Malaria Indicator Survey 2016 - WHO · The 2016 Sierra Leone Malaria Indicator Survey (2016 SLMIS)...
Transcript of Malaria Indicator Survey 2016 - WHO · The 2016 Sierra Leone Malaria Indicator Survey (2016 SLMIS)...

SIERRA LEONE
Malaria Indicator Survey
2016
Final Report
National Malaria Control Programme
Statistics Sierra Leone
College of Medicine and Allied Health Services University of Sierra Leone
Catholic Relief Services
Freetown, Sierra Leone
ICF Rockville, Maryland
United States
December 2016

The 2016 Sierra Leone Malaria Indicator Survey (2016 SLMIS) was implemented by the National Malaria Control Programme (NMCP), Statistics Sierra Leone (SSL), the College of Medicine and Allied Health Services (COMAHS) of the University of Sierra Leone (USL), and Catholic Relief Services (CRS) from June-August 2016. ICF provided technical assistance. Funding for the 2016 SLMIS was provided through CRS with funds from the Global Fund (GF). Additional information about the 2016 SLMIS may be obtained from the headquarters of the Ministry of Health and Sanitation, Youyi Building, Brookfields, Freetown, Sierra Leone. Information about the survey may also be obtained from ICF, 530 Gaither Road, Rockville, MD 20850, United States; Telephone: +1-301-407-6500; Fax: +1-301-407-6501; E-mail: [email protected]; Internet: www.DHSprogram.com. Recommended citation: National Malaria Control Programme (NMCP) [Sierra Leone], Statistics Sierra Leone, University of Sierra Leone, Catholic Relief Services, and ICF. 2016. Sierra Leone Malaria Indicator Survey. Freetown, Sierra Leone: NMCP, SSL, CRS, and ICF.

Contents • iii
CONTENTS
TABLES AND FIGURES ............................................................................................................................ v PREFACE .................................................................................................................................................... ix ACRONYMS AND ABBREVIATIONS .................................................................................................... xi HOW TO READ AND UNDERSTAND THE 2016 SLMIS TABLES ................................................ xiii MAP OF SIERRA LEONE ........................................................................................................................ xx
1 INTRODUCTION AND SURVEY METHODOLOGY .............................................................. 1 1.1 Survey Objectives ................................................................................................................ 1 1.2 Sample Design ..................................................................................................................... 1 1.3 Questionnaires ..................................................................................................................... 2 1.4 Anaemia and Malaria Testing .............................................................................................. 2 1.5 Pretest .................................................................................................................................. 3 1.6 Training of Field Staff ......................................................................................................... 4 1.7 Fieldwork ............................................................................................................................. 4 1.8 Laboratory Testing .............................................................................................................. 5 1.9 Data Processing ................................................................................................................... 5 1.10 Response Rates .................................................................................................................... 5 1.11 Malaria Control in the Context of the Ebola Epidemic ....................................................... 6
2 CHARACTERISTICS OF HOUSEHOLDS AND WOMEN ...................................................... 9 2.1 Drinking Water Sources and Treatment .............................................................................. 9 2.2 Sanitation ........................................................................................................................... 10 2.3 Housing Characteristics ..................................................................................................... 11 2.4 Household Wealth ............................................................................................................. 11 2.5 Household Population and Composition ........................................................................... 12 2.6 Educational Attainment of Women ................................................................................... 13 2.7 Literacy of Women ............................................................................................................ 14
3 MALARIA PREVENTION .......................................................................................................... 27 3.1 Ownership of Insecticide-Treated Nets ............................................................................. 28
3.1.1 Sources of ITNs ................................................................................................... 30 3.1.2 Mosquito net preferences ..................................................................................... 30
3.2 Household Access and Use of ITNs .................................................................................. 30 3.3 Use of ITNs by Children and Pregnant Women ................................................................ 33 3.4 Malaria in Pregnancy ......................................................................................................... 34
4 MALARIA IN CHILDREN ......................................................................................................... 45 4.1 Care Seeking for Fever in Children ................................................................................... 45 4.2 Diagnostic Testing of Children with Fever ....................................................................... 46 4.3 Use of Recommended Antimalarials ................................................................................. 47 4.4 Prevalence of Low Haemoglobin in Children ................................................................... 48 4.5 Prevalence of Malaria in Children ..................................................................................... 50
5 MALARIA KNOWLEDGE ......................................................................................................... 59 5.1 General Knowledge of Malaria ......................................................................................... 59 5.2 Knowledge of Causes of Malaria ...................................................................................... 60 5.3 Knowledge of Symptoms of Malaria and of Severe Malaria ............................................ 60 5.4 Knowledge of Malaria Prevention ..................................................................................... 61 5.5 Knowledge of Malaria Treatment ...................................................................................... 62

iv • Contents
5.6 Correct Knowledge of Malaria .......................................................................................... 63 5.7 Knowledge of Specific Groups Most Affected by Malaria ............................................... 64 5.8 Exposure to Malaria Messages .......................................................................................... 64
REFERENCES ........................................................................................................................................... 75
APPENDIX A SAMPLE DESIGN .......................................................................................................... 77 APPENDIX B ESTIMATES OF SAMPLING ERRORS ..................................................................... 81 APPENDIX C SAMPLE IMPLEMENTATION ................................................................................... 89 APPENDIX D SURVEY PERSONNEL ................................................................................................. 91 APPENDIX E QUESTIONNAIRES ..................................................................................................... 449

Tables and Figures • v
TABLES AND FIGURES
1 INTRODUCTION AND SURVEY METHODOLOGY .............................................................. 1 Table 1.1 Results of the household and individual interviews ............................................... 5
2 CHARACTERISTICS OF HOUSEHOLDS AND WOMEN ...................................................... 9 Table 2.1 Household drinking water .................................................................................... 16 Table 2.2 Household sanitation facilities ............................................................................. 17 Table 2.3 Household characteristics .................................................................................... 18 Table 2.4 Wealth quintiles ................................................................................................... 19 Table 2.5 Household possessions ......................................................................................... 20 Table 2.6 Household population by age, sex, and residence ................................................ 21 Table 2.7 Household composition ....................................................................................... 22 Table 2.8 Background characteristics of respondents .......................................................... 23 Table 2.9 Educational attainment of women ........................................................................ 24 Table 2.10 Literacy of women ............................................................................................... 25 Figure 2.1 Household drinking water by residence ............................................................... 10 Figure 2.2 Household toilet facilities by residence ............................................................... 10 Figure 2.3 Household wealth by residence............................................................................ 12 Figure 2.4 Population pyramid .............................................................................................. 13 Figure 2.5 Education of survey respondents by urban/rural residence .................................. 14 Figure 2.6 Trends in literacy by region ................................................................................. 15
3 MALARIA PREVENTION .......................................................................................................... 27 Table 3.1 Household possession of mosquito nets ............................................................... 36 Table 3.2 Source of mosquito nets ....................................................................................... 37 Table 3.3 Preferences of mosquito net ................................................................................. 38 Table 3.4 Access to an insecticide-treated net (ITN) ........................................................... 39 Table 3.5 Use of mosquito nets by persons in the household .............................................. 40 Table 3.6 Use of existing ITNs ............................................................................................ 41 Table 3.7 Use of mosquito nets by children ......................................................................... 42 Table 3.8 Use of mosquito nets by pregnant women ........................................................... 43 Table 3.9 Use of Intermittent Preventive Treatment (IPTp) by women during pregnancy .. 44 Figure 3.1 Household ownership of ITNs ............................................................................. 28 Figure 3.2 Trends in ITN ownership ..................................................................................... 29 Figure 3.3 ITN ownership by district .................................................................................... 29 Figure 3.4 Sources of ITNs ................................................................................................... 30 Figure 3.5 Access to and use of ITNs ................................................................................... 31 Figure 3.6 Trends in ITN access and use .............................................................................. 31 Figure 3.7 ITN use by household population ........................................................................ 32 Figure 3.8 ITN use by household population in households owning ITNs ........................... 32 Figure 3.9 ITN use by children and pregnant women ........................................................... 33 Figure 3.10 ITN use by children under 5 ................................................................................ 34 Figure 3.11 Trends in IPTp use by pregnant women .............................................................. 35

vi • Tables and Figures
4 MALARIA IN CHILDREN ......................................................................................................... 45 Table 4.1 Prevalence, care seeking and diagnosis of children with fever ............................ 53 Table 4.2 Source of advice or treatment for children with fever ......................................... 54 Table 4.3 Type of antimalarial drugs used ........................................................................... 55 Table 4.4 Coverage of testing for anaemia and malaria ....................................................... 56 Table 4.5 Haemoglobin <8.0 g/dl in children ...................................................................... 57 Table 4.6 Prevalence of malaria in children ......................................................................... 58 Figure 4.1 Trends in care seeking for fever in children by source of care ............................ 46 Figure 4.2 Diagnostic testing of children with fever by region ............................................. 47 Figure 4.3 Trends in ACT use by children under age 5 ........................................................ 48 Figure 4.4 Prevalence of low haemoglobin in children by district ........................................ 49 Figure 4.5 Low haemoglobin among children by household wealth..................................... 49 Figure 4.6 Trends in prevalence of malaria in children by district ........................................ 51 Figure 4.7 Prevalence of malaria in children by district........................................................ 51
5 MALARIA KNOWLEDGE ......................................................................................................... 59 Table 5.1 General knowledge of malaria ............................................................................. 66 Table 5.2 Knowledge of causes of malaria .......................................................................... 67 Table 5.3 Knowledge of malaria symptoms ........................................................................ 68 Table 5.4 Knowledge of symptoms of severe malaria ......................................................... 69 Table 5.5 Knowledge of ways to avoid malaria ................................................................... 70 Table 5.6 Knowledge of malaria treatment .......................................................................... 71 Table 5.7 Correct knowledge of malaria .............................................................................. 72 Table 5.8 Knowledge of specific groups most affected by malaria ..................................... 73 Table 5.9 Media exposure to malaria messages ................................................................... 74 Figure 5.1 Trends in knowledge of symptoms, causes, and prevention of malaria ............... 61 Figure 5.2 Knowledge of malaria treatment .......................................................................... 62 Figure 5.3 Trends in composite malaria knowledge ............................................................. 63 Figure 5.4 Source of malaria messages ................................................................................. 65
APPENDIX A SAMPLE DESIGN .......................................................................................................... 77 Table A.1 Households ........................................................................................................... 77 Table A.2 Enumeration areas ................................................................................................ 78 Table A.3 Sample allocation ................................................................................................. 79 Table A.4 Sample allocation of women ................................................................................ 79
APPENDIX B ESTIMATES OF SAMPLING ERRORS ..................................................................... 81 Table B.2 Sampling errors: Total sample, Sierra Leone MIS 2016 ...................................... 83 Table B.3 Sampling errors: Urban sample, Sierra Leone MIS 2016 .................................... 83 Table B.4 Sampling errors: Rural sample, Sierra Leone MIS 2016 ..................................... 83 Table B.5 Sampling errors: Eastern Region sample, Sierra Leone MIS 2016 ...................... 83 Table B.6 Sampling errors: Northern Region sample, Sierra Leone MIS 2016 ................... 84 Table B.7 Sampling errors: Southern Region sample, Sierra Leone MIS 2016 ................... 84 Table B.8 Sampling errors: Western Region sample, Sierra Leone MIS 2016 .................... 84 Table B.9 Sampling errors: Kailahun sample, Sierra Leone MIS 2016 ............................... 84 Table B.10 Sampling errors: Kenema sample, Sierra Leone MIS 2016 ................................. 85 Table B.11 Sampling errors: Kono sample, Sierra Leone MIS 2016 ..................................... 85 Table B.12 Sampling errors: Bombali sample, Sierra Leone MIS 2016 ................................ 85 Table B.13 Sampling errors: Kambia sample, Sierra Leone MIS 2016 ................................. 85 Table B.14 Sampling errors: Koinadugu sample, Sierra Leone MIS 2016 ............................ 86 Table B.15 Sampling errors: Port Loko sample, Sierra Leone MIS 2016 .............................. 86

Tables and Figures • vii
Table B.16 Sampling errors: Tonkolili sample, Sierra Leone MIS 2016 ............................... 86 Table B.17 Sampling errors: Bo sample, Sierra Leone MIS 2016 ......................................... 86 Table B.18 Sampling errors: Bonthe sample, Sierra Leone MIS 2016 ................................... 87 Table B.19 Sampling errors: Moyamba sample, Sierra Leone MIS 2016 .............................. 87 Table B.20 Sampling errors: Pujehun sample, Sierra Leone MIS 2016 ................................. 87 Table B.21 Sampling errors: Western Area Rural sample, Sierra Leone MIS 2016 .............. 87 Table B.22 Sampling errors: Western Area Urban sample, Sierra Leone MIS 2016 ............. 88
APPENDIX C SAMPLE IMPLEMENTATION ................................................................................... 89 Table C.1 Household age distribution .................................................................................. 89 Table C.2 Age distribution of eligible and interviewed women ........................................... 90 Table C.3 Completeness of reporting ................................................................................... 90 Table C.4 Births by calendar years ....................................................................................... 90


Acronyms and Abbreviations • xi
ACRONYMS AND ABBREVIATIONS
ACT Artemisinin-based combination therapy Ag Antigen ANC Antenatal care ASAQ Artesunate + amodiaquine CDC US Centers for Disease Control and Prevention Co-PR Co-principal recipient COMAHS College of Medicine and Allied Health Services CRS Catholic Relief Services CSPro Census Survey Processing Software DHS Demographic and Health Survey DPC Directorate of Disease Prevention and Control DPI Directorate of Planning and Information EA Enumeration area FISIM Financial intermediation services indirectly measured g/dl Grams per decilitre the Global Fund Global Fund to Fight AIDS, Tuberculosis, and Malaria GPS Global positioning system Hb Haemoglobin HDR Human Development Report HMM Home management of malaria HRP2 Histidine-rich protein 2 IPT Intermittent preventive treatment IPTp Intermittent preventive treatment in pregnancy IRB Institutional review board IRS Indoor residual spraying ITN Insecticide-treated net KAP Knowledge, Attitudes, and Practices LLIN Long-lasting insecticidal net MDGs Millennium Development Goals MERG Monitoring and Evaluation Reference Group MICS Multiple Indicator Cluster Survey MIS Malaria Indicator Survey MoHS Ministry of Health and Sanitation NMCP National Malaria Control Programme NMSP National Malaria Strategic Plan

xii • Acronyms and Abbreviations
PSM Procurement and supply management PSU Primary sampling unit RBM Roll Back Malaria RBM-MERG Roll Back Malaria Monitoring & Evaluation Reference Group RDT Rapid diagnostic test/testing SLMIS Sierra Leone Malaria Indicator Survey SLPHC Sierra Leone Population and Housing Census SP Sulphadoxine-pyrimethamine SRs Sub-recipients SSL Statistics Sierra Leone TWG Technical working group UNDP United Nations Development Programme UNICEF United Nations Children’s Fund USL University of Sierra Leone WHO World Health Organization

Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS) • xiii
READING AND UNDERSTANDING THE 2016 SIERRA LEONE MALARIA INDICATOR SURVEY (SLMIS)
he 2016 Sierra Leone Malaria Indicator Survey (SLMIS) report is very similar in content to the 2013 SLMIS but is presented
in a new format. The new style features more figures to highlight trends, subnational patterns, and background characteristics. The text has been simplified to highlight key points in bullets and to clearly identify indicator definitions in boxes.
The tables in this report are located at the end of each chapter instead of being imbedded in the chapter text. This final report is based on approximately 35 tables of data. While the text and figures featured in each chapter highlight some of the most important findings from the tables, not every finding can be discussed or displayed graphically. For this reason, data users should be comfortable reading and interpreting tables.
The following pages provide an introduction to the organization of MIS tables, the presentation of background characteristics, and a brief summary of sampling and understanding denominators. In addition, this section provides some exercises for users as they practice their new skills in interpreting MIS tables.
T

xiv • Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS)
EXAMPLE 1: PREVALENCE OF MALARIA IN CHILDREN
Table 4.6 Prevalence of malaria in children
Percentage of children age 6-59 months classified in two tests as having malaria, by background characteristics, Sierra Leone MIS 2016
Malaria prevalence according
to RDT Malaria prevalence according
to microscopy Background characteristic RDT positive
Number of children
Microscopy positive
Number of children
Age in months 6-8 30.3 413 23.3 414 9-11 34.2 378 25.3 379 12-17 43.0 749 30.3 750 18-23 45.6 592 30.1 596 24-35 57.1 1,395 40.0 1,397 36-47 56.3 1,557 46.9 1,560 48-59 63.1 1,559 50.1 1,561
Sex Male 53.5 3,316 40.4 3,322 Female 52.0 3,329 39.9 3,336
Mother’s interview status Interviewed 51.3 5,016 38.2 5,017 Not interviewed1 57.1 1,629 46.0 1,641
Residence Urban 31.5 2,545 25.2 2,555 Rural 65.9 4,099 49.4 4,103
Region Eastern 59.8 1,467 40.4 1,468 Northern 64.6 2,362 51.8 2,364 Southern 59.2 1,411 39.5 1,411 Western 18.8 1,404 20.9 1,414
District Kailahun 67.0 564 45.0 564 Kenema 59.3 536 37.7 535 Kono 49.5 367 37.5 369 Bombali 47.7 526 37.6 528 Kambia 59.4 265 48.3 265 Koinadugu 78.1 383 57.9 383 Port Loko 69.8 515 58.5 515 Tonkolili 68.3 673 55.7 673 Bo 57.1 594 39.7 593 Bonthe 46.8 184 26.1 184 Moyamba 60.6 330 39.9 330 Pujehun 69.2 304 46.8 304 Western Area Rural 33.5 711 34.9 721 Western Area Urban 3.8 693 6.3 693
Mother’s education2 No education 55.2 3,038 41.2 3,040 Primary 57.5 729 43.2 729 Secondary 38.7 1,222 28.4 697 More than secondary * 26 * 26
Wealth quintile Lowest 66.9 1,427 51.7 1,427 Second 68.1 1,433 52.4 1,434 Middle 62.4 1,306 44.9 1,307 Fourth 43.9 1,355 31.8 1,359 Highest 14.4 1,124 14.5 1,131
Total 52.7 6,644 40.1 6,658
1 Includes children whose mothers are deceased. 2 Excludes children whose mothers are not interviewed. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.
Step 1: Read the title and subtitle. They tell you the topic and the specific population group being described. In this case, the table is about children age 6-59 months who were tested for malaria.
Step 2: Scan the column headings—highlighted in green in Example 1. They describe how the information is categorized. In this table, the first column of data shows children who tested positive for malaria according to the rapid diagnostic test or RDT. The second column lists the number of children age 6-59 months who were tested for malaria using RDT in the survey. The third column shows children who tested positive for malaria
1
2 3
4
5

Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS) • xv
according to microscopy. The last column lists the number of children age 6-59 months who were tested for malaria using microscopy in the survey.
Step 3: Scan the row headings—the first vertical column highlighted in blue in Example 1. These show the different ways the data are divided into categories based on population characteristics. In this case, the table presents prevalence of malaria by age, sex, mother’s interview status, urban-rural residence, region, district, mother’s educational level, and wealth quintile.
Step 4: Look at the row at the bottom of the table highlighted in red. These percentages represent the totals of children age 6-59 months who tested positive for malaria according to the different tests. In this case, 52.7% of children age 6-59 months tested positive for malaria according to RDT, while 40.1% tested positive for malaria according to microscopy.
Step 5: To find out what percentage of children age 6-59 in rural areas tested positive for malaria according to microscopy, draw two imaginary lines, as shown on the table. This shows that 49.4% of children age 6-59 months in rural areas tested positive for malaria according to microscopy.
Step 6: By looking at patterns by background characteristics, we can see how malaria prevalence varies across Sierra Leone. Resources are often limited; knowing how malaria prevalence varies among different groups can help program planners and policy makers determine how to most effectively use resources.
Practice: Use the table in Example 1 to answer the following questions about malaria prevalence by microscopy:
a) Is malaria prevalence higher among boys or girls?
b) Is there a clear pattern in malaria prevalence by age?
c) What are the lowest and highest percentages (range) of malaria prevalence by region?
d) What are the lowest and highest percentages (range) of malaria prevalence by district?
e) Is there a clear pattern in malaria prevalence by mother’s education level?
f) Is there a clear pattern in malaria prevalence by wealth quintile?
Answers:
a) There is nearly no difference in malaria prevalence by microscopy between boys (40.4%) and girls (39.9%).
b) Yes, malaria prevalence generally increases with age from 23.3% among children age 6-8 months to 50.1% among children age 48-59 months.
c) Malaria prevalence is lowest in Western Region (20.9%) and highest in Northern Region (51.8%).
d) Malaria prevalence varies from a low of 6.3% in Western Area Urban district to a high of 58.5% in Port Loko.
e) Malaria prevalence is lowest among children whose mothers have secondary education (28.4%).
f) Yes, malaria prevalence generally decreases as household wealth increases; malaria prevalence is highest among children living in households in the second (52.4%) and lowest (51.7%) wealth quintiles and is lowest among children in households in the highest wealth quintile (14.5%).

xvi • Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS)
EXAMPLE 2: USE OF MOSQUITO NETS BY PREGNANT WOMEN
Table 3.8 Use of mosquito nets by pregnant women
Percentages of pregnant women age 15-49 who, the night before the survey, slept under a mosquito net (treated or untreated), under an insecticide-treated net (ITN), under a long-lasting insecticidal net (LLIN), and under an ITN or in a dwelling in which the interior walls have been sprayed against mosquitoes (IRS) in the past 12 months; and among pregnant women age 15-49 in households with at least one ITN, the percentage who slept under an ITN the night before the survey, by background characteristics, Sierra Leone MIS 2016
Among pregnant women age 15-49 in all households
Among pregnant women age 15-49 in households with at
least one ITN1
Background characteristic
Percentage who slept under any
mosquito net last night
Percentage who slept
under an ITN1 last night
Percentage who slept
under an LLIN last night
Number of women
Percentage who slept
under an ITN1 last night
Number of women
Residence Urban 31.4 30.7 30.7 267 65.7 124 Rural 53.0 52.8 52.8 404 79.0 270
Region Eastern 51.2 49.5 49.5 167 76.4 108 Northern 44.7 44.7 44.7 245 73.1 150 Southern 60.9 60.9 60.9 128 84.2 92 Western 19.0 19.0 19.0 130 (56.7) 44
District Kailahun (46.2) (46.2) (46.2) 49 (77.6) 29 Kenema (71.8) (71.8) (71.8) 55 (92.9) 43 Kono 36.9 32.6 32.6 63 (56.0) 37 Bombali 51.8 51.8 51.8 60 (84.8) 37 Kambia 46.4 46.4 46.4 33 (71.1) 21 Koinadugu (63.5) (63.5) (63.5) 31 (87.6) 23 Port Loko 31.0 31.0 31.0 73 (62.9) 36 Tonkolili (43.3) (43.3) (43.3) 48 (62.5) 33 Bo 67. 8 67.8 67.8 64 (90.3) 48 Bonthe (55.8) (55.8) (55.8) 13 * 10 Moyamba (63.8) (63.8) (63.8) 21 * 15 Pujehun (46.5) (46.5) (46.5) 30 (71.7) 20 Western Area Rural (28.1) (28.1) (28.1) 53 * 22 Western Area Urban (12.6) (12.6) (12.6) 77 * 21
Education No education 47.4 47.4 47.4 348 82.0 201 Primary 33.5 33.5 33.5 121 56.1 72 Secondary 45.5 44.1 44.1 197 73.3 119 More than secondary * * * 4 * 3
Wealth quintile Lowest 52.5 52.5 52.5 152 87.5 91 Second 45.3 44.6 44.6 123 66.1 83 Middle 57.2 57.2 57.2 123 80.6 87 Fourth 40.4 39.1 39.1 135 73.3 72 Highest 27.2 27.2 27.2 137 (61.2) 61
Total 44.4 44.0 44.0 671 74.8 395
Note: Table is based on women who stayed in the household the night before the interview. Numbers in parentheses are based on 25-49 unweighted cases. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed. 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months.
Step 1: Read the title and subtitle. In this case, the table is about two separate groups of pregnant women: all pregnant women age 15-49 in all households (a) and pregnant women age 15-49 in households with at least one insecticide-treated net (ITN) (b).
Step 2: Identify the two panels. First, identify the columns that refer to all pregnant women age 15-49 in all households (a), and then isolate the columns that refer only to pregnant women age 15-49 in households with at least one ITN (b).
Step 3: Look at the number of women included in this table. How many pregnant women age 15-49 in all households were interviewed? It’s 671. Now look at the second panel. How many pregnant women age 15-49 in households with at least one ITN were interviewed? It’s 395.
1
2
3 3
4
a 4
b

Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS) • xvii
Step 4: Only 671 pregnant women age 15-49 in all households and 395 pregnant women in households with at least one ITN were interviewed in the 2016 SLMIS. Once these pregnant women are further divided into the background characteristic categories, there may be too few cases for the percentages to be reliable.
� What percentage of pregnant women age 15-49 in all households in Kailahun district slept under an ITN the night before the survey? 46.2%. This percentage is in parentheses because there are between 25 and 49 pregnant women (unweighted) in this category. Readers should use this number with caution—it may not be reliable. (For more information on weighted and unweighted numbers, see Example 3.)
� What percentage of pregnant women age 15-49 with more than secondary education in households with at least one ITN slept under an ITN the night before the survey? There is no number in this cell—only an asterisk. This is because fewer than 25 pregnant women with more than secondary education in households with at least one ITN were interviewed in the survey. Results for this group are not reported. The subgroup is too small, and therefore the data are not reliable.
Note: When parentheses or asterisks are used in a table, the explanation will be noted under the table. If there are no parentheses or asterisks in a table, you can proceed with confidence that enough cases were included in all categories that the data are reliable.

xviii • Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS)
EXAMPLE 3: UNDERSTANDING SAMPLING WEIGHTS IN SLMIS TABLES
A sample is a group of people who have been selected for a survey. In the 2016 SLMIS, the sample is designed to represent the national population age 15-49. In addition to national data, most countries want to collect and report data on smaller geographical or administrative areas. However, doing so requires a minimum sample size per area. For the 2015 SLMIS, the survey sample is representative at the national, regional, and district levels, and for urban and rural areas.
To generate statistics that are representative of the country as a whole and the 14 districts, the number of women surveyed in each district should contribute to the size of the total (national) sample in proportion to size of the district. However, if some districts have small populations, then a sample allocated in proportion to each district’s population may not include sufficient women from each district for analysis. To solve this problem, districts with small populations are oversampled. For example, let’s say that you have enough money to interview 8,501 women and want to produce results that are representative of Sierra Leone as a whole and its districts (as in Table 2.8). However, the total population of Sierra Leone is not evenly distributed among the districts: some districts, such as Western Area Urban, are heavily populated while others, such as Bonthe are not. Thus, Bonthe must be oversampled.
A sampling statistician determines how many women should be interviewed in each district in order to get reliable statistics. The blue column (1) in the table at the right shows the actual number of women interviewed in each district. Within the districts, the number of women interviewed ranges from 504 in Bonthe to 753 in Western Area Rural district. The number of interviews is sufficient to get reliable results in each district.
With this distribution of interviews, some districts are overrepresented and some districts are underrepresented. For example, the population in Western Area Urban district is about 13% of the population in Sierra Leone, while Bonthe’s population contributes only 2.6% of the population in Sierra Leone. But as the blue column shows, the number of women interviewed in Western Area Urban accounts for only about 7.5% of the total sample of women interviewed (637/8,501) and the number of women interviewed in Bonthe district accounts 5.9% of the total sample of women interviewed (504/8,501). This unweighted distribution of women does not accurately represent the population.
In order to get statistics that are representative of Sierra Leone, the distribution of the women in the sample needs to be weighted (or mathematically adjusted) such that it resembles the true distribution in the country. Women from a small district, Bonthe, should only contribute a small amount to the national total. Women from a large district, like Western Area Urban, should contribute much more. Therefore, DHS statisticians mathematically calculate a “weight” which is used to adjust the number of women from each district so that each district’s contribution to the total is proportional to the actual population of the district. The numbers in the purple column (2) represent the “weighted” values. The weighted values can be smaller or larger than the unweighted values at district level. The total national sample size of 8,501 women has not changed after weighting, but the distribution of the women in the districts has been changed to represent their contribution to the total population size.
How do statisticians weight each category? They take into account the probability that a woman was selected in the sample. If you were to compare the red column (3) to the actual population distribution of
Table 2.8 Background characteristics of respondents
Percent distribution of women age 15-49 by selected background characteristics, Sierra Leone MIS 2016
Women Background characteristic
Weighted percent
Weighted number
Unweighted number
District Kailahun 7.9 670 526 Kenema 7.7 656 577 Kono 7.2 610 600 Bombali 8. 6 732 675 Kambia 4.3 363 621 Koinadugu 5.1 434 597 Port Loko 7.3 617 540 Tonkolili 8.7 739 696 Bo 8.4 710 547 Bonthe 2.6 225 504 Moyamba 5.3 452 664 Pujehun 4.1 349 564 Western Area Rural 9.5 812 753 Western Area Urban 13.3 1,133 637
Total 15-49 100.0 8,501 8,501
3 2 1

Reading and Understanding the 2016 Sierra Leone Malaria Indicator Survey (SLMIS) • xix
Sierra Leone, you would see that women in each district are contributing to the total sample with the same weight that they contribute to the population of the country. The weighted number of women in the survey now accurately represents the proportion of women who live in Western Area Urban and the proportion of women who live in Bonthe.
With sampling and weighting, it is possible to interview enough women to provide reliable statistics at national and provincial levels. In general, only the weighted numbers are shown in each of the SLMIS tables, so don’t be surprised if these numbers seem low: they may actually represent a larger number of women interviewed.

xx • Map of Sierra Leone

Introduction and Survey Methodology • 1
INTRODUCTION AND SURVEY METHODOLOGY 1
he 2016 Sierra Leone Malaria Indicator Survey (SLMIS) was conducted by the National Malaria Control Programme (NMCP) of the Ministry of Health and Sanitation (MoHS), in collaboration with Catholic Relief Services (CRS), College of Medicine and Allied Health Sciences University
of Sierra Leone (COMAHS-USL), and Statistics Sierra Leone (SSL). Data collection took place from 29 June 2016 to 4 August 2016. ICF (formerly ICF International) provided technical assistance. The 2016 SLMIS was funded by the Global Fund. Other agencies and organisations that facilitated the successful implementation of the survey through technical or logistical support were the World Health Organization (WHO) and the United Nation Children’s Fund (UNICEF).
1.1 SURVEY OBJECTIVES
The 2016 SLMIS, a comprehensive, nationally-representative household survey, was designed in line with the Roll Back Malaria Monitoring and Evaluation Working Group (RBM-MERG) guidelines. The primary objective of the survey was to provide up-to-date estimates of basic demographic and health indicators related to malaria. On site in Sierra Leone, the survey team collected data on vector control interventions such as mosquito nets and indoor residual spraying of insecticides, on intermittent preventive treatment of malaria in pregnant women, and on care seeking and treatment of fever in children. Young children were also tested for anaemia and for malaria infection. Knowledge of malaria was assessed among interviewed women. The information collected during the survey will assist policy makers and programme managers in evaluating and designing programmes and strategies for improving malaria control. The broader goal is to improve the health of the country’s population and provide estimates of indicators defined in the 2016-2020 National Malaria Strategic Plan (MoHS 2015a).
1.2 SAMPLE DESIGN
The 2016 SLMIS followed a two-stage sample design and was intended to allow estimates of key indicators for the following domains:
� National � Urban and rural areas � Four regions: Northern, Southern, Eastern and Western � Fourteen administrative districts: Bo, Bombali, Bonthe, Kailahun, Kambia, Kenema, Koinadugu,
Kono, Moyamba, Port Loko, Pujehun, Tonkolili, Western Area Rural, and Western Area Urban.
Data was disaggregated by district because the health system is managed by district.
The first stage of sampling involved selecting sample points (clusters) from the sampling frame. Enumeration areas (EAs) delineated by Statistics Sierra Leone for the 2015 Sierra Leone Population and Housing Census (SLPHC) were used as the sampling frame (SSL 2016). A total of 336 clusters were selected with probability proportional to size from the 12,856 EAs covered in the 2015 SLPHC. Of these clusters, 99 were in urban areas and 237 in rural areas. Urban areas were oversampled within regions in order to produce robust estimates for that domain.
The second stage of sampling involved systematic selection of households. A household listing operation was undertaken in all of the selected EAs in May 2016, and households to be included in the survey were randomly selected from these lists. Twenty households were selected from each EA, for a total sample size of 6,720 households. Because of the approximately equal sample sizes in each district, the sample is not
T

2 • Introduction and Survey Methodology
self-weighting at the national level. Results shown in this report have been weighted to account for the complex sample design. See Appendix A for additional details on the sampling procedures.
All women age 15-49 who were either permanent residents of the selected households or visitors who stayed in the household the night before the survey were eligible to be interviewed. With the parent’s or guardian’s consent, children age 6-59 months were tested for anaemia and for malaria infection.
1.3 QUESTIONNAIRES
Three questionnaires—the Household Questionnaire, the Woman’s Questionnaire, and the Biomarker Questionnaire—were used for the 2016 SLMIS. Core questionnaires available from the RBM-MERG were adapted to reflect the population and health issues relevant to Sierra Leone. The modifications were decided upon at a series of meetings with various stakeholders from the National Malaria Control Programme (NMCP) and other government ministries and agencies, nongovernmental organisations, and international donors. The questionnaires were in English, and they were programmed onto tablet computers, enabling use of computer-assisted personal interviewing (CAPI) for the survey.
The Household Questionnaire was used to list all the usual members of and visitors to selected households. Basic information was collected on the characteristics of each person listed in the household, including his or her age, sex, and relationship to the head of the household. The data on the age and sex of household members, obtained from the Household Questionnaire, were used to identify women eligible for an individual interview and children age 6-59 months eligible for anaemia and malaria testing. Additionally, the Household Questionnaire captured information on characteristics of the household’s dwelling unit, such as the source of water, type of toilet facilities, materials used for the floor, ownership of various durable goods, and ownership and use of mosquito nets.
The Woman’s Questionnaire was used to collect information from all women age 15-49. These women were asked questions on the following main topics:
� Background characteristics (age, residential history, education, literacy, religion, and ethnicity) � Reproductive history for the last 6 years � Prenatal care and preventive malaria treatment for the most recent birth � Prevalence and treatment of fever among children under age 5 � Knowledge about malaria (symptoms, causes, how to prevent, and types of antimalarial
medications) � Preferences in mosquito nets and sources of media messages about malaria
The Biomarker Questionnaire was used to record the results of the anaemia and malaria testing of children 6-59 months, as well as the signatures of the fieldworker and the parent or guardian who gave consent.
Consent statements were developed for each tool (the Household, Woman’s, and Biomarker questionnaires). Further consent statements were formulated for malaria testing, anaemia testing, and treatment of children with positive malaria rapid diagnostic tests (RDTs). Signatures were obtained for each consent statement on a separate paper form and were confirmed on the digital form with the interviewer’s signature at each point of consent.
1.4 ANAEMIA AND MALARIA TESTING
Blood samples for biomarker testing were collected by finger- or heel-prick from children age 6-59 months. Each field team included one laboratory technician who carried out the anaemia and malaria testing and prepared the blood smears. A nurse provided malaria medications for children who tested positive for malaria, in accordance with the approved treatment protocols. The field laboratory technicians requested written, informed consent for each test from the child’s parent or guardian before the blood

