Medication Summary - 123seminarsonly.com€¦ · Web viewAxillary or sentinel lymph node...
Transcript of Medication Summary - 123seminarsonly.com€¦ · Web viewAxillary or sentinel lymph node...

0Background
Worldwide, breast cancer is the most frequently diagnosed life-threatening cancer in women and the leading cause of cancer death among women.
Many early breast carcinomas may be asymptomatic; pain or discomfort is not usually a symptom of breast cancer.
o Breast cancer is often first detected as an abnormality on a mammogram before it is felt by the patient or healthcare provider.
o The general approach to evaluation of breast cancer: triple assessment: clinical examination, imaging (usually mammography and/or
ultrasonography), and needle biopsy Surgery is considered primary treatment for breast cancer.
o Many patients with early-stage breast cancer are cured with surgery alone.
Anatomy
1. Chest wall2. Pectoralis muscles3. Lobules4. Nipple5. Areola6. Milk duct7. Fatty tissue8. Skin
The basic units of the breast are the terminal duct lobular units (TDLUs), which produce the fatty breast milk.
o Two-thirds of the lactiferous tissue is within 30-mm of the base of the nipple. o The terminal lactiferous ducts drain the milk from TDLUs into 4–18 lactiferous ductswhich
drain to the nipple the milk-glands-to-fat ratio is 2:1 in a lactating woman 1:1 in a non-lactating woman.
o Connective tissues (collagen, elastin), white fat, and the suspensory Cooper's ligaments. o Sensation in the breast is provided by the peripheral nervous system innervation, by means of the
front anterior and lateral cutaneous branches of the fourth-, the fifth-, and the sixth intercostal nerves
o T-4 nerve , which innervates the dermatomic area, supplies sensation to the nipple-areola complex.

Pectoralis major muscles o extend from the level of the second rib to the level of the sixth rib in the front of the human rib
cage Breast tissue can extend from the clavicle to the middle of the sternum
o At the sides of the chest, the breast tissue can extend into the axilla and can reach as far to the back as the latissimus dorsi muscle, extending from the lower back to the humerus bone
The superficial tissue layer (superficial fascia) is separated from the skin by 0.5–2.5 cm of subcutaneous fat (adipose tissue).
The suspensory Cooper’s ligaments are fibrous-tissue prolongations that radiate from the superficial fascia to the skin envelope.
The adult breast contains 14–18 irregular lactiferous lobes that converge to the nipple, to ducts 2.0–4.5 mm in diameter; lactiferous ducts are immediately surrounded with dense connective tissue that functions as a support framework.
The glandular tissue of the breast is biochemically supported with estrogeno when a woman reaches menopause and her body estrogen levels decrease
milk gland tissue then atrophies resulting in a breast composed of adipose tissue, superficial fascia, suspensory ligaments, and the skin envelope.
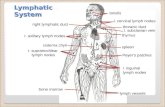
75 per cent of the lymph from the breast travels to the ipsilateral axillary lymph nodeso The axillary lymph nodes include the pectoral, subscapular, and humeral lymph-node groups,
which drain to the central axillary lymph nodes and to the apical axillary lymph nodes. 25 per cent of the lymph travels to the parasternal nodes, to the other breast, and to the abdominal lymph
nodes


Epidemiology Over the past 25 years, breast cancer incidence rates have risen globally, with the highest rates in
Westernized countries. o Reasons for this trend include change in reproductive patterns, increased screening, dietary
changes, and decreased activity. In the US:
o 207,090 new cases of female invasive breast cancer were predicted to occur in 2010 & 1,970 cases in men.
o In addition to invasive breast cancer54,010 new cases of in situ breast cancer were expected to occur among women 85% were expected to be ductal carcinoma in situ (DCIS).
The current lifetime risk of breast cancer in the US is estimated at 12.7% for all women, 13.3% for non-Hispanic whites, and 9.98% for black women.
o black women are more likely than white women to be diagnosed with larger, advanced-stage tumors (>5 cm).
The various types of breast cancers are listed below by percentage of cases:
Infiltrating ductal carcinoma is the most commonly diagnosed breast tumor and has a tendency to metastasize via lymphatics; this lesion accounts for 75% of breast cancers
Approximately 64,000 cases of DCIS are diagnosed annually in the US Over the last 25 years, lobular carcinoma in situ (LCIS) incidence has doubled and is currently 2.8 per
100,000 women; the peak incidence is in women aged 40-50 years Infiltrating lobular carcinoma comprises less than 15% of invasive breast cancers Medullary carcinoma accounts for about 5% of cases and generally occurs in younger women Mucinous (colloid) carcinoma is seen in fewer than 5% of invasive breast cancer cases. Tubular carcinoma of the breast is comprises 1-2% of all breast cancers Papillary carcinoma is usually seen in women older than 60 years and accounts for approximately 1-2%
of all breast cancers Metaplastic breast cancer accounts for less than 1% of breast cancer cases, tends to occur in older
women (average age of onset in the sixth decade), and has a higher incidence in blacks Mammary Paget disease comprises 1-4% of all breast cancers and has a peak incidence in the sixth
decade of life (mean age, 57 y)

History Many early breast carcinomas are asymptomatic, particularly if they were discovered during a breast-
screening program. Larger tumors may present as a painless mass. 5% of patients with a malignant mass present with breast pain.
Risk Factors Estimated Relative RiskAdvanced age >4Family history
Family history of ovarian cancer in women < 50y >5
One first-degree relative >2
Two or more relatives (mother, sister) Ashkenazi Jewish descent
>5>2
Personal history Personal history 3-4
Positive BRCA1/BRCA2 mutation >4
Breast biopsy with atypical hyperplasia 4-5
Breast biopsy with LCIS or DCIS 8-10
Reproductive history Early age at menarche (< 12 y) 2
Late age of menopause 1.5-2
Late age of first term pregnancy (>30 y)/nulliparity 2
Use of combined estrogen/progesterone HRT 1.5-2Current or recent use of oral contraceptives 1.25Lifestyle factors
Adult weight gain 1.5-2
Sedentary lifestyle
Alcohol Consumption
1.3-1.5
1.5

Breast cancer showing an inverted nipple, lump and skin dimpling
Histology Breast cancers usually are epithelial tumors of ductal or lobular origin. The following features are all important in deciding on a course of treatment for any breast tumor:
Size Status of surgical margin Presence or absence of estrogen receptors and progesterone receptors Nuclear and histologic grade DNA content S-phase fraction Vascular invasion Tumor necrosis Quantity of intraductal component
Histologic grade
Histologic grade is the best predictor of disease prognosis in carcinoma in situ, but it is dependent on the grading system used
o ex. Van Nuys classification (high-grade, low-grade comedo, low-grade noncomedo) The grading of invasive carcinoma is also important as a prognostic indicator, with higher grades
indicating a worse prognosis.
Grading System in Invasive Breast Cancer (Modified Bloom and Richardson)

