M2VA Vol. 16 Issue 6 (Oct. 2012)
-
Upload
kmi-media-group -
Category
Documents
-
view
222 -
download
1
description
Transcript of M2VA Vol. 16 Issue 6 (Oct. 2012)

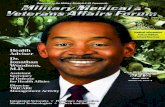
Dedicated to the Military Medical & VA Community
Force Protector
Vice Adm. Matthew L. Nathan
Surgeon GeneralU.S. Navy
Health Analytics O Cardiac Life Support Emergency Communications
Exclusive Interview with:
Col. Jeff ClarkCommander, U.S. Army Europe Regional Medical CommandCommand Surgeon U.S. Army Europe
Command Profile
October 2012Volume 16, Issue 6
www.M2VA-kmi.com
Combat Support
Hospitals

Propaq®—Focused on Your Data Needs Your next-generation Propaq® is here. The standard in vital signs monitoring now has advanced data communications for all levels of care.
Experience CountsZOLL, with over 25 years of experience
manufacturing resuscitation technologies
for the military, understands that to meet
today’s demands, you require more than
the best monitoring technology available.
In addition to providing the trusted and
proven vital signs monitoring you have
come to expect from Propaq, the ZOLL
Propaq M and Propaq MD now have
significantly enhanced data communications,
allowing you to capture patient care data
from the point of injury through definitive
care. Our new open data architecture is
designed to support the military’s emerging
telemedicine solutions, EHR systems, and
custom reporting needs (TCCC, AF3899).
© 2012 ZOLL Medical Corporation, Chelmsford, MA, USA. ZOLL is a registered trademark of ZOLL Medical Corporation. Propaq is a trademark of Welch Allyn.
For more information, call 1-800-804-4356 or visit us at www.zoll.com/propaqdata.

Military Medical & Veterans Affairs Forum OctOber 2012VOlume 16 • Issue 6
Features cOVer / Q&a
16
Departments
2
3
14
27
Editor’s Perspective
Program Notes
Vital Signs
Resource Center
InDustry InterVIew
28
Vice Admiral Matthew L. NathanSurgeon General
U.S. Navy
Kirk Ririe Chief Executive Officer BioFire Diagnostics Inc.
Getting the Word Out FastWhen disaster strikes, health providers need to communicate. It’s critical that technology and solutions are in place at the time of need.By Henry Canaday
5
A Shock to the SystemTechnologies used to provide treatment vital to keeping the wounded warfighter alive, with perspectives from military and industry suppliers.By J.B. Bissell
12
Analyzing the SystemWith so much data available to health providers, it’s vital that this data is analyzed with the goal of improving health care and reducing costs.By Brian O’Shea
24
Combat Support HospitalsWith a Department of Defense budget crunch on the horizon, the new combat support hospital could be simpler and cheaper to deploy and operate, while upgrading some of the equipment and technologies used in the CSH.By Peter Buxbaum8
Exclusive Interview with:Colonel Jeff ClarkCommander
Command Surgeon, U.S. Army Europe. Every day wounded warriors evacuated from Afghanistan will arrive at Landstuhl Regional Medical Center where they will receive the absolute finest medical care in the world. Landstuhl Regional Medical Center is the only overseas U.S. Level I trauma center and serves as the ROLE IV strategic evacuation center for AFRICOM, CENTCOM, EUCOM and SOCOM.
20
COMMANd PROFiLE U.S. Army Europe Regional Medical Command

Since September 11, 2001, more than 2 million servicemembers have deployed to Iraq or Afghanistan, and after more than a decade of long deployments and oftentimes intense combat conditions, the White House is re-affirming its commitment to support the emotional and mental health of servicemembers and their families. Recently President Barack Obama signed the executive order “Improving Access to Mental Health Services for Veterans, Service Members, and Military Families.”
The order directs the Secretaries of Defense, Health and Human Services, Education, Veterans Affairs, and Homeland Security to expand suicide prevention strategies and take steps to meet the current and future demand for mental health and substance abuse treatment services for veterans, servicemembers and their families.
Late last year, the Subcommittee on Health held a hearing entitled “Understanding and Preventing Veteran Suicide” to track the progress being made to prevent suicide and steps taken to identify at-risk servicemembers and veterans by the Departments of Defense and Veterans Affairs.
“The statistics are sobering—18 veterans commit suicide each day with almost a third receiving care from the Department of Veterans Affairs at the time of their death,” said Rep. Ann Marie Buerkle, Subcommittee Chairwoman on Health. “Each month, there are 950 veterans being treated by VA who attempt suicide. What’s more, data from the Department of Defense indicate servicemembers took their lives at an approximate rate of one every 36 hours from 2005 to 2010.”
The executive order also directs the Departments of Veterans Affairs and Defense to jointly develop and implement a national suicide prevention campaign focused on connecting veterans and servicemembers to mental health services. This 12-month campaign, which began on September 1, 2012, will focus on the positive benefits of seeking care and encourage veterans and servicemembers to proactively reach out to support services.
It seems that despite a growing amount of support from the federal government, the numbers for suicides among servicemembers continue to increase. If you know someone who may be in need of help, let them know that there are options. People contemplating suicide often refer to ending their life as a last resort when they feel they have no other way out of their situation. The help is out there; sometimes they just need a push in the right direction. If you have any questions about Military Medical & Veterans Affairs Forum, feel free to contact me at any time.
Dedicated to the Military Medical & VA Community
eDItOrIal
EditorBrian O’Shea [email protected] EditorHarrison Donnelly [email protected] Editorial ManagerLaura Davis [email protected] Buxbaum • Henry CanadayKenya McCullum
art & DesIgn
Art DirectorJennifer Owers [email protected] Graphic DesignerJittima Saiwongnuan [email protected] Designers Amanda Kirsch [email protected] Morris [email protected] Waring [email protected]
aDVertIsIng
Associate PublisherCharles Weimer [email protected]
KmI meDIa grOupPublisherKirk Brown [email protected] Executive OfficerJack Kerrigan [email protected] Financial OfficerConstance Kerrigan [email protected] Vice PresidentDavid Leaf [email protected] McKaughan [email protected] Castro [email protected] AssistantCasandra Jones [email protected] Show CoordinatorHolly Foster [email protected]
OperatIOns, cIrculatIOn & prODuctIOn
Circulation & Marketing AdministratorDuane Ebanks [email protected] SpecialistsTuesday Johnson [email protected] Walker [email protected] Villanueva [email protected] Winston [email protected]
a prOuD member OF:
subscrIptIOn InFOrmatIOn
Military Medical & Veterans Affairs ForumISSN 1097-1033
is published eight times a year by KMI Media Group. All Rights Reserved.
Reproduction without permission is strictly forbidden. © Copyright 2012.
Military Medical & Veterans Affairs Forum is free to qualified members of the U.S. military,
employees of the U.S. government and non-U.S. foreign service based in the U.S.
All others: $65 per year. Foreign: $149 per year.
cOrpOrate OFFIces
KMI Media Group15800 Crabbs Branch Way, Suite 300
Rockville, MD 20855-2604 USATelephone: (301) 670-5700
Fax: (301) 670-5701Web: www.M2VA-kmi.com
mIlItary meDIcal & Veterans aFFaIrs FOrum
Volume 16, Issue 6 • September 2012
Brian O’SheaEditor
EDITOR’S PERSPECTIVE
KmI meDIa grOup leaDershIp magazInes anD websItes
www.GIF-kmi.com
Geospatial Intelligence
Forum
www.BCD-kmi.com
June 2012Volume 1, Issue 1
www.BCD-kmi.com
Border Threat Prevention and CBRNE Response
Border Protector
Michael J. Fisher
ChiefU.S. Border PatrolU.S. Customs and Border Protection
Wide Area Aerial Surveillance O Hazmat Disaster ResponseTactical Communications O P-3 Program
SPECIAL SECTION:Integrated Fixed Towers
Leadership Insight:Robert S. BrayAssistant Administrator for Law Enforcement/Director of the Federal Air Marshal Service
Border & CBRNE Defense
www.MAE-kmi.com
Military AdvancedEducation
www.MIT-kmi.com
Military Information Technology
www.GCT-kmi.com
Ground Combat
Technology
www.MLF-kmi.com
Military Logistics Forum
www.M2VA-kmi.com
Military Medical & Veterans
Affairs Forum
www.MT2-kmi.com
Military Training Technology
www.SOTECH-kmi.com
Special Operations Technology
www.TISR-kmi.com
Tactical ISR Technology
www.USCGF-kmi.com
U.S. Coast Guard Forum

Program Notes
Name Change Reflects Growing Breadth of Services in Molecular Diagnostics
Idaho Technology Inc. recently announced it has changed the corporate name to BioFire Diagnostics Inc. to more accurately reflect its business strategy and strong momentum in the marketplace. The company has also re-launched its website to reveal its new branding.
“We are excited to announce our new name to our customers and industry members,” said Kirk Ririe, chief executive officer of BioFire Diagnostics. “The new name reflects the passion and energy of the company and management team, and highlights our expanded presence in the clinical diagnostics market. We have established strong momentum in the diagnostics marketplace and the new branding under BioFire Diagnostics better reflects the markets we serve. We believe we are in an excellent position to continue building our business by driving growth of our broad molecular diagnostic product portfolio.”
BioFire Diagnostics will continue to focus on leveraging its novel FilmArray pathogen detection system to develop multiplex diagnostic tests for various clinical applications. The FilmArray Respiratory Panel (RP) is FDA-cleared for 20 viral and bacterial respiratory pathogens. BioFire now provides the only FDA cleared clinical diagnostic test for eight of the 20 organisms in its panel. In addition to the FilmArray RP, the company is developing similar FilmArray panels for pathogen identification in blood culture, gastrointestinal infections, meningitis and much more.
In addition to its enthusiasm around the clinical diagnostics space, BioFire will continue to lead in the development of reliable and sensitive biosurveillance products such as its PCR-based biodetection system Razor Ex and the FilmArray BioSurveillance System.
Lou Banks; [email protected]
Edge Innovation Network Membership Grows
Royal Philips Electronics recently announced it has joined the Edge Innovation Network, a collaborative, open-environment initiative enabling industry and academia, with government input, to work together to enhance the delivery cycle of new technologies and innovative capabilities to warfighters and first responders.
“Joining the Edge Innovation Network will connect Philips directly with our government customers through a collaborative environment with other Edge members,” said Joe Robinson, senior vice president of government and enterprise solutions for Royal Philips Electronics. “Through this interaction, we can better understand their needs, and accelerate the development of new capabilities and technologies to help them fulfill their various missions both home and abroad. As a leader in cardiac care, acute care and home health care, energy efficient lighting solutions and new lighting applications, Philips is a natural fit with Edge.”
Pete Palmer, director of the Edge Innovation Network said, “The power of the Edge is found in the collaboration of Edge members to rapidly deliver mission critical capabilities, technologies and solutions that can be fielded immediately.”
Sponsored by General Dynamics C4 Systems, there are 12 Edge Innovation Centers worldwide and over 275 Edge members. Recent new members include Science Applications International Corporation, Alexandria, Va.; University of Southern California, Playa Vista, Calif.; National Technical Systems, Calabasas, Calif.; Bionic Power, Burnaby, British Columbia; and Tirraappendi Inc. Redmond, Wash.
Veterans Affairs Department Awards Contract to Treat Tinnitus American soldiers returning
from service abroad and other veterans who suffer from debilitating tinnitus now have access to advanced treatment covered by the U.S. Department of Veterans Affairs (VA). Starting August 15, the VA will begin providing SoundCure Serenade customized sound therapy for veterans suffering from tinnitus, or “ringing in the ears.”
“We are very pleased to make this valuable treatment available to our nation’s troops serving us in so many ways,” stated Bill Perry, CEO of SoundCure.
“Improvised explosive devices and other explosions and noise damage can leave soldiers with a painful—and constant—reminder of their time on the battlefield. We are proud to work through the VA to provide a tinnitus solution and relief to military personnel.”
Tinnitus, which is most commonly the result of damage to the auditory system, is the number one disability affecting veterans. In the military, exposure to weapons systems, aircraft and other loud equipment that can cause damage is a daily
occurrence. According to the American Tinnitus Association, the 2011 estimated cost of annual tinnitus disability payments for war veterans was over $1 billion. Severe tinnitus can be extremely incapacitating, causing stress, anxiety and problems sleeping or concentrating.
In the U.S., the VA system consists of more than 170 medical centers and about 350 community clinics, with more facilities overseas. The number of veterans on the rolls for tinnitus was estimated to be over 800,000 in 2011.
The FDA-cleared Serenade handheld device is anchored by S-Tones. This novel treatment uses soft tones that are modulated at a specific rate and were created from independent university research. S-Tones were designed to provide relief to patients at volumes softer than the patient’s tinnitus to reduce, rather than add to, the patient’s sound burden. Serenade generates customized sound therapy for the patient’s unique tinnitus after testing and programming by a VA audiologist.
www.M2VA-kmi.com M2VA 16.6 | 3

