Linda Gibson, President & CEO - California Hospice and...
Transcript of Linda Gibson, President & CEO - California Hospice and...
Topics
Community-based palliative care –the unfunded approach
Partners in Palliative Care Pilot with Partners in Palliative Care Pilot with Partnership Health Plan of California (PHC) – the funded approach
Why Start an Unfunded Palliative Care Program?
� To promote Hospice program growth and improve length of stay
� To fill care delivery gaps in the community
� To reach the Latino population� To reach the Latino population
� A Warm hand-off for discharged Hospice patients
� To control the message about Hospice
� A new way to engage Physicians and other referral sources
Eligibility� Progressive advanced illness and
� Significant and complex symptoms
� Multiple recent hospitalizations
� In need of advance care planning
� Uncertainly regarding goals of care� Uncertainly regarding goals of care
� In need of support in end-of-life decision making
� May be receiving curative therapy
� May be in a skilled nursing facility
“Would you be surprised if your patient died in the next year?”
Care Delivery ModelServices Staffing Setting
Initial Assessment RN Home *
Pain / symptom management Primary Care, Medical Director, RN
HomeTelephone
Advance Care Planning / POLST RN Home
Coordination of Care RN HomeCoordination of Care RN HomeTelephone
Monday – Friday (8 a.m. – 5 p.m.) Telephonic Support
RN / Volunteer RN Telephone
Care Management Plan RN HomeTelephone
Help with practical needs Volunteers Home
Reimbursement: Fee-for-service, $60.00 / month & sliding fee
* Home, Skill Nursing Facility, Board & Care, Assisted Living, Retirement
Other Considerations� Need to be very clear about scope of services and
frequency of visits:
� Monthly visits
� Weekly telephone calls� Weekly telephone calls
� Occasional social work and spiritual care consultation
� Focus is on education, coordination and consultation
� Use of volunteers helps to control costs and provides a richer patient experience
� RN case load = 45 – 50 patients
� Requires surprisingly little marketing and outreach
Lessons Learned� Exceedingly well received in the community
� Physicians, families love the program
� Need to have a plan to move patients to Hospice when eligibleeligible
� Improves ability to keep discharged Hospice patients in the fold
� Allowing volunteers to stay with the patient during transitions from / to Hospice facilitates continuity
� Has helped Hospice LOS
� ROI improves every year
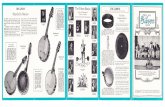
46
55 55
44
40
50
60
Transitions Palliative Care
Average Daily Census Comparison
2011-2015
= August 2014 YTD
21
0
10
20
30
2011 2012 2013 2014 2015
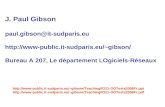
Transitions – Transfers to Hospice - MLOS
35
40
MLOS Hospice
15 16
23
34
22
17
20 19
0
5
10
15
20
25
30
2011 2012 2013 2014
Transitions – Transfers to Revenue
1000000
1200000
1400000
195,415
583,121
1,084,626
1,290,976
0
200000
400000
600000
800000
2011 2012 2013 2014
Expense - $206,218
Napa Valley Hospice & Adult Day ServicesNapa Valley Hospice & Adult Day Services
Partnership Health Plan of California
Partnership HealthPlan of California
Mission: To help our members, and the communities we serve, be healthy
Membership: 540,000 in 14 countiesMembership: 540,000 in 14 counties
Model: Not-for-profit, Community Organized Health System
Primary Care: 77% at FQHC, RHC or Native Health Center
Offering and Honoring Choices TM
� Partnership HealthPlan’s Initiative to promote
Advance Care Planning and Palliative Care.
� 14 Projects
� Purpose:
“Ensure that our members and their families are
knowledgeable about healthcare treatment options,
empowered to define their treatment goals, and able to
make informed choices about the interventions they
prefer during the last years of life.”
