Melatonin activates the Nrf2-ARE pathway when it protects against early brain injury in a...
-
Upload
zhong-wang -
Category
Documents
-
view
213 -
download
0
Transcript of Melatonin activates the Nrf2-ARE pathway when it protects against early brain injury in a...
Melatonin activates the Nrf2-ARE pathway when it protects againstearly brain injury in a subarachnoid hemorrhage model
Introduction
Melatonin (N-acetyl 5-methoxytryptamine) and its metab-olites have been demonstrated to fortify the antioxidantsystem by scavenging free radicals, stimulating antioxidant
enzymes and the synthesis of glutathione (GSH), increasingthe activities of other antioxidants, protecting antioxidativeenzymes from oxidative damage, and augmenting theefficiency of the mitochondrial electron transport chain
[1–4]. Melatonin is a powerful antioxidant and it easilycrosses cell membranes and cannot be reduced to its formerstate in redox cycling [5]. Several reports from experimental
studies have demonstrated that melatonin plays protectiveroles in subarachnoid hemorrhage (SAH) including reduc-ing early brain injury (EBI) and neurological symptoms [6],
decreasing mortality [7], preventing vasospasm and apop-
tosis of endothelial cells of vessels [8], and alleviating focalcerebellum injury [9]. Our earlier research has demonstratedthe protective role of melatonin in cerebral vasospasm after
SAH through its antioxidative and anti-inflammatoryproperties [10]. To date, however, none of the previousstudies concerning melatonin and SAH focused on theunderlying signaling pathway related to oxidative stress,
and also the molecular mechanism of melatonin in SAHmodel remains unclear.Protective genes, whose products could reduce oxidative
stress, contain a common promoter element called theantioxidant response element (ARE). Several transcriptionfactors can bind ARE; however, the nuclear factor E2-
related factor 2 (Nrf2) is responsible for activating tran-scription in response to oxidative stress [11]. Undernumerous stimuli, Nrf2 translocates from the cytoplasm
Abstract: Melatonin has beneficial effects against early brain injury (EBI) by
modulating cerebral oxidative stress after experimental subarachnoid
hemorrhage (SAH); however, few investigations relate to the precise
underlying molecular mechanisms. To date, the relation between melatonin
and nuclear factor erythroid 2-related factor 2 and antioxidant responsive
element (Nrf2-ARE) pathway has not been studied in SAH models. This
study was undertaken to evaluate the influence of melatonin on Nrf2-ARE
pathway in rats after SAH. Adult male SD rats were divided into four
groups: (i) control group (n = 18); (ii) SAH group (n = 18); (iii)
SAH + vehicle group (n = 18); and (iv) SAH + melatonin group
(n = 18). The rat SAH model was induced by injection of 0.3 mL fresh
arterial, nonheparinized blood into the prechiasmatic cistern in 20 s. In
SAH + melatonin group, melatonin was administered i.p. at 150 mg/kg at 2
and 24 hr after the induction of SAH. Brain samples were extracted at 48 hr
after SAH. Treatment with melatonin markedly increased the expressions of
Nrf2-ARE pathway-related agents, such as Nrf2, heme oxygenase-1,
NAD(P)H:quinone oxidoreductase 1, and glutathione S-transferase a-1.Administration of melatonin following SAH significantly ameliorated EBI,
including brain edema, blood–brain barrier (BBB) impairment, cortical
apoptosis, and neurological deficits. In conclusion, post-SAH melatonin
administration may attenuate EBI in this SAH model, possibly through
activating Nrf2-ARE pathway and modulating cerebral oxidative stress by
inducing antioxidant and detoxifying enzymes.
Zhong Wang1, Chao Ma1,Cheng-Jie Meng1, Guo-QingZhu2, Xue-Bo Sun1, Lei Huo2, JianZhang2, Hui-Xiang Liu3,Wei-Chun He4, Xu-Ming Shen5,Zhang Shu5 and Gang Chen1
1Department of Neurosurgery, The First
Affiliated Hospital of Soochow University,
Suzhou, Jiangsu Province, China;2Department of Surgery, Suzhou Municipal
Hospital, Suzhou, Jiangsu Province, China;3Department of Neurosurgery, Zhangjiagang
Hospital, Soochow University, Suzhou,
Jiangsu Province, China; 4Department of
Neurosurgery, Zhangjiagang Hospital of
Traditional Chinese Medicine, Suzhou,
Jiangsu Province, China; 5Department of
Surgery, Taicang People�s Hospital, Suzhou,
Jiangsu Province, China
Key words: early brain injury, melatonin,
nuclear factor erythroid 2-related factor 2,
subarachnoid hemorrhage
Address reprint requests to Gang Chen,
Department of Neurosurgery, The First Affili-
ated Hospital of Soochow University, 188 Shizi
Street, Suzhou 215006, China.
E-mail: [email protected]
Z. W. and C. M. equally contributed to this
work.
Received October 10, 2011;
Accepted January 5, 2012.
