Medical Tribune February 2015 RG
-
Upload
sdafitawijaya -
Category
Documents
-
view
13 -
download
4
description
Transcript of Medical Tribune February 2015 RG

RESEARCH
REVIEWSAfIibercept effective in Japanese patients with wet AMD
RESEARCH
REVIEWSCatheter ablation beneficial for elderly patients with AF
NEWSAsthma associated with new-onset sleep apnea
FEATUREWhere there’s smoke
FEBRUARY 2015
New guideline recommends treating obesity before comorbidities

FEBRUARY 2015 2
ELVIRA MANZANO
A new pharmacotherapy guideline for man-
aging obesity recommends treating obesity
before obesity-related comorbidities, a move ex-
perts described as a shift in current practice.
“The old paradigm was to treat each comor-
bidity with medications, then manage obesity,”
said Dr. Caroline M. Apovian from Boston Medi-
cal Center, Boston, Massachusetts, US, and
chair of the taskforce that authored the guide-
line. “The new approach is for physicians to
target obesity first to diminish the associated
complications such as hyperglycemia, dyslipid-
emia and hypertension, rather than treating the
comorbidities caused by the excess weight.”
Use of approved weight-loss medications as
adjuncts to diet and exercise is recommended
in patients who have not been successful with
lifestyle modification alone. For patients with
diabetes, weight loss therapy is the primary ap-
proach to improve glycemic control and reduce
cardiovascular risk.
The guideline, released by The Endocrine
Society, with support from the European So-
ciety of Endocrinology and The Obesity Soci-
ety, also transitions patients off the drugs that
cause weight gain. [J Clin Endocrinol Metab 2015;doi:10.1210/jc.2014-3415]
Obese patients with type 2 diabetes (T2D),
for example, should be started on metformin,
and if necessary followed with glucagon-like
New guideline recommends treating obesity before comorbidities
peptide-1 (GLP-1) analogs or sodium-glucose-
linked transporter-2 (SGLT-2) inhibitors that have
the additional advantage of inducing weight
loss, the guideline said.
For obese diabetic patients with hyperten-
sion, angiotensin-converting enzyme (ACE) in-
hibitors, angiotensin receptor blockers (ARBs)
and calcium channel blockers are the recom-
mended first-line therapy. A weight loss of 5-10
percent generally lowers blood pressure where-
as 3 percent reduces blood glucose levels, said
Apovian.
Sympathomimetic agents (phentermine and
diethylpropion) should not be used in patients
with uncontrolled hypertension or a history of
heart disease.
For patients with chronic inflammatory dis-
eases (ie, rheumatoid arthritis), use of non-ste-
roidal anti-inflammatory drugs (NSAIDs) and dis-
ease-modifying antirheumatic drugs (DMARDs)
is advised as corticosteroids commonly cause
weight gain, the guideline said.
Ungraded best practice recommendation
meanwhile advised against off-label use of med-
ications approved for other diseases to promote
weight loss.
Professor Donna Ryan from the Pennington
Biomedical Research Center, Louisiana State
University, Louisiana, US, and member of the
panel said sweeping changes in obesity man-
agement can help physicians identify patients
who need additional support.

FEBRUARY 2015 3
ELVIRA MANZANO
The US Food and Drug Administration (FDA)
has approved the factor Xa inhibitor edoxa-
ban (Savaysa®, Daiichi Sankyo Co., Ltd) to low-
er the risk of stroke and systemic embolism in
patients with nonvalvular atrial fibrillation (AF).
Edoxaban, administered orally once daily,
is also approved to treat deep vein thrombosis
(DVT) and pulmonary embolism (PE) in patients
who have previously been given a parenteral an-
ticoagulant for 5-10 days.
Dr. Norman Stockbridge, director, division of
cardiovascular and renal products, FDA Center
for Drug Evaluation and Research, said it is im-
portant to have a variety of these types of drugs
available to patients. The approval was largely
based on a randomized double-blind trial com-
paring two different dosages of edoxaban (30
and 60 mg) with warfarin in 21,105 patients with
moderate-to-high-risk AF. Patients treated with
edoxaban had less major bleeding than those
receiving older anticoagulant warfarin. [N Engl J Med 2013; 369:2093-2104]
In the Hokusai VTE study, edoxaban was
noninferior to warfarin in terms of the primary
Edoxaban approved to reduce stroke risk in nonvalvular AF
efficacy endpoint of recurrent symptomatic ve-
nous thromboembolism (VTE, 3.2 vs 3.5 per-
cent, respectively) and caused less bleeding in
a broad spectrum of patients, including those
with severe PE. [N Engl J Med 2013; 369:1406-
1415]
The FDA however cautioned that edoxaban,
as with other anti-clotting drugs, may increase
the risk of bleeding and healthcare profession-
als should counsel patients taking the drug. The
agency also required edoxaban manufacturer
to carry a boxed warning that the drug is less
effective in AF patients with a creatinine clear-
ance (CrCL) of >95 mL/min. Physicians should
also measure CrCL before initiating edoxaban.
Patients with CrCL levels over 95 mL/min should
be administered a different anticoagulant.
Premature discontinuation of edoxaban also
increases the risk of stroke.
Edoxaban joins three other new oral antico-
agulants – dabigatran, rivaroxaban and apix-
aban – which are designed to overcome the
limitations of warfarin.
Warfarin requires extensive monitoring and
dose adjustment and interacts with food and
other drugs.

FEBRUARY 2015 FORUM 4
Beyond Haiyan: The challenges of maintaining the drug supply chain in catastrophes CHRISTINE AILEEN M CHING
T hink about medical workers flying in, but
upon arrival, the donated medicines have
been shipped to another storm-stricken prov-
ince. What should be done if the delivered box-
es contain drugs that are not useful in emer-
gency situations, such as chemotherapeutic
agents? What if the products have labels only in
Chinese? How can doctors manage infections
when amoxicillin is the only antibiotic avail-
able? These are just some of the things that
could happen when there is no proper drug
supply chain system set in place in preparation
for disasters.
Disaster-proneA year ago, news agencies all over the world
aired how typhoon Haiyan, one of the stron-
gest recorded typhoons to make landfall, rav-
aged central Philippines. As the government
and international community flew in to send
aid to the affected regions, the infrastructure
damage, manpower losses and downed com-
munication lines revealed gaps in preparation
and response procedures for disasters of this
magnitude. One particular area of concern in
providing medical support in this crisis is the
management of the drug supply chain, which
ideally enables better distribution, access, utili-
zation and health outcomes and reduced wast-
age of medicines resources.(1)
Being commonly exposed to natural calami-
ties, the country is in need of substantial prepa-
ration for catastrophes, especially with the threat
of climate change that is set to change the defi-
nition of normal environmental conditions in the
coming years.
WHO assessmentIn a rapid WHO-commissioned evaluation
of the medicines supply system in selected
Haiyan-affected areas, it was found out that the
policies on donated medicines were not prop-
erly implemented as evidenced by stock-outs,
expired medicines and wastages as a result of
the problems in procurement, storage and dis-
tribution, and utilization of both donated and
government-supplied medicines. The problems

MT(SG)FEB15-FINAL.indd 6 1/30/15 5:54 PM

FEBRUARY 2015 FORUM 6
with access, timeliness and appropriateness of
medicines immediately after Haiyan and in the
rehabilitation phase highlight the necessity for a
proper management system in national, provin-
cial and municipal levels of the devolved health
care system.(2)
Existing vertical programThe selection of medicines by the govern-
ment is based on the Philippine National Drug
Formulary (PNDF) while the procurement pro-
cess follows the Philippine Procurement Act (RA
9184). The Department of Health Package List
for Emergencies and Disasters managed by the
Health Emergency Management Staff, which
is similar to other vertical programs, centrally
procures and allocates health supplies during
emergencies and disasters to augment local
supplies The Department of Health is respon-
sible for coordinating and providing medicines
assistance to the local health facilities, and in
times of disaster, has the power to assume man-
agement of these local facilities.
Dr. Jean Michel-Cann, a WHO consultant,
explained the different challenges in the differ-
ent areas of the drug management cycle dur-
ing disasters.(1) In product selection, the dona-
tions are not always included in the PNDF. Local
prescribers would often not prescribe products
with other available dosage strengths or dosage
forms not in the PNDF, resulting in product un-
derutilization and wastage.
Push system vs. pull systemThe government follows a push system in
most of its vertical programs, including the
preparation for disasters, where allocation is
determined by the national level coordinators
in the supply chain. However, immediately af-
ter a disaster, the pull system is more reliable,
where quantities are requested based on the
available data on the affected areas. During di-
sasters, there is a high risk for loss of data, so a
contingency plan of preparing and retrieving a
backup data should be in place. There are also
significant losses of products especially if the
extent of damage is so grave that the storage
areas themselves have been damaged. In ad-
dition, a sudden unpredictable increase in de-
mand compounded by the need for timeliness
is very crucial. An efficient pull system helps
avoid over-stocking of slow-moving products
and optimizes the allocated storage spaces for
the products that are more commonly utilized,.
Inadequacy in the local supply usually results in
stock-outs and emergency purchases from oth-
er suppliers or pharmacies. However, for these
purchases, only products listed in the PNDF can
be reimbursed.
Expired medicinesAnother area of concern is the wastage of
medicines and supplies, which arises from
oversupply and underutilization of some drugs,
and the influx of medications that are expired or
near-expiry. Most of these medicines that are ex-
pired or near-expiry are donated medicines that
were delivered directly into the health care facili-
ties and were not checked or approved. These
medicines cannot be used due to their question-
able quality and may harm patients instead of
helping them.

FEBRUARY 2015 FORUM 7
Storage and distributionAn often overlooked issue during disasters is
the maintenance of the quality and efficacy of
medicines by proper storage and distribution.
Humidity levels, temperature, and direct sunlight
may contribute to the degradation of products,
significantly decreasing their shelf-life. The prob-
lems are due to the damage to available storage
areas, absence of electricity, or simply that the
health care facilities are not prepared to handle
the sudden arrival of medicines. With these con-
ditions, it is not uncommon to see the donated
medicines stacked in cartons along hallways, or
big rooms or outside buildings exposed to en-
vironmental forces.. Distribution channels are
also not coordinated and unplanned, resulting
in parallel channels that lead to duplication of
stocks or oversupply in one area and lack of sup-
plies in another. Transportation for medicines is
also a very big concern, in addition to human
resources knowledgeable on how to handle the
drug supplies.
Data collection Finally, during disasters, data collection is
given the least priority, and stocks are often not
properly monitored and accounted for. The uti-
lization data does not return to higher levels in
the drug supply chain management, resulting in
inappropriate procurement. The assessment of
the drug supply chain shows that even during
normal circumstances, many Rural Health Units
do not have the proper inventory management
and trained personnel to handle medicines.
Manual documentation is also being practiced
from regional to the rural health level, with no
feedback to the national government despite
the presence of a National Online Stock and In-
ventory Reporting System (NOSIRS).
In a nutshellThe problems with donated medicines are
mostly due to lack of coordination among gov-
ernment agencies and donors, unavailability
of proper transportation and storage facilities,
and an updated inventory system that will pro-
vide feedback to help meet the actual needs
on the ground. Despite existing protocols, gov-
ernance, which is key to implementation and
monitoring of these protocols in emergency
situations, are not given due attention. More-
over, greater integration of procedures should
be considered to facilitate efficient receipt and
delivery of donations. Finally, health personnel
at all levels of care must be made aware of the
considerations in accepting donated products.
The proper handling of supplies should be as-
signed to people who are well-trained in this
responsibility. (The author, who is assistant professor with the UP Manila College of Pharmacy, attended the recent National Stakeholders’ Meeting on Ensuring Drug Accessibility During Disasters and Health Emer-gencies.)
References(1) National Stakeholders’ Meeting on Ensuring Drug Accessibility During Disasters and Health Emergencies, November 11, 2014. Manila.(2) Robles, YR, Loquias, MM, and Capule, FR. Assessment of the medicines supply system in selected Haiyan-affected areas (Un-published; presented at the National Stakeholder’s Meeting).

