Journal Scabies
-
Upload
alfian-hari-gunawan -
Category
Documents
-
view
216 -
download
0
description
Transcript of Journal Scabies
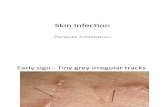
Tropical medicineroundsScabiescommunityprevalenceandmassdrugadministrationintwoFijianvillagesKarinHaar1,*, MD,MMED,MPH,LuciaRomani2, MSD,RaikanikodaFilimone3, MBBS,DipDerm,MMED,KamalKishore4, MBBS,MD,DPH,MeciuselaTuicakau3, MBBS,DDM,JosefaKoroivueta3, DSM,FACTM,JohnM.Kaldor2, PhD,HandanWand2, PhD,AndrewSteer5, MBBS,PhD,andMargotWhitfeld6, FACD1UniversityofSydney,NewSouthWales,Australia,2KirbyInstitute,UniversityofNewSouthWales,NewSouthWales,Australia,3MinistryofHealth,Suva,Fiji,4Fiji NationalUniversity,Suva,Fiji,5UniversityofMelbourne,Victoria,Australia,and6DepartmentofDermatology,St.VincentsHospital Sydney,NewSouthWales,AustraliaCorrespondenceDr.MargotWhitfeld, FACDDepartmentofDermatologySt.VincentsHospital SydneySuite4Level 466PacicHwyStLeonardsNSW2065AustraliaE-mail:[email protected]*Presentaddress:RobertKoch-Institute,Dept.forInfectiousDiseaseEpidemiology,HIV/AIDS,STIandBloodborneInfectionsUnit,DGZ-Ring1,Berlin,Germany.Conictsofinterest:None.doi:10.1111/ijd.12353AbstractBackground Scabies has been estimated to affect approximately 300 million peopleworldwideeachyear.ScabiesratesarehighandposeasignicantpublichealthprobleminFiji.Community-basedcomparisontreatmenttrialshavenotbeenundertaken.Weestimatedscabiesprevalenceandcomparedtheefcacyandtolerabilityofmassdrugadministration(MDA)ofbenzylbenzoatelotion(BB)ororal ivermectin(IVM)intwovillagesinFiji.MethodsAprospectiveMDAtrial wasundertakenintwoFijianvillages, comparingthreedailyapplicationsofBBwithsingledoseIVMorpermethrincreamforthoseagedundertwoyears.Thetherapieswereofferedtoall communitymembersregardlessofthepresenceofscabiesoritssymptoms.Thedifferenceinprevalencewasmeasuredbeforeandaftertheinterventionandabsoluteriskreduction(ARR)andrelativerisk(RR)calculated.ResultsIntheBBgroup,therewere572eligibleparticipants,ofwhom435(76%)enrolledand201(46%)returnedforfollow-up.IntheIVMgroup,therewere667eligibleparticipants,ofwhom325(49%)enrolledand126(39%)returned.Scabiesprevalencewasloweraftertheinterventioninbothgroups.Itfell from37.9to20.0%(ARR18.0%;RR0.52)intheBBgroupandfrom23.7to9.5%(ARR14.2%;RR0.40)intheIVMgroup.Conclusions Our study provides proof of principle that MDA for scabies can reducescabiesprevalenceatthecommunitylevel,andthattherewasnosignicantdifferenceinthistrial betweenBBandoral IVM.IntroductionScabies, due to infestation with theSarcoptesscabiei mite,has beenestimatedtoaffect approximately 300millionpeopleworldwideeachyear. Itsdirect impact isitching,but secondary bacterial infection with Streptococci andStaphylococci is frequent and can lead to serious andpotentiallyfatal complications, includinginvasive bacte-rial infections, renal failure, andchronicrheumaticheartdisease.14.Thehighest ratesof scabiesintheworldarefoundinPacicislandcountries.5Inapopulation-basedsurveyinFiji, 24%ofparticipantshadscabies, withaparticularlyhighprevalenceinyoungchildren(L. Romani, personalcommunication).AprospectivestudyinFijianschoolchil-drendocumentedscabies incidence at 51cases per 100person-years.6Scabiestreatmentisprimarilywithapplicationoftopi-cal agents, including benzyl benzoate and permethrincream, whichwasintroducedtoFiji in2006andisnowthe standard of care.7AsS.scabiei is transmitted by closebodycontact or sharedobjects, treatment of close con-tacts is also recommended. One oral agent, ivermectin(IVM), has beenusedas single dose scabies treatment,repeated at twoweeks if symptoms