodies due to limitedvisualization.14. PONV :PONV is common (53-70% in LC). Prophylacticantiemetics like 5-HT3-antagonist (ondasetron,4-8mgIV, granisetron, 40µg/kg BW IV),dexamethasone (8mgIV), metochopramide(10mg IM/ IV), H2-blocker (ranitidine, 50mgIV)
and acupressure are recommended.Combination of 5-HT3 antagonist anddexamethasone is quite effective.15. PO pain including shoulder tip pain:Shoulder tip pain is common in laparoscopicsurgeries. Diaphragmatic peritoneal irritationproduces pain which is referred to the shouldervia phrenic nerve. The pain is due toconversion of CO2 to carbonic acid in bodyfluids including intrapleural which is irritant tothe peritoneum and subdiaphargmatic gaseousaccumulation.Treatment :i. Removal of all gases at the end of surgery,ii. LA instillation in the subdiaphargmatic
space, application of multimodal analgesiausing NSAIDs and opiods analgesic andLA infiltration in the port sites.
iii. Sitting the patient up early in recovery.16. Deep vien thrombosis :Venous stasis in the lower limbs(40%reduction of femoral venous blood flow) andmicroendothelial injury are due to vasodilata-tion and platelet hyperaggregability (Virchow’striad) are involved during pneumoperitoneum,aggravated by reverse Trendelenburg position.Treatment :Low molecular weight heparin, sequentialcompression in the intraoperative period andearly ambulation are also advocated.17. Infections : Laparoscopy increases risk ofspread of infection and should be treated withantibiotics.18.Spread of malignancy : Tumourimplantation at the port site is possible.19. Incisional hernia : Preventable if meticuloussuturing and care the surgical wound aretaken.ConclusionLaparoscopic surgical techniques have beenrapidly accepted by surgeons worldwide butpresents new challenges to theanesthesiologists. A thorough knowledge of thephysiological changes and the advantagesof keeping IAP less than 12 mm Hg and thespecial hazards and complications likehemorrhage, injuries to organs, CO2 embolism,capnothorax associated with the laparoscopictechniques and vigilant monitoring particularlyserial arterial blood gases and correctmanagement are the backbone for anuneventful and complete success.
CME

JMS * Vol 22 * No. 1 * January, 200836
References1. Lobato EB, Paige GB, Brown MM, et al. Pneumo-
peritoneum as a risk factor for endobronchialintubation during laparoscopic gynecologic surgery.Anesth Analg. 1998 ; 86 : 301.
2. Rudston-Brown B, Draper PN, Warriner B, et al.Venous gas embolism a comparison of CO2and helium in pigs. Can J Anaesth. 1997; 44 : 1102.
3. Walder AD, Aitkenhead AR. Role of vasopressin inthe haemodynamic response to laparoscopiccholecystectomy. Br J Anaesth. 1997 ; 78 : 264.
4. Neudecker J, Sauerland S, Neugebauer E,Bergamaschi R, Bonjer HJ, Cuschieri A, et al. TheEAES clinical practice guidelines onpneumoperitoneum for laparoscopic surgery. SurgEndosc 2002 ; 16 : 1121-1143.
5. Hsieh CH. Laparoscopic cholecystectomy forpatients with chronic obstructive pulmonary disease.Laparoendosc Adv Surg Tech [A] 2003 ; 13 : 5-9.
6. Joris JL, Chiche JD, Canivet JL, et al.Haemodynamic changes induced by laparoscopicand their endocrine correlates :effects of clonidine. J. Am Coll Cardiol. 1998 ; 32 :1389.
7. Branche PE, Duperret SL, Sagnard PE, Boulez JL,Petit PL, Viale JP. Left ventricular loadingmodifications induced by pneumoperitoneum: Atime course echocardiographic study. AnesthAnalg 1998 ; 86 : 482-487.
8. Pang CK, Yap J, Chen PP. The effect of analveolar recruitment strategy on oxygenation duringlaparoscopic cholecystectomy. Anaesth IntensCare 2003 ; 31 : 176-180.
9. Chiu AW, Chang LS, Birkett DH,Babayan RK. Theimpact of pneumoperitoneum, pneumo-retroperitoneum, and gasless laparoscopy on thesystemic and renal haemomo dynamics. J. AmColl Surg 1995 ; 181 : 397-406.
10. Dolgor B, Kitano S, Yoshida T, Bandoh T,Ninomiya K, Matsumoto T. Vasopressin antagonistimproves renal function in a rat model ofpneumoperitoneum. J Surg Res 1998 ; 79 : 109-114.
11. Hazebroek EJ, de Vos tot Nederveen Cappel R,Gommers D, van Gelder T, Weimar W, SteyerbergEW, et al. Antidiuretic hormone release duringlaparoscopic donor nephrectomy. Arch Surg 2002;137 : 600-604.
12. Are C, Kutka M, Talamini M, Hardacre J, Mendoza-Sagaon M, Hanley E, et al. Effect of laparoscopicantireflux surgery upon renal blood flow. Am J Surg2002 ; 183 : 419-423.
13. McDougall EM, Bennett HF, Monk TG, Siegel CL, LiD, McFarland EG, et al. Functional MR imaging ofthe porcine kidney: Physiologic changes ofprolonged pneumoperitoneum. JSLS1997;1:29-35.
14. Cisek LJ, Gobet RM, Peters CA.Pneumoperitoneum produces reversible renaldysfunction in animals with normal and chronicallyreduced renal function. J Endourol 1998;12: 95-100.
15. Perez J, Taura P, Rueda J, Balust J, Anglada T,Beltran J, et al. Role of dopamine in renaldysfunction during laparoscopic surgery. SurgEndosc 2002 ; 16 : 1297-1301.
CME16. Backlund M, Kellokumpu I, Scheinin T, Von Smitten
K, Tikkanen I, Lindgren L. Effect of temperature ofinsufflated CO2 during and after prolongedlaparoscopic surgery. Surg Endosc 1998;12:1126-1130.
17. Coloma M, Chiu JW, White PF, Armbruster SC. Theuse of esmolol as an alternative to remifentanilduring desflurane anesthesia for fast-trackoutpatient gynecologic laparoscopic surgery.Anesth. Analg. 2001 ; 92 : 352-357.
18. LeLorier J, Bombardier C, Burgess E, Moist L, WrightN, Cartier P,et al. Practical considerations for the useof nonsteroidal anti-inflammatory drugs and cyclo-oxygenase-2 inhibitors in hypertension and kidneydisease. Can J Cardiol 2002;18:1301-1308.
19. Yokoyama Y, Alterman DM, Sarmadi AH, Baveja R,Zhang JX, Huynh T, et al. Hepatic vascular responseto elevated intraperitoneal pressure in the rat. J SurgRes 2002 ; 105 : 86-94.
20. Schilling MK, Redaelli C, Krahenbuhl L, Signer C,Buchler MW. Splanchnic microcirculatory changesduring CO2 laparoscopy. J Am Coll Surg 1997 ;184 : 378-382.
21. Kotake Y, Takeda J, Matsumoto M, Tagawa M,Kikuchi H. Subclinical hepatic dysfunction inlaparoscopic cholecystectomy and laparoscopiccolectomy. Br J Anaesth 2001 ; 87 : 774-777.
22. Tuech JJ, Pessaux P, Regenet N, Rouge C,Bergamaschi R, Arnaud JP. LaparoscopicCholecystectomy in cirrhotic patients. SurgLaparosc Endosc Percutan Tech 2002;12 :227-231.
23. Hsing CH, Hseu SS, Tsai SK, et al. Thephysiological effect of CO2 pneumoperitoneumin pediatric laparoscopy. Acta Anaesthesiol Sin.1995; 33 : 1.
24. Tobias JD, m Holcomb GW, Rasmuggen GE, etal. General anaesthesia using the laryngeal maskairway during brief, laparoscopic inspection of theperitoneum in children. J Laparoendosc Surg.1996 ; 6 : 175.
25. Halachmi S, El-Ghoneimi A, Bissonnette B, et al.Hemodynamic and respiratory effect of pediatricurological laparoscopic surgery: a retrospectivestudy. J Urol. 2003 ; 170(4 pt2) : 1651-1654.
26. Pennant JH. Anesthesia for laparoscopy in thepediatric patient. Anesthesiol Clin North Am. 2001 ;19(1) : 69-88.
27. Weber A, Munoz J, Garteiz D,et al. Use ofsubdiaphragmatic bupivacaine instillation of controlpostoperative pain after laparoscopic surgery. SurgLaparosc Endosc 1997 ; 7 : 6-8.
28. Rademader BMP,Kalkaman CJ, Odoom J,et al.Intraperitoneal lacal anaesthetics after laparoscopiccholecystectomy : effects on postoperative pain,metabolic responses and lung function. Br.J Anaesth1994 ; 72 : 263-6.
29. Bonjer HJ, Hazebroek EJ, Kazemier G, Giuffrida MC,Meijer WS, Lange JF. Open versus closedestablishment of pneumoperitoneum inlaparoscopic surgery. Br J Surg 1997;84 : 599-602.