Introduction and Survey Methodology • 3
samples were collected, according to the protocols approved by the Sierra Leone Ethics Committee and the institutional review board at ICF (formerly ICF International).
Anaemia testing. A single-use, retractable, spring-loaded, sterile lancet was used to make a finger- or heel-prick. A drop of blood from this site was then collected in a microcuvette. Haemoglobin analysis was carried out on site using a battery-operated portable HemoCue® analyser, which produces a result in less than one minute. Results were given to the child’s parent or guardian verbally and in writing. Parents of children with a haemoglobin level under 8 g/dl were advised to take the child to a health facility for follow-up care and were given a referral letter with the haemoglobin reading to show to staff at the health facility. Results of the anaemia test were recorded on the Biomarker Questionnaire and on a brochure left in the household that also contains information on the causes and prevention of anaemia.
Malaria testing using a rapid diagnostic test (RDT). Using the same finger- or heel-prick that was used for anaemia testing, another drop of blood was tested immediately using the Sierra Leone-approved SD BIOLINE Malaria Ag P.f. (HRP-II)™ rapid diagnostic test (RDT). This qualitative test detects the histidine-rich protein II antigen of malaria, Plasmodium falciparum (Pf), in human whole blood (Standard Diagnostics, Inc.). The parasite, transmitted by a mosquito, is the major cause of malaria in Sierra Leone. The diagnostic test includes a disposable sample applicator that comes in a standard package. A tiny volume of blood is captured on the applicator and placed in the well of the testing device. All field laboratory technicians were trained to perform the RDT in the field, in accordance with manufacturers’ instructions. RDT results were available in 20 minutes and recorded as either positive or negative, with faint test lines being considered positive. As with the anaemia testing, malaria RDT results were provided to the child’s parent or guardian in oral and written form and were recorded on the Biomarker Questionnaire.
Children who tested positive for malaria were offered a full course of medicine according to standard procedures for uncomplicated malaria treatment in Sierra Leone. To ascertain the correct dose, nurses on each field team were trained to use treatment guidance charts and to ask about any medications the child might already be taking. The nurses were also trained to identify signs and symptom of severe malaria. The nurses provided the age-appropriate dose of ACT along with instructions on how to administer the medicine to the child.
Malaria testing using blood smears. In addition to the RDT, thick blood smears were prepared in the field. Each blood smear slide was given a bar code label, with a duplicate affixed to the Biomarker Questionnaire. An additional copy of the bar code label was affixed to a blood sample transmittal form to track the blood samples from the field to the laboratory. The slides were dried in a dust-free environment and stored in slide boxes. The thick smear slides were collected regularly from the field, along with the completed Biomarker Questionnaires, and transported to the laboratory for logging and microscopic reading. Thick blood smears were stained with Giemsa stain and examined to determine the presence of Plasmodium infection. All stained slides were read by two independent microscopists masked from RDT results. Slides with discrepant RDT results were reanalysed by a third microscopist for final validation.
The microscopic results were quality checked by internal and external quality control processes. Internal quality control consisted of an independent microscopist who read 5% of all slides in the study. External quality control was conducted through the COMAHS-USL laboratory where 10% of samples were independently read.
1.5 PRETEST
The training for the pretest took place from 29 April 2016 to 20 May 2016. Overall, 35 people participated in the training, including four supervisors, four biomarker specialists, four nurses, four data collectors, and four laboratory scientists. CRS, SSL, USL, NMCP, and ICF staff members led the training and served as the supervisory team for the pretest fieldwork. Participants were trained to administer paper questionnaires, use computer-assisted personal interviewing (CAPI), and collect blood samples for anaemia and

4 • Introduction and Survey Methodology
parasitaemia testing. The pretest training consisted of the survey overview and objectives, techniques of interviewing, field procedures, a detailed description of all sections of the Household and the Woman’s questionnaires, instruction on the CAPI data collection application, and 6 days of field practice. At the end of fieldwork, a debriefing session was held, and the questionnaires and CAPI applications were modified based on the findings from the field.
1.6 TRAINING OF FIELD STAFF
The training, which was coordinated by ICF, CRS, NMCP, SSL, COMAHS-USL, and other members of the technical working group, took place 3-24 June 2016 at the Hill Valley Hotel Conference Centre in Freetown. The NMCP, in collaboration with the SSL, recruited 129 people to attend the 3-week interviewer, supervisor, and biomarker training. All the field staff participated in a 1-week training session, focusing on how to fill out the Household and Woman’s questionnaires, mock interviews, and interviewing techniques on paper questionnaires. The second week focused on filling out the Household and Women’s Questionnaires using the CAPI application. Two quizzes were administered to assess how well the participants absorbed the training materials, both on the paper questionnaires and using the CAPI application as data collection tools.
During the third week of training, NMCP conducted a briefing on the epidemiology of malaria and the malaria control programme in Sierra Leone for all the field personnel. The rest of the training was conducted in two parallel sessions: one for the interviewers and field supervisors and one for the health personnel and laboratory technicians. The training of interviewers and field supervisors focused on the use of CAPI for data collection, assigning households to interviewers, and transferring data for completed questionnaires in completed clusters to the central data processing centre at CRS headquarters.
ICF conducted a 2-week training of health personnel and laboratory technicians, which focused on preparing blood samples to test for anaemia and using the RDT to test for malaria. The training involved presentation, discussion, and actual testing for anaemia and malaria. The technicians were trained to identify children eligible for testing, administer informed consent, conduct the anaemia and malaria rapid testing, and make a proper thick blood smear. They were also trained to store the blood slides, record test results on the Biomarker Questionnaire, and provide the results to the parents/guardians of the children tested. Finally, health personnel received a briefing on correct treatment protocols.
All participants took part in 3-day field practice exercises in the West Area Rural district and in Aberdeen in the West Area Urban district. Health technicians were also trained on how to record children’s anaemia and malaria results on the respective brochures and how to fill in the referral slip for any child who was found to be severely anaemic.
1.7 FIELDWORK
Twenty-eight teams were organised for field data collection. Each team consisted of one field supervisor, one health professional to interview and administer treatment, one experienced survey implementer with map reading skills, one laboratory technician to conduct biomarker testing, and one driver. The field staff also included 14 district coordinators and 14 district runners who collected slides from the field teams and delivered them to the COMHAS-USL laboratory at Jui.
The CRS arranged for printing of questionnaires, manuals, consent forms, brochures, and other field forms. CRS organised field supplies such as backpacks and identification cards. CRS and SSL coordinated the fieldwork logistics.
Field data collection for the 2016 SL MIS started on 27 June 2016. For maximum supervision, all 28 teams were visited by national monitors, largely members of the technical working group, at least once in every week. Fieldwork was completed on 4 August 2016.

Introduction and Survey Methodology • 5
1.8 LABORATORY TESTING
Prior to the start of the field staff training, an ICF staff person worked with the laboratory technicians at the SLMIS Malaria Laboratory at COMAHS-USL to ensure training of the laboratory staff on the MIS protocol. Additionally, ICF staff worked on site with the laboratory staff for one week in May 2016 to assist the team with microscopy.
Standard protocols were used to read blood slides for the presences of malaria parasites. All microscopic slides were stained with Giemsa and read by laboratory technicians. Blood smears were considered negative if no parasites were found after counting 200 fields. For quality control, all slides were read by a second laboratory technician, and a third reviewer, the laboratory director, settled any discrepant readings. In addition, 10% of the slides were re-read by an independent, external microscopist to ascertain the quality of microscopy reading.
1.9 DATA PROCESSING
Data for the 2016 SLMIS were collected through questionnaires programmed onto the CAPI application. The CAPI were programmed by ICF and loaded with the Household, Biomarker, and Woman’s Questionnaires. Using the cloud, the field supervisors transferred data on a daily basis to a central location for data processing at CRS in Freetown. To facilitate communication and monitoring, each field worker was assigned a unique identification number.
ICF provided technical assistance for processing the data using Censuses and Surveys Processing (CSPro) system for data editing, cleaning, weighting, and tabulation. In the CRS central office, data received from the field teams’ CAPI applications were registered and checked against any inconsistencies and outliers. Data editing and cleaning included an extensive range of structural and internal consistency checks. Any anomalies were communicated to the CRS so that the CRS and ICF data processing teams could resolve data discrepancies. The corrected results were maintained in master CSPro data files at ICF and used for analysis in producing tables for the final report.
1.10 RESPONSE RATES
Table 1.1 shows that of the 6,720 households selected for the sample, 6,719 were occupied at the time of fieldwork. Among the occupied households, 6,719 were successfully interviewed, yielding a total household response rate of nearly 100%. In the interviewed households, 8,526 eligible women were identified to be eligible for individual interview and 8,501 were successfully interviewed, yielding a response rate of 99.7%.
Table 1.1 Results of the household and individual interviews
Number of households, number of interviews, and response rates, according to residence (unweighted), Sierra Leone MIS 2016
Residence Total Result Urban Rural
Household interviews Households selected 1,980 4,740 6,720 Households occupied 1,980 4,739 6,719 Households interviewed 1,980 4,739 6,719
Household response rate1 100.0 100.0 100.0
Interviews with women age 15-49 Number of eligible women 2,801 5,725 8,526 Number of eligible women interviewed 2,796 5,705 8,501
Eligible women response rate2 99.8 99.7 99.7 1 Households interviewed/households occupied 2 Respondents interviewed/eligible respondents

6 • Introduction and Survey Methodology
1.11 MALARIA CONTROL IN THE CONTEXT OF THE EBOLA EPIDEMIC
In May 2014, Sierra Leone experienced its first cases of Ebola Virus Disease (EVD) in the remote eastern part of the country, at its intersection with Guinea and Liberia. The outbreak quickly progressed from a localised to a generalised epidemic, shifting from the sparsely populated east to more densely-settled urban and peri-urban areas in the west. Epidemiological reports have shown that the number of cases, widespread distribution (all 14 districts), and intense transmission of EVD from May 2014 onwards in Sierra Leone were unprecedented, outpacing the morbidity and mortality figures of neighbouring Guinea and Liberia. By September 2015, there were 8,704 confirmed cases and 3,585 deaths, making Sierra Leone the worst affected country in West Africa and the world (MoHS 2015b).
Evidence shows that the lack of infection prevention and control contributed to the rapid spread of the virus. Additionally, resources meant for other programmes, including malaria, were diverted to the containment of EVD, potentially reversing gains in addressing child mortality (Millennium Development Goal [MDG] 4), maternal mortality (MDG 5), and HIV/AIDS, malaria, and other diseases (MDG 6).
Health workers responding to the Ebola crisis were highly affected by the epidemic, given their high risk of exposure and infection through routine service delivery. By June 2015, 296 health care workers had been infected with EVD, with 221 deaths (74.6%), 11 of whom were specialised physicians. Prior to the EVD outbreak, the ratio of skilled providers to population was very low, at just 3.4:10,000, compared with optimal levels of 25:10,000. This critical loss of front-line health workers has exacerbated already inadequate human resources in the health sector. Increasing the number of skilled workers and their capacity is a central challenge for the post-Ebola recovery period.
The initial clinical presentation of EVD is very similar to that of malaria, i.e., fever, anorexia, fatigue, headache, and joint pains—posing a problem of differential diagnosis for both patients and health care workers. During the outbreak, patients who had signs and symptoms of malaria were often frightened to seek care, either due to fear of having EVD or fear of being mistakenly referred to Ebola holding centres with suspected EVD. In addition, patients with signs and symptoms of malaria were probably more likely to seek self-treatment through the private informal sector or to die at home for lack of access to prompt diagnosis and effective treatment. For cases that were referred, given the similarities of clinical presentation, the likelihood of persons with malaria being retained as suspected Ebola cases in holding centres was very high.
The ability to provide proper case management for malaria during the EVD outbreak was additionally challenged by lack of diagnostic capacity. In many health facilities, testing with RDTs or microscopy was temporarily suspended for fear of contracting Ebola, due to lack of personal protective equipment (PPE) for use by laboratory technicians and personnel performing these tests. Use of RDT did increase somewhat over the duration of the EVD outbreak because health workers got training on infection prevention and control and PPEs were increasingly available.
The EVD outbreak led to a decline in the utilisation of health care facilities for non-Ebola-related health needs, such as antenatal care visits, particularly in urban areas such as Freetown. The Ministry of Health and Sanitation in collaboration with UNICEF conducted the Sierra Leone Health Facility Survey 2014 to assess the impact of the EVD outbreak on Sierra Leone’s health system among 1,185 peripheral health units (MoHS 2014). Results showed that 48 of these facilities were closed at the time of assessment, with a similar number reporting temporary closure since the start of the epidemic. Although 96% of peripheral health units were operational in October 2014, the country recorded a drop in the coverage of key maternal and child health interventions, including malaria interventions, between May and September 2014:
� The number of antenatal care visits declined by 27% nationally from May to September 2014. Western Area (33%) and the Northern Province (32%) were the worst affected areas. Among the districts, Kambia witnessed a staggering 48% drop in the number of women coming for the 4th ANC visit. At the other end of the spectrum, Moyamba registered a decline of only 10%.

Introduction and Survey Methodology • 7
� The number of insecticide-treated nets (ITNs) distributed during ANC visits dropped by 63% nationally. The period under study coincided with the mass campaign to distribute ITNs to all households in the country (5-11 June 2014). Hence, the decline in ANC-distributed ITNs could also be attributed to the effect of the increasing availability of ITNs in households resulting from the mass campaign.
� The number of women coming to health facilities for delivery also declined significantly, by 27% nationally. Among provinces, the Northern Province experienced the strongest decline at 30%. Among districts, Kambia and Pujehun saw the largest declines at 41% each, whereas in Pujehun, the number of deliveries in health facilities declined by only 5%.
� The number of children under 5 treated for malaria declined by 39% between May and September. This decline took place at the height of the malaria season, during which malaria cases typically spike (in 2013, during the same period, the number of children under 5 coming for malaria treatment had increased by 20%).
The decline in essential child and maternal health interventions observed during the EVD outbreak was probably for multiple reasons. One likely factor is a decreased utilisation of health services, which resulted from a lack of trust in the health staff, a loss of confidence in the health system (as non-Ebola cases would mingle with Ebola cases), and safety-related concerns. Intervention coverage was also affected by the destruction of personal belongings in houses with confirmed Ebola Virus Disease as part of standard decontamination procedures. Beds, furniture, mosquito bed nets, utensils, plates, cups, and window curtains were reportedly burned.
All of these factors likely contributed to the trends in malaria intervention and malaria morbidity measured in the 2016 SLMIS.


Characteristics of Households and Women • 9
CHARACTERISTICS OF HOUSEHOLDS AND WOMEN 2
Key Findings
x Drinking water: Most urban households (91%) have access to an improved source of drinking water, but only slightly more than half (56%) of rural households do.
x Sanitation: Almost half of households (49%) use an unimproved toilet facility, 16% use an improved, not shared toilet facility, and 35% use an improved, shared toilet facility.
x Household Wealth: The majority of households in Western Area region are in the highest wealth quintile (68 %), while the majority of households in Southern region are in the lowest wealth quintile (31%).
x Electricity: One-fifth of households in Sierra Leone have electricity (47% in urban areas and 3% in rural areas).
x Bank Account/Village Savings/Osusu: Four in 10 households own a bank account (51% in urban areas and 34% in rural areas).
x Literacy: Overall, younger women are more likely to be literate than older women. Sixty-four percent of women age 15-24 are literate compared with 20% of women age 45-49.
nformation on the socioeconomic characteristics of the household population in the 2016 SLMIS provides context to interpret demographic and health indicators and also can indicate the representativeness of the survey. This information also sheds light on the living conditions of the
population.
In this chapter, there is information on source of drinking water, sanitation, wealth, ownership of durable goods, and composition of household population. In addition, the chapter presents characteristics of the survey respondents such as age, education, and literacy. Socioeconomic characteristics are useful for understanding the factors that affect use of health services and other health behaviours related to malaria control.
2.1 DRINKING WATER SOURCES AND TREATMENT
Improved sources of drinking water Include piped water, public taps, standpipes, tube wells, boreholes, protected dug wells and springs, and rainwater. Because the quality of bottled water is not known, households using bottled water for drinking are classified as using an improved source only if their water source for cooking and handwashing are from an improved source. Sample: Households
I

10 • Characteristics of Households and Women
Improved sources of water protect against outside contamination so that water is more likely to be safe to drink. In Sierra Leone, almost 70% of households have access to an improved source of drinking water (Table 2.1). Ninety-one percent of urban households and 56% of rural households have access to improved water sources.
Urban and rural households rely on different sources of drinking water. Only about 1 in 10 urban households have piped water in their dwelling or yard (Figure 2.1). A majority (37%) of households in urban areas access drinking water from protected dug wells. In contrast, rural households mainly rely on unimproved sources (44%), followed by protected dug wells (17%). Only 2% of rural households have piped water into their dwelling or yard, and 22% travel 30 minutes or more to fetch drinking water (Table 2.1).
Trends: The proportion of households obtaining water from improved sources increased from 56% in the 2013 SLMIS to 70% in the 2016 SLMIS. However, the gains are concentrated in urban households; the proportion of urban households with access to improved drinking water sources increased from 73% to 91%, compared with an increase from 49% to 56% in rural households over the same period.
2.2 SANITATION
Improved toilet facilities Include any non-shared toilet of the following types: flush/pour flush toilets to piped sewer systems, septic tanks, and pit latrines; ventilated improved pit (VIP) latrines; and pit latrines with slabs Sample: Households
Nationally, only 16% of households use an improved toilet facility, defined as a non-shared facility constructed to prevent contact with human waste and thus reduce the transmission of cholera, typhoid, and other diseases. Another 35% of households use an improved facility shared with other households (Table 2.2). Households in urban areas are more likely to use improved, non-shared facilities (26%) compared with rural households (8%) (Figure 2.2). The most commonly used improved, non-shared toilet facility is the pit latrine with a slab (9% of all households). Only 4% of households use an improved, non-shared facility that flushes to a septic tank. This proportion is higher among urban
Figure 2.1 Household drinking water by residence
Figure 2.2 Household toilet facilities by residence
9
4430
4
1
239
1927
9
1915
20
1416
194 10
Urban Rural All
Piped water intodwelling/yard/plotPublic tap/standpipe
Tubewell or borehole
Protected well orspringRain/bottled/sachetwaterUnimproved source
Percent distribution of households by source of drinking water
726 18
22
67
49
51
24
35
268 16
Urban Rural All
Improved facilityShared facilityUnimproved facilityNo facility/bush/field
Percent distribution of households by type of toilet facilities

Characteristics of Households and Women • 11
households (9%) than among rural households (less than 1%). Almost half (49%) of all households use an unimproved facility, and 18% lack access to any facility and use the bush or a field.
Trends: There has been no marked increase in the proportion of households with improved, non-shared toilet facilities since the 2013 SLMIS (10% in 2013 and 16% in 2016). However, the proportion of households with improved toilet facilities (shared or not shared) increased from 36% in the 2013 SLMIS to 51% in the 2016 SLMIS.
2.3 HOUSING CHARACTERISTICS
The 2016 SLMIS collected data on household features such as access to electricity, flooring material, number of sleeping rooms, and types of fuel used for cooking. The responses to these questions, along with information on ownership of household durable goods, contribute to the creation of the household wealth index and provide information that may be relevant for other health indicators.
Exposure to cooking smoke, especially to smoke produced from solid fuels, is potentially harmful to health. The use of solid fuels for cooking is nearly universal in both rural and urban households in Sierra Leone, with the major sources being charcoal and wood (Table 2.3).
Overall, 20% of households in Sierra Leone have access to electricity. Forty-seven percent of urban households and only 3% of rural households have access to electricity. There has been a slight increase in households reporting access to electricity, from 14% in the 2013 SLMIS to 20% in the 2016 SLMIS.
Earth or sand is the most common flooring material in Sierra Leone, used by 49% of all households. As expected, rural households are substantially more likely to have floors made of earth or sand (71%) than are urban households (16 %). Cement is the second most common flooring material, used by 39% of all households. Cement floors are more common in urban households (60%) than in rural households (26%).
The number of rooms a household uses for sleeping is an indicator of socioeconomic level and of crowding in the household, which can facilitate the spread of disease. Forty-five percent of households use three rooms for sleeping, 29% use two rooms, and 25% use only one room. There are slight urban-rural differences in the number of rooms used for sleeping, as 51% of rural households use three or more rooms for sleeping compared with 37% of households in urban areas (Table 2.3).
2.4 HOUSEHOLD WEALTH
Wealth index Households are given scores based on the number and kinds of consumer goods they own, ranging from a television to a bicycle or car, plus housing characteristics such as source of drinking water, toilet facilities, and flooring materials. These scores are derived using principal component analysis. National wealth quintiles are compiled by assigning the household score to each usual (de jure) household member, ranking each person in the household population by their score, and then dividing the distribution into five equal categories, each with 20% of the population. Sample: Households
By definition, 20% of the total household population is in each wealth quintile. However, the population distributions are unequal when stratifying by urban and rural areas. Forty-seven percent of the population in urban areas is in the highest quintile compared with only 2% of the population in rural areas. On the other hand, only 3% of the urban population falls in the lowest wealth quintile, compared with 32% of the rural population (Figure 2.3).

12 • Characteristics of Households and Women
Regionally, the Southern Region has the highest percentage of population in the lowest quintile (31%) compared with the Northern Region (27%), the Eastern Region (15%), and the Western Region (1%). At the district-level, Bonthe has the highest percentage of population in the lowest quintile (45%), and the population of Western Area Urban has the highest percentage in the highest wealth quintile (93%) (Table 2.4).
Household Durable Goods
Data from the survey revealed information on ownership of household effects, means of transport, agricultural land, bank accounts (including village savings and loans and osusu, which are traditional group saving schemes). Urban households are more likely than rural households are to own a radio (71% versus 50%), television (43% versus 2%), mobile telephone (90% versus 52%), and motor cycle/scooter (12% versus 9%). Urban households are also more likely to own a bank account or be part of a village savings and loans or osusu (51% versus 34%). In contrast, rural households are more likely than urban households are to own agricultural land (76% versus 25%), and farm animals (62% versus 37%). See Table 2.5.
2.5 HOUSEHOLD POPULATION AND COMPOSITION
Household A person or group of related or unrelated persons who live together in the same dwelling unit(s), who acknowledge one adult male or female as the head of the household, who share the same housekeeping arrangements, and who are considered a single unit.
De facto population All persons who stayed in the selected households the night before the interview (whether usual residents or visitors)
De jure population All persons who are usual residents of the selected households, whether or not they stayed in the household the night before the interview
In the 2016 SLMIS, 39,256 people stayed overnight in 6,719 households. The overall sex ratio is 92 males per 100 females. The sex ratio is 88 males per 100 females in urban areas and 95 males to 100 females in rural areas. Sixty percent of the population lives in rural areas.
Age and sex are important demographic variables and are the primary basis of demographic classification. Table 2.6 shows the distribution of the de facto household population in the 2016 SLMIS by 5-year age groups, according to sex and residence.
Figure 2.3 Household wealth by residence
3
284
31
13
24
33
12
47
2
Urban Rural
Percent distribution of de jure population by wealth quintiles
HighestFourthMiddleSecondLowest

Characteristics of Households and Women • 13
The population pyramid in Figure 2.4 shows the population distribution by sex and by 5-year age groups. The broad base of the pyramid shows that Sierra Leone’s population is young, which is typical of developing countries with a high fertility rate and low life expectancy. Almost half of the population (46%) is under age 15, 50% is age 15-64, and only 4% of the population is age 65 and older (Table 2.6).
On average, households in Sierra Leone consist of six persons (Table 2.7). Men predominantly head households in Sierra Leone (75%). The proportion of households headed by women is higher in urban areas than in rural areas (28% versus 23%).
2.6 EDUCATIONAL ATTAINMENT OF WOMEN
Studies have consistently shown that educational attainment has a strong effect on health behaviours and attitudes. Generally, the higher the level of education a woman has attained, the more knowledgeable she is about both the use of health facilities and health management for herself and for her children.
Table 2.9 shows the percent distribution of women age 15-49 by highest level of schooling attended or completed, and median years completed, according to background characteristics. The results show that over half of women age 15-49 have no education. Only 37% of women have completed primary school. Additionally, 35% of women have at least some secondary education and only 1% of women have more than secondary education.
Trends: The percentage of interviewed women with no formal education decreased from 62% in the 2013 SLMIS to 52% in the 2016 SLMIS. The percentage of women with at least some secondary education increased from 28% in 2013 to 35% in 2016.
Figure 2.4 Population pyramid
10 6 2 2 6 10
<55-9
10-1415-1920-2425-2930-3435-3940-4445-4950-5455-5960-6465-6970-7475-79
80+Age
Percent distribution of the household population
Male Female
261210

14 • Characteristics of Households and Women
Patterns by background characteristics
� Women in rural areas are less likely than are those in urban areas to have attended school (36% vs. 64%, respectively) (Figure 2.5).
� The Northern Region has the highest proportion of women with no education (60%) compared with 55% in the Eastern Region, 54% in the Southern Region, and 35% in the Western Region.
� By district, Koinadugu has the highest percentage of women with no education (69%) compared with Western Area Urban which has the lowest (28%).
� Results show that women in the lowest household wealth quintile are least likely to be educated; 72% of women in the lowest wealth quintile have no education compared with 27% of women in the highest wealth quintile.
2.7 LITERACY OF WOMEN
Literacy Respondents who have attended secondary school or higher are assumed to be literate. All other respondents were given a sentence to read, and they were considered literate if they could read all or part of the sentence. Sample: Women age 15-49
Knowing the level and distribution of literacy among the population is an important factor in the design and delivery of health messages and interventions. The results show that, overall, 40% of women age 15-49 in Sierra Leone are literate (Table 2.10).
Figure 2.5 Education of survey respondents by urban/rural residence
36
6452
11
16
1438
18
27
15
28
Urban Rural Total
Percent distribution of women age 15-49 by highest level of schooling attended or
completed
Completedsecondary orgreater
Somesecondary
Some primary/completedprimary
No education
Note: Percentages do not add to 100% due to rounding

Characteristics of Households and Women • 15
Trends: Literacy rose from 33% to 40% of interviewed women between the 2013 SLMIS and the 2016 SLMIS. All regions except for Western Region experienced increases in the percentage of literate women between the 2013 SLMIS and the 2016 SLMIS (Figure 2.6).
Patterns by background characteristics
� Sixty-four percent of women age 15-24 are literate compared with 20% of women age 45-49.
� Women in urban areas are twice as likely as are rural women to be literate (58% versus 25%).
� Women in the Western Region are most likely to be literate (63%) compared with Eastern Region in which only 31% of women are literate.
� Literacy levels vary substantially by district; 70% of women in Western Area Urban are literate, compared with only 25% of women in Koinadugu.
� The literacy rate increases with wealth, rising from 18% of women in the lowest quintile to 69% in the highest quintile.
LIST OF TABLES
For detailed information on household population and housing characteristics, see the following tables:
� Table 2.1 Household drinking water � Table 2.2 Household sanitation facilities � Table 2.3 Household characteristics � Table 2.4 Wealth quintiles � Table 2.5 Household possessions � Table 2.6 Household population by age, sex, and residence � Table 2.7 Household composition � Table 2.8 Background characteristics of respondents � Table 2.9 Educational attainment of women � Table 2.10 Literacy of women
Figure 2.6 Trends in literacy by region
20 19
31
72
3331 3237
63
40
EasternRegion
NorthernRegion
SouthernRegion
WesternRegion
National
Percentage of literate women age 15-49
2013 SLMIS 2016 SLMIS

16 • Characteristics of Households and Women
Table 2.1 Household drinking water
Percent distribution of households and de jure population by source of drinking water, time to obtain drinking water, and treatment of drinking water, according to residence, Sierra Leone MIS 2016
Households Population Characteristic Urban Rural Total Urban Rural Total
Source of drinking water Improved source 91.3 56.0 70.1 90.8 55.2 69.5
Piped into dwelling/yard plot 9.9 2.4 5.4 9.0 2.5 5.1 Piped to neighbour 9.5 1.7 4.8 8.9 1.6 4.5 Public tap/standpipe 20.0 13.7 16.2 19.8 13.4 15.9 Tube well or borehole 9.1 18.6 14.8 9.1 17.8 14.3 Protected dug well 36.6 16.8 24.7 38.0 17.0 25.5 Protected spring 1.9 1.9 1.9 2.3 2.0 2.1 Rain water 1.1 0.8 0.9 1.2 0.8 1.0 Bottled water, improved source for
cooking/washing1 0.3 0.0 0.1 0.2 0.0 0.1 Sachet water, improved source for
cooking/washing1 2.8 0.2 1.3 2.2 0.2 1.0
Unimproved source 8.7 44.0 29.9 9.2 44.8 30.5 Unprotected dug well 4.0 6.9 5.7 4.4 7.0 6.0 Unprotected spring 1.7 12.3 8.1 1.8 12.6 8.3 Tanker truck/cart with small tank 0.3 0.1 0.2 0.4 0.1 0.3 Surface water 2.2 24.7 15.7 2.5 24.9 15.9 Bottled water, unimproved source for
cooking/washing1 0.1 0.0 0.0 0.0 0.0 0.0 Sachet water, unimproved source for
cooking/washing1 0.4 0.1 0.2 0.2 0.1 0.1
Total 100.0 100.0 100.0 100.0 100.0 100.0
Time to obtain drinking water (round trip) Water on premises 39.4 12.0 23.0 39.3 12.2 23.1 Less than 30 minutes 42.2 63.3 54.9 41.5 63.0 54.4 30 minutes or longer 17.4 21.9 20.1 17.7 22.0 20.3 Don’t know/missing 1.1 2.8 2.1 1.5 2.8 2.3
Total 100.0 100.0 100.0 100.0 100.0 100.0
Number 2,688 4,031 6,719 15,837 23,700 39,538 1 Because the quality of bottled water is unknown, households using bottled water for drinking are classified as using an improved or unimproved source according to their water source for cooking and washing.

Characteristics of Households and Women • 17
Table 2.2 Household sanitation facilities
Percent distribution of households and de jure population by type and location of toilet/latrine facilities, according to residence, Sierra Leone MIS 2016
Households Population Type and location of toilet/latrine facility Urban Rural Total Urban Rural Total
Improved facility Flush/pour flush to piped sewer system 0.8 0.1 0.4 0.6 0.2 0.4 Flush/pour flush to septic tank 8.6 0.4 3.7 8.4 0.5 3.6 Flush/pour flush to pit latrine 2.6 0.1 1.1 2.6 0.1 1.1 Ventilated improved pit (VIP) latrine 1.5 0.5 0.9 1.9 0.6 1.1 Pit latrine with slab 12.9 7.1 9.4 14.5 7.8 10.5 Composting toilet 0.1 0.1 0.1 0.1 0.1 0.1 Total 26.4 8.3 15.5 28.1 9.2 16.8
Shared facility1 Flush/pour flush to piped sewer system 0.4 0.1 0.2 0.5 0.1 0.3 Flush/pour flush to septic tank 1.5 0.1 0.6 1.3 0.1 0.6 Flush/pour flush to pit latrine 3.0 0.2 1.3 2.7 0.2 1.2 Ventilated improved pit (VIP) latrine 3.2 0.9 1.8 2.7 0.9 1.6 Pit latrine with slab 42.9 21.6 30.1 41.1 20.6 28.8 Composting toilet 0.4 1.4 1.0 0.4 1.2 0.9 Total 51.4 24.3 35.1 48.7 23.1 33.3
Unimproved facility Flush/pour flush not to sewer/septic tank/
pit latrine 0.8 0.0 0.3 0.8 0.0 0.3 Pit latrine without slab/open pit 11.9 36.6 26.7 12.6 37.5 27.5 Bucket 0.9 0.2 0.5 0.8 0.2 0.4 Hanging toilet/hanging latrine 2.1 4.9 3.7 1.9 4.8 3.6 No facility/bush/field 6.5 25.8 18.1 7.0 25.3 17.9 Other 0.1 0.0 0.0 0.1 0.0 0.1 Total 22.2 67.4 49.3 23.2 67.7 49.9
Total 100.0 100.0 100.0 100.0 100.0 100.0 Number 2,688 4,031 6,719 15,837 23,700 39,538 1 Facilities that would be considered improved if they were not shared by two or more households.

18 • Characteristics of Households and Women
Table 2.3 Household characteristics
Percent distribution of households by housing characteristics, percentage using solid fuel for cooking, and percent distribution by frequency of smoking in the home, according to residence, Sierra Leone MIS 2016
Housing characteristic
Residence Total Urban Rural
Electricity Yes 46.9 2.5 20.3 No 53.1 97.5 79.7 Total 100.0 100.0 100.0
Flooring material Earth, sand 16.4 71.2 49.3 Dung 0.2 1.1 0.7 Wood/planks 3.4 0.2 1.5 Palm/bamboo 0.0 0.2 0.2 Parquet or polished wood 0.2 0.5 0.4 Vinyl or asphalt strips 1.6 0.0 0.6 Ceramic tiles 13.6 0.8 5.9 Cement 59.8 25.7 39.3 Carpet 4.7 0.1 2.0 Other 0.1 0.0 0.0 Total 100.0 100.0 100.0
Rooms used for sleeping One 32.3 20.3 25.1 Two 30.4 28.8 29.4 Three or more 37.3 50.9 45.4 Total 100.0 100.0 100.0
Cooking fuel Electricity 0.3 0.0 0.1 LPG/natural gas/biogas 0.6 0.2 0.4 Kerosene 0.1 0.0 0.0 Coal/lignite 0.2 0.0 0.1 Charcoal 63.9 4.7 28.4 Wood 33.7 94.4 70.1 No food cooked in household 1.1 0.5 0.7
Total 100.0 100.0 100.0
Percentage using solid fuel for cooking1 97.9 99.2 98.7
Number 2,688 4,031 6,719
LPG = Liquefied petroleum gas 1 Includes coal/lignite, charcoal, and wood

Characteristics of Households and Women • 19
Table 2.4 Wealth quintiles
Percent distribution of the de jure population by wealth quintiles, and the Gini Coefficient, according to residence and region, Sierra Leone MIS 2016
Wealth quintile Total
Number of persons
Gini coefficient Residence/region Lowest Second Middle Fourth Highest
Residence Urban 2.5 4.3 13.4 32.7 47.1 100.0 15,837 0.23 Rural 31.7 30.5 24.4 11.5 1.9 100.0 23,700 0.29
Region Eastern 15.4 25.2 26.9 24.0 8.5 100.0 9,432 0.28 Northern 27.1 26.7 24.2 15.2 6.8 100.0 13,764 0.23 Southern 30.9 20.2 20.4 17.7 10.8 100.0 8,683 0.34 Western 0.5 1.3 3.6 26.3 68.3 100.0 7,658 0.22
District Kailahun 21.1 30.7 33.1 14.9 0.3 100.0 3,369 0.21 Kenema 13.6 24.0 26.1 24.8 11.5 100.0 3,109 0.29 Kono 10.8 20.2 20.6 33.5 14.8 100.0 2,955 0.26 Bombali 20.7 23.3 17.7 18.2 20.1 100.0 3,177 0.31 Kambia 31.8 30.6 22.2 11.9 3.5 100.0 1,732 0.24 Koinadugu 39.7 26.5 22.6 11.1 0.2 100.0 2,247 0.22 Port Loko 22.0 23.4 28.0 22.2 4.4 100.0 3,071 0.27 Tonkolili 27.2 30.9 28.6 10.5 2.9 100.0 3,538 0.24 Bo 16.3 19.8 19.0 20.3 24.6 100.0 3,404 0.31 Bonthe 45.2 14.3 18.5 17.6 4.4 100.0 1,283 0.32 Moyamba 42.7 17.0 20.8 17.9 1.6 100.0 2,119 0.32 Pujehun 34.2 28.6 24.0 13.0 0.3 100.0 1,876 0.25 Western Area
Rural 1.2 2.9 7.6 52.1 36.3 100.0 3,346 0.23 Western Area
Urban 0.0 0.0 0.5 6.3 93.2 100.0 4,313 0.09
Total 20.0 20.0 20.0 20.0 20.0 100.0 39,538 0.30

20 • Characteristics of Households and Women
Table 2.5 Household possessions
Percentage of households possessing various household effects, means of transportation, agricultural land, and livestock/farm animals by residence, Sierra Leone MIS 2016
Residence Total Possession Urban Rural
Household effects Radio 70.9 50.1 58.4 Television 43.1 2.2 18.6 Mobile phone 89.7 52.0 67.1 Computer 10.5 0.4 4.4 Non-mobile telephone 0.5 0.1 0.3 Refrigerator 28.9 0.5 11.9
Means of transport Bicycle 9.1 6.1 7.3 Animal drawn cart 0.5 0.2 0.3 Motorcycle/scooter 11.9 9.1 10.3 Car/truck 5.2 0.5 2.4 Boat with a motor 0.6 0.7 0.7
Ownership of agricultural land 24.8 76.4 55.7
Ownership of farm animals1 36.7 61.6 51.7
Ownership of bank account/ village savings and loans/ osusu 51.2 33.7 40.7
Number 2,688 4,031 6,719 1 Cows, bulls, other cattle, horses, donkeys, goats, sheep, chickens or other poultry

Characteristics of Households and Women • 21
Table 2.6 Household population by age, sex, and residence
Percent distribution of the de facto household population by 5-year age groups, according to sex and residence, Sierra Leone MIS 2016
Urban Rural Total Age Male Female Total Male Female Total Male Female
<5 18.7 16.0 17.3 19.7 18.8 19.2 19.3 17.7 18.4 5-9 13.6 13.2 13.4 17.5 15.7 16.6 16.0 14.7 15.3 10-14 12.7 14.0 13.4 12.2 11.7 11.9 12.4 12.6 12.5 15-19 10.6 10.2 10.4 8.3 7.1 7.7 9.2 8.4 8.8 20-24 7.7 9.9 8.8 5.2 6.9 6.1 6.2 8.1 7.2 25-29 6.4 9.6 8.1 5.0 7.9 6.5 5.6 8.6 7.2 30-34 5.9 5.7 5.8 4.8 6.0 5.4 5.3 5.9 5.6 35-39 7.0 5.6 6.3 6.4 6.4 6.4 6.6 6.1 6.4 40-44 4.9 2.7 3.8 4.2 3.3 3.7 4.5 3.0 3.7 45-49 4.0 1.9 2.9 4.5 2.5 3.5 4.3 2.3 3.2 50-54 2.2 4.2 3.3 3.1 5.1 4.1 2.7 4.8 3.8 55-59 2.1 1.9 2.0 2.4 2.3 2.3 2.3 2.1 2.2 60-64 1.4 1.5 1.5 2.1 1.9 2.0 1.8 1.7 1.8 65-69 1.1 1.2 1.1 1.8 1.4 1.6 1.5 1.3 1.4 70-74 0.7 0.7 0.7 1.2 1.3 1.2 1.0 1.0 1.0 75-79 0.5 0.5 0.5 0.8 0.7 0.7 0.7 0.6 0.7 80 + 0.4 0.7 0.6 0.8 1.0 0.9 0.6 0.9 0.8 Don’t know/missing 0.2 0.1 0.1 0.1 0.1 0.1 0.1 0.1 0.1
Total 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0
Number of persons 7,361 8,381 15,743 11,450 12,063 23,513 18,812 20,444 39,256

22 • Characteristics of Households and Women
Table 2.7 Household composition
Percent distribution of households by sex of head of household and by household size; mean size of household according to residence, Sierra Leone MIS 2016
Residence Total Characteristic Urban Rural
Household headship Male 72.0 76.8 74.9 Female 28.0 23.2 25.1
Total 100.0 100.0 100.0
Number of usual members 1 4.2 2.9 3.4 2 5.5 4.1 4.7 3 9.7 10.9 10.4 4 16.4 15.1 15.6 5 16.2 17.2 16.8 6 14.3 16.0 15.3 7 10.4 10.9 10.7 8 7.2 7.9 7.6 9+ 16.1 15.0 15.4
Total 100.0 100.0 100.0 Mean size of households 5.9 5.9 5.9
Number of households 2,688 4,031 6,719
Note: Table reflects de jure household members, that is, usual residents.