Score1 2 3
A. Tubule formation >75% 10-75% < 10%
B. Mitotic count per high-power field (microscope- and field-dependent)
< 7 7-12 >12
C. Nuclear size and pleomorphism Near normalLittle variation
Slightly enlargedModerate variation
Markedly enlargedMarked variation
10 year survival 85% Grade I cancer if the total score (A + B + C) is 3-510 year survival 65% Grade II cancer if the total score (A + B + C) is 6 or 710 year survival 45% Grade III cancer if the total score (A + B + C) is 8 or 9
Ductal carcinoma in situ
Screening mammography has resulted in a dramatic increase in the detection of DCIS.

o Approximately 64,000 cases of DCIS are diagnosed annually in the US. o Ninety percent of DCIS cases are identified on mammography as suspicious calcifications,
linear, clustered, segmental, focal, or mixed distribution. DCIS is divided into comedo (ie, cribriform, micropapillary, solid) and noncomedo subtypes
o provides additional prognostic information on the likelihood of progression or local recurrence
Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
Breast cancer. Intraductal carcinoma, noncomedo type. Distended duct with intact basement membrane, micropapillary, and early cribriform growth pattern.
Ductal Carcinoma in Situ Subtypes
DCIS Characteristic Comedo NoncomedoNuclear grade High LowEstrogen receptor Negative PositiveHER2 overexpression Present AbsentDistribution Continuous MultifocalNecrosis Present AbsentLocal recurrence High LowPrognosis Worse Better

Lobular carcinoma in situ
Approximately, 10-20% of women with LCIS develop invasive breast cancer within 15 years after their LCIS diagnosis.
LCIS arises from the terminal duct apparatus and shows a rather diffuse distribution throughout the breast
o which explains its presentation as a nonpalpable mass in most caseso Over the last 25 years, LCIS incidence has doubled and is currently 2.8 per 100,000 women.
The peak incidence is in women aged 40-50 years.
Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells. Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells.
Infiltrating ductal carcinoma
Infiltrating ductal carcinoma is the most commonly diagnosed breast tumor and has a tendency to metastasize via lymphatics.
This lesion, which accounts for 75% of breast cancers, has no specific histologic characteristics other than invasion through the basement membrane
DCIS is a frequently associated finding on pathologic examination.
Infiltrating ductal carcinoma. Low-grade carcinoma with well-developed glands invading the fibrous stroma.


Infiltrating lobular carcinoma
Infiltrating lobular carcinoma has a much lower incidence and comprises less than 15% of invasive breast cancer.
It is characterized histologically by the “Indian file” arrangement of small tumor cells. Like ductal carcinoma, infiltrating lobular carcinoma typically metastasizes to axillary lymph nodes
first. However, it also has a tendency to be more multifocal.
o Despite this, the prognosis is comparable to that of ductal carcinoma.
Medullary carcinoma
Roughly 30% of patients have lymph node metastasis. Medullary carcinoma is relatively uncommon (5%)
o Generally occurs in younger women. Most patients present with a bulky palpable mass with axillary lymphadenopathy.
o Diagnosis of this type of breast cancer depends on the following histologic triad:
1. Sheets of anaplastic tumor cells with scant stroma
2. Moderate or marked stromal lymphoid infiltrate
3. Histologic circumscription or a pushing border
DCIS may be observed in the surrounding normal tissues. ER, PR, and HER2 are typically negative, and TP53 is commonly mutated.
Mucinous carcinoma
Mucinous (colloid) carcinoma is another rare histologic type seen in fewer than 5% of invasive breast cancer cases.
It usually presents during the seventh decade of life as a palpable mass or appears mammographically as a poorly defined tumor with rare calcifications.
Mucin production is the histologic hallmark with 2 main forms:o type A and B, with AB lesions possessing features of both. o Type A mucinous carcinoma represents the classic variety with larger quantities of extracellular
mucin o Type B is a distinct variant with endocrine differentiation.
DCIS is not a frequent occurrence, although it may be found. Most cases are ER- and PR-positive, but HER2 overexpression is rare. Additionally, these carcinomas predominantly express glycoproteins MUC2 and MUC6. Overall, patients with mucinous carcinoma have an excellent prognosis (>80% 10-year survival).
Type AColloid (mucinous) carcinoma. Nests of tumor cells in pool of extracellular mucin.

Tubular carcinoma
Tubular carcinoma of the breast is an uncommon histologic type involving 1-2% of all breast cancers. Characteristic features of this type include a single layer of epithelial cells with low-grade nuclei and
apical cytoplasmic snoutings arranged in well-formed tubules and glands. Tubular components comprise more than 90% of pure tubular carcinomas and at least 75% of mixed
tubular carcinomas. This type of breast cancer has a low incidence of lymph node involvement and a very high overall
survival rate. Patients are often treated with only breast-conserving surgery and local radiation
Papillary carcinoma
Papillary carcinoma of the breast encompasses a spectrum of histologic subtypes There are 2 common types:
o cystic (noninvasive form) and micropapillary ductal carcinoma (invasive form). This form of breast cancer is usually seen in women older than 60 years and accounts for approximately
1-2% of all breast cancers. Papillary carcinomas are centrally located in the breast and can present as bloody nipple discharge. They are strongly ER- and PR-positive. Cystic papillary carcinoma has a low mitotic activity Lymph node metastasis is seen frequently in this subtype (70-90% incidence), and the number of lymph
nodes involved appears to correlate with survival.
Papillary carcinoma. Solid papillary growth pattern with early cribriform and well-developed thin papillary fronds.
Metaplastic breast cancer
MBC accounts for less than 1% of breast cancer cases, tends to occur in older women (average age of onset in the sixth decade), and has a higher incidence in blacks.
It is characterized by a combination of adenocarcinoma plus mesenchymal and epithelial components. A wide variety of histologic patterns includes the following:
o Spindle-cell carcinomao Carcinosarcomao Squamous cell carcinoma of ductal origino Adenosquamous carcinomao Carcinoma with pseudosarcomatous metaplasiao Matrix-producing carcinoma

This diverse group of malignancies is identified as a single entity based on a similarity in clinical behavior.
When compared with infiltrating ductal carcinoma, MBC tumors are:o Largero More rapidly growingo Commonly node-negativeo Typically ER-, PR-, and HER2-negative.
Mammary Paget disease
MPD is relatively rare, comprising 1-4% of all breast cancers. Peak incidence is seen in the sixth decade of life (mean age, 57 y).
o The overall 5-year and 10-year survival rates are 59% and 44%, respectively. This adenocarcinoma is localized within the epidermis of the nipple-areola complex and composed of the
histologic hallmark Paget cells within the basement membrane. o Paget cells are large, pale epithelial cells with hyperchromatic, atypical nuclei, dispersed between the
keratinocytes singly or as a cluster of cells. Lesions are predominantly unilateral, developing insidiously as a scaly, fissured, oozing, or erythematous
nipple-areola complex. Retraction or ulceration of the nipple is often noted, along with symptoms of itching, tingling, burning, or
pain.