$41.8M to Develop Medical Products for the Army
General Dynamics’ Information Technology unit has won a $41.8 million task order to support the U.S. Army Medical Materiel Development Activity’s (USAMMDA’s) efforts to develop advanced medical products. General Dynamics recently said it received the task order from the U.S. Army Medical Research Materiel Command under the TRICARE Evaluation, Analysis and Management Support contract vehicle. The contract, which has a four-year and seven month performance period, calls for services in support of vaccine, drug and medical device development programs of the USAMMDA.
As part of the contract, General Dynamics will render a broad range of services to assist the USAMMDA in guiding new medical technologies through the regulatory process to obtain U.S. Food and Drug Administration certification, according to the announcement.
Marcus Collier, General Dynamics Information Technology’s SVP of Health and Civilian Solutions division, said the company will help the USAMMDA develop advanced medical solutions through the delivery of its combined health, military and IT expertise.
Work will also include the development of plans to deploy new medical products into service. General Dynamics, together with partner, Tunnell Government Services Inc., will provide health, medical research, clinical trial and regulatory expertise as well as information, acquisition and program management support services.
General Dynamics intends to employ 30 new workers to accomplish the task which will be performed at Fort Detrick, Md. USAMMDA has worked with General Dynamics for four years.
National PTSD Consortium to Improve Diagnosis, Treatment
Half of patients suffering from post traumatic stress disorder (PTSD) are not identified, and treatment for those who are diagnosed is only partially effective, leading Draper Laboratory to form a consortium of nationally-recognized experts on PTSD to improve diagnostic tools and treatment outcomes.
PTSD has been diagnosed in more than 200,000 troops returning from combat in Iraq and Afghanistan, but it is also commonly found in civilians who have been involved in an accident or assault, or have suffered the unexpected loss of a loved one. Approximately 8 percent of the U.S. population will suffer from PTSD at some point in their lives, which can lead to panic attacks, substance abuse, depression, suicide, and a host of serious medical complications, most notably cardiovascular disorders.
The current state of the art in PTSD diagnosis is based on clinical interviews, so doctors have to rely on patients’ subjective reports. Although the clinical history is a good start, PTSD diagnoses would be better informed if reliable biomarkers of the condition were available, as is the case in many other areas of medicine.
The team plans to develop solutions based on objective, clinical decision making by using
sophisticated algorithms to integrate data from a spectrum of biomarkers including neuroimaging, psychophysiology, chemical assays and gene expression. The resulting diagnostic and treatment protocols will be more objective and personalized, complementing today’s primarily subjective means of evaluation and treatment selection.
“Although some biological characteristics that point to a PTSD diagnosis have already been identified, more comprehensive study is critical to examine the integrated roles of multiple potential biological factors of the condition,” according to Dr. Roger Pitman, director of the PTSD Research Laboratory at Massachusetts General Hospital and Professor of Psychiatry at Harvard Medical School. “This will help clinicians develop personalized treatment plans to improve outcomes, rather than relying on ‘one-size-fits-all’ approaches.”
Reducing inconclusive diagnoses and avoiding ineffective treatments, in turn, will help significantly reduce costs, both for patients as well as society, Pitman said.
The technology platform underlying the proposed solutions to PTSD diagnosis and treatment will be derived from those Draper has developed for a variety of systems for NASA and the Department of Defense. These systems
synthesize data from multiple sources to create actionable information. One example is Draper’s Timeliner system, which currently collects data from hundreds of sources to automate operations and diagnose points of failure in real time aboard the International Space Station and in power plants.
“We have the most advanced data fusion technology in critical decision making available to apply to PTSD diagnosis and personalized treatment care,” said Dr. Len Polizzotto, Draper’s vice president in charge of the program.
Bringing together a national team of leading PTSD experts from a variety of disciplines and institutions offers several advantages over pursuing the problem as a single organization, including the ability to look at the full spectrum of factors from neuroimaging to gene expression, and conduct human and animal studies in parallel, thus accelerating knowledge and development of solutions.
“No one of us could do this alone, but collaboratively, we will be able to create a solution to one of the most expensive health care problems our nation is facing in both cost and human toll,” said Dr. David Diamond, psychology professor at the University of South Florida.
Program Notes Compiled by KMi Media Group staff
Airworthiness Release Announced
SunTech Medical partner Remote Diagnostic Technologies Ltd. (RDT) has been granted air certification by USAARL for a fleetwide Airworthiness Release (AWR) from the United States Army for its medical monitor, Tempus IC Professional.
The achievement of the AWR certifies Tempus’ use by the military in the most extreme environments in which it is deployed. Its accurate blood pressure readings are provided using SunTech’s compact, non-invasive blood pressure Advantage module, capable of clinically-reliable measurements in emergency medicine situations. The handheld, durable Tempus provides all the patient monitoring features required by modern war fighters, with unique patient record data collecting and sharing capabilities.
The AWR has been signed-off on for the required aircraft and MEDEVAC platforms, approving its use on all U.S. Army UH/HH-60A/L/M, MH-60K and MH-47G helicopters.
www.M2VA-kmi.com4 | M2VA 16.6

The Joint Task Force National Capital Region Medical Command (JTF CapMed) leads military health care in the Washington, D.C. area. It is responsible for Walter Reed National Military Medical Center and Fort Belvoir Community Hospital and for working with health agen-cies in Washington, D.C., Northern Virginia and Maryland.
“We have invested heavily in communications,” said Colonel Paul Duray, director of current operations. “We stood up an operations center and have standard communication tools, landline, cell phone and information management system. Last year we invested in the land mobile radio because, after an attack, land line and cell phones may not be reliable.”
JTF CapMed is thus able to communicate with its hospitals and with civilian partners like the Maryland Institute of Emergency Medical Services Systems, the D.C. Department of Health and the Northern Virginia Hospital Alliance, all of which also use the land mobile radio.
Maryland, D.C. and Northern Virginia also decided to develop a common operating picture platform, HC Standard R, which provides near real-time situational awareness. JTF CapMed invested $3.6 million to join its civilian partners on the system.
One worry is how the land mobile radio will work in an area-wide emergency if land lines and cell systems get knocked out. Civilian and military radios must now use different frequency bands, so emergency centers would need two radios relaying infor-mation.
Two solutions are being explored: lobbying Congress for one emergency band for civilian and emergency users; and acquiring a radio that can hop between the two frequencies.
JTF CapMed also uses the Everbridge mass notification system. With Everbridge, the command’s key operations personnel can com-municate critical information to any or all staff members, anywhere, anytime, and through any medium, such as mobile phone, land line, email, text message, instant message and pager. Everbridge contacts individuals based on their preferences, stops sending messages after confirmed receipt and compiles results on a dashboard. The technol-
ogy was employed during massive snowfall in 2010.Dr. Daniel Bochicchio, director of the Office
of Emergency Management at the Veterans Health Administration (VHA), divides emergency communi-cations into three categories.
First, “systems for keeping veteran patients informed include traditional telephone systems to notify patients when care may be compromised by events affecting VHA facilities or emergencies affect-ing home care,” Bochicchio said. Local media have long been used by VHA to inform veterans, and Face-book and Twitter are now being used. “Facebook and Twitter were used very successfully to inform local
beneficiaries of the evacuation of Hampton VA Medical Center last year during Hurricane Irene.” VHA can also activate a nationwide veteran call center for toll-free access to scripted information in emergencies.
Col. Paul Duray
Maintaining coMMunications when eMergencies happen. By henry canaday, M2Va correspondent
www.M2VA-kmi.com M2VA 16.6 | 5

To communicate with staff, a legacy system is being replaced by an enhanced personnel accountability sys-tem that automatically pulls contact information from other VA systems, send alerts to select personnel and enables employees to report status. An employee call center provides toll-free access to scripted information.
To communicate with administration leadership and other federal agencies, VHA has additional systems, including internet portals to share information among its central office, Veterans Integrated Service Networks and federal partners. VHA also maintains access to the Homeland Security information network, a secure and trusted web-based portal for information sharing and collaboration.
The VA nationwide teleconferencing system con-nects all VHA levels and facilities to each other and with federal, state, local and tribal partners.
VHA maintains over 300 handheld satellite tele-phones to back up landline and cellular systems, has direct access to 60 vehicle-mounted very small aper-ture terminals and another 45 man-portable satellite phones. Satellite communications kits are maintained by 12 VHA regional emergency managers.
Finally, VHA maintains access to the Homeland Security data net-work to transmit homeland data in support of activities classified as secret.
Private firms provide a number of products that enable emergency medical communications.
AtHoc does mass emergency notification with a software solution deployed behind customer firewalls to protect private information. “The system reaches hundreds of thousands of people by telephone, email, text message, desktop alert, pager, giant voice, Cisco unified communications and fire alarm,” explained Dubhe Beinhorn, vice president of public sector. AtHoc tools have not yet notified the general pubic, “but that is the direction we are headed.”
AtHoc systems have been sold to the Air Force for 500,000 airmen, the Navy for 550,000 sailors, the VA for 400,000 people, the Transportation Security Adminis-tration for 100,000, Customs and Border Protection for 60,000 and to the Army for 80 percent of soldiers. “We have half of the federal government, many state and local governments and hospitals in Baltimore and Austin,” Beinhorn said.
AtHoc emphasizes using all alert modes and devices. It not only alerts but captures responses. “We call this personnel accountability,” Beinhorn said. “For example, if there is a fire in the building, it will learn who is not in the building, who is not working today, and who is in the building and needs help. It will send out a real-time report accounting for everybody.”
AtHoc’s new citizen-centric future will feature applications that run on smartphones and Androids so alerts can be sent from, as well as received by, these devices.
Cassidian Communications offers a comprehensive emergency notification portfolio, according to Benjamin Brewer, business devel-opment and certifications manager. The company’s Communicator! NXT solution is a highly intelligent, list-driven platform for resource
mobilization and mass notification. And GeoCast Web is a map-based notification system that lets users send layered geospatial alerts to
precisely targeted audiences. “For example, if there is an active shooter on campus, system operators can notify one group to avoid the area and another group to shelter in place, all while isolating the area in which the shooter is from receiving notification,” Brewer said.
The solutions and services of Cassidian Communi-cations are widely used by both the public and private sectors. Their client base includes over 100 civilian federal agencies; nearly 300 Department of Defense installations within the continental U.S. and overseas; over one-third of Fortune 500 companies, including healthcare operations and public utilities; and 700+ state and local public safety organizations. The com-pany’s solutions can be deployed on facility premises, use organic telephone and network assets supporting software as a service, or even a combination of the two. Redundancy of these critical systems ensures commu-nications will not fail, especially in large-scale events such as inclement weather or earthquakes.
Cassidian Communications integrates with third-party notification systems, sensors and building-man-agement systems via an application programming interface. “For example, if a chilled water system goes down, a manual system lacking integration indicates system failure but relies on operators to intervene in
order to push information out to the appropriate parties,” Brewer explained. “The notification solutions of Cassidian Communications seamlessly integrate with building management systems that moni-tor power, diesel tanks and HVAC, and when certain conditions are met, trigger pre-determined alerts.”
Cooper Notification does mass notification and emergency com-munications. Vice President of Marketing Ted Milburn said Cooper does indoor, outdoor and communication on personal devices like laptops, smartphones and cell phones.
The hi-res “map” graphic articulates the multi-tenancy benefit of the AtHoc Solution, articulating the ability to support many widely geographically-dispersed units within an organization while sustaining multiple communications channels and devices, where the needs may vary for each location. [Photo courtesy of AtHoc]
Ted Milburn
Dubhe Beinhorn
www.M2VA-kmi.com6 | M2VA 16.6

“We work with indoor paging units, giant voice and large horns for outdoors and voicemail, email and screen pop-ups,” Milburn said. “It’s important to manage all three environments and to get the right mes-sage out fast, because in a hospital an emergency can be over very fast.” Cooper tools can be used to communicate with either hospital staff or with the public.
Cooper usually works with integrators to provide turnkey solutions to hospitals. “We have done a voice tower in a war zone for the military and do a lot of work for the military in battle areas,” Milburn noted.
Customers increasingly want to manage all emergency communi-cations at one push of a button and make this easy for less-trained staff to do. “You need to make all the elements work together,” Milburn said. “We don’t recommend you rip out your infrastructure and install our equipment, but it is important to integrate all the elements.”
Alertus sees a lot of interest from both military units and civilian hospitals but so far has not sold its system to military hospitals. Vice President of Homeland Security Solutions Rick Tiene thinks these would be a natural for Alertus products.
“We are most well known for our Alert Beacon,” Tiene said. The beacon, about 9 inches across, mounts on a wall. It is ringed with light-emitting diodes that flash different colors and has a screen in the middle that displays emergency messages and instructions.
“Instead of a fire alarm, which gives no information, the beacon tells people exactly what to do,” Tiene explained. “Many people do not pay any attention to alarm sounds, unless confirmed.” The beacon can instruct people, for example, to evacuate by a particular exit or to stay in their rooms and lock doors. It can be put in hallways, lobbies or individual rooms.
Alertus also makes desktop alerts with pop-up messages on work-station PCs, customized for location and necessary actions.
Alertus can tie beacons into an existing public address system with a text-to-speech translator so that, as the beacon displays a message, the PA system broadcasts it. Or it can attach a speaker to each beacon for the same dual visual and audible instruction.
Federal Signal offers a notification messaging solution, SmartMsg, that delivers messages by land and mobile telephone, text, email, pager, and PC pop-up to staff, clients and first responders. SmartMsg inter-faces with PA systems, radio networks, Cisco Digital Signs and works with fire alarms, patient-tracking and equipment-monitoring systems.
SmartMsg is used by hospitals such as Ingham Regional Medical Center in Michigan and Riverside Medical in Illinois, and by the Arkan-sas Department of Health.
John VonThaden, vice president for Alerting and Notification Sys-tems, said integration with third-party systems differentiates Smart-Msg. “And we believe recipients should decide how to receive alerts, which can change depending on time or day.” SmartMsg’s customiz-able ScenarioMgr allows automation of standard operating procedures for communications during any scenario.
Currently deploying, SmartMsg 7.0 is a complete ground-up rede-sign of the application. “We’ve raised our dialing capacity to the highest in the industry, added additional security features, built an entire web-based offering, and are just about to roll out a new template manage-ment system for our ExpressMsg tool,” VonThaden said. ExpressMsg allows creation of hotkeys (pre-defined messages) triggered for code events or security situations. O
For more information, contact M2VA Editor Brian O’Shea at [email protected] or search our online archives
for related stories at www.m2va-kmi.com.
www.M2VA-kmi.com M2VA 16.6 | 7