Characteristics of Households and Women • 23
Table 2.8 Background characteristics of respondents
Percent distribution of women age 15-49 by selected background characteristics, Sierra Leone MIS 2016
Women Background characteristic
Weighted percent
Weighted number
Unweighted number
Age 15-19 19.6 1,665 1,646 20-24 19.5 1,658 1,600 25-29 20.1 1,705 1,669 30-34 14.3 1,218 1,235 35-39 14.2 1,208 1,242 40-44 7.2 608 627 45-49 5.2 439 482
Religion Christian 24.9 2,115 1,916 Muslim 75.0 6,373 6,570 Traditional 0.0 4 7 None 0.1 8 8
Ethnic group Krio 0.9 81 57 Mande 32.2 2,739 2,890 Temne 33.2 2,824 2,652 Madingo 3.0 254 207 Loko 2.0 166 146 Sherbro 1.4 122 174 Limba 9.9 839 791 Kissi 2.0 167 161 Kono 5.5 465 452 Susu 2.5 214 264 Fullah 3.1 264 248 Krim 0.0 2 1 Yalunka 0.4 31 49 Koranko 3.5 301 381 Vai 0.1 5 8 Other 0.3 27 20
Residence Urban 44.2 3,759 2,796 Rural 55.8 4,742 5,705
Region Eastern 22.8 1,936 1,703 Northern 33.9 2,884 3,129 Southern 20.4 1,736 2,279 Western 22.9 1,945 1,390
District Kailahun 7.9 670 526 Kenema 7.7 656 577 Kono 7.2 610 600 Bombali 8.6 732 675 Kambia 4.3 363 621 Koinadugu 5.1 434 597 Port Loko 7.3 617 540 Tonkolili 8.7 739 696 Bo 8.4 710 547 Bonthe 2.6 225 504 Moyamba 5.3 452 664 Pujehun 4.1 349 564 Western Area Rural 9.5 812 753 Western Area Urban 13.3 1,133 637
Education No education 51.7 4,393 4,779 Primary 13.8 1,173 1,197 Secondary 33.5 2,848 2,470 More than secondary 1.0 87 55
Wealth quintile Lowest 18.3 1,555 2,017 Second 18.7 1,591 1,893 Middle 18.9 1,604 1,725 Fourth 20.2 1,721 1,501 Highest 23.9 2,029 1,365
Total 15-49 100.0 8,501 8,501
Note: Education categories refer to the highest level of education attended, whether or not that level was completed. na = Not applicable

24 • Characteristics of Households and Women
Table 2.9 Educational attainment of women
Percent distribution of women age 15-49 by highest level of schooling attended or completed, and median years completed, according to background characteristics, Sierra Leone MIS 2016
Highest level of schooling
Total
Median years
completed Number of
women Background characteristic
No education
Some primary
Completed primary1
Some secondary
Completed secondary2
More than secondary
Age 15-24 25.7 14.1 3.8 44.9 10.7 0.8 100.0 6.1 3,323
15-19 15.9 17.1 4.7 55.3 6.8 0.2 100.0 6.3 1,665 20-24 35.5 11.1 2.9 34.4 14.7 1.4 100.0 5.6 1,658
25-29 58.6 11.4 2.2 20.3 6.4 1.1 100.0 - 1,705 30-34 69.8 8.6 1.7 14.7 4.1 1.2 100.0 - 1,218 35-39 74.4 9.2 1.8 10.4 2.8 1.4 100.0 - 1,208 40-44 75.9 4.9 2.9 13.3 2.4 0.6 100.0 - 608 45-49 75.3 6.0 3.4 9.8 3.9 1.6 100.0 - 439
Residence Urban 36.3 8.1 2.8 37.8 12.9 2.2 100.0 6.0 3,759 Rural 63.9 13.3 2.9 17.8 2.1 0.1 100.0 - 4,742
Region Eastern 55.1 15.0 3.6 22.7 3.4 0.1 100.0 - 1,936 Northern 59.5 11.5 2.3 22.7 3.8 0.3 100.0 - 2,884 Southern 53.6 11.8 2.7 25.2 6.3 0.4 100.0 - 1,736 Western 35.0 5.5 2.9 37.9 15.2 3.6 100.0 6.6 1,945
District Kailahun 53.0 21.7 3.2 20.4 1.3 0.3 100.0 - 670 Kenema 61.0 10.1 1.3 23.0 4.5 0.0 100.0 - 656 Kono 51.2 12.9 6.6 24.8 4.5 0.1 100.0 - 610 Bombali 49.5 8.1 2.9 32.9 6.4 0.2 100.0 0.3 732 Kambia 60.0 15.2 1.8 21.8 1.1 0.0 100.0 - 363 Koinadugu 69.4 8.1 0.9 17.4 4.2 0.0 100.0 - 434 Port Loko 59.2 18.1 1.4 19.3 2.0 0.0 100.0 - 617 Tonkolili 63.5 9.6 3.3 18.9 4.0 0.8 100.0 - 739 Bo 45.8 12.5 0.6 30.1 10.1 1.0 100.0 2.4 710 Bonthe 59.5 6.1 6.1 23.2 5.1 0.0 100.0 - 225 Moyamba 56.9 11.9 3.9 22.4 4.9 0.0 100.0 - 452 Pujehun 61.1 13.9 3.4 20.1 1.4 0.1 100.0 - 349 Western Area
Rural 44.9 5.9 3.7 35.6 7.4 2.4 100.0 4.7 812 Western Area
Urban 27.9 5.2 2.3 39.5 20.8 4.4 100.0 7.2 1,133
Wealth quintile Lowest 72.3 12.9 2.5 11.7 0.5 0.0 100.0 - 1,555 Second 63.8 15.0 3.3 16.6 1.2 0.2 100.0 - 1,591 Middle 55.2 13.9 3.2 24.0 3.6 0.1 100.0 - 1,604 Fourth 47.4 8.4 2.2 33.5 8.3 0.3 100.0 2.5 1,721 Highest 27.3 6.3 2.9 42.2 17.5 3.8 100.0 7.0 2,029
Total 51.7 11.0 2.8 26.7 6.8 1.0 100.0 - 8,501 1 Completed grade 6 at the primary level 2 Completed grade 6 or 7 at the secondary level

Characteristics of Households and Women • 25
Table 2.10 Literacy of women
Percent distribution of women age 15-49 by level of schooling attended and level of literacy, and percentage literate, according to background characteristics, Sierra Leone MIS 2016
Secondary school or
higher
No schooling or primary school
Total Percentage
literate1 Number of
women Background characteristic
Can read a whole
sentence
Can read part of a sentence
Cannot read at all
No card with required language
Blind/ visually
impaired
Age 15-24 56.4 1.8 5.2 36.5 0.0 0.0 100.0 63.5 3,323
15-19 62.3 3.3 6.4 28.0 0.0 0.0 100.0 72.0 1,665 20-24 50.5 0.3 4.0 45.1 0.0 0.0 100.0 54.9 1,658
25-29 27.8 0.1 4.2 67.9 0.0 0.0 100.0 32.1 1,705 30-34 19.9 0.0 4.3 75.6 0.1 0.0 100.0 24.3 1,218 35-39 14.6 0.1 3.8 81.4 0.1 0.0 100.0 18.5 1,208 40-44 16.3 0.4 3.2 79.8 0.3 0.0 100.0 19.9 608 45-49 15.3 0.0 4.9 79.7 0.0 0.2 100.0 20.2 439
Residence Urban 52.9 0.9 4.4 41.9 0.0 0.0 100.0 58.1 3,759 Rural 20.0 0.7 4.6 74.6 0.1 0.0 100.0 25.3 4,742
Region Eastern 26.2 0.7 3.8 69.0 0.2 0.0 100.0 30.8 1,936 Northern 26.8 0.9 4.6 67.7 0.0 0.0 100.0 32.3 2,884 Southern 31.9 0.8 4.3 63.0 0.0 0.0 100.0 37.0 1,736 Western 56.6 0.6 5.3 37.5 0.0 0.0 100.0 62.5 1,945
District Kailahun 22.1 0.9 5.2 71.3 0.5 0.0 100.0 28.2 670 Kenema 27.5 0.9 3.8 67.8 0.0 0.0 100.0 32.2 656 Kono 29.3 0.4 2.4 67.8 0.0 0.0 100.0 32.2 610 Bombali 39.5 0.8 5.4 54.3 0.0 0.0 100.0 45.7 732 Kambia 22.9 0.6 5.0 71.6 0.0 0.0 100.0 28.4 363 Koinadugu 21.6 1.0 2.4 75.0 0.0 0.0 100.0 25.0 434 Port Loko 21.2 0.5 5.3 72.9 0.0 0.1 100.0 27.0 617 Tonkolili 23.7 1.5 4.4 70.4 0.1 0.0 100.0 29.5 739 Bo 41.1 0.5 2.3 56.1 0.0 0.0 100.0 43.9 710 Bonthe 28.3 0.2 6.9 64.6 0.0 0.0 100.0 35.4 225 Moyamba 27.3 1.6 6.3 64.8 0.0 0.0 100.0 35.2 452 Pujehun 21.6 0.7 4.0 73.6 0.0 0.0 100.0 26.4 349 Western Area
Rural 45.4 1.2 4.9 48.4 0.0 0.0 100.0 51.6 812 Western Area
Urban 64.7 0.2 5.5 29.6 0.0 0.0 100.0 70.4 1,133
Wealth quintile Lowest 12.3 0.5 5.2 82.0 0.0 0.0 100.0 18.0 1,555 Second 18.0 1.2 5.5 75.2 0.2 0.0 100.0 24.6 1,591 Middle 27.7 0.9 4.0 67.4 0.0 0.0 100.0 32.5 1,604 Fourth 42.1 0.8 2.6 54.4 0.0 0.0 100.0 45.5 1,721 Highest 63.5 0.6 5.3 30.6 0.0 0.0 100.0 69.4 2,029
Total 34.5 0.8 4.5 60.1 0.1 0.0 100.0 39.8 8,501 1 Refers to women who attended secondary school or higher and women who can read a whole sentence or part of a sentence


Malaria Prevention • 27
MALARIA PREVENTION 3
Key Findings
Ownership of Insecticide-Treated Nets (ITNs):
x More than half (60%) of households in Sierra Leone own at least one ITN.
x Sixteen percent of households had at least one ITN for every two people.
Sources of ITNs:
x About three-quarters of ITNs owned by households were obtained from mass campaigns, 11% from antenatal care visits, and 5% each from routine immunisation visits and from shops or markets.
Access to an ITN:
x Nearly 4 in 10 people (37%) have access to an ITN. This means 37% of Sierra Leoneans could sleep under an ITN if every ITN in a household were used by two people.
Use of ITNs:
x Thirty-nine percent of the household population, 4% of children under 5, and 44% of pregnant women slept under an ITN the night before the survey.
x In households owning at least one ITN, 63% of the household population, 71% of children under 5, and 75% of pregnant women slept under an ITN the previous night.
x Use of ITNs is high among those with access. Eighty-nine percent of ITNs owned by households were used the night before the survey.
Intermittent Preventive Therapy (IPTp):
x Seventy-one percent of pregnant women received at least two doses, and 31% received at least three doses, of SP/Fansidar for prevention of malaria in pregnancy.
his chapter describes the population coverage rates of some of the key malaria control interventions in Sierra Leone, including the ownership and use of insecticide-treated nets (ITNs) and intermittent preventive treatment in pregnancy (IPTp). Malaria control efforts focus on scaling-up these
interventions.
The Sierra Leone Malaria Control Strategic Plan 2016-2020 envisages universal coverage of the population with ITNs through routine distribution and mass campaigns in order to reduce the burden of malaria (MoHS 2015a). ITNs are routinely distributed free of charge to children less than age one on successful completion of Penta 3 immunisation (third dose of a vaccine against diphtheria, pertussis,
T

28 • Malaria Prevention
tetanus, Haemophilus influenzae type b, and hepatitis B) and to pregnant women during the first antenatal care visit.
3.1 OWNERSHIP OF INSECTICIDE-TREATED NETS
Ownership of insecticide-treated nets Households that have at least one insecticide-treated net (ITN). An ITN is defined as: (1) a factory-treated net that does not require any further treatment (long-lasting insecticidal net or LLIN) or (2) a net that has been soaked with insecticide within the past 12 months. Sample: Households
Full household ITN coverage Percentage of households with at least one ITN for every two people. Sample: Households
It is well understood that proper use of ITNs protects households and the entire local community from malaria. The distribution and use of ITNs is one of the central interventions for preventing malaria infection in Sierra Leone. The National Malaria Control Programme Strategic Plan 2016-2020 prioritises increasing ITN ownership with at least one ITN from the 2013 baseline of 62% to 100% by the year 2020 (MoHS 2015a).
In addition to reaching all households across the country with ITN distribution, the national strategy aims to provide enough ITNs to cover all household residents. This indicator is operationalised as one ITN for every two household members.
The 2016 SLMIS revealed that 60% of households in Sierra Leone own at least one insecticide-treated net (ITN). Only 16% of households have one net for every two people who stayed in the household the night prior to the survey. Thus to meet strategic goals the scope of distribution needs to expand to reach the 40% of households who do not own any ITNs. In addition, the quantity of ITNs distributed needs to increase to provide sufficient ITNs for the 44% of households that own at least one ITN but have an insufficient supply for the number of household residents (Figure 3.1; Table 3.1).
Figure 3.1 Household ownership of ITNs
No ITN40%
At least 1 ITN, but not enough
for all HH members
44%
At least 1 ITN for every 2
people in the HH
16%
Percent distribution of households

Malaria Prevention • 29
Trends: Ownership of ITNs increased from 37% in the 2008 SLDHS to 62% in the 2013 SLMIS and remained at similar levels in 2016 (60%) (Figure 3.2). The percentage of households with enough ITNs to cover the full household population increased from 7% in the 2008 SLDHS to 17% in the 2013 SLMIS and remained at similar levels in 2016 (16%).
Patterns by background characteristics
Rural households are slightly more likely to own at least one ITN (65%) than urban households (54%). ITN ownership is lower in the Western Region (40%) than in the Eastern, Northern, and Southern regions (70%, 57%, and 70% respectively). A similar regional pattern appears in the percentage of households owning at least one ITN for every two persons (7% in the Western Region compared with 21%, 12%, and 25% in the Eastern, Northern and Southern regions, respectively).
Although no particular or unique pattern was observed on household possession of ITNs by wealth status; 49% of the households in the highest wealth quintile owned at least ITN, compared with 58% of the households in the lowest wealth quintile.
Household ownership of at least one ITN is highest in Bo, Kenema, and Kailahun (76%) districts. Western Area Rural and Western Area Urban were found had the lowest ITN ownership, 42% and 40%, respectively (Figure 3.3).
Figure 3.2 Trends in ITN ownership
Figure 3.3 ITN ownership by district
37
62 60
SLDHS 2008 SLMIS 2013 SLMIS 2016
Percentage of households owning at least one insecticide-treated net (ITN)

30 • Malaria Prevention
3.1.1 Sources of ITNs
The majority of ITNs owned by households (74%) were obtained from mass distribution campaigns. Eleven percent of ITNs came from routine ANC visits and 5% through the immunisation programme. An additional 5% of ITNs were obtained from shops or markets (Figure 3.4 and Table 3.2).
3.1.2 Mosquito net preferences
Preferences for various social marketing goods significantly affect the consistent use of products. In this regard, the 2016 SLMIS assessed respondents’ preferences for shape, colour, and material of mosquito nets (Table 3.3). Most respondents (54%) prefer conical, 44% prefer rectangular, and 2% did not have a clear preference. Sixty-six percent of respondents prefer the nets with blue colour, 25% prefer white, and 7% prefer green nets. Eighty percent of respondents preferred a soft net material, while 20% preferred a hard material.
Trends: Preferences have changed from the 2013 SLMIS, in which 33% preferred conical and 55% preferred rectangular.
3.2 HOUSEHOLD ACCESS AND USE OF ITNS
Access to an ITN Percentage of the population that could sleep under an ITN if each ITN in the household were used by up to two people. Sample: De facto household population
Use of ITNs Percentage of population that slept under an ITN the night before the survey. Sample: De facto household population
ITNs act as both a physical and a chemical barrier against mosquitoes. By reducing the vector population, ITNs may help to reduce malaria risk at the community level as well as to individuals who use them.
Access to an ITN is measured by the proportion of the population that could sleep under an ITN if each ITN in the household were used by up to two people. Comparing ITN access and ITN use indicators can help programmes identify if there is a behavioural gap in which available ITNs are not being used. If the difference between these indicators is substantial, the programme may need to focus on behaviour change and how to identify the main drivers or barriers to ITN use to design an appropriate intervention. This analysis helps ITN programmes determine whether they need to achieve higher ITN coverage, promote ITN use, or both.
Figure 3.4 Sources of ITNs
National distribution
73%
ANC distribution
11%
EPI distribution
5%
Shop/market5%
Other6%
Percent distribution of households

Malaria Prevention • 31
The majority of Sierra Leoneans (63%) do not have access to an ITN. Overall, only 37% of the population have access to an ITN (37% could sleep under an ITN if each ITN in the household were used by up to two people) (Table 3.4). Thirty-nine percent of the population reported using an ITN the night before the survey (Table 3.5). Comparing these two population-level indicators, it is evident that the proportion of the population using ITNs is similar to the proportion with access to an ITN (39% and 37%, respectively); there is no gap between ITN access and ITN use at the population level (Figure 3.5). ITN use is very high among those with access.
Table 3.6 shows that 89% of the ITNs owned by households were used the night before the survey. In short, although encouraging ITN use behaviours is always desirable, the data show that achieving the strategic goal of universal coverage in Sierra Leone will require emphasis on improving ITN distribution.
Trends: The proportion of the household population with access to an ITN and the proportion using an ITN the night before the survey increased from 19% for both indicators in the 2008 SLDHS to 37% and 39%, respectively, in the 2013 SLMIS. No additional change occurred between the 2013 SLMIS and the 2016 SLMIS (Figure 3.6). The levels of ITN use are as high as the levels of ITN access revealing that when nets are available they are being used; this trend has continued across all surveys.
Figure 3.5 Access to and use of ITNs
Figure 3.6 Trends in ITN access and use
3241 37
31
44 39
Urban Rural Total
Percentage of the household population with access to an ITN and who slept under
an ITN the night before the survey, by residence
Access to an ITN Slept under an ITN
19
37 37
19
39 39
2008 SLDHS 2013 SLMIS 2016 SLMIS
Percentage of the household population that have access to an ITN and
percentage of the population that slept under an ITN the night before the survey
Slept under ITNAccess to ITN

32 • Malaria Prevention
Patterns by background characteristics
� ITN access is higher in the household population in rural areas compared with the population in urban areas (41% and 32%, respectively) and is highest in Bo district (53%) and lowest in Western Area Rural (21%).
� ITN utilisation is higher in household populations in rural compared with urban areas (44% and 31%, respectively). ITN utilisation is highest in household populations in Bo (56%) and Kenema (55%) and lowest in Western Area Rural (21%) and Western Area Urban (19%) (Figure 3.7).
� In households owning at least one ITN, populations were most likely to use an ITN in Moyamba (74%) and least likely to use an ITN in Western Area Urban (42%) (Figure 3.8).
Figure 3.7 ITN use by household population
Figure 3.8 ITN use by household population in households owning ITNs

Malaria Prevention • 33
3.3 USE OF ITNS BY CHILDREN AND PREGNANT WOMEN
Malaria is endemic in Sierra Leone with transmission occurring year-round. Natural immunity to the disease is acquired over time for those living in high malaria transmission areas (Doolan et al. 2009). Children under 5 are prone to severe malaria infection due to lack of acquired immunity. For about 6 months following birth, antibodies acquired from the mother during pregnancy protect the child, but this maternal immunity is gradually lost when the child starts to develop his/her own immunity to malaria. Age is an important factor in determining levels of acquired immunity to malaria as acquired immunity does not prevent infection but rather protects against severe disease and death. The pace at which immunity develops depends on the exposure to malarial infection, and in high malaria-endemic areas, children are thought to attain a high level of immunity by their fifth birthday. Such children may experience episodes of malaria illness but usually do not suffer from the severe, life-threatening conditions.
Malaria transmission in Sierra Leone is stable and adults usually acquire some degree of immunity; however, pregnancy suppresses immunity and women in their first pregnancies are at increased risk for severe malaria. Malaria in pregnancy is frequently associated with the development of anaemia, which interferes with the maternal-foetus exchange and can lead to low-birth-weight infants, placental parasitaemia, foetal death, abortion, stillbirth, and prematurity (Shulman and Dorman 2003).
As stated in the Sierra Leone National Strategic Plan 2016-2020, all children under 5 and all pregnant women should sleep under an ITN or LLIN every night to prevent malaria complications. ITNs are distributed free to all pregnant women during their first antenatal visit, to children 12-59 months upon completion of Penta 3 immunisation and to the entire population during mass campaigns (MoHS 2015a).
Table 3.7 and Table 3.8 show the percentage of children under age 5 and the percentage of pregnant women who slept under an ITN the night before the survey. Overall, 44% of children in Sierra Leone under age 5 and 44% of pregnant women slept under an ITN the previous night.
Not surprisingly, ITN use is higher among children and pregnant women that slept in households that own at least one ITN than among children and pregnant women in all households, as 40% of all households do not own an ITN. In households with at least one ITN, 71% of children under 5 and 75% of pregnant women slept under an ITN the night before the survey (Table 3.7 and Table 3.8).
Trends: Net use increased from 26% to 45% among children under age 5 and from 27% to 47% in pregnant women between the 2008 SLDHS and 2013 SLMIS. Between the 2013 SLMIS and the 2016 SLMIS, levels of ITN use in these populations remained steady (44% ITN use in both children and pregnant women) (Figure 3.9).
Patterns by background characteristics
� ITN use among children under 5 decreases with age. Forty-eight percent of children less than 12 months slept under an ITN the night before the survey, compared with 41% of children age 48-59 months.
� Children in rural areas are more likely than children in urban areas to use ITNs (48% and 38%, respectively). The same pattern is seen in ITN use by pregnant women (53% and 31% for rural and urban, respectively).
Figure 3.9 ITN use by children and pregnant women
2645
44
27
4744
2008 SLDHS 2013 SLMIS 2016 SLMIS
Percentage of children and pregnant women using an ITN the night before the
survey
Pregnant women
Children under 5

34 • Malaria Prevention
� ITN use is highest in children living in the Southern (56%) and Eastern (59%) regions compared with the Northern Region (40%) and Western Region (26%). A similar pattern in ITN use among pregnant women is evident with the highest use in Southern and Eastern regions (61% and 51%) followed by Northern Region (45%) and Western Region (19%).
� By district, ITN use ranges from 26% in Western Area Urban and Western Area Rural to 66% in Kenema for children under 5 (Figure 3.10) and 13% in Western Area Urban to 72% in Kenema for pregnant women.
3.4 MALARIA IN PREGNANCY
Intermittent preventive treatment (IPTp) during pregnancy (IPTp2+) Percentage of women who took at least two doses of SP/Fansidar with at least one dose received during an antenatal care visit during their last pregnancy. Sample: Women age 15-49 with a live birth in the 2 years before the survey
Intermittent preventive treatment (IPTp) during pregnancy (IPTp3+) Percentage of women who took at least three doses of SP/Fansidar with at least one dose received during an antenatal care visit during their last pregnancy. Sample: Women age 15-49 with a live birth in the 2 years before the survey
Malaria infection during pregnancy is a major public health problem in Sierra Leone, with substantial risks for the mother, her foetus, and the neonate. Intermittent preventive treatment of malaria in pregnancy (IPTp) is a full therapeutic course of antimalarial medicine given to pregnant women at routine antenatal care visits to prevent malaria. IPTp helps prevent maternal malaria episodes, maternal and foetal anaemia, placental parasitaemia, low birth weight, and neonatal mortality.
The World Health Organization (WHO) recommends a three-pronged approach for reducing the negative health effects associated with malaria in pregnancy (MIP): prompt diagnosis and treatment of confirmed infection, use of long-lasting insecticidal nets (LLINs), and IPTp (WHO 2004).
Sulfadoxine-pyrimethamine (SP), also known as Fansidar, is the recommended drug for IPTp in Sierra Leone. For over 10 years, the Ministry of Health and Sanitation (MOHS) has been implementing IPTp, defined as provision of at least two doses of sulfadoxine-pyrimethamine (SP)/Fansidar to protect the mother and her child from malaria during routine antenatal care visits in the second and third trimesters of pregnancy (IPTp2+). In 2016 the National Malaria Control Programme adopted the 2012 WHO recommendation to administer one dose of SP/Fansidar at each antenatal care (ANC) visit after the first trimester, with at least 1 month between doses (WHO 2012a; WHO 2012b). The household survey indicator used to measure coverage of this intervention is the percentage of women with a live birth in the
Figure 3.10 ITN use by children under 5

Malaria Prevention • 35
2 years preceding the survey who received three or more doses of SP/Fansidar to prevent malaria during her most recent pregnancy (IPTp3+).
Ninety percent of women with a live birth in the 2, years preceding the survey received one or more doses of SP/Fansidar during an ANC visit to prevent malaria. Seventy-one percent of these women received two or more doses of SP/Fansidar, at least one during an ANC visit, and 31% received three or more doses of SP/Fansidar, at least one during an ANC visit (Table 3.9).
Trends: The percentage of women receiving IPTp1+ has increased from 17% in the 2008 SLDHS to 79% in the 2013 SLMIS to 90% in the current survey. The proportion of women receiving two or more doses of SP/Fansidar for IPTp has increased from 10% in the 2008 SLDHS to 62% in the 2013 SLMIS and 71% in the 2016 SLMIS. IPTp3+ was 31% in the 2016 SLMIS which is the baseline for this indicator from which to measure future progress (Figure 3.11).
Patterns by background characteristics
� The use of IPTp2+ is lower in urban than in rural areas. Seventy-six percent of women in rural areas received at least two doses of SP/Fansidar, compared with only 64% of women in urban areas.
� IPTp2+ coverage decreases with increasing wealth quintile; 76% of women in the lowest wealth quintile received at least two doses of IPTp, compared with 58% of women in the highest wealth quintile.
� With respect to region of residence, IPTp2+ coverage was similarly high in Eastern, Northern and Southern regions (73%, 76%, 73%, respectively) but was much lower (60%) in the Western Region.
� IPTp2+ coverage ranged from 51% in Western Area Urban to 87% in Kambia.
LIST OF TABLES
For detailed information on malaria, see the following tables:
� Table 3.1 Household possession of mosquito nets � Table 3.2 Source of mosquito nets � Table 3.3 Preferences of mosquito nets � Table 3.4 Access to an insecticide-treated net (ITN) � Table 3.5 Use of mosquito nets by persons in the household � Table 3.6 Use of existing ITNs � Table 3.7 Use of mosquito nets by children � Table 3.8 Use of mosquito nets by pregnant woman � Table 3.9 Use of Intermittent Preventive Treatment (IPTp) by women during pregnancy
Figure 3.11 Trends in IPTp use by pregnant women
17
7990
10
6271
31
2008 SLDHS 2013 SLMIS 2016 SLMIS
Percentage of women with a live birth in the 2 years before the survey who received at least 1, 2, or 3 doses of
SP/Fansidar with at least one during an ANC visit
IPTp2+
IPTp1+
IPTp3+

36 • Malaria Prevention
Table 3.1 Household possession of mosquito nets
Percentage of households with at least one mosquito net (treated or untreated), insecticide-treated net (ITN), and long-lasting insecticidal net (LLIN); average number of nets, ITNs, and LLINs per household; and percentage of households with at least one net, ITN, and LLIN per two persons who stayed in the household last night, by background characteristics, Sierra Leone MIS 2016
Percentage of households with at
least one mosquito net Average number of nets per
household
Number of households
Percentage of households with at least one net for every two persons who stayed in the household last
night
Number of households
with at least one person
who stayed in the
household last night
Background characteristic
Any mosquito
net
Insecticide- treated
mosquito net (ITN)1
Long- lasting
insecticidal net (LLIN)
Any mosquito
net
Insecticide- treated
mosquito net (ITN)1
Long- lasting
insecticidal net (LLIN)
Any mosquito
net
Insecticide- treated
mosquito net (ITN)1
Long- lasting
insecticidal net (LLIN)
Residence Urban 54.5 53.7 53.7 1.0 1.0 1.0 2,688 11.4 11.1 11.1 2,687 Rural 66.0 64.8 64.7 1.3 1.3 1.3 4,031 20.0 19.6 19.6 4,031
Region Eastern 71.9 70.5 70.5 1.4 1.3 1.3 1,663 21.8 21.3 21.3 1,663 Northern 59.5 57.5 57.5 1.2 1.1 1.1 2,230 13.0 12.3 12.3 2,230 Southern 70.5 70.4 70.3 1.5 1.5 1.5 1,496 25.1 25.0 25.0 1,496 Western 41.0 41.0 41.0 0.6 0.6 0.6 1,330 6.5 6.5 6.5 1,329
District Kailahun 77.0 75.8 75.8 1.4 1.4 1.4 620 24.3 24.0 24.0 620 Kenema 76.0 75.8 75.8 1.5 1.4 1.4 558 26.9 26.7 26.7 558 Kono 60.8 57.8 57.8 1.1 1.1 1.1 485 12.7 11.6 11.6 485 Bombali 53.7 53.7 53.7 1.1 1.1 1.1 531 15.0 14.7 14.7 531 Kambia 68.8 67.6 67.6 1.4 1.4 1.4 273 14.1 14.0 14.0 273 Koinadugu 61.9 61.9 61.9 1.1 1.1 1.1 350 6.9 6.9 6.9 350 Port Loko 53.6 51.1 51.1 0.9 0.9 0.9 556 15.1 13.9 13.9 556 Tonkolili 65.2 60.1 60.1 1.4 1.3 1.3 520 12.3 11.1 11.1 520 Bo 76.4 76.4 76.4 1.6 1.6 1.6 631 27.2 27.2 27.2 631 Bonthe 72.8 72.7 72.7 1.6 1.6 1.6 216 31.0 31.0 31.0 216 Moyamba 60.8 60.8 60.8 1.4 1.4 1.4 340 19.4 19.4 19.4 339 Pujehun 67.4 67.2 66.5 1.4 1.4 1.4 310 22.7 22.6 22.5 310 Western Area
Rural 42.0 42.0 42.0 0.7 0.7 0.7 495 3.7 3.7 3.7 495 Western Area
Urban 40.4 40.4 40.4 0.6 0.6 0.6 835 8.1 8.1 8.1 834
Wealth quintile Lowest 59.5 57.8 57.7 1.1 1.0 1.0 1,432 15.9 15.3 15.3 1,432 Second 68.6 67.9 67.9 1.3 1.3 1.3 1,338 20.7 20.5 20.5 1,338 Middle 70.7 69.7 69.6 1.5 1.5 1.5 1,244 19.6 19.4 19.4 1,244 Fourth 60.8 59.4 59.4 1.2 1.2 1.2 1,266 14.7 14.0 14.0 1,266 Highest 48.9 48.6 48.6 0.9 0.9 0.9 1,440 12.4 12.2 12.2 1,439
Total 61.4 60.3 60.3 1.2 1.2 1.2 6,719 16.6 16.2 16.2 6,718 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months.

