Against all Odds: Interpreting Relative Risks and Odds Ratios
Log Odds
-
Upload
popa-tiberiu -
Category
Documents
-
view
219 -
download
0
description
Transcript of Log Odds

S. Luncă, S.-T. Makkai-Popa, V. Porumb, Natalia Velenciuc, C. Roată, G. Dimofte
Second Surgical Oncology Clinic - Regional Institute Of Oncology, Iasi,
Romania

*Prognostic markers*evaluate the patient’s overall outcome*selection of patients for treatment*does not directly predict the response to a treatment
*Predictive markers*evaluate the likelihood of benefit from a specific clinical intervention
*the different outcomes of two or more interventions, including toxicity.
Sunali Mehta, Andrew Shelling, Anita Muthukaruppan et al, Predictive and prognostic molecular markers for cancer medicine, Therapeutic Advances in Medical Oncology
2010;2(2):125-148

*Treatment decisions - Modified Astler–Coller (MAC) classification
*TNM (UICC 2002) dual system*cTNM – choice of treatment*pTNM – prognostic assessment
Labianca R, Nordlinger B, Beretta GD et al, Primary colon cancer: ESMO Clinical Practice Guidelines for
diagnosis, adjuvant treatment and follow-up, Ann Oncol 2010; 21 (5): 70-77

NCCN Guidelines

*Cancer + predictive marker – 43985 hits on Pubmed*Cancer + prognostic marker -60048 hits on Pubmed*Why are they not integrated in clinical practice?*Can we improve what we already use?*N staging – at least 12 lymphnodes*Staging error – statistics?*Better surgical technique of surgeons who achieve higher numbers of lymph nodes?

*to correlate different lymph node based scoring systems with either disease- free survival or the type of relapse in order to improve the classical TNM staging system

*Retrospective study – 2 years – patients presenting with local or distant recurrence of disease, after curative resections for colorectal cancer
*Exclusion criteria:*Presence of a macroscopically visible metastasis at the time of the first surgery;
*Neoadjuvant radio- and chemotherapy – because of the possible down staging effect of the neoadjuvant therapy on lymph node status;
*Previous neoplastic disease – other than the colo- rectal cancer that is suspected to be responsible for the recurrence;
*Patients who underwent the first procedure in another clinic – because of the fact that complete medical records were inaccessible;
*Patients with incomplete pathology records – where either or both the number of invaded lymph nodes and the number of harvested lymph nodes was not clearly stated – 14 patients (15.38%)
*Number of patients enrolled – 25

*Lymph node ratio (LNR) = invaded nodes/harvested nodes
*Logarithmic odds ratio (LODDS) = log [(invaded nodes + 0.5)/ (harvested nodes-invaded nodes + 0.5)]
Persiani R, Cananzi FC, Biondi A, Paliani G, Tufo A, Ferrara F, Vigorita V, D’Ugo D, Log odds of positive lymph nodes in colon cancer: a meaningful ratio-based lymph node classification system, World J Surg, 2012, 36(3):667–674.

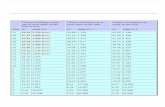
Descriptive statistics of the study group and the correlations of
clinical variables to the time to relapse

Table showing the results of the Spearman’s rank correlation test between the number of invaded lymph
nodes, the number of harvested lymph nodes, LNR, LODDS and the pN classification

Table showing correlations between the type of relapse and various
lymph node based scores

Kaplan–Meier survival curves for groups of patients defined according to the LODDS
ratio (p less than 0,05)

*LNR only contains information about the number of invaded lymph nodes and not the total number of harvested lymph
*LODDS retains at least as much information about lymph node involvement as the pN staging but can be calculated even in the cases where the total number of resected lymph nodes is less than 12
* a high LNR ratio and a high LODDS ratio correlated with the appearance of a metastasis at statistically significant levels (p=0.013 for the number of invaded lymph nodes, p=0.007 for LNR and p=0.004 for LODDS)
*pN and LODDS can be used to stratify patients depending on disease-free survival but not LNR