J. Pineal Res. 2012Doi:10.1111/j.1600-079X.2012.00978.x
� 2012 John Wiley & Sons A/S
Journal of Pineal Research
1
Mo
lecu
lar,
Bio
log
ical
,Ph
ysio
log
ical
an
d C
lin
ical
Asp
ects
of
Mel
ato
nin
to the nucleus and sequentially binds to ARE. Nrf2transactivates the expression of a group of cytoprotectiveenzymes, such as heme oxygenase-1 (HO-1), NAD(P)H:
quinone oxidoreductase-1 (NQO1), and glutathioneS-transferase a-1 (GST-a1) [12]. Nrf2-ARE pathway isconsidered to be a multiorgan protector and is reported toplay an important role in several central nervous system
(CNS) diseases such as SAH [13], cerebral ischemia [14],ischemia–reperfusion injury [15], traumatic brain injury[16], and intracerebral hemorrhage [17].
In the previous research regarding melatonin and Nrf2,Negi et al. [18] investigated the effects of melatonin onNrf2 activation and neuroinflammation in a model of
experimental diabetic neuropathy. They put forward thatmelatonin modulates neuroinflammation by decreasingoxidative stress by increasing Nrf2 expression, which mightbe responsible, at least in part, for its neuroprotective effect
in diabetic neuropathy. However, no study investigated theinfluence of melatonin on Nrf2 pathway in SAH models,and also little work has been carried out concerning the
effects of melatonin on brain damage during the early stageof SAH in prechiasmatic blood injection model. Thus, theaim of the current study was to determine whether
melatonin could modulate Nrf2-ARE pathway and atten-uate EBI in this rat SAH model.
Materials and methods
Animals
Male Sprague Dawley rats (300–350 g) were purchasedfrom Animal Center of Chinese Academy of Sciences,
Shanghai, China. The rats were housed in temperature- andhumidity-controlled animal quarters with a 12-hr light/darkcycle. All procedures were approved by the Institutional
Animal Care Committee and were in accordance with theguidelines of the National Institutes of Health on the careand use of animals.
Prechiasmatic cistern subarachnoid hemorrhagemodel
Following the intraperitoneal anesthesia with a mixture ofketamine (100 mg/kg) and xylazine (0.5 mg/kg), animalhead was fixed in the stereotactic frame. Experimental SAH
model was produced using stereotaxic insertion of a needlewith a rounded tip and a side hole into the prechiasmaticcistern according to our previous study [13]. The needle was
tilted 45� in the sagittal plane and placed 7.5 mm anteriorto bregma in the midline, with the hole facing the right side.It was lowered until the tip reached the base of the skull,2–3 mm anterior to the chiasma (about 10–12 mm from the
brain surface), and retracted 0.5 mm. Loss of CSF andbleeding from the midline vessels were prevented byplugging the burr hole with bone wax before inserting the
needle. The amount of 0.3 mL nonheparinized fresh auto-logous arterial blood was slowly injected into the prechias-matic cistern for 20 s with a syringe pump under aseptic
technique. Control animals were injected with 0.3 mLsaline. The animals were allowed to recover 45 min afterSAH. After operation procedures, the rats were then
returned to their cages and the room temperature kept at23 ± 1�C. Twenty millilitre of 0.9% NaCl was injectedsubcutaneously right after the operation to prevent dehy-
dration. Heart rate and rectal temperature were monitored,and the rectal temperature was kept at 37 ± 0.5�C, usingphysical cooling (ice bag) when required, throughoutexperiments. It was observed in this study that inferior
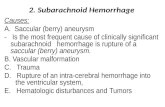
basal temporal lobe was always stained by blood. Hence,the brain tissue adjacent to the clotted blood was taken tothe analysis in our study (Fig. 1).
Experimental design
The experimental groups consisted of control group(n = 18), SAH group (n = 18), SAH + vehicle group(n = 18), and SAH + Melatonin (n = 18). In the animalsof SAH + melatonin group, melatonin (150 mg/kg diluted
in 5 mL/kg vehicle) was administered at 2 and 24 hr afterblood injection. Rats of SAH + vehicle group receivedequal volumes (5 mL/kg) of vehicle (1% ethanol in 1 mL
saline) at corresponding time points. Both melatonin andvehicle were administered intraperitoneally. The dose waschosen according to Ayer et al. [7] because they observed
beneficial effects on reducing brain water content andsubsequent mortality following SAH. All the rats werekilled on 48 hr after SAH.
Six rats in each group were sacrificed using the fixation-perfusion method. The cortex was taken for terminaldeoxynucleotidyl transferase-mediated dUTP nick endlabeling (TUNEL) method. Another six rats in each group
were exsanguinated and decollated. The brain sample wasremoved and rinsed in 0.9% normal saline (4�C) severaltimes to wash away blood and blood clot. And then, the
tissue was frozen in liquid nitrogen immediately formolecular biological and biochemical experiments. The leftsix rats in each group were for detecting blood–brain
barrier (BBB) impairment (Evens blue study).
Western blot analysis
The frozen brain samples were mechanically lysed in 20 mm
Tris, pH 7.6, which contains 0.2% SDS, 1% Triton X-100,1% deoxycholate, 1 mm phenylmethylsulphonyl fluoride,
and 0.11 IU/mL aprotinin (all purchased from Sigma-Aldrich, Inc., St. Louis, MO, USA). Lysates werecentrifuged at 12,000 g for 20 min at 4�C. The protein
concentration was estimated by the Bradford method usingthe Nanjing Jiancheng (NJJC) protein assay kit (NanjingJiancheng Bioengineering Institute, Nanjing, China). The
samples (60 lg per lane) were separated by 8% SDS-PAGEand electro-transferred onto a polyvinylidene-difluoridemembrane (Bio-Rad Lab, Hercules, CA, USA). Themembrane was blocked with 5% skimmed milk for 2 hr
at room temperature and incubated overnight at 4�C withprimary antibodies directed against Nrf2 and HO-1 (bothfrom Santa Cruz Biotechnology, Santa Cruz, CA, USA) at
the dilutions of 1:200 and 1:150, respectively. The glycer-aldehyde-3-phosphate dehydrogenase (GAPDH) (diluted in1:6000; Sigma-Aldrich, Inc.) was used as a loading control.
