PREPARATION AND CHARACTERIZATION OF POLY (Ɛ-CAPROLACTONE) NANOSUSPENSION CONTAINING SATRANIDAZOLE
Journal Home Page BRITISH … · Preparation of Ezogabine nanosuspension ... Characterization of...
Transcript of Journal Home Page BRITISH … · Preparation of Ezogabine nanosuspension ... Characterization of...
Journal Home Page www.bbbulletin.org
BRITISH BIOMEDICAL BULLETIN
Original Article
Study the Effect of Surfactant Concentration and Ultrasonication Time on Aqueous Solubility, Particle Size
and In-vitro Drug Diffusion of Ezogabine Nanosuspension by 32 Factorial Designs
Pawar Anil R.*1,3, Choudhari Pravin D.4, Ghule Prashant J2, Pawar Amol R.1 and Bankar Prakash V.1
1Quality Assurance Department, MES`s College of Pharmacy, Affiliated To Savitribai Phule Pune University, Sonai, Taluka-Newasa, District-Ahmednagar, Maharashtra, India-414105 2Mula Rural Institute of Pharmacy, Sonai, Taluka -Newasa, Dist-Ahmednagar, Maharashtra, India-414105 3Research Scholar, PRIST University, Thanjavur, Tamilnadu 4Modern college of Pharmacy, Nigdi, Pune
A R T I C L E I N F O Received 09 Feb. 2016 Received in revised form 05 March 2016 Accepted 15 March 2016 Keywords: Nanosuspension, Ezogabine, Intranasal, Factorial design, Nanoprecipitation. Corresponding author: Quality Assurance Department, MES`s College of Pharmacy, Affiliated To Savitribai Phule Pune University, Sonai, Taluka-Newasa, District-Ahmednagar, Maharashtra, India-414105
E-mail address: [email protected]
A B S T R A C T
Objectives: The objective of the existing study was to prepare ezogabine nanosuspension for intranasal administration and study the effect of surfactant concentration (0.1, 0.2, 0.3 ml), ultrasonication time (10, 20, 30 min) on aqueous solubility, particle size and in-vitro drug diffusion of drug. Methods: All the nanosuspensions of ezogabine were prepared using the nanoprecipitation–ultrasonication technique at different surfactant conc. and ultrasonication time. There have been still few of published researches on formulation of ezogabine using co-crystal, solid dispersion. The formulation was studied using design of experiments by employing a 2-factor, 3-level factorial design. The nanosuspensions were studied for saturation solubility, particle size, in-vitro drug diffusion, pH, drug content, viscosity, FT-IR study and nasal cilio toxicity studies. Results: The average saturation solubility, particle size and in-vitro drug diffusion of nanosuspensions was found in the range of 0.2931-0.8121mg/ml, 155.2-454.4nm and 88.14-97.91% at 2.5hrs.respectively.The pH, drug content and viscosity of nanosuspensions was found in the range of 5.48-6.16, 96.43-99.12%, 110.7138.5 cps respectively. The statistical analysis of data revealed that surfactant conc.(X1) and ultrasonication time (X2) has a significant effect on saturation solubility (p=0.0001), whereas a surfactant conc. (X1) has no effect and ultrasonication time has significant effect on particle size (p=0.0042). The surfactant conc. (X1) has no significant effect and ultrasonication time has significant effect on in-vitro drug diffusion (p=0.0020).FT-IR study revealed that there was no significant change in principle peak of the drug in physical mixture (Ezogabine, Tween 80 and Poloxamer 188).Nasal Cilio toxicity study showed no nasociliary damage, indicates safety of formulation. Conclusion: This examination verified the prospective of the
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
experimental design in understanding the effect of formulation variables on the development of nanosuspensions. The results reassures, nanosuspension are encouraging for solubility
enhancement.
Introduction
The formulation of poorly water-soluble drugs has always been a challenging problem faced by pharmaceutical scientists and it is expected to increase because approximately 40% or more of the new chemical entities being generated through drug discovery programmers are poorly water-soluble1.