Mal
aria
Pre
vent
ion
• 3
7
Tabl
e 3.
2 S
ourc
e of
mos
quito
net
s
Per
cent
dis
tribu
tion
of m
osqu
ito n
ets
by s
ourc
e of
net
, acc
ordi
ng to
bac
kgro
und
char
acte
ristic
s, S
ierr
a Le
one
MIS
201
6
Bac
kgro
und
char
acte
ristic
Mas
s di
strib
u-tio
n ca
mpa
ign
AN
C v
isit
Imm
uni-
satio
n vi
sit
Gov
ern-
men
t ho
spita
l/ he
alth
ce
ntre
M
obile
cl
inic
Com
-m
unity
he
alth
w
orke
r
Priv
ate
hosp
ital/
clin
ic
Mis
sion
/ fa
ith-
base
d ho
spita
l
Mis
sion
/ fa
ith-
base
d cl
inic
PV
T m
obile
cl
inic
N
GO
P
harm
acy
Sho
p/
mar
ket
Sch
ool
Oth
er
Don
’t kn
ow/
mis
sing
To
tal
Num
ber
of
mos
quito
ne
ts
Type
of n
et
ITN
1 73
.6
10.6
4.
7 2.
0 0.
2 1.
1 0.
1 0.
0 0.
0 0.
0 0.
9 0.
2 4.
8 0.
2 1.
6 0.
0 10
0.0
7,79
9 O
ther
2 34
.7
11.7
5.
7 10
.9
0.0
0.3
0.8
0.0
0.0
0.0
0.0
0.0
26.4
0.
0 9.
5 0.
0 10
0.0
135
Res
iden
ce
Urb
an
64.3
10
.2
4.6
3.5
0.2
1.7
0.2
0.1
0.1
0.0
1.7
0.4
9.6
0.4
3.0
0.1
100.
0 2,
648
Rur
al
77.2
10
.8
4.8
1.5
0.1
0.7
0.1
0.0
0.0
0.0
0.4
0.1
3.0
0.1
1.1
0.0
100.
0 5,
287
Reg
ion
Eas
tern
64
.4
14.1
7.
0 3.
4 0.
1 1.
5 0.
1 0.
2 0.
0 0.
1 1.
4 0.
1 4.
7 0.
2 2.
5 0.
1 10
0.0
2,26
1 N
orth
ern
75
.9
11.6
4.
4 1.
2 0.
2 0.
2 0.
1 0.
0 0.
0 0.
0 1.
1 0.
0 3.
4 0.
0 1.
7 0.
0 10
0.0
2,57
8 S
outh
ern
83
.2
6.7
3.3
0.7
0.2
1.2
0.0
0.0
0.0
0.0
0.1
0.4
3.2
0.4
0.7
0.0
100.
0 2,
231
Wes
tern
59
.9
8.8
3.5
5.2
0.0
2.0
0.2
0.0
0.2
0.0
0.7
0.2
16.8
0.
0 2.
6 0.
0 10
0.0
864
Dis
tric
t
K
aila
hun
61.9
11
.2
5.5
7.7
0.3
3.0
0.3
0.1
0.1
0.1
3.5
0.0
3.2
0.0
3.1
0.0
100.
0 89
7 K
enem
a 69
.3
15.0
11
.1
0.6
0.0
0.4
0.0
0.3
0.0
0.0
0.0
0.2
2.2
0.2
0.5
0.2
100.
0 81
7 K
ono
61.2
17
.6
3.5
0.8
0.0
0.6
0.0
0.0
0.0
0.0
0.3
0.1
10.6
0.
7 4.
5 0.
0 10
0.0
547
Bom
bali
80.2
13
.5
0.4
0.4
0.0
0.2
0.0
0.0
0.0
0.0
1.0
0.0
2.7
0.0
1.6
0.0
100.
0 57
2 K
ambi
a 84
.0
8.0
5.2
0.1
0.0
0.3
0.0
0.0
0.0
0.0
0.0
0.0
2.2
0.0
0.2
0.0
100.
0 37
5 K
oina
dugu
76
.9
5.8
8.7
1.5
0.0
0.8
0.0
0.0
0.0
0.3
5.0
0.0
0.7
0.0
0.2
0.0
100.
0 39
0 P
ort L
oko
66.8
15
.3
2.8
1.8
0.0
0.0
0.0
0.0
0.0
0.0
0.4
0.0
10.3
0.
0 2.
7 0.
0 10
0.0
526
Tonk
olili
74.3
12
.3
6.1
2.0
0.7
0.0
0.5
0.0
0.0
0.0
0.0
0.1
1.2
0.0
2.6
0.2
100.
0 71
5 B
o 80
.8
5.5
1.6
1.4
0.4
1.8
0.0
0.0
0.0
0.0
0.1
1.0
5.6
0.8
1.1
0.0
100.
0 98
1 B
onth
e 95
.0
1.7
1.0
0.7
0.0
0.9
0.0
0.0
0.0
0.0
0.0
0.0
0.3
0.0
0.5
0.0
100.
0 35
3 M
oyam
ba
79.9
11
.9
6.5
0.0
0.0
0.2
0.0
0.0
0.0
0.0
0.0
0.0
0.7
0.1
0.7
0.0
100.
0 46
8 P
ujeh
un
82.6
8.
1 5.
7 0.
0 0.
0 1.
0 0.
0 0.
0 0.
0 0.
0 0.
0 0.
0 2.
6 0.
0 0.
0 0.
0 10
0.0
429
Wes
tern
Are
a R
ural
44
.2
16.8
3.
8 2.
7 0.
0 2.
4 0.
0 0.
0 0.
0 0.
0 0.
4 0.
0 27
.3
0.0
2.4
0.0
100.
0 35
4 W
este
rn A
rea
Urb
an
70.7
3.
2 3.
2 6.
9 0.
0 1.
8 0.
4 0.
0 0.
3 0.
0 0.
9 0.
4 9.
4 0.
0 2.
7 0.
0 10
0.0
510
Wea
lth q
uint
ile
Low
est
76.6
11
.2
5.6
1.8
0.1
0.7
0.0
0.0
0.0
0.1
0.3
0.0
2.1
0.1
1.3
0.1
100.
0 1,
530
Sec
ond
75.2
13
.3
4.2
1.8
0.2
0.7
0.1
0.0
0.1
0.0
0.5
0.0
2.8
0.0
1.2
0.0
100.
0 1,
751
Mid
dle
74.5
11
.4
5.7
1.5
0.1
1.1
0.2
0.2
0.0
0.1
1.5
0.0
1.9
0.0
1.9
0.0
100.
0 1,
893
Four
th
72.8
9.
7 4.
2 2.
6 0.
1 1.
0 0.
0 0.
0 0.
0 0.
0 0.
9 0.
2 6.
5 0.
0 1.
9 0.
1 10
0.0
1,51
7 H
ighe
st
63.1
6.
2 3.
8 3.
5 0.
3 1.
9 0.
2 0.
0 0.
1 0.
0 0.
9 0.
8 15
.6
1.0
2.6
0.0
100.
0 1,
244
Tota
l 72
.9
10.6
4.
7 2.
2 0.
1 1.
0 0.
1 0.
0 0.
0 0.
0 0.
8 0.
2 5.
2 0.
2 1.
7 0.
0 10
0.0
7,93
5 A
NC
= A
nten
atal
car
e 1 A
n in
sect
icid
e-tre
ated
net
(ITN
) is
(1) a
fact
ory-
treat
ed n
et th
at d
oes
not r
equi
re a
ny fu
rther
trea
tmen
t (LL
IN) o
r (2)
a n
et th
at h
as b
een
soak
ed w
ith in
sect
icid
e w
ithin
the
past
12
mon
ths.
2 A
ny n
et th
at is
not
an
ITN

38 • Malaria Prevention
Table 3.3 Preferences of mosquito net
Percent distribution of household by preferred shape of mosquito net, by preferred colour of mosquito net and by preferred hardness of mosquito material, according to background characteristics, Sierra Leone MIS 2016
Preferred shape
Total
Preferred colour
Total
Preferred hardness of net material
Total Number Background characteristic Conical
Rect-angular Either
Don’t know White Blue Green Other
Soft (poly-ester)
Hard (poly-ethyl-ene)
Don’t know
Residence Urban 65.1 33.5 1.4 0.1 100.0 31.0 62.7 4.5 1.8 100.0 84.8 14.8 0.4 100.0 2,688 Rural 46.6 51.2 2.3 0.0 100.0 21.7 67.7 7.9 2.7 100.0 77.1 22.8 0.1 100.0 4,031
Region Eastern 55.9 42.1 2.0 0.0 100.0 27.0 64.4 6.2 2.4 100.0 70.7 29.3 0.0 100.0 1,663 Northern 43.0 54.2 2.8 0.0 100.0 23.3 66.5 6.5 3.7 100.0 77.1 22.8 0.2 100.0 2,230 Southern 55.9 43.1 1.1 0.0 100.0 18.7 69.9 10.2 1.3 100.0 88.7 11.2 0.1 100.0 1,496 Western 67.8 30.8 1.2 0.2 100.0 34.5 61.5 2.9 1.1 100.0 87.7 11.7 0.6 100.0 1,330
District Kailahun 55.2 42.7 2.1 0.0 100.0 25.3 62.1 8.4 4.2 100.0 57.1 42.9 0.0 100.0 620 Kenema 49.4 48.8 1.8 0.0 100.0 22.7 69.7 7.1 0.6 100.0 76.0 24.0 0.0 100.0 558 Kono 64.4 33.5 2.1 0.0 100.0 34.3 61.2 2.4 2.0 100.0 82.0 18.0 0.0 100.0 485 Bombali 48.1 51.0 1.0 0.0 100.0 19.8 72.8 6.9 0.5 100.0 83.3 16.7 0.0 100.0 531 Kambia 32.7 63.6 3.6 0.0 100.0 32.3 60.7 4.7 2.3 100.0 79.5 19.6 0.9 100.0 273 Koinadugu 60.9 38.9 0.2 0.0 100.0 13.2 77.1 2.4 7.3 100.0 65.4 34.6 0.0 100.0 350 Port Loko 29.7 68.1 2.2 0.0 100.0 25.3 67.0 6.1 1.6 100.0 68.5 31.5 0.0 100.0 556 Tonkolili 45.4 47.9 6.7 0.0 100.0 26.9 55.4 10.1 7.7 100.0 86.6 13.2 0.2 100.0 520 Bo 68.4 30.0 1.6 0.0 100.0 17.7 71.6 8.3 2.4 100.0 90.1 9.7 0.2 100.0 631 Bonthe 47.1 51.3 1.6 0.1 100.0 21.2 65.9 12.1 0.8 100.0 89.8 9.9 0.3 100.0 216 Moyamba 37.9 62.1 0.0 0.0 100.0 19.5 68.4 11.9 0.2 100.0 80.9 19.1 0.0 100.0 340 Pujehun 56.2 43.0 0.8 0.0 100.0 18.1 70.6 10.6 0.7 100.0 93.6 6.4 0.0 100.0 310 Western Area
Rural 69.0 29.4 1.0 0.5 100.0 26.0 70.5 2.1 1.4 100.0 88.5 10.8 0.8 100.0 495 Western Area
Urban 67.1 31.6 1.2 0.0 100.0 39.5 56.1 3.4 0.9 100.0 87.3 12.2 0.6 100.0 835
Wealth quintile Lowest 39.9 56.9 3.3 0.0 100.0 19.0 68.6 8.6 3.7 100.0 74.7 25.2 0.1 100.0 1,432 Second 47.6 50.3 2.1 0.0 100.0 22.0 68.1 7.3 2.6 100.0 75.1 24.7 0.2 100.0 1,338 Middle 50.6 47.5 1.8 0.0 100.0 22.7 66.3 8.8 2.2 100.0 81.7 18.3 0.0 100.0 1,244 Fourth 61.4 37.4 1.2 0.0 100.0 25.8 68.0 4.6 1.5 100.0 83.3 16.7 0.0 100.0 1,266 Highest 70.3 28.4 1.1 0.2 100.0 37.0 58.1 3.4 1.5 100.0 86.4 12.9 0.7 100.0 1,440
Total 54.0 44.1 1.9 0.0 100.0 25.4 65.7 6.5 2.3 100.0 80.2 19.6 0.2 100.0 6,719

Malaria Prevention • 39
Table 3.4 Access to an insecticide-treated net (ITN)
Percentage of the de facto population with access to an ITN in the household, by background characteristics, Sierra Leone MIS 2016
Background characteristic
Percent with access to an
ITN1,2 De facto
population
Residence Urban 31.5 15,743 Rural 40.9 23,513
Region Eastern 44.5 9,317 Northern 34.6 13,704 Southern 46.8 8,632 Western 21.6 7,603
District Kailahun 49.3 3,363 Kenema 48.9 3,058 Kono 34.4 2,896 Bombali 34.1 3,146 Kambia 41.3 1,733 Koinadugu 34.0 2,229 Port Loko 31.1 3,064 Tonkolili 35.3 3,532 Bo 52.5 3,406 Bonthe 48.1 1,287 Moyamba 41.2 2,102 Pujehun 41.8 1,837 Western Area Rural 20.6 3,326 Western Area Urban 22.4 4,278
Wealth quintile Lowest 35.7 7,855 Second 41.0 7,836 Middle 43.7 7,877 Fourth 36.1 7,837 Highest 29.3 7,851
Total 37.1 39,256 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months. 2 Percentage of the de facto household population who could sleep under an ITN if each ITN in the household were used by up to two people

40 • Malaria Prevention
Table 3.5 Use of mosquito nets by persons in the household
Percentage of the de facto household population who slept the night before the survey under a mosquito net (treated or untreated), under an insecticide-treated net (ITN), under a long-lasting insecticidal net (LLIN), and under an ITN or in a dwelling in which the interior walls have been sprayed against mosquitoes (IRS) in the past 12 months; and among the de facto household population in households with at least one ITN, the percentage who slept under an ITN the night before the survey, by background characteristics, Sierra Leone MIS 2016
Household population
Household population in households with at least one
ITN1
Background characteristic
Percentage who slept under any
mosquito net last night
Percentage who slept
under an ITN1 last night
Percentage who slept
under an LLIN last night
Number of persons
Percentage who slept
under an ITN1 last night
Number of persons
Age2 <5 44.9 44.1 44.1 7,365 71.3 4,554 5-14 32.3 31.8 31.8 10,789 50.8 6,745 15-34 36.0 35.5 35.4 11,302 59.2 6,765 35-49 47.7 47.0 46.9 5,194 75.8 3,216 50+ 45.0 44.4 44.4 4,561 72.8 2,785
Sex Male 37.1 36.5 36.5 18,812 59.9 11,475 Female 41.3 40.6 40.6 20,444 65.8 12,615
Residence Urban 31.5 31.1 31.1 15,743 54.9 8,917 Rural 44.5 43.7 43.6 23,513 67.7 15,173
Region Eastern 48.7 48.1 48.1 9,317 67.7 6,616 Northern 37.2 35.8 35.8 13,704 60.4 8,131 Southern 49.9 49.8 49.7 8,632 71.6 6,007 Western 19.4 19.4 19.4 7,603 44.2 3,336
District Kailahun 54.0 53.1 53.1 3,363 69.9 2,556 Kenema 55.4 55.4 55.4 3,058 73.4 2,309 Kono 35.4 34.5 34.5 2,896 57.1 1,752 Bombali 38.1 38.0 38.0 3,146 69.9 1,712 Kambia 45.9 45.4 45.3 1,733 66.2 1,190 Koinadugu 37.1 37.1 37.1 2,229 57.2 1,445 Port Loko 33.9 32.6 32.6 3,064 63.1 1,581 Tonkolili 35.1 31.1 31.1 3,532 49.9 2,202 Bo 55.7 55.7 55.7 3,406 72.2 2,630 Bonthe 51.4 51.3 51.3 1,287 70.6 935 Moyamba 44.3 44.3 44.3 2,102 74.1 1,258 Pujehun 44.3 44.2 43.7 1,837 68.6 1,184 Western Area Rural 20.7 20.6 20.6 3,326 46.6 1,468 Western Area Urban 18.5 18.5 18.5 4,278 42.3 1,868
Wealth quintile Lowest 40.8 39.8 39.7 7,855 69.7 4,485 Second 45.2 44.7 44.6 7,836 65.7 5,325 Middle 46.4 45.7 45.7 7,877 66.1 5,454 Fourth 37.7 37.0 37.0 7,837 61.6 4,703 Highest 26.2 26.0 26.0 7,851 49.6 4,122
Total 39.3 38.6 38.6 39,256 63.0 24,090
Note: Numbers in parentheses are based on 25-49 unweighted cases. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed. 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months. 2Excludes 23 persons for whom age information was not available.

Malaria Prevention • 41
Table 3.6 Use of existing ITNs
Percentage of insecticide-treated nets (ITNs) that were used by anyone the night before the survey, by background characteristics, Sierra Leone MIS 2016
Background characteristic
Percentage of existing ITNs1 used last night
Number of ITNs1
Residence Urban 86.4 2,609 Rural 90.2 5,191
Region Eastern 90.4 2,215 Northern 92.1 2,492 Southern 88.5 2,230 Western 77.4 863
District Kailahun 91.0 887 Kenema 90.1 806 Kono 89.9 522 Bombali 92.2 570 Kambia 97.1 370 Koinadugu 93.1 390 Port Loko 90.0 506 Tonkolili 90.2 655 Bo 89.2 981 Bonthe 91.3 352 Moyamba 88.1 468 Pujehun 84.9 428 Western Area Rural 88.8 353 Western Area Urban 69.5 510
Wealth quintile Lowest 92.9 1,493 Second 90.5 1,722 Middle 89.4 1,869 Fourth 90.4 1,484 Highest 79.5 1,231
Total 89.0 7,799 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months.

42 • Malaria Prevention
Table 3.7 Use of mosquito nets by children
Percentage of children under age 5 who, the night before the survey, slept under a mosquito net (treated or untreated), under an insecticide-treated net (ITN), under a long-lasting insecticidal net (LLIN), and under an ITN or in a dwelling in which the interior walls have been sprayed against mosquitoes (IRS) in the past 12 months; and among children under age 5 in households with at least one ITN, the percentage who slept under an ITN the night before the survey, by background characteristics, Sierra Leone MIS 2016
Children under age 5 in all households
Children under age 5 in households with at least one
ITN1
Background characteristic
Percentage who slept under any
mosquito net last night
Percentage who slept
under an ITN1 last night
Percentage who slept
under an LLIN last night
Number of children
Percentage who slept
under an ITN1 last night
Number of children
Age in months <12 49.2 48.0 48.0 1,413 76.4 888 12-23 46.8 46.1 46.1 1,364 76.0 828 24-35 45.0 43.8 43.8 1,412 72.0 859 36-47 43.1 42.7 42.7 1,581 67.1 1,006 48-59 41.1 40.6 40.6 1,596 66.6 972
Sex Male 44.5 43.8 43.8 3,680 70.9 2,276 Female 45.3 44.4 44.4 3,686 71.8 2,278
Residence Urban 38.3 37.6 37.6 2,777 67.0 1,560 Rural 48.9 48.0 48.0 4,588 73.6 2,994
Region Eastern 58.8 57.8 57.8 1,648 76.9 1,239 Northern 40.3 38.8 38.8 2,650 65.5 1,570 Southern 56.0 56.0 55.9 1,559 79.8 1,094 Western 26.2 26.2 26.2 1,509 60.8 652
District Kailahun 60.0 58.1 58.1 617 74.4 482 Kenema 66.4 66.4 66.4 592 81.5 482 Kono 47.0 45.9 45.9 439 73.4 275 Bombali 43.4 43.4 43.4 562 78.6 310 Kambia 49.2 48.7 48.5 299 70.0 207 Koinadugu 40.3 40.3 40.3 428 63.2 273 Port Loko 35.2 34.2 34.2 606 66.5 311 Tonkolili 38.7 34.3 34.3 755 55.4 468 Bo 64.5 64.5 64.5 634 81.6 501 Bonthe 54.4 54.4 54.4 220 76.4 157 Moyamba 49.5 49.5 49.5 356 84.8 208 Pujehun 48.3 48.1 47.7 349 73.5 229 Western Area Rural 26.4 26.4 26.4 784 62.1 334 Western Area Urban 26.1 26.1 26.1 724 59.4 318
Wealth quintile Lowest 44.7 43.4 43.3 1,601 76.7 906 Second 50.1 49.6 49.5 1,606 70.7 1,126 Middle 50.9 50.2 50.2 1,458 71.1 1,029 Fourth 42.6 41.4 41.4 1,495 71.5 865 Highest 34.0 33.9 33.9 1,205 64.9 629
Total 44.9 44.1 44.1 7,365 71.3 4,554
Note: Table is based on children who stayed in the household the night before the interview. 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months.

Malaria Prevention • 43
Table 3.8 Use of mosquito nets by pregnant women
Percentages of pregnant women age 15-49 who, the night before the survey, slept under a mosquito net (treated or untreated), under an insecticide-treated net (ITN), under a long-lasting insecticidal net (LLIN), and under an ITN or in a dwelling in which the interior walls have been sprayed against mosquitoes (IRS) in the past 12 months; and among pregnant women age 15-49 in households with at least one ITN, the percentage who slept under an ITN the night before the survey, by background characteristics, Sierra Leone MIS 2016
Among pregnant women age 15-49 in all households
Among pregnant women age 15-49 in households with at
least one ITN1
Background characteristic
Percentage who slept under any
mosquito net last night
Percentage who slept
under an ITN1 last night
Percentage who slept
under an LLIN last night
Number of women
Percentage who slept
under an ITN1 last night
Number of women
Residence Urban 31.4 30.7 30.7 267 65.7 124 Rural 53.0 52.8 52.8 404 79.0 270
Region Eastern 51.2 49.5 49.5 167 76.4 108 Northern 44.7 44.7 44.7 245 73.1 150 Southern 60.9 60.9 60.9 128 84.2 92 Western 19.0 19.0 19.0 130 (56.7) 44
District Kailahun (46.2) (46.2) (46.2) 49 (77.6) 29 Kenema (71.8) (71.8) (71.8) 55 (92.9) 43 Kono 36.9 32.6 32.6 63 (56.0) 37 Bombali 51.8 51.8 51.8 60 (84.8) 37 Kambia 46.4 46.4 46.4 33 (71.1) 21 Koinadugu (63.5) (63.5) (63.5) 31 (87.6) 23 Port Loko 31.0 31.0 31.0 73 (62.9) 36 Tonkolili (43.3) (43.3) (43.3) 48 (62.5) 33 Bo 67.8 67.8 67.8 64 (90.3) 48 Bonthe (55.8) (55.8) (55.8) 13 * 10 Moyamba (63.8) (63.8) (63.8) 21 * 15 Pujehun (46.5) (46.5) (46.5) 30 (71.7) 20 Western Area Rural (28.1) (28.1) (28.1) 53 * 22 Western Area Urban (12.6) (12.6) (12.6) 77 * 21
Education No education 47.4 47.4 47.4 348 82.0 201 Primary 33.5 33.5 33.5 121 56.1 72 Secondary 45.5 44.1 44.1 197 73.3 119 More than secondary * * * 4 * 3
Wealth quintile Lowest 52.5 52.5 52.5 152 87.5 91 Second 45.3 44.6 44.6 123 66.1 83 Middle 57.2 57.2 57.2 123 80.6 87 Fourth 40.4 39.1 39.1 135 73.3 72 Highest 27.2 27.2 27.2 137 (61.2) 61
Total 44.4 44.0 44.0 671 74.8 395
Note: Table is based on women who stayed in the household the night before the interview. Numbers in parentheses are based on 25-49 unweighted cases. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed. 1 An insecticide-treated net (ITN) is (1) a factory-treated net that does not require any further treatment (LLIN) or (2) a net that has been soaked with insecticide within the past 12 months.

44 • Malaria Prevention
Table 3.9 Use of Intermittent Preventive Treatment (IPTp) by women during pregnancy
Percentage of women age 15-49 with a live birth in the 2 years preceding the survey who, during the pregnancy preceding the last birth, received one or more doses of SP/Fansidar at least one of which was received during an ANC visit, received two or more doses of SP/Fansidar at least one of which was received during an ANC visit, and received three or more doses of SP/Fansidar at least one of which was received during an ANC visit, according to background characteristics, Sierra Leone MIS 2016
Background characteristic
Percentage who received one or more
doses of SP/Fansidar1
Percentage who received two or more
doses of SP/Fansidar1
Percentage who received three or more
doses of SP/Fansidar1
Number of women with a live birth in the
2years preceding the
survey
Residence Urban 90.9 64.1 24.7 938 Rural 89.9 75.9 34.9 1,513
Region Eastern 92.1 72.6 32.7 571 Northern 88.0 75.7 36.0 918 Southern 92.3 73.2 30.8 455 Western 90.7 60.3 20.3 507
District Kailahun 86.1 67.8 45.5 213 Kenema 94.0 77.5 27.3 185 Kono 97.4 73.3 22.8 172 Bombali 89.2 83.0 17.2 187 Kambia 96.8 86.6 40.3 119 Koinadugu 72.3 60.9 38.7 143 Port Loko 84.3 66.1 38.0 203 Tonkolili 94.3 81.1 44.3 268 Bo 90.2 76.3 32.4 154 Bonthe 93.2 72.4 35.6 72 Moyamba 95.6 84.4 31.5 116 Pujehun 91.1 58.1 24.7 112 Western Area Rural 90.4 67.5 23.4 288 Western Area Urban 91.1 50.7 16.2 219
Education No education 89.3 73.2 31.8 1,387 Primary 92.7 71.5 35.3 375 Secondary 90.9 67.8 27.2 675 More than secondary * * * 14
Wealth quintile Lowest 90.7 76.2 36.1 543 Second 89.2 74.0 34.3 512 Middle 90.6 73.5 36.6 493 Fourth 91.3 71.4 27.3 510 Highest 89.4 58.4 17.6 392
Total 90.3 71.3 31.0 2,451
Note: An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed. 1 Received the specified number of doses of SP/Fansidar, at least one of which was received during an ANC visit

Malaria in Children • 45
MALARIA IN CHILDREN 4
Key Findings
Fever prevalence:
x One in four children under age 5 had fever in the 2 weeks before the survey (27%).
Care-seeking for fever:
x Advice or treatment was sought for 71% of children with fever in the 2 weeks before the survey.
Source of advice or treatment:
x Among children with recent fever for whom care was sought, 88% received advice or treatment from the public sector, 11% from the private sector, and only 2% elsewhere.
Testing:
x Fifty-one percent of children with a recent fever received a finger or heel prick for testing.
Type of antimalarial drug used:
x Among children under 5 with a recent fever who received an antimalarial, 97% received artemisinin combination therapy.
Severe anaemia:
x One in10 children age 6-59 months has a haemoglobin level less than 8g/dl.
Malaria:
x Four in ten children age 6-59 months tested positive for malaria via microscopy.
his chapter presents data useful for assessing how well fever management strategies are implemented. Specific topics include care seeking for febrile children, diagnostic testing of children with fever, and therapeutic use of antimalarial drugs. Prevalence of anaemia and malaria
among children age 6-59 months is also assessed.
4.1 CARE SEEKING FOR FEVER IN CHILDREN
Care seeking for children under 5 with fever Percentage of children under 5 with a fever in the 2 weeks before the survey for whom advice or treatment was sought from a health provider, a health facility, or a pharmacy. Sample: Children under 5 with a fever in the 2 weeks before the survey
T

46 • Malaria in Children
One of the key case management objectives of the National Malaria Control Programme (NMCP) is to ensure that all suspected malaria cases have access to confirmatory diagnosis and receive effective treatment (MOHS 2015a).
Fever is a key symptom of malaria and other acute infections in children. Malaria fevers require prompt and effective treatment to prevent malaria morbidity and mortality. Twenty-seven percent of children under age 5 had fever in the 2 weeks preceding the survey. Advice or treatment was sought for 71% of the children with fever in the 2 weeks preceding the survey, and timely care seeking (the same or next day following fever onset) occurred for 50% of the febrile children (Table 4.1).
Among children with recent fever for whom care was sought, most received advice or treatment from the public health sector (88%); among these children seeking care from public health facilities, 67% sought care from a government health centre, and 15% from a government hospital. Only 11% sought advice from a private sector source (Table 4.2).
Trends: The percentage of children who sought care from a health provider, a health facility, or a pharmacy increased from 63% in the 2013 SLMIS to 71% in the 2016 SLMIS. The change appears to be driven by an increase in care seeking from public sources, which rose from 53% to 63% between the 2013 SLMIS and the 2016 SLMIS (Figure 4.1).
Patterns by background characteristics
� Care seeking for children with fever was more common for those less than age 12 months compared with older children age 48-59 months (79% and 62%, respectively) (Table 4.1).
� The percentage of children with fever for whom advice or treatment was sought was high in the Southern, Eastern, and Northern regions (76%, 75%, and 71%, respectively) but was only 58% in Western Region.
� Pujehun had the highest percentage of children for whom advice or treatment was sought (85%) while West Area Rural had the lowest (50%).
� Similarly, the percentage of children under 5 for whom advice or treatment was sought the same or next day following fever onset varied from 85% in Pujehun to 28% in West Area Rural.
4.2 DIAGNOSTIC TESTING OF CHILDREN WITH FEVER
Diagnosis of malaria in children under 5 with fever Percentage of children under 5 with a fever in the 2 weeks before the survey who had blood taken from a finger or heel for testing. This is a proxy measure of diagnostic testing for malaria. Sample: Children under 5 with a fever in the 2 weeks before the survey
National Malaria Control Programme policy recommends prompt parasitological confirmation by microscopy or, alternatively, by rapid diagnostic tests (RDTs) for all patients suspected of malaria before treatment is started (MoHS 2015c). Adherence to this policy cannot be directly measured through household surveys; however, the 2016 SLMIS asked interviewed women with children under 5 who had a
Figure 4.1 Trends in care seeking for fever in children by source of care
53
11 10
6363
8 2
71
Publicsector
Privatesector
Othersource
Anysource
Percent of children under age 5 with fever in the 2 weeks preceding the survey for whom advice or treatment was sought
from specific sources.
2013 SLMIS 2016 SLMIS

Malaria in Children • 47
fever in the 2 weeks before the survey if the child had blood taken from a finger or heel for testing during the illness. This information is used as a proxy measure for adherence to the NMCP policy of conducting diagnostic testing for all suspected malaria cases.
In the 2016 SLMIS, 51% of children with a fever in the 2 weeks before the survey had blood taken from a finger or heel, presumably for malaria testing (Table 4.1).
Trends: The percentage of children who had blood taken from a finger or heel for testing increased from 40% in the 2013 SLDHS to 51% in the 2016 SLMIS. This shows improved adherence to the malaria treatment policy of testing before treatment.
Patterns by background characteristics
� The percentage of children with recent fever who had blood taken from a finger or heel for testing decreases with increasing age. Fifty-nine percent of children less than age 12 months had blood taken from a finger or heel for testing, compared with 43% of children age 48-59 months.
� Fifty-four percent of children under age 5 with recent fever from rural areas had blood taken from a finger or heel for testing, compared with 47% in urban areas.
� Sixty percent of children under 5 with recent fever in the Southern Region had blood taken from a finger or heel for testing, compared with only 29% in the Western Region (Figure 4.2).
� At the district level, the percentage of children under 5 with recent fever who had blood taken from a finger or heel for testing was greatest in Moyamba and Pujehun (71%) and lowest in Western Area Urban (27%).
4.3 USE OF RECOMMENDED ANTIMALARIALS
Artemisinin-based combination therapy (ACT) for children under 5 with fever Among children under 5 with a fever in the 2 weeks before the survey who took any antimalarial drugs, the percentage who took an artemisinin-based combination therapy (ACT). Sample: Children under 5 with a fever in the 2 weeks before the survey who took any antimalarial drug
Artemisinin-based combination therapy (ACT) is the recommended first-line antimalarial drug for the treatment of uncomplicated malaria in Sierra Leone. This policy has been recommended since 2004 and implemented since 2006 (MOHS 2015).
Figure 4.2 Diagnostic testing of children with fever by region
56
50
60
29
51
Eastern Region
Northern Region
Southern Region
Western Region
Total
Percent of children under age 5 with fever in the 2 weeks preceding the survey who had blood taken from a finger or heel for
testing

48 • Malaria in Children
According to the results shown in Table 4.3, most children under age 5 with recent fever who received an antimalarial took an ACT, either artesunate + amodiaquine (ASAQ) or artemether + lumefantrine (AL) (97%). One percent of children with fever who received an antimalarial took SP/Fansidar, 1% took chloroquine, 1% took amodiaquine, and 1% took other antimalarials while less than 1% took quinine or artesunate. The distribution of antimalarial drug use by children under age 5 with recent fever did not vary substantially by background characteristics (Table 4.3).
Trends: There has been a large increase in the percentage of children under age 5 using ACTs among those with recent fever who received any antimalarials, from 21% in the 2008 SLDHS to 84% in the 2013 SLMIS to 97% in the 2016 SLMIS (Figure 4.3).
4.4 PREVALENCE OF LOW HAEMOGLOBIN IN CHILDREN
Prevalence of low haemoglobin in children Percentage of children age 6-59 months who had a haemoglobin measurement of less than 8 grams per decilitre (g/dl) of blood. The cutoff of 8 g/dl is often used to classify malaria-related anaemia. Sample: Children age 6-59 months
Anaemia, defined as a reduced level of haemoglobin in blood, decreases the amount of oxygen reaching the tissues and organs of the body and reduces their capacity to function. Anaemia is associated with impaired motor and cognitive development in children. The main causes of anaemia in children are malaria and inadequate intake of iron, folate, vitamin B12, or other nutrients. Other causes of anaemia include intestinal worms, haemoglobinopathy, and sickle cell disease. Although anaemia is not specific to malaria, trends in anaemia prevalence can reflect malaria morbidity, and they respond to changes in the coverage of malaria interventions (Korenromp 2004). Malaria interventions have been associated with a 60% reduction in the risk of anaemia using a cut-off of 8g/dl (RBM 2003).
Among eligible children age 6-59 months from interviewed households, almost all (99%) consented and were tested for anaemia (Table 4.4).
Trends: The national prevalence of haemoglobin <8g/dl in children age 6-59 months has not changed from the 2008 SLDHS to the 2013 SLMIS to the 2016 SLMIS (10% in each case).
Figure 4.3 Trends in ACT use by children under age 5
21
84
97
2008 SLDHS 2013 SLMIS 2016 SLMIS
Among children under age 5 with a fever in the 2 weeks before the survey who took an antimalarial, percentage who took any artemisinin-based combination therapy
(ACT)

Malaria in Children • 49
Patterns by background characteristics
� The prevalence of low haemoglobin in children age 6-59 months is almost twice as high in rural compared with urban areas (12% and 7%, respectively) (Figure 4.4).
� Koinadugu has the highest percentage of children age 6-59 months with low haemoglobin (20%) and Kono and West Area Urban have the lowest (3% and 2%, respectively).
� The prevalence of low haemoglobin in children age 6-59 months decreases with increasing wealth quintile, from 13% among children in the lowest wealth quintile to 3% among children in the highest (Figure 4.5).
Figure 4.4 Prevalence of low haemoglobin in children by district
Figure 4.5 Low haemoglobin among children by household wealth
13 13
10 9
3
10
Lowest Second Middle Fourth Highest Total
Percentage of children age 6-59 months
Poorest Wealthiest

50 • Malaria in Children
4.5 PREVALENCE OF MALARIA IN CHILDREN
Malaria prevalence in children Percentage of children age 6-59 months infected with malaria according to microscopy results. Sample: Children age 6-59 months
As is the case in many other countries in sub-Saharan Africa, malaria is the leading cause of death in Sierra Leone among children under 5. Malaria transmission is high throughout the year, contributing to development of partial immunity within the first 2 years of life. However, many people, including children, may have malaria parasites in their blood without showing any signs of infection. Such asymptomatic infection not only contributes to further transmission of malaria but also increases the risk of anaemia and other associated morbidity among the infected individuals.
In the 2016 SLMIS, 40% of children age 6-59 months were positive for malaria parasites according to microscopy results (Table 4.6). Rapid diagnostic tests (RDTs) were done in conjunction with microscopy to facilitate treatment of infected children during the survey fieldwork. Results from these RDTs are also presented in Table 4.6 for reference. Fifty-three percent of children age 6-59 months tested positive for malaria antigens using RDTs.
The differences in malaria prevalence observed between the RDT and microscopy results are expected. Microscopic detection of malaria parasites depends on the visualisation of stained parasites under a microscope, whereas the diagnosis of malaria by RDT relies on the interaction between a parasite antigen present in the blood and an antibody in the RDT formulation. Therefore, direct comparisons of malaria results from microscopy with those from RDTs should be avoided. The First Response SD Bioline, like many other commercially available RDTs, detects the P. falciparum-specific, histidine-rich protein-2 (HRP-2) rather than the parasite itself. Because HRP-2 remains in the blood for up to a month following parasite clearance with antimalarials (Moody 2002), in areas highly endemic for P. falciparum, its persistence often leads to higher malaria prevalence estimates detected using RDTs compared with those measured using microscopy.
Another factor likely to affect comparisons of malaria prevalence estimates is the season of data collection. There are two major seasons, a summer rainy season (May-October) with heavy rains in July and August, and a dry season from November to April. Despite these seasonal fluctuations, the tropical climate in Sierra Leone has rainfall patterns, temperature, and humidity that supports continuous malaria transmission all year round.
The 2016 SLMIS was conducted in July and August of 2016 at the peak of malaria season. Normally a spike in malaria cases occurs during these months. The 2013 SLMIS, in comparison, was conducted in February and March 2013, during the dry period when malaria transmission is lower.