After the membrane was washed for 10 min each for sixtimes in PBS + Tween 20 (PBST), it was incubated in the
Wang et al.
2
appropriate horseradish peroxidase (HRP)-conjugated sec-ondary antibody (diluted 1:400 in PBST) for 2 hr. Theblotted protein bands were visualized by enhanced chemi-luminescence Western blot detection reagents (Amersham,
Arlington Heights, IL, USA) and were exposed to X-rayfilm. Developed films were digitized using an EpsonPerfection 2480 scanner (Seiko Corp, Nagano, Japan).
Optical densities were obtained using Glyko Bandscansoftware (Glyko, Novato, CA, USA). The tissue of sixanimals was used for western blot analysis at each time
point. All experiments have been repeated at least threetimes.
Immunohistochemical study
Immunohistochemistry on formalin-fixed paraffin-embed-ded sections was performed to determine the immunoreac-
tivity of Nrf2 and HO-1. Sections were deparaffinized andrehydrated in graded concentrations of ethanol to distilledwater. Endogenous peroxidase activity was blocked with
3% H2O2 for 5 min, followed by a brief rinse in distilledwater and a 15-min wash in PBS. Sections were placed in10 mm citrate buffer (pH 6.0) and heated in microwave
oven at 95�C for 30 min. Sections were cooled at roomtemperature for 20 min and rinsed in PBS. Nonspecificprotein binding was blocked by 40-min incubation in 5%horse serum. Sections were incubated with primary anti-
bodies (anti-NRf2 and anti-HO-1, both diluted 1:200;respectively, from Santa Cruz Biotechnology, Inc.) for1 hr at room temperature, followed by a 15-min wash in
PBS. Sections were incubated with HRP-conjugated IgG(1:500 dilution; Santa Cruz Biotechnology, Inc.) for 60 minat room temperature. DAB was used as chromogen, and
counterstaining was performed with hematoxylin. Sectionsincubated in the absence of primary antibody were used asnegative controls. Microscopy of the immunohistochemi-
cally stained tissue sections was performed by an experi-enced pathologist blinded to the experimental condition.The number of positively immunostained cells in eachsection was counted in 10 microscope fields (at ·200magnification) throughout the identical regions of thestudied brain, and the mean per visual field was calculated.
Quantitative real-time polymerase chain reaction
The mRNA levels of HO-1, NQO1, and GST-a1 were
determined by quantitative real-time polymerase chainreaction (PCR). Total cellular RNA was isolated fromsample brain using Trizol Reagents (Invitrogen Life Tech-
nologies, Carlsbad, CA, USA) as per the manufacturer�sdirection. RNA quality was insured by gel visualization andspectrophotometric analysis (OD260/280). The quantity ofRNA was measured using the OD260. RNA was transcribed
to cDNA using MMLV Reverse Transcriptase (Promega,Madison, WI, USA) and oligo dT primers. The primerswere synthesized by Kangcheng Biotechnology (Shanghai,
China) and were shown in Table 1. Quantitative real-timePCR analysis was performed by using the Rotor-Gene�3000 real-time DNA analysis system (Corbett Research,
Sydney, Australia), applying real-time SYBR Green PCRtechnology. The reaction mixtures contained dilutedcDNA, SYBR Green I Nucleic Acid Stain (Invitrogen LifeTechnologies), 20 lm of each gene-specific primer, and
nuclease-free water to a final volume of 25 lL. Test cDNAresults were normalized to b-actin measured on the sameplate. All samples were analyzed in triplicate.
Brain water content
Brain edema was determined using the wet/dry method aspreviously described where % brain water = [(wetweight ) dry weight)/wet weight] · 100% [7]. Briefly, brain
(A) (B)
Fig. 1. Schematic representation of the areas taken for assay.
Melatonin and Nrf2-ARE pathway in SAH
3
samples were rapidly removed from the skull and placedseparately into preweighed and labeled glass vials andweighed. The vials were then placed in an oven for 72 hr at100�C and then re-weighed to obtain dry weight content.
Blood–brain barrier permeability
Blood–brain barrier permeability was determined by Evansblue (EB) extravasation at 48 hr after SAH. Briefly, 2% EBwas injected intravenously at a dose of 2 mL/kg. Animals
were then re-anesthetized after 1 hr with urethane(1000 mg/kg) and perfused using saline to remove intra-vascular EB dye. Animals were then decapitated, and the
brains removed and homogenized in phosphate-bufferedsaline. Trichloroacetic acid was then added to precipitateprotein, and the samples were cooled and centrifuged. Theresulting supernatant was measured for absorbance of EB
at 610 nm using a spectrophotometer.