Prognostic and Predictive Factors
Numerous prognostic and predictive factors for breast cancer have been identified by the College of American Pathologists (CAP) to guide the clinical management of women with breast cancer.
Breast cancer prognostic factors include the following:
Axillary lymph node status Tumor size Lymphatic/vascular invasion Patient age Histologic grade Histologic subtypes (eg, tubular, mucinous [colloid], papillary) Response to neoadjuvant therapy ER/ PR status HER2 gene amplification and/or overexpression
Breast cancer predictive factors include the following:
ER/PR status HER2 gene amplification and/or overexpression
Cancerous involvement of the lymph nodes in the axilla is an indication of the likelihood that the breast cancer has spread to other organs. Survival and recurrence are independent of level of involvement but directly related to the number of involved nodes.
Patients with node-negative disease have an overall 10-year survival rate of 70% and a 5-year recurrence rate of 19%. In patients with lymph nodes that are positive for cancer, the recurrence rates at 5 years are as follows:
1-3 positive nodes: 30-40% 4-9 positive nodes: 44-70% More than 10 positive nodes: 72-82%
Hormone-positive tumors have a more indolent course and are responsive to hormone therapy. ER and PR assays are routinely performed on tumor material by pathologists, and immunohistochemistry (IHC) is a semiquantitative technique that is observer and antibody dependent.
Five-year survival rates are highly correlated with tumor stage, as follows:
Stage 0: 99-100% Stage I: 95-100% Stage II: 86% Stage III: 57% Stage IV: 20%
This prognostic information can guide physicians in making therapeutic decisions. Pathologic review of the tumor tissue for histological grade along with the determination of estrogen/progesterone receptor status and HER2 status is necessary for determining prognosis. Evaluation of lymph node involvement by sentinel lymph node biopsy or axillary lymph node dissection is generally[18] necessary as well. (See Staging.)

HER2
Before the routine use of trastuzumab (Herceptin, a monoclonal antibody) in adjuvant therapy, HER2 overexpression was associated with a more aggressive tumor phenotype and worse prognosis (higher rate of recurrence and mortality), independent of other clinical features (eg, age, stage, tumor grade), especially in patients who did not receive adjuvant chemotherapy.
Additionally, HER2 status has been shown to be predictive for response to certain chemotherapeutic agents (ie, doxorubicin [Adriamycin]; and HER2-targeted therapies trastuzumab and lapatinib [Tykerb, a small-molecule oral tyrosine kinase inhibitor directed specifically to the HER2 receptor]).
Retrospectively analyzed results from clinical trials have shown that HER2-positive patients benefit from anthracycline-based regimens secondary to the coamplification of topoisomerase II with HER2. Preliminary data also suggest that HER2 may predict response to and benefit from paclitaxel in the adjuvant setting.
Go to Breast Cancer and HER2 for complete information on this topic.
StagingThe American Joint Committee on Cancer (AJCC) staging system groups patients into 4 stages based on tumor size (T), lymph node status (N), and distant metastasis (M). See Table 5, below.
Primary tumor (T)
Tumor size definitions are as follows:
Tx: Primary tumor cannot be assessed T0: No evidence of primary tumor Tis: (DCIS) Carcinoma in situ Tis: (LCIS) Carcinoma in situ Tis: Paget disease of the nipple with no tumor (Paget disease associated with a tumor is classified
according to the size of the tumor.) T1: Tumor 2 cm or smaller in greatest diameter T1mic: Microinvasion 0.1 cm or less in greatest dimension T1a: Tumor >0.1 but not >0.5 cm in greatest diameter T1b: Tumor >0.5 but not >1 cm in greatest diameter T1c: Tumor >1 cm but not >2 cm in greatest diameter T2: Tumor >2 cm but not >5 cm in greatest diameter T3: Tumor >5 cm in greatest diameter T4: Tumor of any size, with direct extension to (a) the chest wall or (b) skin only, as described below T4a: Extension to the chest wall, not including the pectoralis muscle T4b: Edema (including peau d’orange) or ulceration of the skin of the breast or satellite skin nodules
confined to the same breast T4c: Both T4a and T4b T4d: Inflammatory disease
Regional lymph nodes (N)
Regional lymph node definitions are as follows:

Nx: Regional lymph nodes cannot be assessed (eg, previously removed) N0: No regional lymph node metastasis N1: Metastasis in movable ipsilateral axillary lymph node(s) N2: Metastasis in ipsilateral axillary lymph node(s) fixed or matted, or in clinically apparent ipsilateral
internal mammary nodes in the absence of clinically evident axillary lymph node metastasis N2a: Metastasis in ipsilateral axillary lymph nodes fixed to one another or to other structures N2b: Metastasis only in clinically apparent ipsilateral internal mammary nodes and in the absence of
clinically evident axillary lymph nodes N3: Metastasis in ipsilateral infraclavicular or supraclavicular lymph node(s) with or without axillary
lymph node involvement, or clinically apparent ipsilateral internal mammary lymph node(s) and in the presence of axillary lymph node
N3a: Metastasis in ipsilateral infraclavicular lymph node(s) N3b: Metastasis in ipsilateral internal mammary lymph node(s) and axillary lymph node(s) N3c: Metastasis in ipsilateral supraclavicular lymph node(s)
Distant metastasis
Metastases are defined as follows:
Mx: Distant metastasis cannot be assessed M0: No distant metastasis M1: Distant metastasis
Table 5. TNM Staging System for Breast Cancer (Open Table in a new window)
Stage Tumor Node MetastasesStage 0 Tis N0 M0Stage I T1 N0 M0Stage IIA T0
T1
T2
N1
N1
N0
M0
M0
M0
Stage IIB T2
T3
N1
N0
M0
M0
Stage IIIA T0 N2 M0

T1
T2
T3
N2
N2
N1-2
M0
M0
M0
Stage IIIB T4
T4
T4
N0
N1
N2
M0
M0
M0
Stage IIIC Any T N3 M0Stage IV Any T Any N M1Five-year survival rates are highly correlated with tumor stage, as follows:
Stage 0: 99-100% Stage I: 95-100% Stage II: 86% Stage III: 57% Stage IV: 20%
This prognostic information can guide physicians in making therapeutic decisions. Pathologic review of the tumor tissue for histological grade along with the determination of estrogen/progesterone receptor status and HER2 status is necessary for determining prognosis.
Evaluation of lymph node involvement by sentinel lymph node biopsy or axillary lymph node dissection has also been considered necessary for staging and prognosis, as recommended in the 2009 edition of the National Comprehensive Cancer Network (NCCN) breast cancer guidelines, but the 2011 update modifies this recommendation. The 2011 NCCN breast cancer guidelines state that lymph node evaluation is optional in the following cases:
Strongly favorable tumors When no result would affect the choice of adjuvant systemic therapy Elderly patients Patients with comorbid conditions
The 2011 NCCN guidelines state that for staging, sentinel lymph node biopsy is preferred over axillary lymph node dissection.[6, 18] .

