Med Chronic microsporidian infectionofthenasal mucosae, … · isms measured approximately 1 pim in...
Transcript of Med Chronic microsporidian infectionofthenasal mucosae, … · isms measured approximately 1 pim in...
-
Genitourin Med 1992;68:179-181
Chronic microsporidian infection of the nasalmucosae, sinuses and conjunctivae in HIV disease
C J N Lacey, A M T Clarke, P Fraser, T Metcalfe, G Bonsor, A Curry
AbstractA case of chronic infection of the nasalmucosae, sinuses and conjunctivae witha microsporidian parasite in associationwith HIV infection and immunedeficiency is reported. This micro-sporidian resembles both Ence-phalitozoon cuniculi and the newly de-scribed Encephalitozoon hellem by elec-tron microscopy. This occurred in anadult male resident in the UK with nohistory of foreign travel. Although thereare previous descriptions of conjunctivalinfections from the USA, this is the firstdescription of infection of the nasalepithelium. Further studies are under-way to classify this protozoan.
Department ofGenitourinaryMedicineC J N LaceyP FraserDepartment ofPathologyAM T ClarkeDepartment ofOphthalmologyT MetcalfeDepartment ofRadiologyG BonsorGeneral Infirmary,Great George St,Leeds LSl 9N2, UKDepartment ofPathology, WithingtonHospital, ManchesterA CurryAddress correspondence to:Dr C LaceyAccepted for publication13 February 1992
IntroductionMicrosporidia are obligate, intacellular,spore-forming protozoal parasites. They arewidespread in the natural world and have longbeen recognised as a cause of disease in non-human hosts. However, only six micro-sporidial infections in patients without HIVinfection have been documented.' Reports ofmicrosporidial infection in patients withAIDS first appeared in 1985,23 describing anew genus and species Enterocytozoon bienusi,predominantly infecting the small intestineand usually presenting with chronic diarrhoeaand weight loss. Studies have suggested that30% of patients with HIV disease and patho-gen negative chronic diarrhoea haveEnterocytozoon bienusi infection.45 Recentwork utilising duodenal biopsy specimensfrom HIV infected individuals with and with-out diarrhoea, and presumptively HIVnegative individuals has provided evidence ofthe pathogenicity of Enterocytozoon bienusi,without evidence of a state of commensal
6
carriage.Encephalitozoon cuniculi usually infects
non-human mammals. Infection usuallybegins in intestinal epithelial cells, and inanimals first liver and then other extra-intes-tinal sites are infected, presumably via blood,lymph, or infected macrophages.7 In lateinfection central nervous system vasculitis andinterstitial nephritis predominate. Two non-HIV infected children with encephalitozooninfection and CNS involvement have beendescribed.' Infection with protozoa mor-phologically identical to Encephalitozooncuniculi was first described in HIV infection inassociation with a hepatic lesion,8 and then ina case of peritonitis.9
Reports of microsporidian ocular infectionin patients with AIDS first appeared early in1990.101 Ocular infection presents with symp-toms of foreign-body sensation, blurred visionor photophobia. Ophthalmological examina-tion discloses conjunctivitis, decreased visualacuity, and a diffuse punctate keratopathy.Corneal or conjunctival scrapings or biopsiesstained with Giemsa reveal oval dark-stainingspores. Confirmation of the identity of theinfecting microsporidia in these cases ofhepatitis, peritonitis, and kerato-conjunc-tivitis has been by demonstrating theirmorphological similarity to Encephalitozooncuniculi by electron microscopy. However,Didier et al recently isolated such micro-sporidia in cell culture from AIDS patientswith kerato-conjunctivitis. Three such isolateswere shown to be a new species, Ence-phalitozoon hellem, morphologically similar toEncephalitozoon cuniculi by electron micro-scopy, but distinct by SDS-PAGE analysis.'2
Case reportA 26 year old married bisexual man was firstshown to be HIV antibody positive at routinescreening in 1986. In January 1988 heremained well with CD4 0.40 x 109/1, HIVp24 Ag + ve, /2-microglobulin 41 mg/l. Hefirst developed bilateral conjunctivitis inOctober 1988. Nasal obstruction and dischargebecame prominent in February 1989. By thisstage he was unwell with weight loss andrelapsing fevers and investigations showedCD4 0-19 x 109/1, HIV p24 Ag < 100> 500 i/ml, f2-microglobuJin 4.6 mg/l.Zidovudine was commenced at 1 g/day with agood initial response. However, he continuedto have episodic conjunctivitis, chronic nasalobstruction and discharge, as well as clinicaland radiological evidence of sinusitis. Thiscondition failed to respond to multiple coursesof antibiotics and nasal decongestants. In June1990 a diffuse punctate keratopathy was notedin both eyes, ENT examination showed mul-tiple nasal polyps, and CT showed extensiveopacities in the maxillary antra, and ethmoidand sphenoid sinuses, as well as minor cerebralatrophy. A full description of the ophthalmo-logical findings and subsequent ocular responseto treatment is being published elsewhere.'3 Hewas admitted to hospital in October 1990 withPneumocystis carinii pneumonia and treatedwith intravenous pentamidine. Followingrecovery a formal nasal polypectomy was per-formed under general anaesthesia. After for-malin fixation nasal polypectomy specimens
179
on June 17, 2021 by guest. Protected by copyright.