Terminal deoxynucleotidyl transferase-mediateddUTP nick end labeling staining and quantitation ofapoptotic cells
The formalin-fixed tissues were embedded in paraffinand sectioned at 4 lm thickness with a microtome. Thesections were detected for apoptotic cells by TUNELmethod. TUNEL: in situ cell death detection kit POD
(ISCDD; Boehringer Mannheim, Germany) was used.The procedures were according to the protocol of the kitand our previous study [13]. The positive cells were
identified, counted, and analyzed under the light micro-scope by an investigator blinded to the grouping. Theextent of brain damage was evaluated by apoptotic index,
which was the average number of TUNEL-positive cellsin each section counted in 10 microscopic fields (at ·200magnifications).
Neurologic scoring
Three behavioral activity examinations (Table 2) were
performed at 48 hr after SAH using the scoring systemreported previously to record appetite, activity, and neuro-logical deficits [19].
Statistical analysis
All data were presented as mean ± S.E.M. SPSS 12.0 wasused for statistical analysis of the data. The Mann–WhitneyU-test was used to compare the behavior and activity scoreamong groups. The other measurements were analyzed by
one-way analysis of variance (ANOVA) or Student�s t-test.Statistical significance was inferred at P < 0.05.
Results
There were no significant differences in body weight,temperature, or injected arterial blood gas data among
the experimental groups (data not shown). After theinduction of SAH, all animals will stop breathing for about30 s. Sixteen rats died after blood injection, and the
mortality in SAH animals is 16/70 (23%).Fig. 2 showed low levels of Nrf2 and HO-1 in control
group. On day 2 (48 hr) after SAH, the levels of Nrf2 and
HO-1 were significantly increased in SAH group andSAH + vehicle group compared with control rats (P <0.05) (Fig. 2). There was no statistically significant differ-ence between SAH group and SAH + vehicle group (P >
0.05) (Fig. 2). After melatonin injections, the increasedexpression of Nrf2 and HO-1 was markedly further inducedin animals of SAH + melatonin group (P < 0.01) (Fig. 2).
Immunohistochemical study showed that positive Nrf2and HO-1 were mainly located at the neurons, with littleexpression at glial cells. The immunoreactivity of Nrf2 and
HO-1 was weak in the cortex samples in control group withonly a few Nrf2- or HO-1-positive cells in the brain (Figs 3and 4). More Nrf2 and HO-1 positively immunostainedneurons appeared in SAH group and SAH + vehicle group
(Figs 3 and 4). In SAH + melatonin group, the number ofNrf2- or HO-1-positive cells was more than SAH + vehiclegroup (Figs 3 and 4). Both Nrf2 and HO-1 immunoreac-
tivities of parenchymal cells in the cortex were progressivelyinduced by melatonin therapy at 48 hr after blood injection(P < 0.01).
The mRNA of these proteins expressed at a low level inthe rat brains of control group. The levels of HO-1, NQO1,and GST-a1 mRNA were significantly increased in the
Table 1. Polymerase chain reaction primer sequences
Targetgenes Sense primer (5¢–3¢) Antisense primer (5¢–3¢)
Annealingtemperature (�C)
Numberof cycles Size (bp)
NQO1 GCGTCTGGAGACTGTCTGGG CGGCTGGAATGGACTTGC 60 40 170HO-1 GCGAAACAAGCAGAACCCA GCTCAGGATGAGTACCTCCCA 58 40 185GST-a1 CGGTACTTGCCTGCCTTTG ATTTGTTTTGCATCCACGGG 59 40 248b-actin CCCATCTATGAGGGTTACGC TTTAATGTCACGCACGATTTC 60 40 150
GST-a1, glutathione S-transferase a-1; HO-1, heme oxygenase-1; NQO1, NAD(P)H: quinone oxidoreductase-1.
Table 2. Behavior and activity scores
Category Behavior Score
Appetite Finished meal 0Left meal unfinished 1Scarcely ate 2
Activity Walk and reach at leastthree corners of the cage
0
Walk with some stimulations 1Almost always lying down 2
Deficits No deficits 0Unstable walk 1Impossible to walk 2
Wang et al.
4
cortex in SAH and SAH + vehicle groups as comparedwith that of control group (P < 0.01). The mRNAexpressions had no significant difference between SAHgroup and SAH + vehicle group (P > 0.05). The mRNA
expressions of HO-1, NQO1, and GST-a1 in the brains ofSAH + melatonin group were significantly up-regulatedthan those of the SAH + vehicle group (Fig. 5).
As shown in Fig. 6, the concentration of NQO1 andGST-a1 was low in the rat brain of control group.Compared with control group, cortical levels of these
antioxidant and detoxifying enzymes were greatly inducedafter SAH (P < 0.01). Melatonin administration afterSAH could lead to significantly increased NQO1 andGST-a1 activity in rat brain tissue (P < 0.05).
Significant increase (P < 0.05) in water content wasdetected in the brain samples at 48 hr after SAH whencompared with rats in control group (Fig. 7). The mean
value of brain water content in the cortex was decreased bymelatonin administration (P < 0.05) as compared withSAH + vehicle group.