A pharmaceutical nanosuspension is defined as very finely colloid2, biphasic3, dispersed solid drug particles in an aqueous vehicle; size below 1 μm stabilized by surfactants4 and polymers5 prepared by suitable methods for drug delivery6 applications. Nanosuspensions have revealed their potential to solve the problem7 associated with the delivery of poorly water and lipid soluble drugs. Drug particle size reduction leads to an increase in the surface area and consequently the rate of dissolution as described by the Noyes-Whitney8. In addition an increase in saturation solubility is postulated by the particle size reduction due to an increased dissolution pressure explained by the ostwald-freundlich9. The nanoprecipitation technique for nanoparticle manufacture was first developed and patented by Fessi and coworkers10. This technique presents numerous advantages, in that it is a straight forward technique, rapid and easy to perform11. Different hydrophobic drugs have already been formulated successfully in this way, for instance naproxen, clofazamine nimesulid, amphotericin B, omeprazole, nifedipine and spironolactone12 1donepezil, nitrendipine, acetazolamide.
Ezogabine is an anticonvulsant used for thetreatment of partial epilepsies.
Ezogabine acts as a neuronal KCNQ/Kv7 potassium channel opener13. Intranasal delivery is considered as a viable and attractive route of administration for various therapeutic agents14. The intranasal route is preferred over oral because oral administration of ezogabine shows adverse effects such as gastrointestinal disorders (nausea, constipation, dyspepsia and dry mouth), metabolism and urinary disorders (dysuria, urinary hesitation, haematuria, chromaturia, urinary retention and nephrolithiasis)15. A 32 factorial design is a well-established model tostudy the effect of selected formulation variables on the characters of the drug products16.
Materials and Methods
Materials Ezogabine [Ethyl-N-(2-amino-4-
{[(4-fluorophenyl) methyl] amino} phenyl) carbamate] was received as a gift sample from Lupin Pharma, Aurangabad, Maharashtra, India. Tween 80, Poloxamer 188 and methanol were purchased from Loba ChemPvt. Ltd, Mumbai.All other chemicals were of analytical grade or highest grade commercially available.
Preparation of Ezogabine nanosuspension
Ezogabine nanosuspension was prepared by the nanoprecipitation–ultrasonication17-19 method with different conc. of surfactant (0.1, 0.2 and 0.3 ml). The Surfactant (Tween 80) and Poloxamer 188 (20mg) were dissolved in distilled water (10 ml), mixed and labeled as mixture 1. This mixture was kept on magnetic stirrer for 15 min. to get homogeneous mixture.
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
Ezogabine (10 mg) was dissolved using defined volume of methanol (2ml). This solution was slowly added drop wise to mixture 1 with continuous stirring on magnetic stirrer for 1 hr. After 15 minutes, the solutions were kept in ultrasonicator (Citizen Digital Ultrasonic Cleaner, CD-4820) for the specified time (10, 20 and 30 min). Thus, the nanosuspension was formed and preserved for further use.
We can administer the prepared nanosuspension by intranasal route, so that drug reaches into the brain directly via nose to brain pathway. The amount of the drug reaches to the brain can be assess with the help of HPLC. The another methods to evaluate the effect of formulation on in-vivo administration are as follows, a. Determination of anticonvulsant
property either by using chemical or electrical method.
b. Determination of Locomotor activity by using actophotometer.
c. Determination anxiolytic response by using Elevated plus maze apparatus.
32 Full Factorial Designs
A 32 full factorial design was applied to examine the combined effect of two formulation variables [Surfactant conc.(X1) and ultrasonication time(X2)] on saturation solubility (Y1), particle size (Y2) and in-vitro drug diffusion (Y3)
20. Total nine combinations of Ezogabine nanosuspension were prepared according to the design given in Table 1 21. The levels of parameters used are given in Table 2. The graphs and mathematical models were computed using Design Expert 9.0.6.2 (Stat- Ease, USA) software.
Characterization of Nanosuspension
Saturation solubility studies Nanosuspension equivalent to 10 mg
of ezogabine were taken and separately introduced into 25 ml stoppered conical
flask containing 10 ml distilled water. The flasks were sealed and placed in rotary shaker for 24 hrs. at 37°C and equilibrated for 2 days. The samples were collected after the specified time interval and it was filtered and diluted with distilled water appropriately. The diluted samples were analyzed using UV spectrophotometer (Shimadzu- 1800, Japan) at 218.2 nm23. Particle size analysis
Average particle size of formulations was determined by Beckman coulter particle size analyzer (Delsa™ Nano Common) using water as dispersion medium. Nanosuspensions were dispersed in double distilled water before running sample in the instrument, to ensure that the light scattering signal, as indicated by particles count per second, was within instrument’s sensitivity range 24.
