Latissimus dorsi myocutaneous free flap vascularised by an extra-anatomic graft in the lower limb...
-
Upload
jack-fisher -
Category
Documents
-
view
213 -
download
0
Transcript of Latissimus dorsi myocutaneous free flap vascularised by an extra-anatomic graft in the lower limb...

British Journal of Plastic Surgery (1983) 36,480-482 0 1983 The Trustees of British Association of Plastic Surgeons
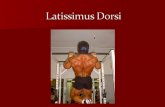
Latissimus dorsi myocutaneous free flap vascularised by an extra-anatomic graft in the lower limb following traumatic disruption of the popliteal artery
J. FISHER, T. A.
Department of Plastic Surgery, National Naval Medical Centre, Bethesda, Maryland and William S. Middleton Memorial Veterans Hospital, Madison, Wisconsin, USA
Summary-A case is presented in which the thoracodorsal artery of a latissimus dorsi free flap was anastomosed to an autogenous reverse saphenous bypass graft. The bypass graft was used to revascularise a leg with traumatic disruption of the popliteal artery and an open cornminuted fracture of the distal tibia and fibula with extensive soft tissue loss. At Z-year follow up, isotope scans showed patency of the extra-anatomic graft and a good flow into the thoracodorsal artery.
Extensive soft tissue injuries of the lower limb are trauma accounted for approximately one-quarter frequently associated with popliteal artery dis- of popliteal vessel injuries. In their series of 83 ruption. Snyder et al. (1979) reported that blunt popliteal artery injuries, 27 cases required arterial
Fig. 1
Femw&
Artery
Graft -
,Popliteal
Artery
- Latissimus
Dorsi
Flap
Posterior
Tibia1
Artery
Fig. 2 Fig. 3
Figure l-Open comminuted fracture of the distal left leg. The arrow indicates the extra-anatomic vascular graft linking the femoral artery to the posterior tibia1 artery. Figure 2-Diagram of the extra-anatomic vein graft and the area covered by the latissimus dorsi free flap. Figure 3-X-ray to show non-union of the distal tibia 16 months after free tissue transfer.
480

LATISSIMUS DORSI MYOCUTANEOUS FREE FLAP VASCULARISED BY AN EXTRA-ANATOMIC GRAFT 481
vein grafts and the single failure in this group was associated with incomplete soft tissue coverage.
The use of free tissue transfers for recon- struction of the lower extremity has become a common practice (Serafin and Smith, 1979). Many extremities that previously would have been ampu- tated are now successfully salvaged. Early in the evolution of free tissue transfers to the lower extremity, end-to-end arterial anastomoses were performed (Daniel and Taylor, 1973; O’Brien et al., 1973). However, in the last few years, prefer- ence has been directed toward end-to-side vascular anastomoses with maintenance of distal flow (Ikuta et al., 1975; Godina, 1979). Single vessel extremities are no longer considered a contra- indication to the use of free tissue transfers. In extremities in which revascularisation has been accomplished with an “extra-anatomic” graft, one may be dealing with the equivalent of a single vessel leg. By combining the technique of “extra- anatomic” vascular grafting with that of micro- vascular tissue transfer, it is possible to revascular- ise an extremity and to use the bypass graft as a source of blood supply for the free tissue transfer.
Case report
A 23-year-old man sustained bilateral open tibia1 frac- tures in May, 1980, when struck by an automobile. His
initial treatment consisted of debridement of the wounds and fixation of the fractures with external fixators to each leg. Approximately 2 days after the injury the skin over the patient’s left foot became mottled with dimin- ished peripheral pulses. An arteriogram revealed dis- ruption of the popliteal artery above the trifurcation. An autogenous reverse saphenous vein graft was performed between the distal femoral and the distal posterior tibia1 artery.
Approximately 3 weeks after the injury, the Hoffman external fixators were removed: the patient was placed in bilateral long-leg plaster casts and transferred to the National Naval Medical Cente at Bethesda, Maryland. Upon receiving the patient, we initially performed an arteriogram which revealed a patent graft and retrograde filling of the posterior tibia1 artery. The patient had a large soft tissue defect in the distal third of the leg with an open comminuted fracture. He also had an open comminuted fracture of the contralateral lower extremity.
In July, a latissimus dorsi free flap was used for coverage of the distal third of the revascularised left leg. The initial plan was to use the posterior tibia1 vessel proximal to its anastomosis with the bypass graft. However, because of poor retrograde flow through the posterior tibia1 vessel, this plan was abandoned. A segment of the 45 cm extra-anatomic vascular graft was exposed in the mid lower leg and an end-to-side arterial anastomosis was performed between the thoracodorsal artery and the graft (Figs. 1 and 2). The thoracodorsal vein was anastomosed to the intact saphenous vein of the
Fig. 4 Fig. 5 Fig. 6
Figure 4-X-ray of the distal tibia to show union after bone grafting. Figure 5-Appearance of the extremity 24 months after free tissue transfer. Figure 6-Technetium scan to show flow through the extra-anatomic graft (large arrow) and the thoracodorsal vessel (small arrow) to the latissimus dorsi free flap 24 months after free tissue transfer.