JMS * Vol 22* No. 1 * January, 2008 37
A 59 year old female, known case ofhypertension since 12 years was admitted incoronary care unit of PGIMER, Chandigarhwith history of increasing shortness of breathtwo days prior to admission. She also hadhistory of restlessness associated with cold andcalmy skin since the morning of admission.There was history of cerebrovascular accident10 days back with a large left parietal infarcton CT head (Fig 1). On examination, she wasrestless, tachypnoic (RR=40/min), pulse of 106/min, BP of 70/60 mmHg on dopamine andnoradrenaline support.Chest was clear andcardiovascular examination revealed normalS1 & S2 with no murmur. On neurologicalexamination, shewas conscious,oriented with righthemi paresis and upgoing right plantar.Her right lower limbwas swollen andtender with clinicalevidence of deepvein thrombosis.
On investigation, ECG showed sinus
Low dose intrapulmonary artery rt-PA thrombolysis in a patient with massiveacute pulmonary thromboembolism with history of recent cerebrovascularaccident: a case report1Dhanaraj Singh Chongtham, 2S. Reddy
tachycardia, normal axis with 1mm STsagging in lead V1 to V6 with CPK-MB of 27iu/L. Echocardiography revealed dilated RA/RV,paradoxical IVS motion, mild TR (RVSP=RAP+ 28mmHg) with small LV cavity andgood contractility(EF=50%). CompressionUSG both lower limb showed right femoro-popliteal deep vein thrombosis. An emergencyCT angio chest showed saddle thrombusextending into both pulmonary arteries(Fig 2).
1. Assistant Professor of Medicine, Regional Institute ofMedical Sciences (RIMS), Imphal. Formerly Senior Resi-dent, Cardiology, Postgraduate Institute of Medical andResearch (PGIMER), Chandigarh, 2. SeniorResident cardiology, Department of cardiology, PGIMER,Chandigarh.
Corresponding author :Dr. Dhanaraj Singh ChongthamAssistant Professor of Medicine, RIMS, ImphalE-mail: dhanaraj_chongtham @ yahoo.com
CASE REPORT
Fig 2. CT pulmonary angiography showing thrombus in leftpulmonary artery.
Patient was initially supported with IV fluid,double ionotropes, oxygen inhalation,antiplatelet and LMWH (Enoxaparin) therapy.Her condition deteriorated in spite of thetreatment with falling PaO2, arterial oxygensaturation and increasing tachypnoea. Shewas put on mechanical ventilator with CMVmode under sedation .
In view of the intractable hypotension in spiteof the optimum dose of double ionotropicagents with type 1 respiratory failure needingventillatory support, decision for low doseintra-arterial rtPA thrombolysis was taken withthe idea that it may reduce the chances of IC
Fig 1 .NCCT head showing largeleft parietal infarction of the brain.

JMS * Vol 22 * No. 1 * January, 200838
broken up with 6F pigtail catheter by manualmanipulation (Fig 3). A local in situintrapulmonary artery 4 mg bolus rtPA wasgiven followed by infusion of 46 mg in 45 min.It was followed by subcutaneous Enoxaparintherapy as her partial thromboplastin time after2h of lysis was 46sec. A repeatEchocardiogram study next day showedimprovement in RV contractility and reductionin RV size. Patient’s hemodynamicparameters gradually improved andionotropes were tapered off by day 3. Patienthad small GI bleed of about 150 ml on dayone, which was treated with iv proton pumpinhibitor (pantoprazole). No further recurrenceof GI bleed was noted afterwards. There wasno subsequent deterioration of theneurological status of the patient. She wasgradually weaned off ventilator by day 5. Arepeat CT head showed no evidence of ICbleed. She was planned for maintaining onoral anticoagulant treatment with warfarin witha target INR of 2 to 3. A decision for puttingIVC filter was also taken to prevent furtherrecurrence of pulmonary embolism fromdislodged right lower limb DVT and was putbefore the patient was discharged from thehospital.
DiscussionThrombolysis in acute pulmonary embolism isan approved modality of treatment in patientswith features of RV dysfunction or hypotensionwith a window period of two weeks from theonset of symptoms.1 It results in more rapidclot dissolution than treatment with heparinalone. Thrombolytic therapy appears to reduce
mortality in patients with shock due to massivePE, probably by rapidly restoring pulmonaryblood flow and improving RV function. It alsoenhances the resolution of small peripheralemboli and reduces recurrence of PE.
FDA approved thrombolytic regimens for PEincludes2 : 1) Streptokinase: 250,000 IU as aloading dose over 30 min, followed by 100,000iu/h for 24h – approval in 1977. 2) Urokinase:4,400 iu/kg as a loading dose over 10 min,followed by 4,400 iu/kg/h for 12 to 24h –approval in 1978. 3) rt-PA: 100mg as acontinuous peripheral intravenous infusionover 2h – approval in 1990.
In an international multicenter randomized trial3,it was found that a smaller bolus of rt-PA 0.6mg/kg/15 min(maximum of 50mg) is safer thana larger dose administered over 2h. Localthrombolytic therapy has several potentialadvantages over systemic administration. Firstby delivering the drug directly into thepulmonary artery, local therapy might beaccompanied by more rapid and or morecomplete clot lysis. Second, because of highlocal drug concentration, low dose mightachieve the same degree of thrombolysis ashigher systemic doses. Finally, local therapymight be accompanied by a lower risk ofbleeding, especially if lower doses are used.
A randomized control trial compared peripheralintravenous and local pulmonary artery infusionof rtPA in patients with angiographicallydocumented PE.4 Both routes of administrationcaused similar rate of lysis, bleeding andinduction of a systemic lytic state. It is the onlycontroled study comparing between these twomodes of administration.
Local pharmacological thrombolysis using lowdoses of urokinase or rt-PA and either high-pressure intraembolic infusion or mechanicalclot disruption has been investigated. In onereport6, six patients with contraindication tosystemic thrombolysis received low-doseintraembolic thrombolysis using specialcatheter in a nonrandomized study, systemicfibrinolysis and bleeding did not occur, and allpatients were found to have at least a 20%angiography improvement by 1h and 50 to 90%
CASE REPORT
Fig 3. 6 F Pigtail catheter inpulmonary artery causingcatheter fragmentation ofPulmonary thrombus followedby intrapulmonary arteryadministration of rtPA.
bleed in this patientwho had recent CVAwith large leftparietal infarct. Shewas taken up in thec a r d i a cc a t h e t e r i z a t i o nlaboratory and ap u l m o n a r yangiogram donethere showed totalcut off of mainpulmonary artery.Thrombus in MPAwas mechanically

JMS * Vol 22* No. 1 * January, 2008 39
CASE REPORT
improvement by 24h6.
Various methods of catheter embolectomy andmechanical fragmentation of thrombus havebeen described.5 These catheterizationmethods include mechanical fragmentation ofthrombus with a standard pulmonary arterycatheter, clot pulverization with a rotatingbasket catheter, percutaneous rheolyticthrombectomy and pigtail rotational catheterembolectomy.
The present index case was taken up in thecatheterization laboratory and mechanicalfragmentation of thrombus was done with 6Fpigtail catheter under manual manipulation.
In view of the associated large left parietalinfarct with higher chances for subsequent ICbleed, low dose (50mg) intrapulmonary artery
thrombolysis was given. She respondedclinically by improvement in hemodynamicparameters with complete withdrawal ofionotropes by day 2. Repeat echocardiographystudy 24h later also showed improvement inRV function.
Recent history of cerebrovascular accident withparietal infarct is a relative contraindication forthrombolysis in patients with acute PE.However, in patients with massive PEpresenting in shock with respiratory failure, therisk of IC bleed with thrombolysis is to bebalanced against the worse outcome asexpected without thrombolysis. This casereport described such a high-risk patient whowas successfully treated with low dose intra-arterial rt-PA and manual fragmentation of thethrombus with pigtail catheter.
References1. Konstantinides S, Geibel A, Heusel G, et al.
Heparin plus alteplase compared with heparinalone in patients with sub massive pulmonaryembolism. N Eng J Med. 2002 ; 347 : 1143.
2. Goldhaber S Z, Contemporary pulmonary EmbolismThrombolysis. Chest 1995; 107 : 45S-51S.
3. Goldhaber S Z, Agnelli G, et al. Reduced Dose bo-lus Alteplase Vs conventional Alteplase infusion forpulmonary Embolism thrombolysis. An InternationalMulticenter Randomized Trial Chest 1994 ; 106 :718-24.
4. Verstraete M, Miller G A H, et al. Intravenousand intrapulmonary recombinant tissue-typeplasminogen activator in the treatment of acutemassive pulmonary embolism. Circulation 1988;77: 353-60.
5. Zites DP, Libby P, Bonow RO Braunwald E.Braunwald’s Heart Disease, 7th editon. Philadelphia,Pennsylvania : Elsevier Saunders ; 2005 .p. 1789-1806.
6. Tapson VF, Davidson CJ, Bauman, et al. Rapidthrombolysis of massive pulmonary emboliwithout systemic fibrinolysis: intraimbolic infusionof thrombolytic therapy. Am Rev Respir Dis. 1992;145 : A719.