In-vitro drug diffusion study
The freshly excised goat nasal mucosa except the septum part was collected from the slaughter house in phosphate buffer (PB), pH 6.4. The membrane was kept in PB (pH 6.4) for 15 min to equilibrate. The superior nasal conche was identified and separated from the nasal membrane; the excisedsuperior nasal membrane was mounted on Franz diffusion cell. The tissue was stabilized using PB (pH 6.4) in both the compartments and allowed to stir for 15 min. on amagnetic stirrer. After 15 min, solution from both the compartments was removed and fresh PB (pH 6.4) was filled in the acceptor compartment. The mounting of the nasal membrane was done using glue at the brim of the donor to avoid leakage of the test sample and supported with thread crossing over the cell. Franz diffusion cell used for in-vitro diffusion studies had a diameter of 4.2 cm. The temperature of the receiver chamber containing 30 ml of diffusion media (PB, pH 6.4) was controlled
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
at 37°C ±1 under continuous stirring with teflon-coated magnetic bar at a constant rate, in a way that the nasal membrane surface just flushes the diffusion fluid. A volume of 1 ml of each selected formulation was placed in the donor compartment of Franz diffusion cell. Samples from the receptor compartment were withdrawn at predetermined time intervals and analyzed. Each sample removed was replaced by an equal volume of diffusion media. Each study was carried for a period of 2.5 hrs. during which the drug in receiver chamber (mg/ml) across the goat nasal membrane was calculated at each sampling point 25.
pH
The pH is an important property of nasal formulation and should be maintain between 4.5- 6.5 to avoid irritation on application. The pH of all formulations was measured by calibrated digital pH meter (Equip-Tronics EQ-636)26. Viscosity
The viscosity of all formulations was measured by Brookfield viscometer (Brookfield LVDV-I Prime) using spindle-61 at 25°C27.
Drug Content
About 1 ml of nanosuspension preparation was taken and diluted appropriately with distilled water and the drug content of the samples were estimated by UV-Visible spectrophotometer (Schimadzu-1800, Japan) at 218.2 nm 28.
Drug-Excipients Compatibility Studies
The FT-IR spectra of Ezogabine pure drug, excipients, physical mixture of drug and excipients were recorded using KBr disk method by FT-IR Spectrophotometer (Shimadzu 8300 and Hyper IR software from Shimadzu, Japan)29.
Nasal Cilio Toxicity Study Freshly excised goat nasal mucosa,
except for the septum, was collected from the slaughter house in phosphate buffer (pH 6.4). Three goat nasal mucosa pieces (P1, P2 and P3) with uniform thickness were selected and mounted on Franz diffusion cells. P1 was treated with 0.5 ml of PB (pH 6.4, negative control), P2 with 0.5 ml of isopropyl alcohol (positive control) and P3 was treated with Ezogabine nanosuspension for 1 hr. After 1 hr, the mucosa were rinsed with PB (pH 6.4) and subjected to histological studies by using eosin- hematoxylin stain to evaluate the toxicities of nanosuspension formulation and photographed by using digital microscopy (Motic BA210, china)30.
Result and Discussion
The responses observed for all the formulations such as saturation solubility (Y
1), particle size (Y
2) and in-vitro drug
diffusion (Y3) with variables surfactant
conc. (X1) and ultrasonication time (X
2) are
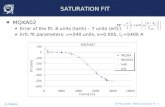
given in table 3. Saturation solubility
The saturation solubility of all formulations was found to be in the range of 0.2921 to 0.8121 mg/ml. The linear model was suggested for saturation solubility. ANOVA analysis of the data is given in Table 5. The Statistical analysis of data revealed that surfactant conc. (X1) and ultrasonication time (X2) has significant effect on saturation solubility. Related contour plots & 3 D surface plot are shown in Fig. 1 (a, b).