The Army’s combat support hospitals are going to be getting a facelift, at least if the folks at the Army Medical Department (AMEDD) Center and School have their way. AMEDD has been revising the design of the standard Army combat support hospital (CSH) to make it more modular and flexible. With a Department of Defense budget crunch on the horizon, the new CSH could be simpler and cheaper to deploy and operate, while upgrading some of the equipment and technologies used in the CSH.
The CSH is known as a Role III medi-cal facility, so called because it receives
patients in a theater of operation after they have passed through the first two echelons of care and before they are trans-ported, if necessary, to more advanced care facilities in Ger-many and the United States. The Army, Navy and Air Force all currently operate Role III facili-ties in Afghanistan. The Army’s redesign has yet to be approved but is currently being reviewed for possible future deployment.
“The current CSH is a fairly monolithic 248-bed unit,” said Dr. James Kirkpatrick, senior
clinical consultant at AMEDD’s Depart-ment of Combat and Doctrine Develop-ment. “We are trying to change this into
a CSH that can be comprised of several separate components that can be mixed and matched in a flexible and modular fashion. Instead of being of one standard design, the new CSH will be assem-bled with augmentation detachments like a set of lego blocks.”
treating patients in a theater of operation.By peter BuxBauM
M2Va correspondent
James kirkpatrick
www.M2VA-kmi.com8 | M2VA 16.6

If the redesigned CSH eventually sees the light of day, field medical personnel will be able to build a CSH to suit their mission needs. “If the need is for trauma capacity, they can use the surgical detach-ment, which will include additional oper-ating tables and 24 more intensive care beds,” said Kirkpatrick. “If the problem is not trauma but chronic disease or detainee operations, they can use a medical aug-mentation which will give them more beds and more providers but won’t increase the trauma capability.”
The impetus for the CSH redesign was to improve the utility and efficiency of the current CSH. “We never really needed all that capability in theater,” said Kirkpatrick. “We wanted to be able to add a CT scan and a microbiology lab to the CSH. We also want to be able to accommodate the downsizing in personnel and equipment that the Army is undergoing.”
In Afghanistan, the Army operates a Role III facility in Helmand province, while the Air Force’s facility is located at the Bagram air base, and the Navy operates out of a facility in Kandahar that opened in 2010. The Navy facility offers a number of surgical sub-specialties as well as intensive care, related Captain Michael McCarten, the former commanding officer of the Kandahar facility and currently the deputy director of the Medical Resources Plans and Policy Division at the Chief of Naval Operations.
“Kandahar is a very high-end facility,” he said. “We have a medical staff that is very trauma-oriented with four general and three specialty surgeons. Staffing-wise we are prepared for anything. From an equip-ment standpoint, it is state of the art and we are wanting for nothing.”
Kandahar’s high-end trauma bays have access to CT scanners and all the equip-ment necessary to make a quick diagnosis and head the patient off to surgery. “We can get a patient in the door and onto an operating table within 15 to 18 minutes,” said McCarten. “The place is very geared to its mission.”
Role III facilities accept patients that have already been cared for on or near the battlefield. In the Army, the first phase of care involves self care and buddy care. All soldiers are trained on how to clear airways, apply tourniquets and dressings, and extract their fellows from burning buildings and vehicles.
“Every soldier carries a first aid kit and has been trained on how to give aid while suppressing enemy fire,” said Kirkpatrick. “They have more training and carry more equipment at the point of injury than had just a few years ago.”
Also on the battlefield, each squad or crew includes a combat lifesaver who has been trained with additional skills and who carries more equipment. Each platoon includes a combat medic. “Med-ics have to pass training at the level of an emergency technician,” said Kirkpatrick. “They carry a fairly extensive equipment set including fluids for IV or intra-osseous administration, pain meds and antibiotics. The idea is to get the patient to surgeons who can do damage control quickly.”
Damage control, the second level of care, is performed by forward surgical teams, typically located at brigade medical facilities. The next level up from there is the Role III CSH.
The Navy’s Role III facility at Kandahar is unusual in that it is located adjacent to contested areas. “We have experienced evacuation times of 39 minute or less from the point of injury to the operating table,” said McCarten. “It is unprecedented to have this facility so close to the violence.”
The Air Force’s role at Bagram has been focused on the evacuation of patients out of theater and to facilities that offer the fourth and fifth levels of care. The level four facility is located in Landstuhl, Germany, while level fives include the joint Army/Navy medical center in Bethesda, Md., and the burn center at Fort Sam Houston in San Antonio.
The modules for the proposed Army CSH are built around a 32-bed facility which includes two operating tables, an intensive care unit with two beds, and an intermediate care unit with 20 beds. The facility is equipped with a CT scanner, emergency and trauma triage equipment, and a microbiology lab. It is staffed with general, orthopedic and ob-gyn surgeons, two emergency doctors and physician’s assistants, an internist to run the inter-mediate care ward, and an intensive care subspecialist to run the ICU.
The basic field hospital can then be augmented with a number of detachments. “There is a surgical augmentation which doubles the number of operating tables and includes more surgical specialists such
www.M2VA-kmi.com M2VA 16.6 | 9

as urological, thoracic and oral-maxillo-facial,” said Kirkpatrick. “There is an ICU detachment, which adds to that capacity. The medical detachment provides more beds and physicians without increasing the emergency capability. It is also possible to expand the intermediate care ward. You can put together whatever configuration you want to match your requirements.”
The modularity that the Army is seeking with the proposed new CSH is supported by manufacturers of shelter systems that are suitable for use as medical facilities.
DHS Technologies makes the Deploy-able Rapid Assembly Shelter (DRASH) line of shelters, which have been used by the Army to set up medical facilities and tacti-cal operation centers. “Because our sys-tems are modular, you can build any kind of facility you want,” said Ken Hall, the DRASH area west regional manager. The Joint Task Force-Bravo forward surgical team is among the military units to use DRASH shelters for medical facilities.
The DRASH shelter’s components include materials such as titanite,
Private Thai Nguyen of the 369th Combat Support Hospital out of San Juan, Puerto Rico, fastens a tent flap Wednesday afternoon at Foward Operating Base Schoonover, in Fort Hunter Liggett, Calif. The 369th CSH and the 317th Engineer Company helped each other set up their maintenance tents in preparation for their mission during exercise Pacific Warrior 2008. [Photo courtesy of DoD]
Above: PAXLight LED Field Hospital LightLeft: LED stringable shelter lights[Photos courtesy of Jameson]
www.M2VA-kmi.com10 | M2VA 16.6

For more information, contact M2VA Editor Brian O’Shea at [email protected] or search our
online archives for related stories at www.m2va-kmi.com.
a composite that makes up most of the shelter’s frame and is three times stronger than standard 6061 aluminum and has 100 percent memory retention. Xytex is a specially coated fabric that is fire retardant, mildew resistant, water repellent and resistant to abrasion and ultraviolet rays.
Drash recently intro-duced shelters featuring the new Xytex 500 fabric, which uses nanotechnology to provide protection against microbes. “Upon contact with microorganisms, the proprietary formulation in Xytex 500 disrupts the microbes’ cell membrane, resulting in their demise,” said Hall. “Shelters with Xytex 500 can provide a sterile environment where surgeries and other com-plex medical procedures can occur in the field.”
Utilis USA manufactures shelters with a focus on ease of transportability and setup. “Our customers are looking for durable shelters that go up faster,” said Tom Eggers, a company director. “Some-times they want them packed up smaller and more man-portable.” The company design has already been chosen for the Joint Expeditionary Collective Protection program’s standalone medium and large configuration which provides a filtered overpressure and a liner resistant to chem-ical and biological agents.
A 650 square-foot Utilis shelter can go up in three to five minutes, according to Eggers. Utilis was chosen by the Air Force Surgeon General’s Expeditionary Medical Support Health Response Team to provide a leaner, faster and more effective system. “The setup for the entire medical facility was cut down from 24 hours to five hours,” said Eggers. “This is possible because our shelters include fewer parts, most of which are made of robust extruded aluminum. Our patented folding frame is easy to fold and put up and has been proven in the field. The fabric is separate from the frame, which makes it more man portable. The entire shelter can be packed in four bags.”
Utilis recently introduced the Compact TM60 Tall, which facilitates transporting
in the back of an HMMWV or a TRICON shipping con-tainer. The company has not incorporated anti-microbial materials but is considering the introduction of a liner that is resistant to chemical and biological agents.
The Navy is engaged in research and development to make medical equipment more suitable to the aus-tere environments in which field hospitals typically operate. “The Navy has a very robust R&D pipeline,” said McCarten, “where we are always looking at ways to get better. One thing we are investigating is how we make equipment smaller and more capable, more dustproof and shockproof.”
The Army has conducted a series of war fighting experiments to prove out its
notions for the modular CSH. “The experi-ments are essentially scenario-driven war games where we take a hypothetical situation and use our newly designed unit to see whether it provides the right capa-bilities,” said Kirkpatrick.
Among the scenarios tested have been humanitarian assistance following an earthquake, counterinsurgency opera-tions, and forcible entry into a hostile country. In the last situation, “we wanted casualties to be extracted as quickly as possible while making our footprint on the ground as small as could be,” said Kirkpatrick. “We showed with that experi-ment that the modular units allowed us to achieve good clinical outcomes in terms of so the survival of casualties without hav-ing to put a huge amount of force on the ground.”
The Army is currently evaluating the new CSH and will likely decide whether to proceed in the near future. If the answer is positive, the new CSH could be fielded as early as 2015. O
ken Hall
Tom eggers
www.M2VA-kmi.com M2VA 16.6 | 11

ShockIn life, timing can be everything. Meeting that special someone, landing a
dream job, and other blissful happenings often depend on the moment. Unfor-tunately, death can also hang in the balance of a few precious ticks of the clock. This is especially true in matters of the heart. Though, if help arrives quickly, a potentially deadly event can result in yet another positive right-place-at-the-right-time occurrence. In fact, according to the American Heart Association website, “Cardiac arrest is reversible in most victims if it’s treated within a few minutes.”
And treating it with an automated external defibrillator (AED) is prob-ably the easiest and most effective way to reverse the victim’s condition. Even more encouraging is the fact that virtually anybody can operate today’s AED devices. “Ten years ago, AEDs were expensive and designed to be operated only by EMS or medical personnel,” said Greg Slusser, vice president at Defibtech. “We revolutionized the market by designing affordable AEDs that could be used even by non-medical laypersons.”
Combine this ease-of-use revolution with the physiological impor-tance of an immediate response and the result is an exponential increase in saved lives. “A Johns Hopkins study published in the Journal of the American College of Cardiology found that laypersons trained to operate an
AED achieved a survival rate of 40 percent compared to an overall national survival rate of 8 percent,” said Slusser.
“This difference was due to the laypersons having access to an easy-to-use AED onsite rather than having to wait for EMS to arrive. This is important
because sudden cardiac arrest victims must be treated within only a few minutes for best results—about 90 percent of victims who receive shocks within the first
minute after arrest survive, according to the Sudden Cardiac Arrest Association. The chances of survival decrease by 7 to 10 percent with each passing minute. After 10
minutes, less than 5 percent of victims survive.”
watch, Learn—and saVe
Over the course of the last decade, the military also has taken note of the significance of AEDs. “There have been some changes the vendors promote, but the single biggest change for the Navy
would have to be the issuance of a CNO-level policy dictating implementation, directing activities to fund, and directing clear lines of responsibility,”
said Julius L. Evans, public affairs officer for Naval Medical Logistics Command. “Training, access, maintenance and follow-up of use all
have been addressed.”Defibtech and other industry leaders have also worked to
address these types of issues—and more. “We design and manufacture the Lifeline family of AEDs and accessories—and no other product,” Slusser said. “All Defibtech AEDs meet the military ‘shock and drop’ standard: They can be dropped and bumped and still perform reliably when they are needed. Defibtech AEDs have passed vigorous vibra-tion tests for ground, helicopter and jet aircraft and can be safety stored in temperatures ranging from 32 to 122 degrees Fahrenheit. They’re virtually waterproof and dustproof, operate at low and high altitudes (-500
to the SystemsaVing LiVes with aeds.
By J.B. BisseLL, M2Va correspondent
A
www.M2VA-kmi.com12 | M2VA 16.6