http://sti.bmj.com
/G
enitourin Med: first published as 10.1136/sti.68.3.179 on 1 June 1992. D
ownloaded from
http://sti.bmj.com/
-
Lacey, Clarke, Fraser, Metcalfe, Bonsor, Curry
t .. ;i 1'.-1~%%
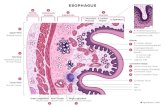
Figure 1 Nasal epithelium showing surface epithelial cells with cytoplasmic vacuolescontaining multiple spores (arrowed). Scale bar represents 10 pm.
were embedded in paraffin wax (Ralwax 1,BDH) and 4,m sections were stained withhaematoxylin and eosin, PAS and Grocottstains. A specimen was also embedded inmethacrylate derived plastic (Immunobed,Park Scientific Ltd, Northampton) and 2 pmsections were stained by a two-stage May-Grunwald-Giemsa method. These prepara-tions were examined by light microscopy. Theyrevealed a polypoid nasal mucosa with aneutrophil infiltrate within the epithelium and aneutrophil, lymphocyte and plasma cell infil-trate in the adjacent submucosa. Many super-ficial epithelial cells contained numerous round
Figure 2 Sagittal magnetic resonance image showing inflammatory massfilling the nasalairway (arrowed) and sphenoid sinus.
to oval organisms within the cytoplasm demon-strated by Giemsa staining (fig 1). These organ-isms measured approximately 1 pim indiameter, were gram positive and did not stainwith either PAS or Grocott stains. These lightmicroscopic appearances were those of aprotozoan infection of the nasal mucosa.Comeal and nasal specimens were also
examined by electron microscopy. Thisshowed a species of encephalitozoon infectingboth epithelia. A full description of the ultra-structure is being published separately.'4
In January 1991 the patient developed AIDSdementia complex with spastic paraparesis ofthe legs and memory loss. Repeat CT and MRIshowed dilatation of third and lateral ven-tricles, generalised involutional change andhigh signal material filling the nasal airway (fig2).By May 1991 nasal obstruction and dis-
charge were again problematic with multiplenasal polyps present on examination. Furtherpolypectomy was therefore performed. In viewof the observation ofsome degree ofresponse ofintestinal microsporidiosis to oral albendazole(Blanshard C, personal communication)therapy with this agent was instituted. Alben-dazole 400 mg bd was given for one month andobliquely oriented coronal CT was performedto demonstrate the nasal airway and sinusespre- (fig 3) and post- (fig 4) medical therapy.Both scans revealed erosion of the medial wallsof the maxillary antra. During the course oftreatment the patient's nasal symptomsimproved, and there was significant regressionof sinus opacification. The patient remainedfree of nasal symptoms until his death inOctober 1991 from AIDS dementia complex.
DiscussionThe recent .demonstration that three micro-sporidial isolates from cases of kerato-conjunc-tivitis similar to our patient are distinct from,but closely related to Encephalitozoon cuniculi,underlies our limited knowledge concerningthe epidemiology of microsporidiosis inhumans. Bergquist and colleagues, forexample, investigated 30 Swedish homosexualmen at risk of AIDS in 1984 using a serologicassay for antibodies to Encephalitozoon cuniculiand found a 33% antibody prevalence.'5 Didiershowed that antibodies against E hellem cancross react with E cuniculi 'while any antibodyresponse against Enterocytozoon bienusi has notbeen defined.We have therefore described a man with
HIV infection and immune deficiency who hasan opportunistic infection of the cornea, con-junctiva and nasal mucosae with a micro-sporidian parasite similar to Encephalitozooncuniculi and Encephalitozoon hellem. He has alsoradiological, computed tomographic andmagnetic resonance imaging evidence ofopacification of the maxillary antra, ethmoidand sphenoid sinuses unresponsive to conven-tional antibacterial therapy or nasal polypec-tomy, presumably caused by infection with thesame organism. Late in the course of hismicrosporidian infection there was clear com-
180 on June 17, 2021 by guest. P
rotected by copyright.http://sti.bm
j.com/
Genitourin M
ed: first published as 10.1136/sti.68.3.179 on 1 June 1992. Dow
nloaded from
http://sti.bmj.com/
-
Chronic microsporidian infection of the nasal mucosae, sinuses and conjunctivae in HIV disease
Figure 3 Oblique coronal CT post-second polypectomy pre-albendazole showingopacification of the maxillary antra and ethmoid sinuses.
puted tomographic evidence of bony destruc-tion of the maxillary antra. Administration ofalbendazole produced symptomaticimprovement and radiological regression ofsinus infection. The manifestations of hisocular pathology are typical of previously de-scribed cases but this is the first case in an HIVinfected subject described outside the USA.This subject has frequent contact with cats anddogs in his home environment and has never
Figure 4 Oblique coronal CT post albendazole showing regression of opacification anddeficiency of the medial wall of the left maxillary antrum (arrowed).
