Leiomyosarcoma of the stomach. A clinical and pathological study
Transcript of Leiomyosarcoma of the stomach. A clinical and pathological study
LEIOMYOSARCOMA OF T H E STOMACH A Clinical and Pathological S t u d y
J O m BERG, M.D., AND GORDON MCNEER, M.D.
EIOMYOSARCOMA of the stomach is so rarely L encountered in the surgical practice of any one individual that accumulation of data has usually been the result of the stim- ulation of intellectual curiosity by a single clinical experience followed by a study of the medical literature. Furthermore, in those larger series of consecutive cases reported from the major surgical clinics, there has not seemed to be a concerted attempt to correlate patho- logical features with treatment and end re- sults. Though confirmation of the observa- tions of others is a worthy contribution, our study has led us to hope that a wider objec- tive might be obtained.
I n our review of end results in the treat- ment of primary gastric cancers at Memorial Center, we observed that an unduly large pro- portion of 5-year survivors were patients with tumors of mesodermal origin. Furthermore, leiomyosarcoma was found to be more ame- nable to excisional surgery than any other single histological variety of gastric cancer. It became increasingly clear that this was due to the fact that the majority of cases of this type of tumor of the stomach were of a low grade of histological malignancy. This study has led us to believe that we might be able not only to discuss treatment in general but also to apply the summation of our knowledge to the management of the individual case with a rea- sonably correct prediction of the end result.
CLINICAL MATERIAL
During the years 1935-1955, while 1,623 pa- tients with carcinoma of the stomach were seen at Memorial Center, there were 24 pa- tients with gastric leiomyosarcomas and 38 pa- tients with presumably primary malignant lymphomas of the stomach.
From the Pathology Laboratories and the Gastric and Mixed Tumor Services, Memorial Center for Can- cer and Allied Diseases, New York, N.Y.
Presented at the Twelfth Annual Cancer Symposium of the James Ewing Society, April 2, 1959.
The roentgenological diagnosis of myomatous tu- mors of the stomach was performed by Robert S. Sherwin, M.D.
Thus leiomyosarcomas appeared to be slightly less common than the lymphomas and made up about 1.3% of all primary gastric neoplasms seen during that period.
While the histological basis for defining an intramural tumor of the stomach as a leiomyo- sarcoma ,rather than a schwannian sarcoma, fibrosarcoma, liposarcoma, or some other va- riety will be considered in more detail later, it can be stated here that during this 20-year period only one malignant connective tissue gastric tumor was encountered that might possibly have represented anything but lei@ myosarcoma. This tumor was described as an anaplastic liposarcoma located in the greater omentum. Observers differed in their opinions as to whether the wall of the stomach was or was not actually involved. Since in some of the gastric leiomyosarcomas in this series the bulk of the tumor lay outside of the stomach proper, it is conceivable that this case of lipo- sarcoma might have had a similar origin. In any event, it has been our experience that lei- omyosarcomas and malignant lymphomas of the stomach are uncommon but that other sarcomas of the stomach are relatively much rarer.
Of the 24 patients with leiomyosarcomas in our series, 3 were under observation for the management of recurrences 1 to 4 years after the primary tumor had been surgically re- moved at other hospitals. T h e remaining 21 patients came as candidates tor diagnosis and/ or definitive treatment.
CLINICAL CHARACTERISTICS
Age. T h e youngest patient in the series was a 33-year-old woman, and there were 3 patients in their 70’s. The median age in the series was 53 years; 79% of the patients were between 40 and 70 years of age.
Sex. T h e cases were equally divided among the sexes, there being 12 men and 12 women. T h e women were an average of 5 years younger than the men at the time of diagnosis.
Race. There were 3 Negro patients and 1 Hindu in this series. Since our 36 cases of ma-
25
‘26 CANCER Jnn unry-Feb runry 1960 Vol. 13
lignant gastric lymphoma occurred only in white patients, even this small number of dark-skinned patients suggests a racial differ- ence in the distribution of leiomyosarcoma. This observation has been made by others.
Other Clinical 0 bseruations. Hysterectomy for uterine leiomyomas had been performed in the case of 3 of the 12 women patients, while a large fibroadenoma was removed from the breast of another. A “malignant gastric ulcer” had been excised 19 years before the appearance of sarcoma in the stomach of I male patient. Yet another developed gastric cancer 6 years after local excision of a small leiomyosarcoma of the stomach. One instance of leiomyosarcoma was found incidentally dur- ing the resection of an esophageal carcinoma.