Particle size
The average particle size of all the formulations was of nano size, ranging from 155.2 to 454.4 nm. The linear model was suggested for particle size distribution as
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
given in Table 4. ANOVA analysis of the data is given in Table 5. The Statistical analysis of data revealed that surfactant conc. (X1) has no significant effect on particle size where as ultrasonication time (X2) has significant effect on particle size. Related contour plots &3 D surface plot are shown in Fig. 2 (a, b).
In-vitro drug diffusion
The in-vitro drug diffusion for all the formulation was found to be in the range of 88.14% to 97.91%at 2.5 hrs. The linear model was suggested for in-vitro drug diffusion. ANOVA analysis of the data is given in Table 5. The Statistical analysis of data revealed that surfactant conc. (X1) has no significant effect on in-vitro drug diffusion, whereas ultrasonication time (X2) has significant effect on in-vitro drug diffusion. Related contour plots & 3 D surface plot are shown in Fig. 3 (a, b).
The equation in terms of coded factors can be used to make predictions about the response for given levels of each factor. By default, the high levels of the factors are coded as +1 and the low levels of the factors are coded as -1. The coded equation is useful for identifying the relative impact of the factors by comparing the factor coefficients (Table 6).
pH
The pH of all formulations was found to be in the range of 5.48-6.16.
Viscosity
The viscosity of all formulations was found to be in the range of 110.7-138.5 cps.
Drug Content
The drug content of all formulations was found to be96.43-99.12% by calibration
curve methods
Drug-excipients compatibility studies The peaks analyzed (Table 7) and IR
spectra shown in fig.4 indicate that there was no physical and/or chemical interaction in between drug and studied excipients. The frequencies of functional groups of drug ezogabine remained intact in physical mixture containing different excipients. So it was concluded that there was no major interaction occurred. Nasal Cilio Toxicity
The nasal mucosa treated with phosphate buffer pH 6.4 (negative control) showed no nasociliary damage and the nasal membrane remained intact. The nasal mucosa treated with isopropyl alcohol (positive control) showed an extensive damage to nasal mucosa coupled with loss of nasal cilia. However, with selected nanosuspension (AP8), no damage to nasal mucosa could be observed as shown in fig.5 which showed the safety of the excipients used in the formulations.
Conclusion
The Ezogabine nanosuspension was attempted by nanoprecipitation with ultrasonication techniques to improve aqueous solubility of drug. Factorial Design can be used for a systematic approach for designing and optimizing the desired formulation based on different process. Surfactant conc. had a significant effect on saturation solubility and no significant effect on particle size and in-vitro drug diffusion. Ultrasonication time had significant effect on saturation solubility, particle size and in-vitro drug diffusion. The selected formulation (AP8) showed better results, so it was used for further investigation. Finally the experimental results had shown promising observations in terms of pH, drug content and viscosity. No major drug polymer interaction was detected by FT-IR analysis. Nasal Cilio toxicity study showed
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
that the nanosuspension was safe for intranasal administration. The selected formulation (AP8) showed 26 fold increased in aqueous solubility of ezogabine. So, we concluded that nanosuspension with specified ultrasonication time represents a promising alternative to current drug delivery systems aiming to improve the aqueous solubility of drugs with low solubility.
Acknowledgement
The authors express their gratitude to management and Principal of MES’s College of Pharmacy, Sonai, for their support and encouragement. The authors also thanks to Lupin pharma, Aurangabad, for giving gift sample of Ezogabine.
Conflict of Interest
Nil References
1. K. S. Wagh, S. K. Patil, A.K. Akarte, D. T. Baviskar, International Journal of Pharmaceutical Sciences Review and Research,8(2): 61- 65(2011).
