K.15 Acute Rheumatic Fever
-
Upload
winson-chitra -
Category
Documents
-
view
219 -
download
0
Transcript of K.15 Acute Rheumatic Fever
-
7/30/2019 K.15 Acute Rheumatic Fever
1/31
Acute Rheumatic Fever
Muhammad Ali
Pediatric Cardiology Division
University of Sumatera Utara
-
7/30/2019 K.15 Acute Rheumatic Fever
2/31
Cause
ARF is believed to be an immunologic lesion thatoccurs as a delayed sequela of group A streptococcalinfection of the pharynx but not of the skin. Theattack rate of ARF after streptococcal infectionvaries with the severity of the infection, rangingfrom 0.3% to 3%.
Important predisposing factors include family historyof rheumatic fever, low socioeconomic status
(poverty, poor hygiene, medical deprivation), and agebetween 6 and 15 years (with a peak incidence at 8years of age).
-
7/30/2019 K.15 Acute Rheumatic Fever
3/31
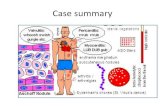
Pathology
The inflammatory lesion is found in many parts of thebody, most notably in the heart, brain, joints, andskin. Valvular damage most frequently involves themitral, less commonly the aortic, and rarely thetricuspid and pulmonary valves.
Aschoff bodies in the atrial myocardium are believedto be characteristic of rheumatic fever. These
consist of inflammatory lesions associated withswelling, fragmentation of collagen fibers, andalterations in the staining characteristics ofconnective tissue.
-
7/30/2019 K.15 Acute Rheumatic Fever
4/31
Clinical Manifestations
ARF is diagnosed by the use
of revised Jones criteria
The criteria are three groups of important
clinical and laboratory findings:
(1) five major manifestations
(2) four minor manifestations(3) supporting evidence of an antecedent
group A streptococcal infection.
-
7/30/2019 K.15 Acute Rheumatic Fever
5/31
-
7/30/2019 K.15 Acute Rheumatic Fever
6/31
HISTORY
History of streptococcal pharyngitis, 1 to 5weeks (average, 3 weeks) before the onset ofsymptoms, is common. The latent period maybe as long as 2 to 6 months (average, 4months) in cases of isolated chorea.
Pallor, malaise, easy fatigability, and other
history, such as epistaxis (5% to 10%) andabdominal pain, may be present.
Family history of rheumatic fever frequentlyis positive.
-
7/30/2019 K.15 Acute Rheumatic Fever
7/31
MAJOR MANIFESTATIONSArthritis Arthritis, the most common manifestation of ARF
(70% of cases) involves large joints
(e.g., knees, ankles, elbows, wrists).Often more than one joint, either simultaneouslyor in succession, is involved
characteristic migratory nature of the arthritis.Swelling, heat, redness, severe pain, tenderness, and limitationof motion are common.
The arthritis responds dramatically to salicylate therapy; ifpatients treated with salicylates (with documented therapeuticlevels) do not improve in 48 hours, the diagnosis of ARF probably
is incorrect.
Such patients have been categorized as havingpoststreptococcal reactive arthritis; the relationship of thisdisease to acute rheumatic fever remains undetermined.
-
7/30/2019 K.15 Acute Rheumatic Fever
8/31
CarditisCarditis occurs in 50% of patients:
Tachycardia (out of proportion to the degree of fever) is common; itsabsence makes the diagnosis of myocarditis unlikely.
A heart murmur of valvulitis (caused by mitral regurgitation [MR]and/or aortic regurgitation [AR]) is almost always present; without themurmurs of MR and/or AR, carditis should not be diagnosed.
the presence of MR or AR by echo and Doppler studies, withoutaccompanying auscultatory findings, cannot be taken as the solecriterion for valvulitis.
Pericarditis (friction rub, pericardial effusion, chest pain, and ECGchanges) may be present.
Cardiomegaly on chest x-ray films is indicative of pericarditis,pancarditis, or congestive heart failure (CHF).
Signs of CHF (gallop rhythm, distant heart sounds, cardiomegaly) areindications of severe carditis.
-
7/30/2019 K.15 Acute Rheumatic Fever
9/31
Erythema Marginatum Occurs in
-
7/30/2019 K.15 Acute Rheumatic Fever
10/31
Subcutaneous NodulesFound in 2% to 10% of patients,particularly in those withrecurrences.
Hard, painless, nonpruritic, freely movable, swelling,and 0.2 to 2 cm in diameter.
Symmetris, singly or in clusters, on the extensorsurfaces of both large and small joints, over thescalp, or along the spine.
Not transient, lasting for weeks, and have a significantassociation with carditis.