persist.810Thefrequencyof reinfestationinendemicsettings hasledtoconsiderationof massdrugadministration(MDA)as a public health option for scabies control. Small,2013TheAuthors.International Journal ofDermatologypublishedbyJohnWiley&SonsLtdonbehalfofTheInternational SocietyofDermatology.ThisisanopenaccessarticleunderthetermsoftheCreativeCommonsAttribution-NonCommercial License,whichpermitsuse,distributionandreproductioninanymedium,providedtheoriginal workisproperlycitedandisnotusedforcommercial purposes.1uncontrolled studies in closed communities such as prisonsandagedcarefacilitieshavesuggestedthat treatment ofentirecommunities cansharplyreducetheprevalenceofinfestation,8,1113using either topical treatment or oralIVM, the latter perhaps offering better adherence andfewersideeffects.14Toassessthepotential roleofMDAinanopencommunitysettinginthegeneral population,we studied oral vs. topical MDA in two Fijian villages.MaterialsandmethodsWeperformedaprospectivetrial comparingtheefcacyandtolerabilityoftwoMDAtreatmentregimensforthecontrol ofscabiesbyofferingtreatmenttoall communitymembersregardlessofthepresenceofscabiesoritssymptoms.Hence,all familymembersofstudyparticipants,includingasymptomaticfamilymembersofpatientswithscabieslivingineithervillage,wereofferedtreatmentimmediatelyafterexaminationandincludedinthestudy.WeconductedthestudyintwoFijiansubdivisions(localadministrativeareas) inJuneandJuly2004. ThesiteswereselectedbytheFiji Ministryof Healthashavingapproximatelythesamenumber of inhabitantsandbeingwithina2-hour driveof thecapital, Suva, but relativelyisolatedfromeachother andfromother communities.Allocationtotreatment wasdecidedbyadministrativechancebasedontheavailabilityof medicationat start point. IntheTailevusubdivision, threecloselylinkedsettlements(Sawakasa, Dakuinuku, andLodoni, total population572)wereclassiedasonesite. IntheRewasubdivision,Raralevuvillagewasselected(total population667). All Fijiannationalslivingineither of thetwositeswereconsideredeligiblefor thestudyandwereenrolledafter signingtheconsent forms, withparentssigningfor their children. Studyparticipantswereregisteredbyname, age, andsexandwereweighedat initial visit. After enrollment, participantswereidentiedonlybytheir numericcodeandnofurther identifyingdatawereusedinthestudy.Participantswereaskedtocompletequestionnairesatenrollmentandfollow-upvisit,ineitherEnglishorFijian,andassistedbythelocal communitynurseifnecessary.Eachparticipantwasexaminedbyahealthcareprofessional withexperienceinscabiesdiagnosisandtreatmentandreviewedbyaseniordoctorifanyskinlesionswereseen.Thediagnosisofscabieswasmadeclinically,basedonthepresenceofcharacteristiclesionswithorwithoutahistoryofitch.Suspectedscabieslesions,eitherpapules,pustules,orcrustedlesionsonthetrunkandlimbs,werecountedandotherdermatologicalconditions,suchasboilsandsores,eczema,andtineaweredocumentedbeforeandaftertreatment.Ifappropriate,oralantibioticsweregivenforsecondarilyinfectedlesionsandtherapyprovidedforotherskinconditions.Theextentofscabieswasquantiedasmild(10lesionsorfewer),moderate(1149),severe(50ormore),orcrusted(conuentlesions,toomanytocount).1517Thediagnosisofinfectedlesionswasmadebasedonthepresenceoferythema,crusting,orpustules.InterventionsAll MDAstudyparticipantsintheRewasubdivisionsite(IVMgroup)aged2yearsandoverwithnomedical contraindicationsreceivedasingledoseoforal IVMat200lg/kgbodyweight(Stromectol3mgtablets;MerckSharp&Dohme,SouthGranville,NSW,Australia),roundedtowhole3mgIVMtablets.IVMwastakenorallyunderdirectobservation,immediatelyafterexamination.Childrenaged