MT(SG)FEB15-FINAL.indd 8 1/30/15 5:54 PM

FEBRUARY 2015 NEWS 9
Cooking with biogas rather than solid fuels may protect against CVDLIANNE COWIE
Poor households in low-and middle-income
countries often use solid fuels for cooking,
which increases their exposure to pollutants and
thus the risk of high blood pressure. However, a
recent study has reported that switching to alter-
native fuels such as biogas may protect against
such effects.
“More than two fifths of the world’s popula-
tion cooks with solid fuels... These fuels are of-
ten burnt in inefficient stoves inside poorly ven-
tilated houses producing high levels of several
health-damaging pollutants, in particular fine
particles of a diameter of up to 2.5 µm (PM2.5)
and mixture of other pollutants,” said the study
authors, led by Maniraj Neupane from the Cen-
ter of International Health, Ludwig-Maximilians-
Universitaet, Munich, Germany. In their cross-
sectional study, the researchers determined
whether sustained use of biogas fuel for at least
10 years altered blood pressure levels among
adult female cooks ≥30 years of age in rural
Nepal. Systolic and diastolic blood pressure
(BP) were compared among 219 and 300 cooks
from households that used biogas or firewood,
respectively. The cooks were matched by age,
body mass index, and socioeconomic status
and were stratified into two age groups to ac-
count for postmenopausal changes (30 to 50
years and >50 years). [Environmental Research
2015;136:343-351]
The results showed that biogas use was as-
sociated with a substantial reduction in 24-hour
kitchen carbon monoxide levels. In addition, a
mean 9.8 mmHg reduction in systolic BP (95%
confidence interval [CI], -20.4 – 0.8) and 6.5
mmHg reduction in diastolic BP (95% CI, -12.2 –
-0.8) were observed among women >50 years
of age from biogas households after adjusting
for smoking, kitchen characteristics, ventila-
tion status, and additional fuel use. The odds of
developing hypertension were reduced by 68
percent in this group (odds ratio 0.32, 95% CI,
0.14–0.71), but no such effects were observed
among younger women.
“Sustained use of biogas for cooking for at least
[10] years is associated with lower systolic and dia-
stolic blood pressure as well as reduced risk of de-
veloping hypertension in female cooks older than
50 years,” concluded the authors. “Although the
findings of our study need to be confirmed by well-
designed longitudinal studies, our study suggests
that household biogas... could be an alternative en-
ergy source to improve cardiovascular health of mil-
lions of cooks exposed to household air pollution
[worldwide].”

FEBRUARY 2015 NEWS 10
Asthma associated with new-onset sleep apneaELVIRA MANZANO
Adults with asthma may be at increased
risk for new-onset obstructive sleep apnea
(OSA), according to new research.
OSA is characterized by repeated episodes
of complete or partial blockage of the upper
airway lasting 20 to 30 seconds during sleep,
which can reduce oxygen flow to vital organs.
“The longer the duration of asthma, the more
likely an individual is to develop OSA,” said
study author Dr. Mihaela Teodorescu from the
University of Wisconsin School of Medicine and
Public Health in Madison, Wisconsin, US. Left
untreated, OSA can lead to serious complica-
tions, including worsening asthma and cardio-
vascular disease.
The study involved a random sample of in-
dividuals participating in the population-based
prospective Wisconsin Sleep Cohort Study who
were recruited to undergo overnight polysom-
nography studies at 4-year intervals from 1988
through March 2013. Overall, there were 1,105
4-year follow-up intervals involving 547 individu-
als who were free of OSA (apnea-hypopnea in-
dex [AHI] of <5 events/hour) at baseline. [JAMA
2015;313:156-164]
Of 81 participants with asthma, 22 (27 per-
cent) developed incident OSA over the first
4-year follow-up interval, as compared to only
75 of 466 (16 percent) participants without asth-
ma. An analysis of all available 4-year intervals
showed there were 45 incident cases of OSA
among participants with asthma over the course
of 167 (27percent) 4-year intervals. By contrast,
there were 160 incident cases (17 percent) of
OSA among those without asthma (p difference
=0.007) over the course of 938 4-year intervals.
The differences in OSA risk were observed
despite the same average BMI changes in
patients with or without asthma during the
4-year follow-up intervals, said the authors.
Asthma was also associated with new-onset
OSA with habitual sleepiness (p=0.045).
In addition, asthma duration was related
to both incident OSA and OSA with habitual
sleepiness (p=0.01 and p=0.02, respective-
ly).
The findings lend further support to a po-
tential causal role of asthma in the devel-
opment of OSA, said the authors. However,
more studies investigating the mechanisms
underlying this association and the value of
periodic OSA evaluation in patients with asth-
ma are needed, they concluded.

FEBRUARY 2015 NEWS 11
Link between allergy and asthma clearELVIRA MANZANO
There is a clear connec tion between allergy
and asthma, and many patients have both
hay fever and asthma, says an allergy specialist.
Pharmacy assistants need to be aware that
patients coming in with allergic rhinitis may also
have undiagnosed asthma, said allergy special-
ist Vincent Crump of the Auckland Allergy Clinic
in Auckland New Zealand.
In atopic patients who have a genetic predis-
position to getting asthma, eczema or hay fever,
it is common to have both hay fever and asthma,
with one often being undiagnosed, Crump said.
“Many patients with allergic rhinitis related to
grass pollen will also get seasonal asthma when
their hay fever is very bad, and, because they
are more trou bled by their hay fever symptoms,
they might not seek help specifi cally for the
asthma symptoms.”
It is important that all patients with allergic
rhinitis are assessed by a doctor for asthma, he
said. How ever, asthma is not necessarily worse
in the spring months when pollen is abundant.
It also depends on what the allergic trigger for
the in dividual is, Crump said. “If they are allergic
to pollens, then their asthma could be worse in
spring or summer.
“However, if they are allergic to dust mites
or their pets, their symptoms could be worse in
win ter, when they spend more time locked up
indoors and wearing their woollen clothes which
har bor dust mites.”
Controlling both asthma and hay fever is
important if patients do have both diseases,
Crump said. “Patients with both hay fever and
asthma will have their asthma better controlled
when their rhi nitis is treated adequately, even
if their rhinitis symptoms are not their primary
concern.”
The role of pharmacistsPharmacists have a crucial role in educat-
ing asthma patients, said Jim Reid, deputy
dean of the University of Otago’s Dunedin
School of Medicine, Dunedin, New Zealand.
Reid did an informal study of asthma pa-
tients which found 30 percent could not tell
the dif ference between their reliever and pre-
venter inhalers. Many asthma patients do not
understand the importance of prophylaxis or
preventative medication, and commonly say
their blue reliever inhaler is the only one that
works. Another problem is poor inhaler tech-
nique, Reid said.
Pharmacists should be on the lookout for
asthmatics who regu larly pick up scripts for
reliever inhalers without any preventative
medication, he added.
All asthmat ics should have an “action
plan” which spells out when they need to
seek help, Crump said. Asthma patients
should be referred to a doctor if their reliever
inhaler is not reliev ing their symptoms, or
if they need to use their reliever more than
twice a week.

FEBRUARY 2015 NEWS 12
Certolizumab pegol improves productivity, social participation of patients with psoriatic arthritis LIANNE COWIE
Patients with psoriatic arthritis (PsA) can
benefit from treatment with certolizumab
pegol (CZP), which offers significant improve-
ments in productivity at home and at work and
also increases social participation, according to
a multinational group of researchers.
In their ongoing phase III, multicenter trial,
409 patients diagnosed with adult-onset active
psoriatic arthritis of ≥6 months’ duration were
randomized to placebo (n=136) or subcutane-
ous certolizumab pegol (400 mg loading dose
at weeks 0, 2, and 4 followed by 200 mg ev-
ery 2 weeks [n=138] or 400 mg every 4 weeks
[n=135]) for 24 weeks. The arthritis-specific
Work Productivity Survey was used to assess
the impact of psoriatic arthritis on paid work and
household productivity as well as participation
in social activities during the preceding month.
[Ann Rheum Dis 2015;74:44-51]
At baseline, 56.6 percent of placebo recipi-
ents were employed, compared with 60.1 per-
cent and 61.5 percent of patients who received
certolizumab pegol 200 mg or 400 mg, respec-
tively. At study end, the number of days of ab-
senteeism (full day of work missed) and pre-
senteeism (days where work productivity was
reduced by ≥50 percent due to arthritis) were
significantly reduced among employees who
received certolizumab
pegol, compared with
placebo (absenteeism
-1.0 – -1.8 vs -1.0 day,
respectively, and pre-
senteeism -3.0 – -3.8 vs
-0.3 days, respectively;
p<0.05). In addition, pa-
tients treated with certoli-
zumab pegol gained sig-
nificantly more household work days per month
(average 3.0–3.5 vs 1.0 day; p<0.05) and re-
ported greater participation in family, social, and
leisure activities.
“The rapid improvements seen in CZP-treat-
ed patients in paid work productivity, house-
hold productivity and participation in fam-
ily, social and leisure activities, alongside the
clinical improvements seen, suggest that CZP
is a potentially valuable treatment option for
PsA patients,” concluded the study authors,
led by Dr. A. Kavanaugh, Division of Rheuma-
tology, Allergy and Immunology, University of
California San Diego, California, US. “These
beneficial effects with respect to PsA patients’
workplace and household productivity could
ultimately result in gains in the quality of life
and in the economic burden of this chronic
inflammatory disease, particularly in those of
working age.”