2. T. Lenhardt,G. Vergnault, P. Grenier, D. Scherer, P. Langguth,The AAPS journal,10 (3): 435-438(2008).
3. N. Arunkumar, M. Deecarman, C. Rani, Asian Journal of Pharmaceutics, 3:168-173(2009).
4. Xiaohui Pu, Jin Sun, Mol Li, Zhonggui He, current nanoscience. Bentham science publisher’s ltd, 5: 417-427(2009).
5. G.G.Liversidge, K.C.Cundy, Int. J. Pharm., 125(1):91-97(1995).
6. R. L. Shid, S. N.Dhole, N. Kulkarni, S. L.Shid,Int. J. Pharm. Sci. Rev. Res.22(1): 98-106(2013).
7. K.C.Senthil, B.N. VedhaHari, S. P. Sharavanan, Journal of Pharmacy Research, 3(10): 2404-2407(2010).
8. R.H. Muller, C. Jacobs, O. Kayser, Adv. Drug Deliv. Rev, 47(1): 3-19(2001).
9. K. P. Kreuter, Advanced Drug Delivery Reviews7: 71-86(1991).
10. H. Fessi, F. Puissieux, J. P. Devissaguet, C. Thies, US Patent US5118528, 2(1988).
11. D. Quintanar-Guerrero, E. All´emann, H. Fessi, E. Doelker, Drug Dev. Ind. Pharm, 24:1113–1128(1998).
12. P. Kocbek, S. Baumgartner, J. Kristl, International Journal of Pharmaceutics, 312:179–186(2006).
13. Pvv. Satyanarayana, A. S. Madhavi, International Journal of Research in Pharmacy and Chemistry, 2(4): 1093- 1098(2012).
14. Bhavna, Md Shadab, M. Ali, R. Ali, International Journal of Biological Macromolecules ,67: 418–425(2014).
15. Summary of Product Characteristics, http://www.ema.europa.eu/.
16. M.Mothilal, M. C. Krishna, S.P.Surya, V. Manimaran, N.Damodharan, International Journal of Pharmacy and Pharmaceutical Sciences, 7(6):449-455(2014).
17. J. Sandhya, A. Pavani, R. R. Reddy,International Journal of Pharmaceutical Sciences Review and Research, 24(1): 177-181(2014).
18. B. P. Sahu, M. K. Das, International Journal of PharmTech Research, 5(2); 553-561 (2013).
19. P. Verma, R N Gupta, A. K. Jha, British Biomedical Bulletin, 2(2): 329-342 (2014).
20. H. P. Thakkar, B. V. Patel, S. P. Thakkar, J Pharm Bioallied Sci., 3(3): 426–434(2011).
21. D. J. Patel, J. K.Patel, V. M. Pandya, R. R. Jivani, R. D. Patel, International Journal of PharmTech Research, 2(1): 155-161 (2010).
22. A. Memon, P. U. Patel, H. M. Sheth, D. J. Patel, International Journal of Pharmaceutical Frontier Research, 3(1): 42-53 (2013).
23. N. Nagajyothi, M. Dhanalakshmi, S. Thenmozhi, R. Natarajan, N.N. Rajendran, International Journal of Pharmacy & Life Sciences,5(2):3318-3324(2014).
24. V. Agarwal, M. Bajpai, Tropical Journal of Pharmaceutical Research, 13 (4): 497-503(2014).
25. R. B. Patel, M. R. Patel, K. K. Bhatt, B. G. Patel, Bulletin of Faculty of Pharmacy, Cairo University, 51: 243–253(2013).
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
26. A. Kapil, G. Aggarwal, S.L. Hari Kumar, Asian Journal of Biochemical and Pharmaceutical Research, 1 (5): 101-116(2015).
27. R. K. Kotecha, S. Bhadra, K. Rajesh, International Journal of Pharmacy and Pharmaceutical Sciences, 5(4):490-497(2013).
28. R. N. Patel, Umashankar M. S.,M. C. Mamatha, Am. J Pharm Tech Res., 2(3): 1062-1080(2012).
29. U. K. Sharma , A. Verma , S. K. Prajapati , H. Pandey , A. C. Pandey, Appl Nanosci,5:143–155(2015).
30. P. Maurya, A. Mittal, K. Sharma, S. Alam, ANALELE Universitatii Dunarea,1: 93-105(2013).
31. G. Bhatt, A. Raturi, P. Kothiyal, American Journal of Advanced Drug Delivery, 1(3): 197-211 (2013).
32. S. D. Paul, R. Mazumder, S. Bhattacharya, A. K. Jha, British Biomedical Bulletin, 1(2): 119-125 (2013).
33. N. Nagajyothi, M. Dhanalakshmi, S. Thenmozhi, R. Natarajan, N.N. Rajendran,
International Journal of Pharmacy & Life Sciences,5(2):3318-3324(2014).