travelled outside the UK. We know that Ence-phalitozoon cuniculi can spread horizontallyamong mammals via contaminated excretal6and one could postulate domestic animals as asource of this patient's infection.This subject's symptoms of ocular and nasal
infection were first noted up to 2 years prior todemonstration of his microsporidial infection.This symptom complex developed relativelyearly in the course of his immune deficiency, inparallel with symptoms of systemic HIV dis-ease at a time when his CD4 count was of theorder of 0-200 x 1O9/1. We found ence-phalitozoon easy to demonstrate by Giemsastains or electron microscopy once suitabletissue specimens were obtained.This case report extends the known tissue
tropism of these organisms. This case appearsto be a rarity, but precise definition of thefrequency of microsporidial upper respiratorytract infection may depend on the developmentof serological assays. This in turn may dependupon propagation of such organisms andcurrently protozoa derived from the patient'spolypectomy specimens are growing in tissueculture (Canning E U, personal communi-cation). This man's infection appeared to re-spond well to albendazole. Encephalitozoonmay be overlooked using light microscopy withcertain stains and electron microscopy is atpresent vital in identification.
The authors thank Dr J T Lamb and Mr J DFenwick for advice and assistance, ClareMidgley for secretarial services, and StephenToms for help with the illustrations.
1 Bryan RT. Microsporidia. In: Mandell GL, Douglas RG,Bennett, JE eds. Principles and Practice of InfectiousDiseases. 3rd ed. New York: Churchill Livingstone,1990:2130-4.
2 Modigliani R, Bories C, Le Carpentier Y, et al. Diarrhoeaand malabsorption in acquired immune deficiency syn-drome: A study of four cases with special emphasis onopportunistic protozoan infestations. Gut 1985;26:179-87.
3 Dobbins WO III, Weinstein WM. Electron microscopy ofthe intestine and rectum in acquired immunodeficiencysyndrome. Gastroenterology 1985;88:738-59.
4 Orenstein JM, Chiang J, Steinberg W, Smith PD, Rotter-dam H, Kotler DP. Intestinal microsporidiosis as a causeof diarrhoea in Human Immunodeficiency Virus-infec-ted patients: a report of 20 cases. Hum Pathol 1990;21:475-81.
5 Van Gool T, Hollister WS, Schattenkerk JE, et al. Diagnosisof Enterocytozoon bienusi microsporidiosis in AIDSpatients by recovery of spores from faeces. Lancet1990;336:697-8.
6 Schattenkerk JKME, Van Gool T, Van Ketel RJ, et al.Clinical significance of small-intestinal microsporidosis inHIV-1 infected individuals. Lancet 1991;337:895-8.
7 Canning EU, Lom J. The Microsporidia of Vertebrates.London: Academic Press; 1986:208.
8 Terada S, Reddy R, Jeffers LJ, et al. Microsporidian hepatitisin the acquired immunodeficiency syndrome. Ann InternMed 1987;107:61-2.
9 Zender HO, Arrigoni E, Eckert J, Kapanci Y. A case ofEncephalitozoon cuniculi peritonitis in a patient withAIDS. Am J Clin Pathol 1989;92:3526.
10 Lowder CY, Meisler DM, McMahon JT, Longworth DL,Rutherford I. Microsporidia infection of the cornea in anHIV-positive man. Am J Ophthalmol 1990;109:242-4.
11 Anon. Microsporidian kerato-conjunctivitis in patients withAIDS. MMWR 1990;39(11):188-9.
12 Didier ES, Didier PJ, Friedberg DN, et al. Isolation &characterization of a new human microsporidian, Ence-phalitozoon hellem (n.sp) from three AIDS patients withkerato-conjunctivitis. J Infect Dis 1991;163:617-21.
13 Metcalfe T, Doran R, Rowland P, Curry A, Lacey CJN.Microsporidial kerato-conjunctivitis in a British patientwith AIDS. Br J Ophthalmol 1992 (in press).
14 Canning EU, Curry A, Lacey CJN, Fenwick JD. Ultrastruc-ture of encephalitozoon sp. infecting the conjunctival,corneal and nasal epithelia of a patient with AIDS. Eur JProtistology 1992 (in press).
15 Bergquist R, Morfeldt-Mansson L, Pehrson PO, et al.Antibody against Encephalitozoon cuniculi in Swedishhomosexual men. Scand J Infect Dis 1984;16:389-91.
16 Cox JC, Gallichio HA, Walden HB. Application ofimmuno-fluorescence to the establishment of an Encephalitozooncuniculi-free rabbit colony. Lab Anim Sci 1977;27:204-9.
181 on June 17, 2021 by guest. P
rotected by copyright.http://sti.bm
j.com/
Genitourin M
ed: first published as 10.1136/sti.68.3.179 on 1 June 1992. Dow
nloaded from
http://sti.bmj.com/