Malaria in Children • 51
Trends: National malaria prevalence has not changed significantly between the 2013 SLMIS and the 2016 SLMIS; however, some district-level changes have occurred. Malaria prevalence declined from 57% to 38% in Kono, from 52% to 38% in Bombali, from 61% to 48% in Kambia, and from 19% to 6% in West Area Urban. In Port Loko, malaria prevalence rose from 49% to 59% between the 2013 SLMIS and the 2016 SLMIS (Figure 4.6).
Patterns by background characteristics
� Malaria prevalence increases with age from 23% in children age 6-8 months to 50% in children age 48-59 months (Table 4.6).
� Malaria prevalence is higher among children in the lowest wealth quintiles (52%) compared with the highest wealth quintiles (15%).
� Malaria prevalence is higher among children whose mothers have no formal education (41%) than among those whose mothers had a secondary education (28.4%).
� Malaria prevalence is almost two times higher in rural areas (49%) than in urban areas (25%).
� By region, malaria prevalence according to microscopy is highest in the Northern Region (52%) relative to the Eastern and Southern Regions (40% in both), and Western Region (21%).
� Among the districts, the highest malaria prevalence is found in Port Loko (59%) and the lowest in Western Area Urban (6%) (Figure 4.7).
Figure 4.6 Trends in prevalence of malaria in children by district
Figure 4.7 Prevalence of malaria in children by district
0
10
20
30
40
50
60
70
Percentage of children age 6-59 months who tested positive for malaria by microscopy
2013 SLMIS 2016 SLMIS

52 • Malaria in Children
LIST OF TABLES
For detailed information on malaria, see the following tables:
� Table 4.1 Prevalence, care seeking, and diagnosis of children with fever � Table 4.2 Source of advice or treatment for children with fever � Table 4.3 Types of antimalarial drugs used � Table 4.4 Coverage of testing for anaemia and malaria in children � Table 4.5 Haemoglobin <8.0g/dl in children � Table 4.6 Prevalence of malaria in children

Malaria in Children • 53
Table 4.1 Prevalence, care seeking and diagnosis of children with fever
Percentage of children under age 5 with fever in the 2 weeks preceding the survey; and among children under age 5 with fever, the percentage for whom advice or treatment was sought, the percentage for whom advice or treatment was sought the same or next day, and the percentage for whom blood was taken from a finger or heel for testing, Sierra Leone MIS 2016
Children under age 5 Children under age 5 with fever
Background characteristic
Percentage with fever in the 2 weeks
preceding the survey
Number of children
Percentage for whom advice or treatment was sought1
Percentage for whom advice or treatment was sought the same or
next day
Percentage who had blood taken from a finger or heel
for testing Number of
children
Age in months <12 24.9 1,281 79.4 54.7 58.9 318 12-23 33.5 1,174 75.6 53.7 57.1 394 24-35 29.1 1,037 68.1 45.0 46.7 302 36-47 23.8 1,194 68.5 53.8 46.1 285 48-59 22.0 1,119 61.6 41.4 42.9 246
Sex Male 26.8 2,881 70.5 48.3 49.6 774 Female 26.4 2,922 72.2 52.3 52.7 771
Residence Urban 24.2 2,236 69.0 46.3 46.7 540 Rural 28.2 3,568 72.6 52.4 53.5 1,005
Region Eastern 29.3 1,295 74.8 53.8 56.3 380 Northern 27.6 2,117 70.8 49.1 49.7 585 Southern 32.8 1,167 75.9 56.5 59.5 383 Western 16.1 1,225 57.7 34.9 29.4 198
District Kailahun 30.4 489 69.8 50.8 54.9 149 Kenema 19.2 444 71.7 62.1 56.8 85 Kono 40.3 362 81.6 52.0 57.4 146 Bombali 31.0 454 81.4 61.5 56.3 141 Kambia 26.9 261 82.0 50.9 69.8 70 Koinadugu 30.6 347 53.6 38.6 43.5 106 Port Loko 16.9 491 54.8 40.0 28.7 83 Tonkolili 32.7 565 75.6 48.9 50.0 185 Bo 35.0 461 65.4 42.4 47.1 161 Bonthe 23.6 163 80.8 55.8 58.2 38 Moyamba 28.1 271 81.0 46.9 70.8 76 Pujehun 39.5 271 86.4 84.8 70.5 107 Western Area Rural 18.1 673 50.1 28.0 30.8 122 Western Area Urban 13.8 552 (69.9) (46.0) (27.1) 76
Mother’s education No education 26.5 3,467 69.4 50.3 52.0 917 Primary 27.9 843 71.0 44.3 49.5 235 Secondary 26.4 1,408 77.1 54.2 51.4 374 More than secondary * 27 * * * 5
Wealth quintile Lowest 28.1 1,251 64.6 44.7 48.0 352 Second 28.7 1,250 74.5 52.9 53.7 359 Middle 29.4 1,144 76.3 55.4 58.2 336 Fourth 24.3 1,204 72.8 53.5 54.0 293 Highest 21.5 955 67.5 42.1 36.3 206
Total 26.6 5,804 71.4 50.3 51.1 1,545 1 Excludes advice or treatment from a traditional practitioner Numbers in parentheses are based on 25-49 unweighted cases. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.

54 • Malaria in Children
Table 4.2 Source of advice or treatment for children with fever
Percentage of children under age 5 with fever in the 2 weeks preceding the survey for whom advice or treatment was sought from specific sources; and among children under age five with fever in the two weeks preceding the survey for whom advice or treatment was sought, the percentage for whom advice or treatment was sought from specific sources, by background characteristics, Sierra Leone MIS 2016
Percentage for whom advice or treatment was sought
from each source:
Background characteristic
Among children with fever
Among children with fever for
whom advice or treatment was
sought
Among children with fever who took any ACT
the same or next day
Any public sector source 63.0 87.5 83.4 Government hospital 10.9 15.2 11.1 Government health centre 47.9 66.5 67.2 Mobile clinic 1.3 1.8 0.9 Community health worker 4.1 5.7 5.1
Any private sector source 8.2 11.3 8.6 Private hospital 1.0 1.4 1.0 Private clinic 1.4 1.9 2.0 Mission/faith based hospital 0.9 1.2 1.4 Mission/faith based clinic 0.2 0.3 0.3 Pharmacy 4.0 5.6 2.8 Mobile clinic 0.4 0.5 0.5 Other private medical sector 0.3 0.4 0.6
Any other source 1.6 2.2 0.6 Shop 0.1 0.1 0.2 Traditional healer 0.3 0.4 0.1 Drug peddler 0.9 1.3 0.2 Other 0.3 0.4 0.1
Number of children 1,545 1,112 693
CHW = Community health worker

Malaria in Children • 55
Table 4.3 Type of antimalarial drugs used
Among children under age 5 with fever in the 2 weeks preceding the survey who took any antimalarial medication, the percentage who took specific antimalarial drugs, by background characteristics, Sierra Leone MIS 2016
Percentage of children who took:
Number of children with
fever who took anti-malarial
drug Background characteristic Any ACT1 SP/Fansidar Chloroquine
Amodia-quine Quinine pills
Artesunate rectal
Other anti- malarial
Age in months <6 (95.8) (0.0) (0.0) (0.0) (0.0) (0.0) (4.2) 29 6-11 93.1 0.5 3.0 3.4 0.0 0.0 0.9 133 12-23 98.7 1.3 0.4 1.1 0.1 0.4 0.9 231 24-35 95.8 0.7 1.3 1.3 0.3 0.4 1.2 175 36-47 98.7 1.2 0.4 0.8 1.1 1.0 1.0 173 48-59 94.0 1.3 2.8 0.4 1.2 0.2 0.8 135
Sex Male 96.4 0.7 1.9 0.7 0.6 0.4 0.8 427 Female 96.5 1.2 0.8 1.9 0.4 0.4 1.4 449
Residence Urban 93.8 2.1 2.9 2.3 0.5 1.0 1.5 306 Rural 97.9 0.4 0.5 0.7 0.5 0.1 0.9 570
Region Eastern 99.2 0.3 0.3 0.0 0.3 0.0 1.2 219 Northern 95.3 1.3 1.2 2.6 0.7 0.3 1.7 325 Southern 98.5 0.3 0.2 0.7 0.6 0.4 0.1 240 Western 88.5 3.2 7.2 1.6 0.0 2.0 1.5 92
District Kailahun 100.0 0.0 0.0 0.0 0.0 0.0 0.0 77 Kenema 98.1 0.0 0.0 0.0 0.0 0.0 1.9 58 Kono 99.3 0.7 0.9 0.0 0.7 0.0 1.8 84 Bombali 98.6 1.4 0.0 0.0 0.0 0.0 1.4 83 Kambia 92.5 4.7 2.1 1.3 0.0 1.6 2.0 52 Koinadugu 100.0 0.0 1.1 5.6 0.0 0.0 4.0 51 Port Loko (86.3) (2.2) (4.0) (7.5) (0.0) (0.0) (0.0) 29 Tonkolili 94.4 0.0 1.1 2.4 2.2 0.0 1.1 110 Bo 98.1 0.0 0.5 1.5 0.0 0.0 0.0 90 Bonthe 100.0 0.0 0.0 0.0 0.0 0.0 0.0 25 Moyamba 97.7 1.5 0.0 0.5 1.5 2.1 0.0 50 Pujehun 99.0 0.0 0.0 0.0 0.8 0.0 0.2 76 Western Area Rural (81.8) (0.0) (14.5) (0.6) (0.0) (0.0) (3.1) 46 Western Area Urban (95.1) (6.4) (0.0) (2.5) (0.0) (3.9) (0.0) 47
Mother’s education No education 96.8 0.5 1.5 1.0 0.4 0.0 1.3 510 Primary 96.7 2.0 0.9 0.9 0.5 2.8 1.3 131 Secondary 96.1 1.1 1.2 2.2 0.7 0.0 0.5 232 More than secondary * * * * * * * 3
Wealth quintile Lowest 97.2 0.4 1.0 0.4 0.9 0.4 0.7 183 Second 98.5 0.3 0.5 0.5 0.5 0.0 1.2 210 Middle 96.7 0.2 0.2 3.2 0.0 0.1 1.3 210 Fourth 95.3 1.2 4.0 0.0 0.1 0.0 1.6 161 Highest 92.6 4.4 1.9 2.5 1.2 2.4 0.3 112
Total 96.5 1.0 1.3 1.3 0.5 0.4 1.1 876 1ACT = Artemisinin-based combination therapy (artesunate + amodiaquine (ASAQ) or artemether + lumefantrine (AL)) Numbers in parentheses are based on 25-49 unweighted cases. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.

56 • Malaria in Children
Table 4.4 Coverage of testing for anaemia and malaria
Percentage of eligible children age 6-59 months who were tested for anaemia and malaria, by background characteristics, Sierra Leone MIS 2016
Percentage tested for Background characteristic Anaemia
Malaria by RDT
Malaria by microscopy
Number of children
Age in months 6-8 98.4 98.2 98.4 420 9-11 99.3 99.1 99.3 382 12-17 98.6 98.3 98.4 762 18-23 99.4 98.8 99.4 600 24-35 98.9 98.8 98.9 1,412 36-47 98.7 98.5 98.7 1,581 48-59 98.4 98.2 98.3 1,587
Sex Male 98.6 98.4 98.6 3,369 Female 98.9 98.6 98.8 3,375
Mother’s interview status Interviewed 98.7 98.6 98.7 5,085 Not interviewed1 99.0 98.2 98.9 1,659
Residence Urban 98.9 98.6 98.9 2,582 Rural 98.6 98.5 98.6 4,162
Region Eastern 99.0 98.9 99.0 1,484 Northern 98.2 98.1 98.2 2,407 Southern 98.6 98.5 98.5 1,432 Western 99.6 98.8 99.6 1,421
District Kailahun 99.5 99.5 99.5 567 Kenema 98.7 98.7 98.5 543 Kono 98.8 98.1 98.8 374 Bombali 99.8 99.4 99.8 529 Kambia 96.0 96.0 96.0 276 Koinadugu 98.7 98.7 98.7 388 Port Loko 96.4 96.4 96.4 534 Tonkolili 99.0 99.0 99.0 680 Bo 99.8 99.6 99.6 596 Bonthe 94.9 94.9 94.9 194 Moyamba 98.4 98.4 98.4 335 Pujehun 98.9 98.9 98.9 307 Western Area Rural 99.3 97.9 99.3 726 Western Area Urban 99.8 99.8 99.8 694
Mother’s education2 No education 98.6 98.5 98.6 3,083 Primary 98.4 98.2 98.2 742 Secondary 99.1 99.1 99.1 1,233 More than secondary * * * 26
Wealth quintile Lowest 98.7 98.7 98.7 1,446 Second 98.7 98.5 98.6 1,455 Middle 98.2 98.1 98.2 1,331 Fourth 98.7 98.4 98.7 1,376 Highest 99.7 99.0 99.7 1,135
Total 98.8 98.5 98.7 6,744
1 Includes children whose mothers are deceased. 2 Excludes children whose mothers are not interviewed. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.

Malaria in Children • 57
Table 4.5 Haemoglobin <8.0 g/dl in children
Percentage of children age 6-59 months with haemoglobin lower than 8.0 g/dl, by background characteristics, Sierra Leone MIS 2016
Background characteristic
Haemoglobin <8.0 g/dl
Number of children
Age in months 6-8 10.6 414 9-11 11.9 379 12-17 13.1 750 18-23 9.9 596 24-35 11.9 1,397 36-47 9.1 1,560 48-59 7.5 1,562
Sex Male 10.9 3,322 Female 9.2 3,337
Mother’s interview status Interviewed 10.1 5,017 Not interviewed1 10.1 1,642
Residence Urban 6.7 2,555 Rural 12.2 4,104
Region Eastern 8.6 1,469 Northern 12.3 2,364 Southern 10.2 1,411 Western 7.8 1,414
District Kailahun 13.1 564 Kenema 7.6 536 Kono 3.0 369 Bombali 8.4 528 Kambia 11.0 265 Koinadugu 20.2 383 Port Loko 10.5 515 Tonkolili 12.9 673 Bo 9.8 594 Bonthe 6.8 184 Moyamba 10.2 330 Pujehun 13.0 304 Western Area Rural 13.2 721 Western Area Urban 2.2 693
Mother’s education2 No education 10.4 3,039 Primary 12.4 730 Secondary 8.0 1,222 More than secondary * 26
Wealth quintile Lowest 13.3 1,428 Second 13.1 1,435 Middle 10.0 1,306 Fourth 9.4 1,359 Highest 3.1 1,131
Total 10.1 6,659
Note: Table is based on children who stayed in the household the night before the interview. Prevalence of anaemia is based on haemoglobin levels and is adjusted for altitude using CDC formulas (CDC 1998). Haemoglobin is measured in grams per decilitre (g/dl). 1 Includes children whose mothers are deceased 2 Excludes children whose mothers are not interviewed An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.

58 • Malaria in Children
Table 4.6 Prevalence of malaria in children
Percentage of children age 6-59 months classified in two tests as having malaria, by background characteristics, Sierra Leone MIS 2016
Malaria prevalence according
to RDT Malaria prevalence according
to microscopy Background characteristic RDT positive
Number of children
Microscopy positive
Number of children
Age in months 6-8 30.3 413 23.3 414 9-11 34.2 378 25.3 379 12-17 43.0 749 30.3 750 18-23 45.6 592 30.1 596 24-35 57.1 1,395 40.0 1,397 36-47 56.3 1,557 46.9 1,560 48-59 63.1 1,559 50.1 1,561
Sex Male 53.5 3,316 40.4 3,322 Female 52.0 3,329 39.9 3,336
Mother’s interview status Interviewed 51.3 5,016 38.2 5,017 Not interviewed1 57.1 1,629 46.0 1,641
Residence Urban 31.5 2,545 25.2 2,555 Rural 65.9 4,099 49.4 4,103
Region Eastern 59.8 1,467 40.4 1,468 Northern 64.6 2,362 51.8 2,364 Southern 59.2 1,411 39.5 1,411 Western 18.8 1,404 20.9 1,414
District Kailahun 67.0 564 45.0 564 Kenema 59.3 536 37.7 535 Kono 49.5 367 37.5 369 Bombali 47.7 526 37.6 528 Kambia 59.4 265 48.3 265 Koinadugu 78.1 383 57.9 383 Port Loko 69.8 515 58.5 515 Tonkolili 68.3 673 55.7 673 Bo 57.1 594 39.7 593 Bonthe 46.8 184 26.1 184 Moyamba 60.6 330 39.9 330 Pujehun 69.2 304 46.8 304 Western Area Rural 33.5 711 34.9 721 Western Area Urban 3.8 693 6.3 693
Mother’s education2 No education 55.2 3,038 41.2 3,040 Primary 57.5 729 43.2 729 Secondary 38.7 1,222 28.4 697 More than secondary * 26 * 26
Wealth quintile Lowest 66.9 1,427 51.7 1,427 Second 68.1 1,433 52.4 1,434 Middle 62.4 1,306 44.9 1,307 Fourth 43.9 1,355 31.8 1,359 Highest 14.4 1,124 14.5 1,131
Total 52.7 6,644 40.1 6,658
1 Includes children whose mothers are deceased. 2 Excludes children whose mothers are not interviewed. An asterisk indicates a figure is based on fewer than 25 cases and has been suppressed.

Malaria Knowledge • 59
MALARIA KNOWLEDGE 5
Key Findings
x General knowledge: 98% of women have heard of malaria.
x Knowledge of causes: 94% of women report mosquito bites as a cause of malaria.
x Knowledge of symptoms: 69% of women recognise fever as a symptom of malaria.
x Knowledge of symptoms of severe malaria: 92% of women recognise at least one symptom of severe malaria.
x Knowledge of prevention: 90% report use of treated mosquito nets as a prevention method.
x Knowledge of treatment: 85% report ACT as medication to treat malaria.
x Correct knowledge of malaria: 85% of women know the symptoms, preventive measures, and treatment for malaria.
x Media exposure to malaria messages: 82% of women saw or heard a message about malaria in the 6 months before the survey.
his chapter presents data that are useful for assessing general knowledge about malaria, including signs and symptoms, causes, and preventive measures.
5.1 GENERAL KNOWLEDGE OF MALARIA
General knowledge of malaria Percentage of interviewed women who have heard of malaria Sample: Women age 15-49
In Sierra Leone knowledge about malaria is high among women. In the 2016 SLMIS, 98% of women had heard of malaria (Table 5.1). A series of additional questions assessing knowledge of specific aspects of malaria risk, prevention, and treatment were asked of women who reported having heard of the disease.
Trends: The percentage of women who have heard about malaria has not changed significantly from the 2013 SLMIS to the 2016 SLMIS (96% and 98%, respectively).
Patterns by background characteristics
� A significant proportion of women have heard of malaria regardless of age, region, urban or rural residence, educational level, and household wealth quintile.
T

60 • Malaria Knowledge
� The percentage of women who have heard of malaria is lowest in Moyamba (87%) and Bonthe (90%) districts compared with over 95% in all other districts.
5.2 KNOWLEDGE OF CAUSES OF MALARIA
Knowledge of causes of malaria Percentage of interviewed women who recognise mosquito bites as a cause of malaria. Sample: Women age 15-49 who have heard of malaria
Even though almost all women mentioned mosquito bites as a cause of malaria (94%), almost half (47%) volunteered additional responses that are not actual causes of the disease (Table 5.2). Common responses included ‘dirty surroundings’ (26%), ‘cold or changing weather’ (10%), and ‘drinking dirty water’ (7%), which could be considered misconceptions of causes of malaria.
Trends: Among women who have heard of malaria, the percentage who mentioned mosquito bites as a cause of malaria continues to be high compared with the previous MIS. The trend did not change significantly from the 2013 SLMIS to the 2016 SLMIS (91% and 94%, respectively).
Patterns by background characteristics
� Knowledge of mosquito bites as the cause of malaria was high among women across all subgroups.
� The belief that cold or changing weather can cause malaria was more prevalent among rural women than among urban women (14% vs. 5%), but the inverse was true for the belief that dirty surroundings cause malaria (22% among rural women, 31% among urban women).
� There are few variations between women in urban and rural locations, among women from various wealth quintiles, and among women with low versus high levels of education regarding misconceptions about causes of malaria.
5.3 KNOWLEDGE OF SYMPTOMS OF MALARIA AND OF SEVERE MALARIA
Knowledge of symptoms of malaria Percentage of interviewed women who identify fever as a symptom of malaria Sample: Women age 15-49 who have heard of malaria
Knowledge of symptoms of severe malaria Percentage of interviewed women who identify any of the symptoms of malaria Sample: Women age 15-49 who have heard of malaria
When women were asked if they knew any symptoms of malaria, 69% of women identified fever as a symptom of malaria, 33% identified loss of appetite, 30% said body weakness, and 29% mentioned headache. A much smaller percentage of women mentioned other symptoms. However, one-third of women did not mention fever, which is considered to be the most common and earliest symptom of malaria (Table 5.3). Women were also asked to identify symptoms of severe malaria. Ninety-two percent were able to identify at least one symptom of severe malaria (Table 5.4). Forty-two percent of women who

Malaria Knowledge • 61
had heard of malaria mentioned vomiting everything, 38% mentioned convulsion, 29% anaemia, and 11% confusion1 as symptoms of severe malaria.
Trends: The percentage of women who mentioned fever as a symptom of malaria has remained fairly stable from the 2013 SLMIS to the 2016 SLMIS (64% and 69%, respectively).
Patterns by background characteristics
� The percentage of women who recognise fever as a symptom of malaria is lowest in the Eastern Region (64%), and is highest in the Southern Region (75%).
� The percentage of women recognising fever as a symptom of malaria is lowest in Kono (50%) followed by Port Loko (54%), and is highest in Moyamba and Bombali (87%, and 85%, respectively).
� Knowledge of any of the symptoms of severe malaria is highest in women in Port Loko (99%), Koinadugu, Bombali, and Pujehun (98% in each) and is lowest in women in Western Area Urban (81%).
5.4 KNOWLEDGE OF MALARIA PREVENTION
Knowledge of malaria prevention Percentage of interviewed women who cite sleeping under a treated net as a way to avoid getting malaria Sample: Women age 15-49 who have heard of malaria
Nine in ten women who have heard of malaria cited sleeping under a treated net as a way of avoiding malaria. Seventeen percent of women also mentioned other effective ways of avoiding malaria, such as indoor residual spraying (IRS) and taking preventive medication. Nine percent of women mentioned ineffective malaria prevention methods such as burning leaves, not drinking dirty water, not eating bad food (immature sugarcane/leftover food), and not getting soaked with rain (Table 5.5).
Trends: The percentage of women who have heard of malaria who cited sleeping under a treated net as a way to avoid getting malaria increased from 50% in the 2013 SLMIS to 90% in the 2016 SLMIS.
Patterns by background characteristics
� The percentage of women reporting sleeping under treated nets as a way to avoid malaria does not vary much by background characteristics such as age, urban and rural residence, region, education, or household wealth quintile.
� The percentage of women in Kailahun recognising the use of a treated net as a means of preventing malaria is lowest among all of the districts (79%), followed by Port Loko (84%), compared with Kenema and Pujehun in which 95% of women mentioned sleeping under treated nets.
1 Confusion here means ‘altered consciousness’ as in the national treatment guidelines.
Figure 5.1 Trends in knowledge of symptoms, causes, and prevention of
malaria
96
64
91
50
98
69
94 90
Heard ofmalaria
Fever assymptom of
malaria
Mosquitobites ascause ofmalaria
Treatedmosquitonets as
prevention
Percentage of women
2013 SLMIS 2016 SLMIS

62 • Malaria Knowledge
5.5 KNOWLEDGE OF MALARIA TREATMENT
Knowledge of malaria treatment Percentage of interviewed women who mention ACT as a drug to treat malaria Sample: Women age 15-49 who have heard of malaria
Knowledge of malaria treatment is high among women in Sierra Leone regardless of their background characteristics. When women were asked what medicines are used to treat malaria, 85% mentioned ACT. Other responses included SP/Fansidar (12%), chloroquine (8%), and quinine (7%). Approximately 19% of women mentioned traditional medicine or herbs as treatment for malaria, and 15% mentioned aspirin, Panadol, or paracetamol. Only 4% of women did not know any treatments for malaria (Table 5.6).
Trends: The percentage of women who reported that an ACT can used to treat malaria increased from 69% in the 2013 SLMIS to 85% in the 2016 SLMIS.
Patterns by background characteristics
� Knowledge of ACT as a malaria treatment was lowest among the youngest and oldest age groups of women (79% among women age 15-19 and 77% among women age 45-49).
� The percentage of women who mentioned ACT as a malaria treatment ranged from a low of 71% in Port Loko to a high of 98% in Pujehun.
� There is little variation between women of different levels of education regarding knowledge on correct treatment of malaria, with 85% of least educated women and 87% of highest educated women (above secondary level) having correct knowledge on malaria treatment.
� There is little variation between women of different income levels in their knowledge of treatment of malaria; the percentage ranges from 79% of women in the lowest wealth quintile to 85% of women in the highest wealth quintile.
� Women in rural locations are more liable to mention traditional medicine or herbs as malaria treatment compared with women in urban locations (25% and 12%, respectively).
� The percentage of women who mentioned traditional medicine or herbs as a malaria treatment declined with increasing levels of education (24% of women with no education compared with 0% of women with more than secondary education). Similar patterns were seen for household wealth; 33% of women in the lowest wealth quintile mentioned traditional medicine or herbs as a malaria treatment compared with only 8% of those in the highest wealth quintile.
Figure 5.2 Knowledge of malaria treatment
7987 88 88 87 84
7785
15-19 20-24 25-29 30-34 35-39 40-44 45-49 Total
Percentage with knowledge of ACT as malaria treatment, by age

Malaria Knowledge • 63
5.6 CORRECT KNOWLEDGE OF MALARIA
Correct knowledge of malaria Percentage of interviewed women with complete composite knowledge of malaria Sample: Women age 15-49 who have heard of malaria
Correct knowledge of malaria is defined based on responses correctly identifying symptoms of malaria, preventive measures, and treatment, either alone or in combination with another response as defined in the notes in Table 5.7. Definitions are consistent with those used in the 2013 SLMIS2. The percentage of women with correct knowledge of malaria is high and does not vary greatly by background characteristics. Almost all women recognise the correct symptoms of malaria (99%), recognise the correct ways of preventing malaria (98%), and recognise the correct treatment of malaria (86%). The composite measure shows 85% of women with correct composite knowledge of malaria in all domains.
Trends: From the 2013 SLMIS to the 2016 SLMIS, the percentage of women who mentioned the correct knowledge of symptoms of malaria did not change (99%). The percentage who mentioned the correct knowledge of preventive measures increased from 87% to 98%, the percentage who mentioned correct knowledge of treatment increased from 72% to 86%, and those who had correct knowledge in all domains increased from 66% to 85%.
Patterns by background characteristics
� Correct knowledge of malaria was lowest among the youngest and oldest age groups of women (79% among women age 15-19 and 76% among women age 45-49 years).
� The percentage of women with correct knowledge of malaria ranged from a low of 72% in Port Loko to a high of 97% in Pujehun.
� The percentage of women with complete knowledge of malaria increased with increasing levels of education (84% of women with no education compared with 91% of women with more than secondary education). Similar patterns were seen for household wealth; 78% of women in the lowest wealth quintile compared with 87% of those in the highest wealth quintile had complete knowledge of malaria.
2 Correct knowledge of malaria includes responses of the following symptoms of malaria: fever, excessive sweating, feeling cold, headache, nausea/vomiting, diarrhoea, dizziness, loss of appetite, body ache/joint pain/body weakness, pale eyes, jaundice, dark urine, or anaemia. Correct knowledge of prevention includes responses of the following measures: a treated mosquito net/treated net/regular mosquito net, use mosquito repellent, avoid mosquito bites, take preventive medication, indoor residual spray (IRS), use mosquito coils, cut grass around house, eliminate stagnant water, keep surroundings clean, use mosquito screens on windows, use store-bought insect killer. This column excludes responses that mention burn leaves, don’t drink dirty water, don’t eat bad food (immature sugarcane/leftover food), and don’t get soaked in rain. Correct knowledge of treatment includes responses of ACT or quinine. Correct composite knowledge includes the correct responses for symptoms of malaria, preventative measures, and treatment according to the definitions specified above.
Figure 5.3 Trends in composite malaria knowledge
9987
72 66
99 9886 85
Correctknowledge of
symptoms
Correctknowledge of
prevention
Correctknowledge of
treatment
Correctcompositeknowledge
Percentage of women
2013 SLMIS 2016 SLMIS

64 • Malaria Knowledge
5.7 KNOWLEDGE OF SPECIFIC GROUPS MOST AFFECTED BY MALARIA
Specific groups most affected by malaria Percentage of interviewed women who indicated children under 5 and pregnant women as most likely to be affected by malaria Sample: Women age 15-49 who have heard of malaria
Nationally, 82% of all the women interviewed recognise that children are most affected by malaria, and 39% recognise that pregnant women are also most likely to be affected by malaria (Table 5.8). Twenty-three percent of women responded that anyone is likely to be affected, 22% mentioned adults, and 13% mentioned older adults.
Trends: In the 2013 SLMIS 78% of women interviewed mentioned children as the group most likely to be affected by malaria, and 43% mentioned pregnant women; this may be compared with 82% and 39%, respectively, in the 2016 SLMIS.
Patterns by background characteristics
� The percentage of women responding that children were most likely to be affected by malaria did not differ greatly by background characteristics.
� There are district-level variations in the percentage of women responding that children were most likely to be affected by malaria ranging from a low of 70% of women in Port Loko to a high of 91% of women in Moyamba and Kenema.
� Similarly, there are district-level variations in the percentage of women responding that pregnant women were most likely to be affected by malaria. These ranged from a low of 25% of women in Western Area Urban and 27% of women in Kailahun to a high of 64% of women in Kenema.
5.8 EXPOSURE TO MALARIA MESSAGES
Exposure to malaria messages Percentage of interviewed women who heard a message about malaria in the past 6 months Sample: Women age 15-49
Eighty-two percent of interviewed women reported seeing or hearing a message about malaria in the 6 months preceding the survey. When asked the source of malaria messages seen or heard in the past 6 months, 69% of interviewed women age 15-49 mentioned government hospitals/clinics, 71% mentioned sources accessed at the home3, 65% mentioned peer sources4, and 55% mentioned radio (Table 5.9). The less common sources are community meetings5 (35%), posters or billboards (26%), television (11%), newspapers (8%), and other unspecified sources (23%).
Trends: In the 2013 SLMIS, 99.6% of interviewed women heard a malaria message in the 6 months before the survey compared with 82% in the 2016 SLMIS. The percentage of women hearing malaria messages by radio declined from 70% in the 2013 SLMIS to 55% in the 2016 SLMIS.
3 Community health clubs, community health workers, at home, or from friends or family. 4 School health club or peer educators 5 Drama groups, community meetings, town criers, or faith/religious leaders

Malaria Knowledge • 65
Patterns by background characteristics
� The percentage of women seeing or hearing malaria messages is lowest in Southern Region (72%) and highest in the Northern Region (88%).
� At the district level, the percentage of women seeing or hearing malaria messages ranges from 59% in Bonthe to 95% or greater in Western Area Urban, Pujehun, and Tonkolili.
LIST OF TABLES
For detailed information on malaria, see the following tables:
� Table 5.1 General knowledge of malaria � Table 5.2 Knowledge of causes of malaria � Table 5.3 Knowledge of malaria symptoms � Table 5.4 Knowledge of symptoms of severe malaria � Table 5.5 Knowledge of ways to avoid malaria � Table 5.6 Knowledge of malaria treatment � Table 5.7 Correct knowledge of malaria � Table 5.8 Knowledge of specific groups most affected by malaria � Table 5.9 Media exposure to malaria messages
Figure 5.4 Source of malaria messages
6971
6835
2611
558
23
82
Government clinic/hospitalHomePeers
CommunityPosters or billboards
TVRadio
NewspaperAnywhere else
Any source
Percentage of women who saw or heard malaria messages in the past 6 months,
by source

66 • Malaria Knowledge
Table 5.1 General knowledge of malaria
Percentage of women age 15-49 who reported having heard of malaria, and of those who have heard of malaria, percentage who can recognise fever as a sign of malaria, percentage who reported mosquito bites as the cause of malaria, and percentage who reported that sleeping under a mosquito net can protect against malaria, by background characteristics, Sierra Leone MIS 2016
Background characteristic
Percentage of women who
have heard of malaria
Number of women
Percentage who recognise fever as a symptom of
malaria
Percentage who reported
mosquito bites as a cause of
malaria
Percentage who reported treated mosquito nets as
a prevention method
Number of women who
have heard of malaria
Age 15-19 95.9 1,665 68.8 92.8 88.1 1,598 20-24 97.7 1,658 69.9 94.0 91.1 1,620 25-29 97.7 1,705 68.9 94.3 92.4 1,666 30-34 99.1 1,218 70.6 94.9 89.3 1,206 35-39 97.2 1,208 69.5 93.4 87.9 1,174 40-44 98.4 608 67.9 93.4 87.4 598 45-49 98.2 439 66.8 90.2 87.1 431
Residence Urban 98.8 3,759 70.2 95.2 90.5 3,716 Rural 96.5 4,742 68.4 92.3 88.9 4,578
Region Eastern 97.1 1,936 64.4 90.4 86.5 1,880 Northern 98.4 2,884 69.8 93.1 90.3 2,838 Southern 94.9 1,736 75.3 96.3 92.7 1,647 Western 99.1 1,945 68.0 95.3 88.9 1,928
District Kailahun 95.4 670 68.3 87.4 79.2 639 Kenema 97.8 656 74.2 95.4 95.1 642 Kono 98.3 610 49.5 88.1 85.0 599 Bombali 98.2 732 84.9 95.3 96.3 718 Kambia 98.9 363 69.2 92.3 92.3 359 Koinadugu 96.9 434 72.7 92.6 87.0 420 Port Loko 98.3 617 53.5 91.6 84.4 606 Tonkolili 99.4 739 67.1 92.9 90.2 735 Bo 99.8 710 66.6 95.2 92.1 709 Bonthe 90.4 225 75.7 97.2 91.0 203 Moyamba 86.6 452 86.9 98.0 92.3 392 Pujehun 98.4 349 79.7 96.1 95.4 344 Western Area Rural 98.8 812 73.0 95.3 90.2 802 Western Area Urban 99.4 1,133 64.5 95.3 88.0 1,126
Education No education 97.1 4,393 68.7 92.7 88.6 4,267 Primary 96.1 1,173 65.0 90.9 87.9 1,128 Secondary 98.8 2,848 71.6 96.0 91.7 2,812 More than secondary 100.0 87 74.8 99.3 92.3 87
Wealth quintile Lowest 95.8 1,555 69.8 92.4 88.6 1,490 Second 97.1 1,591 65.9 91.9 87.8 1,546 Middle 97.1 1,604 70.1 91.9 88.1 1,558 Fourth 98.0 1,721 70.4 95.4 92.2 1,686 Highest 99.2 2,029 69.7 95.8 90.7 2,013
Total 97.6 8,501 69.2 93.6 89.6 8,293