FEBRUARY 2015 DRUG PROFILE 13
Lixisenatide: The latest GLP-1R agonist for glycemic control in type 2 diabetesThe advent of the incretin-based therapies, comprising two distinct classes – the
glucagon-like peptide 1 receptor (GLP-1R) agonists and dipeptidyl peptidase-4
(DPP-4) inhibitors – have provided clinicians with a much-needed fresh approach to
controlling glucose in type 2 diabetes. This drug profile describes lixisenatide, the
newest addition to the GLP-1R agonist class. Lixisenatide became available in 2012
following extensive investigations within the GetGoal phase III clinical trial program,
which included many Asian sites.
Cathy Chow, PhD
IntroductionResearch into the pathophysiology of type
2 diabetes has led to significant advances in
pharmacotherapy for this chronic disease. Chief
among these has been the development of
agents that modify the incretin system.
In non-diabetic individuals, the incretin sys-
tem amplifies insulin biosynthesis and secretion
via the action of two hormones, glucagon-like
peptide 1 (GLP-1) and glucose-dependent insu-
linotropic polypeptide (GIP). [Mol Cell Endocri-nol 2009;297:127-136, Diabetes 2007;56:1951-
1959] GLP-1 and GIP are released from the
gastrointestinal tract in response to eating,
stimulating release of insulin from the pancreatic
beta cells. In type 2 diabetic individuals, how-
ever, the incretin system is dysregulated; spe-
cifically, release of GLP-1 and GIP in response
to oral food intake is decreased, which conse-
quently reduces insulin synthesis and secretion
and, ultimately, impairs the incretin effect. [Mol Cell Endocrinol 2009;297:127-136, Diabetes
2007;56:1951-1959]
Two distinct pharmacologic approaches
have evolved in type 2 diabetes targeting the
incretin system: GLP-1R agonism and DPP-4
inhibition. DPP-4 inhibitors block endogenous
DPP-4, the enzyme that mediates breakdown
of GLP-1 and GIP, thereby increasing levels of
these hormones. [Lancet 2006;368:1696-1705,
Clin Ther 2012;34:993-1005, Int J Clin Pract 2006;60:1454-1470] Meanwhile, the GLP-1R
agonists mimic the action of GLP-1, exerting a
direct, pharmacologic, intrinsic biologic effect at
the receptor. [Drug Des Devel Ther 2013;8:25-
38] Liraglutide, exenatide (twice daily or once
weekly) and lixisenatide are the currently avail-
able GLP-1R agonists. These agents have dem-
onstrated efficacy, safety and tolerability, with a
lower risk of hypoglycemia than that observed
with either insulin or sulfonylureas. [Diabetes Obes Metab 2014;16:588-601]

FEBRUARY 2015 DRUG PROFILE 14
LixisenatideLixisenatide is a potent and selective GLP-1R
agonist. [Lyxumia Injection, Solution. Product
Information. March 2014] It is a 44-amino acid
chain peptide based on the structure of exen-
din-4, with the difference being that it is ami-
dated at the C terminal (proline removed and
replaced by six lysine residues). [Regul Pept 2010;164:58-64] Lixisenatide is indicated for
the treatment of adults with type 2 diabetes to
achieve glycemic control in combination with
metformin; metformin plus sulfonylurea; basal
insulin plus metformin; or basal insulin plus sul-
fonylurea; when these agents, together with diet
and exercise, do not provide adequate glycemic
control. [Lyxumia Injection, Solution. Product In-
formation. March 2014]
Pharmacology Mechanism of action
Lixisenatide has three main mechanisms of
action: (1) it stimulates insulin secretion when
there is increased blood glucose but not in nor-
moglycemia; (2) it suppresses glucagon secre-
tion without affecting the rescue mechanism of
glucagon secretion in hypoglycemia; and (3) it
may have insulinotropic activity based on ani-
mal studies, including enhancement of insulin
biosynthesis and stimulation of beta cell prolif-
eration. [Lyxumia Injection, Solution. Product
Information. March 2014]
Clinically, treatment with lixisenatide effec-
tively reduces glycated hemoglobin (HbA1c),
fasting plasma glucose and post-prandial glu-
cose levels. This last effect can be very pro-
nounced, differentiating lixisenatide from the
other GLP-1R agonists. [Core Evid 2011;6:67-
79] Interestingly, the loss of post-prandial glu-
cose control is thought to be a central factor for
the development of type 2 diabetes. [Diabetes
Care 2007;30:263-269, Diabetes Obes Metab
2013;15:642-649] Lixisenatide treatment may
also promote weight loss and reduce the need
for exogenous insulin. [Drug Des Devel Ther 2013;8:25-38]
Clinical efficacy
The GetGoal program of phase III random-
ized controlled clinical trials extensively investi-
gated the efficacy and safety of lixisenatide 20
µg once daily, either as monotherapy or add-on
therapy to basal insulin, metformin and/or sulfo-
nylurea, across the spectrum of type 2 diabetes
scenarios (Table). [Diabetes Ther 2014;5:367-
383, Diabetes Care 2013;36:2543-2550, Dia-betes Care 2011;54 Suppl 1:A784, Diabetes Care 2012;3:70-79, Diabetologia 2011;54 Suppl
1:A785, Poster 1010-P presented at the 72nd
Scientific Sessions of the American Diabetes
Table: GetGoal Phase III Clinical Trial Program
Study Lixisenatide intervention,
details
HbA1c (percent) FPG (mmol/L) PPG (mmol/L)
GetGoal-Mono (n=361)
monotherapy (1-step vs
2-step dose)-0.5*** to -0.7*** -0.9** to -1.1*** -3.1*** to -3.7***
GetGoal-F1 (n=482)
+ metformin (1-step vs
2-step dose)-0.4*** to -0.5** -0.56*** to -0.53** N/A
GetGoal-M (n=680)
+ metformin (evening vs
morning dose)-0.9*** to -0.8*** -0.81** to -1.19**
-4.5* (morning dose) NS
(evening dose)
GetGoal-S (n=855)
+ sulfonylurea ± metformin
-0.9*** -0.99*** -6.19***
GetGoal-P (n=484)
+ pioglitazone ±metformin
-0.9*** -1.16*** N/A
GetGoal-L-Asia (n=311)
+ basal insulin ± sulfonylurea
-0.8*** -0.4** -7.96***
GetGoal-L (n=496)
+ basal insulin ± metformin
-0.7** NS -5.54***
GetGoal-Duo-I (n=898)
+ optimally titrated basal insulin +
OAD-0.7*** +0.34 (NS) -3.09***
GetGoal-X (n=634)
versus exenatide ± metformin (non-
inferiority trial)-0.8 -1.22 (NS) N/A
All values are mean differences from baseline, significance level as compared with placebo. One-step dose increase was 10 to 20 μg; two-step dose increase was 10 to 15 to 20 μg. *p<0.05; **p<0.005; ***p<0.0005. Non-inferiority achieved at predefined margin of 0.4 percent. OAD, oral antidiabetic drug; FPG, fasting plasma glucose; PPG, post-prandial glucose; NS, not significant; N/A, not available. [Adapted from Diabetes Ther 2014;5:367-383]

FEBRUARY 2015 DRUG PROFILE 15
Association, June 8–12, 2012, Philadelphia,
PA, USA, Diabetes Obes Metab 2012;14:910-
917, Diabetes Care 2013;36:2489-2496, Dia-betes Care 2013;36:2497-2503, Diabetes Care
2013;36:2945-2951] These data collectively
demonstrated significant reductions in HbA1c,
fasting plasma glucose and post-prandial glu-
cose levels with lixisenatide monotherapy or
combination therapy, with either weight loss
or no weight gain. [Diabetes Obes Metab
2014;16:588-601]
Of note, the GetGoal-L-Asia trial was con-
ducted exclusively in patients from Japan, Ko-
rea, Taiwan and the Philippines. [Diabetes Obes Metab 2012;14:910-917] This was based on the
rationale that drugs targeting the incretin system
appear to be particularly effective in Asian pa-
tients as they tend to have a pathophysiology of
insulin deficiency more than insulin resistance,
with some evidence for a profound underly-
ing GLP-1 insufficiency. [Diabetes Obes Metab
2012;14:910-917, J Diabetes Invest 2010;1:8-23,
J Diabetes Invest 2010;1:56-59, J Diabetes In-vest 2012;3:70-79]
Dosing and administration
Lixisenatide is injected subcutaneously in the
thigh, abdomen or upper arm. It is administered
once daily within the hour prior to the first meal
of the day or the evening meal. The starting dose
is 10 µg once daily for 14 days, which is then in-
creased to 20 µg once daily as the maintenance
dose. If a dose is missed, lixisenatide should be
injected within the hour prior to the next meal.
When added to metformin, the metformin dose
should not require adjustment. When added to
basal insulin or sulfonylurea, however, a reduc-
tion in these existing therapies may be consid-
ered to reduce the risk of hypoglycemia, de-
pending on the individual response. [Lyxumia
Injection, Solution. Product Information. March
2014]
Adverse events
Lixisenatide was generally well tolerated in
clinical trials, with gastrointestinal events (nau-
sea and vomiting) being the most frequently re-
ported, which were mostly mild and transient.
[Lyxumia Injection, Solution. Product Informa-
tion. March 2014] Severe symptomatic hypogly-
cemia was uncommon.
Future directions Lixisenatide is the first once-daily prandial
GLP-1R agonist, and the latest GLP-1R ago-
nist, to become available. It is the most stud-
ied agent in its class in combination with basal
insulin and, given its effectiveness, tolerability
and safety as add-on therapy to basal insulin
or oral antidiabetic drugs, it represents an im-
portant, new pharmacologic option for type 2
diabetes.