Symptoms. Asymptomatic. O f the 21 primary leiomyosarcomas, 2 were found incidentally during the course of operations for other intra- abdominal conditions. An zdditional case was discovered as the result of a routine gastroin- testinal roentgenographic examination made an an asymptomatic patient in the Strang Can- cer Prevention Clinic of Memorial Center. (It is worthy of note here that none of these 3 small tumors has recurred within the 5-year period after resection.) A diagnosis of gastric sarcoma was established for 1 patient whose symptoms originally led to the finding of pul- monary metastases of undisclosed origin.
Dzrrntion of Symptoms. Only 4 patients re- ported symptoms of more than 1 year’s dura- tion. Diagnosis was established within 6 months in the case of 9 paticnts. Eight pa- tients complained of mild to moderate indi- gestion as their first symptom. Two patients had indigestion for 5 and I0 years respectively before seeking medical advice, whereas in the remainder persistence of symptoms demanded attention within I year of onset.
Synzfifomntic. T h e 17 patients who came to Rlemorial Center with symptoms referable to the gastric tumors suffered Zrom a varietv of complaints. FOW described the presence of an abdominal mass as the first warning of disease, whereas a fifth made a similar observation soon after the onset of vague symptoms of in- digestion. While the tumors of 2 of these pa- tients were inoperable and a third recurred within a year of surgery, thc other 2 were re- sectable and the patients have remained free of cancer well beyond the 5-year follow-up period.
In 1 individual the history was so typical of peptic ulcer that he was treated by the usual
methods without benefit of roentgenographic investigation. Upon examination in this clinic he was found to have massive, inoperable can- cer. Pain was a predominant complaint in 5 patients, though an initial symptom in only 1. Frank hematemesis was observed in 1 and weakness in another, though the weakness de- scribed by 2 others might well have been the result of loss of blood from the stomach.
ROENTGENOLOGICAL DIAGNOSIS
Benign and malignant muscle tumors of the stomach constitute a particularly interesting and challenging group of lesions for the roent- gen diagnostician. This is because many of these tumors are recognizable by radiological means as belonging to this histological cate- gory. However, it is not possible to tell whether such a tumor is a benign or malignant one. T h e reasons for this histological variety of gastric neoplasm being recognizable to the roentgenologist depend upon the location of site of origin, the usual cell structure (which is spherical), and the frequent presence of a more or less characteristic type of ulceration. On the basis of our studies, the combination of 2 or 3 of these roentgenological characteristics makes possible the designation of the histo- logical type in fully 50% of cases.
Two-thirds of the tumors in this series showed a spherical shape, while the rest were oval or irregular and lobulated. Most a p pearetl to measure 3 to 6 in. in size with varia- tions of from 1 to 20 in. Nine showed ulcer- ation. There was no evidence of calcification within any tumor, a point that seems some- what unusual. However, it is possible that the barium, by hiding parts of the tumor, pre- vented recognition of the small calcific fleck or flecks that are sometimes found in tumors arising in muscle.
T h e ulcerations were seen to occur upon the mucosal or intraluminal aspect of the tumors. Thew excavations varied in size from M in. to nearly 1 in. in diameter. In 1 tumor, several ulcerations were seen. About half the new growths with ulcerations showed a rather shal- low niche, while the other half had deep ul- cers. One tumor revealed a sinus tract that penetrated deeply into the mass. T h e edges of the ulcerations were generally sharp, and the configuration of the mouth of the ulcer was circular or oval.
TVnZZ Location. T h e relationship of the myo- genic tumors to the gastric wall was evaluated
h'o. 1 LEIOMYOSARCOMA OF STOMACH - Berg & McNeer 27
roentgenologically. It was found that 50y0 of the tumors were mural in location. It was these that usually represented a sharp, regular, abrupt mucosal margination characteristic of the submucosal, mural origin of a space-occu- pying defect in a hollow viscus. This sharp margin that is evident on full face view is manifested also in profile studies as a right angle margin or slightly overhanging edge. About 33% of the tumors had their bulk out- side the stomach, and they presented as a soft tissue mass sometimes displacing the stomach itself as well as nearby organs. T h e remainder were either chiefly intraluminal or chiefly ex- traluminal, but they showed some degree of submucosal disturbance or in other words an intramural component. About 40% of the to- tal number of tumors caused some degree of gastric displacement, but this was usually of a minor or local type.