Mal
aria
Kno
wle
dge
• 6
7
Tabl
e 5.
2 K
now
ledg
e of
cau
ses
of m
alar
ia
Am
ong
wom
en a
ge 1
5-49
, the
per
cent
age
who
cite
spe
cific
cau
ses
of m
alar
ia, a
ccor
ding
to b
ackg
roun
d ch
arac
teris
tics,
Sie
rra
Leon
e M
IS 2
016
K
now
ledg
e of
wha
t cau
ses
mal
aria
Bac
kgro
und
char
acte
ristic
M
osqu
ito
bite
s
Eat
ing
imm
atur
e su
gar
cane
E
atin
g co
ld fo
od
Eat
ing
dirty
food
Drin
king
be
er/p
alm
w
ine
Drin
king
di
rty w
ater
Get
ting
soak
ed
with
rain
Col
d or
ch
angi
ng
wea
ther
W
itchc
raft
Inje
ctio
ns/
drug
s
Eat
ing
oran
ges
or
man
gos
Eat
ing
plen
ty o
il
Sha
ring
razo
rs/
blad
es
Bed
bug
s
Dirt
y su
rrou
nd-
ings
O
ther
Any
m
isco
n-ce
ptio
n1 D
on’t
know
N
umbe
r of
wom
en
Age
15-1
9 92
.8
0.9
1.8
6.0
0.8
7.0
2.7
8.5
0.5
0.3
5.6
1.8
0.4
2.8
27.9
1.
3 49
.8
2.4
1,59
8 20
-24
94.0
0.
6 1.
2 4.
9 1.
2 6.
2 2.
6 8.
4 0.
3 0.
3 5.
4 1.
4 0.
4 1.
5 26
.6
0.8
45.1
0.
9 1,
620
25-2
9 94
.3
0.7
1.6
4.4
0.8
5.5
4.2
10.2
0.
5 0.
3 4.
5 2.
0 0.
2 2.
3 25
.1
1.2
44.9
0.
9 1,
666
30-3
4 94
.9
0.9
1.7
4.7
0.8
7.5
5.1
11.7
0.
8 0.
7 4.
8 1.
4 0.
2 2.
6 21
.9
2.5
47.2
1.
0 1,
206
35-3
9 93
.4
0.6
0.7
4.7
0.8
6.7
3.5
11.5
0.
4 0.
0 4.
9 1.
7 0.
0 3.
0 24
.0
1.9
46.2
1.
3 1,
174
40-4
4 93
.4
0.2
1.5
4.9
1.3
6.3
4.0
12.1
0.
6 0.
4 4.
5 1.
5 0.
3 4.
1 29
.5
0.5
51.7
2.
0 59
8 45
-49
90.2
0.
8 1.
5 6.
4 0.
8 7.
3 4.
5 13
.1
1.1
0.5
4.0
1.7
0.3
2.6
26.3
1.
9 50
.9
2.2
431
Res
iden
ce
U
rban
95
.2
0.5
1.2
4.7
0.6
6.8
2.6
5.0
0.3
0.1
5.3
2.3
0.2
1.1
30.5
1.
1 45
.9
1.1
3,71
6 R
ural
92
.3
0.9
1.7
5.3
1.2
6.3
4.5
14.4
0.
7 0.
5 4.
7 1.
1 0.
3 3.
7 21
.8
1.7
48.3
1.
7 4,
578
Reg
ion
E
aste
rn
90.4
0.
5 2.
1 5.
0 0.
2 7.
9 6.
6 16
.0
0.7
0.1
2.6
0.6
0.1
1.3
34.9
1.
9 57
.4
2.1
1,88
0 N
orth
ern
93
.1
1.0
1.6
5.8
1.9
5.7
3.6
13.1
0.
8 0.
7 6.
8 2.
0 0.
4 4.
4 18
.3
1.4
46.6
1.
5 2,
838
Sou
ther
n
96.3
0.
6 1.
1 4.
4 0.
5 6.
7 2.
9 6.
8 0.
3 0.
0 2.
5 0.
1 0.
3 2.
7 22
.5
1.8
40.8
0.
6 1,
647
Wes
tern
95
.3
0.5
0.9
4.4
0.5
6.3
1.6
3.2
0.1
0.2
6.7
3.6
0.1
0.8
30.3
0.
7 43
.6
1.3
1,92
8
Dis
tric
t
Kai
lahu
n 87
.4
1.2
1.7
3.6
0.3
7.1
5.1
16.9
1.
2 0.
3 2.
9 1.
4 0.
3 2.
0 16
.9
3.0
44.9
3.
3 63
9 K
enem
a 95
.4
0.1
1.8
2.5
0.4
5.3
3.7
13.4
0.
0 0.
0 2.
6 0.
0 0.
0 0.
3 58
.5
0.7
70.9
1.
2 64
2 K
ono
88.1
0.
1 2.
8 9.
2 0.
0 11
.4
11.3
18
.0
1.0
0.0
2.4
0.4
0.2
1.6
29.0
2.
0 56
.3
1.9
599
Bom
bali
95.3
1.
6 1.
8 5.
9 4.
2 5.
0 1.
7 7.
4 0.
2 0.
2 6.
7 1.
0 0.
0 2.
0 26
.4
0.4
48.0
1.
0 71
8 K
ambi
a 92
.3
0.4
0.6
7.2
1.4
3.8
4.2
14.5
1.
6 0.
0 1.
9 0.
0 0.
0 0.
6 10
.8
0.4
35.4
2.
0 35
9 K
oina
dugu
92
.6
0.2
2.8
7.0
0.3
6.7
2.6
25.1
1.
4 0.
0 7.
7 1.
4 0.
1 2.
1 15
.8
2.2
53.8
0.
7 42
0 P
ort L
oko
91.6
2.
0 1.
7 7.
8 1.
3 8.
6 2.
2 8.
0 1.
2 2.
6 9.
1 6.
7 1.
6 4.
7 19
.6
2.2
52.0
0.
9 60
6 To
nkol
ili 92
.9
0.4
1.3
2.8
1.1
4.6
6.7
15.4
0.
4 0.
5 6.
6 0.
3 0.
0 9.
7 14
.6
1.7
42.0
2.
6 73
5 B
o 95
.2
0.0
0.8
1.4
0.0
3.8
2.0
2.2
0.0
0.0
2.1
0.0
0.1
4.2
23.8
1.
8 35
.0
0.7
709
Bon
the
97.2
0.
9 1.
4 4.
5 1.
0 3.
9 0.
3 6.
6 0.
8 0.
0 1.
1 0.
0 2.
1 0.
5 8.
9 0.
0 26
.0
1.7
203
Moy
amba
98
.0
2.1
2.4
7.3
1.2
11.2
3.
8 2.
9 0.
0 0.
0 4.
6 0.
3 0.
1 0.
7 21
.3
0.0
46.7
0.
0 39
2 P
ujeh
un
96.1
0.
0 0.
2 7.
4 0.
5 9.
3 5.
4 20
.8
1.1
0.0
1.5
0.0
0.0
3.2
29.2
4.
8 54
.9
0.4
344
Wes
tern
Are
a R
ural
95
.3
0.6
0.6
4.9
0.6
5.0
2.9
4.6
0.2
0.4
7.0
0.7
0.2
0.3
26.2
0.
7 41
.7
1.0
802
Wes
tern
Are
a U
rban
95
.3
0.5
1.0
4.1
0.4
7.2
0.6
2.2
0.0
0.0
6.6
5.7
0.0
1.2
33.2
0.
8 45
.0
1.4
1,12
6
Educ
atio
n
No
educ
atio
n 92
.7
0.8
1.5
4.9
1.2
6.7
4.6
12.8
0.
9 0.
4 5.
7 1.
4 0.
3 3.
1 21
.9
1.5
47.2
1.
7 4,
267
Prim
ary
90.9
0.
9 1.
7 5.
1 1.
0 5.
9 3.
7 11
.4
0.4
0.7
4.0
1.8
0.4
2.8
23.4
1.
8 47
.3
1.3
1,12
8 S
econ
dary
96
.0
0.6
1.2
4.9
0.5
6.3
2.3
6.1
0.1
0.1
4.2
2.0
0.2
1.5
31.8
1.
2 47
.0
1.1
2,81
2 M
ore
than
sec
onda
ry
99.3
0.
0 2.
1 12
.1
2.1
15.8
0.
0 0.
7 0.
0 0.
0 3.
0 0.
0 0.
0 5.
8 43
.1
0.0
50.6
0.
0 87
Wea
lth q
uint
ile
Lo
wes
t 92
.4
1.0
2.4
5.5
1.5
6.9
4.8
16.6
0.
9 0.
5 4.
4 0.
9 0.
3 4.
1 16
.7
1.8
47.2
1.
7 1,
490
Sec
ond
91.9
0.
5 1.
9 5.
2 1.
1 6.
7 5.
7 15
.5
0.6
0.5
5.8
1.3
0.4
3.8
21.5
2.
1 49
.6
1.5
1,54
6 M
iddl
e 91
.9
1.1
1.1
5.1
1.1
5.3
3.8
11.1
0.
7 0.
3 4.
1 0.
8 0.
2 3.
0 24
.6
1.8
47.1
1.
9 1,
558
Four
th
95.4
0.
3 1.
1 5.
6 0.
8 7.
3 2.
8 7.
5 0.
5 0.
3 4.
7 1.
4 0.
4 1.
5 28
.7
0.7
46.4
0.
8 1,
686
Hig
hest
95
.8
0.7
1.0
4.0
0.3
6.5
1.7
3.0
0.0
0.0
5.5
3.4
0.1
0.8
34.0
1.
0 46
.1
1.2
2,01
3
Tota
l 93
.6
0.7
1.5
5.0
0.9
6.5
3.6
10.2
0.
5 0.
3 5.
0 1.
7 0.
2 2.
5 25
.7
1.4
47.2
1.
4 8,
293
1 Exc
lude
s m
osqu
ito b
ites
and
don’
t kno
w

68 •
Mal
aria
Kno
wle
dge
Tabl
e 5.
3 K
now
ledg
e of
mal
aria
sym
ptom
s
Am
ong
wom
en w
ho h
ave
ever
hea
rd o
f mal
aria
, per
cent
age
of w
omen
age
15-
49 w
ho k
now
var
ious
sym
ptom
s of
mal
aria
, by
back
grou
nd c
hara
cter
istic
s, S
ierr
a Le
one
MIS
201
6
K
now
ledg
e of
mal
aria
sym
ptom
s
Bac
kgro
und
char
acte
ristic
Fe
ver
Exc
essi
ve
swea
ting
Feel
ing
cold
H
eada
che
Nau
sea
and
vom
iting
D
iarr
hoea
D
izzi
ness
Lo
ss o
f ap
petit
e
Bod
y ac
he o
r jo
int p
ain
Pal
e ey
es
Bod
y w
eakn
ess
Ref
usin
g to
eat
or
drin
k Ja
undi
ce
Dar
k ur
ine
Ana
emia
O
ther
D
on’t
know
N
umbe
r of
wom
en
Age
15
-19
68.8
11
.6
40.6
31
.9
21.4
4.
4 12
.9
27.4
23
.0
18.6
26
.7
1.1
3.9
11.5
1.
9 0.
9 1.
0 1,
598
20-2
4 69
.9
16.5
43
.0
29.7
23
.3
3.7
15.4
31
.5
25.9
15
.5
30.3
0.
9 2.
8 8.
5 1.
4 1.
1 0.
5 1,
620
25-2
9 68
.9
16.1
37
.7
24.9
18
.5
3.9
16.2
33
.9
28.5
16
.9
29.9
1.
1 2.
9 8.
1 2.
2 0.
7 0.
7 1,
666
30-3
4 70
.6
14.2
40
.5
27.3
20
.2
4.6
15.6
35
.3
31.1
17
.7
29.2
0.
7 3.
9 8.
1 1.
8 0.
8 1.
1 1,
206
35-3
9 69
.5
16.8
42
.9
26.3
20
.6
2.7
16.6
37
.9
30.2
15
.8
31.3
1.
0 2.
6 7.
2 2.
1 1.
6 0.
4 1,
174
40-4
4 67
.9
17.8
44
.1
35.2
19
.9
2.2
15.2
32
.8
34.2
18
.9
30.0
2.
0 2.
6 7.
8 1.
8 1.
8 0.
7 59
8 45
-49
66.8
13
.2
48.3
31
.3
18.5
4.
4 15
.9
32.3
28
.3
18.5
31
.5
1.8
2.1
7.3
3.2
1.3
0.2
431
Res
iden
ce
Urb
an
70.2
11
.8
34.6
31
.1
23.3
3.
3 17
.9
38.9
31
.1
14.4
32
.7
0.5
3.1
8.7
1.3
0.6
0.3
3,71
6 R
ural
68
.4
17.8
47
.0
27.0
18
.5
4.2
13.1
27
.9
25.5
19
.3
27.0
1.
6 3.
2 8.
6 2.
5 1.
4 1.
0 4,
578
Reg
ion
Eas
tern
64
.4
13.3
47
.4
26.0
17
.7
3.3
16.6
34
.1
26.5
17
.9
37.2
0.
2 4.
2 7.
5 1.
9 2.
0 1.
7 1,
880
Nor
ther
n
69.8
20
.4
42.5
27
.6
22.9
4.
7 12
.7
30.6
27
.3
18.9
24
.0
2.7
3.1
9.9
2.8
1.0
0.5
2,83
8 S
outh
ern
75
.3
15.0
49
.5
29.4
15
.4
3.4
13.9
22
.7
21.2
18
.3
24.7
0.
3 2.
3 7.
1 1.
6 1.
2 0.
3 1,
647
Wes
tern
68
.0
9.2
27.1
32
.9
24.8
3.
4 19
.0
43.4
36
.2
12.7
34
.5
0.2
2.8
9.3
0.9
0.3
0.4
1,92
8
Dis
tric
t
K
aila
hun
68.3
6.
0 39
.2
20.5
6.
3 4.
5 19
.0
25.3
11
.5
11.0
33
.0
0.2
0.7
2.9
2.5
1.0
1.7
639
Ken
ema
74.2
26
.5
64.8
44
.1
28.6
2.
2 21
.1
49.9
47
.6
17.3
39
.9
0.0
1.9
8.4
1.5
0.8
0.7
642
Kon
o 49
.5
6.7
37.7
12
.3
18.1
3.
0 9.
3 26
.8
20.0
25
.8
38.8
0.
5 10
.4
11.5
1.
9 4.
3 2.
8 59
9 B
omba
li 84
.9
8.6
34.4
31
.5
28.3
6.
4 12
.0
25.8
15
.0
14.8
21
.9
0.5
2.7
7.2
3.0
1.0
0.1
718
Kam
bia
69.2
21
.8
37.2
25
.6
34.3
2.
7 16
.5
35.0
44
.0
21.4
20
.7
0.7
0.5
5.0
1.0
0.4
1.1
359
Koi
nadu
gu
72.7
17
.0
43.4
15
.0
11.2
4.
3 2.
2 17
.5
18.9
8.
9 35
.1
0.0
3.7
10.0
2.
6 0.
4 0.
4 42
0 P
ort L
oko
53.5
16
.5
38.5
31
.4
16.6
4.
0 15
.6
33.7
24
.7
20.2
21
.5
2.1
2.2
7.3
2.2
0.2
0.4
606
Tonk
olili
67.1
36
.3
55.9
28
.8
24.0
4.
7 15
.1
37.9
38
.0
26.4
23
.3
7.9
5.4
16.8
4.
1 2.
1 0.
7 73
5 B
o 66
.6
20.5
54
.8
32.1
13
.5
0.3
13.7
19
.3
22.6
14
.0
26.6
0.
4 0.
9 4.
5 0.
9 0.
4 0.
5 70
9 B
onth
e 75
.7
13.1
39
.6
26.8
20
.7
12.0
19
.7
19.1
12
.6
15.8
18
.4
1.0
4.5
8.6
0.7
0.6
0.7
203
Moy
amba
86
.9
14.1
55
.4
36.2
14
.8
3.9
7.5
28.3
23
.3
15.9
24
.1
0.2
2.1
3.2
1.2
0.0
0.0
392
Puj
ehun
79
.7
6.0
37.6
17
.7
16.8
4.
1 18
.0
25.2
21
.0
31.7
25
.1
0.1
4.0
16.0
4.
3 4.
5 0.
0 34
4 W
este
rn A
rea
Rur
al
73.0
10
.2
26.0
32
.4
24.5
5.
6 18
.6
41.2
31
.4
18.2
32
.3
0.1
3.1
12.5
1.
4 0.
5 0.
0 80
2 W
este
rn A
rea
Urb
an
64.5
8.
5 27
.9
33.3
24
.9
1.8
19.3
45
.0
39.6
8.
8 36
.0
0.3
2.6
7.0
0.6
0.1
0.6
1,12
6
Educ
atio
n
N
o ed
ucat
ion
68.7
17
.1
44.8
27
.3
19.0
3.
7 14
.2
31.2
28
.5
16.3
27
.0
1.3
2.5
7.1
1.9
1.1
0.8
4,26
7 P
rimar
y 65
.0
12.1
39
.6
25.9
17
.3
4.4
14.1
27
.8
21.3
20
.1
27.3
1.
1 2.
8 8.
2 2.
4 1.
8 1.
0 1,
128
Sec
onda
ry
71.6
13
.3
37.5
32
.1
24.5
3.
8 17
.2
37.1
29
.3
17.1
34
.5
0.8
4.3
10.9
1.
8 0.
7 0.
5 2,
812
Mor
e th
an s
econ
dary
74
.8
17.1
28
.6
36.5
25
.6
0.0
24.7
38
.2
44.3
23
.7
24.7
0.
0 4.
3 16
.2
1.2
0.0
0.0
87
Wea
lth q
uint
ile
Low
est
69.8
18
.0
45.7
26
.0
15.7
4.
4 11
.9
25.7
23
.5
17.0
24
.7
1.8
2.9
7.3
2.5
1.0
1.1
1,49
0 S
econ
d 65
.9
18.8
48
.5
26.2
19
.6
4.3
14.5
28
.6
27.0
19
.0
27.2
1.
7 2.
8 10
.3
2.4
1.2
0.9
1,54
6 M
iddl
e 70
.1
15.8
44
.7
27.1
19
.5
4.3
13.7
28
.7
26.7
20
.6
29.6
1.
5 3.
4 9.
0 2.
3 1.
7 0.
9 1,
558
Four
th
70.4
13
.5
38.1
29
.4
21.4
3.
9 16
.0
36.5
25
.4
18.0
30
.2
0.6
4.0
8.0
1.7
1.1
0.3
1,68
6 H
ighe
st
69.7
10
.9
33.1
33
.7
25.4
2.
5 18
.9
41.4
35
.2
12.4
34
.3
0.2
2.6
8.6
1.0
0.5
0.5
2,01
3
Tota
l 69
.2
15.1
41
.4
28.8
20
.7
3.8
15.3
32
.8
28.0
17
.1
29.5
1.
1 3.
1 8.
6 1.
9 1.
1 0.
7 8,
293

Malaria Knowledge • 69
Table 5.4 Knowledge of symptoms of severe malaria
Among women who have ever heard of malaria, percentage of women age 15-49 who know various symptoms of severe malaria, by background characteristics, Sierra Leone MIS 2016
Knowledge of malaria symptoms among women who have heard of malaria, percentage who cite specific symptoms of severe malaria
Background characteristic
At least one
symptom1
Shivering/ shaking/
convulsion Vomiting
everything Confusion Low blood (anaemia)
Difficulty breathing Dizziness Jaundice Other Don’t know
Number of women
Age 15-19 91.1 37.8 44.7 10.5 27.8 4.8 19.6 26.0 3.0 7.9 1,598 20-24 90.0 35.5 42.9 12.0 25.6 5.3 19.2 27.7 4.2 8.5 1,620 25-29 90.1 35.9 41.8 8.9 27.6 5.3 18.9 26.5 3.9 8.3 1,666 30-34 92.8 37.0 37.1 11.1 31.7 4.9 19.9 31.0 2.7 6.3 1,206 35-39 94.2 40.0 42.4 10.3 31.3 5.2 18.6 30.8 3.1 4.8 1,174 40-44 95.0 40.6 44.4 12.5 30.8 7.3 18.7 24.9 5.2 3.9 598 45-49 93.9 41.9 39.4 9.5 31.1 5.3 21.0 26.5 5.2 4.1 431
Residence Urban 89.4 33.2 39.5 10.4 22.8 4.5 18.4 30.4 3.4 9.1 3,716 Rural 93.8 41.1 44.1 10.8 33.6 5.9 20.0 25.6 3.9 5.2 4,578
Region Eastern 89.6 41.4 46.8 10.2 34.7 5.6 26.6 28.1 9.3 6.2 1,880 Northern 96.3 40.4 43.6 10.8 37.9 8.4 19.7 26.3 1.7 3.4 2,838 Southern 93.8 41.3 48.7 12.9 21.8 3.2 15.9 23.1 2.5 5.6 1,647 Western 85.7 26.5 29.4 8.9 15.5 2.2 14.4 33.6 2.1 14.0 1,928
District Kailahun 90.7 38.6 40.8 9.9 31.3 2.9 23.2 12.1 12.1 3.5 639 Kenema 90.8 56.2 55.9 16.0 47.9 9.8 32.7 37.5 3.3 8.6 642 Kono 87.2 28.4 43.6 4.4 24.3 4.0 23.7 35.1 12.8 6.4 599 Bombali 98.3 44.7 48.2 11.0 35.3 2.8 14.3 26.4 0.7 1.7 718 Kambia 95.9 38.6 51.9 8.0 32.5 1.8 24.9 22.4 3.8 3.5 359 Koinadugu 97.6 43.2 34.0 9.0 27.2 5.4 19.1 21.3 2.4 1.7 420 Port Loko 98.7 29.0 46.4 10.0 37.1 18.6 28.7 19.5 0.6 1.0 606 Tonkolili 92.0 44.8 38.3 13.5 49.8 10.5 15.6 36.6 2.0 8.0 735 Bo 92.1 23.8 46.1 13.1 16.3 4.9 17.8 21.8 1.7 7.1 709 Bonthe 92.9 48.2 50.4 3.0 9.6 2.7 16.9 38.2 2.8 5.6 203 Moyamba 93.8 62.1 56.5 23.9 26.2 2.3 9.1 9.7 0.0 6.2 392 Pujehun 97.7 49.8 44.1 6.1 35.5 0.8 19.1 32.2 6.7 2.0 344 Western Area Rural 92.3 41.1 29.9 5.2 18.2 1.6 20.3 30.1 2.3 7.6 802 Western Area Urban 80.9 16.1 28.9 11.5 13.5 2.6 10.1 36.1 2.0 18.5 1,126
Education No education 92.3 40.4 41.8 10.5 29.7 5.5 18.9 25.9 3.0 6.7 4,267 Primary 91.0 34.7 43.0 10.8 28.7 4.6 19.7 25.1 5.4 6.5 1,128 Secondary 91.4 34.2 42.4 10.5 27.1 5.2 19.5 31.4 4.0 7.5 2,812 More than secondary 92.7 44.0 32.6 18.6 36.5 6.9 25.6 37.3 0.0 7.3 87
Wealth quintile Lowest 93.0 41.5 44.7 10.2 31.1 5.9 18.7 22.5 3.9 5.5 1,490 Second 94.2 41.3 43.9 9.6 36.3 5.3 21.6 26.5 4.1 4.7 1,546 Middle 93.3 40.5 43.5 12.8 32.1 6.6 20.8 27.9 4.9 5.1 1,558 Fourth 93.6 40.1 42.9 10.4 27.9 5.3 20.7 27.4 3.3 4.9 1,686 Highest 86.5 27.4 36.8 10.3 19.5 3.7 15.6 32.9 2.4 12.9 2,013
Total 91.8 37.6 42.0 10.6 28.8 5.3 19.3 27.8 3.7 6.9 8,293 1 Respondent had heard of malaria and cited shivering/shaking/convulsion, vomiting everything, confusion, low blood (anaemia), difficulty breathing, dizziness, and/or jaundice as a symptom of severe malaria.

70 • Malaria Knowledge
Table 5.5 Knowledge of ways to avoid malaria
Among women age 15-49 who have ever heard of malaria, the percentage of women who cite specific ways to avoid getting malaria, according to background characteristics, Sierra Leone MIS 2016
Background characteristic
Sleep under a treated
net
Use mosqui-
to repel-lent
Avoid mosqui-to bites
Take pre-
ventive medica-
tion
Indoor residual spray (IRS)
Use mosqui-to coils
Cut the grass
around the
house
Elimi-nate stag-nant water
Keep sur-
round-ings
clean Cut the grass
Use mosqui-
to screens on the win-dows
Store bought insect killer
Miscon-cep-tions1 Other
Don’t know
Number of
women
Age 15-19 88.1 5.0 15.6 15.6 2.6 12.0 10.3 14.8 42.7 4.9 0.6 0.0 7.7 1.7 1.0 1,598 20-24 91.1 4.6 14.7 15.0 1.8 13.8 9.7 12.2 43.4 5.6 0.7 0.1 7.8 1.0 1.1 1,620 25-29 92.4 4.0 17.4 11.9 2.8 15.3 8.5 13.4 42.3 5.5 0.6 0.0 8.4 1.5 0.8 1,666 30-34 89.3 3.5 18.8 15.4 2.1 12.8 8.1 14.4 45.6 5.5 0.2 0.0 8.1 1.1 1.7 1,206 35-39 87.9 4.6 17.4 16.7 2.4 12.4 8.7 14.6 45.0 5.9 0.5 0.8 8.9 1.5 1.3 1,174 40-44 87.4 4.1 22.3 13.6 2.8 13.8 11.8 17.5 45.6 8.7 0.4 0.0 10.5 1.9 1.8 598 45-49 87.1 3.9 18.9 13.0 4.4 10.7 7.3 14.0 42.9 4.7 0.3 0.0 11.7 2.7 2.2 431
Residence Urban 90.5 5.1 14.3 15.5 4.0 17.2 7.2 14.3 49.3 5.9 0.9 0.1 7.5 1.3 1.0 3,716 Rural 88.9 3.7 19.5 13.8 1.3 10.0 10.9 13.9 39.2 5.5 0.2 0.1 9.2 1.6 1.5 4,578
Region Eastern 86.5 6.1 27.6 11.2 1.7 7.6 14.3 25.6 49.5 12.9 0.3 0.3 14.8 2.3 2.1 1,880 Northern 90.3 3.3 17.4 17.8 2.2 13.9 7.6 11.3 39.4 4.1 0.2 0.0 9.0 0.8 1.0 2,838 Southern 92.7 4.2 13.4 11.9 1.6 7.5 11.3 9.6 39.2 2.4 0.1 0.0 3.0 1.7 0.7 1,647 Western 88.9 4.3 9.8 15.5 4.4 22.7 4.8 10.9 48.3 3.6 1.6 0.2 6.3 1.4 1.4 1,928
District Kailahun 79.2 8.5 16.1 10.0 0.6 4.1 6.0 20.9 40.4 5.3 0.3 0.0 7.6 2.1 3.5 639 Kenema 95.1 7.9 48.3 13.5 3.0 15.2 32.1 36.4 62.2 29.7 0.5 0.0 24.8 0.6 0.9 642 Kono 85.0 1.5 17.9 10.1 1.6 3.2 4.1 18.9 45.6 3.0 0.2 0.9 11.6 4.4 1.7 599 Bombali 96.3 3.3 3.8 9.1 1.7 8.5 1.5 7.4 57.0 1.1 0.4 0.0 8.1 0.3 0.9 718 Kambia 92.3 1.7 20.4 6.2 1.6 10.7 15.4 10.1 36.7 10.0 0.1 0.0 10.1 0.5 0.3 359 Koinadugu 87.0 4.2 18.7 19.4 0.4 2.3 3.8 8.9 43.0 1.5 0.0 0.0 9.3 0.6 1.1 420 Port Loko 84.4 2.4 28.3 16.6 4.0 21.1 9.5 12.0 22.3 5.1 0.2 0.2 9.0 0.7 0.8 606 Tonkolili 90.2 4.3 19.4 31.9 2.5 21.4 10.4 16.4 35.6 4.9 0.1 0.0 9.4 1.5 1.6 735 Bo 92.1 1.1 12.8 6.7 2.4 8.3 3.1 4.7 38.5 2.3 0.0 0.0 2.5 2.1 0.9 709 Bonthe 91.0 2.8 8.1 15.8 1.4 10.6 22.5 12.3 28.4 0.9 0.2 0.0 2.1 0.7 1.7 203 Moyamba 92.3 13.1 20.8 20.3 1.4 8.6 9.1 8.1 40.4 0.9 0.3 0.0 1.0 0.0 0.1 392 Pujehun 95.4 1.4 9.5 10.7 0.4 2.9 23.9 19.6 45.6 5.1 0.2 0.0 6.7 3.5 0.2 344 Western Area Rural 90.2 3.7 11.7 10.1 2.2 28.1 7.4 16.0 43.6 5.4 2.5 0.4 7.5 1.3 1.8 802 Western Area Urban 88.0 4.7 8.5 19.3 6.0 18.8 2.9 7.3 51.6 2.3 0.9 0.2 5.4 1.5 1.0 1,126
Education No education 88.6 3.4 18.3 13.5 1.4 12.7 10.5 13.6 39.8 6.5 0.5 0.1 9.5 1.3 1.7 4,267 Primary 87.9 4.0 17.3 12.6 2.2 12.0 8.3 12.6 39.8 5.0 0.1 0.5 7.6 1.6 1.4 1,128 Secondary 91.7 5.7 15.6 16.6 4.0 14.5 7.6 15.7 50.7 4.6 0.8 0.0 7.4 1.6 0.6 2,812 More than secondary 92.3 8.9 11.9 28.1 12.5 14.8 6.3 7.4 62.0 5.7 0.0 2.9 3.1 2.0 0.7 87
Wealth quintile Lowest 88.6 4.0 18.1 14.8 1.0 8.8 11.2 12.5 35.4 4.5 0.1 0.2 8.5 1.4 2.1 1,490 Second 87.8 3.0 19.8 14.2 1.3 10.8 10.4 14.5 41.7 6.2 0.3 0.1 10.0 1.7 1.5 1,546 Middle 88.1 4.8 20.3 14.5 1.5 10.1 10.9 15.0 40.7 7.9 0.3 0.2 10.2 1.8 1.1 1,558 Fourth 92.2 4.2 16.7 11.8 2.2 15.8 9.8 16.2 45.7 5.8 0.9 0.0 8.0 1.4 1.1 1,686 Highest 90.7 5.3 12.4 17.2 5.5 18.7 5.1 12.6 52.1 4.3 0.9 0.2 6.3 1.1 0.8 2,013
Total 89.6 4.3 17.2 14.6 2.5 13.2 9.2 14.1 43.7 5.7 0.5 0.1 8.5 1.5 1.3 8,293 1 Respondent had heard of malaria and cited burn leaves, don’t drink dirty water, don’t eat bad food (immature sugarcane/leftover food), and/or don’t get soaked with rain as ways to avoid malaria.

Malaria Knowledge • 71
Table 5.6 Knowledge of malaria treatment
Among women aged 15-49 who have heard of malaria, the percentage who cite specific various drugs to treat malaria, according to background characteristics, Sierra Leone MIS 2016
Background characteristic
ACT (AS+AQ and AL) Chloroquine SP/Fansidar Quinine
Aspirin/ Panadol/
paracetamol
Traditional medicine/
herbs Other Don’t know Number of
women
Age 15-19 78.8 8.4 9.2 7.2 15.2 17.3 1.8 7.9 1,598 20-24 87.0 6.7 13.1 7.3 13.9 16.2 1.3 2.7 1,620 25-29 87.7 8.6 13.8 4.9 13.8 19.2 1.6 2.6 1,666 30-34 87.9 8.6 14.9 6.3 16.5 17.2 0.8 2.6 1,206 35-39 87.1 9.3 13.1 5.8 14.6 22.1 2.1 2.5 1,174 40-44 83.9 7.9 10.1 10.1 14.2 25.6 2.2 2.6 598 45-49 76.6 9.6 10.3 6.2 13.9 30.4 2.3 4.7 431
Residence Urban 86.2 10.5 14.4 8.6 15.0 12.2 2.0 3.9 3,716 Rural 83.9 6.5 10.8 4.9 14.3 25.2 1.4 3.6 4,578
Region Eastern 85.8 12.4 11.8 12.8 13.7 15.4 1.9 5.7 1,880 Northern 82.3 6.8 10.5 3.1 17.6 29.6 1.8 2.0 2,838 Southern 87.3 5.5 12.9 4.0 10.9 14.8 1.6 3.6 1,647 Western 86.0 9.0 15.4 7.8 14.4 12.2 1.2 4.4 1,928
District Kailahun 80.7 9.6 4.8 4.3 10.5 17.3 1.9 6.3 639 Kenema 96.7 15.7 14.8 30.0 16.8 11.4 0.8 1.8 642 Kono 79.5 11.8 16.1 3.4 13.8 17.7 3.0 9.3 599 Bombali 91.6 6.3 12.2 5.7 26.9 16.0 3.2 1.7 718 Kambia 76.2 4.6 9.1 4.2 12.3 23.1 2.0 1.9 359 Koinadugu 85.5 6.4 3.7 1.7 17.3 32.4 2.4 1.0 420 Port Loko 71.0 10.9 13.5 1.9 17.0 35.2 0.4 4.4 606 Tonkolili 83.6 5.1 10.9 1.9 11.7 40.0 1.2 1.0 735 Bo 82.3 4.8 6.9 3.8 14.2 16.9 2.5 7.3 709 Bonthe 82.9 10.0 14.4 10.4 11.5 17.8 0.0 2.7 203 Moyamba 89.5 7.0 19.9 3.7 5.2 18.4 0.0 0.3 392 Pujehun 97.6 2.5 16.6 0.9 10.2 4.7 2.3 0.4 344 Western Area Rural 89.9 6.7 4.2 4.9 17.3 19.4 0.8 3.9 802 Western Area Urban 83.3 10.7 23.3 9.9 12.3 7.0 1.5 4.8 1,126
Education No education 85.0 8.0 10.9 5.4 15.5 24.2 1.0 3.2 4,267 Primary 82.7 6.1 11.9 3.3 14.4 21.9 2.5 4.5 1,128 Secondary 85.7 9.5 14.8 9.5 13.4 11.8 2.3 4.4 2,812 More than secondary 87.1 10.2 14.1 12.6 15.2 0.0 2.0 1.4 87
Wealth quintile Lowest 79.4 5.8 10.2 3.8 15.3 32.8 1.5 2.8 1,490 Second 85.4 7.2 10.4 4.7 15.2 25.2 1.1 3.2 1,546 Middle 86.7 8.1 10.1 6.5 12.1 19.3 1.9 3.6 1,558 Fourth 87.6 8.7 12.1 6.9 17.0 16.2 1.1 3.7 1,686 Highest 85.1 10.8 17.6 9.9 13.7 7.7 2.4 5.0 2,013
Total 84.9 8.3 12.4 6.6 14.6 19.4 1.6 3.7 8,293

72 • Malaria Knowledge
Table 5.7 Correct knowledge of malaria
Percentage of women age 15-49 who have heard of malaria and have correct knowledge of malaria indicators, by background characteristics, Sierra Leone MIS 2016
Knowledge of indicators
Background characteristic
Correct knowledge of symptoms of
malaria1
Correct knowledge of preventative measures2
Correct knowledge of treatments3
Correct knowledge in all
domains4 Number of
women
Age 15-19 98.9 97.6 80.1 79.0 1,598 20-24 99.5 98.1 88.2 86.8 1,620 25-29 99.3 98.0 88.6 87.3 1,666 30-34 98.8 97.6 88.4 86.8 1,206 35-39 99.6 97.4 88.2 86.6 1,174 40-44 99.3 97.4 85.0 83.5 598 45-49 99.8 96.3 78.1 76.0 431
Residence Urban 99.6 98.3 87.7 86.6 3,716 Rural 98.9 97.2 84.6 82.9 4,578
Region Eastern 98.2 96.1 86.4 84.1 1,880 Northern 99.5 98.2 83.2 81.9 2,838 Southern 99.7 98.7 88.4 87.3 1,647 Western 99.6 97.6 87.7 86.6 1,928
District Kailahun 98.1 93.7 81.8 79.1 639 Kenema 99.3 99.1 97.1 95.9 642 Kono 97.1 95.4 79.8 76.9 599 Bombali 99.9 98.2 92.4 90.8 718 Kambia 98.9 99.0 77.7 76.4 359 Koinadugu 99.6 97.3 86.3 84.4 420 Port Loko 99.6 98.9 72.1 71.8 606 Tonkolili 99.3 97.5 84.0 83.0 735 Bo 99.5 98.2 84.5 82.9 709 Bonthe 99.3 97.6 83.7 82.3 203 Moyamba 100.0 99.9 89.8 89.7 392 Pujehun 100.0 98.8 97.6 96.5 344 Western Area Rural 100.0 97.7 90.7 88.8 802 Western Area Urban 99.4 97.6 85.6 85.1 1,126
Education No education 99.2 97.1 85.7 83.8 4,267 Primary 98.9 97.4 83.4 82.1 1,128 Secondary 99.5 98.5 87.3 86.5 2,812 More than secondary 100.0 99.3 91.3 90.6 87
Wealth quintile Lowest 98.9 96.8 80.2 78.3 1,490 Second 99.0 97.2 86.1 84.7 1,546 Middle 99.1 97.5 87.4 85.5 1,558 Fourth 99.7 98.1 88.3 86.7 1,686 Highest 99.5 98.4 87.1 86.7 2,013
Total 99.3 97.7 86.0 84.6 8,293 1 Includes responses for women who mention the following symptoms of malaria: fever, excessive sweating, feeling cold, headache, nausea and vomiting, diarrhoea, dizziness, loss of appetite, body ache or joint pain, pale eyes, body weakness, refusing to eat or drink, jaundice, dark urine, or anaemia. 2 Includes responses for women who mention a treated mosquito net/treated net, use mosquito repellent, avoid mosquito bites, take preventive medication, indoor residual spray (IRS), use mosquito coils, cut grass around house, eliminate stagnant water, keep surroundings clean, use mosquito screens on windows, use store-bought insect killer. This column excludes responses that mention burn leaves, don’t drink dirty water, don’t eat bad food (immature sugarcane/leftover food), and don’t get soaked in rain. 3 Includes responses for women who mention ACT or quinine. 4 Includes responses for women who mention the correct responses for symptoms of malaria, preventive measures, and treatment.