-
7/30/2019 K.15 Acute Rheumatic Fever
11/31
Sydenham's Chorea Sydenham's chorea (St. Vitus' dance)
is found in 15% of patients with ARF.
more often in prepubertal girls (8 to 12 years) than in boys.
neuropsychiatric disorder consisting of both neurologic signs
(choreic movement and hypotonia) and psychiatric signs (e.g.,emotional lability, hyperactivity, separation anxiety, obsessionsand compulsions).
begins with emotional lability and personality changes.
spontaneous, purposeless movement of chorea (which lasts 4 to
18 months), followed by motor weakness.
-
7/30/2019 K.15 Acute Rheumatic Fever
12/31
The distractability and inattentiveness outlast the choreicmovements.
The adventitious movements, weakness, and hypotonia continuefor an average of 7 months (up to 17 months) before slowly
waning in severity. Recently, elevated titers of antineuronal antibodies
recognizing basal ganglion tissues have been found in over 90%of patients. The levels of the antineuronal antibody titer arepositively related to the severity of choreic movements.
These findings suggest that chorea may be related todysfunction of basal ganglia and cortical neuronal components.
Sydenham's Chorea
-
7/30/2019 K.15 Acute Rheumatic Fever
13/31
MINOR MANIFESTATIONS
Arthralgia refers to joint pain without the objective changes ofarthritis. It must not be considered a minor manifestation whenarthritis is present.
Fever (usually with a temperature of at least 102F [38.8C]) is
present early in the course of untreated rheumatic fever.
In laboratory findings, elevated acute-phase reactants (elevatedC-reactive protein levels and elevated erythrocytesedimentation rate) are objective evidence of an inflammatoryprocess.
A prolonged PR interval on the ECG is neither specific for ARFnor an indication of active carditis.
-
7/30/2019 K.15 Acute Rheumatic Fever
14/31
EVIDENCE OF ANTECEDENT GROUP A STREPTOCOCCALINFECTION
A history of sore throat or of scarlet fever unsubstantiated by
laboratory data is not adequate evidence of recent group Astreptococcal infection.
Positive throat cultures or rapid streptococcal antigen tests forgroup A streptococci are less reliable than antibody testsbecause they do not distinguish between recent infection and
chronic pharyngeal carriage. Antigen detection tests are veryspecific but not very sensitive; a negative test result should beconfirmed by a conventional throat culture.
Streptococcal antibody tests are the most reliable laboratoryevidence of antecedent streptococcal infection capable ofproducing ARF. The onset of the clinical manifestations of ARFcoincides with the peak of the streptococcal antibody response.
-
7/30/2019 K.15 Acute Rheumatic Fever
15/31
Antistreptolysin O (ASO) titer is well standardized andtherefore is the most widely used test. It is elevated in 80%of patients with ARF and in 20% of normal individuals.
Only 67% of patients with isolated chorea have an elevatedASO titer. ASO titers of at least 333 Todd units in childrenand 250 Todd units in adults are considered elevated.
A single low ASO titer does not exclude ARF. If three otherantistreptococcal antibody tests (antideoxyribonuclease B,
antistreptokinase, and antihyaluronidase tests) are obtained,a titer for at least one antibody test is elevated in about95% of patients.
The antideoxyribonuclease B test is favored over othertests. Titers of 240 Todd units or greater in children and
120 Todd units or greater in adults are considered elevated.
The Streptozyme test (Wampole Laboratories) is a relativelysimple slide agglutination test, but it is less standardized andless reproducible than the other antibody tests.
-
7/30/2019 K.15 Acute Rheumatic Fever
16/31
OTHER CLINICAL FEATURES
Abdominal pain, rapid sleeping heart rate,tachycardia out of proportion to fever,
malaise, anemia, epistaxis, and precordial painare relatively common but not specific.
A positive family history of rheumatic fever
also may heighten the suspicion but cannot beused as a diagnostic manifestation.
-
7/30/2019 K.15 Acute Rheumatic Fever
17/31
Diagnosis
The revised Jones criteria are used for the diagnosis of ARF.
Only the major and minor criteria and evidence of an antecedentgroup A streptococcal infection are included in the criteria,although other findings play a supporting role.
A diagnosis of ARF is highly probable when either two majormanifestations or one major and two minor manifestations, plus
evidence of antecedent streptococcal infection, are present.
The absence of supporting evidence of a previous group Astreptococcal infection makes the diagnosis doubtful.
Exceptions to the Jones criteria include the following three
specific situations:
Chorea may occur as the only manifestation of rheumatic fever. Indolent carditis may be the only manifestation in patients who
come to medical attention months after the onset of rheumaticfever.