Afurosa. T h e mucosal lining revealed ab- normalities in all except a few cases that were almost entirely extragastric in location. Gen- erally the mucosal pattern was stretched, thinned, somewhat fixed, and occasionally re- ticulated. Usually the stretched mucosa was quite smooth and structureless unless broken by the presence of ulceration. As noted before, a sharp margin around the mucosal defect was commonly seen.
S u m m a r y of Roentgm Findings. T h e pres- encc of a mural defect of water density, spheri- cal shape, with smooth, abrupt, regular mu- cosal edges, and a stretched, smooth, or slightly reticulated mucosal surface with intraluminal ulceration made the roentgen identification of myogenic tumors of the stomach quite depend- able. The careful application of the principles developed by Schatzki and Hawes' for the identification of intraluminal, mural, and in- tramural masses is particularly important in the roentgen detection of myomatous n e e plasms. This means that both mucosal and contour studies are needed, and both profile and full face views should be obtained.
DIFFERENTIAL DIAGNOSIS
When the roentgen appearance was not typical of a myogenic tumor, polypoid carci- noma was the most frequent diagnosis offered. Once or twice i t was possible only to state that an extragastric tumor mass was present. The pancreas was the suspected site of origin once. When the myogenic tumors were small, the differential diagnosis from a neoplasm of mu-
cosal origin was impossible. Adenomatous polyp was mentioned diagnostically several times. Only a descriptive diagnosis as to the prcsence of a mass lesion was made on a few occasions. T h e limitation of the roentgen method for distinguishing between a mural and a inucosal lesion when the defect is of small sire is very well recognized. Pancreatic rests, because of the presence of a duct opening, can cause difficulty in differential diagnosis. However, in our experience ulcera- tion is not visualized in the small myomas and myosarcomas. Pancreatic rests are usually small.
GROSS PATHOLOGY
Size. T h e findings in 19 operable cases were closely correlated with the size of the primary tumor in each case. Twelve of the tumors were 10 cm. or less in greatest diameter. In every case they were single lesions without either gross or microscopic evidence of metastases. By contrast, 6 of the 7 larger tumors showed either omental metastases or extension into the liver or both. Two of these were held to be completely inoperable, and a tliircl was treated by a palliative subtotal gastrectomy.
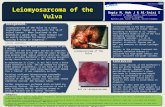
C'lrerntion. In most cases the symptoms ref- erable to bleeding or epigastric pain could he explained by the tendency of these tumors to show ulceration of the gastric mucosa. U1- ceration could be seen grossly in 7 of the 17 resected specimens (Fig. l), and in 3 instances it was multiple. One patient had 4 distinct ulcers over a 5.5-cm. tumor.
Location. T h e smaller tumors tended to be located in the wall of the stomach, but the larger the tumor the greater were the chances that the bulk of the mass would be outside the stomach proper. At times the connection with the stomach was by means of a small point, at others by a broader base. When the tumor arose from the anterior wall of the stomach or from the greater curvature, growth tended to be into the omentum. Extragastric location was associated more often with the larger myogenic tumors. When the tumor originated from the posterior wall or the lesser curvature, there tended to be direct exten- sion into the retroperitoneal tissues and liver. This, of course, was seen most frequently when the tumors were especially large, but it also occurred with tumors as small as 5 cm. in diameter. T h e propensity of these tu- mors for invasion of the structures with which
28 CANCER January-February 1960 Vol. 13
FIG. 1. A 12-cm. leiomyosarcoma with 3 ulcerations. The letters indicate the following: A, esophageal orifice; B. spleen; C, onientuni; D, pylorus; and E, pancreas.
they come into contact means, of course, that any capsule or apparent line of surgical cleavage cannot be relied upon as a true mar- gin between tumor and seemingly healthy adjacent tissues.
Texture. T h e cut surfaces of most of these tumors look like cellular uterine myomas, possessing yellow-white tissue bulging forth in interweaving bands (Fig. 2). The consist- ency varies from extremely firm to encephaloid (Fig. 3). Only one of the tumors in this series was predominately cystic. In this case there were many cysts filled with bloody fluid, the over-all mass measuring 15 cm. in diameter. It may be a coincidence that this case repre- sented the only example of clinical cure in which the sarcoma was larger than 10 cm.