to 15,000 feet) and exceeded 1,000 pounds on a crush test.”
In addition to withstanding the harsh environments where the military operates, “AEDs are designed to be used by individuals that are stressed, in a time-critical situation,” Evans said. “The operation has to be simple and mistake proof. It has to be so intuitive that anyone can use it. It has to have such clear instructions that the pads cannot be incor-rectly placed. It has to work in noisy environ-ments and must prevent users from shocking themselves. Design of the simplest of medical devices requires consideration of a multitude of factors, with all of the design integrated to make a usable product.”
As for this type of usable simplic-ity, Defibtech’s relatively new Lifeline View AED—along with the Lifeline Pro and Lifeline ECG—is setting a new standard for providing soldiers in extreme air, sea and land environ-ments with the knowledge and confidence they need to save a life.
“The confidence comes from an innova-tive, exclusive LCD video feature integrated into units that literally shows rescuers how to perform each step of a sudden cardiac arrest rescue with the AED in real time, all in accor-dance with the latest AHA guidelines,” Slusser explained. “The color video is reinforced by loud and clear audio and corresponding text that can be understood in noisy environments. For example, when the audio says and text reads, ‘Place pads on patient’s chest,’ the video shows exactly where to place the pads.”
Embedded help videos also can be used to review the critical steps and allow men and women to become more comfortable with the AED before they have to actually use it during truly life-threatening circumstances. “At any time, a potential user can watch the help videos right on the AED screen, to review everything from where to place the pads on the patient to how to perform CPR,” added Defibtech co-founder and chief executive offi-cer Dr. Glenn Laub, who also is a professor and chairman of cardiac surgery at Drexel College of Medicine and clinical section chief at Hahn-emann University Hospital in Philadelphia. “This gives people reassurance that during the stress of an actual rescue they will be ready to confidently provide life-saving assistance.”
pLug and pLay
Sometimes life-saving assistance doesn’t need to get as far as an AED. “Not every victim of sudden cardiac arrest will need a shock, but all will need CPR,” explained Brenda M. Butler,
vice president of government sales for the Zoll Government Division. Obviously, then, high-quality CPR improves patient outcomes. “That why Zoll builds Real CPR Help into all of its AEDs and virtually every defibrillator the company sells. Real CPR Help technology provides real-time feedback on CPR quality.”
That feedback includes compression depth and rate indicators, a display of the elapsed time between com-pressions, and more. In other words, the responder can actu-ally see what’s happening on the monitor screen to ensure that his or her efforts are as effective as possible.
The Propaq MD, Zoll’s lat-est addition to their product portfolio, was designed specifi-cally for deployed military and has all the functionality of the company’s popular Propaq M monitor, but adds a defibrillator. So, if it’s determined while performing and monitoring CPR that a shock is needed, the capability to do just that is right there. “In addition, Zoll offers patented See-Thru CPR technology, which filters out compression artifact on the ECG monitor, thereby reducing the duration of pauses during resuscitation,” said Butler. “While pauses in CPR are inevitable, with See-Thru CPR technology, a filtered signal is displayed on the screen, allowing the rescuer the ability to determine whether an organized, shockable rhythm has developed.”
Monitoring CPR action, filtering out pulse rhythms, and providing crucial information about whether a heart can be shocked back to normal is multi-tasking at its best, but Butler maintains that for the first responder, who may or may not be trained medical personnel, it’s all still quite straightforward. “Whether it is a ‘lay-rescuer’ removing the Zoll AED from a wall on a military base, or a trauma surgeon using the Propaq MD in a deployed environ-ment, the device should be intuitive and easy to use,” she said.
Even Zoll’s more “advanced monitoring/defibrillation technology permits true ‘plug and play’ capability,” Butler added. “When an SpO2 sensor, or invasive blood pressure cable, is connected to the Propaq MD, the waveforms are automatically displayed on the monitor screen, so there’s no need to press any addi-tional buttons. To avoid information overload, the Propaq M and Propaq MD allow you to configure the device to have a large, simple numeric display for basic rescuers, or a more advanced screen, with multiple waveforms, for
the most critical of patients. It is this custom-ization that provides the intuitive feel.”
good things, sMaLL packages
Saving a life is a fundamentally spontane-ous event, so this intuitive feel is essentially a required element in any of the necessary equip-
ment. Like other companies, Cardiac Science guarantees simplicity is built into all of its devices. “Our goal is to ensure each of our products are the easiest to use in the indus-try,” said Pete McLean, sales manager for Cardiac Science’s U.S. Department of Defense/Federal Government division. “For example, our Powerheart AED G3 Plus Automatic can deliver a life-saving shock to the patient without the user
having to press a shock button. And our Rescue Coach technology demonstrates the effective-ness of our voice prompts.”
Portability is another area in which Cardiac Science excels. “One of our newest products, CareCenter MD, is a 12-lead ECG that’s the size of an iPhone,” McLean said. “It’s literally changing the way medics look at potential cardiac-related events. With its compact size, weight and features, medics have told us that CareCenter MD is the first truly portable, expe-ditionary 12-lead ECG.”
Small packages, though, often contain some of the best rewards. “As a computer-based product, a medic can proactively monitor a patient; view a real-time/continuous 12-lead in either resting, rhythm, stat or stress con-figurations; group leads anyway they choose; measure intervals; look at average beats; and customize reports, data and patient details. The computer software will even provide a diagno-sis,” McLean added. “Further, a servicemember can print a strip, save and compare ECGs, and even email the ECG anywhere they choose.”
Finally, the CareCenter MD software has redundancy features already built in. “Data-base replication allows workstations to operate independently and share data when connected to the network,” explained McLean. “Not only does this ensure data availability, but it enables medics to have a complete view of a service person’s cardiac history no matter where they are.”
And perhaps more importantly, no matter when a life-threatening episode takes place, because when it comes to saving soldiers’ lives, timing truly is everything. O
to the System
Brenda M. Butler
www.M2VA-kmi.com M2VA 16.6 | 13

All Platform Litter
Ferno Military Systems’ AllEvac All Platform Evacuation (APE) Litter, is designed for dismounted, vehicle, helicopter and fixed wing operations. The APE Litter’s folding handles make it optimum for every ground or air platform used by U.S. forces. Self-leveling feet allow for rapid insertion into to rotary wing platforms without gouging or scratching the aircraft’s floor. Quick-release hinges allow the APE to be easily folded or deployed in seconds, while the APE’s unique spreader bar design provides a simple and rapid lock-out or folding process.
Aircraft aluminum construction provides low weight and durability in extreme conditions. The entire APE Litter is infinitely sustainable with removable and replaceable litter beds, as well as field exchangeable frame components. The handles and frame sections can be field replaced at any time utilizing a Phillips head screwdriver and a 3/8th wrench or nut driver. Also available is the new APE Litter spare parts kit, which allows deployed units to utilize a parts cache. In addition, deployed units may cannibalize one or more damaged litters for parts, in order to keep the remainder of inventory in service. The APE is the ultimate “full system” NATO combat litter,” and represents the future of tactical litter evacuation.
Carson Chinn; [email protected]
Defense Against Hemorrhage
Combat Gauze from Z-Medica is an advanced hemostatic agent combined with the simplicity of gauze. It is the first gauze to stop arterial and venous bleeding rapidly. Designed at the request of military end-users, now standard issue to all branches of the U.S. military and is recommended by the Committee on Tactical Combat Casualty Care as first-line treatment for life-threatening hemorrhage in wounds not amenable to tourniquet placement. Powerful, yet cool with no exothermic reaction, so it won’t burn, Combat Gauze is pliable to pack into even penetrating traumatic wounds. This product is flexible to cover any size or shape. Gauze is easy to use and easy to remove. It is so intuitive and greatly improves hemorrhage control in the most demanding tactical setting. Combat Gauze does not break down or dissolve in the wound, alleviating emboli concerns. Its ease of use makes it ideal for issue to medical and non-medical personnel alike.
Jason Cauley;[email protected]
Tactical Field Care
Designed by combat medics and DARPA specifically for tactical field care when size, weight and simple/rapid use are paramount, the SAVe from AutoMedx replaces bag-valve
devices. It is no longer necessary to take compressed, flammable gas onto the battlefield. Ventilations are provided through the included four-legged head strap mask, or linked directly to an ET tube or other airway adjunct. Controls consist of a single knob, keeping the training burden low. The sensors and suppressible alarms allow for spontaneous breathing and ensure proper tidal volume is reaching the patient. The preset pressure limit prevents over inflation.
Manually bagging a patient prevents responders from performing other critical tasks and has been linked to a high incidence of gastric insufflation, hyperventilation and increased intra-thoracic pressure leading to decreased coronary perfusion pressure.
A rechargeable battery driven pump delivers an American Heart Association compliant tidal volume and respiratory rate for 5-plus hours. It is cost effective by improve triage capabilities and elevating the standard of care. While the SAVe accepts supplemental oxygen input, no compressed gas is required for it to ventilate a patient.
James Evans;[email protected]
www.M2VA-kmi.com14 | M2VA 16.6
VITAL SIGNS

Water Filtration
The Seldon WaterBox 300 MIL can turn 30,000 liters of raw water into water that exceeds USEPA Drinking Water standards. The self-priming system can pump up to 4.3 meters of lift at a rate of 2.3 liters per minute. Setup time is less than five minutes.
Seldon uses the material properties and filtering capabilities of the carbon nanotube. The result is the Nanomesh Filtration Technology. The Seldon WaterBox removes 99.9999 percent of bacteria, 99.99 percent of viruses, and 99.9 percent of cysts, as well as reducing chemicals and harmful materials like mercury and lead without chemicals or heat.
The WaterBox is portable, rugged and dependable. It’s been tested in every possible field situation, and used by the Naval Special Warfare Group, the U.S. Army Special Forces, the U.S. Marine Corps and the U.S. Air Force.
Mike Brown;[email protected]
Collecting Patient Data
The WVSM from Athena GTX is a medical monitoring unit that wirelessly collects patient vital signs data from a blood pressure cuff, pulse oximetry clip and a lead electrocardiogram (ECG) configuration. The WVSM is worn by the patient, stays with the patient and begins to record data as close as possible to the point of injury. The device stores these data and when in range of a PDA or computer running companion software, it wirelessly transmits and displays the information, including: Plethysmographic (pleth) waveform, ECG waveform, heart rate or pulse rate, NIBP (non-invasive blood pressure), diastolic, systolic and mean arterial pressure. The display also has data sections requiring manual inputs such as temperature, Glascow Coma Score and respiration rate.
Mike Langley; [email protected]
Lifesaving Needle
The Tactical Advanced Lifesaving IO Needle (TALON) intraosseous infusion system from Vidacare is the next generation IO device for the delivery of lifesaving fluids and medications. Not only does the TALON provide first responders with rapid and accurate IO access, it is FDA-cleared to access all seven IO sites on the human body. There’s no powered tools or multiple needles necessary. One TALON means universal IO access.
With seven-site access in one solution, why carry around multiple needles and tools when one system is all you need? More possible IO sites mean more treatment options. The TALON even meets all of the Committee on Tactical Casualty Care preferences for IO devices.
Moreover, the TALON is skill level 1 applicable. Simple steps for use mean simple insertion. Instruction and training ensure that every person on the battlefield can utilize the TALON. Use of the sternal stabilizer allows for easy, minimal pressure insertion.
The TALON packs light, tight and compact in 1.4 ounce. Use of the TALON means needing fewer types of needles. And there’s no special removal tool that has to be brought along.
Ruben Trevino; [email protected]
www.M2VA-kmi.com M2VA 16.6 | 15
Compiled by KMi Media Group staff

Vice Admiral Matthew L. Nathan is the 37th surgeon general of the Navy and chief of the Navy’s Bureau of Medicine and Surgery.
Nathan received his Bachelor of Science degree from Georgia Tech, and his Doctor of Medicine from The Medical College of Georgia in 1981. He completed internal medicine specialty training in 1984 at the University of South Florida before serving as the Internal Medicine department head at Naval Hospital Guantanamo Bay, Cuba. In 1985, Nathan transferred to Naval Hospital, Groton, Conn., as leader of the Medical Mobilization Amphibious Surgical Support team. In 1987, Nathan transferred to Naval Medical Center San Diego as head, Divi-sion of Internal Medicine with additional duty to the Marine Corps, 1st Marine Division.
In 1990, he served as a department head, Naval Hospital Beaufort, S.C., before reporting to Naval Clinics Command, London, U.K., where he participated in military-to-military engagements with post-Soviet Eastern European countries. In 1995, he was assigned as special-ist assignment officer at the Bureau of Naval Personnel, providing guidance to over 1,500 U.S. Navy Medical Corps officers. In 1998, he accepted a seat at the Joint Industrial College of the Armed Forces located in Washington, D.C., graduating in 1999 with a master’s degree in “Resourcing the National Strategy.” Nathan went on to serve as the fleet surgeon, Forward Deployed Naval Forces, commander, U.S. 7th Fleet, aboard the flagship USS Blue Ridge (LCC 19), out of Yokosuka, Japan. In 2001, he transferred as deputy commander, Navy Medical Center Portsmouth, Va.
In 2004, Nathan assumed command of Naval Hospital Pensacola with additional oversight of 12 clinics in four states where he oversaw Navy medical relief efforts following Hurricanes Ivan, Dennis and Katrina. Despite all facilities receiving crippling blows, his command still garnered the TRICARE/DoD award for “highest patient satisfac-tion in a medium-sized facility.” In June 2006, he transferred as the fleet surgeon to the commander, U.S. Fleet Forces Command, instru-mental in organizing the Fleet Health Domain integration with the Fleet Readiness Enterprise while providing medical global force man-agement. In 2007, Nathan was assigned as commander, Naval Medical Center Portsmouth and Navy Medicine Region East with command of over 18,000 personnel and an operating budget exceeding $1.2 billion.
Nathan also served as commander, Walter Reed National Military Medical Center and Navy Medicine, National Capital Area, where he was the Navy component commander to the largest military medical integration and construction project in Department of Defense history.
Nathan is board certified and holds Fellow status in the American College of Physicians and the American College of Healthcare Execu-tives. He also holds an appointment as clinical professor of medicine at the Uniformed Services University of the Health Sciences. He is a
recipient of the American Hospital Association “Excellence in Leader-ship” award for the Federal Sector.
Nathan’s personal awards include the Distinguished Service Medal (1); Legion of Merit (5); Meritorious Service Medal (2); Navy and Marine Corps Commendation Medal, and Navy and Marine Corps Achieve-ment Medal (2).
Q: Can you give an overview of the Bureau of Medicine and Surgery [BUMED]?
A: The Navy Bureau of Medicine and Surgery is the headquarters com-mand for Navy and Marine Corps medicine. BUMED is the site where the policies and direction for Navy Medicine are developed to ensure our patient and family-centered care vision is carried out. BUMED exercises direct control over naval hospitals, medical centers, dental clinics, pre-ventive medicine units and technical schools for Medical Department personnel both inside the U.S. and around the world. BUMED also maintains command and control of many of the lower echelon support commands that are not involved with direct patient care, including the Navy Medicine Education and Training Command, Navy and Marine Corps Public Health Center, Naval Medical Research Command, Naval Medical Logistics Command, and several others. BUMED is responsible for all medical support for the U.S. Marine Corps and the U.S. Navy.
Vice Admiral Matthew L. NathanSurgeon General of the Navy
Chief of the Navy’s Bureau of Medicine and Surgery
www.M2VA-kmi.com16 | M2VA 16.6
Force ProtectorEnsuring Patient and Family Centered Care
Q&AQ&A