JMS * Vol 22 * No. 1 * January, 200840
CASE REPORT
A 58 year old male patient was admitted tothe male ENT ward on 17th August'05 withthe complaints of pain at the area of left uppermolar teeth for one month and left sidedheadache, nasal obstruction and painfulswelling of the left face followed by gradualdevelopment of nasal obstruction since thelast 2 weeks. There was history of extractionof the 2 left upper molar teeth for caries teethone month back. Patient gave history of newexperience of intense irritation inside the noseand increase in swelling of the face wheneverhe consumed non-vegetarian food since hedeveloped the symptoms. On examination,patient had mild fever, mild degree of proptosiswith hyperemia in the left eye, swollen leftside of face and tenderness of left maxillarysinus. Left nostril was found congested withcrust formation and a polyp was seen at themiddle meatus.
Routine hematological and biochemicalinvestigations reports were within normallimits except the ESR was 85 mm/1st hr.ELISA test for HIV antibody was non reactive.There was no history of tuberculosis. X-raychest PA view was normal. Contrast axial CTscan of PNS showed focal hyper attenuationin the soft tissue mass with destruction of
Allergic fungal rhinosinusitis in an immunocompetent patient: a case report
1M. Usharani Devi, 2Binay Debbarma, 3H. Lokhendro Singh, 4Kh. Sulochana Devi, 5M. Madhumangol Singh,1Kh. Ranjana Devi
Endoscopic polypectomy with uncinectomyand Caldwell-Luc operation was performed onthe left side of the maxillary sinus. Themaxillary sinus was found to be enlarged andfilled with peanut butter and axle greaselooking necrotic tissue which was curetted out.There was also erosion in the posterior wallof left maxilla, communicating with pterygopalatine fossa. There was profuse bleedingduring the excision. The curetted materialswere sent for staining, aerobic, anaerobic andfungal cultures for isolation and identificationof the causative organisms andhistopathological examination.
Microbiologically, the samples were processedby 10% KOH mount, Gram stain, ZiehlNeelsen stain, aerobic, anaerobic and fungalcultures. Fungal culture was done on two SDA(Sabouraud's dextrose agar) media withchloramphenicol. The media were incubatedat 25ºC (room temperature) and 37ºC for 4weeks to isolate the dimorphic fungi.
Microscopic examinations of caseatic necrotic
1. Assistant Professor; 3. Associate Professor; 4. Pro-fessor, Deptt. of Microbiology, 2. Junior Resident; 5. Pro-fessor of Otorhinolaryngology, Regional Institute ofMedical Sciences (RIMS), Imphal.
Corresponding author:Dr. M.Usharani Devi. Dept.of Microbiology, RIMS, Imphal,Manipur. PIN-795004.e-mail address: [email protected]
Fig 1. Axial CECT of PNS showing focal hyperattenuation in distorted left maxilla.
ostium and left medial wall of maxilla (Fig 1).

JMS * Vol 22* No. 1 * January, 2008 41
CASE REPORT
tissue material in the stained films includingthe Z-N stain did not show the presence ofany microorganism. KOH mount revealedbranched septed hyphae, measuring the sizeof 3-6µm. Fungal culture at 37ºC after 1 weekrevealed powdery, green colonies with thereverse being white in color. Lacto PhenolCotton Blue (LCB) examination showedsmooth conidiophores, size about 300µm withsingle sterigmata covering upper half of thevesicle (Fig 2).
plugs were found in the first washing whichwas negative for fungal culture and theretained fluid of second washout was clear.X-ray of PNS showed reduced haziness onthe affected maxillary sinus compared toprevious X-ray. During the treatment periodthe serum creatinine level was found to beraised a little above the normal level butreturned to normal level at the end ofmedication. The routine blood examinationsand liver function tests were monitored duringthe treatment and were found to be withinnormal limits. The patient was discharged oncapsule itraconazole 200mgs daily for onemonth with advice for follow up at one monthlyinterval.
DiscussionThe combination of nasal polyposis, crustformation and sinus cultures yieldingAspergillus spp. was first noted in 1976 bySafirstein1, who also observed the clinicalsimilarity with allergic bronchopulmomaryAspergillosis (ABPA). Subsequently thisdisease was known as allergic fungalrhinosinusitis (AFS).
The AFS is a disease condition where theeosinophilic host responses occurred inpresence of fungi within the nose andparanasal sinuses and produces slowaccumulation of allergic fungal mucin in thesinus cavity. As its quantity increase, theinvolved paranasal sinus had manifestationsof nasal polyps, expansile mucocele formationwhich produced bony remodeling anddecalcification occurred, causing the diseaseto mimic invasion into adjacent anatomicspaces. This destruction often gives rise toexophthalmos, facial dysmorphia or intracranialextension without tissue invasion.2 AFSresponses to surgery therapy are very goodeventually replaced by recurrence in theabsence of ongoing therapy.7
Non-invasive Aspergillosis of the sinusescausing proptosis of the eye with bony erosionin immunocompetent person has been welldocumented3 in western countries. But itsincidence is rare in the eastern part of ourcountry as per available literature.
The fungal disease has been described at CT
Fig 2. Lacto Phenol CottonBlue preparation showingconidiophores with singleseries of sterigmata charac-teristic of A. fumigatus.
Similar type of colony morphology was seenat 25ºC but growth was seen after 2 weeks ofincubation (slow growth). Finally the fungalgrowth was identified as Aspergillusfumigatus. Bacterial culture showed no growthafter 48 hours of incubation at 37ºC.Histological examination showed focalnecrosis with edematous mucosa and feweosinophils (Fig 3). Histopathologicaldiagnosis was inflammatory tissue and noevidence of malignancy.
The patient was treated with fluconazole150mg daily for five days as soon as thepositive fungal culture report comes in additionto antibiotic cover up. There was no sign ofresponse of treatment with fluconazole. Theantifungal drug was changed to amphotericin-B infusion, given in the dose of 50 mg in 5%dextrose infusion once a day after an initialsensitivity dose and repeated on every thirdday. A course of prednisolone was also given.After 5 doses of treatment patient respondedto amphotericin-B infusion. A total of 44 dosesof amphotericin-B were infused and the patientbecame clinically symptom free.
The left maxillary sinus was washout withnormal saline for twice at the gap of one weekbefore the patient was discharged. Mucus
Fig 3. Photomicrograph ofmaxillary tissue showingfocal necrosis (F.N),(H&E×40).

JMS * Vol 22 * No. 1 * January, 200842
CASE REPORT
as a rim of soft tissue attenuation of variablethickness along the bone walls of theparanasal sinuses and these findings haveproved indistinguishable from those of bacterialinfection or neoplastic disease.4
Initially we suspected the patient to be sufferingfrom carcinoma of maxilla with extension in theleft orbit. But the two episodeshistopathological examination of excised ofpolypoid tissue showed inflammatory polyp anddid not suggest any fungal disease.
Aspergillosis of sinuses arises as a secondarydisease, superimposed upon a chronic sinusitisas described by Stammberger.6 In our patientalso he was having caries teeth for 2 yearsand had started having symptoms after theteeth extraction. It indicates that thesuperimposed infection had occurred throughroot of the teeth. Patient was immuno-competent because he was not suffering fromchronic diseases but the patient's generalcondition was poor because he was not eatingproperly and avoiding proteineous food dueto fear from protein allergy. We supplementedwith parental infusions and vitamins to buildhim up.
The patient was diagnosed to be a case ofallergic fungal rhinosinusitis because of thepresence of polyp, peanut butter and axlegrease looking necrotic tissue in the largemaxillary cavity, the CT scan finding, the
hyphae at KOH preparation and the growth ofAspergillus fumigatus on culture which fulfilledthe criteria's given by Bent and Kuhn too.5
The AFS management depends on completeremoval of all fungal mucin by surgery andprevention of recurrence through eitherimmunomudalation (immunotherapy orcorticosteroids) or fungistatic antimicrobials.7
In our case we removed the allergic fungalmucin i.e peanut butter and axle grease lookingnecrotic tissue from left maxillary sinus,pterygopalatine fossa and polypoid tissue fromthe nose endoscopically.
We treated the patient with amphotericin-B asit is said to be the drug of choice when there isdocumented bony invasion.6 A course ofprednisolone with initial dose of 40mg daily individed dose and tapered off over a period of30 days was given for immunomodalation.Patient became completely symptom free andwas discharged with advice for follow up atmonthly interval because the disease is veryprone to recur.
Acknowledgement:The authors are thankful to the Director, RIMS,Imphal for allowing us to publish this case report.We also express our gratitude and love to thepatient who have voluntarily agreed to take hisphotograph for the publication of this paper in thejournal.
References
1. Safirstein B. Allergic bronchopulmonaryaspergillosis with obstruction of the upperrespiratory tract. Chest 1976; 70:788-790.
2. Marple B F. Allergic fungal rhinosinusitis: Cur-rent theories and management strategies.Laryngoscope.2001; 111:1006-1019.
3. Manning S C, Markel M, Kriesel K, Vuitch F,Marple B. Computed tomography and mag-netic resonance diagnosis of allergic fungalsinusitis. Laryngoscope.1997; 107:170-176.
4. Zinreich S J, Kennedy D W, Jan M, Curtin HD, Epstein J I, Leslie C. Huff et al. Fungalsinusitis: Diagnosis with CT and MR imaging.
Head and Neck radiology. 1988; 169:439-444.
5. Bent J, Kuhn F. Diagnosis of allergic fungalsinusitis. Otolaryngol Head Neck Surg.1994;111:580-588.
6. Stammberger H. Functional endoscopicsinus surgery. Philadelphia: B.C. Decker,1990. p. 398-427.
7. Bradley FM, Richard LM. Allergic fungal si-nusitis in: John H. Krouse, Stephen J.Chadwich, Bruce R.Gordon, M. JenniferDerebery editors. Allergy and Immunology anotolaryngologic approach. Philadelphia:Lippincott Williams & Wilkins; 2002.p.232-248.