Additional TestingThe 2011 NCCN guidelines, like the 2009 version, recommends the following laboratory studies for all asymptomatic women with early-stage breast cancer (stages I and II):
Complete blood cell (CBC) count with differential Liver function tests (LFTs) Renal function tests Serum calcium
In addition, women with stage III (locally advanced or inflammatory breast cancer) or symptomatic disease should have a chest x-ray or CT scan of the chest, CT scan of the abdomen and pelvis, and bone scan for evaluation of distant metastasis. Tumor markers (carcinoembryonic antigen [CEA] and CA15.3 or CA27.29) may also be obtained in these patients.[6, 18]
Genetic testing for BRCA1 and BRCA2 can be performed in selected high-risk patients with a strong family history of breast or ovarian carcinoma. However, genetic counseling and discussion of subsequent management and treatment options should be performed before testing.
HER2 testing
Although several methods for HER2 testing have been developed, approximately 20% of current HER2 testing may be inaccurate; therefore, the American Society of Clinical Oncology (ASCO) and CAP have recommended guidelines in HER2 testing to ensure accuracy. Breast cancer specimens should initially undergo HER2 testing by a validated immunohistochemistry (IHC) assay (ie, HercepTest, Dako, Glostrup, Denmark) for HER2 protein expression.[7] The scoring method for HER2 expression is based on the cell membrane staining pattern and is as follows:
3+: Positive HER2 expression - Uniform intense membrane staining of more than 30% of invasive tumor cells
2+: Equivocal for HER2 protein expression - Complete membrane staining that is either nonuniform or weak in intensity but has circumferential distribution in at least 10% of cells
0 or 1+: Negative for HER2 protein expression
Breast cancer specimens with equivocal IHC should undergo validation using a HER2 gene amplification method, such as fluorescence in situ hybridization (FISH). More centers are relying on FISH alone for determining HER2 status.
In general, FISH testing is thought to be more reliable than IHC, but it is more expensive. Equivocal IHC results can be seen in 15% of invasive breast cancers, whereas equivocal HER2 FISH results are seen in less than 3% of invasive breast cancer specimens and those that had previously been considered HER2 positive. Discordant results (IHC 3+/FISH negative or IHC less than 3+/FISH positive) have been observed in approximately 4% of specimens. Currently, no data support excluding this group from treatment with trastuzumab.
Newer methodologies for establishing HER2 status, including reverse transcriptase–polymerase chain reaction (RT-PCR) and chromogenic in situ hybridization (CISH), have not yet been validated. The interpretation for HER2 FISH testing (HER2/CEP17 ratio and gene copy number) is given below:
Positive HER2 amplification: FISH ratio is greater than 2.2 or HER2 gene copy is greater than 6.0 Equivocal HER2 amplification: FISH ratio of 1.8-2.2 or HER2 gene copy of 4.0-6.0 Negative HER2 amplification: FISH ratio is less than 1.8 or HER2 gene copy of less than 4.0

Go to Breast Cancer and HER2 for complete information on this topic.
Oncotype Dx assay
The Onco type Dx assay (Genomic Health, Inc, Redwood City, Calif) has been validated in and approved by the FDA for women with early-stage, ER-positive, node-negative breast cancer treated with tamoxifen, where the recurrence score (RS) correlated with both relapse-free interval and overall survival. This assay is an RT-PCR-based assay of 21 genes (16 cancer genes and 5 reference genes) performed on paraffin-embedded breast tumor tissue.
Using a formula based on the expression of these genes, a recurrence score can be calculated that correlates with the likelihood of distant recurrence at 10 years. Breast tumors with a recurrence score of less than 18 are considered low risk; a score of 18-30 is considered intermediate risk; and a score greater than 30 is considered high risk.
Furthermore, the Onco type Dx assay has been shown retrospectively in the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14 and B-20 studies to predict benefit from chemotherapy and hormonal therapy in hormone-sensitive, node-negative tumors.
Women with a low recurrence score showed a significantly greater improvement in disease-free survival (DFS) with the addition of tamoxifen versus chemotherapy, whereas women with a high recurrence score had a significant improvement in disease-free survival with the addition of chemotherapy. Among women with 1-3 node-positive, hormone receptor-positive disease, the Onco type Dx recurrence score was a significant predictor of recurrence, with a 21% decrease in recurrence risk for each 10-point drop in the recurrence score.
In general, results from these studies would indicate that a select group of node-positive, hormone receptor-positive patients with a low recurrence score would not benefit from an anthracycline-based regimen. The benefit of adding chemotherapy to hormonal therapy in tumors with an intermediate score is still controversial; The Trial Assigning Individualized Options for Treatment [TAILORx] Trial, a large, prospective, randomized phase III study sponsored by the National Cancer Institute (NCI), is addressing this important question.
TX AND MANAGEMENT
Approach ConsiderationsSurgery is considered primary treatment for breast cancer, as many patients with early-stage disease are cured with surgery alone. The goals of breast cancer surgery include complete resection of the primary tumor with negative margins to reduce the risk of local recurrences, and pathologic staging of the tumor and axillary lymph nodes for providing necessary prognostic information. Several different types of operations are available for the treatment of breast cancer.
Adjuvant treatment for breast cancer involves radiation therapy and a variety of chemotherapeutic and biologic agents.
Treatment of Invasive Breast CancerSurgical treatment of invasive breast cancer may consist of lumpectomy or total mastectomy.In breast cancer patients who have clinically negative nodes, surgery typically includes sentinel lymph node dissection for staging the axilla. Go to Surgical Treatment of Breast Cancer for more information on these topics. In addition to surgery, the use of radiation therapy, chemotherapy, or both may be indicated.

Breast-conserving radiation therapy
The purpose of radiation therapy following breast-conserving surgery is to eradicate local subclinical residual disease while reducing local recurrence rates by approximately 75%. Based on results from several randomized controlled studies, radiation to the intact breast is considered standard of care, even in the lowest-risk disease with the most favorable prognostic features.
There are 2 general approaches used to deliver radiation therapy: conventional external beam radiotherapy (EBRT) and partial-breast irradiation (PBI). Whole-breast radiotherapy (WBRT) consists of EBRT delivered to the breast at a dose of 50-55 Gy over 5-6 weeks. This is often followed by a boost dose specifically directed to the area in the breast where the tumor was removed.
Common side effects of radiation therapy include fatigue, breast pain, swelling, and skin desquamation. Late toxicity (lasting 6 mo or longer following treatment) may include persistent breast edema, pain, fibrosis, and skin hyperpigmentation. Rare side effects include rib fractures, pulmonary fibrosis, cardiac disease (left breast treatment), and secondary malignancies such as radiation-induced sarcoma (0.5%).
Partial-breast irradiation is employed in early stage breast cancer following breast-conserving surgery as a way of delivering larger fraction sizes while maintaining a low risk of late effects. Several techniques that can deliver this therapy include interstitial brachytherapy (multiple catheters placed through the breast) and intracavitary brachytherapy (a balloon catheter inserted into the lumpectomy site [ie, MammoSite]).
Treatment is typically for 5 days, twice daily. These techniques have shown low local recurrence rates comparable to EBRT in several nonrandomized studies.
The American Society of Breast Surgeons (ASBrS) recommends the following selection criteria when considering patients for treatment with accelerated partial breast irradiation:
Age 45 years and older Invasive ductal carcinoma or DCIS Total tumor size (invasive and DCIS) 3 cm or smaller Negative microscopic surgical margins of excision Axillary lymph node/sentinel lymph node negative
Potential complications of partial-breast irradiation are catheter placement, followed by removal secondary to inadequate skin spacing, infection, seroma, fibrosis, chronic pain, or disease recurrence.
Postmastectomy radiation therapy
Clinical practice guidelines developed by ASCO along with several prospective, randomized clinical trials recommend postmastectomy radiation therapy be performed using the following criteria:
Positive postmastectomy margins Primary tumors larger than 5 cm Involvement of 4 or more lymph nodes
Patients with more than 4 positive lymph nodes should also undergo prophylactic nodal radiation therapy at doses of 4500-5000 cGy to the axillary and supraclavicular regions. For patients who undergo axillary lymph node dissection and are found to have no lymph node involvement, axillary radiation therapy is not recommended.