The BUMED headquarters has nine codes, or departments, that develop policy for a wide range of topics for our lower echelon com-mands to execute. The nine codes are:
• M1: Manpower and Personnel —Total Force• M2: Research and Development• M3: Medical Operations• M4: Logistics and Facilities• M5: Future and Strategic Planning • M6: Chief Information Office• M7: Education and Training• M8: Comptroller and Resource Management• M9: Wounded, Ill and Injured
Within our Total Force structure, we also maintain a robust staff dedicated to the interests and requirements of our many Navy Medi-cine reservists. This team has been particularly important throughout the past 10 years of conflict as many reservists who represent a unique and diverse population have been called up to deploy.
Q: What do you see as the main role or function of Navy Medicine?
A: The foundation of Navy Medicine is force health protection and direct support to the warfighter. It’s what we do and why we exist. We are in the readiness business. Navy Medicine operates forward and is globally engaged, no matter what the environment and regardless of the challenge. Whether it is on the sea, above the sea, below the sea, on the battlefield or on the homefront, Navy Medicine enables our sailors and Marines to carry out their mission. From the most advanced medi-cal suites and staffs serving on amphibious ships, to the flight surgeons supporting the naval aviation enterprise, to the independent duty corpsman serving in submarines, or to the Navy corpsman embedded with Marines or special forces; Navy Medicine enables the warfighter. Where ever a sailor or Marine goes, Navy Medicine is there.
In executing our force health protection mission, the 63,000 active duty and reservists, government civilians and contractors of Navy Medicine are engaged in all aspects of expeditionary medical operations in support of warfighter. The continuum of care we provide includes all dimensions of physical and mental well-being. Nowhere is our com-mitment to force health protection more evident than in our active engagement in military operations in Iraq and Afghanistan. As these overseas contingency operations evolve, and in many respects become increasingly more dangerous, we are seeing a burgeoning demand to provide expeditionary combat casualty care in support of joint opera-tions. The Navy Medicine team of doctors, nurses, corpsmen, dentists and mental health providers is working in tandem with the Army and Air Force medical personnel and coalition forces to ensure the physical and mental well-being of our troops and civilians alike.
Mission readiness for our sailors and Marines at home and abroad is our first priority, but there is no greater honor than the opportunity to provide care to our wounded, ill and injured. They are heroes and we, who are fortunate enough to care for them, understand this responsi-bility. As our wounded warriors return from combat to begin the heal-ing process, they deserve a seamless and comprehensive approach to their recovery. We help them to heal in body, mind and spirit. Our focus is multi-disciplinary-based care, bringing together medical treatment providers, social workers, case managers, behavioral health providers and chaplains. We are working closely with our line counterparts with programs like the Marine Corps’ Wounded Warrior Regiments that
coordinate with battalion surgeons, deployed units, and medical treat-ment facilities to set up anticipated medical appointments, ensuring a majority of medical needs are assessed prior to demobilization.
Q: As the Navy surgeon general, what are your priorities and goals?
A: Since becoming the Navy surgeon general in November 2011, my priority has been to ensure that Navy Medicine is strategically aligned with the imperatives and priorities of the Secretary of the Navy, Chief of Naval Operations and Commandant of the Marine Corps. We are fully engaged in executing the operational missions and core capabilities of the Navy and Marine Corps—and we do this by maintaining warfighter health readiness, deploying forward and delivering the continuum of care from the battlefield to the bedside while protecting the health of all those entrusted to our care.
My focus remains in alignment with our Navy and Marine Corps leadership as we support the defense strategic guidance. To ensure the fulfillment of our mission, I have outlined three strategic goals for the BUMED enterprise: readiness, value and jointness.
Readiness: We will provide agile, adaptable and scalable capabili-ties prepared to engage globally across the range of military operations within maritime and other domains in support of the National Defense Strategy. The ability to be ready and prepared to respond to the needs of our nation is inherent in our ethos. We must maintain a persistent state of high readiness so that we are always ready to respond to needs to support everything from kinetic action to humanitarian assistance and disaster response missions. Readiness is the hallmark of Navy Medicine.
Value: We will provide exceptional value to those we serve by ensur-ing full and efficient utilization of our services, highest quality care through best health care practices and best use of resources. When we say “value,” we are asking our enterprise to consider the dynamic of cost, capability and quality in all we do. Providing simply everything at any cost is not sustainable.
Jointness: We will lead Navy Medicine to jointness and improved interoperability by pursuing the most effective ways of mission accom-plishment. The synergy of creating efficiencies, removing redundancies and allowing transparency will elevate care and reduce costs.
Navy Medicine must promote healthy Naval forces to ensure warfighters are prepared to execute their mission. The Naval forces require the right medical capabilities to deliver consistent, appropriate and timely health care services across the entire range of joint military operations, which is why I am making it a priority to focus on jointness as we adapt Navy Medicine and plan for the future. In the upcoming years, Navy Medicine will focus on providing military health support for medical stability operations; maintaining health deployment readi-ness—the medically deployable status of all active duty and reserve servicemembers; and minimizing casualties in the deployed forces through prevention of disease and non-battle injuries. In addition, Navy Medicine provides expeditionary combat casualty care in sup-port of requirements across the spectrum of joint military operations, ensuring that functional operating room and ICU beds are in place to meet warfighter requirements.
Q: What is on the horizon for BUMED in the coming years?
A: Navy Medicine is the pinnacle of excellence—answering the call across any dynamic—from kinetic operations to global engagement. Our health care is patient-centered, preserves health and maintains
www.M2VA-kmi.com M2VA 16.6 | 17

readiness. Agility, professionalism, an ethos of care and the ability to deploy to any environment or sea state are our hallmarks. Moving for-ward, we must innovate, position our direct care system to recapture private sector care, and deliver best value to our patients. We must inte-grate the incredible strides we have made in comabat casualty care in the Iraq/Afghanistan theater to be deployable to any scenario or region.
Navy Medicine would not be able to accomplish its mission without a robust research and development [R&D] community. The ongoing work of our researchers is having a direct impact on the treatment we are able to provide, from the battlefield to the bedside. Many wounded warriors are walking, talking and leading productive lives today because of the research and medical advance-ments in wound management, wound repair and reconstruction, as well as extremity and internal hemorrhage control and phantom limb pain in amputees. Our R&D programs are truly force multi-pliers to Navy Medicine’s success and enable us to remain agile in the world-class health care we provide to our servicemembers and beneficiaries. How military medicine takes on this challenge will set the stage for decades to come, especially with respect to the quality, accessibility and reliability of support veterans and their families will receive.
BUMED will examine its patient- and family-centered care model. Patient- and family-centered care is Navy Medicine’s core concept of care. It identifies each patient as a participant in his or her own health care and recognizes the vital importance of the fam-ily, military culture and the chain of command in supporting our patients. Navy Medicine will accomplish this through its Medical Home Port model and improved access to care at Navy Medicine facilities. The naval forces will have the right medical capabilities to deliver consistent, appropriate and timely health care services.
Additionally, Navy Medicine must maintain the right workforce to deliver medical capabilities across the full range of military operations through the appropriate mix of accession, retention, education and training incentives. Navy Medicine will establish an overarching organizational structure that directly aligns all aspects of manpower, personnel, training and education resulting in cohesive development, oversight and execution of the total force strategy for Navy Medicine. My goal is to achieve a 95-100 percent manning rate and establish and implement a comprehensive train-ing and education strategy for the Navy Medicine enterprise.
Q: How does BUMED work with industry to ensure medical facili-ties are properly equipped to deliver quality health care?
A: BUMED centrally manages equipment purchases through its subordinate command, the Naval Medical Logistics Command [NMLC]. Through this command, we are able to stay abreast of advancements in medical equipment requirements by working with industry and clinicians through routine collaborations.
NMLC has a staff of logisticians, analysts, clinical engineers, biomedical equipment technicians, contracting officers and attor-neys dedicated to helping customers define their requirements and enhance the standard of care, understanding the marketplace to support the requirements, ensuring patient safety and providing cost-effective, efficient contracts to satisfy those requirements.
NMLC also supports a number of high profile programs that include engineering support for medical and dental space configu-ration for new ship construction and maintaining authorized medi-cal and dental materiel allowance lists for the operational forces.
Also, in the spirit of “jointness,” Navy Medicine is actively engaged with the other services and DoD Health Affairs to find transparent com-mon practice, efficiencies, standardization and remove redundancies.
Q: How important are international partnerships to BUMED?
A: We are a maritime nation and a maritime service. It is in our DNA to be forward, engaged, and to build and sustain collaborative energy and partnerships throughout the world. Over 70 percent of the Earth’s surface is covered by water, more than 80 percent of the Earth’s popu-lation lives near a coastline, and more than 90 percent of the world’s commerce travels by sea. The naval mission of maintaining the safety and security of our sea lanes—being 100 percent “on watch”—and Navy Medicine’s role in keeping our sailors and Marines fit and ready to do just that has never been more important. We can’t do this without our worldwide partners.
Navy Medicine’s mission is one with a truly global footprint. We are forward deployed with operating forces overseas and our research units provide a global health benefit around the world. Navy Medicine personnel serve as ambassadors worldwide and are the heart and soul of the U.S. Navy as a “Global Force for Good.” Building partnerships around the world is imperative to our ability to meet mission and be a responsive and effective organization. I believe this to be so important that I recently stood up an office dedicated to Global Health Engagement which will develop our policies and build lasting partnerships worldwide.
Global health engagement includes our humanitarian assistance/disaster response [HA/DR] missions. These HA/DR missions directly support the Navy’s Maritime Strategy and they continue to expand because they have proven to be highly successful in building global rela-tionships. With past support to critical missions like Operation Unified Response in Haiti following the 2010 earthquake, Navy Medicine serves the international leader in HA/DR response.
More recently, Navy Medicine personnel provided essential support to Operation Tomodachi after the devastating earthquake and tsunami in Japan in 2011. As the foremost experts in radiation health issues, our Navy Medicine radiation health officers and radiation health technicians answered the international call for assistance to Japan and provided paramount support following the Fukushima nuclear plant disaster. They provided onsite monitoring of radioactive fallout, counseling to those affected and advice to Navy and Marine Corps commanding gen-erals and combatant commanders in the Pacific area of responsibility. Their presence and expertise provided relief and solace to an extremely concerned population.
The Navy hospital ships also conduct planned deployment humani-tarian assistance missions where they work with local ministries of health to bring care to the people of foreign nations. USNS Comfort’s mission in Central and South America and the Caribbean for Continu-ing Promise 2011, as well as USNS Mercy’s 2012 Pacific Partnership mission to Southeast Asia, provide further evidence of our contin-ued commitment to the global efforts to foster security and stability worldwide. Our hospital ships are executing our Maritime Strategy by building the trust and cooperation we need to strengthen our regional alliances and empower partners around the world. With each success-ful deployment, we increase our interoperability with host and partner nations, non-governmental organizations and the interagency.
Q: How does BUMED share resources in reference to the Veterans Administration and Department of Defense Health Resources Shar-ing and Emergency Operations Act?
www.M2VA-kmi.com18 | M2VA 16.6