HISTOLOGICAL PATHOLOGY
Tissue was available for examination in 19 of the 21 cases of primary lesions and in 2 of the 3 cases of recurrent sarcoma. Histo-
logically these tumors formed a heterogeneous group. They varied greatly both as to degree of anaplasia and as to cell type. The nuclear differences were important because they were closely correlated with the subsequent behav- ior of the tumors. The cytoplasmic differences were not so correlated; they were important as possible sources of confusion.
T h e classical pattern of leiomyosarcoma is illustrated in Fig. 4. The cells and nuclei are spindle shaped, and there is abundant cyto- plasm. There is a tendency, irregularly mani- fested, for the cells and nuclei to lie parallel to one another and so to form bands. Rlicro- scopically the most obvious difference between this tumor and a benign myoma is the in- creased number of nuclei in a field. However this is variable and can be misleading. T h e occasional sarcoma will have a great deal of ground substance between the spindle cells. T h e basic difference lies in the character of the nuclei in the tumor. In the sarcomas, in contrast to benign myomas, the nuclei are
hyperchromatic and vary significantly in size and shape. This change is the diagnostic sine qua non and the common thread through all the variations of pattern.
Figure 5 illustrates one of the variations of the basic pattern that has been a source of confusion. Most leiomyomas show occasional rows of aligned nuclei. Sometimes this tend- ency is extremely prominent. When it is cou- pled, as it is in the illustration, with a glassy cytoplasm and ground substance that is un- like sarcoplasm, the superficial resemblance to neurilemoma can be striking. Careful pe- rusal of the whole tumor, however, will usually reveal more typically myomatous areas. In any case, direct comparison of a tumor of this type with a true neurilemoma will demonstrate a multitude of small but important differ- ences. We, in fact, could find no example of
No. 1 LEIOMYOSARCOMA OF S r o m c H - Berg G. hfcNeer 29 a primary neurogenic tumor of the stomach in our material.
Figure 6 illustrates the most common type of major deviation from the typical histo- logical pattern of leiomyosarcoma. I t was seen in 7 cases in this series. In 2 it was the only pattern, and in 4 it was associated with the classic design. In one of these latter cases and in another in which there was no spindle cell element, there were large areas of hydropic degeneration (which will be discussed subse- quently). The point to be made about tumors with the pattern shown in Fig. 6 is that it is a cytoplasmic change. While the nuclei are somewhat less oval than those seen in Fig. 4, the important factor is the absence of any formation of the cytoplasm into spindle, ori- ented cells. There is less material between nuclei, so the first reaction may be to rate this
FIG. 2. Tumor surface resembling a
FIG. 3. Encephaloid myosarcoma. FIG. 4. Classical leiomyosarcoma pat-
uterine leioni yoma.
tern.
30 CANCER January-February 1960 Vol. 13
FIG. 5. Area rewmbling neurilemoma in a recurrent leiom yosarcoma. FIG. 6. .4 non-spindle cell area in the same tumor as in Fig. 5. FIG. 7. .4 cellular area from another large leiomyosarcoma. FIL. 8. Pseudolipoid degeneration in a 10-cm. leiomyosarcoma. The patient is well 5 years after resection.
type as relatively anaplastic. Actually, this may not be the case. Comparison shows that the nuclei as shown in Fig. 4 are more variable and more truly hyperchromatic than those seen in Fig. 6, giving us every reason to con- sider the former the more aggressive cancer. In support of this thesis, the sarcoma shown in Fig. 4 also possessed a higher rate of mi- tosis.
Figure 7 illustrates a variation o f this non- myomatous pattern in which the cytoplasm stains more prominently. In this particular case, also, the nuclei are moderately anaplas- tic, though this was not an invariable obser- vation.
Figure 8 illustrates the histological variety o f leiomyosarcoma that is most confusing at first glance. Most of the cells show cyto-
plasmic clear spaces (hydropic degeneration) to the point where any suggestion of myoma is lost. This change is associated with nuclear pyknosis, as the illustration makes clear. This is perhaps the best clue to the fact that what one is seeing is not a pattern of growth, and especially not a liposarcoma, but a degenera- tive process. This pattern was present in large areas in 5 cases (and a few cells showed the changes in several other cases). In 1 case this pattern was the only one seen and a t first i t was a diagnostic problem, but in the re- maining cases multiple sections clearly demonstrated its origin from the classical leiomyosarcoma. Again we observed that this histological pattern was not associated with especially anaplastic tumors or with cases that bore a particularly poor prognosis.