PPI Therapy: Safety Considerations
Professor Prateek Sharma
Associate Professor of Medicine, Division of Gastroenterology and Hepatology, University of Kansas School of Medicine, Kansas City, Missouri, USA
Proton-pump inhibitors (PPI) are generally safe drugs. However, some PPIs do have a few important safety considerations.
The first safety consideration is with regard to the use of PPIs in patients receiving clopidogrel. The efficacy of clopidogrel is dependent on its conversion to active metabolites via cytochrome P2C19. It has been hypothesized that PPIs competitively inhibit clopidogrel activation. The Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation (PRINCIPLE) – Thrombolysis in Myocardial Infarction (TIMI) 44 study showed that in patients undergoing elective percutaneous coronary intervention, clopidogrel-receiving patients on PPIs showed significantly lower inhibition of platelet aggregation (23.2%) compared with those not on PPI (35.2%; p=0.02).1 However, other TIMI trials suggested that PPIs should not be withheld from patients on clopidogrel or prasugrel when it is clinically indicated.1
It should also be emphasized that PPI-related attenuation of clopidogrel efficacy is not a class effect. For example, dexlansoprazole has no clinically significant effect on clopidogrel active metabolite pharmacodynamics as measured by inhibition of platelet aggregation and inhibition of platelet reactivity index (Figure 3).2 As a result, the US Food and Drug Administration (FDA) has differentiated the PPIs in the updated label of clopidogrel: “Avoid concomitant use of [clopidogrel] with omeprazole or esomeprazole … Dexlansoprazole, lansoprazole and pantoprazole had less effect on the antiplatelet activity of [clopidogrel] than did omeprazole or esomeprazole.3
The US FDA also warns that PPIs may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine, especially in patients who received high-dose, long-term PPI therapy (a year or longer).4 In addition, PPIs may also be associated with an increased risk of Clostridium difficile-associated diarrhea, especially in hospitalized patients.5 Hence, the US FDA recommended that patients
should use the lowest PPI dose and the shortest duration of therapy required to treat the underlying condition.
Overall, some safety concerns have been raised regarding the use of PPIs. While literature does support some of these risks, serious adverse events are quite rare. Like any medical intervention, the clinical risk/benefit of PPI therapy should be evaluated, and should not be withheld when benefits outweigh risks. Further minimize risks of PPI therapy by making rational decisions in PPI choice and administration. REFERENCES:1. Ho PM, et al. JAMA 2009;301:937-944.2. Frelinger AL III et al. J Am Coll Cardiol. 2012;59:1304-1311.3. Plavix® (clopidogrel) prescribing information. Bridgewater, New Jersy, USA: Sanofi-Aventis; 2013.4. US Food and Drug Administration. FDA Drug Safety Communication: Possible increased risk of fractures of the hip, wrist,
and spine with the use of proton pump inhibitors. Maryland: US Food and Drug Administration; 2011.5. US Food and Drug Administration. FDA Drug Safety Communication: Clostridium difficile-associated diarrhea can
be associated with stomach acid drugs known as proton pump inhibitors (PPIs). Maryland: US Food and Drug Administration; 2012.
〉 Figure 3. Effect of dexlansoprazole vs omeprazole on clopidogrel platelet inhibition2
Discussion with Professors Peura & Sharma
0.24.7
35.2
Dexlansoprazole 60 mgb
Positive control (Omeprazole 80 mg)b
IPA = Inhibition of PlateletAggregation; PRI = PlateletReactivity Index.aADP 5 µM.bN=40 randomized per arm.
0
20
40
% Decrease in IPAa
With Clopidogrel and PPICoadministration for 9 Days
% Decrease in Inhibition of PRIWith Clopidogrel and PPI
Coadministration for 9 Days
Ch
ang
e, %
22.5
Sponsored as a service to the medical profession by Takeda Pharmaceuticals (Asia Pacific) Pte. Ltd. For Healthcare Professionals Only.
Editorial development by MIMS MedComms. The opinions expressed in this publication are not necessarily those of the editor, publisher or sponsor. Any liability or obligation for loss or damage however so arising is hereby disclaimed. © 2015 MIMS. All rights reserved. No part of this publication may be reproduced by any process in any language without the written permission of the publisher.
MIMS Pte Ltd, 6 Shenton Way, #15-08, OUE Downtown 2, Singapore 068809. Tel: +65-6290 7400 Fax: +65-6290 7401 Email: [email protected] Website: www.mims.com D
EX-F
PA-1
2201
4-20
Q What is the basis of the 25%-75% ratio of drug release with dexlansoprazole capsule?
A Several studies were conducted to determine the optimal regimen for this unique drug delivery system, and the 25%-75% ratio was found to be the most efficient in prolonging the area under the curve of dexlansoprazole.
Q Can dexlansoprazole be given via nasogastric tube (NGT)?
A The capsule can be opened and the granules administered with water via a French 16 NGT or larger.
Q Will a prokinetic affect the pharmacokinetics of dexlansoprazole?
A The effect of a prokinetic on dexlansoprazole has not been studied. However, the release of dexlanso-prazole from the microgranules is not time-dependent, but pH dependent. Hence, the second peak of drug release will occur once the microgranules reach the appropriate site in the intestines, regardless of time. A prokinetic may increase this by only a few seconds.
Q How do you manage a patient with non-erosive reflux disease that does not respond to high-dose proton-pump inhibitors (PPI), in the setting where pH monitoring is not available, as in the case in most of Asia?
A Ideally, these patients should undergo pH monitoring. However, in the absence of this modality, you may presume that the patient has a non-acid disease. You may
want to consider giving a prokinetic or agents that decrease visceral hypersensitivity,
such as tricyclic antidepressants.
Q What is the role of PPIs in the treatment of extra-esophageal reflux disease?
A The management of extra-esophageal reflux disease is directed at
relieving symptoms. In this context, remember that it is also multifactorial.
Hoarseness, chronic cough, or asthma, may be due to reflux, smoking,
angiotensin-converting enzyme inhibitors, voice overuse, post-nasal
drip or allergies. Reflux may be treated with PPIs, but other causes
should also be identified and treated as well.
Q When should dexlansoprazole be given in relation to clopidogrel to minimize
drug interaction?
A There is currently no data evaluating how timing of administration of
dexlansoprazole affects interaction with clopidogrel. However, considering that
dexlansoprazole has minimal impact on platelet aggregation, you can probably give
it at any time in relation to clopidogrel.
Q From 15% to 30% of Asians are poor metabolizers of PPIs and other substrates
of CYP2C19. Does this affect the safety of PPIs?
A In poor metabolizers, there may be an increase in PPI effect, with a corresponding increase in adverse events (AE). In these patients, AEs should be monitored. Further minimize risks by using PPIs that are less likely to cause drug interactions.
Q Should acid suppressive therapy to prevent or treat gastrointestinal (GI) bleeding be given to patients who just underwent percutaneous cardiac intervention?
A Patients at high risk of GI bleeding due to age, history of gastric ulcers, or history of gastric ulcer bleed, should receive gastroprotection, and a PPI should be considered. Many of these patients would be receiving clopidogrel. Based on the recommendation of the US Food and Drug Administration, it is best not to take risks, and choose PPIs that are less likely to interact with clopidogrel (eg, dexlansoprazole, lansoprazole, or pantoprazole) may be used.
Patients with high-risk, active bleeding should be treated with endoscopic haemostasis and intravenous PPI for 72 hours followed by oral PPI.
The decision to discontinue clopidogrel depends on how long the stent has been in place. If the stent has been deployed over a year ago, clopidogrel may be safely discontinued. If it has been in place from 6 to 12 months, discuss the safety of discontinuing clopidogrel with the patient’s cardiologist.

FEBRUARY 2015 RESEARCH REVIEWS 17
Zonisamide an effective treatment for alcohol dependence
Zonisamide appears to have similar efficacy
to topiramate in the treatment of patients
with alcohol dependence, but may be better tol-
erated, according to a recent study.
Under double-blind placebo-controlled con-
ditions, zonisamide was compared to two anti-
convulsant drugs, topiramate and levetiracetam
(positive controls), in 85 alcohol-dependent
patients (37 women) aged 21–65 years. Alco-
hol dependence was defined as consuming
≥35 standard drinks (for men) or ≥28 standard
drinks (for women) per week consecutively
for at least 4 weeks. [J Clin Psychopharmacol 2015;35:34-42]
The patients were randomized to levetirace-
tam 2000 mg/day (n=21), topiramate 300 mg/
day (n=21), zonisamide 400 mg/day (n=19),
or placebo (n=24) for 14 weeks (including a
2-week taper period). Neuropsychological eval-
uations were performed at week 1 (before drug
therapy) and at week 12 (at the end of mainte-
nance therapy) to evaluate cognitive function-
ing, including working memory, language func-
tion, executive function, visual processing, and
psychomotor performance.
At study end, both zonisamide and topiramate
significantly reduced the number of drinks con-
sumed per day, the percent days drinking, and
the percent days heavy drinking. Levetiracetam
only reduced the percent days heavy drinking.
Topiramate was found to increase mental slow-
ing, while both topiramate and zonisamide were
associated with modest reductions in verbal flu-
ency and working memory.

FEBRUARY 2015 RESEARCH REVIEWS 18
Catheter ablation beneficial for elderly patients with AF
Catheter ablation maintains normal sinus
rhythm and lowers stroke risk and mortal-
ity among elderly patients with atrial fibrillation
(AF).
Researchers determined the long-term safety
and efficacy of the procedure in 261 patients
aged ≥75 years who had AF; they compared
observed outcomes between these patients and
an additional 63 patients who were eligible for
the study, but who either declined or were un-
suitable for ablation. All patients were followed-
up every 3 months. The primary endpoints for
analysis were maintenance of normal sinus
rhythm and the incidence of stroke, death, and
major bleeding. [Heart Rhythm 2015;12:44-51]
After a mean follow-up of 3 ± 2.5 years, 216
(83 percent) patients who underwent catheter
ablation remained in normal sinus rhythm com-
pared with 14 (22 percent) patients who did not
(p<0.0001). The 1- and 5-year survival rates
among the patients with normal sinus rhythm
following ablation were 98 percent and 87 per-
cent, respectively. Among patients who under-
went ablation but did not maintain normal sinus
rhythm, the survival rates were 86 percent and
52 percent, respectively. The 1- and 5-year sur-
vival rates among the patients who did not un-
dergo ablation were 97 percent and 42 percent.
Normal sinus rhythm was identified as an in-
dependent parameter favoring survival (hazard
ratio [HR], 0.36, 95% confidence interval [CI],
0.2–0.63; p=0.0005). In contrast, older age
(HR, 1.09, 95% CI 1.01–1.16, p=0.02) and an
ejection fraction <40 percent (HR, 2.38, 95%
CI, 1.28–4.4; p=0.006) were found to be unfa-
vorable parameters.

FEBRUARY 2015 RESEARCH REVIEWS 19
Sufentanil sublingual tablet system a safe, effective option for postoperative pain
The novel sufentanil sublingual tablet system
(SSTS) is both safe and effective for man-
aging postoperative pain, according to a recent
US-based study.
In the phase III double-blind trial, which was
conducted at 13 hospitals in the US between
March 2012 and January 2013, 178 male and
female patients with moderate-to-severe post-
operative pain were randomized to the SSTS
(n=128) or placebo (n=50) after undergoing
open abdominal surgery. The SSTS dispensed
a 15 µg sufentanil tablet with a 20-minute lock-
out, and an identical system was used to dis-
pense the placebo. Pain intensity scores were
recorded at baseline and up to 72 hours after
treatment initiation. Patient and health care pro-
vider global assessments of the method of pain
control were also recorded. [Reg Anesth Pain Med 2015;40:22-30]
The mean summed pain intensity differ-
ence (SPID) over 48 hours was significantly
higher among patients in the SSTS group com-
pared with placebo recipients (105.60 vs 55.58;
p=0.001). Moreover, significantly higher mean
SPID and total pain relief scores were observed
among patients in the SSTS group at all time-
points from 1 or 2 hours up to 72 hours after
treatment initiation. Significantly more “good”
or “excellent” ratings of pain relief were also
recorded by patients and health care providers
for the SSTS compared with placebo at all time-
points (p<0.001). Safety parameters were simi-
lar between the two groups.

FEBRUARY 2015 RESEARCH REVIEWS 20
Rice consumption not associated with CVD risk
Publicity surrounding the possible associa-
tion between rice consumption and arsenic
exposure has raised concerns that habitual rice
consumption may increase the risk of developing
cardiovascular disease, but there is no evidence
of any such association in the US population.
The study investigators prospectively exam-
ined the association between consumption of
white and brown rice and cardiovascular dis-
ease risk among 207,556 women and men
who were free of cardiovascular disease and
cancer at baseline. A total of 73,228 women
were participants in the Nurses’ Health Study
(1984-2010), 92,158 women were participants
in the Nurses’ Health Study II (1991-2011), and
42,170 men were participants in the Health
Professionals Follow-Up Study (1986-2010).
Rice consumption was assessed using food-
frequency questionnaires and the incidence
of fatal and non-fatal cardiovascular events
(including coronary artery disease and stroke)
was recorded from self-reports or obtained
from patient medical records. [Am J Clin Nutr 2015;101:164-172]
A total of 12,391 cases of cardiovascular dis-
ease (7,719 coronary artery disease and 4,672
stroke) were observed over 4,393,130 person-
years of follow-up. After adjusting for major
cardiovascular risk factors, consumption of ≥5
servings of rice per week compared with <1
serving per week did not lead to a remarkable
increase in the risk of developing cardiovascular
disease, regardless of whether individuals con-
sumed white rice (hazard ratio [HR], 0.98, 95%
confidence interval [CI], 0.84–1.14) or brown
rice (HR, 1.01, 95% CI, 0.79–1.28).

FEBRUARY 2015 RESEARCH REVIEWS 21
AfIibercept effective in Japanese patients with wet AMD
Aflibercept, a novel anti-vascular endothelial
growth factor agent, has been found to be
both safe and effective in the treatment of Japa-
nese patients with wet age-related macular de-
generation (AMD).
In the double-masked, multicenter VIEW 2
trial, 1,240 patients from 172 sites in Europe,
the Middle East, Asia Pacific, and Latin America
were randomized to intravitreal aflibercept 0.5
mg every 4 weeks, 2 mg every 4 weeks, 2 mg
every 8 weeks after 3 monthly injections, or ra-
nibizumab 0.5 mg every 4 weeks. Vision mainte-
nance and best corrected visual acuity (BCVA)
were assessed at week 52. The present report
relates to a subgroup analysis that was per-
formed using data obtained from 101 Japanese
patients included in the trial. [Br J Ophthalmol 2015;99:92-97]
All of the Japanese patients treated with in-
travitreal aflibercept (n=70) maintained their vi-
sion at week 52, compared with 96 percent of
the Japanese patients treated with ranibizumab.
BCVA was improved in all treatment groups,
with decreases in central retinal thickness and in
the mean area of choroidal neovascularization
present in all treated patients. The incidence
of adverse events was also similar among the
treatment groups.
The researchers note that outcomes from the
Japanese population were consistent with those
from the total VIEW 2 population.