Meta-analyses have shown postmastectomy radiation therapy combined with regional nodal radiation therapy significantly decreases the rate of local relapse and breast cancer mortality. Currently, the benefit of radiation therapy for women with 1-3 positive axillary lymph nodes is uncertain, and studies are ongoing.
Adjuvant Therapy for Breast CancerDepending on the model of risk reduction, adjuvant therapy has been estimated to be responsible for 35-72% of the reduction in mortality rate. Adjuvant treatment of breast cancer is designed to treat micrometastatic disease, or breast cancer cells that have escaped the breast and regional lymph nodes but which have not yet had an established identifiable metastasis. Treatment is aimed at reducing the risk of future recurrence, thereby reducing breast cancer-related morbidity and mortality. Go to Adjuvant Therapy for Breast Cancer for more information on this topic.
Treatment of Carcinoma in Situ
Ductal carcinoma in situ
Currently, the standard treatment of DCIS is surgical resection with or without radiation. Adjuvant radiation and hormonal therapies are often reserved for younger women, patients undergoing lumpectomy, or comedo subtype.
Approximately 30% of women with DCIS in the US are treated with mastectomy with or without reconstruction, 30% with conservative surgery alone, and 40% with conservative surgery followed by whole-breast radiation therapy. Axillary or sentinel lymph node dissection is not routinely recommended for patients with DCIS. Studies have identified metastatic disease to the axillary nodes in 10% of patients.
In DCIS, whole-breast radiotherapy is delivered over 5-6 weeks after surgery, reducing the local recurrence rate by approximately 60%. Roughly 50% of local recurrences are invasive breast cancer. Meta-analyses of randomized controlled trials comparing radiation therapy versus observation after surgery for DCIS have demonstrated slightly higher rates of contralateral breast cancer after radiation therapy (3.85% vs 2.5%). Studies comparing accelerated partial breast radiation given over 5 days to standard whole-breast radiotherapy are currently under way.
Tamoxifen is the only hormonal therapy currently approved for adjuvant therapy in patients treated with breast-conserving surgery and radiation for DCIS. Currently, a clinical trial evaluating the role of the aromatase inhibitor anastrozole as adjuvant therapy in DCIS has met its accrual and results are anticipated.
Lobular carcinoma in situ
The National Surgical Adjuvant Breast and Bowel Project (NSABP) P-1 trial prospectively studied the efficacy of tamoxifen in the prevention of breast cancer and included patients with LCIS.[8] The researchers found a 55% risk reduction in women treated with tamoxifen.
Overall, treatment options include observation and close follow-up care with or without tamoxifen, and bilateral mastectomy with or without reconstruction. No evidence exists of therapeutic benefit from local excision, axillary dissection, radiotherapy, or chemotherapy. The presence of LCIS in the breast of a woman with ductal or lobular cancer does not require further immediate surgery on the opposite breast. Mirror biopsy of the contralateral breast, once advocated in the treatment of LCIS, is mainly of historic interest.
Treatment of Locally Advanced and Inflammatory Breast Cancer

Originally, the reason for grouping LABC and IBC was the recognition that both diseases had little or no chance of cure from local therapy alone, and they were considered inoperable for that reason. The definition of locally advanced disease has broadened to include patients who are technically operable but who have large primary tumors (>5 cm).
It is important to recognize, however, that the reasons for using neoadjuvant therapy are different in women who have large primary tumors, in which the goal is to increase the possibility of breast-conserving surgery, than in those who have disease that meets the original criteria of LABC or IBC, for whom the administration of systemic treatment is essential to make definitive local treatment possible with the intent of cure.
Because the prognosis for women with T3N0 (stage IIB) and T3N1 (stage IIIA) breast cancer is better overall than it is for those with classically defined LABC (IIIB, IIIC) or IBC (IIIB, T4d), it is important to know the relative proportions of patients in each category when results of a clinical trial are reported. Not only may one expect better disease-free and overall survival for stage IIB and IIIA patients, but also the likelihood of achieving a pathologic complete response (pCR) from neoadjuvant treatment, a well-recognized surrogate for long-term outcome, is inversely related to tumor size.
It is also important to recognize that staging criteria in the sixth edition of the AJCC Cancer Staging Handbook differs from its predecessors in ways that are relevant to the patient groups discussed here: women with T3 tumors were previously considered to have stage III disease and are so reported in the older literature; women with resectable tumors who are found to have 4 or more involved axillary lymph nodes after initial surgery, formerly called stage II, are currently grouped as IIIA.
The revised staging system is better for defining prognostic subgroups, but the practical relevance of grouping together all patients who typically receive "up front" chemotherapy remains, as their treatment outcomes are usually reported as a function of the particular neoadjuvant program employed.
Inflammatory breast cancer
IBC is a clinical diagnosis that implies presentation with the cardinal signs of inflammation (calor, rubor, and tumor) involving the breast, although the calor (warmth) may be subtle and the tumor (mass) may not be appreciated as something discrete. Indeed, even when a localized mass is apparent in IBC, the true extent of the disease (as shown by performing skin biopsies from the surrounding, normal-appearing skin) is usually greater than apparent on physical examination. It was originally described as having an erysipeloid border, but only a minority of cases have this component of a raised edge.
In Western countries, the frequency of IBC is low, between 1% and 2% of all breast cancers, but it is much higher in some parts of the world, such as northern Africa, for reasons that are not known. IBC tends to occur at a younger age than LABC. Pathologically, it was originally associated with the classic finding of involvement of subdermal lymphatics, although this finding is not in itself diagnostic of IBC (it may occur with LABC as a secondary phenomenon).
This disease is more likely to stain negatively by IHC for ER and PR, somewhat more likely to be positive for HER2 overexpression, and both angiogenesis and lymphangiogenesis appear to be increased by microvessel density or RNA-based gene expression arrays. Within IBC, however, may be found the same molecular subtypes of breast cancer as originally described for non-inflammatory breast cancer.
Locally advanced breast cancer
LABC is more common in the US than is IBC, and, by the definition used here, may account for 10-15% of patients (this drops to about 5% if one uses the stricter definition of inoperable). Epidemiologically, LABC is associated with lower socioeconomic class and, probably for that reason, with black race in the US.