Occasionally, patients with rheumatic fever recurrences may notfulfill the Jones criteria.
-
7/30/2019 K.15 Acute Rheumatic Fever
18/31
Tips help in applying the Jones criteria:
Two major manifestations are always stronger than one major plus twominor manifestations.
Arthralgia or a prolonged PR interval cannot be used as a minormanifestation in the presence of arthritis or carditis, respectively.
The absence of evidence of an antecedent group A streptococcalinfection is a warning that ARF is unlikely (except when chorea ispresent).
The vibratory innocent (Still's) murmur is often misinterpreted as amurmur of MR and thereby is a frequent cause of misdiagnosis (oroverdiagnosis) of ARF. The murmur of MR is a regurgitant-type systolicmurmur (starting with the S1), but the innocent murmur is low pitchedand an ejection type. A cardiology consultation during the acute phaseminimizes the frequency of misdiagnosis.
The possibility of the early suppression of full clinical manifestationsshould be sought during the history taking. Subtherapeutic doses ofaspirin or salicylate-containing analgesics (e.g., Bufferin, Anacin) maysuppress full manifestations.
-
7/30/2019 K.15 Acute Rheumatic Fever
19/31
Differential Diagnosis
Juvenile rheumatoid arthritis (JRA) is often misdiagnosed as acuterheumatic fever. The following findings suggest JRA rather than ARF:involvement of peripheral small joints, symmetrical involvement of large
joints without migratory arthritis, pallor of the involved joints, a moreindolent course, no evidence of preceding streptococcal infection, andthe absence of prompt response to salicylate therapy within 24 to 48hours.
Other collagen vascular diseases (systemic lupus erythematosus, mixedconnective tissue disease); reactive arthritis, including
poststreptococcal arthritis; serum sickness; and infectious arthritis(such as gonococcal) occasionally require differentiation.
Virus-associated acute arthritis (rubella, parvovirus, hepatitis B virus,herpesvi ruses, enteroviruses) is much more common in adults.
Hematologic disorders, such as sicklemia and leukemia, should beconsidered in the differential diagnosis.
-
7/30/2019 K.15 Acute Rheumatic Fever
20/31
Clinical Course
Only carditis can cause permanent cardiac damage. Signs of mildcarditis disappear rapidly in weeks, but those of severe carditismay last for 2 to 6 months.
Arthritis subsides within a few days to several weeks, evenwithout treatment, and does not cause permanent damage.
Chorea gradually subsides in 6 to 7 months or longer and usuallydoes not cause permanent neurologic sequelae.
-
7/30/2019 K.15 Acute Rheumatic Fever
21/31
Management
When ARF is suggested by history and physical examination, oneshould obtain the following laboratory studies: complete bloodcount, acute-phase reactants (ESR and CRP), throat culture,ASO titer, chest x-ray films, and ECG.
Cardiology consultation is indicated to clarify whether there is
cardiac involvement; two-dimensional echo and Doppler studiesare usually performed at that time.
Benzathine penicillin G, 0.6 to 1.2 million IU/IM,is given to eradicate streptococci. This servesas the first dose of penicillin prophylaxis as well.
In patients allergic to penicillin, erythromycin,40 mg/kg per day in two to four doses for 10days, may be substituted for penicillin.
-
7/30/2019 K.15 Acute Rheumatic Fever
22/31
Anti-inflammatory or suppressive therapy withsalicylates or steroids must not be started until adefinite diagnosis is made. Early suppressive therapymay interfere with a definite diagnosis of ARF by
suppressing full development of joint manifestationsand suppressing acute-phase reactants.
When the diagnosis of ARF is confirmed, one musteducate the patient and parents about the need to
prevent subsequent streptococcal infection throughcontinuous antibiotic prophylaxis. In patients withcardiac involvement, the need for prophylaxis againstinfective endocarditis also should be emphasized.
-
7/30/2019 K.15 Acute Rheumatic Fever
23/31
Bed rest of varying duration is recommended. The duration depends on the type and severity of the
manifestations and may range from a week (for isolated
arthritis) to several weeks for severe carditis. Bed rest is followed by a period of indoor ambulation of varyingduration before the child is allowed to return to school.
-
7/30/2019 K.15 Acute Rheumatic Fever
24/31
The erythrocyte sedimentation rate is a helpful guide to therheumatic activity and therefore to the duration of restriction
of activities. Full activity is allowed when the erythrocytesedimentation rate has returned to normal, except in childrenwith significant cardiac involvement.
-
7/30/2019 K.15 Acute Rheumatic Fever
25/31
Therapy with anti-inflammatory agents should be started assoon as ARF has been diagnosed.