JMS * Vol 22* No. 1 * January, 2008 43
A 36 year old lady presented with the historyof burns (burst of kerosene stove) leading tocontractures of face, neck, chest and upperarm. The burns were 5 months old. Primarymanagement was done by the surgical teamin the ward and the patient was later referredfor release of neck contracture and harvestingof split skin graft(SSG).
Management of post burn neck contracture: a case report
1Kh. Maniram Singh, 2Sanjib Singh Nepram, 1S. Sarat Singh, 1L. Deban Singh, 3N. Ratan Singh,4Gojendra Rajkumar
1. Associate Professor; 3. Senior Registrar; 4. AssistantProfessor, Department of Anaesthesiology, 2.AssistantProfessor, Department of Plastic surgery, RegionalInstitute of Medical Sciences (RIMS), Imphal, Manipur.
Corresponding author:Dr. Kh. Maniram. Singh, Department of Anaesthesiology,RIMS, Imphal, 795004, Manipur.
of neck and SSG under general anaesthesiawith controlled ventilation but directlaryngoscopy and surgical access to airwayseemed impossible. So the release of the neckcontracture was planned under ketamine untilairway was secured.
Patient was pre-oxygenated with 100% oxygen
Fig 2. Preoperative photo-graph showing post burnneck contracture.
Fig 1. Preoperative photo-graph showing scar over theanterior aspect of neck.
Fig 3. Post release of con-tracture showing adequateneck extension.
CASE REPORT
On examination, her vital signs were stableand systemic examination was un-remarkable.All the investigations were within normallimits. The contractures involved mainly theface, neck and chest and there was a fixedflexion deformity of the neck (chinapproximated to sternum) (Fig 1). The anterioraspect of the neck was not visible. The angleof the mouths were moderately cicatrized andmouth opening was reduced (Fig 2).
She was scheduled for release of contractures
for 5 min. Glycopyrro-late 0.2mg IV andmidazolam 3mg IVwere given prior toinduction. Induction ofanaesthesia was donewith ketamine hydro-chloride 100mg IV andthe surgeon was
informed to release the neck contracture untiladequate neck extension was achieved(Fig 3). Following release of the contracture,endotracheal intubation was facilitated withatracurium in the first attempt. Anaesthesiawas maintained with nitrous oxide, oxygen,non-depolarizing muscle relaxant, systemicanalgesic and isoflurane using Bain’s circuit,and skin harvesting could be continued withoutany complications.
DiscussionSevere post burn neck contractures representa challenge to the anaesthesiologist. The usualtechnique of general anaesthesia byintravenous induction and muscle relaxantswould have been disastrous if the airway wasnot secured.
Laryngeal mask airway (LMA), Fibre-optic

JMS * Vol 22 * No. 1 * January, 200844
laryngoscope, local tumescent anaesthesiaand ketamine are few options in securing theairway in such conditions.1,2,3,4 However,inhalational induction technique, intubatingLMA, a trachlite, retrograde approach andcombitube may be useful. Tracheostomy andcricothyrotomy can be a lifesaving method ofairway preservation.
Fibre-optic laryngoscope and laryngeal maskare expensive and may not be available inmost places like ours.5 Pawan Agarwal, hasconducted thirty cases of post burn neckcontractures under tumescent localanaesthesia supplemented with intermittentdose of intravenous ketamine withoutendotracheal intubation.3 But in our case, weused ketamine to release neck contracturethough chance of apnoea may occasionallyoccur and other procedures for skin harvesting
are conducted under controlled ventilation tosecure the airway, which is almost similar withthe study of Jandova J and his coworkers6.Inhalational anaesthesia and nasotrachealintubation with or without non-depolarizingmuscle relaxants7 were not favourable in suchconditions because of risk of epistaxis andbronchospasm. Succinylcholine was not usedas the potential for exccessive potassiumrelease after burn could still occur for anindefinite period upto 6 months or longer8.Rocuronium could be an alternative choice butwe chose atracurium instead. Again retrogradeintubation is not possible because of presenceof massive scar in the anterior aspect of neck.
ConclusionIt is concluded that release of post burn neckcontractures under ketamine is a safe, simpleand effective method and can be used as aroutine practice.
References1. Nath G, Major V. The laryngeal mask in the
management of a difficult airway. Anaesth IntenCare1992;4:518-519.
2. Divatia JV, Upadhye SM, Sareen R. Fibre-opticintubation in cicatrical membranes of pharynx.Anaesthesia 1992;47:486-489.
3. Agarwal P. Safe method for release of severepost burn neck contracture under tumescentlocal anaesthesia and ketamine. Indian JPlastic Surg 2004;37(1):51-54.
4. White PF, Way WL, Trevor AJ. Ketamine itspharmacology and therapeutic uses.Anaesthesiology 1982;56:119.
5. Afilato M, Guttman A, Stern E, Lloyd J,
Colacone TA, Tselios C. Fibre-optic intubationin the emergency department. A case series.J Emerg Med 1993;11:387-391.
6. Jandova J, Kallnigova R, Kapoungova Z, BrozL. Combined technique of anaesthesia in earlyand late neck reconstruction. Acta Chir Plast.1997;39(2):56-59.
7. Layon AJ, Vetter TR, Hannaph, et al.Anaesthetic technique to fabricate a pressuremask for controlling scar formation from facialburns. J Burn care Rehabil. 1991; 12:349.
8. John DA, Tobey RE, Homer LD, et al. Onset ofsuccinylcholine-induced hyperkalemiafollowing denervation. Anesthesiology1976;45:294-299.
CASE REPORT

JMS * Vol 22* No. 1 * January, 2008 45
Mrs. SD G2P1+0 (second gravida, primipara),30 years old with 24 weeks and 2 dayspregnancy attended antenatal clinic ofObstetrics and Gynaecology department,Regional Institute of Medical Sciences, Imphalfor the first time on 15th March 2006. She wasfrom a rural area belonging to a middle levelsocio-economic group. Her last child birth was1 year and 5 months ago. Her last menstrualperiod (LMP) was on 26th September 2005.Previous medical, surgical and obstetricalhistory was unremarkable and there was nohistory of blood transfusion. There was nohistory of any congenital malformation in thefamily.
On examination, her blood pressure (BP),temperature and pulse rate were within normallimits. Cardiovascular system (CVS), centralnervous system (CNS) and chest were normal.Per abdominal examination revealed a 30weeks size gravid uterus with an oblique liewith non audible foetal heart sound (FHS). Onper vaginal examination, cervix was dilatedjust allowing the tip of a finger and uneffaced,vertex was at -2 station.
On investigations, routine laboratory testswere within normal limits. She shared thesame blood group and Rh typing as herhusband i.e. O Rh positive. Transabdominalsonography (TAS) revealed-
A large cystic lesion measuring about8.43cm X 10 cm in the neck region of thefoetus with septation and echo free pattern(Fig 1).Generalized subcutaneous oedema withincreased skin thickness all over the body,limbs and scalp were also observed.Bilateral pleural effusion and ascitis werealso seen (Fig 2).Foetal parameters: BPD (Biparietaldiameter)-19 Weeks 4 Days HC (Headcircumference) -19 Weeks 4 DaysFL (Foetal length) - 18 Weeks 4 DaysFHR (Foetal heart rate) - 146 beats per minuteDoppler indices of the umbilical arterysuggested increased placentalimpedence.
Supportive treatments were given and shedelivered a female baby weighing 2.5 Kg. at
Non-immune hydrops foetalis: a case report
CASE REPORT
1Y.Ajitkumar Singh, 2L.Ranjit Singh, 3M.Rameshwar Singh, 2Kh. Ibeyaima Devi, 1L.Bimolchandra Singh
1.Registrar; 2.Associate Professor; 3.AssistantProfessor, Department of Obstetrics and Gynaecology,Regional Institute of Medical Sciences (RIMS), Imphal.
Corresponding Author :Dr. Y. Ajitkumar Singh, Deptt. of Obs. & Gynae., RIMS,Imphal - 4.
3.54 pm on 16th March 2006 with an Apgarscore of 0/10 following induction with 0.5 mgPGE2 (Dinoprostone) gel instillation. Babywas markedly deformed (Fig 3) with multiplebirth defects viz. cystic hygroma, anasarca,pericardial effusion, pleural effusion andincreased skin thickness. Placenta weighed
u
u
u
u
u
Fig 1. TAS showing cysticlesion in the neck region offoetus.
Fig 2. TAS showing pleuraleffusion and ascites of thefoetus.