LABC encompasses both relatively indolent neglected tumors and those that have grown rapidly as a result of their inherent biology. It is as heterogeneous as invasive breast cancer in general, and, in most case series, LABC has a better long-term outcome than IBC, even when only inoperable cases are considered.
Evaluation of lymph nodes and response
Patients with LABC or IBC with clinically positive nodes should undergo a core biopsy before initiating chemotherapy. Those with clinically negative nodes may undergo sentinel node biopsy before they start treatment, or sentinel node determination may be delayed until after treatment is completed.
Theoretically, it should be preferable to perform sentinel node sampling up front, because chemotherapy might eradicate preexistent disease in the sentinel node and result in a false negative, and/or altered lymphatic drainage in large tumors might affect accuracy of the procedure. However, data from the NSABP B-27 neoadjuvant trial suggest that the false-negative rate for sentinel node biopsies performed after neoadjuvant chemotherapy is about 11%, comparable to the false-negative rate for patients undergoing initial resection.[9]
In general, the best single test to evaluate the status of measurable tumor is ultrasonography, preferably done by the same operator to avoid interobserver variability. The mass often appears larger on physical examination than it does on sonogram, which can more effectively discriminate hypoechoic masses from surrounding stroma and/or hematoma. In IBC, MRI may be an important adjunct to response assessment. The role of PET scanning in the routine assessment of response remains to be determined.
No current imaging technique appears to be highly accurate for the prediction of complete pathologic response. Thus, the purpose of regular size assessment is to exclude continuation of therapy in a patient with a growing tumor (seen in < 5% with the initial treatment) and to suggest when maximal response of grossly evident disease has been achieved, as this may be the optimal time to proceed to resection.
Systemic Treatment of Metastatic Breast CancerMarked advancements are being made in the treatment of early stage breast cancer, but many women still develop recurrence and metastasis. In addition, 5-10% of breast cancer patients have metastatic disease at presentation. Although treatments for metastatic breast cancer continue to improve, there remains no cure once distant metastases develop.
Furthermore, although occasional patients with metastatic breast cancer benefit from surgical resection for an isolated recurrence and many require radiation therapy for palliation at a specific site (or definitive treatment of brain metastasis), in general, recurrent or metastatic breast cancer must be approached systemically such that the therapeutic effect reaches all sites of disease. There are 2 main interventions: hormone therapy and chemotherapy. Go to Adjuvant Therapy for Breast Cancer for more information on these topics.
Surgery in Metastatic Breast Cancer Treatment As modern systemic chemotherapy has become more effective, some patients with intact primary tumors and metastasis can have long-term stable distant disease or even no evidence of residual metastatic disease following treatment. Recently, interest has increased in the role of surgical intervention for the intact primary tumor for these metastatic breast cancer patients. Several single-institution cohort and retrospective studies have examined this question, concluding that surgical resection of the intact primary tumor may provide a survival advantage.
It is still unknown whether a selection bias affects the findings of a survival advantage in favor of surgery, and no prospective, randomized control trial has ever been performed to address this question. However, the dogma

to never operate in the setting of metastatic disease has certainly been dispelled in favor of critical evaluation of whether surgically achieved local control can lead to improved survival as a part of multimodal treatment.
Pharmacologic Breast Cancer Risk Reduction Two selective estrogen receptor modulators (SERMs), tamoxifen and raloxifene (Evista), are approved for reduction of breast cancer risk in high-risk women. Two NSABP trials (NSABP P1 and P2) showed that tamoxifen reduced the risk of DCIS and invasive breast cancer by 30-50%. In the NSABP P2 prevention trial, raloxifene was as effective as tamoxifen in reducing the risk of invasive breast cancer but was 30% less effective than tamoxifen in reducing the risk of DCIS.
ACOG has updated its practice guidelines regarding pharmacologic intervention (eg, tamoxifen, raloxifene, aromatase inhibition) for breast cancer risk reduction.[10] Some of the highlights of the expert panel's literature review are as follows:
Tamoxifen use for 5 years reduces risk of breast cancer for at least 10 years in premenopausal women, particularly ER-positive invasive tumors. Women 50 years or younger have few adverse effects with tamoxifen, and vascular/vasomotor adverse effects do not persist post treatment.
Tamoxifen and raloxifene are equally effective in reducing risk of ER-positive breast cancer in postmenopausal women. Raloxifene is associated with lower rates of thromboembolic disease, benign uterine conditions, and cataracts than tamoxifen. Evidence does not exist on whether either agent decreases mortality from breast cancer.
Recommendations include the following:
For women with increased risk for breast cancer, offer tamoxifen (20 mg/d for 5 y) to reduce the risk of invasive ER-positive breast cancer
In postmenopausal women, raloxifene (60 mg/d for 5 y) may also be considered Aromatase inhibitors (eg, anastrozole, exemestane, letrozole), fenretinide, or other SERMs are not
recommended for use outside of a clinical trial
Long-term Monitoring
Follow-up guidelines
There is no consensus among oncologists as to the appropriate and optimal follow-up for long-term breast cancer survivors. The majority of relapses, both local and distant, occur within the first 3 years, especially in higher risk and ER-negative patients. The 2007 ASCO guidelines do not support the use of tumor biomarkers, including CEA, CA15.3, and CA27.29, for monitoring patients for recurrence after primary breast cancer therapy.
Table 6, below, lists the NCCN’s recommendations for breast cancer patients in the adjuvant setting.
Table 6. Follow-up Recommendations for Breast Cancer Survivors per NCCN Guidelines (Open Table in a new window)
Intervention* Year 1 Year 2 Year 3-5 Year 6+History and physical examination q3-4 mo q4 mo q6 mo AnnuallyMammography Annually (or 6 mo after Annually Annually Annually

post-BCS irradiation)
Chest x-ray NR NR NR NRPelvic examination† Annually Annually Annually AnnuallyBone density‡ q1-2 yBCS = breast-conserving surgery; NR = not recommended.* Bone scan, blood counts, LFTs, and tumor markers are not routinely recommended
and should be performed if clinically indicated.
† For patients with an intact uterus on tamoxifen.
‡ For patients at risk for osteoporosis.
Postsurgical imaging
Women who have had surgery for breast cancer may still require breast cancer screening with mammography. If a woman had a total mastectomy, then the other breast requires yearly follow-up, because she is still at higher risk of developing cancer in the remaining breast. If she had subcutaneous mastectomy, partial mastectomy, or lumpectomy, then that breast itself requires follow-up mammography.
The first mammogram is best performed 6 months postoperatively to provide a baseline for the new postoperative and radiation changes. Thereafter, mammography may be performed every 6-12 months for screening and follow-up. Go to Postsurgical Breast Imaging for more information on this topic.
Monitoring of metastatic disease
Recommendations for monitoring disease response in the metastatic setting vary. In general, monthly evaluations consisting of a history and physical examination to evaluate progression of disease and toxicities are reasonable.
Tumor markers, such as CEA, CA15.3, and CA27.29, can be used in conjunction with diagnostic imaging, history, and physical examination for monitoring while on active therapy. CA15.3 and CA27.29 levels correlate with the course of disease in 60-70% of patients, whereas CEA levels correlate in 40% of patients.
However, data are insufficient to recommend the use of CEA, CA15.3, or CA27.29 alone for monitoring response to treatment. Caution should be used when interpreting rising CEA, CA15.3, or CA27.29 levels during the first 4-6 weeks of a new therapy, as spurious early rises may occur.
Standardized guidelines for imaging are not yet established and should be tailored to each patient. In general, CT scanning (chest, abdomen, and pelvis), MRI, bone scanning, or PET/CT scanning are performed when symptoms change or tumor markers rise.
Circulating tumor cells are cells present in the blood that possess antigenic or genetic characteristics similar to a primary tumor type. The FDA has recently approved the CellSearch System (Veridex, Raritan, NJ) for the detection of circulating tumor cells in patients with metastatic breast cancer. This system captures circulating