No. 1 LEIOMYOSARCOMA OF STOMACH Berg & McNeer 31
T h e classification of patterns of leiomyo- sarcoma is not exhausted by these types, nor is it felt that these variations have special meanings. Though we have no particularly good case to illustrate another important type, there was one case referred from another hospital that looked largely angiomatous but in which there was some small but definite histological proof of the basic myogenous na- ture. Our present philosophy, then, is that any malignant connective tissue tumor in the gastric wall may be held to be a myosarcoma until proved otherwise. Confusion is likely when only a small amount of material is ex- amined. Thorough study of the tumor in question by comparison with standard tumors of the various cell strains should resolve the difficulties. The reason that i t is worthwhile to identify a gastric sarcoma is that the prog- nosis of the case then may be estimated with some reasonable degree of accuracy by taking into account two parameters, size of tumor and mitotic activity.
MICROSCOPIC EVAL~JATION OF MALIGNANCY
Little need be added to the points made by Stout3 and by Giberson et al.1 When the mitotic rate was high throughout the tumor, the patient invariably died of recurrent sar- coma despite treatment. This was observed in 5 of our 19 primary cases. While 4 of these tumors were large when first seen, 1 was only 5 cm. in diameter. By contrast, when mitoses were found either rarely or inconstantly, the prognosis was much better. Of the 14 remain- ing patients, only 2 are known to have died of recurrent sarcoma. One of these had multi- ple distant metastases when first seen, and the other patient had omental metastases. An- other patient in this category also had omental metastases but was lost to follow-up (in India) after remaining lree of recurrence for 2% years.
Within this group of lower grade tumors an attempt was made to correlate the presence or absence of metastases with the usual meas- ures of anaplasia, nuclear hyperchromasia, nuclear variation in size and shape, and the loss of nuclear polarity. Perhaps because the series was not large, such correlations were neither clear nor striking. T h e primary use of these parameters was to draw the line be- tween sarcomas and benign leiomydmas. One must rely entirely upon this type of cell ana- plasia to diagnose a sarcoma because under
the microscope the benign lesions are as poorly encapsulated as are the tumors capable of metastasis. Figure 9 represents about the least atypia that we could confidently label sar- coma in the light of our present experience. We observed this picture with fair uniformity throughout the sections taken from a massive (4 kg.) specimen removed during a palliative subtotal gastric resection.
TREATMENT
Surgeiy. T h e only treatment known to be effective for gastric myosarcomas is excisional surgery. The extent of surgery in our series was dictated by the size and extent of the tumor. Four smaller tumors, favorably located, were excised along with an adequate margin of normal gastric wall. There were no recur- rences in this group (all of the tumors proved to be of a low grade of histological malig- nancy). In the other 12 resectable cases the operation performed was subtotal or total gastrectoniy, with the choice again determined by the location and extent of the tumor. There were recurrences in 2 of 7 patients when sub- total gastrectomy was performed. One of these patients, with a relativeIy small but very ana- plastic tumor, died of hepatic metastases but without recurrence in the operative area. In the other instance also, the tumor was ana- plastic; it was quite large (18 cm.) and had invaded the liver. Wound recurrence was quite prompt. The 1 recurrence among 5 pa- tients treated by total gastrectomy was ob-
FIG. 9. Histologically low grade leiomyosarcoma in a patient who presented with a massive and nonre- sectible stomach tumor.
32 CANCER Janualy-February 1960 Vol. 13
served in a man who had had omental metas- tases at the time of operation.
X-ray Therapy. Radiation therapy was given in all of the 10 instances of recurrent or inoperable sarcoma. In no case did it pro- duce notable regression of tumor.
End Results. The total group consisted of 24 patients. Three of these were seen for re- current sarcoma sometime after the primary tumor had been resected elsewhere. These pa- tients died of uncontrollable sarcoma 7 years, 6 years, and 2 years respectively after the ini- tial resec t ion4 years, 4 years, and 1 year respectively after they were first seen in our hospital.