JMS * Vol 22 * No. 1 * January, 200846
2000 to 3500 live births.1 Variouschromosomal, foetal structural abnormalitiesand infections are the main causes of foetalhydrops.2 In our case foetus has cystic hygroma.Cystic hygroma was the most common structuralfoetal malformation in the series of Rose et al.3
An increase of the nuchal translucencythickness is probably the first stage of foetalhydrops. Depending on the severity of theunderlying defect, the next manifestation isgeneralized skin oedema with eventualplacental oedema, ascitis and pleuraleffusion.4 Similar ultrasound findings wereobserved in our case.
NIHF has become more common than immune
hydrops foetalis. Mortality was of 81% andcomplications more frequent.5 So considerableemphasis must be placed on early antenataldiagnosis to achieve a precocious treatmentand to improve the present poor prognosis.Rose et al3 diagnosed NIHF prenatally at 17.3weeks. Unfortunately our case was diagnosedat the beginning of the third trimester becauseof late reporting by the patient. Serum humanchorionic gonadotropin (hCG) is elevated inNIHF at second trimester but wasunremarkable when NIHF presented later.6
Prenatal pericardial and pleural effusion orcongenital anomalies carry a very poorprognosis in patients with NIHF.7 Maeda et al8observed that albumin and/or packed red cellinjection into foetal abdominal cavity was aneffective procedure for in utero treatment ofNIHF without pleural effusion, but none couldbe recovered in utero when it was associatedwith pleural effusion. In our case, we could notsave the foetus.
Since non-immune hydrops becomesproportionately more common, radiologistsshould be aware that the diagnosis of ‘hydropsfoetalis’ is not synonymous with‘erythroblastosis’. 9
References1. Yanez Maldonado E, San Martin Herrasti JM,
Garcia Alousa A, Izquierdo Puente JC. Non-immunologic hydrops. Report of 2 cases,Ginecol obstet Mex. July 2000; 68:282-5.
2. Heinonen S, Ryynanen M, Kirkinen P. Etiologyand outcome of second trimester non-immunologic foetal hydrops. Acta ObstetGynecol Scand. Jan 2000;79(1):15-8.
3. Rose CH, Bofill JA, Le M, Martin RW. Non-immune hydrops foetalis: prenatal diagnosisand perinatal outcomes. J Miss State MedAssoc. April 2005; 46(4):99-102.
4. Jauniaux E. Diagnosis and management ofearly non-immune hydrops foetalis. PrenatDiagn. Dec 1997; 17(13):1261-8.
5. Cervantes Pardo A, Castillo Diaz LM, GarciaMoreno M, Martinez Villalta E, Torres Tortosa
P, Borrajo Guadarrama E. Non-immunehydrops foetalis. Review of 11 cases. An EspPediatr. Jan 1988; 28(1):43-7.
6. Saller DN Jr, Canick JA, Oyer CE. Thedetection of non-immune hydrops throughsecond-trimester maternal serum screening.Prenat Diagn. May 1996; 16(5):431-5.
7. Rejjal AR, Rahbeeni Z, al-Zahrani AF.Prognostic factors and prenatal managementin non-immune hydrops foetalis are still adilemma. J Perinat Med.1997; 25(4):388.
8. Maeda H, Koyanagi T, Nakano H .Intrauterinetreatment on non-immune hydrops foetalis,Early Hum Dev. Jun-July 1992;29(1-3):241-9.
9. Houstan CS, Ninan A, Best TB.Radiology ofnon-immune hydrops foetalis, J. Can Assocradiol. Jun 1982; 33(2): 107-9.
CASE REPORT
Fig 3. Photograph showingnon-immune hydrosfoetalis with placenta.
700 grams, lookedoedematous andhypertrophied. Shewas discharged onthe following day.
DiscussionNon immune hydropsfoetalis (NIHF) is anuncommon entity, it isobserved in 1 in

JMS * Vol 22* No. 1 * January, 2008 47
Leri-Weill Dyschondrosteosis: a case report
1S. Subhaschandra singh, 2W. Jatishwor, 3S. Ranjan
CASE REPORT
A 50 years old female presented with pain,deformity and limitation of movement of thewrist joints since her young adolescent age.She was short stature and married with threechildren. Two of the children, a son and adaughter were short stature. She was ofnormal intelligence. X-ray of both wrists withthe forearms revealed the following findings(Fig 1 a & b) –1. Relatively long ulna compared to radius.2. Triangular shaped distal radius epiphysis.3. Decreased carpal angle.4. Wedging of the carpal bones between the
deformed radius and protruding ulna.5. Increased width between distal radius and
ulna.6. Normal metacarpals and phalanges.
X-ray of both legs revealed short tibias andfibulas with relatively longer fibulas, i.e.tibio-fibular disproportion (Fig 2).
These are characteristics of “MadelungDeformity” . Short stature, normal intelligence,bilateral symmetrically involvement and chil-dren with dwarfism favored the possibility ofLeri-Weill dyschondrosteosis. Mesomelicdwarfism with the presence of tibio-fibular dis-proportion and by exclusion of other causesof Madelung deformity, the diagnosis of Leri-
Weill dyschondrosteosis was made. Therewere no biochemical or endocrinalabnormality detected. No genetic work up wasdone on this case.
DiscussionLeri- Weill dyschondrosteosis is an automasaldominant disease and a form of mesomelicskeletal dysplasia with Madelung deformity ofthe distal radius and ulna, proximal carpal
bones and Mesomelicdwarfism1,2, being ahallmark. As far asstature is concerned,final height infemales isapproximately 1.45mand in males 1.55m.There is also great
1. Registrar; 2. Associate Professor, Department ofRadiodiagnosis, Regional Institute of Medical Sciences(RIMS), Imphal, Manipur, 3. Consultant Radiologist,Babina Diagnostic Centre, Imphal.
Corresponding author:S. Subhaschandra singh, MD, Asst. Prof., Dept. ofRadiodiagnosis, RIMS, Imphal, Manipur- 795004.E-mail: [email protected].
variation among patients with identicalmutations belonging to the same family.Females are more frequently affected thanmales and growth failure as well as clinicalfeatures, such as bilateral Madelung deformity,has been described as being more severe infemales than in males. A female to male ratiois about 4 to 1 and female are more severelyaffected 3,4. SHOX gene (short stature homebox
Fig 1. X-ray both wrists AP (a) and Lateral (b) showingfeatures of Madelung Deformity
Fig 2. X-ray both legs AP viewshows relatively long fibula.