The pattern of EB extravasation following SAH is shownin Fig. 8. Rats in SAH or SAH + vehicle group demon-strated a significant increase (P < 0.01) in BBB permeabil-ity to EB relative to rats of control group. Administration
of melatonin significantly inhibited EB extravasation(P < 0.05) after SAH.Few TUNEL-positive apoptotic cells were found in the
control group rat brains (Fig. 9A). In SAH andSAH + vehicle groups, the apoptotic index in the cortexwas found to be significantly increased compared with that
in control animals (P < 0.01) (Fig. 9B,C). There was nostatistically significant difference between SAH group andSAH + vehicle group (P > 0.05). In SAH + melatonin
group, when compared with that in the SAH + vehiclegroup, the apoptotic index in the studied cortex wassignificantly decreased (P < 0.01) (Fig. 9D).As compared with control group, clinical behavior
function impairment caused by SAH was evident in SAHsubjects (P < 0.01, Table 3). No significant difference wasseen between the SAH group and SAH + vehicle group
(P > 0.05). Melatonin-treated rats showed better perfor-mance in this scale system than vehicle-treated rats at 24 hrafter SAH (Table 3), and the difference was statistically
significant (P < 0.01, Table 3).
Discussion
Early brain injury is the most common cause of disabilityand death in patients suffering from aneurysmal SAH [20].
Fig. 2. Expressions of nuclear factor erythroid 2-related factor 2(Nrf2) and heme oxygenase-1 (HO-1) in the brain samples incontrol group (n = 6), subarachnoid hemorrhage (SAH) group(n = 6), SAH + vehicle group (n = 6), and SAH + melatoningroup (n = 6). Upper, Representative autoradiogram of the pro-teins expression following SAH by western blot. We detected Nrf2at 68 kDa, HO-1 at 31.7 kDa, and the loading control GAPDH at37 kDa. Lane 1, control group; Lane 2, SAH group; Lane 3,SAH + vehicle group; Lane 4, SAH + melatonin group. Bottom,Quantitative analysis of the western blot results for the expressionof Nrf2 and HO-1. The expression of Nrf2 and HO-1 was signifi-cantly increased in the animals of SAH and SAH + vehicle groupscompared with the control group (P < 0.05). The increased levelwas markedly up-regulated in SAH + melatonin group(P < 0.01). Bars represent the mean ± S.E.M. *P < 0.05 com-pared with control group; NSP > 0.05 compared with SAH group;##P < 0.01 compared with SAH + vehicle group.
Fig. 3. Immunohistochemical study of nuclear factor erythroid 2-related factor 2 (Nrf2) and heme oxygenase-1 (HO-1) on brain samples.Few Nrf2- and HO-1-positive cells were observed in the control group, which indicates the constitutional activation of Nrf2-ARE pathwayin the normal cortex of rats. Increased Nrf2- and HO-1-positive cells (arrows) stained as brown could be found in the brain of the rats in thesubarachnoid hemorrhage (SAH) groups. Further up-regulated Nrf2 and HO-1 immunoreactivities (arrows) were observed in the neuronsof SAH brains treated with melatonin (scar bar, 50 lm). ARE, antioxidant responsive element.
Melatonin and Nrf2-ARE pathway in SAH
5
Treatment of EBI is considered as a major goal in themanagement of patients surviving SAH. However, the exactmolecular mechanism of EBI still remains obscure, whichhas hindered the development of effective and specific
treatment paradigms for EBI. The term EBI refers to theimmediate injury to the brain as a whole, within the first48 hr of the ictus, secondary to SAH [21]. The possible
mechanisms about EBI may include: the elevation ofintracranial pressure, reduction in cerebral blood flow(CBF), suppression of cerebral perfusion pressure, fall in
brain oxygenation, BBB breakdown, brain edema, and
Fig. 5. The mRNA expressions of heme oxygenase-1 (HO-1),NAD(P)H: quinone oxidoreductase-1 (NQO1), and glutathione S-transferase a-1 (GST-a1) in the brains in control group (n = 6),subarachnoid hemorrhage (SAH) group (n = 6), SAH + vehiclegroup (n = 6), and SAH + melatonin group (n = 6). SAH couldinduce a marked increase in HO-1, NQO1, and GST-a1 mRNAexpression in the rat SAH brains compared with control group.After melatonin administration, the mRNA expressions of Nrf2-ARE pathway-related agents were significantly up-regulated ascompared with SAH + vehicle group. **P < 0.01 versus controlgroup, ##P < 0.01 versus SAH + vehicle group, NSP > 0.05versus SAH group. Nrf2-ARE, nuclear factor erythroid 2-relatedfactor 2 and antioxidant responsive element.
Fig. 6. Changes in NAD(P)H: quinone oxidoreductase-1 (NQO1)and glutathione S-transferase a-1 (GST-a1) enzymes activity in thebrain as determined by biochemical tests in control group (n = 6),subarachnoid hemorrhage (SAH) group (n = 6), SAH + vehiclegroup (n = 6), and SAH + melatonin group (n = 6). SAH couldinduce the significantly increased activity of NQO1 and GST-a1 inrat brain tissue. In SAH + melatonin group, the cortical activityof NQO1 and GST-a1 was markedly up-regulated as comparedwith that of SAH + vehicle group. **P < 0.01 versus controlgroup; #P < 0.05 and ##P < 0.01 versus control group;NSP > 0.05 compared with SAH group.