482 BRITISH JOURNAL OF PLASTIC SURGERY
extremity. Post-operatively the free latissimus dorsi flap did well. In September, 1980, the patient was taken out of bilateral Hoffman external fixators and placed in bilateral plaster casts. Examination of the left lower extremity in November 1981 revealed a healed free flap with adequate protective sensation of the foot. However, a mobile non-union of the left tibia1 fracture persisted (Fig. 3) for which a left postero-lateral bone graft was performed and an external fixation device applied. By June, 1982, the patient demonstrated healing of the left tibia1 non-union and was walking on the extremity (Figs. 4 and 5). Two years after the free tissue transfer, a Technetium 99 m methylene diphosph- onate bone scan with early views of the extremity showed arterial flow through the autogenous extra-anatomic graft and into the thoraco-dorsal vessel (Fig. 6).
Discussion
Prior to the advent of free tissue transfers, the reconstruction of an extremity as severely injured as this would have been difficult. At follow up 2 years after the accident, the fracture site was healed and isotope flow studies showed patency of the extra-anatomic vascular graft as well as the anas- tomosed thoracodorsal artery. This case demon- strates the feasibility of using free tissue transfers in conjunction with extra-anatomic vascular grafts.
Godina, M. (1979). Microvascular latissimus dorsi myocu- taneous flap. Transactions of VII International Congress of Plastic and Reconstructive Surgery, Rio de Janeiro.
Ikuta, Y., Watari, S., Kawamura, K., Sbima, R., Matsuishi, Y., Miyoshi, K. and Tsuge, K. (1975). Free flap transfers by end-to-side arterial anastomoses. British Journal of Plastic Surgery, 28, 1.
O’Brien, B. M., MacLeod, A. M., Hayhurst, J. W., and Morrison. W. A. (1973). Successful transfer of a large island flap from the groin to the foot by microvascular anas- tomoses. Plastic and Reconstructive Surgery, 52,271.
Serafin, D. and Smith, D. H. (1979). Composite tissue transplantation in soft tissue reconstruction of the lower extremity. In Serafin, D. and Buncke, H. J. Jr., Micro- surgical Composite Tissue Transplantation. St Louis: C. V. Mosby Company.
Snyder, W. H., Watkins, W. L., Whiddon, L. L. and Bone, G. E. (1979). Civilian popliteal artery trauma: an eleven-year experience with 83 injuries. Surgery, 85, 101.
The Authors
Jack Fisher, MD, Assistant Professor of Plastic Surgery, Mayo Medical School, Mayo Clinic. Rochester, MN.
Steven Macht, MD, bDS, Assistant Professor and Chief, Division of Plastic Surgery, George Washington University, Washington DC.
Thomas A. Lange, MD, Assistant Professor, Division of Orthopaedic Surgery, Wm. S. Middleton Memorial Veterans Hospital and University of Wisconsin Hospital and Clinics, Madison, Wisconsin.
References
Daniel, R. K. and Taylor, G. I. (1973). Distant transfer of an island flap by microvascular anastomoses. Plastic and Requests for reprints: Jack Fisher, MD, Mayo Clinic, Division Reconstructive Surgery, 52, 111. of Plastic Surgery, Rochester, MN 55905, USA.