FEBRUARY 2015 RESEARCH REVIEWS 22
Exercise therapy can reduce need for total hip replacement in patients with hip OA
Patients with radiographic hip osteoarthritis
(OA) who have mild-to-moderate symp-
toms may find that exercise therapy can reduce
the need for total hip replacement, according
to a recent study.
The analysis was based on data collected
from the long-term follow-up of 109 patients
aged 40–80 years with OA who participated
in a randomized trial investigating the effi-
cacy of exercise therapy plus patient educa-
tion or patient education alone for maintain-
ing the native hip. Patient education consisted
of three group sessions while the exercise
therapy program was designed for patients
with hip OA and included strengthening, flex-
ibility, and functional exercises performed 2–3
times a week for 12 weeks. [Ann Rheum Dis
2015;74:164-169]
During the 3.6–6.1-year follow-up period,
22 patients in the exercise therapy group un-
derwent total hip replacement compared with
31 patients who only participated in the edu-
cation sessions. The 6-year cumulative sur-
vival of the native hip was 41 percent and 25
percent, respectively (p=0.034). Participation
in the exercise program had a protective effect
(hazard ratio 0.56, 95% confidence interval
0.32–0.96). Although self-reported hip func-
tion was better among patients in the exercise
group, pain and stiffness were not significant-
ly different between the groups.
The researchers concluded that their find-
ings support offering exercise therapy as a
first-line treatment for hip OA in patients with
mild-to-moderate symptoms.

FEBRUARY 2015 FEATURE 23
Where there’s smokeA haze has periodically wafted over Southeast Asia for 20 years. But despite rising
public health concern, the problem remains as opaque as the smoke itself, Mike Ives
reports.
At the age of 13, Tan Yi Han could not see the
edge of his schoolyard. It was 1998 in Sin-
gapore, the wealthy city-state known for its tidy
streets and clean, green image. But for much
of that particular school year, clouds of smoke
shrouded the skyline. The record-setting air pol-
lution, which had begun in 1997 and lasted for
months, caused a 30 percent spike in hospital
visits. It would later be remembered as one of
Southeast Asia’s worst-ever “haze episodes”.
Haze episodes have occurred in Southeast
Asia nearly every year since. Back in 1998, and
for years afterwards, Tan didn’t think too deeply
about them. Yet at some point in his late 20s,
he began to wonder: where did the haze come
from? And why did it keep coming back?
Air pollution kills around 7 million people
every year, according to the World Health Or-
ganization (WHO), accounting for one in eight
deaths worldwide in 2012. The main causes of
death were stroke and heart disease, followed
by chronic obstructive pulmonary disease
(COPD), lung cancer, and respiratory infections
among children.
It is especially bad in the Asia-Pacific region,
which has a population of over 4.2 billion and
high population density. China and India alone,
with a combined population of around 2.7 bil-
lion, are both enormous sources and victims of
air pollution.
In 2010, 40 percent of the world’s premature
deaths caused by air pollution were in China,
the world’s largest emitter of carbon dioxide,
according to a survey published in the Lancet. The University of Hong Kong’s School of Pub-
lic Health reported more than 3,000 premature
deaths in the city in 2013, and the situation in
many mainland Chinese cities is reckoned to
be far worse. A poll by the US Pew Research
Center found that 47 percent of Chinese citizens
thought air pollution to be a “very big” problem
in 2013 (up from 31 percent in 2008). It is now
a central focus for many Chinese environmental
groups and a growing source of anxiety for the
country’s leadership.
Similar health concerns are building in India,
where air pollution is now the fifth-leading cause
of death. Between 2000 and 2010, the annual
number of premature deaths linked to air pol-
lution across India rose six-fold to 620,000, ac-
cording to the Centre for Science and Environ-

FEBRUARY 2015 FEATURE 24
ment, a public-interest research and advocacy
group in New Delhi. In May 2014, the WHO said
that New Delhi had the worst air of 1,600 cities
surveyed worldwide and that rising air pollution
had increased the risk of strokes, cancers and
heart disease. Another 2014 study has linked a
significant drop in India’s wheat and rice crop
yields to rising levels of two air pollutants – black
carbon from rural cooking stoves and ground-
level ozone formed from motor vehicle exhausts,
industrial emissions, and chemical solvents –
between 1980 and 2010.
In both China and India, air pollution is one
consequence of a massive exodus from farm to
city that has occurred in recent decades. The
change has contributed to rising emissions from
both vehicles and factories, especially coal-fired
power plants, and an emerging middle class
that increasingly desires a range of consumer
goods that are common in Europe and the US.
Southeast Asia has encountered similar
problems in recent decades as its economies
and populations have boomed. In fact, accord-
ing to the WHO, nearly one million of the 3.7 mil-
lion people who died from ambient air pollution
in 2012 lived in Southeast Asia.
But on top of smokestacks and tailpipes, the
region faces an added burden: smoke haze pro-
duced in Indonesia that is a by-product of the
world’s US$50 billion palm-oil industry.
In the summer of 2013, a plane carried Tan Yi
Han over the Straits of Malacca to Pekanbaru,
the capital of Riau province, the largest palm-
oil production region in Indonesia. Tan, then a
28-year-old financial consultant, was volunteer-
ing with the Global Environment Centre, a Ma-
laysian group that has worked for years to pre-
vent and mitigate haze. He travelled to the heart
of neighbouring Indonesia, just after a record-
breaking haze episode hit peninsular Malaysia.
On a driving tour in Riau, he saw endless
acres of burned-out landscapes. Fires had turned
swampy peat bogs, the area’s natural vegeta-
tion, into land whose parched surface resembled
charcoal. These fires are to dry out the peatlands
for agricultural uses, mainly the cultivation of oil
palms. But in some villages, fires had even de-
stroyed existing oil palm trees that belonged to
multinational companies or local farmers.
Tan had a memorable encounter in the village
of Rantau Bais. A couple there plied him with tea
and snacks, then quietly asked if he could spare
any of his own food for them. Their daughter
had developed a respiratory problem because
of the haze. The surprise medical bill, coupled
with the fire destroying their oil palm crops, had
left the family penniless and hungry.
Until that moment, he had mostly thought of
peat blazes as “forest fires,” as they are often
called in media reports. But here was a visceral
reminder that the fires affect working land and
real people. “It really touched me,” said Tan. “I
made a promise to myself that I’d do my best
to prevent them from suffering from fires again.”
It was an issue, he felt, that required far more
public discussion – and when the time was right,
action. “I must get more people involved,” he
had thought, “and turn this into a movement.”
Hazy skies may all look similar, but the emis-
sions from any particular source are unique. A
factory smokestack in Beijing releases a differ-
ent mix of chemical compounds into the atmo-

FEBRUARY 2015 FEATURE 25
sphere than an automobile tailpipe in New Delhi
does. And the extent of pollution in a given city
will depend on how carefully emissions are con-
trolled, and how easily they can be dispersed.
Vehicle and factory emissions have been
analysed for decades in high-income countries,
but haze smoke, and its impact on health, is not
well understood. “Not many people have in-
vestigated it even though it’s a very important
phenomenon,” said Mikinori Kuwata, an atmo-
spheric chemist at Singapore’s Nanyang Tech-
nological University.
Unlike factory and vehicle emissions, wildfire
smoke is not regulated by tailpipe scrubbers,
catalytic converters or other pollution-mitigating
applications. The composition of the smoke also
varies widely according to the type of material
that is burning. Peatlands, for example, typically
take a longer time to burn than drier matter – just
as a damp piece of wood takes longer to burn
in a campfire. According to the US Environmen-
tal Protection Agency, peat fires burn at lower
temperatures and produce smoke that is more
harmful, and in larger quantities, than the aver-
age forest fire or grassland fire does.
The emissions from a given peat fire will large-
ly depend on the peat’s composition, its burning
temperature and how far below the ground the
fire occurs. But such details aren’t yet available
in Indonesia, whose peatlands cover an area
roughly the size of the UK. As a result, Kuwata
told me, “We do not have a very reliable inven-
tory” of the country’s peatland fire data. Kuwata
burns Indonesian peat in his Singapore labo-
ratory to study its chemical properties, but his
work is limited, he said, because he can never
be sure whether his experiments mirror reality.
Indonesia has an enormous repository of
tropical peatlands – and, for a generation, areas
of these have been burned to prepare the land
for the cultivation of oil palms. Peat smoke now
contributes around 40 percent of Indonesia’s
overall greenhouse gas emissions. Palm oil is
an ingredient in a range of consumer products,
from lipstick to ice cream. Yet it has also helped
to give its source country the dubious distinction
of being the world’s third-largest greenhouse
gas emitter after China and the US – as well as a
leading source of hazardous smoke haze.
On a summer afternoon, the skies were a
milky white in Riau, the Indonesian province that
produces about a quarter of Indonesia’s palm
oil. My first stop was the headquarters of WALHI,
an NGO in the city of Pekanbaru that lobbies the
Indonesian government for action on haze and
other environmental problems.
I arrived at WALHI’s headquarters, a low-rise
residential building near the Pekanbaru airport,
just as a group of farmers and environmental
activists were discussing haze, over coffee and
cigarettes, with Sri Nurhayati Qodriyatun, a re-
searcher for the Secretary General of Indone-
sia’s parliament.

FEBRUARY 2015 FEATURE 26
Qodriyatun said her boss had dispatched her
to Riau to compile a report on haze. At the meet-
ing, she explained that, according to govern-
ment estimates, forest fires were generally not
occurring in areas owned by large plantations.
The crowd stirred.“Government statements about haze are
false!” shouted an activist from a local NGO,
Forest Rescue Riau Network. “And there’s no
coordination between ministers – they just pass
the blame around!”
The exchange underscored the long-running
debate across Southeast Asia about who, ex-
actly, is responsible for Indonesia’s peat fires.
Farmers and environmental groups often ac-
cuse companies, many of which are headquar-
tered in Singapore or Malaysia, of malfeasance.
But many companies say such criticism is over-
blown, and that they have largely reformed their
destructive land-clearing practices in recent
years through voluntary reform initiatives like the
Roundtable on Sustainable Palm Oil, an indus-
try-led consortium.
Whoever is right, said Qodriyatun, the fires
have damaged Indonesia’s international reputa-
tion, and the Indonesian government pays little
attention to their health implications in Riau and
beyond.
“Personally, I don’t think the government is
managing this well,” she told me after the meet-
ing. “Usually they just react after the fires start,
but they should think more about prevention.”
Peat fires, though, are notoriously hard to
predict and extinguish. They start and spread
easily, and sometimes uncontrollably, depend-
ing on conditions like wind speed, the depth of
the soil and the dryness of the air.
“It’s really hard to know how bad a fire will be
when it starts,” said Dedy Tarsedi, a farmer in
the Riau village of Bungaraya. We were sitting in
a roadside café flanked by oil palm trees. Tarse-
di told me that oil palm is the crop of choice for
Bungaraya farmers because it is more valuable
than paddy rice. A hectare of oil palm, he said,
typically earns a farmer around 48 million Indo-
nesian rupiah (nearly US$4,000) per year. Paddy
rice, by contrast, brings in just 40 million rupiah.
But as oil palm cultivation has increased in
the village, so have fires. And they affect both
corporate plantations and smallholder farmers.
“If a fire happens and we can’t control it, we’ll
report it,” said Maman, a Bungaraya farmer. But
sometimes, even helicopters are powerless to
stop the burning, he added. “And during the re-
ally bad fires, a lot of the kids cough and end up
at the clinic with health problems.”
In 2009, Indonesia passed a law banning
fires on peat plantations. Farmers in Bunga-
raya told me that, as a result, they had started
to clear peat bogs manually, without using fire.
But Tarsedi said manual clearance is more la-
bour-intensive and requires extra fertilisers. And
that, he said, requires extra time and money that
most farmers don’t want to part with.
When the wind blows from the west, smoke
can whip east across the Straits of Malacca and
into both Singapore and Kuala Lumpur (the
capital of nearby Malaysia) – collectively home
to about 7 million people. Southeast Asia is not
the only place where the burning of vegetation
occurs over large areas; most of the world’s fires