Fig. 7. Alterations in brain water content in control group(n = 6), subarachnoid hemorrhage (SAH) group (n = 6),SAH + vehicle group (n = 6), and SAH + melatonin group(n = 6). The brain water content was increased significantly at48 hr after SAH. Melatonin treatment markedly reduced brainwater content. No difference of brain water content was detectedbetween SAH and SAH + vehicle groups *P < 0.05 versus con-trol group, #P < 0.05 versus SAH + vehicle group, NSP > 0.05versus SAH group.
Fig. 8. Alterations in Evans blue (EB) extravasation in controlgroup (n = 6), subarachnoid hemorrhage (SAH) group (n = 6),SAH + vehicle group (n = 6), and SAH + melatonin group(n = 6). SAH could induce a marked increase in blood–brainbarrier extravasation in the rat brain compared with control group.After melatonin administration, the EB extravasation was signifi-cantly reduced as compared with SAH + vehicle group.**P < 0.01 versus control group, ##P < 0.01 versusSAH + vehicle group, NSP > 0.05 versus SAH group.
Fig. 4. Quantitative analysis showed the low percentage of nuclearfactor erythroid 2-related factor 2 (Nrf2) and heme oxygenase-1(HO-1) in the control group. In contrast, the level of Nrf2 and HO-1 activation was increased in the subarachnoid hemorrhage (SAH)and SAH + vehicle groups. After melatonin therapy, both pro-teins were progressively activated in the treatment group. Barsrepresent the mean ± S.E.M. (n = 6, each group). **P < 0.01compared with control group, ##P < 0.05 compared withSAH + vehicle group.
Wang et al.
6
neuronal cell death [22], among which oxidative stressplayed an important role in the pathogenesis of EBI [23].
Several researchers have reported the neuro-protectiveproperties of melatonin in different models of SAH. In
cisterna magna SAH model, melatonin treatment reversedmalondialdehyde, GSH, myeloperoxidase, and Na+-K+-ATPase activities and the formation of reactive oxygenspecies as well as SAH-induced histopathological altera-
tions, while increased brain water content, impaired BBB,and cerebral vasospasm were also reversed by melatonintreatment [6, 8, 10]. However, this model was not appro-
priate for EBI research, because the brain injury was mostlyrelated to severe vasospasm of basilar artery. In contrast infilament perforation SAH model, data from another team
demonstrated that melatonin (150 mg/kg i.p.) tended toreduce brain water content following SAH but had no effecton the lipid peroxidation of brain samples. Their result
suggested that melatonin significantly reduced mortalityand brain water content in rats following SAH through amechanism unrelated to oxidative stress [7]. Nevertheless,no data were found related to the effect of melatonin on
(A) (B)
(C) (D)
Fig. 9. Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) immunohistochemistry staining of the cortex incontrol group (n = 6), subarachnoid hemorrhage (SAH) group (n = 6), SAH + vehicle group (n = 6), and SAH + melatonin group(n = 6). (A) control group rats showing few TUNEL apoptotic cells; (B) SAH group rats showing strong TUNEL staining; (C)SAH + vehicle group rats showing more TUNEL apoptotic cells stained as brown; (D) SAH + melatonin group rats showing lessTUNEL apoptotic cells than SAH or SAH + vehicle group (scar bar, 50 lm). Administration of melatonin significantly decreased theapoptotic index in rat brain following SAH. **P < 0.01 versus control group, ##P < 0.01 versus SAH + vehicle group, NSP > 0.05versus SAH group.
Table 3. Clinical behavior scores in each group
Group Mean score
Control (n = 18) 0.53SAH (n = 18) 2.67**SAH + vehicle (n = 18) 2.72NS
SAH + Melatonin (n = 18) 1.33##
**P < 0.01 compared with control group.NSP > 0.05 compared with SAH group.##P < 0.01 compared with SAH + vehicle group.SAH, subarachnoid hemorrhage.
Melatonin and Nrf2-ARE pathway in SAH
7
EBI in prechiasmatic SAH model, and also the insidemechanism remains unknown.In the current study, we used a modified model created
by Prunell et al. [24–26] in previous studies, which has alsoproven that this prechiasmatic SAH model was the mostsuitable for studies of the pathological and pathophysio-logical processes of SAH after comparison with intracranial
endovascular perforation SAH model and cisterna magnaSAH model. The prechiasmatic SAH model could induce asignificant acute reduction in CBF, combined with a
substantial degree of neuronal death. The mortality rate isacceptable, and the procedure is reproducible and easy toperform [26]. In the present research, we found that Nrf2-
ARE pathway was activated in the cortex during early stageof SAH in rats and could be further up-regulated bythe administration of melatonin, which could increase theexpressions of antioxidant and detoxifying enzymes. At the
same time, after melatonin administration, the brainedema, BBB permeability, and apoptotic cell death wereameliorated. Most of our data were in agreement with the
previous studies from other SAH research teams, but webelieve that different models could be a reason to explaindissimilar results.