JMS * Vol 22 * No. 1 * January, 200848
CASE REPORT
containing gene) defect that ishaploinsufficiency due to heterozygotemutations the pseudo-autosomal SHOX geneis the main cause of Leri-weilldyschondrosteosis.3 Characteristic MadelungDeformity is present in 74% of Leri- Weilldyschondrosteosis.3 The process of shortstature and wrist deformity usuallybegins in adolescence with premature fusionof the medial aspect of the distal radialepiphysis, resulting in asymmetrical growth.2
Binder et al5 observed that the growth failurein Leri-Weill dyschondrosteosis occurredbefore the age of 6 years, partly alreadybefore birth. Growth velocity after the age ofsix was normal. It was also observed that thedisturbance in growth was not as severe as inTurner syndrome. It was demonstrated thatgrowth failure was observed during the firstyear of life with a mean height loss of 2.16SDS in childhood, whereas pubertal growthwas mildly or not affected. Furthermore, it wasshown that children with a severe degree ofwrist deformity were significantly shorter thanthose with mild deformities.5
A German surgeon, Madelung first describedthe characteristic wrist deformity, i.e. ‘MadelineDeformity’ in 1878 before Leri -Weilldychondrosteosis was described.2 The causesof this deformity may be - (i) post-traumatic,(ii) extension injuries of the wrist, (iii) MultipleHereditary Exostosis, (iv) Turner Syndrome and
(v) Idiopathic. Idiopathic variety is commonlybilateral than unilateral and asymmetrical inseverity. There is symmetry of the bilateralwrists deformity in this index case. No historyof trauma in childhood was present. No exos-tosis was seen in the radiographs. The preva-lence of Madelung deformity is higher indyschondrosteosis versus Turner Syndromepopulation.3 The metacarpal bones werenormal in the index case, and the fourthmetacarpal bone may be short in TurnerSyndrome. In Leri-Weill dyschondrosteosis,there is typical Madelung deformity withlimitation of motion at wrist and elbow andmesomelic dwarfism. Additional findings thatmay be seen in dyschondrosteosis aredeformed tibial metaphysis, flattening ofmedial epiphysis. Skull and axial skeletal ischaracteristically normal.2 The patients tallerthan 25th percentile for height probably do nothave dyschondrosteosis.6 There is reportedassociation of Leri-Weill Dyschondrosteosiswith middle ear deformity and conductivehearing loss.7 Tibio-fibular disproportion withtibia varum and long fibula are seen in 50% ofthe cases.8 There may be fusion of the C1and C2 vertebrae. Increased predisposition ofHodgkin’s in patients with dyschondrosteosishas been reported.4 There are therapeutictrials using recombinant growth hormone withvariable results depending on the time ofinitiation of treatment.5
References1. Langer Jr L O. Dyschondrosteosis, a heritable
bone dysplasia with characteristicroengentnographic features. Am. J. Roentgen1965; 95:178-188.
2. Greenfeild GB. Radiology of Bone Diseases,Fourth Edn. Philadelphia: J.B Loppincott Com-pany; 1986.p. 275 -276.
3. Ross JL, Bellus G;Scott CI, Aboudi Jr J;Griegelioniene G, Zin AR. Mesomelic andrhizomelic short stature: the phenotype of com-bined Leri- Weill dyschondrosteosis andachondroplasia or hypochondroplasia. Am. J.Med. Gent 2003; 116A:61-65.
4. Gokhale DA, Evans DG, Growther D, Woll P.;Watson CJ, Dearden SP, et al. Moleculargenetic analysis of a family with history of
Hodgkin’s disease and Dyschondrosteosis.Leukemia1995; 9: 826-833.
5. Binder G, Renz A, Martinez A, et al. J. ClinEndocrinology &metabolism 2004; 89(9): 4403-4408.
6. Felman AH, Kirkpatrick JA, Jr Madelung.Deformity: observation in 17 patients. Radiol-ogy 1969; 93:1037-1042.
7. Nassif R, Harboyan G. Madelung Deformitywith conductive hearing loss. Arch. Otolaryng.1970; 91:175-178.
8. Dawe C, Wynne-Davies R, Fulford G E.Clinical Variation in Dyschondrosteosis:areport on 13 individuals in 8 families. J. BoneJoint Surg. 1982 ; 64B:377-381.

JMS * Vol 22* No. 1 * January, 2008 49
Psychiatric disorders in Parkinson’s disease: an update
Parkinson’s Disease (PD) is a neuro-degenerative disorder involving disturbancesin motor control. Over 60% of patients willexperience psychiatric symptoms/disorders inthe course of their illness. This reviewhighlights recent developments inneuropsychiatric disorders in Parkinson’sdisease and progressions in treatment.
Anxiety and Parkinson’s diseaseAnxiety disorders have recently beenreviewed1and generalized anxiety disorderseems to be he most common and best studiedin PD2. A few papers have suggested newrating scales to evaluate anxiety disorders inPD. In some cases, psychological factors suchas depressive symptoms on anxiety contributemore to a low quality of life than motorsymptoms.3 In PD patients, anxiety is oftenrelated to the off state, that is, more anxietywith less mobility. In many cases there iscomorbidity between anxiety and depressionin patients with PD and anxiety in particular isoften not recognized by the physician.4
Selective serotonin reuptake inhibitor drugs areeffective and generally well tolerated inpatients with PD when treating mixeddepression and anxiety states.5 Benzodiazepineshould be avoided or only used with great
caution because of detrimental effects onbalance and cognitive functions.5
Depression and Parkinson’s diseasePatients with PD experience affectiveepisodes. This was noticed by JamesParkinson in the original description of thedisease.6 Recently several new epidemiolo-gical achievements have been accomplished.Depression in patients with PD has been foundin more than 40% in consecutive series.7,8 Thiswas also found in Cumming’s Seminal review.9An interesting approach using logisticregression has investigated if risk factors foridiopathic depression in general are alsomarkers for depression in PD.10
Not only does PD increase the risk fordepression, but also depression is, in fact, arisk factor for PD and may in some cases bethe presenting symptom of PD.11,12,13 Anincreased incidence of hypothyroidism in PDhas been found and therefore the level ofthyroid –stimulating hormone and free T4 –hormone should be examined in PD patientswith any ‘mood’ symptom.14 Hypothyroidismshould be treated with thyroid hormonereplacement therapy and this will often in itselfcorrect the mood symptoms.14 In cases ofpersisting symptoms an antidepressant shouldbe added, since it has recently been shownthat hypothyroidism can act as a risk factor fordepression. An interesting open levelrandomized trial of pramipexol, administeredas an antidepressant in moderately depressedpatients with advanced PD and already on L-dopa treatment, clearly needs replication.15
1. Assistant Professor, Department of Psychiatry,2. Assistant Professor, Department of Medicine, RegionalInstitute of Medical Sciences(RIMS), Imphal.
Corresponding author:Th. Bihari Singh, Assistant Professor, Department ofPsychiatry, RIMS, Imphal.
UPDATE
1Th. Bihari Singh, 2Santa Naorem, 2N. Biplab Singh, 2Robinson Ningshen

JMS * Vol 22 * No. 1 * January, 200850
Pramipexole was used as an add-on drug andno patients with severe depression wereincluded. In a neuropsychological evaluationof pramipexole, it was suggested that it mayworsen cognitive function in PD patients.16 ACochrane review that located 42 conductedstudies concluded that only three met thecriteria for meta-analysis.17 This only illustratesthe need for clinical trials to answer the veryimportant question of how depression shouldbe treated in patients with PD.
Psychosis and Parkinson’s diseasePsychosis in patients with PD occurs inapproximately 30%. In PD many cases ofpsychosis are caused by levodopa therapy18
and often in the form of complex visualhallucinations or, in mild cases, illusions. Inmost cases the patients vividly see smallanimals or have an ideation of presence ofpeople in the room. This is the most frustratingexperience both for the patients and spouses.Psychosis is a strong risk factor for nursinghome placement.19 In younger patientspsychosis is usually drug induced orsecondary to depression. In older patients itshould be remembered that psychosis couldbe the harbinger of dementia.20
PD patients with psychosis should be treatedin a three step approach. First of all it isimportant to identify underlying causes likeurinary infection, stroke or metabolic changesthat should explain a confusional state.Secondly the antiparkinsonian medication,levodova and anticholinergic drugs, should begradually reduced if possible. As a last resort,an antipsychotic drug should be administeredto the patient. The first line of drug treatmentis clozapine in moderate doses (15-50 mg/day).Placebo controlled, double blind trials havedemonstrated its effectiveness in treating thepsychosis in PD patients. The advantages arethat it improves tremor, does not worsen motorfunctions in general, can be administered oncedaily and is safe in low doses.21,22 Side effects
are sedation, orthostatic hypotension andsialorrhoea. The drawbacks are the risk ofblood dyscrasia and therefore specializedmonitoring of white blood cell count isrequired.23 Both resperidone and olanzepinehave been reported to increase motordysfunction in patients with PD.23 The fourth,new generation antipsychotic drug that hasbeen evaluated in drug trials in PD patients isquetiapine. Quetiapine seems to be lesseffective, less potent and less free of motorworsening in patients with PD compared withclozapine. However, quetiapine is easier to use,better tolerated and has a low risk of intolerablemotor worsening. Some authors recommendquetiapine as first-line drug treatment inpatients with psychosis24, with clozapine assecond line of treatment. Long follow-up studiesare warranted and clozapine has been betterstudied in this respect.25
Resperidone and olanzapine are recommendedonly if clozapine or quetiapine is not toleratedbecause of the risk of worsening motorfunctioning in PD patients on resperidone orclozapine.21,25 Other treatment modalities wouldbe ziprasidone, ondansetron and electro-convulsive therapy/Ziprasidone is the newestatypical antipsychotic drug, but no studies havebeen published about its use in patients withPD. Ondansetron is an antiemetic and aselective 5- HT3 antagonist. Zoldan et al26
reported ondansetron improved psychoticsymptoms in patients with PD, but this needsreplication. Electroconvulsive therapy shouldonly be considered when several drugtherapies have been unsuccessful.
ConclusionIn conclusion, many psychiatric complicationsin patients with PD need to be assessed byclinicians to decide the right evaluationprogramme. Several recently developedtreatments are available, but some need furtherevaluation and replication of interestingfindings.
Cambridge, UK: Cambridge University Press:2002.
References1. Stasrkstein SE, Merallo M. Psychiatric and
Cognitive disorders in Parkinson’s disease,
UPDATE