FEBRUARY 2015 FEATURE 27
occur in Africa and South America. But South-
east Asia’s fires are unique, says Miriam Marlier,
an atmospheric researcher at Columbia Univer-
sity, because they occur so close to dense ur-
ban centres.
There are no comprehensive studies on how
repeated exposure to peat smoke affects human
health over the long term, much less how peat
smoke’s chemical properties differ from other
kinds of biomass smoke. Yet emerging research
offers early clues.
US researchers have found that peat fires
in the southern states during the summer of
2008 caused a spike in emergency room visits
for heart failure and asthma-related respiratory
complications. In a follow-up study, published in
June 2014, they burned semi-charred peat from
the fires in the vicinity of lab mice. Subsequent
pulmonary problems in the mice were mainly
linked to coarser-grained smoke particles and
cardiac problems to finer-grained particles.
A primary concern from a health perspective
is that peat fires tend to generate larger amounts
of fine-grained particulate matter, called PM2.5,
than normal forest fires. That is worrying main-
ly because finer-grained particles are thought
to penetrate further into the bloodstream than
coarser ones do, posing a potentially higher risk
to the heart and other internal organs. Finer-
grained particles are also harder to block with
the simple surgical masks that many people in
Asian cities have traditionally worn as protection
against air pollution.
A widely cited 2012 study, published in the
journal Environmental Health Perspectives, esti-
mated that about 339,000 deaths between 1997
and 2006 were associated with landscape fires.
About four in five deaths were linked to chronic,
rather than sporadic, exposure. Sub-Saharan Af-
rica and Southeast Asia accounted for 157,000
and 110,000 deaths, respectively, and the rate
of mortality spiked during years dominated by
El Niño weather phenomenon, which typically
correlates with drier conditions in Southeast
Asia. “Reducing population level exposure to
air pollution from landscape fires is a worthwhile
endeavor that is likely to have immediate and
measurable health benefits,” the researchers
concluded.
Another 2012 study, by Miriam Marlier and
other scientists from American and British insti-
tutions, found that between 1 and 11 per cent
of Southeast Asia’s population was repeatedly
exposed to pollution above the WHO’s recom-
mended air quality levels during sporadic haze
episodes between 1997 and 2006. Elevated
exposure during El Niño years caused around
15,000 cardiovascular-linked adult deaths per
year, the researchers wrote. Roughly two-thirds
of those were linked to fine-grained PM2.5 par-
ticles, while the other third were linked to levels
of ozone. However, there was not enough evi-
dence available to determine exactly how the
toxicity of PM2.5 in peat fires differed from that
of PM2.5 emissions in American cities.
Some scientists suggest that peat smoke’s
long-term effects on humans may be broadly
similar to those of urban air pollution, which also
includes PM2.5 particles. No one is sure be-
cause so little research has been done to test
the theory.
Rajasekhar Balasubramanian, an American

FEBRUARY 2015 FEATURE 28
environmental engineer who studies haze at the
National University of Singapore, speculates that
long-term exposure to haze episodes could po-
tentially make the population less healthy over
time, even if people continue to live long lives. In
a 2013 study, he and his colleagues found that
the air above Singapore during a smoke haze
episode contained arsenic, chromium, cadmi-
um and other carcinogenic elements. They esti-
mated that normal urban levels of PM2.5 pollu-
tion would cause about 12 out of every million
Singaporeans to develop cancer over a lifetime,
but if haze were to occur for 10 days per year
over 70 straight years, the number of likely can-
cer cases would increase by nearly half.
Yet there still is no coordinated international
effort to analyse haze in a truly interdisciplinary
fashion. That is partly due to the sporadic and
unpredictable nature of haze, Balasubramanian
said: Southeast Asia’s highly variable weather
makes it tricky to predict when haze will appear
or where it could spread. He likens a particle of
peat smoke to a grasshopper that jumps into
the air, shoots along horizontally, then quickly
zooms back to earth – only to jump again.
Another problem, Balasubramanian said, is
that the general public does not yet view haze as
a serious health threat. “People view it as, ‘Oh,
yeah, it’s a problem that occurs in Indonesia’,” he
told me one afternoon in his office at the National
University of Singapore. For governments and
funding bodies, “the priority’s more mitigation:
how to mitigate human exposure to this haze is-
sue, rather than to study the problem itself”.
The task of mitigating pollution is also cloud-
ed by politics. Countries in Southeast Asia have
little control over what blows across their bor-
ders: unlike the European Union, the Associa-
tion of Southeast Asian Nations (ASEAN) lacks
the legal authority to force its members to act
against their own interests.
A case in point is ASEAN’s 2002 trans-bound-
ary haze agreement, a non-binding document in
which the group’s 10- member states pledged
to prevent and monitor peat fires. The agree-
ment called for technology exchanges and
other measures to improve regional dialogue
and cooperation on haze. It was initially hailed
as a landmark achievement, but until Septem-
ber 2014, Indonesia’s parliament had refused to
ratify it. Laode M. Syarif, an environmental law-
yer based in the Indonesian capital of Jakarta,
said that was mainly because Indonesia has
long tried to use the haze agreement as a way
to leverage Singapore into overturning a refusal
to extradite Indonesian citizens who are wanted
for crimes in their homeland.
ASEAN tends to view economic develop-
ment, national sovereignty and mutual non-in-
terference as its highest priorities, said Helena
Varkkey, a senior lecturer in the Department of
International and Strategic Studies at the Uni-
versity of Malaya. In her view, ASEAN has taken
a mild-mannered approach to haze fighting out
of deference to powerful palm-oil companies,
many of them based in Singapore or Malaysia.
Indeed, many analysts have said that Indo-
nesia’s land concessions – areas allocated for
commercial plantations – are deeply entwined
with corruption. A popular joke has it that, if In-
donesia’s overlapping concession maps were
all counted as national territory, the country

FEBRUARY 2015 FEATURE 29
would grow in size. But companies and offi-
cials mostly refuse to share those maps with the
public. “It’s a mess,” said Andika Putraditama,
a research analyst at the Jakarta office of the
World Resources Institute, a research organisa-
tion headquartered in Washington, DC. It’s also
another reason why Indonesia’s peatlands con-
tinue to burn.
Against this backdrop, Tan Yi Han, the Singa-
porean financial consultant and self-styled haze
activist, is hoping to influence the regional debate
on haze. In early 2014, he founded a citizens’ or-
ganisation called People’s Movement to Stop
Haze, or PM Haze, to kick-start the discussion.
“My gut feeling is, we need influence,” Tan
said at a Sunday-evening PM Haze meeting.
There was only one other participant: Putera
Zenata, an Indonesian schoolteacher who had
joined the group after finding Tan online. The
venue was Zenata’s modest apartment in a mid-
dle-class Singapore neighbourhood.
In June 2014, one of Tan’s hometown news-
papers, the Independent, dubbed him “Singa-
pore’s intrepid haze fighter”. But PM Haze, with
10 active members and no outside funding, is
well behind many established advocacy and re-
search groups that fight air pollution elsewhere
in Asia. In New Delhi, the Centre for Science and
the Environment has proposed specific ways
that the government could tackle air pollution –
for example, by cracking down on open fires.
And in Beijing, the Institute of Public and Envi-
ronmental Affairs is promoting a pollution-moni-
toring mobile phone app as a way of ramping up
pressure on polluting companies.
By his own admission, Tan has very little ex-
perience in the non-profit sector. He told me that
he has no plans to pressure the government or
companies into action – at least not yet. For the
moment, he said, PM Haze is simply trying to
learn about the problem, in all its complexity,
and then communicate its findings to the Sin-
gaporean public. In early November 2014, the
group developed the content for an information-
al “haze exhibition” in Singapore that drew an
estimated 800 visitors. And in the longer term,
Tan said, they would like to film a documentary
in Indonesia.
“My personal goal is to stop haze by 2023,” he added casually.
That could be a pipe dream. But according to
Wilson Ang, Assistant Director for Sustainability
at the Singapore Institute of International Affairs,
the haze of June 2013 made the Singaporean
public “much more involved” in the issue. Along
with PM Haze, the episode spawned the creation
of the Haze Elimination Action Team, another
grassroots community group. Both groups have
since gone on site visits to Indonesia, opened
dialogues with palm-oil companies, and offered
feedback or recommendations to Singaporean
officials. “Such a ground-up approach is very
much welcomed by the government,” said Ang.

FEBRUARY 2015 FEATURE 30
Haze, however, is still a growing public health
concern for many countries, especially lower-in-
come ones. “We put a lot of legislation in place
to control point sources, and still, when you add
it up, ambient conditions don’t get better,” said
Jacqueline McGlade, Chief Scientist at the United
Nations Environment Programme. Other chal-
lenges, she told me, are linking air pollution data
with research on impacts and holding govern-
ments accountable for enforcing pollution laws.
More than ever, air pollution is a prominent tar-
get of policy reforms and public health interven-
tions. Many lower-income countries, grappling
with the environmental and health consequences
of their booming populations, are tightening air
pollution standards. International aid and devel-
opment agencies are also rolling out projects to
monitor or regulate particulate emissions.
In Southeast Asia, haze has recently resur-
faced on ASEAN’s political radar. In early July
2014, officials from Riau province announced
that they would conduct a large-scale “compli-
ance audit” of local officials and agroforestry
companies linked to peatlands. On 5 August,
Singapore’s parliament passed a law that al-
lows the government to fine both domestic
and international companies up to two million
Singapore dollars (US$1.5 million) for causing
or contributing to haze. And on 16 September,
Indonesia’s parliament finally ratified ASEAN’s
2002 trans-boundary haze agreement after 12
years of resistance.
Also that summer, a senior adviser to Joko
“Jokowi” Widodo, then Indonesia’s President-
Elect, said the new administration planned to re-
new the 2009 Indonesian law that banned peat
burning when it expires in 2015. Widodo himself
said he planned to streamline land governance
by creating a “one-map” forestry policy. “The
haze is caused both by the people and also the
companies,” he told the Straits Times, a Singa-
pore newspaper, in late August. “If we have good,
tough law enforcement, then it can be resolved.”
How significant are these developments?
In conversations with several haze-watching
analysts across Southeast Asia, I heard a wide
range of opinions. Some, like Helena Varkkey,
aren’t especially optimistic, mainly because In-
donesia and ASEAN have so far made so little
progress on the haze problem. Neither the Sin-
gaporean law nor the regional haze agreement,
they pointed out, would be enforceable in Indo-
nesian courts. And if climate change increases
the number of droughts and wildfires around the
world, as many scientists predict it will, the inci-
dence of peatland fires may also rise – and pose
additional enforcement challenges.
But others said it is positive that the Indone-
sian and Singaporean governments are at least
taking action – the sort that could breathe new
life into existing Indonesian laws designed to
tackle haze. The recent political activity gives
them hope that annual peat fires will not be-
come South-east Asia’s status quo for future
generations.
“Jokowi did say that he aims to take action
against the haze,” said Tan Yi Han, the haze
fighter. “That’s just words, but it’s better than
nothing.”
Adapted and reprinted with permission from Mosaic (http://mosaic-science.com/story/where-theres-smoke-Asia-air-pollution-haze).