Malaria Knowledge • 73
Table 5.8 Knowledge of specific groups most affected by malaria
Among women age 15-49 who have heard of malaria, the percentage who cite specific groups most likely to be affected by malaria, according to background characteristics, Sierra Leone MIS 2016
Background characteristic Children Adults
Pregnant woman Older adults Anyone Other Don’t know
Number of women
Age 15-19 78.8 23.3 35.3 11.6 26.8 2.0 1.2 1,598 20-24 82.9 21.6 41.7 15.0 21.6 1.6 1.1 1,620 25-29 83.2 20.2 39.0 11.3 21.5 2.0 1.5 1,666 30-34 83.9 20.3 42.2 12.1 20.7 1.8 1.2 1,206 35-39 82.9 23.2 36.8 11.9 22.8 2.9 1.6 1,174 40-44 80.4 20.3 37.2 14.2 23.5 2.1 1.4 598 45-49 82.9 21.3 40.4 13.2 22.7 2.4 2.0 431
Residence Urban 83.1 20.1 36.5 14.3 23.1 1.9 1.0 3,716 Rural 81.4 22.7 40.8 11.2 22.6 2.2 1.6 4,578
Region Eastern 85.4 26.3 40.4 14.9 15.8 3.8 2.4 1,880 Northern 79.8 19.9 41.8 12.2 25.3 1.8 1.3 2,838 Southern 84.7 27.7 42.2 8.5 21.5 1.3 1.1 1,647 Western 80.3 14.1 30.4 14.4 27.2 1.3 0.7 1,928
District Kailahun 78.2 12.4 27.1 9.8 14.4 3.9 1.9 639 Kenema 90.8 52.8 63.5 22.4 11.2 2.7 2.7 642 Kono 87.3 12.9 29.9 12.3 22.0 4.8 2.8 599 Bombali 87.9 24.4 49.5 12.4 15.7 2.3 2.0 718 Kambia 72.3 15.0 47.6 12.7 34.8 1.7 1.7 359 Koinadugu 79.4 12.5 30.0 8.0 23.9 0.7 0.6 420 Port Loko 69.9 14.0 46.4 13.9 22.5 0.7 0.7 606 Tonkolili 83.8 27.0 34.3 12.8 33.0 2.8 1.4 735 Bo 81.4 36.6 38.0 7.6 26.8 1.0 0.9 709 Bonthe 86.3 20.0 33.3 20.4 4.9 5.0 4.5 203 Moyamba 91.3 22.7 52.0 6.1 10.3 0.2 0.2 392 Pujehun 83.3 19.8 44.9 5.8 33.3 0.9 0.4 344 Western Area Rural 71.5 11.4 37.8 5.9 30.4 0.6 0.5 802 Western Area Urban 86.5 16.1 25.1 20.5 24.9 1.9 0.8 1,126
Education No education 81.3 22.1 39.2 12.6 22.2 2.7 2.0 4,267 Primary 82.6 20.5 37.0 9.4 21.9 1.9 1.3 1,128 Secondary 83.3 21.3 39.1 13.7 24.2 1.2 0.5 2,812 More than secondary 80.3 19.6 46.2 18.3 19.6 0.0 0.0 87
Wealth quintile Lowest 79.8 22.8 40.1 9.2 23.3 2.6 2.2 1,490 Second 82.7 21.2 41.2 13.4 23.6 2.1 1.6 1,546 Middle 83.4 23.6 42.2 13.2 19.1 2.2 1.2 1,558 Fourth 79.1 20.2 38.7 10.5 23.4 2.4 1.5 1,686 Highest 85.0 20.5 33.8 15.8 24.1 1.2 0.6 2,013
Total 82.1 21.6 38.9 12.6 22.8 2.0 1.4 8,293

74 • Malaria Knowledge
Table 5.9 Media exposure to malaria messages
Percentage of women age 15-49 who have seen or heard a message about malaria in the past 6 months through specific sources of media, by background characteristics, Sierra Leone 2016
Background characteristic
Govern-ment clinic/
hospital Home1 School2 Community3 Posters or billboards On TV
On the radio
In the newspaper
Anywhere else Any source
Number of women
Age 15-19 57.8 66.5 32.5 32.3 30.4 11.1 54.3 9.7 19.8 77.5 1,665 20-24 70.3 70.1 20.5 34.7 27.8 12.3 54.2 7.9 20.9 81.8 1,658 25-29 73.4 71.2 14.9 32.1 23.2 10.6 53.5 7.5 24.6 82.4 1,705 30-34 73.8 74.2 18.1 39.0 25.4 12.4 58.9 7.5 25.4 85.5 1,218 35-39 72.6 73.4 13.8 36.8 24.5 10.7 54.6 6.9 24.1 83.8 1,208 40-44 66.9 72.6 14.7 38.4 23.7 9.2 55.0 6.4 25.6 82.3 608 45-49 60.5 71.7 13.2 38.4 20.8 11.0 53.3 7.3 18.9 82.3 439
Residence Urban 67.3 70.8 29.0 32.2 30.4 21.3 58.4 14.0 22.8 81.4 3,759 Rural 69.6 71.0 12.2 37.4 22.3 3.2 51.9 3.0 22.7 82.4 4,742
Region Eastern 72.8 64.6 11.0 30.6 26.6 3.6 54.2 3.6 16.6 80.3 1,936 Northern 70.6 77.7 18.8 46.1 30.5 8.1 56.8 6.0 24.2 87.5 2,884 Southern 60.9 63.6 15.2 23.8 14.6 3.5 47.9 1.5 23.1 71.8 1,736 Western 68.2 73.7 33.4 33.4 28.5 30.3 58.6 20.4 26.5 84.4 1,945
District Kailahun 68.7 54.1 2.1 15.3 8.9 1.5 43.5 2.6 10.8 78.2 670 Kenema 80.8 67.3 14.4 36.7 38.8 5.8 58.7 6.5 23.2 85.1 656 Kono 68.5 73.2 17.2 40.9 32.9 3.6 61.1 1.5 16.0 77.5 610 Bombali 60.1 62.5 30.4 41.1 36.6 25.3 55.9 18.6 24.9 66.9 732 Kambia 67.4 79.9 16.3 63.1 28.1 4.2 57.6 5.8 22.3 89.3 363 Koinadugu 64.3 74.2 17.1 41.0 32.4 0.8 56.2 1.2 3.4 92.9 434 Port Loko 67.4 80.3 15.7 33.1 5.5 3.4 49.9 1.3 24.3 94.3 617 Tonkolili 89.1 91.6 12.1 56.3 45.6 1.1 63.7 0.4 36.4 98.2 739 Bo 50.8 58.3 23.4 14.7 10.1 5.7 44.7 2.0 14.6 62.3 710 Bonthe 49.7 49.6 14.6 25.6 16.2 2.0 29.6 1.6 1.0 58.9 225 Moyamba 59.1 57.5 8.8 23.8 18.8 3.6 42.2 1.7 35.8 73.6 452 Pujehun 90.9 91.1 7.0 41.1 17.2 0.1 73.4 0.4 38.3 97.4 349 Western Area Rural 56.4 55.3 18.4 23.6 17.8 8.8 49.4 8.5 36.1 68.9 812 Western Area Urban 76.6 86.9 44.1 40.5 36.2 45.6 65.2 29.0 19.6 95.4 1,133
Education No education 71.4 72.3 10.0 36.9 20.6 5.0 50.1 3.1 24.0 83.1 4,393 Primary 64.0 65.1 16.6 30.3 18.6 7.7 50.0 3.7 19.4 77.7 1,173 Secondary 66.2 70.8 34.6 33.7 35.9 20.7 63.2 15.4 21.8 81.6 2,848 More than secondary 67.9 84.5 57.0 56.6 69.4 63.1 84.3 56.4 36.7 93.9 87
Wealth quintile Lowest 67.5 67.1 9.1 33.4 18.0 2.3 38.9 1.8 20.4 81.3 1,555 Second 73.8 74.6 13.4 39.6 24.5 3.2 54.2 3.4 24.6 85.7 1,591 Middle 67.9 69.2 15.3 39.2 25.2 3.0 57.2 3.8 22.4 80.3 1,604 Fourth 67.3 67.7 21.2 30.2 26.8 5.9 57.6 5.7 22.6 78.8 1,721 Highest 66.9 75.0 34.8 33.8 32.8 35.3 63.2 20.9 23.6 83.6 2,029
Total 68.6 70.9 19.6 35.1 25.9 11.2 54.8 7.8 22.8 82.0 8,501 1 Respondents saw or heard a message about malaria in the past 6 months from a community health club, a community health worker, at home, or from friends or family. 2 Respondents saw or heard a message about malaria in the past 6 months from a school health club or peer educators. 3 Respondents saw or heard a message about malaria in the past 6 months at a community meeting or from drama groups, a town crier, or faith/religious leaders.

References • 75
REFERENCES
Doolan, D. L., C. Dobano, and J. K. Baird. 2009. “Acquired Immunity to Malaria.” Clin. Microbiol. Rev. 22: 13-36.
Korenromp, E. L., J. Armstrong-Schellenberg, B. Williams, B. Nahlen, R. W. Snow. 2004. “Impact of Malaria Control on Childhood Anemia in Africa – A Quantitative Review.” Trop Med Int Health 9(10): 1050-1065.
Ministry of Health and Sanitation [Sierra Leone]. 2014. Sierra Leone Health Facility Survey 2014. Assessing the Impact of the EVD outbreak on Health Systems in Sierra Leone Survey. http://www.unicef.org/emergencies/ebola/files/SL_Health_Facility_Survey_2014Dec3.pdf
Ministry of Health and Sanitation [Sierra Leone]. 2015a. Sierra Leone Malaria Control Strategic Plan 2016-2020. Freetown, Sierra Leone: Ministry of Health and Sanitation.
Ministry of Health and Sanitation [Sierra Leone]. 2015b. Ebola Virus Disease - Situation Report: Summary of Laboratory Results. 31 January 2015. Freetown, Sierra Leone: Ministry of Health and Sanitation.
Ministry of Health and Sanitation [Sierra Leone]. 2015c. National Malaria Control Policy Document, Revised Version.
Moody, A. 2002. “Rapid Diagnostic Tests for Malaria Parasites.” Clinical Microbiology Review 15:66-78.
National Malaria Control Programme (NMCP), Statistics Sierra Leone, University of Sierra Leone, Catholic Relief Services, and ICF International. 2013. Sierra Leone Malaria Indicator Survey. Freetown, Sierra Leone: NMCP, SSL, CRS, and ICF International.
Roll Back Malaria Partnership. 2003. Monitoring and Evaluation Reference Group Anemia Task Force Meeting Minutes. Presented at WHO Headquarters. Geneva: 2003 Oct 27-28.
Shulman, C. E., and E. K. Dorman. 2003. “Importance and Prevention of Malaria in Pregnancy.” Trans R Soc Trop Med Hyg 97(1):30–55.
Statistics Sierra Leone. 2016. 2015 Sierra Leone Population and Housing Census. Provisional Results. March 2016. https://www.statistics.sl/wp-content/uploads/2016/06/2015-Census-Provisional-Result.pdf.
Statistics Sierra Leone (SSL) and ICF Macro. 2009. Sierra Leone Demographic and Health Survey 2008. Calverton, Maryland, USA: Statistics Sierra Leone (SSL) and ICF Macro.
World Health Organization. 2004. A Strategic Framework for Malaria Prevention and Control during Pregnancy in the African Region. Geneva: World Health Organziation.
World Health Organization. 2012a. WHO Evidence Review Group: Intermittent Preventive Treatment of Malaria in Pregnancy (IPTp) with Sulfadoxine-Pyrimethamine (SP). WHO Headquarters, Geneva, 9-11 July 2012. Meeting report. Geneva: World Health Organization. http://www.who.int/malaria/mpac/sep2012/iptp_sp_erg_meeting_report_july2012.pdf
World Health Organization. 2012b. Global Malaria Programme. Updated WHO Policy Recommendation (October 2012) Intermittent Preventive Treatment of Malaria in Pregnancy Using Sulfadoxine-Pyrimethamine (IPTp-SP). http://who.int/malaria/iptp_sp_updated_policy_recommendation_en_102012.pdf?ua=1


Appendix A • 77
SAMPLE DESIGN Appendix A
A.1 INTRODUCTION
The 2016 Sierra Leone Malaria Indicator Survey (SLMIS) is a representative probability sample designed to produce estimates for the country as a whole, for urban and rural areas separately, for each region, and for each of the 14 districts in Sierra Leone. The 14 districts are distributed over the country’s four regions as follows:
1. Eastern Region: Kailahun, Kenema, and Kono 2. Northern Region: Bombali, Kambia, Koinadugu, Port Loko, and Tonkolili 3. Southern Region: Bo, Bonthe, Moyamba, and Pujehun 4. Western Region: Western Area Rural and Western Area Urban
A.2 SAMPLE FRAME
The sampling frame used for the 2016 SLMIS is the 2015 Sierra Leone Population and Housing Census. A total of 12,858 enumeration areas (EAs) were constructed for the census, with complete coverage of the country’s territory. A final complete list of EAs is available in the Statistics Sierra Leone. This list includes each EA’s identification information and number of households from the census summary sheets. Table A.1 shows the household population distribution by district and by type of residence. In Sierra Leone, 38.5% of residential households are in urban areas, and 35.6% are in the Northern Region.
Table A.1 Households
Distribution of households in the census frame by district and residence, Sierra Leone MIS 2016
Domain Population in frame
Percent of total
population Percent urban Urban Rural Total
Eastern Region 87,982 191,196 279,178 22.53 31.51 Kailahun District 28,015 62,873 90,888 7.34 30.82 Kenema District 42,763 69,254 112,017 9.04 38.18 Kono District 17,204 59,069 76,273 6.16 22.56
Northern Region 96,084 345,445 441,529 35.64 21.76 Bombali District 23,880 67,963 91,843 7.41 26.00 Kambia District 16,854 42,693 59,547 4.81 28.30 Koinadugu District 13,108 59,724 72,832 5.88 18.00 Port Loko District 22,817 89,718 112,535 9.08 20.28 Tonkolili District 19,425 85,347 104,772 8.46 18.54
Southern Region 44,509 218,493 263,002 21.23 16.92 Bo District 31,457 73,851 105,308 8.50 29.87 Bonthe District 7,111 35,363 42,474 3.43 16.74 Moyamba District 3,889 55,771 59,660 4.82 6.52 Pujehun District 2,052 53,508 55,560 4.48 3.69
Western Region 248,531 6,626 255,157 20.60 97.40 Western Area Rural 59,703 6,626 66,329 5.35 90.01 Western Area Urban 188,828 0 188,828 15.24 100.00
Sierra Leone 477,106 761,760 1,238,866 100.00 38.51
Table A.2 shows the distribution of EAs and average EA size (number of residential households) by district and by type of residence. On average, each EA has 96 households (90 in urban areas and 101 in rural areas). The EA average size is 20 households per cluster. Therefore, a 2016 SLMIS cluster corresponds to a census EA.

78 • Appendix A
Table A.2 Enumeration areas
Number of EAs and average EA size by district and by type of residence, Sierra Leone MIS 2016
Domain Number of EAs Average EA size
Urban Rural Total Urban Rural Total
Eastern Region Kailahun District 275 616 891 102 102 102 Kenema District 441 678 1,119 97 102 100 Kono District 201 586 787 86 101 97
Northern Region Bombali District 289 695 984 83 98 93 Kambia District 200 376 576 84 114 103 Koinadugu District 147 601 748 89 99 97 Port Loko District 300 854 1,154 76 105 98 Tonkolili District 207 861 1,068 94 99 98
Southern Region Bo District 323 708 1,031 97 104 102 Bonthe District 71 392 463 100 90 92 Moyamba District 37 579 616 105 96 97 Pujehun District 33 549 582 62 97 95
Western Region Western Area Rural 635 65 700 94 102 95 Western Area Urban 2,139 0 2,139 88 0 88
Sierra Leone 5,298 7,560 12,858 90 101 96
A.3 SAMPLE DESIGN AND IMPLEMENTATION
The sample for the 2016 SLMIS was a stratified sample selected in two stages. In the first stage, 336 EAs were selected with stratified probability proportional to size (PPS) sampling from the sampling frame. EA size was the number of residential households in the EA as recorded in the census. Stratification was achieved by separating every district into urban and rural areas; separate strata were assigned for major towns such as Kenema, Koidu, Makeni, Bo, and Bonthe. Therefore the 2016 SLMIS contained 32 sampling strata (13 rural and 19 urban). Samples were selected independently in each stratum, and a predetermined number of EAs were selected (see Table A.3). Implicit stratification was achieved in each of the explicit sampling strata by sorting the sampling frame according to chiefdoms and sections within the stratum and using the PPS selection procedure.
A household listing operation was carried out in all of the selected EAs before the main survey. In the household listing operation, the 336 selected EAs were visited to draw a location map and a detailed sketch map and to record on the household listing forms the address and the name of the head of the household for all residential households found in the EA. The resulting list of households served as the sampling frame for the selection of households in the second stage. In the second stage, for each selected EA, a fixed number of 20 households was selected from the list created during the household listing. Household selection was performed in the central office prior to the main survey. All women age 15-49 and their young children under age 5 in the selected households were eligible for the interview.
Table A.3 shows the sample allocation of clusters by district and by type of residence. There were 24 clusters in each district. These 24 clusters were then allocated to urban and rural areas and major towns. Among the 336 clusters selected, 99 were in urban areas and 237 were in rural areas. Table A.3 also shows the number of households selected according to sampling strata. The total number of households selected in the 2016 SLMIS was 6,720, 1,980 in urban areas and 4,740 in rural areas.

Appendix A • 79
Table A.3 Sample allocation
Sample allocation of clusters and selected households by district, by town, and by type of residence, Sierra Leone MIS 2016
Domain Sample cluster allocation Selected household allocation
Urban Rural Total Urban Rural Total
Eastern Region Kailahun District 4 20 24 80 400 480 Kenema District 3 16 19 60 320 380 Kenema Town (Kenema) 5 0 5 100 0 100 Koidu Town (Kono) 6 0 6 120 0 120 Kono District 2 16 18 40 320 360
Northern Region Bombali District 2 18 20 40 360 400 Kambia District 4 20 24 80 400 480 Koinadugu District 2 22 24 40 440 480 Makeni (Bombali) 4 0 4 80 0 80 Port Loko District 4 20 24 80 400 480 Tonkolili District 4 20 24 80 400 480
Southern Region Bo District 2 15 17 40 300 340 Bo Town (Bo) 7 0 7 140 0 140 Bonthe District 3 20 23 60 400 460 Bonthe Town (Bonthe) 1 0 1 20 0 20 Moyamba District 4 20 24 80 400 480 Pujehun District 4 20 24 80 400 480
Western Region Western Area Rural 14 10 24 280 200 480 Western Area Urban 24 0 24 480 0 480
Sierra Leone 99 237 336 1,980 4,740 6,720
Table A.4 shows the expected number of eligible women and the expected number of interviewed women by district and type of residence. The total expected number of interviewed women in the 2016 SLMIS was 7,500, with 2,618 women residing in urban areas and 4,882 in rural areas.
Table A.4 Sample allocation of women
Expected number of women age 15-49 found and interviewed by district, by town, and by type of residence, Sierra Leone MIS 2016
Domain
Expected number of eligible women age 15-49
Expected number of interviewed women age 15-49
Urban Rural Total Urban Rural Total
Eastern Region Kailahun District 109 422 531 106 412 518 Kenema District 82 338 420 79 330 409 Kenema Town (Kenema) 136 0 136 132 0 132 Koidu Town (Kono) 164 0 164 159 0 159 Kono District 55 338 393 53 330 383
Northern Region Bombali District 55 380 435 53 371 424 Kambia District 109 422 531 106 412 518 Koinadugu District 55 465 520 53 453 506 Makeni (Bombali) 109 0 109 106 0 106 Port Loko District 109 422 531 106 412 518 Tonkolili District 109 422 531 106 412 518
Southern Region Bo District 55 316 371 53 308 361 Bo Town (Bo) 191 0 191 185 0 185 Bonthe District 82 422 504 79 412 491 Bonthe Town (Bonthe) 27 0 27 26 0 26 Moyamba District 109 422 531 106 412 518 Pujehun District 109 422 531 106 412 518
Western Region Western Area Rural 382 211 593 370 206 576 Western Area Urban 655 0 655 634 0 634
Sierra Leone 2,702 5,002 7,704 2,618 4,882 7,500

80 • Appendix A
A.4 SAMPLE PROBABILITIES AND SAMPLE WEIGHTS
Because of the non-proportional allocation of the sample to the different reporting domains, sampling weights will be required for any analysis using the 2016 SLMIS data to ensure the actual representativeness of the sample. Since the 2016 SLMIS sample was a two-stage stratified cluster sample, sampling weights were calculated based on sampling probabilities that were calculated separately for each sampling stage and for each cluster. We used the following notations:
P1hi: first-stage sampling probability of the ith cluster in stratum h
P2hi: second-stage sampling probability within the ith cluster (households) Phi: overall sampling probability for any households of the ith cluster in stratum h
Let ah be the number of clusters selected in stratum h, Mhi the number of households according to the sampling frame in the ith cluster, and ¦ hiM the total number of structures in stratum h. The probability
of selecting the ith cluster in stratum h is calculated as follows:
hih
hi
a M M¦
Let hib be the proportion of households in the selected cluster compared to the total number of households
in EA i in stratum h if the EA is segmented; otherwise, 1 hib . Then the probability of selecting cluster i in the sample is:
hihi
hih1hi b
M M a = P u
¦
Let hiL be the number of households listed in the household listing operation in cluster i in stratum h, and
let hig be the number of households selected in that cluster. The second-stage selection probability for each household in the cluster is calculated as follows:
hi
hihi L
gP 2
The overall selection probability for each household in cluster i of stratum h is therefore the product of the two-stage selection probabilities:
hihihi PPP 21 u
The sampling weight for each household in cluster i of stratum h is the inverse of its overall selection probability:
hihi PW /1
A spreadsheet containing all of the sampling parameters and selection probabilities was constructed to facilitate the calculation of sampling weights. Household sampling weights and individual sampling weights were obtained by adjusting the above-calculated weight to compensate for household nonresponse and individual nonresponse, respectively. These weights were further normalized at the national level to produce equal numbers of unweighted and weighted cases for both households and individuals. The normalized weights are valid for estimations of proportions and means at any aggregation level but are not valid for estimations of totals.

Appendix B • 81
ESTIMATES OF SAMPLING ERRORS Appendix B
he estimates from a sample survey are affected by two types of errors: non-sampling errors and sampling errors. Non-sampling errors are the results of mistakes made in implementing data collection and data processing, such as failure to locate and interview the correct household,
misunderstanding of the questions on the part of either the interviewer or the respondent, and data entry errors. Although numerous efforts were made during the implementation of the 2016 Sierra Leone Malaria Indicator Survey (SLMIS) to minimize this type of error, non-sampling errors are impossible to avoid and difficult to evaluate statistically.
Sampling errors, on the other hand, can be evaluated statistically. The sample of respondents selected in the 2016 SLMIS is only one of many samples that could have been selected from the same population, using the same design and expected size. Each of these samples would yield results that differ somewhat from the results of the actual sample selected. Sampling errors are a measure of the variability between all possible samples. Although the degree of variability is not known exactly, it can be estimated from the survey results.
Sampling error is usually measured in terms of the standard error for a particular statistic (mean, percentage, etc.), which is the square root of the variance. The standard error can be used to calculate confidence intervals within which the true value for the population can reasonably be assumed to fall. For example, for any given statistic calculated from a sample survey, the value of that statistic will fall within a range of plus or minus two times the standard error of that statistic in 95% of all possible samples of identical size and design.
If the sample of respondents had been selected as a simple random sample, it would have been possible to use straightforward formulas for calculating sampling errors. However, the 2016 SLMIS sample is the result of a multi-stage stratified design, and, consequently, it was necessary to use more complex formulas. Sampling errors are computed in either ISSA or SAS, using programs developed by ICF Macro. These programs use the Taylor linearization method of variance estimation for survey estimates that are means, proportions, or ratios.
The Taylor linearization method treats any percentage or average as a ratio estimate, r = y/x, where y represents the total sample value for variable y and x represents the total number of cases in the group or subgroup under consideration. The variance of r is computed using the formula given below, with the standard error being the square root of the variance:
¦ ¦
»¼
º«¬
ª¸̧¹
·¨̈©
§�
��
H
h h
hm
ihi
h
h
mzz
mm
xfrvarrSE
h
1
2
1
22
2
11)()(
in which
hihihi rxyz � and hhh rxyz � where h represents the stratum, which varies from 1 to H;
mh is the total number of clusters selected in the hth stratum; yhi is the sum of the weighted values of variable y in the ith cluster in the hth stratum; xhi is the sum of the weighted number of cases in the ith cluster in the hth stratum; and f is the overall sampling fraction, which is so small that it is ignored.
T

82 • Appendix B
In addition to the standard error, the design effect (DEFT) for each estimate is also calculated. The design effect is defined as the ratio between the standard error using the given sample design and the standard error that would result if a simple random sample had been used. A DEFT value of 1.0 indicates that the sample design is as efficient as a simple random sample, while a value greater than 1.0 indicates the increase in the sampling error due to the use of a more complex and less statistically efficient design. Relative standard errors and confidence limits for the estimates are also calculated.
Sampling errors for the 2016 SLMIS are calculated for selected variables considered to be of primary interest. The results are presented in this appendix for the country as a whole, for urban and rural areas, for each of the country regions (Eastern, Northern, Southern, and Western), and for each of the country’s 14 districts. For each variable, the type of statistic (mean, proportion, or rate) and the base population are given in Table B.1. Tables B.2 through B.22 present the value of the statistic (R), its standard error (SE), the number of unweighted (N) and weighted (WN) cases, the design effect (DEFT), the relative standard error (SE/R), and the 95% confidence limits (R ± 2SE) for each variable. The DEFT is considered undefined when the standard error considering a simple random sample is zero (when the estimate is close to 0 or 1).
The confidence interval (e.g., as calculated for children with a fever in the last 2weeks) can be interpreted as follows: the overall average from the national sample is 0.266, and its standard error is 0.009. Therefore, to obtain the 95% confidence limits, one adds and subtracts twice the standard error to the sample estimate, that is, 0.266 ± 2 × 0.009. There is a high probability (95%) that the true proportion of children with a fever in the last 2 weeks is between 0.248 and 0.284.
For the total sample, the value of the DEFT, averaged over all variables, is 1.74. This means that, due to multi-stage clustering of the sample, the average standard error is increased by a factor of 1.74 over that in an equivalent simple random sample.

Appendix B • 83
Table B.2 Sampling errors: Total sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.517 0.013 8,501 8,501 2.360 0.025 0.491 0.542 At least some secondary education 0.345 0.014 8,501 8,501 2.699 0.040 0.317 0.373 Ownership of at least one ITN 0.603 0.010 6,719 6,719 1.732 0.017 0.583 0.624 Child slept under an ITN last night 0.441 0.013 7,429 7,365 1.691 0.029 0.416 0.467 Pregnant women slept under an ITN last night 0.440 0.026 661 671 1.302 0.058 0.389 0.491 Received 2+ doses of SP/Fansidar during antenatal visit 0.713 0.017 2,554 2,451 1.851 0.024 0.680 0.747 Child has fever in last 2 weeks 0.266 0.009 5,960 5,804 1.439 0.033 0.248 0.284 Child sought care/treatment from a health facility 0.714 0.017 1,639 1,545 1.402 0.024 0.680 0.748 Child took ACT 0.449 0.018 1,639 1,545 1.313 0.039 0.414 0.484 Child has anaemia (Haemoglobin <8.0 g/dl) 0.101 0.006 6,655 6,659 1.435 0.056 0.089 0.112 Child has malaria (based on rapid test) 0.527 0.014 6,644 6,644 1.951 0.026 0.499 0.555 Child has malaria (based on microscopy test) 0.401 0.012 6,654 6,658 1.733 0.029 0.378 0.424
Table B.3 Sampling errors: Urban sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.363 0.021 2,796 3,759 2.309 0.058 0.320 0.405 At least some secondary education 0.529 0.025 2,796 3,759 2.609 0.047 0.479 0.578 Ownership of at least one ITN 0.537 0.019 1,980 2,688 1.719 0.036 0.498 0.576 Child slept under an ITN last night 0.376 0.025 2,004 2,777 1.832 0.066 0.326 0.426 Pregnant women slept under an ITN last night 0.307 0.042 187 267 1.254 0.137 0.223 0.391 Received 2+ doses of SP/Fansidar during antenatal visit 0.641 0.037 687 938 2.021 0.057 0.567 0.714 Child has fever in last 2 weeks 0.242 0.014 1,655 2,236 1.284 0.060 0.213 0.270 Child sought care/treatment from a health facility 0.690 0.034 436 540 1.402 0.050 0.622 0.759 Child took ACT 0.427 0.032 436 540 1.249 0.076 0.363 0.492 Child has anaemia (Haemoglobin <8.0 g/dl) 0.067 0.010 1,815 2,555 1.426 0.143 0.048 0.087 Child has malaria (based on rapid test) 0.315 0.029 1,810 2,545 2.210 0.091 0.258 0.372 Child has malaria (based on microscopy test) 0.252 0.020 1,815 2,555 1.716 0.077 0.213 0.291
Table B.4 Sampling errors: Rural sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.639 0.012 5,705 4,742 1.961 0.020 0.614 0.664 At least some secondary education 0.200 0.012 5,705 4,742 2.200 0.058 0.176 0.223 Ownership of at least one ITN 0.648 0.012 4,739 4,031 1.771 0.019 0.623 0.672 Child slept under an ITN last night 0.480 0.013 5,425 4,588 1.465 0.027 0.454 0.507 Pregnant women slept under an ITN last night 0.528 0.027 474 404 1.173 0.052 0.473 0.583 Received 2+ doses of SP/Fansidar during antenatal visit 0.759 0.014 1,867 1,513 1.361 0.018 0.731 0.786 Child has fever in last 2 weeks 0.282 0.011 4,305 3,568 1.540 0.040 0.259 0.304 Child sought care/treatment from a health facility 0.726 0.018 1,203 1,005 1.332 0.025 0.690 0.762 Child took ACT 0.460 0.020 1,203 1,005 1.339 0.044 0.419 0.501 Child has anaemia (Haemoglobin <8.0 g/dl) 0.122 0.007 4,840 4,104 1.386 0.056 0.108 0.135 Child has malaria (based on rapid test) 0.659 0.012 4,834 4,099 1.566 0.017 0.636 0.682 Child has malaria (based on microscopy test) 0.494 0.013 4,839 4,103 1.660 0.026 0.468 0.520
Table B.5 Sampling errors: Eastern Region sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.551 0.018 1,703 1,936 1.521 0.033 0.515 0.588 At least some secondary education 0.262 0.020 1,703 1,936 1.833 0.075 0.223 0.301 Ownership of at least one ITN 0.705 0.019 1,440 1,663 1.600 0.027 0.667 0.744 Child slept under an ITN last night 0.578 0.025 1,426 1,648 1.549 0.044 0.528 0.629 Pregnant women slept under an ITN last night 0.495 0.062 144 167 1.453 0.125 0.372 0.619 Received 2+ doses of SP/Fansidar during antenatal visit 0.726 0.035 495 571 1.740 0.048 0.657 0.795 Child has fever in last 2 weeks 0.293 0.021 1,144 1,295 1.469 0.070 0.252 0.334 Child sought care/treatment from a health facility 0.748 0.034 348 380 1.348 0.045 0.680 0.815 Child took ACT 0.480 0.032 348 380 1.104 0.066 0.417 0.543 Child has anaemia (Haemoglobin <8.0 g/dl) 0.086 0.011 1,267 1,469 1.400 0.129 0.063 0.108 Child has malaria (based on rapid test) 0.598 0.028 1,266 1,467 1.804 0.046 0.543 0.653 Child has malaria (based on microscopy test) 0.404 0.022 1,266 1,468 1.449 0.053 0.361 0.447

84 • Appendix B
Table B.6 Sampling errors: Northern Region sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.595 0.016 3,129 2,884 1.863 0.028 0.562 0.627 At least some secondary education 0.268 0.017 3,129 2,884 2.131 0.063 0.234 0.301 Ownership of at least one ITN 0.575 0.018 2,399 2,230 1.776 0.031 0.539 0.611 Child slept under an ITN last night 0.388 0.019 2,863 2,650 1.631 0.049 0.350 0.426 Pregnant women slept under an ITN last night 0.447 0.035 276 245 1.117 0.079 0.377 0.517 Received 2+ doses of SP/Fansidar during antenatal visit 0.757 0.018 1,022 918 1.317 0.024 0.722 0.793 Child has fever in last 2 weeks 0.276 0.015 2,349 2,117 1.471 0.053 0.247 0.305 Child sought care/treatment from a health facility 0.708 0.023 653 585 1.230 0.033 0.662 0.754 Child took ACT 0.427 0.027 653 585 1.302 0.064 0.373 0.482 Child has anaemia (Haemoglobin <8.0 g/dl) 0.123 0.008 2,560 2,364 1.167 0.064 0.107 0.139 Child has malaria (based on rapid test) 0.646 0.017 2,558 2,362 1.605 0.026 0.612 0.680 Child has malaria (based on microscopy test) 0.518 0.017 2,560 2,364 1.585 0.033 0.484 0.552
Table B.7 Sampling errors: Southern Region sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.536 0.032 2,279 1,736 3.030 0.059 0.472 0.599 At least some secondary education 0.319 0.031 2,279 1,736 3.194 0.098 0.257 0.382 Ownership of at least one ITN 0.704 0.017 1,920 1,496 1.677 0.025 0.669 0.739 Child slept under an ITN last night 0.560 0.020 2,017 1,559 1.396 0.036 0.519 0.600 Pregnant women slept under an ITN last night 0.609 0.045 158 128 1.153 0.074 0.519 0.698 Received 2+ doses of SP/Fansidar during antenatal visit 0.732 0.026 635 455 1.450 0.036 0.680 0.785 Child has fever in last 2 weeks 0.328 0.020 1,542 1,167 1.581 0.062 0.288 0.369 Child sought care/treatment from a health facility 0.759 0.030 492 383 1.432 0.040 0.699 0.820 Child took ACT 0.495 0.040 492 383 1.685 0.080 0.416 0.574 Child has anaemia (Haemoglobin <8.0 g/dl) 0.102 0.009 1,795 1,411 1.275 0.093 0.083 0.121 Child has malaria (based on rapid test) 0.592 0.017 1,795 1,411 1.355 0.029 0.558 0.626 Child has malaria (based on microscopy test) 0.395 0.021 1,795 1,411 1.685 0.053 0.353 0.437
Table B.8 Sampling errors: Western Region sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.350 0.033 1,390 1,945 2.561 0.094 0.284 0.416 At least some secondary education 0.566 0.035 1,390 1,945 2.606 0.061 0.497 0.636 Ownership of at least one ITN 0.410 0.033 960 1,330 2.050 0.079 0.345 0.475 Child slept under an ITN last night 0.262 0.032 1,123 1,509 1.881 0.123 0.198 0.327 Pregnant women slept under an ITN last night 0.190 0.049 83 130 1.194 0.256 0.093 0.287 Received 2+ doses of SP/Fansidar during antenatal visit 0.603 0.059 402 507 2.277 0.097 0.485 0.720 Child has fever in last 2 weeks 0.161 0.015 925 1,225 1.139 0.095 0.131 0.192 Child sought care/treatment from a health facility 0.577 0.066 146 198 1.509 0.114 0.445 0.710 Child took ACT 0.361 0.053 146 198 1.218 0.146 0.256 0.467 Child has anaemia (Haemoglobin <8.0 g/dl) 0.078 0.017 1,033 1,414 1.620 0.217 0.044 0.112 Child has malaria (based on rapid test) 0.188 0.029 1,025 1,404 1.911 0.154 0.130 0.246 Child has malaria (based on microscopy test) 0.209 0.030 1,033 1,414 1.953 0.142 0.149 0.268
Table B.9 Sampling errors: Kailahun sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.530 0.022 526 670 1.020 0.042 0.485 0.574 At least some secondary education 0.221 0.032 526 670 1.742 0.143 0.157 0.284 Ownership of at least one ITN 0.758 0.029 480 620 1.477 0.038 0.700 0.816 Child slept under an ITN last night 0.581 0.042 470 617 1.587 0.073 0.497 0.665 Pregnant women slept under an ITN last night 0.462 0.147 37 49 1.811 0.318 0.168 0.755 Received 2+ doses of SP/Fansidar during antenatal visit 0.678 0.073 162 213 2.002 0.107 0.533 0.823 Child has fever in last 2 weeks 0.304 0.032 374 489 1.326 0.107 0.239 0.369 Child sought care/treatment from a health facility 0.698 0.064 120 149 1.401 0.091 0.571 0.825 Child took ACT 0.435 0.041 120 149 0.868 0.095 0.352 0.517 Child has anaemia (Haemoglobin <8.0 g/dl) 0.131 0.016 423 564 0.974 0.123 0.099 0.164 Child has malaria (based on rapid test) 0.670 0.034 423 564 1.368 0.050 0.603 0.738 Child has malaria (based on microscopy test) 0.450 0.026 423 564 1.015 0.058 0.398 0.502