A: BUMED and Department of Veterans Affairs have a long history of health care resource sharing, which was mandated by Public Law 97-174, “The Veterans Administration and Department of Defense Health Resources Sharing and Emergency Operations Act.”
The sharing of Navy and VA health care resources has resulted in over 50 sharing agreements, two joint ventures and one fully inte-grated medical facility. The intent of resource sharing is to promote cost-effective use of federal health care resources by minimizing duplication and underuse of health care resources while benefiting both VA and DoD beneficiaries.
These sharing arrangements cover services such as medical/sur-gical, IM/IT data sharing, pharmacy, radiation therapy, compensation and pension exams, mental health, sleep lab, mammography, labora-tory, optometry, audiology, pathology, pastoral care training, CT/MRI scans, training and equipment.
In addition to the Department of Defense Health Resources Shar-ing and Emergency Operations Act, National Defense Authorization Act for fiscal year 2010 formalized the partnership by authorizing the establishment of a five-year demonstration project. This first-of-its-kind project integrated the North Chicago VA Medical Center and Naval Health Clinic Great Lakes facilities into a single integrated health system, creating the Captain James A. Lovell Federal Health Care Center.
Q: Can you describe BUMED’s involvement in the Joint Incentive Fund [JIF]?
A: BUMED and VA have partnered in many Joint Incentive Proj-ects since 2004. Completed projects become sharing agreements to continue the services started by the JIF project between the two medical facilities. Examples of past JIF projects are: women’s health center, mammography/stereotactic mammography, joint fixed MRI, dedicated fiber-optic connectivity, hospitalist program, digital radi-ography, mobile MRIs, pastoral care training (specific to wounded warriors), sleep lab services.
Q: What are the challenges of maintaining a continuum of care from the battlefield to the bedside?
A: The challenges of the continuity of care begin at the point of injury and are particularly piqued by the severity of the injuries that are sus-tained in a theater of war where the improvised explosive device is the enemy weapon of choice. Amputations, coupled with genitourinary injuries and traumatic brain injury, have been the signature injuries of this conflict. In those first moments post-injury, body armor, hemorrhage control and the first responder training has proven to be critical at a time when survival is not guaranteed.
Salvage surgery, initially completed in the first minutes or hours after the casualty’s arrival at a Role 2 or Role 3 facility, and repeated at 48 hour intervals throughout theater evacuation, generates a post-operative patient with a myriad of clinical requirements that must be met to sustain life. The services have developed an ‘en route critical care’ support capability in Afghanistan to provide lifesaving interven-tions during rotary transport between Role 2 and Role 3 facilities. Following surgery at the Role 3, it is in this phase of the timeline that the Air Force critical care air transport [CCAT] capability is so vitally important. Essentially, the Air Force has developed an ‘ICU in the air’ capability that provides the opportunity for very elaborate and sophisticated interventions. Once in the CCAT system, casualties are
transported back to CONUS where they are admitted to Role 5 facili-ties such as Walter Reed National Military Medical Center.
The sequence of events described above with the interventions that can be completed at each step along the way constitutes the continuity of care and makes the trauma system currently func-tioning in Afghanistan the most effective trauma system in the world. The unprecedented survival rates being recorded are clearly the product of the training and utilization of our medical personnel and the skill and resilience of military aviation personnel.
Q: How do you see Navy Medicine evolving over the next five years?
A: Organizations should change with time. It is our responsibility to constantly evaluate our structure, identify areas of improve-ment and act on those opportunities. Earlier this year I directed senior Navy Medicine leadership to explore realignment options that would result in a more effective, efficient and responsive orga-nization. I believe in an empowered lean and mean headquarters element that listens to the field and provides guidance through coherent codified channels. Tactical and strategic alignment from headquarters to the treatment facility, battlefield, or ship is impera-tive.
As a result, we are engaged in executing a realignment plan for the Navy Medicine enterprise that will meet these requirements. The realignment is designed to enhance accountability, command and control, and ensure representation of Navy equities both across the enterprise and throughout the fleet.
This realignment is also closely linked to my strategic vision for Navy Medicine. We must concentrate on bringing more value and improving jointness while maintaining a high state of medical readiness for our Naval forces that our nation demands.
The biggest change occurred in July when Navy Medicine Support Command [NMSC] was re-scoped and renamed to Navy Medicine Education and Training Command [NMETC]. NMETC’s primary focus is on education and training. The command is headquartered in San Antonio, Texas, and has detachments in Jacksonville, Fla., and Bethesda, Md. NMETC will work closely with BUMED to ensure our medical personnel continue to be equipped with the best training military medicine can provide. They will also work closely with leadership at the Medical Education and Training Campus in San Antonio to ensure our Navy personnel are well-sup-ported and that we maintain seamless and focused training for our corpsmen who keep our sailors and Marines medically fit and ready.
Many of NMSC’s former responsibilities will be absorbed by BUMED codes, with a number of lower echelon commands func-tionally realigned to codes within BUMED. The realignment also established two new codes; M2, which will manage all research and development, and M7, which will manage education and training.
In closing, Navy Medicine is an agile and powerful health care team because of our professional and dedicated shipmates, all of whom are working around the globe to provide outstanding health care and support services to our beneficiaries. As we turn the cor-ner on a decade of war, our heroes are celebrated and our losses are mourned … we have been all in, heavily deployed, and Navy Medi-cine remains strong, capable and mission-ready to deliver world-class care, anytime, anywhere. I have never been more proud of the men and women of Navy Medicine. In any corner of the world, or any sea state … when you need them, they will deliver. O
www.M2VA-kmi.com M2VA 16.6 | 19

Q: Can you give an overview of Army Medi-cine in Europe?
A: Let me put the depth and breadth of Army Medicine in Europe in perspective by sharing a small part of what our dedicated professionals do on a daily basis.
Today, thousands of pounds of medical supplies and equipment are being distributed to hundreds of locations over three different continents. These shipments provide vari-ous units, including 162 embassies, with the supplies they need to care for American men and women serving in U.S. European Command, U.S. Africa Command and U.S. Central Command areas of responsibil-ity. Literally hundreds of critical medical units and missions are made possible by the hardworking professionals at the U.S.
Army Medical Materiel Center, Europe. The USAMMCE team is also responsible for medical maintenance and makes more than 200 pairs of eyeglasses a day for soldiers, sailors, airmen and Marines.
Today, wounded warriors evacuated from Afghanistan will arrive at Landstuhl Regional Medical Center where they will receive the absolute finest medical care in the world. Landstuhl Regional Medical Cen-ter is the only overseas U.S. Level I trauma center and serves as the ROLE IV strategic evacuation center for AFRICOM, CENT-COM, EUCOM and SOCOM. Elsewhere in the same hospital, hundreds of people will arrive for outpatient care delivered by a dedicated team of soldiers, airmen, sail-ors, Marines, civilians and local nationals. Landstuhl is EUCOM’s only medical center,
performing 25 operations and delivering three babies daily, as well as providing a full array of specialty care for servicemembers and families serving in Europe.
More than 1,500 dental procedures will take place today at 20 clinics oper-ated by Europe Regional Dental Command throughout Germany, Italy and Belgium. Warrior-focused oral health care is their mission—offering a full range of compre-hensive and specialty dental services. Our dental professionals serve a key role in sol-dier readiness. USAREUR has the highest dental readiness rate in our Army.
Today ERMC medics are in various stages of deployment—either preparing to go, are already downrange, or are returning home. Other medics are likely engaging in valuable combined training with coalition
eMpowering indiViduaLs to MoVe froM passiVe recipients to actiVe participants in their heaLth.
Command Profile
www.M2VA-kmi.com20 | M2VA 16.6

partners such as the Germans, Latvians, Hungarians, British and others. The 30th Medical Command provides deployable medical assets in support of USAREUR and other contingency operations and strengthens relationships with coalition partners in the region through medical training opportunities.
In the Warrior Transition Battalion-Europe [WTB-E], wounded, ill or injured soldiers are preparing for the next stage of their lives while they focus on healing. Some of them are heading out for scuba diving, ropes courses, kayaking, or other activities designed to build skills and con-fidence that will be useful whether the sol-diers return to duty or transition to civilian life. Others will be meeting with their care teams, setting goals and tracking progress. Thanks to the WTB-E, these soldiers are able to focus on healing while preparing for success when they take the next step in their career/life.
More than 40 installation food inspec-tions will take place today performed by the team at U.S. Army Public Health Command Region–Europe. These inspections are crit-ical to ensuring safe food for America’s sons and daughters serving in the region. Veterinary medicine professionals with the PHCR-E team will complete more than 200 veterinary animal health visits today. Most of the time, the PHCR-E team operates behind the scenes. However, their mission impacts everyone serving in our region.
Currently, research projects are under-way with the U.S. Army Medical Research Unit–Europe. This small team of men and women is busy developing effective behav-ioral health assessment tools and analyzing data for policy recommendations. Their insights are critical in assessing strate-gies that will lead to the best care we can offer our warriors before, during and after deployment.
Hundreds of soldiers, family members, and other beneficiaries will arrive for an outpatient visit today at one of LRMC’s nine clinics in Germany, Belgium and Italy; at the Vicenza Health Center in Italy, or at one of the Bavaria Medical Department Activity’s seven clinics throughout southern Germany. Our patient care teams see more than 3,500 soldiers, family members and other patients daily. More than 2,300
prescriptions will be filled today and more than 1,900 clinical lab tests completed.
As you can see, the mission for Army Medicine in Europe is vast, covering the U.S. European Command, U.S. Africa Command, and U.S. Central Command areas of responsibility. This narrative barely scratches the surface, but I can tell you that we have an impressive Army Medicine team focused on patient-centered care every day.
Q: What programs or initiatives do you plan to implement over the next 12 months?
A: Let me begin with some quotes from our MEDCOM Commander/Army Surgeon General, Lieutenant General Patricia D. Horoho:
In order for us to get to health, we must empower the population we serve, move beyond the 100 minutes, and influ-ence behaviors in the LifeSpace to move forward from a healthcare system to a system of health. –Horoho
If we want to move from health care to health, we need to influence … our soldiers, retirees and family members’
Colonel Jeff Clark is a graduate of David-son College, East Carolina University School of Medicine, the U.S. Army Command and General Staff College and Army War College. Clark earned a Master of Public Health at the University of Washington and a Master of Strategic Studies at the Army War College. He is board certified in family medicine.
Following a family medicine residency at Silas B. Hays Army Community Hospital, Fort Ord, California, Clark served as family physician and flight surgeon, 543rd General Dispensary, Taegu, Korea from 1987-1989. While at Fort Bragg, he served as staff fam-ily physician at the 1st Corps Support Com-mand Clinic, faculty and clinic director of the Womack Army Community Hospital Family Medicine Residency, and senior medical offi-cer of C Co, 307th Medical Battalion, 82nd Airborne Division during Operation Desert Shield/Storm. Clark served as 82nd Airborne Division surgeon from 1993-95. He com-manded the 168th Area Support Medical Bat-talion, Korea from 1997-1999 and served as chief of Primary Care and Family Medicine at Womack Army Medical Center, Fort Bragg, from 1999-2001.
While assigned to the Wuerzburg MEDDAC/67th CSH from 2001-2004, Clark
served as deputy commander for clinical services and as commander of Task Force Medical Falcon, Kosovo. While in com-mand of the 21st Combat Support Hospital, 2005-2007, Clark led unit deployments to New Orleans in support of the Hurricane Katrina Relief Operation and during OIF 06-08 as TF 21 MED provided detainee health care for the Iraqi theater of opera-tions. Following his assignment as chief of preventive medicine for Darnall Army Med-ical Center, Fort Hood, Texas, Clark served as commander, 65th Medical Brigade/USAMEDDAC-Korea and as USFK/UNC/CFC surgeon from 2008-2010. He served as chief of Medical Corps Branch, Human Resources Command, Fort Knox, Ky., prior to commanding Landstuhl Regional Medi-cal Center from 2011-2012.
Clark’s awards and decorations include the Defense Superior Service Medal, Legion of Merit, Bronze Star (1OLC), Meritori-ous Service Medal (7OLC), Combat Medi-cal Badge, Expert Field Medical Badge, Flight Surgeon Badge, and the Parachut-ist’s Badge. He is a member of the Order of Military Medical Merit and recipient of the Republic of Korea Order of National Security Merit, Samil Medal.
Colonel Jeff ClarkCommander, U.S. Army Europe Regional Medical Command and
Command Surgeon, U.S. Army Europe
Compiled by KMi Media Group staff
www.M2VA-kmi.com M2VA 16.6 | 21

lives outside our clinics … There are dif-ficult challenges ahead, but our mission remains clear—in order for us to get to health, we must empower our patients. The need is urgent, the time is now. –Horoho
To empower individuals is to motivate and provide resources for them to move from being passive recipients to active par-ticipants in their health. We are currently implementing the patient-centered medi-cal home/soldier-centered medical home [PCMH/SCMH] models aimed at mak-ing care more accessible, providers more approachable and the health experience more interactive. PCMH/SCMH will offer patients a core group of caregivers who know them well and deliver a personalized care plan unique to the individual.
Access to care will become broader and easier for individuals and they will be encouraged to participate in their health. PCMH/SCMH also promotes more com-munication between the patient and pro-vider, opening the door for supplemental communication that takes place through nontraditional means such as video, tele-phone or secure messaging. Secure mes-saging interaction will allow patients to see lab results and X-rays as well as send messages to their patient care team.
These initiatives will improve care—making it more involved for the individual and the patient care team. The patient care team consists of the provider, his or her medic and a nurse who “own the health” of each patient on their panel. As relation-ships are built, the health experience will be enriched for patients as they become more and more active in the LifeSpace of their health.
Our OCONUS Integrated Disability Evaluation System is a key component of transitioning wounded, injured and ill sol-diers and families to civilian life as service veterans. Our MTFs and our WTB-E work closely together to ensure an efficient and compassionate process, caring for each soldier/family, one at a time.
Horoho has addressed further transi-tions faced by Army Medicine, recognizing this time of great change as an opportu-nity for a strategic reset.
Strategic reset—the transition from combat to a force predominately focused
on training and readiness. For all of us, this strategic reset means finding ways to improve the care experience, as well as the efficiency of the process itself within the AMEDD. It is imperative that we keep our Army Medicine Team trained and con-fident in the unique combat and medical skills acquired during 10 years of conflict. – Horoho
U.S. military forces in Europe are in the midst of a transformation that is as significant as it is historic. Over the next 12-24 months, Army Medicine in Europe will continue to adapt our organizations in a way that best suits the needs of our beneficiaries. Transformation in Europe also coincides with the ending of more than a decade of conflict. I’ve chosen September 30, 2014, as our strategic reset “end state.” By this date, USAREUR trans-formation will be complete, PCMH/SCMH will be fully implemented, and the current overseas contingency operations will be winding down ending a decade of Wounded Warrior care and Army Force Generation support. We will take full advantage of the inherent opportunities during this time of tremendous change and new fiscal reality to efficiently and cost-effectively increase access and patient-centered services. These changes will enable us to better serve our patients as we transition from a health care system to a system for health. Our patient-centered focus will endure as we adapt our goals and strategy to these new realities.
Q: What are the primary challenges the ERMC faces?
A: When accomplishing the mission and caring for soldiers and their families con-flict, good leaders find ways to do both. —Lieutenant General Mike Steele
Between now and September 30, 2014, the number of soldiers serving in Europe will decrease by about 11,000 plus about an equal number of family members; the number of airmen and their families will also decrease. Simultaneously, USAREUR will consolidate into fewer installations. Some will get bigger (Vicenza and Wies-baden); some will get smaller (Baum-holder); some will close (Heidelberg, Bamberg, Schweinfurt).
During this time of tremendous change we will:
• Ensure patient-centered care for all we are privileged to serve. We will always do this, but over the next couple of years it is especially important that our patients trust that whether their installation is getting larger, smaller, or headed towards closure, we will be there for them.
• Take care of our people during this time of change. Many of our people and our families are impacted by transformation. Positions are being reduced or moved; posts where we have lived and worked for decades are getting bigger, smaller, or closing. This change must be synchronized with the school year; many of our people are making life decisions. We will take care of each other during this time of tremendous change.
• Position Army Medicine in Europe for the future reality of September 30, 2014, and beyond. As we accomplish our mission/take care of each other today, we will anticipate and posture ourselves for those we are privileged to serve in the future.
In addition to leading through this enormous transformation, we are also operating in a new fiscal reality. There are untapped opportunities to use systems, processes and technology to improve the health care experience for our patients and for our staff and to ensure that we are both efficient and effective in the use of our resources. We also have to ensure we are staffed appropriately (not under or over) to accomplish our mission and achieve our priorities. This has always been important. The new fiscal reality makes it crucial.
Another key to meeting the chal-lenges of the future is a replacement facility for Landstuhl Regional Medi-cal Center [LRMC]. Dedicated in 1953, LRMC is among the oldest hospitals in the Department of Defense and is in need of replacement. LRMC currently serves as
Command Profile
www.M2VA-kmi.com22 | M2VA 16.6