Twenty-one patients were seen here during the period of initial diagnosis and treatment. Two were deemed to have inoperable cancer because of distant metastases, and they died of sarcoma 1 and 16 months respectively after diagnosis. Nineteen patients were surgically explored, and of these 3 (16%) presentcd in- curable tumors. These patients were all dead within 9 months, 1 dying as a direct result of the operation.
Sixteen patients underwent gastric resection with hope of cure (76.9%). Ten were alive and free of disease when last seen 5 years or more after operation. This figure represents 47.@5 of the 21 patients seen in the primary stage of the disease. Only 3 patients in the curative group are known to have died of the disease. All had recurrences within 2 years of resection and died within 4 years. Two pa- tients died of other causes within a year of operation, and a third was lost to follow-up after 2v2 years. Considering only the 13 deter- minate patients, 77% were alive and free of disease 5 years after operation. T h e absolute 5-year survival rate was 41.7% (all cases).
THE PATTERN OF METASTATIC SPREAD
The most common sites for the first appar- ent metastases in those patients with recurrent tumor were the connective tissues around the stomach, especially the omentum and retro- peritoneum (6 of 10 cases). True lymph node metastases were found in only 1 case and that a t autopsy. In 3 cases hepatic metastases were the first to make themselves evident; in a fourth case they were observed in addition to more extensive tumor in perigastric connec- tive tissue. In 1 case pulmonary metastases were the first to be observed: in another both pulmonary and hepatic metastases were seen.
These 2 cases, in addition to 1 in which there were metastases to bone, represent the only examples in which the sarcomas had spread beyond the abdomen at the time of death. Hence in 70% of the patients for whom we have data, there was no evidence that the tumors, though responsible for the patients’ deaths, had metastasized extra-abdominally. Three of the deaths were due primarily to hepatic involvement. Multiple obstructions of the bowels and vessels and massive tumor growth per se were responsible for death in the other cases.
DISCUSSION AND CONCLUSIONS
It would appear from these data that the main problem in the diagnosis and treatment of gastric leiomyosarcomas is their tendency to remain symptomatically silent until they have grown to large size and have extended from the stomach into adjacent organs. When the sarcomas were found before such exten- sion had occurred and before there were grossly visible metastases, excision appeared to be curative in every case but 1. Because the surgeon’s evaluation of the extent of the sar- coma at the operating table appears to be relatively accurate and because regional lymphatic metastases are rare, elaborate and meticulous lymph node dissections seem un- necessary. Extended operations seem indicated only when demanded by the location and size of the tumor. There is no major difference in this regard between the treatment of be- nign and malignant myogenic tumors of the stomach. This means among other things that the task is simplified for the pathologist who may be asked for a frozen section diagnosis. Once he is in a position to assure the surgeon that the tumor in question is a tumor of con- nective tissue origin, there is no great need to attempt to separate a low grade myosar- coma from a cellular myoma or a neurilemoma since in all cases the principle of treatment is the same-to encompass all gross tumor in the excised surgical specimen.
SUMMARY
A clinical and pathological study of 24 leiomyosarcomas of the stomach is presented. The results of treatment are correlated with the mitotic activity of the tumors and the size and extent of the sarcomas at the time of oper- ation. As long as the tumors did not invade
No. 1 LEIOM\-OSARCOMA OF STOMACH * Berg 6. AlcNeer 33
the liver, the region of the celiac axis, or other vital structures and showed no gross evidence of metastases, excisional surgery recurrent sarcoma.
proved very effective. Only 1 of 13 patients included in this favorable category died of
REFERENCES
1 . GIBERSON, R. G.; DOCKERTY, M. B., and GRAY, ysis of intramural extramucosal lesions of gastroin- testinal tract in general. Am. J . Roentgenol. 48: 1-15, 1942.
3. STOUT, A. P.: Tumors of the Stomach: Atlas of Tumor Pathology, sect. 6, fasc. 21. Washington, D.C. Armed Forces Institute of Pathology. 1953.
H. K.: Leiomyosarcoma of stomach; clinicopatholo ic study of 40 cases. Surg. Gynec. Q Obst. 98: 186-186, 1954.
2. SCHATWI, R., and HAWES, L. E.: Roentgenological appearance of extramucosal tumors of esophagus; anal-