FEBRUARY 2015 CALENDAR 31
F E B R U A R Y
14th World Congress on Public Health 11/2/2015 to 15/2/2015 Kolkata, India Phone: (91) 124 463 6713Email: [email protected] Website: www.14wcph.org
M A R C H
24th Conference of the Asian Pacific Association for the Study of the Liver (APASL)12/3/2015 to 15/3/2015Istanbul, TurkeyInfo: APASL SecretariatTel: (90) 312 440 50 11Fax: (90) 312 441 45 63Email: [email protected]: www.apasl2015.org
World Congress of Nephrology (WCN) 201513/3/2015 to 17/3/2015Cape Town, South AfricaInfo: International Society of NephrologyTel: (32) 2 808 71 81Fax: (32) 2 808 4454Email: [email protected]: www.wcn2015.org
64th Annual Scientific Session of the American College of Cardiology (ACC)14/3/2015 to 16/3/2015San Diego, California, USInfo: ACC Registration and Housing CenterTel: (1) 703 449 6418Email: [email protected]: http://accscientificsession.cardiosource.org/ACC.aspx
6th Association of Southeast Asian Pain Societies (ASEAPS) Congress15/3/2015 to 17/3/2015Manila, PhilippinesInfo: ASEAPS SecretariatTel: (65) 6292 0732Fax: (65) 6292 4721Email: [email protected] Website: www.aseaps2015.org
16th World Congress on Human Reproduction 18/3/2015 to 21/3/2015Berlin, GermanyInfo: Biomedical Technologies srlTel: (39) 070340293Fax: (39) 070307727Email: [email protected]: www.humanrep2015.com
4th Global Congress for Consensus in Pediatrics and Child Health (CIP)19/3/2015 to 22/3/2015Marrakech, MoroccoInfo: Paragon GroupTel: (41) 22 5330948Fax: (41) 22 5802953Email: [email protected]: http://2015.cipediatrics.org/marrakesh/
4th Global Congress for Consensus in Pediatrics and Child Health (CIP)19/3/2015 to 22/3/2015Budapest, HungaryInfo: CIP 2015 SecretariatTel: (41) 22 5330948Fax: (41) 22 5802953Email: [email protected]: http://2015.cipediatrics.org
9th World Congress on Controversies in Neurology (CONy)26/3/2015 to 28/3/2015Budapest, HungaryInfo: CONy SecretariatTel: (49) 15202950431Email: [email protected] Website: comtecmed.com/cony
World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (WCO-IOF)26/3/2015 to 29/3/2015Milan, ItalyInfo: Yolande Piette CommunicationTel: (32) 0 4 254 1225 Fax: (32) 0 4 254 1290 Email: [email protected]: www.wco-iof-esceo.or
U P C O M I N G
7th Asian Oncology Summit10/4/2015 to 12/4/2015Shanghai, ChinaInfo: Elsevier ConferencesEmail: [email protected]: http://asianoncologysummit.com
Royal College of Obstetricians & Gynaecologists (RCOG) World Congress12/4/2015 to 15/4/2015Brisbane, AustraliaInfo: RCOG World Congress 2015, Joint RCOG / RANZCOG Event OfficeTel: (61) 3 9645 6311Fax: (61) 3 9645 6322Email: [email protected]: www.rcog2015.com

FEBRUARY 2015 CALENDAR 32
30th International Conference of Alzheimer’s Disease International (ADI)15/4/2015 to 18/4/2015Perth, AustraliaInfo: ADITel: (44) 845 1800 169Fax: (44) 1730 715 291Email: [email protected]: www.alzint.org/2015
25th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID)25/4/2015 to 28/4/2015Copenhagen, DenmarkInfo: Kenes International – RegistrationTel: (41) 22 908 0488Fax: (41) 22 906 9140Email: [email protected] Website: www.eccmid.org
20th Asian Pacific Society of
Cardiology (APSC) Congress29/4/2015 to 2/5/2015Abu Dhabi, UAE Info: APSC 2015 Organizing CommitteeEmail: [email protected]: www.apsc2015.com
48th Annual Meeting of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN)6/5/2015 to 9/5/2015Amsterdam, NetherlandsInfo: ESPGHAN SecretariatTel: (44) 845 1800 360Email: [email protected]: www.espghan2015.org
21st World Congress on Controversies in Obstetrics, Gynaecology & Infertility (COGI)7/5/2015 to 10/5/2015Guilin, ChinaInfo: COGI SecretariatTel: (972) 73 706 695Fax: (972) 3 725 6266Email: [email protected]: www.congressmed.com/cogichina/index.php/en
From the research bench to your patient’s bedside – JPOG raises the quality of life of women and children in Asia. Pick up a copy today and start earning CME points.
For further details, visit www.jpog.com today.
JPOG is NOW CME-Accredited...
in Hong Kong, Indonesia, Malaysia and Singapore
For over 35 years, JPOG has been the only regional, peer-reviewed journal of paediatrics, obstetrics and
gynaecology in Asia. The bimonthly journal is proud to announce its CME-accreditation in the following Asian
countries: HONG KONG, INDONESIA, MALAYSIA and SINGAPORE.

20 • NEWS • SEPTEMBER 2014
RADHA CHITALE
A review of tree nut consump-tion showed that including about two servings of these
nutrient-rich foods in a person’s diet could decrease plasma glucose levels and fasting glucose.
While tree nuts such as al-
monds, walnuts, coconuts and pe-cans (though not peanuts, which are legumes) are frequently in-cluded in heart-healthy diets such as those from the Mediterranean region or Dietary Approaches to Stop Hypertension (DASH), data linking nut consumption to a lower incidence or risk of type 2 diabetes
is spotty. The review included 12 trials of
450 middle-aged adults with diabe-tes that included key glycemic end-points. [PLoS ONE 9(7):e103376. doi:10.1371/journal.pone.0103376]
Adults who consumed a me-dian 56 g/day of tree nuts showed a 0.07 percent decrease in HbA1c levels and 0.15 mmol/L lower fast-ing glucose, both of which were significant, according to a pooled analysis over a median 8 weeks.
Improvements were not as clear for other glycemic endpoints.
“Although significant advantag-es for fasting insulin and homeo-stasis model assessment of insulin resistance were not seen, the direc-tion of effect favored the tree nut intervention,” the researchers said.
Lead researcher Dr. John Siev-enpiper of the Clinical Nutrition and Risk Factor Modification Centre of St. Michael’s Hospital in Toronto, Canada, said that nuts probably tended to take the place of some carbohydrates in the diet, thereby lowering the dietary glycemic load.
The nuts’ micronutrient profile may also play a role in decreasing diabetes risk and improving gly-cemic control. Magnesium, found in high concentrations in many tree nuts, might be important for insulin-mediated glucose uptake or proper tyrosine-kinase activity in insulin receptors.
And while tree nuts may be low in sugar, they are high in fat, but it is monounsaturated fat, which in some studies have been shown to reduce HbA1c levels in higher quantities.
High quantities of tree nut con-sumption over time may also be important in diabetes control. Stud-ies shorter than 12 weeks were less likely to include patients who had lower HbA1c levels compared to those of 12 weeks or more. Stud-ies with a crossover design had a washout period of up to 8 weeks and demonstrated a corresponding smaller effect of tree nut consump-tion on blood sugar compared to trials with a parallel design.
Limits of the meta-analysis included whether the follow-up period in many of the trials was long enough to significantly affect glycemic control, as well as be-tween-study heterogeneity in out-come monitoring. Still, most of the data pointed towards including tree nuts in the diet for diabetes benefits.
Tree nuts help lower blood sugar in diabetics
Tree nuts appeared to take the place of carbohydrates in the diet and reduce dietary glycemic level.
“ The direction of
effect favored
the tree nut
intervention”
MT(SG)Sep14_FINAL.indd 20 8/29/14 10:44 AM
For A 5-minute UpdateGo to www.mims.asia/video
MIMS Video Series features interviews with leading experts
Find out what these experts have to say about how to improve patient care for osteoporosis and sarcopenia in Asia through awareness building and the use of new therapies
_seriesBrought to you by MIMS
SCAN TO WATCH VIDEO
Professor Peter Ebeling
Widespread vitamin D deficiency and low calcium levels in Asians
How low levels of awareness in the public and in healthcare professionals affect osteoporosis care in Asia
Benefits of fracture registries and fracture liaison registries (FLS) in Asia
Professor Serge Ferrari
Selective estrogen receptor modulators (SERMs), a new class of therapy for post-menopausal woman with osteoporosis
Dr Edith Lau
Treatment plans for post-menopausal women with osteoporosis
Professor Bess Dawson-Hughes
How aging contributes to sarcopenia and impaired muscle function in the elderly

FEBRUARY 2015 CONFERENCE COVERAGE 34
Early initiation of estrogen therapy may slow onset of Alzheimer’s in women
20th World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI), December 4-7, Paris, France
ELVIRA MANZANO
Levels of circulating sex steroid hormones
decline with normal aging, leaving the brain
unprotected against neurotoxic factors. This
makes hormone therapy early after menopause
a logical approach, says an expert.
“Estrogen deficiency, for example, contrib-
utes to Alzheimer’s disease,” said Professor An-
drea Riccardo Genazzani from the University of
Pisa, Pisa, Italy. “Early initiation [of estrogen] at
the time of menopausal transition may prevent
neurocognitive deterioration and activate sec-
ondary prevention and intervention to reduce
the risk of dementia.”
Many observational and preclinical studies
have shown that treatment with estrogens has
beneficial effects on the central nervous system
and cognitive function. Estrogen increased syn-
apse density and enhanced memory in young
animal models, but not in older ones. [Proc Natl Acad Sci 2001;98:8071-8076; J Neuroscience
2002;22:10985-10995]
“These findings suggest that aging substan-
tially modulates the mechanism of estrogen ac-
tion on the hippocampus and memory, and that
estrogen may be more effective in younger ani-
mals,” said Genazzani.
A meta-analysis of studies involving wom-
en with menopausal symptoms also found an
association between hormone therapy and
a decreased risk of dementia. [JAMA 2001;
285:1489-1499] Another study suggested
that post-menopausal estrogen replacement
therapy (ERT) reduced the risk of Alzheimer’s
disease among long-term users of ERT. [JAMA 2002;288:2123-2129]
However, the Women’s Health Initiative (WHI)
studies had contradictory findings – estrogen
therapy initiated alone, or in combination with
progestin, during the late menopausal stage in-
creased the risk of dementia or mild cognitive im-
pairment, regardless of the type of menopause
(natural or surgical). [JAMA 2003;289:2651-
2662; JAMA 2004;291:2947-2958]
“The difference with other studies is that
women in the WHI studies were generally older
[≥65 years] when treatment was started,” said
Genazzani. “This suggests a critical period for
ERT timing.”
“Alzheimer’s in women is a terrible disease
with no possibility of defense. Early, individual-
ized estrogen therapy regimens may be a good
choice for certain women, depending on their