PHC Palliative Care Pilot
� CHCF planning grant (2014)
� Working group of hospice agencies and palliative care physicians contributed to proposed planproposed plan
� PHC awarded CHCF implementation grant (2015)
� Four pilot sites selected:
� Resolution Care (Humboldt County)
� Napa Valley Hospice and Adult Day Services (Napa County)
� Hospice of Yolo (Yolo County)
� Interim HealthCare (Shasta County)
PHC Pilot Eligible Patients� Life expectancy less than 2 years
� Advanced severity (when not “decompensated”)
� Any of six diagnoses:
Congestive Heart FailureCongestive Heart FailureCongestive Heart Failure
COPD
Cirrhosis
Dementia
Frailty Syndrome
Stage IV Cancer
Congestive Heart Failure
COPD
Cirrhosis
Dementia
Frailty Syndrome
Stage IV Cancer
Partners in Palliative Care:
Payment Model
� Global Payment
� Per enrolled member, per month
� One rate if resident of SNF or if skilled nursing services not
includedincluded
� Another rate if in-home nursing included
� Bonus Payments:
� Quality: Bonus per Quarter for Meeting Quality
Metrics
� Shared Savings: Bonus per month if no Emergency
Department visits or Hospitalizations during the month
Engaging the Health Plan
• A history of working together successfully
• Hospice Services
• CBAS services• CBAS services
• Lead agency for community ACP project
• Partner together to put on an annual palliative care educational conference
• Planning Partner, then Pilot for testing a palliative care benefit
What You Need From the Health Plan
• Mission alignment
• Mutual respect
• Common focus on quality• Common focus on quality
• Appreciation for importance of financial sustainability
• Collaborative approach
• Innovative practices – willingness to try new approaches
What You Need From the Health Plan
• Access to data
• Provider lists
• Eligible members (frequent flyers)• Eligible members (frequent flyers)
• Cost data
• Flexibility
• In care model design and implementation
• In eligibility requirements
What You Need From the Health Plan
• Simplified enrollment and billing processes
• Limit data submission requirements
• PMPM works well (we think…)• PMPM works well (we think…)
• Promotional assistance
• Joint press releases
• Letters to providers announcing benefit
Evaluating Payment Models
• Must be financially sustainable for the provider:
• Costs of building a new program
• Financial modeling of assumptions
• Balancing risk and likelihood of success
• Importance of baseline financial stability
Contact Information
Linda J. Gibson
President & CEO
Napa Valley Hospice & Adult Day ServicesAdult Day Services
707.285.9080
Objectives
You will learn to:
� Identify and speak to the priorities and challenges of payer sourceschallenges of payer sources
�Describe the core components of a Community based Palliative Program
Mission Statement – for
Palliative Program
To advance, support and provide a Community based Palliative Care Community based Palliative Care Program. We envision a seamless, less fragmented and more coordinated care system, that also addresses effective stewardship of resources.
Focus of Program
• Provide symptom management and emotional support to patient/family
• Assist with EOL discussions/decisions• Promote a smooth transition to Hospice.• Implement Palliative Care Program to a targeted • Implement Palliative Care Program to a targeted
population in order to reduce ER visits and inpatient hospitalizations
• Promote appropriate utilizations of resources to reduce unnecessary costs
• Promote transition to Hospice when appropriate• Improve patient care
Program Goals� To address physical, psychological, social, spiritual,
practical expectations and needs
� To reduce or eliminate Emergency Room visits (especially for pain/symptom management) and total care costs
� To reduce or eliminate (unplanned) hospital admission and/or readmission
� To promote a seamless transition from curative to � To promote a seamless transition from curative to Palliative to Hospice for patients and their families.