tumor cells using an immunomagnetic process with an epithelial cell adhesion molecule coated with magnetic beads and cytokeratin antibodies.
A circulating tumor cell is identified when it is cytokeratin- and DAPI-positive but CD45-negative. Studies done by Cristofanilli using the CellSearch System have shown a prognostic utility and predictive use for circulating tumor cells in metastatic breast cancer patients.[11] Circulating tumor cell–positive patients (>5 CTCs/7.5 mL blood) were shown to have a worse progression-free survival (17%) and overall survival than the circulating tumor cell–negative patients (36%).
The presence of more than 5 circulating tumor cells before hormonal or chemotherapy treatment and following the first cycle of treatment also predict a worse outcome. However, studies to date have used small sample sizes, and no data have shown that use of circulating tumor cell testing affects overall survival or improves on quality of life.
Per ASCO guidelines, the use of circulating tumor cell testing in breast cancer is not recommended for the diagnosis of breast cancer, nor should test results influence treatment decisions. The Southwest Oncology Group (SWOG) is conducting a large, prospective trial to address the clinical use of circulating tumor cells in breast cancer.
MEDICATION
Medication SummaryAdjuvant treatment for breast cancer involves radiation therapy and a variety of chemotherapeutic and biologic agents. Adjuvant treatment of breast cancer is designed to treat micrometastatic disease, or breast cancer cells that have escaped the breast and regional lymph nodes but which have not yet had an established identifiable metastasis. Treatment is aimed at reducing the risk of future recurrence, thereby reducing breast cancer-related morbidity and mortality.
The 2011 NCCN guidelines include recommendations for the use of two new drugs, denosumab and eribulin, both of which received FDA approval in 2010. The 2011 guidelines support the use of biologic denosumab for the prevention of skeletal events. When compared with zoledronic acid, denosumab, which is administered subcutaneously, delayed the onset of skeletal events by 8% and the time to multiple skeletal events by 23%. In addition, toxicities, such as hypercalcemia and renal failure, were less frequent. The guidelines recommend eribulin, an antimicrotubular drug, as the "preferred single agent" in chemotherapy treatment for women with advanced disease. Trials have shown significant improvement in survival when compared with patients receiving "treatment by physician's choice."[18]
In June 2011, an FDA panel recommended that bevacizumab (Avastin) no longer be used to treat breast cancer, and in November officially rescinded its approval.
Antineoplastic Agents
Class Summary
Various chemotherapy regimens are recommended for the treatment of breast cancer. Common regimens include docetaxel, cyclophosphamide, doxorubicin, carboplatin, methotrexate, and trastuzumab, among others.
View full drug information
Docetaxel (Taxotere)

Docetaxel is indicated for use in combination with doxorubicin and cyclophosphamide for adjuvant treatment of operable node-positive breast cancer. It is also indicated for locally advanced or metastatic breast cancer after failure of prior chemotherapy. It is a semisynthetic taxane, a class of drugs that inhibits cancer cell growth by promoting assembly and blocking the disassembly of microtubules, thereby preventing cancer cell division, leading to cell death.
View full drug information
Carboplatin
Carboplatin is an analog of cisplatin. This is a heavy metal coordination complex that exerts its cytotoxic effect by platination of DNA, a mechanism analogous to alkylation, leading to interstrand and intrastrand DNA cross-links and inhibition of DNA replication. It binds to protein and other compounds containing the SH group. Cytotoxicity can occur at any stage of the cell cycle, but the cell is most vulnerable to the action of these drugs in the G1 and S phases. It has the same efficacy as cisplatin, but with a better toxicity profile. The main advantages over cisplatin include less nephrotoxicity and ototoxicity, not requiring extensive prehydration, and less likelihood of inducing nausea and vomiting; however, it is more likely to induce myelotoxicity.
View full drug information
Doxorubicin (Liposomal)
Doxorubicin is a cytotoxic anthracycline that inhibits topoisomerase II and produces free radicals, which may cause destruction of DNA. It blocks DNA and RNA synthesis by inserting between adjacent base pairs and binding to the sugar-phosphate backbone of DNA, which causes DNA polymerase inhibition. It binds to nucleic acids, presumably by specific intercalation of the anthracycline nucleus with the DNA double helix. It is also a powerful iron chelator. The iron-doxorubicin complex induces production of free radicals that can destroy DNA and cancer cells. Maximum toxicity occurs during the S phase of the cell cycle.
View full drug information
Capecitabine (Xeloda)
Capecitabine is a pyrimidine analog, which, in combination with docetaxel, is indicated for metastatic breast cancer after the failure of prior anthracycline-containing chemotherapy. Monotherapy with capecitabine is indicated for the treatment of patients with metastatic breast cancer resistant to both paclitaxel and an anthracycline–containing chemotherapy regimen or resistant to paclitaxel and for whom further anthracycline therapy is not indicated.[12]
View full drug information
Paclitaxel
Paclitaxel is indicated for adjuvant treatment of node-positive breast cancer (ie, administered sequentially to doxorubicin-containing combination chemotherapy). Dose-dense regimens (ie, more frequent administration) are currently being studied and resulting disease-free interval examined. Mechanisms of action are tubulin polymerization and microtubule stabilization, which, in turn, inhibit mitosis and may result in the breakage of chromosomes.
View full drug information
Gemcitabine (Gemzar)

Gemcitabine is a pyrimidine analog that is metabolized intracellularly to an active nucleotide. It inhibits ribonucleotide reductase and competes with deoxycytidine triphosphate for incorporation into DNA. It is cell-cycle specific for the S phase. Gemcitabine, in combination with paclitaxel, is indicated as a first-line treatment for metastatic breast cancer after the failure of prior anthracycline-containing adjuvant chemotherapy (unless anthracyclines were clinically contraindicated).
View full drug information
Cyclophosphamide
Cyclophosphamide is chemically related to nitrogen mustards. It is indicated for use in patients with carcinoma of the breast. It is activated in the liver to its active metabolite, 4-hydroxycyclophosphamide, which alkylates the target sites in susceptible cells in an all-or-none type of reaction. As an alkylating agent, the mechanism of action of the active metabolites may involve cross-linking of DNA, which may interfere with the growth of normal and neoplastic cells.
View full drug information
Methotrexate (Trexall)
Methotrexate is an antimetabolite that inhibits dihydrofolate reductase, thereby hindering DNA synthesis and cell reproduction in malignant cells. Methotrexate is indicated alone or in combination with other anticancer agents for the treatment of breast cancer.
View full drug information
Epirubicin (Ellence)
Epirubicin is indicated as a part of adjuvant therapy in patients with evidence of axillary-node tumor involvement following resection of primary breast cancer.[13] It is a cell cycle phase inhibitor–nonspecific anthracycline derivative of doxorubicin with maximum cytotoxic effects on the S and G2 phases of the cell cycle.
View full drug information
Vinorelbine (Navelbine)
Vinorelbine is a semisynthetic vinca alkaloid that inhibits tubulin polymerization during the G2 phase of cell division, thereby inhibiting mitosis.
Monoclonal Antibodies
Class Summary
Monoclonal antibodies have been engineered to react against specific antigens on cancer cells, which can help to enhance the patient’s immune response and prevent cancer cell growth.
View full drug information
Denosumab