JMS * Vol 22* No. 1 * January, 2008 51
2. Shiba M, Bower JH, Maraganore DM, et al.Anxiety disorders and depressive disorderspreceding Parkinson’s disease: A case ControStudy. Mov Disord 2000; 15: 669 – 677.
3. Scharg A, Jahanshahi M, Quinn N. Whatcontributes to quality of life in patients withParkinson’s disease? J. Neurol NeurosurgPsychiatry 2000; 69: 308 – 312.
4. Shulman LM, Taback RL, Rabinstein AA,Weiner WJ. Non-recognition of depression andother non-motor symptoms in Parkinson’sdisease. Parkinsonism Relat Disord 2002; 8:193-197.
5. Rabinstein AA, Shulman LM. Management ofbehavioral and psychiatric problems inParkinson’s disease. Parkinsoniasm RelatDisord 2000; 7: 41-50.
6. Victor M, Ropper A H. Adams and Victor’sprinciples of neurology, 7th ed. NewYork:McGraw-Hill Medical Publishing division;2001. p. 1128.
7. Anguenot A, Loll PY, Neall JP, et al. Depressionand Parkinson’s disease: Study of a series of135 Parkinson’s patients (in French). Can JNeurol Sci. 2002; 29: 139 – 146.
8. Brandstadter D, Oertel WH. Depression inParkinson’s disease. Adv Neurol 2003; 91: 371– 381.
9. Cummings JL. Depression and Parkinson’sdisease: A review. Am J Psychiatry 1992; 149:443 – 454.
10. Leentjens AF, Lousberg R, Verhey FR. Yarkersfor depression in Parkinson’s disease. ActaPsychiatr Scand 2002; 106: 196 – 201.
11. Aansaland D, Cumming’s JL. Depression inParkinson’s disease. Acta Psychiatr Scand2002; 106: 161 – 162.
12. Okun MS, Watts RL. Depression associatedwith Parkinson’s disease: Clinical features andtreatment. Neurology 2002; 58: S63 – S70.
13. Nilsson FM, Kessing LV, Bolwig TG. Increasedrisk of developing Parkinson’s disease forpatients with major affective disorder: a registerstudy. Acta Psychiatr Scand 2001; 104: 380 –386.
14. Schuurman AG, Van den Akker M, EnsinckKt, et al. Increased risk of Parkinson’s diseaseafter depression: a retrospective Cohort study.Neurology 2002; 58: 1501 – 1504.
15. Rektorova I, Rektor I, Bares M, et al. Pramipexoland pergolide in the treatment of depressionin Parkinson’s disease : a national multicentreProspective randomized study. Eur J Neuro2003; 10: 399 – 406.
16. Brusa L, Bassi A, Stefani A, et al. Pramipexolein comparison to L-dopa: a neuropsychologicalstudy. J Neural Transm 2003; 110: 373-380.
17. Chung TH, Deane KH, Ghazi – Noori S, et al.Systematic review of antidepressant therapiesin Parkinson’s disease. Parkinsonism RelatDisord 2003; 10: 59 – 65.
18. Factor SA, Molho ES, Podskalny GD, BrownD. Parkinson’s disease: drug inducedpsychiatric states. Adv Neurol 1995; 65: 115 –138.
19. Aarsland D, Larsen JP, Janberg E. Predictorsof nursing home placement in Parkinson’sdisease: a paoplation-based, prospective study.Ja Am Geriatr Soe 2000; 48: 938 – 942.
20. Lenox BR, Lennox GG. Mind and movement :the neuropsychiatry of movement disorders. JNeuro Neurosurg Psychiatry 2002; 72 (Suppl1): 128 – 131.
21. Freidman JH, Fernandez HH. Atypicalantipsychotics in the treatment of drug inducedpsychosis in Parkinson’s disease. Mov Disord2000; 15: 201 – 211.
22. Freidman JH, Fernandez HH. Atypicalantipsychotics in Parkinson’s Sensitivepopulations. J. Geriate Psychiatry Neurol 2000;15: 156 – 170.
23. Fernander HH, Trieschmann ME, FriedmanJH. Treatment of Psychosis in Parkinson’sdisease: Safety consideration . Drug saf 2003;26: 643 – 659.
24. Fernander HH, Trieschmann ME, Burke MA,et al. Long-term outcome of quetiapine use forpsychosis among Parkinsonian’s patients. MovDisord 2003; 18: 510 – 514.
25. Klein C, Gordon J, Pollak L, Rabey JM.Clozapine in Parkinson’s disease psychosis:5 year follow-up review. Clin Neuropharmacol2003; 26: 8 – 11.
26. Zoldan J, Friedberg G, Livneh M, Melamod E.Psychosis in advanced Parkinson’s disease:treatment with ondansetron, a 5HT3 receptorantagonist. Neurology 1995; 45: 1305 – 1308.
UPDATE

JMS * Vol 22 * No. 1 * January, 200852
1. General
Journal of Medical Society, is published from theRegional Institute of Medical Sciences, Lamphelpat,Imphal -795 004, India. It is published three timesa year. The articles are accepted only on thecondition that they are solely contributed to thisjournal. The Editorial Board has the right to revisethe article and make changes (inhouse style) ormay ask the author to rewrite. Papers presented inthe various scientific meetings of the Society shallbe given preference.
2. Scope
The Journal of Medical Society accepts, in English,Review articles, Original research articles, Shortcommunications, Case reports, Earlycommunications and Letters to the Editor, Articlesof general interest on methods in medicine, medicaleducation and update on therapeutics are alsowelcome.
Review articles and Educational forum: Reviewarticles are written by the researchers of aconsiderable experience in the field concerned.The author should review the recent trend or theadvances in that field. The major portion of abovearticles should deal with the up to date developmentsin the field in the last 3-5 years.
Full length research articles and shortcommunications: Original work will be consideredunder these sections depending on the volume andquality of work.
Case Reports: It should be divided into casehistory and discussion with maximum of 6references only. Illustrations/photographs and tableswhen included should be limited to two each.
Early communication: A manuscript will beaccepted for Early communication if it meritspublication. The decision of acceptance orotherwise will be communicated within four weeksof receipt of the manuscript and accepted articleswill be published in the following issue.
Letters to the editor: Comment(s) on previouslyarticles, items of current interest and brief originalcommunications will be published.
INSTRUCTIONS TOAUTHORS
3. Editorial policy
Manuscripts for publication will be considered ontheir individual merits. All manuscripts will besubjected to peer review. Normally all manuscriptswill be sent to all least two reviewers and theircomments along with the editorial board’s decisionwill be forewarded to the contributor for furtheraction. The author may suggest more than 5referees working in the same area for evaluatingthe manuscript. However, the JMS reserves theright to choose referees.
The Journal of Medical Society will insist on ethicalpractices in both human and animalexperimentation. When investigations on humansubjects are reported, evidence for approval by alocal Ethics Committee mustbe given. The journal will not consider any paperwhich is ethically unacceptable.
The quotations, tables or illustrations published inother journals, books etc. should not be reproducedwithout the permission of the publisher or theoriginal author. These materials must beaccompanied by the written permission from thecopyright owners.
Any article accepted for publication/published inthe Journal of Medical Society will be the copyrightof the journal.
4. Submission of the manuscript
a) Three copies of the manuscript should besubmitted neatly typed or printed doublespaced on a A4 size paper only on one side.
b) Manuscripts may also be submitted on a 31/2" PC diskette. The text files have to be inMS-Word or Adobe PageMaker format. Thefigures included as separate files and shouldbe created using standard softwares. A hardcopy (paper copy) of the manuscript mustaccompany the diskette, which must be clearlylabeled. The label must contain the title of themanuscript and the corresponding author’sname and his affiliations, and address.
In case of any discrepancy between paperand disk versions of manuscript, the paperversion will be considered for publication.
c) Final accepted version of .the manuscript mustbe submitted on a diskette.
d) The manuscript must be submitted with astatement, signed by all authors, regarding theoriginally, authorship and copyright transfer.
e) Mailing Address: Three copies of the Articleshould be sent to the Editor, Journal of Medi