Appendix B • 85
Table B.10 Sampling errors: Kenema sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.610 0.034 577 656 1.689 0.056 0.542 0.679 At least some secondary education 0.275 0.033 577 656 1.761 0.119 0.210 0.341 Ownership of at least one ITN 0.758 0.030 480 558 1.519 0.039 0.698 0.817 Child slept under an ITN last night 0.664 0.042 510 592 1.518 0.063 0.580 0.748 Pregnant women slept under an ITN last night 0.718 0.058 48 55 0.873 0.081 0.602 0.834 Received 2+ doses of SP/Fansidar during antenatal visit 0.775 0.035 161 185 1.075 0.045 0.704 0.845 Child has fever in last 2 weeks 0.192 0.034 395 444 1.606 0.175 0.125 0.259 Child sought care/treatment from a health facility 0.717 0.074 75 85 1.376 0.103 0.570 0.864 Child took ACT 0.620 0.057 75 85 1.003 0.093 0.505 0.735 Child has anaemia (Haemoglobin <8.0 g/dl) 0.076 0.024 460 536 1.973 0.322 0.027 0.124 Child has malaria (based on rapid test) 0.593 0.048 460 536 1.803 0.080 0.498 0.688 Child has malaria (based on microscopy test) 0.377 0.036 459 535 1.410 0.096 0.305 0.449
Table B.11 Sampling errors: Kono sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.512 0.037 600 610 1.798 0.072 0.438 0.585 At least some secondary education 0.293 0.031 600 610 1.650 0.105 0.232 0.355 Ownership of at least one ITN 0.578 0.035 480 485 1.559 0.061 0.507 0.648 Child slept under an ITN last night 0.459 0.044 446 439 1.509 0.095 0.371 0.547 Pregnant women slept under an ITN last night 0.326 0.081 59 63 1.308 0.249 0.164 0.488 Received 2+ doses of SP/Fansidar during antenatal visit 0.733 0.045 172 172 1.323 0.061 0.643 0.823 Child has fever in last 2 weeks 0.403 0.041 375 362 1.553 0.102 0.321 0.485 Child sought care/treatment from a health facility 0.816 0.033 153 146 0.956 0.040 0.750 0.882 Child took ACT 0.444 0.055 153 146 1.245 0.124 0.334 0.555 Child has anaemia (Haemoglobin <8.0 g/dl) 0.030 0.011 384 369 1.271 0.371 0.008 0.052 Child has malaria (based on rapid test) 0.495 0.047 383 367 1.716 0.095 0.401 0.589 Child has malaria (based on microscopy test) 0.375 0.053 384 369 2.080 0.141 0.269 0.480
Table B.12 Sampling errors: Bombali sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.495 0.035 675 732 1.814 0.071 0.425 0.565 At least some secondary education 0.395 0.043 675 732 2.261 0.108 0.310 0.480 Ownership of at least one ITN 0.537 0.043 480 531 1.861 0.079 0.452 0.622 Child slept under an ITN last night 0.434 0.055 530 562 1.962 0.126 0.325 0.543 Pregnant women slept under an ITN last night 0.518 0.086 58 60 1.251 0.165 0.346 0.689 Received 2+ doses of SP/Fansidar during antenatal visit 0.830 0.034 182 187 1.172 0.040 0.762 0.897 Child has fever in last 2 weeks 0.310 0.034 439 454 1.404 0.108 0.243 0.377 Child sought care/treatment from a health facility 0.814 0.036 142 141 0.996 0.044 0.741 0.886 Child took ACT 0.479 0.056 142 141 1.177 0.117 0.366 0.591 Child has anaemia (Haemoglobin <8.0 g/dl) 0.084 0.020 501 528 1.425 0.233 0.045 0.123 Child has malaria (based on rapid test) 0.477 0.040 499 526 1.528 0.085 0.396 0.557 Child has malaria (based on microscopy test) 0.376 0.031 501 528 1.360 0.082 0.314 0.438
Table B.13 Sampling errors: Kambia sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE No education 0.600 0.032 621 363 1.632 0.054 0.536 0.665 At least some secondary education 0.229 0.032 621 363 1.907 0.141 0.164 0.293 Ownership of at least one ITN 0.676 0.040 480 273 1.856 0.059 0.597 0.756 Child slept under an ITN last night 0.487 0.052 520 299 1.986 0.107 0.383 0.591 Pregnant women slept under an ITN last night 0.464 0.082 62 33 1.198 0.177 0.300 0.628 Received 2+ doses of SP/Fansidar during antenatal visit 0.866 0.032 205 119 1.322 0.036 0.803 0.930 Child has fever in last 2 weeks 0.269 0.027 451 261 1.202 0.099 0.216 0.322 Child sought care/treatment from a health facility 0.820 0.042 116 70 1.211 0.052 0.735 0.905 Child took ACT 0.655 0.068 116 70 1.538 0.105 0.518 0.792 Child has anaemia (Haemoglobin <8.0 g/dl) 0.110 0.016 460 265 1.069 0.143 0.078 0.141 Child has malaria (based on rapid test) 0.594 0.066 460 265 2.605 0.112 0.461 0.727 Child has malaria (based on microscopy test) 0.483 0.049 460 265 2.027 0.102 0.385 0.582

86 • Appendix B
Table B.14 Sampling errors: Koinadugu sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.694 0.019 597 434 1.012 0.028 0.656 0.732 At least some secondary education 0.216 0.018 597 434 1.048 0.082 0.180 0.251 Ownership of at least one ITN 0.619 0.034 480 350 1.543 0.055 0.550 0.687 Child slept under an ITN last night 0.403 0.044 598 428 1.708 0.109 0.315 0.491 Pregnant women slept under an ITN last night 0.635 0.081 46 31 1.063 0.128 0.473 0.798 Received 2+ doses of SP/Fansidar during antenatal visit 0.609 0.038 206 143 1.089 0.062 0.533 0.685 Child has fever in last 2 weeks 0.306 0.032 506 347 1.473 0.106 0.241 0.371 Child sought care/treatment from a health facility 0.536 0.064 147 106 1.492 0.119 0.409 0.664 Child took ACT 0.368 0.056 147 106 1.372 0.152 0.256 0.479 Child has anaemia (Haemoglobin <8.0 g/dl) 0.202 0.023 536 383 1.232 0.115 0.156 0.249 Child has malaria (based on rapid test) 0.781 0.029 536 383 1.471 0.038 0.723 0.840 Child has malaria (based on microscopy test) 0.579 0.041 536 383 1.707 0.070 0.498 0.660
Table B.15 Sampling errors: Port Loko sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.592 0.041 540 617 1.918 0.069 0.511 0.674 At least some secondary education 0.212 0.038 540 617 2.174 0.181 0.136 0.289 Ownership of at least one ITN 0.511 0.041 479 556 1.800 0.081 0.428 0.593 Child slept under an ITN last night 0.342 0.035 516 606 1.221 0.102 0.272 0.411 Pregnant women slept under an ITN last night 0.310 0.061 66 73 0.994 0.196 0.189 0.431 Received 2+ doses of SP/Fansidar during antenatal visit 0.661 0.040 171 203 1.118 0.060 0.581 0.740 Child has fever in last 2 weeks 0.169 0.027 420 491 1.423 0.159 0.115 0.222 Child sought care/treatment from a health facility 0.548 0.066 74 83 1.132 0.120 0.416 0.680 Child took ACT 0.256 0.071 74 83 1.357 0.278 0.113 0.398 Child has anaemia (Haemoglobin <8.0 g/dl) 0.105 0.017 439 515 1.182 0.164 0.070 0.139 Child has malaria (based on rapid test) 0.698 0.033 439 515 1.410 0.047 0.632 0.764 Child has malaria (based on microscopy test) 0.585 0.038 439 515 1.485 0.066 0.508 0.662
Table B.16 Sampling errors: Tonkolili sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.635 0.034 696 739 1.833 0.053 0.568 0.702 At least some secondary education 0.237 0.030 696 739 1.839 0.125 0.177 0.296 Ownership of at least one ITN 0.601 0.036 480 520 1.590 0.059 0.530 0.673 Child slept under an ITN last night 0.343 0.033 699 755 1.529 0.097 0.276 0.410 Pregnant women slept under an ITN last night 0.433 0.074 44 48 0.960 0.170 0.286 0.581 Received 2+ doses of SP/Fansidar during antenatal visit 0.811 0.033 258 268 1.349 0.041 0.744 0.877 Child has fever in last 2 weeks 0.327 0.024 533 565 1.092 0.073 0.280 0.375 Child sought care/treatment from a health facility 0.756 0.041 174 185 1.218 0.054 0.674 0.837 Child took ACT 0.413 0.048 174 185 1.163 0.115 0.318 0.509 Child has anaemia (Haemoglobin <8.0 g/dl) 0.129 0.013 624 673 0.960 0.101 0.103 0.155 Child has malaria (based on rapid test) 0.683 0.027 624 673 1.299 0.039 0.629 0.737 Child has malaria (based on microscopy test) 0.557 0.029 624 673 1.365 0.052 0.499 0.615
Table B.17 Sampling errors: Bo sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.458 0.062 547 710 2.893 0.135 0.334 0.583 At least some secondary education 0.411 0.057 547 710 2.704 0.139 0.296 0.526 Ownership of at least one ITN 0.764 0.025 480 631 1.283 0.033 0.715 0.814 Child slept under an ITN last night 0.645 0.025 491 634 0.917 0.039 0.595 0.696 Pregnant women slept under an ITN last night 0.678 0.061 53 64 0.893 0.090 0.556 0.800 Received 2+ doses of SP/Fansidar during antenatal visit 0.763 0.046 129 154 1.187 0.061 0.670 0.855 Child has fever in last 2 weeks 0.350 0.041 375 461 1.499 0.117 0.268 0.432 Child sought care/treatment from a health facility 0.654 0.054 126 161 1.148 0.083 0.546 0.763 Child took ACT 0.386 0.079 126 161 1.760 0.204 0.229 0.543 Child has anaemia (Haemoglobin <8.0 g/dl) 0.098 0.018 456 594 1.181 0.182 0.062 0.133 Child has malaria (based on rapid test) 0.571 0.022 456 594 0.852 0.038 0.527 0.614 Child has malaria (based on microscopy test) 0.397 0.038 456 593 1.534 0.095 0.321 0.472

Appendix B • 87
Table B.18 Sampling errors: Bonthe sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.595 0.031 504 225 1.400 0.052 0.533 0.656 At least some secondary education 0.283 0.030 504 225 1.492 0.106 0.223 0.343 Ownership of at least one ITN 0.727 0.036 480 216 1.757 0.049 0.655 0.798 Child slept under an ITN last night 0.544 0.041 491 220 1.393 0.076 0.461 0.626 Pregnant women slept under an ITN last night 0.558 0.105 30 13 1.094 0.188 0.348 0.768 Received 2+ doses of SP/Fansidar during antenatal visit 0.724 0.037 164 72 1.046 0.051 0.651 0.798 Child has fever in last 2 weeks 0.236 0.031 372 163 1.340 0.132 0.173 0.298 Child sought care/treatment from a health facility 0.808 0.041 86 38 0.983 0.050 0.727 0.890 Child took ACT 0.572 0.039 86 38 0.700 0.068 0.494 0.650 Child has anaemia (Haemoglobin <8.0 g/dl) 0.068 0.013 414 184 1.070 0.194 0.042 0.095 Child has malaria (based on rapid test) 0.468 0.038 414 184 1.520 0.082 0.392 0.545 Child has malaria (based on microscopy test) 0.261 0.026 414 184 1.159 0.099 0.210 0.313
Table B.19 Sampling errors: Moyamba sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.569 0.034 664 452 1.788 0.060 0.501 0.638 At least some secondary education 0.273 0.038 664 452 2.209 0.140 0.196 0.349 Ownership of at least one ITN 0.608 0.037 480 340 1.669 0.061 0.534 0.683 Child slept under an ITN last night 0.495 0.044 511 356 1.447 0.089 0.406 0.583 Pregnant women slept under an ITN last night 0.638 0.101 30 21 1.176 0.159 0.435 0.841 Received 2+ doses of SP/Fansidar during antenatal visit 0.844 0.042 164 116 1.494 0.049 0.761 0.927 Child has fever in last 2 weeks 0.281 0.037 392 271 1.577 0.132 0.207 0.355 Child sought care/treatment from a health facility 0.810 0.055 116 76 1.259 0.068 0.699 0.920 Child took ACT 0.422 0.060 116 76 1.205 0.141 0.302 0.541 Child has anaemia (Haemoglobin <8.0 g/dl) 0.102 0.013 474 330 0.963 0.130 0.075 0.128 Child has malaria (based on rapid test) 0.606 0.045 474 330 1.796 0.074 0.516 0.696 Child has malaria (based on microscopy test) 0.399 0.042 474 330 1.694 0.106 0.314 0.483
Table B.20 Sampling errors: Pujehun sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.611 0.031 564 349 1.490 0.050 0.549 0.672 At least some secondary education 0.216 0.038 564 349 2.155 0.174 0.141 0.291 Ownership of at least one ITN 0.672 0.042 480 310 1.974 0.063 0.587 0.757 Child slept under an ITN last night 0.481 0.044 524 349 1.607 0.091 0.394 0.569 Pregnant women slept under an ITN last night 0.465 0.106 45 30 1.410 0.228 0.253 0.676 Received 2+ doses of SP/Fansidar during antenatal visit 0.581 0.060 178 112 1.639 0.104 0.460 0.701 Child has fever in last 2 weeks 0.395 0.034 403 271 1.330 0.086 0.327 0.463 Child sought care/treatment from a health facility 0.864 0.034 164 107 1.268 0.039 0.797 0.931 Child took ACT 0.684 0.040 164 107 1.070 0.058 0.604 0.763 Child has anaemia (Haemoglobin <8.0 g/dl) 0.130 0.019 451 304 1.184 0.150 0.091 0.169 Child has malaria (based on rapid test) 0.692 0.030 451 304 1.324 0.044 0.631 0.753 Child has malaria (based on microscopy test) 0.468 0.037 451 304 1.456 0.079 0.393 0.542
Table B.21 Sampling errors: Western Area Rural sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.449 0.048 753 812 2.631 0.107 0.353 0.545 At least some secondary education 0.454 0.045 753 812 2.484 0.100 0.364 0.545 Ownership of at least one ITN 0.420 0.045 480 495 1.990 0.107 0.330 0.510 Child slept under an ITN last night 0.264 0.054 725 784 2.544 0.205 0.156 0.373 Pregnant women slept under an ITN last night 0.281 0.091 38 53 1.423 0.322 0.100 0.463 Received 2+ doses of SP/Fansidar during antenatal visit 0.675 0.097 277 288 3.353 0.143 0.482 0.869 Child has fever in last 2 weeks 0.181 0.021 614 673 1.257 0.118 0.138 0.223 Child sought care/treatment from a health facility 0.501 0.085 103 122 1.707 0.170 0.331 0.672 Child took ACT 0.266 0.052 103 122 1.166 0.195 0.162 0.370 Child has anaemia (Haemoglobin <8.0 g/dl) 0.132 0.033 655 721 2.043 0.249 0.066 0.198 Child has malaria (based on rapid test) 0.335 0.043 647 711 1.984 0.128 0.249 0.421 Child has malaria (based on microscopy test) 0.349 0.044 655 721 2.049 0.125 0.262 0.436

88 • Appendix B
Table B.22 Sampling errors: Western Area Urban sample, Sierra Leone MIS 2016
Variable R SE N WN DEFT SE/R R-2SE R+2SE
No education 0.279 0.040 637 1,133 2.235 0.143 0.199 0.358 At least some secondary education 0.647 0.042 637 1,133 2.227 0.066 0.562 0.731 Ownership of at least one ITN 0.404 0.045 480 835 1.983 0.110 0.315 0.493 Child slept under an ITN last night 0.261 0.033 398 724 1.232 0.127 0.194 0.327 Pregnant women slept under an ITN last night 0.126 0.050 45 77 0.996 0.396 0.026 0.226 Received 2+ doses of SP/Fansidar during antenatal visit 0.507 0.039 125 219 0.873 0.077 0.429 0.586 Child has fever in last 2 weeks 0.138 0.020 311 552 0.972 0.146 0.097 0.178 Child sought care/treatment from a health facility 0.699 0.077 43 76 1.070 0.110 0.546 0.853 Child took ACT 0.514 0.101 43 76 1.260 0.197 0.311 0.716 Child has anaemia (Haemoglobin <8.0 g/dl) 0.022 0.009 378 693 1.232 0.400 0.004 0.040 Child has malaria (based on rapid test) 0.038 0.008 378 693 0.918 0.220 0.021 0.055 Child has malaria (based on microscopy test) 0.063 0.020 378 693 1.640 0.312 0.024 0.103

Appendix C • 89
SAMPLE IMPLEMENTATION Appendix C
Table C.1 Household age distribution
Single-year age distribution of the de facto household population by sex (weighted), Sierra Leone 2016
Women Men
Age
Women Men
Age Number Percent Number Percent Number Percent Number Percent
0 696 3.4 683 3.6 37 153 0.7 180 1.0 1 682 3.3 645 3.4 38 196 1.0 257 1.4 2 656 3.2 714 3.8 39 129 0.6 107 0.6 3 768 3.8 800 4.3 40 372 1.8 428 2.3 4 812 4.0 783 4.2 41 52 0.3 82 0.4 5 539 2.6 573 3.0 42 76 0.4 182 1.0 6 679 3.3 648 3.4 43 86 0.4 95 0.5 7 723 3.5 705 3.7 44 37 0.2 53 0.3 8 610 3.0 614 3.3 45 225 1.1 465 2.5 9 455 2.2 462 2.5 46 59 0.3 98 0.5 10 621 3.0 660 3.5 47 48 0.2 71 0.4 11 354 1.7 297 1.6 48 86 0.4 111 0.6 12 563 2.8 555 2.9 49 45 0.2 62 0.3 13 523 2.6 394 2.1 50 435 2.1 266 1.4 14 522 2.6 420 2.2 51 145 0.7 46 0.2 15 357 1.7 493 2.6 52 218 1.1 102 0.5 16 355 1.7 317 1.7 53 97 0.5 56 0.3 17 297 1.5 302 1.6 54 81 0.4 45 0.2 18 395 1.9 373 2.0 55 226 1.1 222 1.2 19 303 1.5 247 1.3 56 93 0.5 86 0.5 20 558 2.7 422 2.2 57 41 0.2 43 0.2 21 216 1.1 149 0.8 58 50 0.2 53 0.3 22 341 1.7 259 1.4 59 23 0.1 30 0.2 23 326 1.6 162 0.9 60 236 1.2 222 1.2 24 218 1.1 169 0.9 61 19 0.1 15 0.1 25 746 3.7 393 2.1 62 44 0.2 36 0.2 26 220 1.1 147 0.8 63 26 0.1 29 0.2 27 312 1.5 197 1.0 64 28 0.1 39 0.2 28 317 1.5 199 1.1 65 145 0.7 161 0.9 29 168 0.8 112 0.6 66 17 0.1 12 0.1 30 624 3.1 471 2.5 67 24 0.1 55 0.3 31 102 0.5 74 0.4 68 59 0.3 35 0.2 32 221 1.1 198 1.1 69 19 0.1 20 0.1 33 119 0.6 110 0.6 70+ 528 2.6 436 2.3 34 143 0.7 136 0.7 Don’t know/
missing
35 585 2.9 551 2.9 18 0.1 26 0.1 36 181 0.9 153 0.8 Total 20,444 100.0 18,812 100.0
Note: The de facto population includes all residents and nonresidents who stayed in the household the night before the interview.

90 • Appendix C
Table C.2 Age distribution of eligible and interviewed women
De facto household population of women age 10-54, interviewed women age 15-49; and percent distribution and percentage of eligible women who were interviewed (weighted), by five-year age groups, Sierra Leone 2016
Household population of women age
10-54 Interviewed women age 15-49
Percentage of eligible women
interviewed Age group Number Percentage
10-14 2,584 - - - 15-19 1,708 1,706 19.7 99.9 20-24 1,660 1,657 19.1 99.8 25-29 1,762 1,757 20.3 99.7 30-34 1,210 1,206 13.9 99.6 35-39 1,245 1,245 14.4 100.0 40-44 623 622 7.2 99.9 45-49 463 462 5.3 99.8 50-54 976 - - -
15-49 8,670 8,654 100.0 99.8
Note: The de facto population includes all residents and nonresidents who stayed in the household the night before the interview. Weights for both household population of women and interviewed women are household weights. Age is based on the household questionnaire. na = Not applicable
Table C.3 Completeness of reporting
Percentage of observations missing information for selected demographic and health questions (weighted), Sierra Leone 2016
Subject
Percentage with information
missing Number of
cases
Month Only (Births in the 15 years preceding the survey) 0.64 6,699
Month and Year (Births in the 15 years preceding the survey) 0.09 6,699
Age at Death (Deceased children born in the 15 years preceding the survey) 0.00 243
Respondent’s education (All women age 15-49) 0.00 8,501 Anaemia (Living children age 6-59 months from
the Household Questionnaire) 1.81 6,782
1 Both year and age missing
Table C.4 Births by calendar years
Number of births, percentage with complete birth date, sex ratio at birth, and calendar year ratio by calendar year, according to living (L), dead (D), and total (T) children (weighted), Sierra Leone 2016
Number of births Percentage with complete
birth date1 Sex ratio at birth2 Calendar year ratio3 Calendar year L D T L D T L D T L D T
2016 630 22 652 100.0 100.0 100.0 103.1 111.5 103.4 - - - 2015 1,374 36 1,411 99.6 91.9 99.4 95.2 93.9 95.1 - - - 2014 1,112 59 1,172 99.3 96.2 99.2 96.6 143.9 98.5 88.1 133.8 89.6 2013 1,151 52 1,203 99.0 93.5 98.8 104.1 112.8 104.5 103.9 97.8 103.6 2012 1,104 47 1,151 99.5 94.4 99.3 99.9 132.1 101.0 98.7 121.5 99.4 2011 1,086 26 1,112 99.6 86.8 99.3 103.7 134.4 104.3 196.8 109.4 193.2 2012-2016 5,371 217 5,588 99.4 94.8 99.3 99.2 120.7 100.0 - - - All 6,456 243 6,699 99.5 94.0 99.3 100.0 122.1 100.7 - - -
na = Not applicable 1 Both year and month of birth given 2 (Bm/Bf)x100, where Bm and Bf are the numbers of male and female births, respectively 3 [2Bx/(Bx-1+Bx+1)]x100, where Bx is the number of births in calendar year x

Appendix D • 91
SURVEY PERSONNEL Appendix D
2016 SIERRA LEONE MIS TECHNICAL WORKING GROUP Dr. Foday Sahr, University of Sierra Leone
Role in SLMIS: Principal Investigator
Dr. Mohamed Samai, University of Sierra Leone Role in SLMIS: Co-Principal Investigator
Dr. Samuel J. Smith, Program Manager, National Malaria Control Program Role in SLMIS: Project Manager
Dr. Adikali A. Kamara, Deputy Program Manager, National Malaria Control Program, Role in SLMIS: Assistant Project Manager
Dr. Foday Daffae, Director, Directorate for Disease Prevention and Control in MOHS Role in SLMIS: TWG Member
Mr. Francis Tommy, Principal Statistician, Statistics Sierra Leone Role in SLMIS: TWG Member
Mr. Sahr Yambasu, Principal Statistician/Census Manager, Statistics Sierra Leone Role in SLMIS: TWG Member
Mr. Ebrima Jarju, GF R10 Project Director, Catholic Relief Services Role in SLMIS: Project Manager
Dr. Ngozi Kennedy, Health Specialist, UNICEF Role in SLMIS: TWG Member
Mr. Wogba E.P. Kamara , Senior M&E Specialist, DPPI/MOHS Role in SLMIS: Monitoring & Evaluation Officer
Dr. Louisa Ganda, National Programme Officer, World Health Organization Role in SLMIS: TWG Member
Mr. Alpha S. Swaray, Medical Microbiologist, Ministry of Health and Sanitation Role in SLMIS: Laboratory Manager

92 • Appendix D
2016 SIERRA LEONE MIS TECHNICAL LABORATORY STAFF Alpha S. Swaray, Laboratory Manager
Anthony S. M. Domowa, Microscopist
Idrissa Laybohr Kamara, Microscopist
Philip G. Pessima, Microscopist
Sia Sessie, Microscopist
Mohamed I. Fornah, Microscopist
Alusine Fornah, Microscopist
Tamba Yollah, Microscopist
Mustapha Baion, Microscopist
2016 SIERRA LEONE MIS DATA MANAGERS Mr. Musa Sillah-Kanu, Senior M&E Officer, National Malaria Control Programme
Mr. Fredrick Yamba, M&E Officer, National Malaria Control Programme
Mr. Mohamed M. Bah, M&E Officer, Catholic Relief Services
Mr. Alhaji Kamara, Catholic Relief Services
Ms. Kayla Fishbeck, Catholic Relief Services
2016 SIERRA LEONE MIS SLIDE MANAGERS Zainab Yeabu Bangura
Aminata Salima Kamara
Walton Tucker
Moiyatu Momoh
Princess George
Fancess Kemokai
2016 SIERRA LEONE MIS LOGISTICS OFFICERS Unisa Kamara
Thomas M. Turay
2016 SIERRA LEONE MIS BIOMARKER SUPERVISORS Edwina Conteh
Jerikatu Bangura

Appendix D • 93
Kailahun Team 1 Field Staff Steven J. Amara Coordinator Alpha Fomba Supervisor Abu Bakarr Bangura Nurse Mariama Rashidatu Osman Interviewer Augustine Genda Biomarker Mohamed Kallay Runner Kailahun Team 2 Field Staff Steven J. Amara Coordinator Fatmata Bayoh Supervisor Jokojeh Decker Nurse Lawrence Musa Interviewer Sia Rosaline Allieu Biomarker Mohamed Kallay Runner Kenema Team 1 Field Staff Sylvia Kpaka Coordinator Mawonde Marrah Supervisor Mohamed N. Bockarie Nurse Gladys Johnny Interviewer Mary D. Yamba Biomarker Melvin T. Gbondo Runner Kenema Team 2 Field Staff Sylvia Kpaka Coordinator Mohamed A. Bangura Supervisor Jenifer Anderson Nurse Fatmata Kallon Interviewer Princess Rogers Biomarker Melvin T. Gbondo Runner Kono Team 1 Field Staff Mrs. E. M. Kabba-Kamara Coordinator Ngadie Koroma Supervisor Musu R. Foday Nurse Daniel J. Davies Interviewer Regina V. Lamin Biomarker Abu Bakarr Fawundu Runner Kono Team 2 Field Staff Mrs. E. M. Kabba-Kamara Coordinator Memunatu Kai Supervisor Fatmata R. Sesay Nurse Maada J. Stevens Interviewer Hawanatu Kamara Biomarker Abu Bakarr Fawundu Runner Bombali Team 1 Field Staff Ansumana Bawie Sandy Coordinator Laurel Kargbo Supervisor Lilian Kanu Nurse Alusine Samura Interviewer Aminata Kamara Biomarker Fea Lucy Sandy Runner
Bombali Team 2 Field Staff Ansumana Bawie Sandy Coordinator Victoria A. Koroma Supervisor Abibatu Rahman Bangura Nurse Isata Barrie Interviewer Aminata Kamara Biomarker Fea Lucy Sandy Runner Kambia Team 1 Field Staff John Seppeh Coordinator Umu Hawa Jalloh Supervisor Lucy Sarah Macauley Nurse Tommy Bangura Interviewer Patricia Conteh Biomarker Isata M. Swaray Runner Kambia Team 2 Field Staff John Seppeh Coordinator Eleanor Ngegbai Supervisor Joan Bassie Nurse Hawa Conteh Interviewer Rugiatu Bangura Biomarker Isata M. Swaray Runner Koinadugu Team 1 Field Staff Lamin Kamara Coordinator Albert Ansumana Supervisor Fatmata Y. Kargbo Nurse Abass Tarawallie Interviewer Hawanatu Kamara Biomarker Samuel Torto Runner Koinadugu Team 2 Field Staff Lamin Kamara Coordinator Musa B. Conteh Supervisor Franklyn A. Forey-Marrah Nurse Samuella Lavalie Interviewer Fatmata Koroma Biomarker Samuel Torto Runner Port Loko Team 1 Field Staff Roseline F. Kamara Coordinator Mabinty Fofanah Supervisor Kadiatu Mannah Nurse Alhaji H. Kamara Interviewer Rachael Sesay Biomarker Joe Kebbie Runner Port Loko Team 2 Field Staff Roseline F. Kamara Coordinator Osman Momoh Kamara Supervisor Juliet Bangura Nurse Augusta Macauley Interviewer Kemah Johnny Biomarker Joe Kebbie Runner

94 • Appendix D
Tonkololi Team 1 Field Staff Samuel Grosvenor Coordinator Rugiatu Bangura Supervisor Nanah Dumbuya Nurse Fatmata Koroma Interviewer Gloria Kpaka Biomarker Priscilla Bangura Runner Tonkololi Team 2 Field Staff Samuel Grosvenor Coordinator Henrietta Kargbo Supervisor Marion F. R. Sesay Nurse Alhaji Sesay Interviewer Lamin Kanu Biomarker Priscilla Bangura Runner Bo Team 1 Field Staff Emmanuel Bernard Coordinator Prince A. Fagawa Supervisor Halimatu Kamara Nurse Pheabean Williams Interviewer Beah Joe J. Lebby Biomarker Victor Tommy Runner Bo Team 2 Field Staff Emmanuel Bernard Coordinator Mangu Juana Supervisor Soukhinatu Tunis Nurse Memunatu Turay Interviewer Doris Bio Biomarker Victor Tommy Runner Bonthe Team 1 Field Staff Nelson S. Fofana Coordinator Ishmael Hassan Supervisor Alie Bantama Nurse Abdulai B. Kanu Interviewer Banerdette Massaquoi Biomarker Thomas Cole Runner Bonthe Team 2 Field Staff Nelson S. Fofana Coordinator Edwin B. Jusu Supervisor Priscilla Macfoy Nurse Bridget Mabel Wright Interviewer Dantes Musa Biomarker Thomas Cole Runner Moyamba Team 1 Field Staff James Junisa Coordinator Doris Ganda Supervisor Fatmata Binta Bah Nurse Tira S. Kargbo Interviewer Patrick Moiwo-Ansumana Biomarker Regina Kaisessie Runner
Moyamba Team 2 Field Staff James Junisa Coordinator Emmanuel Gborie Supervisor Erica King Nurse Salifu Mansaray Interviewer David Mattia Biomarker Regina Kaisessie Runner Pujehun Team 1 Field Staff Amadu Amara Coordinator Deborah A. Koroma Supervisor Francess Kemokai Nurse Mohamed Kanu Interviewer Aisha B. Musa Biomarker Idrissa Kemoh Runner Pujehun Team 2 Field Staff Amadu Amara Coordinator Momoh S. Sandy Supervisor Fatmata Rogers Nurse Adama Yambasu Interviewer Khadijatu Vandy Biomarker Idrissa Kemoh Runner Western Rural Team 1 Field Staff Dr. Anita Kamara Coordinator Masseh E. N. Jones Supervisor Francess Yatta Kamara Nurse Adama Umu Bangura Interviewer Isatu Mansaray Biomarker Salamatu Koroma Runner Western Rural Team 2 Field Staff Dr. Anita Kamara Coordinator Ramata Kanneh Supervisor Lorraine Marion Feury Nurse Ann Marie Kargbo Interviewer Ignatius G. Margai Biomarker Salamatu Koroma Runner Western Urban Team 1 Field Staff Prince Koh Coordinator Zainab Bungura Supervisor Margaret N. Jalloh Nurse Francess Nasu Jimmy Interviewer Ross E. P. Stevens Biomarker Mohamed Sankoh Runner Western Urban Team 2 Field Staff Prince Koh Coordinator Ngadi Lombi Supervisor Victoria Dixie Luke Nurse Osman Koroma Interviewer Zainab Juheh Bah Biomarker Mohamed Sankoh Runner

Appendix D • 95
CATHOLIC RELIEF SERVICES (CRS) PROGRAMMING STAFF Kwame Akangah Head of Operations Heather Dolphin Head of Programs Ebrima Jarjou Project Director Francis Zuradam Saareson MIS Coordinator Nancy Mansaray Assistant Program Manager Mohamed M. Bah M&E Coordinator Laima Abu K. Dumbuya Finance Coordinator Memunatu K. Kamara M&E Assistant James Nyakeh Lahai Zonal Coordinator, North/West Dominic Lumeh Zonal Coordinator, East Yayah Mansaray Zonal Coordinator, South Michael K. Mansaray Zonal Coordinator, North Alhaji Kamara IT Manager Yayah Kamara Logistics Officer
ICF STAFF Martin Vaessen Project Lead Adrienne Cox Survey Manager Hamdy Moussa Survey Manager Lia Florey Survey Manager Mike Amakyi Biomarker Specialist Mianmian Yu Data Processing Specialist Harouna Koche Data Processing Specialist Geoffrey Lutwama Data Processing Specialist Han Raggers Data Processing Specialist Mahmoud Elkasabi Sampling Statistician Nancy Johnson Senior Editor Chris Gramer Report Production Specialist Teresa Duberry Report Production Specialist Toni Jones Biomarker Supplies Procurement
Coordinator Elizabeth Britton Electronics Supplies Procurement
Coordinator Trinadh Dontamsetti GIS Specialist Matthew Pagan GIS Specialist


QUESTIONNAIRES Appendix E
• 97Appendix E


• 99Appendix E

100 • Appendix E

• 101Appendix E

102 • Appendix E

• 103Appendix E

104 • Appendix E

• 105Appendix E

106 • Appendix E

• 107Appendix E

108 • Appendix E

• 109Appendix E

110 • Appendix E

• 111Appendix E

112 • Appendix E

• 113Appendix E

114 • Appendix E

• 115Appendix E

116 • Appendix E

• 117Appendix E

118 • Appendix E

• 119Appendix E

120 • Appendix E

• 121Appendix E

122 • Appendix E

• 123Appendix E

124 • Appendix E

• 125Appendix E

126 • Appendix E

• 127Appendix E

128 • Appendix E

• 129Appendix E

130 • Appendix E

• 131Appendix E

132 • Appendix E

• 133Appendix E

134 • Appendix E

• 135Appendix E

136 • Appendix E

• 137Appendix E

138 • Appendix E


![Kenya Malaria Indicator Survey 2015 [MIS22] - The DHS · PDF fileThe 2015 Kenya Malaria Indicator Survey (2015 KMIS) was implemented by the National Malaria Control Programme (NMCP)](https://static.fdocuments.us/doc/165x107/5aabbf2a7f8b9a8d678c317b/kenya-malaria-indicator-survey-2015-mis22-the-dhs-2015-kenya-malaria-indicator.jpg)






![Sierra Leone Malaria Indicator Survey 2013 [MIS15] · Malaria remains one of the biggest public health problems in Sierra Leone. Over the past several years, the country has made](https://static.fdocuments.us/doc/165x107/5fef04e59f9d0e38036f11d7/sierra-leone-malaria-indicator-survey-2013-mis15-malaria-remains-one-of-the-biggest.jpg)



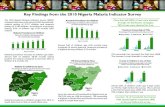

![Sierra Leone Malaria Indicator Survey 2013 [MIS15]aho.afro.who.int/profiles_information/images/7/7f/Sierra-Leone-MIS-2013.pdf · The 2013 Sierra Leone Malaria Indicator Survey (2013](https://static.fdocuments.us/doc/165x107/5d5f109a88c993b62a8bd51f/sierra-leone-malaria-indicator-survey-2013-mis15ahoafrowhointprofilesinformationimages77fsierra-leone-mis-2013pdf.jpg)


![Nigeria Malaria Indicator Survey (MIS) 2015 [MIS20] Malaria Indicator Survey (MIS) 2015 NIGERIA 2015 Malaria Indicator Survey (MIS) The Federal Republic of Nigeria Nigeria Malaria](https://static.fdocuments.us/doc/165x107/5ab7b6f17f8b9a28468bebde/nigeria-malaria-indicator-survey-mis-2015-mis20-malaria-indicator-survey-mis.jpg)
![nigeriahealthwatch.comNigeria Malaria Indicator Survey [MIS8]The 2010 Nigeria Malaria Indicator Survey (2010 NMIS) was implemented by the National Population Commission (NPC) and the](https://static.fdocuments.us/doc/165x107/611886e588a01943f10303d3/malaria-indicator-survey-mis8the-2010-nigeria-malaria-indicator-survey-2010-nmis.jpg)