� To address goals of care and advance care planning
� To assess the individual primary care physicians’ and subspecialists’ preferences in communicating to members of the team
� To assist family members’ emotional adjustments to the changing role in relation to the patient and within the family system through support and education
Structure and Process
Identification of patients who would benefit from Palliative Care Program
� Develop Criteria for evaluation and admission� Develop Criteria for evaluation and admission
� Referral process
� Fax sheet
� MD order
� Authorization process
� Letter of explanation - to family (English and Spanish)
- to PCP
Criteria
Basic Disease Process
� Cancer (metastatic/recurrent)
� Advanced COPD
� Stroke (with decreased function by at least 50%)
� End-stage Renal Disease� End-stage Renal Disease
� Advanced Cardiac Disease i.e.; CHF, Severe CAD, CM (LVEF less than 25%)
� Frail Elderly with Multiple Diagnosis
� Other Life-limiting Illness
CriteriaConcomitant Disease Process
� Liver Disease
� Moderate Renal Disease
� Moderate COPD
� Moderate CHF
Other Condition Complicating Care� Other Condition Complicating Care
Other Criteria to consider in Screening
� Team/patient/family needs help with complex decision – making and determination of goals of care
� Patient has frequent visit to emergency department (greater than 1 time a month for same diagnosis)
� Patient has more than 1 hospital admission for the same diagnosis in the last 30 days
Interdisciplinary Team Based Care
� Communication
� Provide purpose and explanation of Palliative Program � Provide purpose and explanation of Palliative Program to Clinical Team – focus on communication, authorization process and utilization of resources
Evidence Based Outcome
Data
� Data Collected Demonstrating Cost Avoidance or Improved Resource Utilization
� Measuring Quality
� Pain and symptom management� Pain and symptom management
� Patient/family satisfaction
� Advanced care planning
� Improved utilization outcomes
� Hospitalizations
� Hospital readmission rate
� Emergency room visits
Summary & Lessons Learned� California is a highly capitated and competitive market
with diverse population – urban and rural
Culture
Economic – affluent and extreme poverty
� Healthcare – Payer sources (IPA’s, Medical Groups, � Healthcare – Payer sources (IPA’s, Medical Groups, Hospitals – Cancer Center Insurance Plans)
Medicare Advantage Plans
Full risk or shared risk
� Needs Assessment of Payer Source
Identify their goals and outcomes
Reduction of costs with high quality patient care
MCCM Details� The model is designed to:
� Increase access to supportive care services provided by hospice;� Improve quality of life and patient/family satisfaction;� Inform new payment systems for the Medicare and Medicaid programs.
� Number of Participants: 141� California Participants: 4
� Assisted HomeCare Inc. dba Assisted Hospice Care (Los Angeles, California)� Assisted HomeCare Inc. dba Assisted Hospice Care (Los Angeles, California)� Assisted Home Hospice (Los Angeles, California)� Sea Crest Hospice Services, Inc. (Orange County, California)� CareChoices Hospice and Palliative Care Services, Inc. (Orange County, California)� Hospice of Saddleback Valley (Orange County , California)
� 5 year pilot� The model will be phased in over 2 years.
� Participating hospices will be randomly assigned to Phase 1 or Phase 2. � Services will begin starting January 1, 2016 for the first phase of participating hospices and
in January 2018 for the remaining participating hospices. � Participating hospices will receive payment under the model through the standard
Medicare claims process
How does MCCM operate?� The hospices will be paid a $400 per beneficiary per month
(PBPM) fee for providing services under the model for 15 or more calendar days per month.
� If services are provided under the model for fewer than 15 calendar days per month during the first month that the calendar days per month during the first month that the beneficiary is in the model, the hospices will be paid $200 PBPM.
� As the beneficiary is not electing the Medicare hospice benefit, hospices participating in this model will not receive the Medicare Hospice Benefit per diem rates
� Services provided under the model are not subject to a co-pay
Target Population� The target population for the Medicare Care Choices Model is:
� Medicare beneficiaries who are eligible for the Medicare Hospice Benefit and dually eligible beneficiaries who are enrolled in traditional Medicare and eligible for the Medicaid hospice benefit.
� Medicare and dually eligible beneficiaries must not have elected the Medicare Hospice Benefit (or the Medicaid hospice benefit) within the last 30 days prior to participating in the model and satisfy all the eligibility criteria listed in the to participating in the model and satisfy all the eligibility criteria listed in the Request for Applications.
� The model provides Medicare beneficiaries who qualify for coverage under the Medicare hospice benefit and dually eligible beneficiaries who qualify for the Medicaid hospice benefit the option to elect to receive supportive care services typically provided by hospice while continuing to receive curative services
� Participation is limited to beneficiaries with:� advanced cancers� chronic obstructive pulmonary disease� congestive heart failure� human immunodeficiency virus/acquired immunodeficiency syndrome
(HIV/AIDS).