FEBRUARY 2015 CONFERENCE COVERAGE 35
risk profile. We also have to maintain therapy
in younger women in the early postmenopausal
stage and in those who underwent bilateral oo-
phorectomy before the onset of natural meno-
pause to improve their mental well-being,”
Genazzani concluded.
Hormone therapy a viable option to prevent postmenopausal osteoporosisCHUAH SU PING
Hormone replacement therapy (HRT) can
help reduce the incidence of all osteoporo-
sis-related fractures, even in women not at high
risk of fracture, according to an expert.
“In their 2012 Hormone Therapy Position
Statement, the North American Menopause
Society (NAMS) noted that there is clinical evi-
dence that standard-dose hormone therapy
(HT) reduces postmenopausal osteoporotic
fractures, including hip, spine and all non-spine
fractures, even in women without osteoporosis,”
said Professor Robert D. Langer, Associate Dean
for Clinical and Translational Research and Pro-
fessor of Medicine at the University of Nevada
School of Medicine in Reno, Nevada, US.
“Low doses, according to the NAMS, are ef-
fective in maintaining or improving bone mineral
density,” added Langer. He noted that when al-
ternate osteoporosis therapies are not appropri-
ate or cause adverse effects, the extended use
of HT is an option for women at high risk of os-
teoporotic fracture. [Menopause 2012;19:257-
271] This stand is echoed by the International
Menopause Society’s (IMS) recommendations
on menopausal HT, which noted that HT “can
be considered as one of the first-line therapies
for the prevention and treatment of osteoporo-
sis-related fractures.” [Climacteric 2013;16:316-
337]
“While there is still a lack of evidence that
HT stops working with long-term use, the avail-
able evidence indicate that the benefits of HT
on bone mass and fracture reduction dissipate
quickly upon discontinuation of treatment,” said
Langer. To illustrate this, Langer described a
study of 80,955 postmenopausal women us-
ing HT who were followed up from July 2002
to December 2008. After 6.5 years of follow-up,
age- and race-adjusted Cox proportional hazard
models showed that women who discontinued
HT were at 55 percent greater risk of hip frac-
ture compared with those who continued using
HT (HR, 1.55 95% CI, 1.36-1.77). “Hip fracture
risk increased as early as 2 years after cessa-
tion of HT, and this risk incrementally increased
with longer duration of cessation.” [Menopause

FEBRUARY 2015 CONFERENCE COVERAGE 36
2011;18:1172-1177]
Langer noted that at present, while no HT
product is approved for the treatment of os-
teoporosis, many systemic HT products have
government approval for the prevention of post-
menopausal osteoporosis. The IMS however
cautioned in their 2011 Position Statement that
the initiation of HRT for the sole purpose of the
prevention of fractures after the age of 60 years
is not recommended, and should take into ac-
count the possible long-term effects of the spe-
cific dose and method of administration of HRT,
compared with other proven non-hormonal ther-
apies. [Climacteric 2011;14:302-320]
In his conclusion, Langer noted that the updat-
ed 2013 IMS recommendations for menopausal
HT state that it is an effective treatment for the
prevention of fracture in at-risk women before age
60 years or within 10 years after menopause. [Cli-macteric 2013;16:316-337]
Researchers search for ways to preserve fertility during chemotherapyRADHA CHITALE
Chemotherapy can damage ovarian func-
tion enough to significantly reduce fertil-
ity, but pre-treatment with certain drugs may be
able to prevent this, researchers said.
“It would be very good to block the toxic-
ity of chemotherapy or radiotherapy but there
is no drug for this,” said presenter Dr. Philippe
Bouchard, of the Hospital Saint Antoine at Uni-
versite Paris in France.
In addition to follicular damage, ovarian dam-
age can deprive women of estrogen, which is
associated with osteoporosis and neurocogni-
tive impairment and Bouchard noted it should
be preserved, along with ovarian function.
Current methods to preserve fertility include
oocyte and embryo cryopreservation. However,
these are expensive procedures that can delay
cancer therapy and they do not preserve estro-
gen function.
Some fetoprotective agents that shield ovar-
ian function from the effects of chemotherapy or
radiotherapy have shown promising results in
mouse models, Bouchard said.
The chemotherapy adjuvant bortezomib, for
example, has proven an effective shield against
doxorubicin, an anthracycline that is used in
about half of patients treated for cancer, includ-
ing those that are at high risk for reduced fertility
such as breast, bladder and thyroid cancer, as
well as many pediatric cancers such as leuke-
mia and neuroblastoma.
However, doxorubicin can cause follicular
apoptosis in mouse ovaries within 12 hours of
drug administration. Treated mice only recover
about 50 percent of their pre-treatment ovulation

FEBRUARY 2015 CONFERENCE COVERAGE 37
rate and have long-term follicle depletion.
Bortezomib competes with doxorubicin bind-
ing sites in key areas to prevent doxorubicin ac-
cumulation in the follicles. Female mice treated
with bortezomin 1 hour prior to treatment with
DXR reduced DNA damage in ovarian cells and
follicular apoptosis. [PLoS One 2014;9:e108174]
“Bortezomib pre-treatment extended the
number of litters per mouse, improved litter size
and increased pup weight following doxorubi-
cin treatment, thus increasing the duration of
post-chemotherapy fertility and improving pup
health,” the study authors said.
In addition, bortezomib did not interfere with
doxorubicin efficacy as a chemotherapy.
Stem cells use is also on the rise among re-
searchers seeking ways to restore ovarian func-
tion and female fertility following chemotherapy
or radiotherapy, Bouchard said, primarily by acti-
vating dormant ovarian follicles. However, further
translational and clinical research is needed in
this area.

FEBRUARY 2015 HUMOR 38
“I think it’s your heart, but on the other hand it could be your
kidneys, or your liver, how about your lungs, do you think it’s your lungs? In any case you’re entitled
to a second opinion!”
“I can understand a moose’s head, even a fish, but your appendix?”
“I won’t be able to get home in time for supper dear.
I’m having a kidney transplant!”
“It’s a boy. We thought you would never show up!”
“The guy who painted that was probably a medical cartoonist!”
“Does doctor Granfleet know what this is in reference to?”

Essential Clinical Practice Tool On-The-Go
The FREE MIMS app delivers critical prescribing information, medical news and CME articles as well as clinical calculators essential to physicians’ daily practice needs.
With MIMS available across multiple platforms and devices, you can now easily and conveniently � nd the most up-to-date and relevant drug information you need anytime, anywhere.
MIMS mobile/tablet app facebook.com/mimscomwww.mims.com
Join over a million MIMS members who have incorporated MIMS into their daily workfl ow. Connect with MIMS today.
www.mims.com

P U B L I S H E R
Ben Yeo
M A N A G I N G E D I T O R
Greg Town
C O N T R I B U T I N G E D I T O R S
Christina Lau, Jackey Suen, Jenny Ng (Hong Kong), Saras Ramiya, Pank Jit Sin, Joslyn Ngu Kathlin Ambrose (Malaysia), Dr Mel Beluan (Philippines), Radha Chitale, Elvira Manzano, Chuah Su Ping (Singapore)
P U B L I C A T I O N M A N A G E R
Marisa Lam
D E S I G N E R S
Razli Rahman, Anson Suen, Joseph Nacpil, Agnes Chieng, Ryan R.A. Baranda, Sam Shum
P R O D U C T I O N
Edwin Yu, Ho Wai Hung, Jasmine Chay
C I R C U L A T I O N E X E C U T I V E
Christine Chok
A C C O U N T I N G M A N A G E R
Minty Kwan
A D V E R T I S I N G C O - O R D I N A T O R
Jasmine Chay
P U B L I S H E D B Y
MIMS (Hong Kong) Limited 27th Floor, OTB Building, 160 Gloucester Road, Wanchai, Hong Kong Tel: (852) 2559 5888 Fax: (852) 2559 6910 Email: [email protected]
A D V E R T I S I N G E N Q U I R I E S :
C H I N A
Yang Xuan Tel: (8621) 6157 3888 Email: [email protected]
H O N G K O N G
Kristina Lo-Kurtz, Miranda Wong, Marisa Lam, Jacqueline Cheung Tel: (852) 2559 5888 Email: [email protected]
I N D I A
Monica Bhatia Tel: (9180) 2349 4644 Email: [email protected]
K O R E A
Choe Eun Young Tel: (822) 3019 9350 Email: [email protected]
M A L A Y S I A
Sumitra Pakry, Grace Yeoh, Tiffany Collar Tel: (603) 7954 2910 Email: [email protected]
P H I L I P P I N E S
Kims Pagsuyuin, Rowena Belgica, Cor-Marie Bacdayan, Cliford Patrick Tel: (632) 886 0333 Email: [email protected]
S I N G A P O R E
Jason Bernstein, Carrie Ong, Josephine Cheong, Melanie Nyam Tel: (65) 6290 7400 Email: [email protected]
T H A I L A N D
Wipa Sriwijitchok Tel: (662) 741 5354 Email: [email protected]
V I E T N A M
Nguyen Thi Lan Huong, Nguyen Thi My Dung Tel: (848) 3829 7923 Email: [email protected]
E U R O P E / U S A
Kristina Lo-Kurtz Tel: (852) 2116 4352 Email: [email protected]
Medical Tribune is published 12 times a year (23 times in Malaysia) by MIMS Pte Ltd. Medical Tribune is on controlled circulation publication to medical practitioners in Asia. It is also available on subscription to members of allied professions. The price per annum is US$48 (surface mail) and US$60 (overseas airmail); back issues at US$5 per copy. Editorial matter published herein has been prepared by professional editorial staff. Views expressed are not necessarily those of MIMS Pte Ltd. Although great effort has been made in compiling and checking the information given in this publication to ensure that it is accurate, the authors, the publisher and their servants or agents shall not be responsible or in any way liable for the continued currency of the information or for any errors, omissions or inaccuracies in this publication whether arising from negligence or otherwise howsoever, or for any consequences arising therefrom. The inclusion or exclusion of any product does not mean that the publisher advocates or rejects its use either generally or in any particular field or fields. The information contained within should not be relied upon solely for final treatment decisions.
© 2015 MIMS Pte Ltd. All rights reserved. No part of this publication may be reproduced in any language, stored in or introduced into a retrieval system, or transmitted, in any form or by any means (electronic, mechanical, photocopying, recording or otherwise), without the written consent of the copyright owner. Permission to reprint must be obtained from the publisher. Advertisements are subject to editorial acceptance and have no influence on editorial content or presentation. MIMS Pte Ltd does not guarantee, directly or indirectly, the quality or efficacy of any product or service described in the advertisements or other material which is commercial in nature.
Philippine edition: Entered as second-class mail at the Makati Central Post Office under Permit No. PS-326-01 NCR, dated 9 Feb 2001. Printed by KHL Printing Co Pte Ltd, 57 Loyang Drive, Singapore 508968.
ISSN 1608-5086




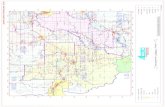


![Home [] · RG 1116/2016 12 RG 2284 /2018' 13 RG 2803/2018 14 RG 359/2019 15 RG 569/2019 16 RG 709/2019 17 RG 2709/2019 18 RG 114/2020 19 RG 120/2020 20 RG 143/2020 21 RG 150/2020](https://static.fdocuments.us/doc/165x107/602fb412feaa17578405f503/home-rg-11162016-12-rg-2284-2018-13-rg-28032018-14-rg-3592019-15-rg-5692019.jpg)