For more information, contact M2VA Editor Brian O’Shea at [email protected] or search our
online archives for related stories at www.m2va-kmi.com.
the evacuation and treatment center for all injured U.S. servicemembers, civilians and contractors, as well as forces from coalition countries serving in Afghani-stan—in addition to members assigned to U.S. Africa Command, U.S. Central Com-mand and U.S. European Command areas of responsibility. A new medical center in the Kaiserslautern military community is the most efficient long-term solution to continue providing the best possible medical care for wounded warriors, ser-vicemembers and families during peace-time and contingencies for decades to come.
Change is not easy. Some people like it. Some do not. Regardless, if we do not lead and manage change, it will manage us. We will manage this time of tremen-dous change to accomplish our mission and create conditions for our people to prosper personally, professionally, spiri-tually, and in their families and relation-ships. Our individual and collective well being is the foundation for how we care for those we are privileged to serve.
Q: Can you give an example of the historic change going on within Army Medicine in Europe?
A: In August, we cased the colors of the Heidelberg Medical Department Activity [MEDDAC] and the Heidelberg Dental Activity [DENTAC]—two historic Army Medicine units that have served for more than seven decades here in Europe.
The origins of both the Heidelberg MEDDAC and Heidelberg DENTAC began during World War II when the 130th Sta-tion Hospital was activated in Texas in 1942. In August 1943, the unit set sail for England in support of the buildup before the invasion of Nazi-occupied Europe. Nine days after D-Day, the 130th moved to France and became a transient hos-pital in the line of evacuation, treating thousands of troops over the next 10 months. After serving in France, the unit was assigned to 7th Army and took up residence near Heidelberg, moving into Nachrichten Kaserne in August 1945.
Shortly thereafter, the unit attained a unique place in military history. In December 1945, General George S.
Patton was involved in an automobile accident near Mannheim, Germany, and was taken to the 130th Station Hospital for treatment. An interdisciplinary team of American and German physicians provided medical assistance to Patton after the accident, but he was unable to recover and died from complications of his injuries on December 21, 1945.
In 1946, the 130th Station Hospital opened a seven-chair dental clinic that would later become the hub for all U.S. Army dental care in the southwest region of Germany. This marked beginnings of a separate dental unit that would operate alongside the health care unit for decades to come. By 1983, the 130th Station Hospital Dental clinic had transformed the Heidelberg DENTAC, responsible for command and control of eight dental clinics throughout the region.
Health care delivery remained the responsibility of the 130th, which was re-designated as the Heidelberg MEDDAC in 1994. At the high point, there were nine outlaying clinics reporting to the Heidel-berg MEDDAC.
Casing the colors of these two units highlights not only the historic trans-formation taking place in Europe, but the legacy of dedicated men and women who successfully accomplished their mis-sion during decades of service here in Heidelberg.
Q: How does the ERMC work with indus-try to provide the highest quality health care?
A: Our partners in industry are an inte-gral part of a team that provides the finest health care that can be found any-where. One example is our partnership with International SOS to provide Tricare services for our beneficiaries living and working overseas. When you look at how geographically dispersed our clinics are from the Landstuhl Medical Center, it’s vital that we have the processes in place to ensure our patients who need medical care not readily available at their local MTF can get that treatment through a network of high quality host nation medical facilities. Our host nation patient liaisons at each of our clinics are critical
to this process and to our motto: “On or off post, you are always our patient.”
Q: Is there anything else you would like to add?
A: Through changes and challenges, we remain committed to patient-centered care while taking full advantage of this time of immense change to improve the health care experience for those we are privileged to serve. Transforming to a system for health is our way ahead—Army Medicine in Europe will lead this endeavor. I could not be more proud of who we are, what we do, and most impor-tantly how we do it. O
Proud to Serve Our Nation’s Heroes and Their FamiliesInternational SOS has administered the TRICARE Overseas Program (TOP) for uniformed service members, retirees and families since 2010.
Providing comprehensive health care services to nearly 500,000 beneficiaries across 207 countries, International SOS makes sure our beneficiaries know what to expect when seeking health care overseas.
It is a distinct honor and privilege to be entering our third year of service.
International SOS is available to assist you 24 hours a day, 365 days a year. www.tricare-overseas.com
Worldwide reach Human touch
Working together, we can help achieve the quadruple aim of military medical excellence
throughout the world.
Compiled by KMi Media Group staff
www.M2VA-kmi.com M2VA 16.6 | 23

Making sense of the magnitude of data available to government health care providers to improve the overall health care of patients as well as reduce the use of resources is a big job that involves the use of health analytics.
The Department of Veterans Affairs (VA) is a data driven organization that has long relied on analytics to measure current and past performance of the health care system and to support quality improvement, said Stephan D. Fihn, M.D. M.P.H., director, Office of Analyt-ics and Business Intelligence, Veterans Health Adminis-tration (VHA).
“VHA produces numerous data reports addressing a vast array of domains including the quality of both processes and outcomes of in- and out-patient care, access to health care, patient experience, patient safety, efficiency, staffing, etc.,” said Fihn. “The Office of Analytics and Business Intelligence maintains nearly 1,000 products that are routinely used by executives, managers and clinicians within VHA and there are a variety of other reports regularly produced by other offices within VA. To the greatest extent possible, we work to link and inter-relate this informa-tion in order to provide a comprehensive picture of our health care system. At the same time, many of our reports provide the capability to ‘drill down’ to facilities, programs and at times, even to the level of the individual patient, to better understand potential trends and problems.”
Analytics are critical to the VA and health care in general, added Fihn.
“Like many aspects of modern life, information related to health care is mushrooming in terms of quantity and complexity,” he said. “This includes not only information from scientific advances but also clinical information about individual patients. Nearly all information generated about patients is now computerized, ranging from clinical notes to diagnostic studies. Many clinical information systems, such
as those used to monitor critically ill patients in ICUs and imaging machines, issue megabytes or gigabytes of data per patient-day. New
systems are constantly coming on-line. Increasingly, a key role of the health care provider is information management.”
To better understand VA’s health care delivery sys-tem and improve clinical and operational processes, application of modern analytics is essential. In doing so they can better identify opportunities to improve health care delivery, target services to patients who are most likely to benefit, and provide timely information to decision-makers.
Although difficult to predict, it is likely that sophis-ticated analytics will play an increasingly important role in the future, said Fihn. The availability of “cloud” data
services, high-speed computing and sophisticated analytics will enable “smart” (i.e., context-sensitive) decision support delivered in real time to program managers, clinicians and patients. Predictive analytics will assist in identifying patients at risk of avoidable adverse outcomes from illness or treatments, so that preventative measures can be undertaken. Clinical management will be individualized for patients based on analy-sis of outcomes for other patients with similar characteristics treated in the same system.
chaLLenges of using heaLth anaLytics
There are numerous challenges to application of health analytics. High performance computing environments are required, said Fihn.
“Enormous effort is required to standardize and link data across multiple databases that were not designed with such uses in mind,” he said. “Ensuring the quality and accuracy of data within these databases is challenging. Ensuring the accuracy of results and delivering them in
using anaLytics to iMproVe heaLth care and conserVe resources.
By Brian o’shea
M2Va editor
Analyzing the Data
Dr. Stephan D. fihn
www.M2VA-kmi.com24 | M2VA 16.6

a timely and effective manner is also difficult. Data users must learn to understand both the strengths of limitations of analytic data.”
The Military Health System (MHS) has also made significant invest-ments in health analytics over the last 10 to 20 years, said Dr. Michael Dinneen, Director, Office of Strategy Management as well as the Office of the Assistant Secretary of Defense for Health Affairs (OASD-HA). MHS applies health analytics on a daily basis from the point of care to the level of the Assistant Secretary of Defense (ASD), who is responsible for stra-tegic course corrections.
“My first point is that we’re applying health analyt-ics all the way from patient-centric systems to where the ASD makes policy decisions,” said Dinneen.
A few examples of this include the implementation of clinical decision support for patient-centered medical home teams. MHS is now monitoring the health of each panel of patients so doctors can improve preventive screening for conditions such as cancer and hyper-tension. That would be step one. At the next level up, clinic managers and hospital commanders are getting dashboards that give them useful information about the performance of the system in areas such as access to care, satisfaction, and quality outputs.
MHS is also using health analytics to help under-stand the readiness of the medical system to be able to support the troops, said Dinneen. The two aspects of readiness would be the force being ready and the medical system being ready to deploy. Moving up one level higher, health analytics begin to make conscious choices about balancing resources between health care interventions and preventive information so that MHS can improve the overall health of the population in the most effective way. Looking to the future, MHS can use the data gathered from daily operations to inform their research agenda.
“Over the past three or four years, the military health system has adopted the Quadruple Aim as our high-level set of strategic goals,” said Dinneen. “The Quadruple Aim consists of improved readiness, better health, better healthcare and responsibly managed costs. Hav-ing readily available health analytics allow us to focus improvement efforts to achieve these higher-level goals. One example where we can improve quality and reduce costs through the use of health analytics is by reducing unnecessary readmissions. We have found that a key to that is to improve the coordination of care across inpatient and outpatient activities. Analysis of our data has allowed us to understand the nature of that process and focus improvement efforts so that patients are not exposed to unnecessary care and risk—neither of which add value to the system nor create value for the patient. ”
Dinneen said one challenge of health analytics is the cultural change of moving from a very individualistic approach to an enter-prise approach, and to do that with balance—the need for individual autonomy with the need for standardization—to get the benefits of shared learning.
“The other challenge we see in health analytics are the challenges of big data,” said Dinneen. “We’re capturing literally a hundred thou-sand complex interactions every day. Our challenge is understanding what are the key things we need to learn from that huge amount of data across both time and space—without getting overwhelmed by the quantity of data—and ensuring we can get quality learning from our information.”
As the delivery of health care and its associated costs continue to challenge the MHS and the nation as a whole, health analytics become that much more critical moving forward in a resource-constrained environment, added Dinneen. Health analytics are integral to a learning organization.
MHS and the VA works with many partners in industry on all levels to meet its health analytic needs. These include large and small players in the information technology sector.
Industry is no stranger to the arena of health analyt-ics, as the benefits of analyzing large amounts of data could have large implications on patient treatments and cost of health care, said Sam Shekar, M.D., M.P.H., the chief medical officer within Northrop Grumman’s Information Systems sector.
“One of the key goals would be to try to figure out what are the factors that can create improved health care and potentially reduce the cost of health care,” said Shekar. “So health analytics very simply put is creating better prevention and treatment decisions through bet-ter data.”
Northrop Grumman Corporation has been working in health care analytics primarily on a national and state level for approximately 20 years. The company is taking the lessons learned from across industry, government or university partners and applying them toward what Northrop is calling the integrated health analytics plat-form (IHAP). IHAP is the result of an internally funded research and development project that is designed to integrate a diverse set of technologies to meet a diverse
set of customer goals, said H. Morgan Crafts Jr., M.B.A., P.M.P., director, technology, Civil Systems Division, Health IT, Northrop Grumman.
“For example, a state health administrator can use the platform to evaluate the impacts of new health legislation or policies,” said Crafts. “A federal agency can look across the whole U.S. and look at what the cost drivers are or the impact of different health activities—for example, hospital acquired infection, or how emergency rooms are being used for primary care for Medicaid patients. Basically, it all comes down to what can we see about individual patients; what are the different things we can do for individuals, ranging from genomic research to chronic disease management or telemedicine? So we have data analysis, integra-tion, visualization and presentation, and we can have different data and different use cases on the other end, but we’re using that same frame-work to be able to answer issues about cost and quality of health care.”
Not only can federal and state agencies utilize health analytics, but payers, providers, pharmaceutical firms, regulators and consumers can all benefit from health analytics as well, said Laura Squier, M.S., manager, federal analytics healthcare, SAS. Squier added that SAS goes beyond basic analytics, which focus on what has happened and more into advanced analytics so organizations can make proactive, intelligent decisions.
SAS’ analytic solutions include a variety of options such as clinical SAS data integration, SAS drug development, SAS fraud framework for health care and SAS health and condition management. Addition-ally, general SAS solutions have also been used by their health care customers such as SAS performance management; HEDIS (healthcare effectiveness data and information set) measures; JCAHO (Joint Com-mission on Accreditation of Healthcare Organizations) accreditation and compliance; Pharmacovigilance for monitoring drug and device
Morgan Crafts Jr.
Dr. Michael Dinneen
Analyzing the Data
www.M2VA-kmi.com M2VA 16.6 | 25