The Sea Crest Care Pathways
Program Goals� Promote the highest quality of life by controlling symptoms such as pain, shortness of
breath, nausea, vomiting, fatigue and anxiety.� Provide psychological, spiritual and relational support for patients, families and staff.� Facilitate communication about the illness process and options for care.� Educate community hospitals, physicians, skilled nursing facilities, families, patients,
and our staff about palliative care practices and philosophies.� Conduct research and promote community efforts to continuously improve the quality of � Conduct research and promote community efforts to continuously improve the quality of
care for people with serious and life-threatening illnesses.� Program advantages and benefits:
� Improved quality of life that allows patients the time to live every moment.� Intensive symptom and comfort management (alleviate pain, fatigue, anxiety, nausea, loss
of appetite, sleeplessness, depression and other complex medical care issues).� 24-hour phone access to RN Program Managers and/or triage nurses that coordinate
medical, psychological, and related support and communication services.� Trusted care coordination for intelligently navigating the health care system.� Education regarding all care options.� Guidance regarding complex treatment, emergency room admission or re-hospitalization
choices.� Physical, emotional and spiritual support to encourage complete well-being throughout
the care continuum.
Medi-Cal Palliative Care
Program Development
• SB 1004 (Hernandez) Enacted in 2014
• DHCS has been consulting with palliative care
experts and stakeholders:experts and stakeholders:
• Develop a shared understanding of palliative care
• Review data findings
• Consider performance measures
• Review October 2, 2015 Medi-Cal Palliative Care
Paper
DHCS Goals for Medi-Cal Palliative Care
1. “Establish standards and provide technical assistance for Medi-Cal managed care plans to ensure delivery of palliative care services.”
2. “Establish guidance on the medical conditions and prognoses that render a [Medi-Cal] beneficiary eligible for the palliative care services.” [Medi-Cal] beneficiary eligible for the palliative care services.”
3. Develop a Medi-Cal palliative care policy that, to the extent practicable, is “cost-neutral to the General Fund on an ongoing basis.”
4. Define Medi-Cal palliative care services, to include but are not limited to “those types of services that are available through the Medi-Cal hospice benefit.”
5. Provide access to both hospice-type services and curative care at the same time, to the extent the services are not duplicative, for beneficiaries eligible for Medi-Cal palliative care.
Medi-Cal Palliative Care Scope
� Medi-Cal palliative care will use specific
definitions of eligible conditions, services, and
providersproviders
� Specificity is needed:
� To meet the requirements of SB 1004
� Long- term success is more likely through an
incremental approach
Delivery System and Dual-Eligible
Considerations
• Initial focus on managed care; further analysis
needed for fee-for-service Medi-Cal
• Initial focus on Medi-Cal only beneficiaries (not • Initial focus on Medi-Cal only beneficiaries (not
dually eligible for Medicare)
• Considering policy options for beneficiaries in
HCBS waiver programs, nursing facilities, and
potentially Cal Medi-Connect.
Proposed Eligible Condition for
Medi-Cal Palliative Care� Late-Stage/High Grade Cancer with significant
functional decline or limitations
� Should DHCS provide more specific
standardized clinical criteria on this condition?
� Allow Medi-Cal Managed Care Organizations
(MCO) to use one of several existing screening
protocols?
Additional Conditions
• Existing palliative care programs generally include
additional conditions, such as advanced Congestive
Heart Failure or end-stage pulmonary disease.Heart Failure or end-stage pulmonary disease.
• Managed care plans that currently (or in future)
authorize palliative care consults and services for
patients with other medical conditions may continue to
do so.
Proposed Palliative Care Services• When reasonable and necessary for the palliation or
management of a qualified serious illness and related conditions, and when provided by qualified personnel:
• “Hospice-Type” Services
• (DHCS All-Plan Letter 13-014)
• Additional Services:
• Palliative Care Consultation, Advance Care Planning
• Care Coordination, Assessment, Interdisciplinary care team, Care Plan
• * Curative Care *
Provider Qualifications• Consider full range of inpatient, outpatient,
community-based providers.
• DHCS is considering options:
• Palliative Care Training
• Palliative Care Certification, Accreditation
• Health Plan Credentialing
• Add Palliative Care component to existing provider
qualifications
Performance Measures
• DHCS developing performance measures
• DHCS considering linking payment to performance • DHCS considering linking payment to performance
measures, particularly in fee-for-service
Questions and Contact Info
DHCS Palliative Care Website:
http://www.dhcs.ca.gov/provgo vpart/Pages/Palliative-Care- and-SB-1004.aspxCare- and-SB-1004.aspx
Contact: [email protected]