JMS * Vol 22* No. 1 * January, 2008 53
cal Society, RIMS, Lamphelpat, Imphal -795004, Manipur India. Fax No. (0385) 310625,E-mail:[email protected]
5. Preparation of the manuscriptAuthors should keep their manuscripts short.
Manuscripts should be typed doubled spaced onone side of good quality A 4 size paper. The fontsize should be less than11 point. Page should benumbered beginning with the title page.
The language of manuscript must be simple andexplicit.
5.1. Full length of original articles
It should be arranged into following sections :
a) Title page, b) Summary and Key words, c)
Introduction, d) Material and Methods, e) Results,f) Discussion, g) Conclusion, i) References, j)Tables and k) Figures.
A word count is mandatory and should not exceed3200.
5.1.1
Title page: It should be paginated as page 1 of thepaper. It should carry title, the author’s names andtheir affiliations, running title, address forcorrespondence including e-mail address and alsothe list of number of pages, number of figures andnumber of tables.
Title: Must not exceed 150 characters and shouldbe informative and specific.
Authors and affiliations: The names of authors andtheir appropriate addresses should be given.Authorship should be clearly defined. Authors arerequired to submit a statement of the contributionsmade by each author.
Running title: A short running title of not more than$0 characters should be given. .
Address for correspondence: The correspondingauthor’s address should be given in the title page.The details of fax number and e-mail address shouldbe provided.
5.1.2. Summary and key words
Summary: It must start on a new page carrying thefollowing information: a) Title (without authors’names or affiliation), b) Summary, c) Key words,
d) Running title. It should not exceed 250 words.The summary must be concise and clear,informative rather than indicative. New andimportant aspects must be emphasized.
The summary must be in a structured formconsisting of AIMS, METHODS, RESULTS,CONCLUSION briefly explaining what was intended,done, observed and concluded. Authors shouldstate the main conclusions clearly and not in vaguestatements. The conclusions and recommendationsnot found in the text of the article should not begiven in the summary.
Key words: Provide 3-5 key words which will helpreaders or indexing agencies in cross indexing thestudy. Use terms from the latest Medical SubjectHeadings (MeSH) list of Index Medicus. A moregeneral term may be used if a suitable MeSH termis not available.
5.1.3 Introduction -
It should start on a new page. Essentially this sectionmust introduce the subject and briefly say how theidea for research originated. Give a concisebackground of the Study. Do not review the literatureextensively but provide the most recent work thathas a direct bearing on the subject. Justificationfor research aims and objectives must be clear!ymentioned without any ambiguity. The purpose ofthe study should be stated at the end.
5.1.4 Materials and Methods
The section should deal with the materials usedand the methodology -how the work was carriedout. The procedure adopted should be describedin sufficient detail to allow the experiment to beinterpreted and repeated by readers, if necessary.The number of subjects, the number of groupsstudied, the study design, sources of drugs withdosage regimen or instruments used, statisticalmethods and ethical .aspects must be mentioned under the section. Themethodology -the data collection procedure -mustbe described in detail. If the procedure is acommonly used one, then giving a reference(previously published) would suffice. If a methodis not well known (though previously published) itis better to describe it briefly. Give explicitdescriptions of modifications or new methods sothat the readers can judge their accuracy,reproducibility and reliability.
The nomenclature, the source of materials andequipment used, with details of the manufacturersin parentheses, should be clearly mentioned. Drugsand chemicals should be precisely identified usingtheir non-proprietary names or generic names. If

JMS * Vol 22 * No. 1 * January, 200854
necessary, the proprietary or commercial namemay be inserted once in parentheses. The firstletter of the drug name should be in small cap {e.g.nifedipine, propranolol) but capitalized forproprietary names {e.g. Depin, Inderal). New oruncommon drug should be identified by thechemical name and structural formula.
The doses of drugs should be given as unit weightper body weight e.g. mg/kg and concentrationsshould be given in terms of molarity e.g. nmol ormmol.
Statistical methods: The details of statistical testsused and the level of significance should be stated.If more than one tests are used it is important toindicate which groups and parameters have beensubjected to which tests.
5.1.5 Results
The results should be stated concisely withoutcomments. It should be presented in logicalsequence in the text with appropriate reference totables and figures. The data given in tables or figuresshould not be presented in both tabular and graphicform. Simple data may be given in the test itselfinstead of figures or tables. Avoid discussions andconclusions in the result section.
5.1.6 Discussion
This section should deal with the interpretation ofresults, rather than recapitulation of them. It isimportant to discuss the new and significantobservations in the light of previous work. Discussalso the weakness or pitfalls in the study. Newhypotheses or recommendations can be putforth.
5.1.7 Conclusion
Avoid unqualified statements and conclusions notcompletely supported by the data. Conclusion mustbe drawn considering the strengths and weaknessof the study. They must be conveyed in the lastparagraph under d[-scussion section. Make sureconclusions drawn to tally with the objectives statedin introduction.
5.1.8 Acknowledgments
It should be typed in a new page. Acknowledgeonly persons who have cohtributed to the scientificcontent or provided technical support may bemention.
5.1.9 References
It should begin on anew page. The number ofreferences should normally be restricted to amaximum of 25 for a full paper. Majority of them
should preferably be of articles published in thelast 5 years.
Papers that have been submitted and accepted butnot yet published may be included in the list of thereferences with the name of the journal andindicated as “In Press”. A photocopy shouldnormally be submitted with the manuscript.Information from the manuscripts submitted but notyet accepted should not be included.
Avoid using abstracts and references. The“unpublished observations” and “personalcommunications” may not be used as referencesbut may be inserted (in parentheses) in the text.
The references must be verified by the author(s)against original documents. Contributors shouldsubmit th~ manuscript (including references) inaccordance to the “Uniform Requirement forManuscripts Submitted to Biomedical Journals”,which can be accessed at http:/ /www.icmje.org/index.html or N Engl J Med 1997;366:309-15.
5.1.10 TablesEach table must be self-explanatory. It should betyped with double spaced on a separate sheet andnumbered consecutively in Arabic numerals. Tableshould have a proper heading and each stub andcolumn should also have subheadings. The numberof observation, subjects and the units of numericalfigures must be given. It is also important to mentionwhether the given values are mean, median, mean.:t. SD or mean .:t. SEM. All significant results mustbe indicated using asterisks. The approximateposition of the tables should be marked in the text.Do not use internal horizontal or vertical lines.
5.1.11 Figures
Each figure must be numbered and a short captionmust be provided. For graphs and flow charts it isnot necessary to submit the photographs. Amanually prepared or computer drawn figure on agood quality paper is acceptable. Raw data forgraphs must be submitted when article is acceptedfor publication. This will enable the Editorial officeto draw the graph on the computer and incorporateit in the text at an appropriate place.
For other diagrams (e.g., tissue structure, ECG andinstrument setup etc.), strongly contrasting blackand white photographic print on a glossy paper mustbe submitted.
Identify each figure/diagrams on the back with atyped label which shows the number of the figure.The name of the leading author, the title ofmanuscript and the top side of the figure. The approxi-

JMS * Vol 22* No. 1 * January, 2008 55
mate position of each figure should be marked onthe margin of the text.
Three figures per article will be printed free ofcharge. The authors will be charged for additionalfigures. The contributor must bear full cost ofprinting color plates if any.
Large/complex tables or figures may be submittedin “Final Print (Camera ready) Format” which willbe scanned and printed as such.
5.2 Short communications
The format is same as that of full papers but thelength including tit!e and references should notexceed 1600 words plus two figures or tables orone of each. The summary should be less than150 words and the number of references shouldnot exceed 12.
5.3. Early communications
The manuscript should not be divided into sub-sections. It may contain up to 1200 words (includinga maximum of 6 references) plus one simple figureor table.
5.4. Letters to Editor
It can have a maximum of 800 words (including amaximum of 4 references) plus one simple figureor table. The manuscript should not have sub-sections.
5.5 Review articles and Educational forum
It should contain title page. Summary (need not bein structured form) and key words. The text propershould be written under appropriate sub- headings.
The authors are encouraged to use flowcharts,boxes, simple tables and figures for betterpresentation. The total number to text words shouldnot exceed 6400 and the total number of figuresand tables should be less than 10.6. Revised manuscript
The authors should revise the manuscript.immediately after the receipt of the comments fromJMS. A note mentioning the changes incorporatedin the revised text as per referee’s comments (pointby point) should be sent. The revised manuscripthas to be submitted in duplicate along with theannotated original paper within 2 weeks. If therevised manuscript is received 2 weeks afterdespatch from the Editorial Office, it will beconsidered as anew submission.
Calling for revision does not guarantee acceptance.The revised manuscripts that require major revisionare likely to be sent to referees for evaluation. Ifthe authors have substantial reasons that theirmanuscript was rejected unjustifiably, they mayrequest for reconsideration. The correspondencein this regard should be sent in triplicate.
7. Proofs
Proofs will be sent to the corresponding author forfinal checking. It is the author’s responsibility togo through the proof meticulously and correct errorsif any. Correction should be restricted to printer’serror only and no substantial addition/ deletionshould be made.
8. Reprints
Reprints must be ordered while returning thecorrected page proofs.