Medical Billing and CodingMedical Billing and Coding Program … · 2019-10-30 · Computers in...
Transcript of Medical Billing and CodingMedical Billing and Coding Program … · 2019-10-30 · Computers in...
Spring 2020
Three Rivers Community College Workforce & Community Education Phone: 860-215-9028 ≈ Fax: 860-215-9902
Email: [email protected] Website: www.threerivers.edu
SNAP E&T and WIOA eligible
SNAP E&T is a voluntary work program.
Participants must be able to work upon
completion of the program
Contact Us Workforce & Community Education 574 New London Turnpike Norwich, CT 06360 (860) 215-9028 Phone (860) 215-9902 Fax email: [email protected] Visit us on the web: www.threerivers.edu
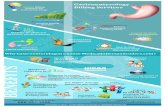
Medical Billing and Coding Program
Current Procedural Terminology (CPT) and
Healthcare Common Procedure Coding System
(HCPCS 11)
Computers in the Medical Office
Refund policy: Withdrawal from any non-credit class must be
submitted in writing to the Workforce & Community Education
office up to one business day prior to the first class. Absolutely
no refunds will be issued after the first class has begun. The
college reserves the right to cancel any course for which there is
insufficient enrollment. In that event, a full refund will be issued.
Please note: Completion of any program does not guarantee
employment.
Medical Billing and Coding Program (Year-Long Program)
Medical Terminology and Anatomy for Coders – $900
Understanding Health Insurance – $450
Computers in Medical Office - $450
ICD-10-CM - $475
Current Procedural Terminology and Healthcare Common
Procedure Coding System (HCPCS 11) – $575
Medical Coding Exam Preparation (AAPC) – $475
Total Tuition: $3,325.00 + Books
Prerequisites: The Medical Billing and Coding course is a non-credit program.
The length of the program is about a year. You must take all required courses to receive a certificate.
You must have a high school diploma or GED to register for
this course.
Students should be familiar with personal computers, file man-
agement, the use of a keyboard, mouse and Windows 8.1 or higher.
Students will be required to purchase required textbooks and
supplies.
You also must be at least 18 years of age Must also success-
fully complete our in-house English and mathematics exam or provide proof of prior college-level English and math. See below.
Entrance Exam Directions: To make an appointment for an entrance exam please sign up as follows: 1. Log onto www.timecenter.com/trcc 2. Click on Make-up, Special Accommodation, & Workforce
Test 3. Click on date and time of your choosing 4. Complete the requested information. When asked for a
Student ID number, please notate “non-credit” and the type of test you are taking (for example, Medical Billing and Coding). You will receive a confirmation text or email of this scheduled appointment.
Note: Please arrive on time for your scheduled appointment (Room A117). There is no food or drink allowed in the Testing Center. There is no use of cell phones, headphones, notes, etc., during testing. Students must present a picture ID in order to enter the Testing Center for their appointment.
Computers in the Med Office-CRN #14233
ICD-10-CM Course-CRN #14234
Legal Name
Former Name (s) - if applicable
Street Address
City State Zip Code
_________-_________-__________ ______/______/________
Telephone Date of Birth
E-mail Address
________/________/___________________
Social Security Number (Required by College)
U.S. Citizen Yes No Gender: Male Female
Race: White Black, non-Hispanic Asian
American Indian Hispanic Decline to State
Ethnicity: Hispanic/Latino Non-Hispanic/Non-Latino
Decline to State (None)
Check (payable to TRCC) Visa MC Discover Amex
____________________________/_____/___________________________
Credit Card # Exp. date $ Amount $
____________________________ Zip Code of Credit Card holder 3 Digit Security Code (required by credit card company)
Acknowledgement Statement:
I certify that the information provided above is, to the best of my knowledge, true and correct, and I consent to the disclosure of this and program participation information between, Three Rivers Community College, Connecticut State Colleges and Universities and state and federal Departments of Labor for the purposes of maintaining accurate student records and to monitor grant performance.
Signature Date
Allied Health Booklet given to student
For office use ONLY:
Student ID @
Entered By Date _____/_____/_____
Medical Billing and Coding Program
Medical coders may read a patient’s medical chart looking at the patient's diagnoses and any procedures performed and then catego-rize those diagnoses and procedures according to a national classifi-cation system, assigning a specific numeric or alphanumeric code to each diagnosis or procedure. A medical coder translates the docu-ments in a patient's chart into codes. Most coders will spend a ma-jority of their time using their computer to enter data into a billing systems or looking for information to clarify notes in the patient’s chart.
This year long non-credit training program will prepare students to sit for the national certification, CPC-A (Certified Professional Coder Apprentice), by the American Academy of Professional Coders (AAPC). Students can earn this credential (CPC-A) after successful-ly passing the national certification examination. This certification is sponsored by the AAPC, a nationally recognized organization offer-ing professional accreditation, education, recognition, and network-ing opportunities to medical coders. The exam fee is not included. Visit them at www.aapc.com or call 800-626-2633 to obtain an appli-cation packet or information. According to the U.S. Bureau of Labor Statistics, jobs for medical records and health information technicians will increase 22% through the year 2020.
Computers in the Medical Office
Prerequisite: Basic computer skills
Students will learn how to use the full-featured and current SimChart for the Medical Office. This course offers medical office training using current, realistic medical office cases while building transfera-ble computerized medical billing and scheduling skills. Students who complete this course will learn the appropriate terminology and skills to use any patient billing software program with minimal additional training. As students’ progress through SimChart they learn to gath-er patient information, schedule appointments and enter transac-tions. The practical, systematic approach is based on real-world
medical office activities. This class meets for 45 hours.
Instructor: Leslie Schwanfelder
Days/Dates: Wednesdays 2/5/20-5/20/20 No Class 2/26/20 Registration deadline 1/29/20 Time: 5:30-8:30pm Room: E119 Tuition: $450.00-books at an additional cost CRN: 14233 CEU’s: 4.5 This course will be utilizing Blackboard Learn. Please make sure that you are able to log into the computers on campus with your banner id and password. Please contact the IT Department at (860) 215-9049 to arrange to activate your account or if you have
difficulties logging on prior to your first class.
ICD-10-CM
Prerequisite: Medical Terminology & Anatomy for Coders
The United States Government recognizes the International Classifica-tion of Diseases,10th Revision, Clinical Modification (ICD-10-CM) for morbidity reporting in the United States. The code set is used to report diagnoses and other reasons for healthcare encounters for billing in inpatient and outpatient settings. In this course, students will study the Official ICD-10-CM Conventions and Guidelines. Students will learn the steps for correct coding and understand the role of the ICD-10-CM in healthcare reimbursement.
Instructor: Leslie Schwanfelder
Days/Dates: Thursdays 2/6/20 –5/21/20 Registration deadline 1/30/20 No class on 2/27 Time: 2/6 - 3/12 5:30 - 8:30pm 3/19 - 5/21 5:30-9:00pm Room: B127 Tuition: $475.00-books at an additional cost CRN: 14234 CEU’s: 5 This course will be utilizing Blackboard Learn. Please make sure that you are able to log into the computers on campus with your banner id and password. Please contact the IT Department at (860) 215-9049 to arrange to activate your account or if you have difficulties logging on
prior to your first class.