safety; outbreak investigation; disease surveillance and biomonitor-ing; SAS financial planning for facilitating regulatory compliance by integrating data management and financial intelligence (including planning, forecasting and reporting) to view a hospital system from any perspective; and decision support/key driver analysis to identify key fac-tors that, for example, impact disability determination or influence the clinical risk for certain diseases and complications.
“All of the SAS solutions are based on the same technology platform and leverage SAS’ market-leading analytic applications,” said Squier. “At its foundation, all of SAS’ solutions are driven by data. SAS technologies are designed to integrate, clean and standardize this data as necessary for the purposes of analytics, and push the results of this information out to the information consumer in the most meaningful way to pro-vide insight.”
The SAS framework for health care analytics includes several ele-ments such as data management capabilities that work with the existing data infrastructure to integrate data from virtually any source, cleanse it and prepare it for analysis.
SAS solutions have been implemented at a number of customer sites across federal health organizations as well as with commercial payers, providers, pharmaceutical firms and regulators.
SAS analytics will also be utilized by the U.S. Air Force medical services. The Air Force will use SAS Business Intelligence software to improve quality of care and outcomes for its more than 1.2 million patients enrolled in Patient Centered Medical Home to increase patient satisfaction and reduce operational costs. SAS high-performance
analytics and predictive modeling also will support research into preventative medicine and disease management.
The SAS Center for Health Analytics and Insights, a health indus-try think tank formed in 2011, is focused on identifying novel ways of applying advanced analytics to the challenges facing the health and life sciences industries.
IBM is another big player in the health analytics market. IBM has invested more than $10 billion to build its capabilities around business analytics. This includes organic and through acquisitions, said Heather Fraser, global life sciences and health care lead, IBM Institute for Busi-ness Value.
“There is an explosion of health care information, and analytics holds the potential for mining that data for new insight,” said Fraser. “Analytics is the ability to see patterns in vast amounts of data and extract actionable business insights. IBM sees health analytics as the key to making the world’s health care systems smarter. For example, doctors are using analytics to ‘liberate data’ from electronic health records to improve care, from determining which diabetics will be sicker longer, to picking the best procedure to manage cardiac care. Through advances in analytics, hospitals and doctors are gaining deep new insight by tackling mountains of data that wasn’t humanly possibly before.”
Key areas IBM health analytics uses are patient analytics, wellness and chronic disease analytics, quality of care analytics, operational efficiency and incentive analytics. Some of these IBM products include IBM Cognos Business Intelligence, IBM SPSS and IBM Content and Predictive Analytics.
Users of IBM’s analytics products include a group of physicians and researchers at Columbia University Medical School who are applying a new kind of analytics to data streaming from stroke patients to spot potentially dangerous complications before they set in. Using a new form of stream computing technology from IBM, predictive analytics can uncover patterns of stroke symptom progression not visible to the naked eye and spot the onset of the condition up to 48 hours sooner than traditional methods. The detection of these early warning signs would give doctors the ability to plan and begin treatments sooner or stop the progression of the condition altogether.
With more than 1.2 million cancer patient records over the past 25 years in a single database, Memorial Sloan Kettering uses IBM health analytics so researchers and clinicians can securely analyze and mine one of the world’s largest collections of cancer patient information to foster additional research and provide better patient care. The institu-tion has been filmless since 1999, digitizing massive amounts or medi-cal imaging data, tissue samples and test results. Automated mining of pathology data including diagnoses, staging and tumor size, as well as free text search across pathology reports, gives clinicians unprecedented access to data and insight in near real time. The Cancer Center is also using a quality of care dashboard that allows everyone within MSKCC to see progress on institutional quality initiatives and drill down on each measure to specific departmental statistics.
Today, data visualization provides the most value, followed by trend analysis and standardized reporting, added Fraser. Over the next 24 months, we’ll see a dramatic rise in the use of simulations and scenario development. Trend analysis or reporting will not go away, but they will no longer be the main sources of value. O
For more information, contact M2VA Editor Brian O’Shea at [email protected] or search our online archives
for related stories at www.m2va-kmi.com.
CONFERENCE REGISTRATION IS NOW
2012 Special OperationsMedical Association
Conference
December 15-18 Tampa Convention Center
Tampa, Florida
Visit our websitewww.specialoperationsmedicine.org
Join the 2000 plus fellow Physicians, PA’s, RN’s, Military and Civilian Medics.
Earn CEU’s and CME’s, and visit ourExhibition � oor to see the latest
technologies and products in the � eld.
www.M2VA-kmi.com26 | M2VA 16.6

The a
dver
tiser
s ind
ex is
pro
vide
d as
a se
rvic
e to
our r
eade
rs. K
MI c
anno
t be h
eld
resp
onsib
le fo
r disc
repa
ncie
s due
to la
st-m
inut
e cha
nges
or a
ltera
tions
. aDVertIsers InDexBioFire Diagnostics Inc. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7www.bio-surveillance.comBioFire Diagnostics Inc. . . . . . . . . . . . . . . . . . . . . . . . . . . . C4www.biofiredx.comCombat Medical Systems . . . . . . . . . . . . . . . . . . . . . . . . . . . 1www.combatmedicalsystems.comInternational SOS Assistance Inc. . . . . . . . . . . . . . . . . . . . 23www.tricare-overseas.comSkedco . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9www.skedco.comSpecial Operations Medical Association . . . . . . . . . . . . . . . 26www.specialoperationsmedicine.orgUtilis USA LLC . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11www.utilisusa.comZoll Medical Corporation . . . . . . . . . . . . . . . . . . . . . . . . . . C2www.zoll.com/propaqdata
calenDarSeptember 25-27, 2012Modern Day MarineQuantico, Va. www.marinemilitaryexpos.com
October 22-24, 2012AUSAWashington D.C.www.ausa.org
October 28-November 1, 2012Joint Forces Pharmacy SeminarSand Diego, Calif.www.jfpsinfo.org
November 11-16, 2012AMSUSPhoenix, Ariz.http://amsusmeeting.org
M2VA RESOURCE CENTER
Growing
June 2012Volume 1, Issue 1
www.BCD-kmi.com
Border Threat Prevention and CBRNE Response
Border Protector
Michael J. Fisher
ChiefU.S. Border PatrolU.S. Customs and Border Protection
Wide Area Aerial Surveillance O Hazmat Disaster ResponseTactical Communications O P-3 Program
SPECIAL SECTION:Integrated Fixed Towers
Leadership Insight:Robert S. BrayAssistant Administrator for Law Enforcement/Director of the Federal Air Marshal Service
Border & CBRNE Defense
Taking its place in KMI Media Group’s family of publications
Border & CBRNE DefenseGeospatial Intelligence ForumGround Combat TechnologyMilitary Advanced Education
Military Logistics ForumMilitary Information Technology
Military Medical & Veterans Affairs ForumMilitary Training Technology
Special Operations TechnologyTactical ISR Technology
U.S. Coast Guard Forum
11For more information on BCD, please contact Editor Brian O’Shea at [email protected]
makes eleven
www.M2VA-kmi.com M2VA 16.6 | 27

Kirk Ririe Chief Executive Officer BioFire Diagnostics Inc.
Using technology developed by his men-tor Dr. Carl Wittwer Ph.D., M.D., Kirk Ririe founded Idaho Technology Inc. in 1990. Now he leads the company forward as BioFire Diagnostics Inc. as it revolutionizes molecu-lar diagnostics with the FilmArray, the first easy-to-use multiplex PCR system.
Q: Idaho Technology recently changed its name to BioFire Diagnostics. What is the reason for the change?
A: We changed the company name to lever-age momentum in the marketplace and cap-ture our fervor and commitment to deliver innovative solutions for biosurveillance and molecular diagnostics. We are proud of our Idaho heritage, but we have evolved con-siderably since the revolutionary invention of the first air thermocylcer and our subse-quent Idaho Falls founding in 1990. Now we are headquartered in Salt Lake City, Utah, and well-known throughout the world for our innovative products in military biosur-veillance, clinical diagnostics, life science research and food security. As we proudly move forward with this change, our passion burns brighter than ever. We have a new name and a new look, but we are still the same risk-taking, boundary-pushing com-pany that creates cool products that are easy to use.
Q: What are some of the innovative prod-ucts released by Idaho Technology/BioFire Diagnostics?
A: In 1990 we dramatically changed PCR [polymerase chain reaction] with the invention of the air thermocycler. PCR is a laboratory procedure used to amplify the quantity of DNA. Ordinary instruments took hours and the air thermocycler reduced run time to 30 minutes. This was followed with the LightCycler that was capable of real-time monitoring and DNA melt analysis. Roche Diagnostics licensed the LightCycler for the clinical market and we retained the rights for military applications, which we used in the ruggedized Rapid, the first PCR and molecular diagnostics system used in
mobile laboratories. We improved ease of use and created the capability of testing at the point of attack with the Razor, the world’s first battery-operated real-time PCR system used in the field. In the life science market, the LightScanner provides high throughput high-res melt analysis. And now we are changing molecular diagnostics with the FilmArray. The FilmArray is the first user-friendly multiplex PCR system that combines sample preparation and extraction, nucleic acid amplification, and detection and analysis into a single instrument. The FDA-cleared FilmArray requires two minutes of hands-on time and tests for a panel of pathogens with comprehensive results available in one hour.
Q: What experience does BioFire Diagnos-tics have working with the military?
A: We have developed and fielded numerous systems successfully for the U.S. Department of Defense. These systems include the Joint Biological Agent Identification and Diagnos-tic System [JBAIDS], which is the biothreat identification and diagnostics standard for the U.S. military, the field-hardened, battery-powered Razor, and a suite of complementary sample preparation and reagent products. Over the past 10 years, BFDX has delivered hundreds of testing platforms and millions of reagents and prep kits for both biothreat identification and diagnostics. We are always working to improve the technology and give the warfighter more capability that is easy to use, reliable and most importantly mission capable.
Q: How does the FilmArray fit with currently fielded military biothreat detection systems and how does it improve CONOPS?
A: The FilmArray is used for both diagnostics and environmental surveillance, filling two important needs with one system. By hav-ing a single system support multiple uses, logistical, training and cost burdens are sig-nificantly reduced.
In the garrison hospital, the system allows for diagnostic testing of multiple sample types from upper respiratory disease pathogens to biothreat agents listed on the Class A and B threat list. Rapid diagnosis and confirmation enables providers to treat patients quickly and more effectively.
In field settings, troops charged with testing swabs, air collections and other envi-ronmental sample types, rapid results provide commanders better situational awareness enabling them to posture operational readi-ness levels, avoid contaminated areas, and validate decontamination of systems or per-sonnel. Biothreat and pandemic surveillance provides a broad range of protection for deployed assets. Using the same system for environmental samples and diagnostic sam-ples enable providers and commanders access to important results accurately and quickly.
Q: Is the FilmArray replacing an old system and what are the major differences or ben-efits over the old method?
A: No, the FilmArray completes our suite of identification tools truly enabling biosurveil-lance. We have the Razor system for point identification deployed far forward—easy to use, battery powered and very fast and accu-rate. The JBAIDS in the research and garrison setting allows sophisticated users to have the system flexibility and throughput needed to test a multitude of samples for many targets. The FilmArray sits in the middle, in deployed facilities, with ease of use for both diagnostics and environmental samples, integrated into both environmental and diagnostic informa-tion systems, casting a very wide net looking for pandemic, biothreat and public health pathogens of interest. The FilmArray bridges the gap from the field to the lab in a smart compact platform, revolutionizing pathogen identification and meeting important mission needs. O
INDUSTRY INTERVIEW Military Medical & Veterans Affairs Forum
www.M2VA-kmi.com28 | M2VA 16.6

November 2012Vol. 16, Issue 7NEXTISSUE
Dedicated to the Military Medical & VA Community
Commander, 59th Medical WingWilford Hall Ambulatory Surgical Center Lackland Air Force BaseDirector San Antonio Military Health System
Cover and in-depth interview with:
Major General (dr.) Byron C. Hepburn
Special SectionNATO Surgeon General RoundtableSurgeons general from the North Atlantic Treaty Organization address the challenges their military medical community will face over the coming decade.
FeaturesChronic Diseases and Health PromotionThe Military Health System recognizes there is an issue with chronic diseases affecting the warfighter today, such as gout and diabetes.
USASOCUnited States Army Special Operations Command discusses upcoming challenges, programs and initiatives.
Dental Technology ShowcaseTechnological innovations used by today’s military to improve the dental health of the warfighter.
Pharmaceutical UpdateAn exclusive interview with Rear Admiral (Upper Half) Thomas J. McGinnis in his capacity as assistant surgeon general, United States Public Health Service, and chief, Pharmaceutical Operations Directorate, responsible for pharmacy operations of the TRICARE Management Activity.
Organization ProfileAn exclusive interview with Navy Captain Paul S. Hammer, director, Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE).
Insertion Order Deadline: Oct. 8 • Ad Materials Deadline: Oct. 15
Bonus distributionJoint Forces PharmacyAMSUS

We’ve always been passionate about the work we do and the clients we serve. And now we
have a name to match our fervor and commitment to deliver innovative solutions for
biomedical research and molecular diagnostics. It’s a new name, and a new look, but we’re still
the same risk-taking, boundary-pushing company that creates cool products to simplify your life.
Learn more at the new BioFireDX.com
FLM
1-A
DS-
0003
-01
Idaho Technology, Inc.
is now