Prednisone (2 mg/kg per day in four divided doses for 2 to 6weeks) is indicated only in cases of severe carditis.
For mild to moderate carditis, aspirin alone is recommended in a
dose of 90 to 100 mg/kg per day in four to six divided doses. An
adequate blood level of salicylates is 20 to 25 mg/100 mL. Thisdose is continued for 4 to 8 weeks, depending on the clinicalresponse. After improvement, the therapy is with drawngradually over 4 to 6 weeks while monitoring acute-phasereactants.
For arthritis, aspirin therapy is continued for 2 weeks andgradually withdrawn over the following 2 to 3 weeks. Rapidresolution of joint symptoms with aspirin within 24 to 36 hoursis supportive evidence of the arthritis of ARF.
-
7/30/2019 K.15 Acute Rheumatic Fever
26/31
Treatment of CHF includes some or all of the following: Complete bed rest with orthopneic position and moist, cool
oxygen. Morphine sulfate, 0.2 mg/kg, at 4-hour intervals for severe CHF
with respiratory distress. Restriction of sodium and fluid intake. Prednisone for severe carditis of recent onset. Digoxin (used with caution, because certain patients with
rheumatic carditis are supersensitive to digitalis), beginning withhalf the usual recommended dose.
Furosemide, 1 mg/kg every 6 to 12 hours, if indicated.
-
7/30/2019 K.15 Acute Rheumatic Fever
27/31
Management of Sydenham's chorea:
Reduce physical and emotional stress and use protective measures asindicated.
Give benzathine penicillin G, 1.2 million units, initially for eradicationof streptococcus and also every 28 days for prevention ofrecurrence, just as in patients with other rheumatic manifestations.Without the prophylaxis, about 25% of patients with isolated chorea(without carditis) develop rheumatic valvular heart disease in 20-year follow-up.
Anti-inflammatory agents are not needed in patients with isolated
chorea.
For severe cases, any of the following drugs may be used:phenobarbital (15 to 30 mg every 6 to 8 hours), haloperidol(starting at 0.5 mg and increasing every 8 hours to 2 g), valproicacid, chlorpromazine (Thorazine), diazepam (Valium), or steroids.
Plasma exchange (to remove antineuronal antibodies) and IV immuneglobulin therapy (to inactivate the effects of the antineuronalantibodies) are in the experimental stages (by the NationalInstitutes of Health), but the preliminary results are promising inreducing the duration of chorea.
-
7/30/2019 K.15 Acute Rheumatic Fever
28/31
Prognosis
The presence or absence of permanent cardiac damage determinesthe prognosis. The development of residual heart disease is
influenced by the following three factors:
Cardiac status at the start of treatment: The more severe thecardiac involvement at the time the patient is first seen, thegreater the incidence of residual heart disease.
Recurrence of rheumatic fever: The severity of valvularinvolvement increases with each recurrence.
Regression of heart disease: Evidence of cardiac involvement atthe first attack may disappear in 10% to 25% of patients 10
years after the initial attack. Valvular disease resolves more
frequently when prophylaxis is followed.
-
7/30/2019 K.15 Acute Rheumatic Fever
29/31
Prevention
POPULATION
Patients with documented histories of rheumatic fever, includingthose with isolated chorea and those without evidence ofrheumatic heart disease, must receive prophylaxis.
DURATION
Ideally, patients should receive prophylaxis indefinitely. Many cardiologists recommend discontinuing the prophylaxis atage 21 to 25 years, provided the patient does not have evidenceof valvular involvement and is not in a high-risk occupation (e.g.,schoolteachers, physicians, nurses).
If the patient has rheumatic valvular disease, the prophylaxisshould be continued longer, possibly for life. The chance ofrecurrence is highest in the first 5 years after the ARF.
-
7/30/2019 K.15 Acute Rheumatic Fever
30/31
METHODS
The method of choice for secondary prevention is benzathinepenicillin G, 1.2 million units given intramuscularly every 28 days
(not once a month). Alternative methods, although not aseffective, are the following:
Oral penicillin V, 250 mg, twice daily. Oral sulfadiazine, 1 g once daily (note that the sulfonamides are
not effective for the prophylaxis of infective endocarditis).
Oral erythromycin ethyl succinate, 250 mg, twice daily.
PRIMARY PREVENTION
Primary prevention of rheumatic fever is possible with a 10-day
course of penicillin therapy for streptococcal pharyngitis. Primary prevention is not possible in patients who developsubclinical pharyngitis and therefore do not seek medicaltreatment (30%) and in patients who develop ARF withoutsymptoms of strepto coccal pharyngitis (30%).
-
7/30/2019 K.15 Acute Rheumatic Fever
31/31
THANK YOU