Monoclonal antibody that specifically targets RANK ligand, an essential regulator of osteoclasts. Indicated to prevent SREs (ie, bone fractures and pain) in patients with bone metastases from solid tumors.
View full drug information
Trastuzumab (Herceptin)
Trastuzumab is a monoclonal antibody that binds to the extracellular human epidermal growth receptor 2 (HER2). It mediates antibody-dependent cellular cytotoxicity against cells that overproduce HER2. It is indicated for adjuvant treatment of HER2-overexpressing, node-positive or node-negative (ER/PR negative or with one high-risk feature) breast cancer, as part of a treatment regimen consisting of doxorubicin, cyclophosphamide, and either paclitaxel or docetaxel; with docetaxel and carboplatin; or as a single agent following multimodality anthracycline-based therapy. It is also used in combination with paclitaxel for first-line treatment of HER2-overexpressing metastatic breast cancer and as a single agent for treatment of HER2-overexpressing breast cancer in patients who have received one or more chemotherapy regimens for metastatic disease.[14]
Tyrosine Kinase Inhibitors
Class Summary
Tyrosine kinase inhibitors play an important role in the modulation of growth factor signaling. They are commonly combined with other forms of chemotherapy or radiation therapy.
View full drug information
Lapatinib (Tykerb)
Lapatinib is a 4-anilinoquinazoline kinase that inhibits intracellular tyrosine kinase domains of epidermal growth factor receptors (EGFR [ErbB1]) and HER2 (ErbB2). It is indicated in combination with capecitabine for advanced or metastatic breast cancer with tumors that over-express HER2 for which previous therapy (ie, anthracycline, taxane, and trastuzumab) was not effective. It is also used in combination with letrozole for the treatment of postmenopausal women with hormone receptor–positive metastatic breast cancer tumors that over expresses the HER2 receptor for whom hormonal therapy is indicated.[15]
Aromatase Inhibitors
Class Summary
Aromatase inhibitors play a role in adjuvant therapy in breast cancer. These agents work by inhibiting aromatase, the enzyme responsible for converting other steroid hormones into estrogen.
View full drug information
Anastrozole (Arimidex)
Anastrozole significantly lowers serum estradiol concentrations by inhibiting the conversion of adrenally generated androstenedione to estrone. It is used as first-line treatment of breast cancer in postmenopausal women with hormone receptor–positive or hormone receptor–unknown locally advanced or metastatic disease. It is also used to treat advanced breast cancer in postmenopausal women with disease progression following tamoxifen therapy.

View full drug information
Letrozole (Femara)
Letrozole is a nonsteroidal competitive inhibitor of the aromatase enzyme system. It inhibits the conversion of androgens to estrogens. Letrozole is indicated for the adjuvant treatment of postmenopausal women with hormone receptor–positive early breast cancer. It is also used for first-line treatment of postmenopausal women with hormone receptor–positive or hormone receptor–unknown locally advanced or metastatic breast cancer. It is also indicated for the treatment of advanced breast cancer in postmenopausal women with disease progression following antiestrogen therapy and for the extended adjuvant treatment of early breast cancer in postmenopausal women who have received 5 years of adjuvant tamoxifen therapy.[16]
View full drug information
Exemestane
Exemestane elicits irreversible steroidal aromatase inactivation by acting as a false substrate for the aromatase enzyme. It binds irreversibly to the aromatase enzyme active site, causing inactivation (ie, suicide inhibition). It significantly lowers circulating estrogen concentrations in postmenopausal women. It differs from tamoxifen in that it inhibits estrogen production, whereas tamoxifen inhibits estrogen at the receptor site. It is indicated for advanced breast cancer in postmenopausal women whose disease has progressed following tamoxifen therapy.
Bisphosphonate Agents
Class Summary
Bisphosphonates are complementary to chemotherapy and hormone therapy because they may lessen the damage to bone from metastatic disease. Bisphosphonates inhibit osteoclast function and reduce the resorption of bone.
View full drug information
Zoledronic Acid (Zometa, Reclast)
Zoledronic acid inhibits bone resorption, possibly by acting on osteoclasts or osteoclast precursors.
Selective Estrogen Receptor Modulators (SERMs)
Class Summary
SERMs stimulate or inhibit the estrogen receptors of various target tissues. Examples of SERMs include tamoxifen, raloxifene, and toremifene.
View full drug information
Tamoxifen
SERMs stimulate or inhibit the estrogen receptors of various target tissues. Examples of SERMs include tamoxifen, raloxifene, and toremifene.
View full drug information

Raloxifene (Evista)
Raloxifene is a selective nonsteroidal benzothiophene, estrogen receptor modulator. It is indicated for risk reduction for invasive breast cancer in postmenopausal women with osteoporosis. In addition, it is indicated for risk reduction in invasive breast cancer in postmenopausal women at high risk of invasive breast cancer.
View full drug information
Toremifene (Fareston)
Toremifene is a nonsteroidal triphenylethylene derivative that binds to estrogen receptors. It may exert estrogenic activities, antiestrogenic activities, or both activities. It is indicated for metastatic breast cancer in postmenopausal women with estrogen-receptor–positive or unknown tumors.[17]
Antimicrotubular agent
Class Summary
May consider use in patients who have received at least 2 chemotherapeutic regimens for metastatic disease.
View full drug information
Eribulin (Halaven)
Microtubule inhibitor. Inhibits growth phase of microtubules, leading to G2/M cell-cycle block, disruption of mitotic spindles, and, ultimately, apoptotic cell death.
Indicated for metastatic breast cancer in patients who have previously received at least 2 chemotherapeutic regimens for the treatment of metastatic disease. Prior therapy should have included an anthracycline and a taxane in either the adjuvant or metastatic setting.
Antineoplastic Agent, Monoclonal Antibody
Class Summary
The NCCN 2011 guidelines still recommend bevacizumab for targeted therapy[18] despite concerns expressed by the FDA.[19, 20]
View full drug information
Bevacizumab
Indicated as a first-line treatment for metastatic colorectal cancer. Murine derived monoclonal antibody that inhibits angiogenesis by targeting and inhibiting vascular endothelial growth factor (VEGF). Inhibiting new blood vessel formation denies blood, oxygen, and other nutrients needed for tumor growth. Used in combination with standard chemotherapy.