In the previous research regarding melatonin and Nrf2-ARE pathway, Crespo et al. [27] investigated the effects ofmelatonin on oxidative stress and Nrf2-ARE pathway in an
animal model of fulminant hepatic failure. They putforward the idea that melatonin treatment resulted in anincreased protein expression of Nrf2 in the cytoplasm andthe nucleus and played a potential hepatoprotective role in
fulminant hepatic failure, partially mediated through theabrogation of oxidative stress and the prevention of thedecreased activity of antioxidant enzymes via the Nrf2-
ARE pathway. Similarly, as mentioned by Tripathi et al.[28] in their literature, they investigated the influence ofmelatonin on urotoxicity associated with cyclophospha-
mide chemotherapy in patients with cancer and found thatmelatonin treatment favorably changed Nrf2 expression,which appeared to be, at least in part, responsible for
observed protection against cyclophosphamide-inducedurotoxicity. In this study, administration of melatoninresulted in significant increase in SAH-induced cerebralexpression and enzymatic activity of the ARE-mediated
down-stream factors HO-1, NQO1 and GST-a1 at bothpretranscriptional and posttranscriptional levels. Thesedata are in agreement with the finding of the previous
reports illustrating the activating effects of melatonin onNrf2 and its target genes [27, 28].Numerous studies have linked melatonin to anti-inflam-
matory and antiapoptotic effects, the amelioration ofmitochondrial dysfunction, protection against excitotoxic-ity, and the stimulation of neuroprotective signaling path-ways [29–31]. These alternate pathways warrant further
study. The mechanisms by which melatonin induced theexpression of Nrf2 and HO-1 are not explained in thiswork. Four major mechanisms have been suggested to be
involved in the actions of melatonin, i.e., binding tomembrane receptors [32], binding to nuclear receptors[33], interactions with cytoplasmic proteins [34], and
scavenging free radicals [35]. However, because Nrf2 andHO-1 expression increases in response to various insults
including oxidative stress, melatonin should prevent theoxidative stress induced by SAH as a result of itsantioxidant scavenging properties. Although the present
study has demonstrated that melatonin supplementationactivated the SAH-induced cerebral Nrf2 up-regulation,changes about the melatonin metabolism after SAH andthe whole signaling pathway in the brain remain unknown.
Further ingenious studies are needed some of which will beconducted in our laboratory.In summary, to the best of our knowledge, this is the first
study to demonstrate the effects of melatonin on the SAH-induced cerebral pathophysiological changes in prechias-matic cistern SAH model. We found that melatonin
administration resulted in the magnification of Nrf2-AREpathway and diminution of the degree of EBI followingSAH. Moreover, the mRNA expressions and activities ofantioxidant and detoxifying enzymes were up-regulated by
the administration of melatonin. The therapeutic benefit ofpost-SAH melatonin administration might be due to itssalutary effect on modulating cerebral Nrf2-ARE pathway
and antioxidant signaling.
Acknowledgements
This work was supported by grants from the NationalNatural Science Foundation of China (No. 81171105 and
81100872), Jiangsu Province�s Outstanding Medical Aca-demic Leader program (NO. LJ201139), a special grantfrom the China Postdoctoral Science Foundation (No.201104540), and grants from Education Department of
Jiangsu Province (No. 11KJB320011) and Suzhou Govern-ment (No. SYS201109).
References
1. Tan DX, Chen LD, Poeggeler B, Manchester LC,
Reiter RJ. Melatonin: a potent, endogenous hydroxyl radical
scavenger. Endocr J 1993; 1:57–60.
2. Tan DX, Manchester LC, Sanchez-Barcelo E, Media-
villa MD, Reiter RJ. Significance of high levels of endoge-
nous melatonin in Mammalian cerebrospinal fluid and in the
central nervous system. Curr Neuropharmacol 2010; 8:162–
167.
3. Bonnetfont-Rousselot D, Collin F, Jore D, Gardes-
Albert M. Reaction mechanism of melatonin oxidation
by reactive oxygen species in vitro. J Pineal Res 2011; 50:328–
335.
4. Galano A, Tan DX, Reiter RJ. Melatonin as a natural ally
against oxidative stress: a physicochemical examination.
J Pineal Res 2011; 51:1–16.
5. Luchetti F, Canonico B, Betti M et al. Melatonin signaling
and cell protection function. FASEB J 2010; 24:3603–3624.
6. Ersahin M, Toklu HZ, Cetinel S, Yuksel M, Yegen BC,
Sener G. Melatonin reduces experimental subarachnoid
hemorrhage-induced oxidative brain damage and neurological
symptoms. J Pineal Res 2009; 46:324–332.
7. Ayer RE, Sugawara T, Chen W, Tong W, Zhang JH.
Melatonin decreases mortality following severe subarachnoid
hemorrhage. J Pineal Res 2008; 44:197–204.
8. Aydin MV, Caner H, Sen O et al. Effect of melatonin on
cerebral vasospasm following experimental subarachnoid
hemorrhage. Neurol Res 2005; 27:77–82.
Wang et al.
8
9. Martinez-Cruz F, Espinar A, Pozo D, Osuna C, Guer-
rero JM. Melatonin prevents focal rat cerebellum injury as
assessed by induction of heat shock protein (HO-1) following
subarachnoid injections of lysed blood. Neurosci Lett 2002;
331:208–210.
10. Fang Q, Chen G, Zhe W, Dong W, Wang Z. Influence of
melatonin on cerebrovascular proinflammatory mediators
expression and oxidative stress following subarachnoid hem-
orrhage in rabbits. Mediators Inflamm 2009; 2009:426346.
11. Lee JM, Johnson JA. An important role of Nrf2-ARE path-
way in the cellular defense mechanism. J Biochem Mol Biol
2004; 37:139–143.
12. Rigg JL, Elovic EP, Greenwald BD. A review of the
effectiveness of antioxidant therapy to reduce neuronal damage
in acute traumatic brain injury. J Head Trauma Rehabil 2005;
20:389–391.
13. Chen G, Fang Q, Zhang J, Zhou D, Wang Z. Role of the
Nrf2-ARE pathway in early brain injury after experimental
subarachnoid hemorrhage. J Neurosci Res 2011; 89:515–523.
14. Shih AY, Li P, Murphy TH. A small-molecule-inducible
Nrf2-mediated antioxidant response provides effective pro-
phylaxis against cerebral ischemia in vivo. J Neurosci 2005;
25:10321–10335.
15. Leonard MO, Kieran NE, Howell K et al. Reoxygenation-
specific activation of the antioxidant transcription factor Nrf2
mediates cytoprotective gene expression in ischemia-reperfu-
sion injury. FASEB J 2006; 20:2624–2626.
16. Jin W, Wang H, Yan W et al. Role of Nrf2 in protection
against traumatic brain injury in mice. J Neurotrauma 2009;
26:131–139.
17. Zhao X, Sun G, Zhang J et al. Transcription factor Nrf2
protects the brain from damage produced by intracerebral
hemorrhage. Stroke 2007; 38:3280–3286.
18. Negi G, Kumar A, Sharma SS. Melatonin modulates neur-
oinflammation and oxidative stress in experimental diabetic
neuropathy: effects on NF-jB and Nrf2 cascades. J Pineal Res
2011; 50:124–131.
19. Yamaguchi M, Zhou C, Nanda A, Zhang JH. Ras protein
contributes to cerebral vasospasm in a canine double-hemor-
rhage model. Stroke 2004; 35:1750–1755.
20. Cahill J, Calvert JW, Zhang JH. Mechanisms of early
brain injury after subarachnoid hemorrhage. J Cereb Blood
Flow Metab 2006; 26:1341–1353.
21. Ostrowski RP, Colohan AR, Zhang JH. Molecular mech-
anisms of early brain injury after subarachnoid hemorrhage.
Neurol Res 2006; 28:399–414.
22. Cahill J, Zhang JH. Subarachnoid hemorrhage: is it time for
a new direction? Stroke 2009; 40:S86–S87.
23. Ayer RE, Zhang JH. Oxidative stress in subarachnoid
haemorrhage: significance in acute brain injury and vaso-
spasm. Acta Neurochir Suppl 2008; 104:33–41.
24. Prunell GF, Mathiesen T, Svendgaard NA. A new
experimental model in rats for study of the pathophysiology of
subarachnoid hemorrhage. Neuroreport 2002; 13:2553–2556.
25. Prunell GF, Svendgaard NA, Alkass K, Mathiesen T.
Inflammation in the brain after experimental subarachnoid
hemorrhage. Neurosurgery 2005; 56:1082–1092.
26. Prunell GF, Mathiesen T, Svendgaard NA. Experimental
subarachnoid hemorrhage: cerebral blood flow and brain
metabolism during the acute phase in three different models in
the rat. Neurosurgery 2004; 54:426–436.
27. Crespo I, Miguel BS, Laliena A et al. Melatonin prevents
the decreased activity of antioxidant enzymes and activates
nuclear erythroid 2-related factor 2 signaling in an animal
model of fulminant hepatic failure of viral origin. J Pineal Res
2010; 49:193–200.
28. Tripathi DN, Jena GB. Effect of melatonin on the expression
of Nrf2 and NF-kappaB during cyclophosphamide-induced
urinary bladder injury in rat. J Pineal Res 2010; 48:324–331.
29. Yon JH, Carter LB, Reiter RJ, Jevtovic-Todorovic V.
Melatonin reduces the severity of anesthesia-induced apoptotic
neurodegeneration in the developing rat brain. Neurobiol Dis
2006; 21:522–530.
30. Leon J, Acuna-Castroviejo D, Escames G, Tan DX,
Reiter RJ. Melatonin mitigates mitochondrial malfunction.
J Pineal Res 2005; 38:1–9.
31. Kilic U, Kilic E, Reiter RJ, Bassetti CL, Hermann DM.
Signal transduction pathways involved in melatonin-induced
neuroprotection after focal cerebral ischemia in mice. J Pineal
Res 2005; 38:67–71.
32. Garcia-Pergan A, Pozo D, Guerrero JM, Calvo JR. Sig-
nal transduction for melatonin in human lymphocytes:
involvement of a pertussis toxin-sensitive G protein. J Immu-
nol 1997; 159:3774–3781.
33. Garcia-Maurin S, Pozo D, Calvo JR, Guerrero JM.
Correlation between nuclear melatonin receptors expression
and enhanced cytokine production in human lymphocytic and
monocytic cell lines. J Pineal Res 2000; 29:129–137.
34. Pozo D, Reiter RJ, Calvo JR, Guerrero JM. Inhibition of
cerebellar nitric oxide synthase and cyclic GMP production by
melatonin via complex formation with calmodulin. J Cell
Biochem 1997; 65:430–442.
35. Reiter RJ. Melatonin: lowering the high price of free radicals.
News Physiol Sci 2000; 15:246–250.
Melatonin and Nrf2-ARE pathway in SAH
9