34. V. Agarwal, M. Bajpai, Tropical Journal of Pharmaceutical Research, 13 (4): 497-503(2014).
35. R. B. Patel, M. R. Patel, K. K. Bhatt, B. G. Patel, Bulletin of Faculty of Pharmacy, Cairo University, 51: 243–253(2013).
36. A. Kapil, G. Aggarwal, S.L. Hari Kumar, Asian Journal of Biochemical and Pharmaceutical Research, 1 (5): 101-116(2015).
37. R. K. Kotecha, S. Bhadra, K. Rajesh, International Journal of Pharmacy and Pharmaceutical Sciences, 5(4):490-497(2013).
38. R. N. Patel, Umashankar M. S.,M. C. Mamatha, Am. J Pharm Tech Res., 2(3): 1062-1080(2012).
39. U. K. Sharma , A.Verma , S. K. Prajapati , H. Pandey , A. C. Pandey, Appl Nanosci,5:143–155(2015).
40. P. Maurya, A. Mittal, K. Sharma, S. Alam, ANALELE Universitatii Dunarea,1: 93-105(2013).
Table 1. Formulation of batches in 32 factorial designs (coded values)
Trail no. Variable Levels in Coded form
X1 X2
1 -1 -1
2 0 -1
3 +1 -1
4 -1 0
5 0 0
6 +1 0
7 -1 +1
8 0 +1
9 +1 +1
.
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
Table 2. Actual values of independent variables in 32 factorial designs22
Coded level -1 0 +1
X1: Surfactant conc.(ml)
0.1 0.2 0.3
X2: Ultrasonication Time (min.) 10 20 30
Table 3. Formulations with their responses
Formulation Code
Variables Responses
X1 X2 Y1 Y2 Y3
Ap1 0.1 10 0.2931 424.2 88.14
AP2 0.2 10 0.3780 399.6 88.18
AP3 0.3 10 0.4621 454.4 90.09
AP4 0.1 20 0.5075 358.2 91.15
AP5 0.2 20 0.5530 238.0 92.62
AP6 0.3 20 0.6439 221.2 92.55
AP7 0.1 30 0.6431 168.2 93.79
AP8 0.2 30 0.8121 155.2 97.91
AP9 0.3 30 0.7484 225.2 94.74
Table 4. Summary of results of regression analysis of saturation solubility, particle size and in-vitro drug diffusion
Source Std. Dev. R Squared Adjusted
R Squared Predicted R Squared
PRESS Suggested
Model
Saturation Solubility (Y1)
Linear 0.042 0.9535 0.9380 0.8836 0.027 Suggested
2FI 0.044 0.9580 0.9328 0.7781 0.051
Quadratic 0.050 0.9679 0.9145 0.6698 0.076
Cubic 0.054 0.9872 08979 -1.3264 0.54 Aliased
Particle Size (Y2)
Linear 53.35 0.8392 0.7856 0.6342 38848.47 Suggested
2FI 58.14 0.8409 0.7454 0.2200 82848.12
Quadratic 60.35 0.8971 0.7256 -0.2519 1.33E +005
Cubic 7.40 0.9995 0.9959 0.9060 9980.01 Aliased
In-vitro Drug Diffusion (Y3)
Linear 1.30 0.8739 0.8319 0.7048 23.62 Suggested
2FI 1.40 0.8771 0.8033 0.4251 46.01
Quadratic 1.54 0.9107 0.7619 -00793 86.38
Cubic 0.39 0.9981 0.9848 0.6537 27.72 Aliased
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
Table 5. ANOVA Table
Source Sum of Squares
df Mean
Square F Value
p- value Prob.>F
Y1 Saturation Solubility[R2= 0.9535]
Model [Linear]
0.22 2 0.11 61.49 0.0001 Significant
X1 0.028 1 0.028 15.82 0.0073
X2 0.19 1 0.19 107.16 <0.0001
Y2 Particle Size [R2= 0.8392]
Model [Linear]
89132.70 2 44566.35 15.66 0.0042 Significant
X1 413.34 1 413.34 0.15 0.7163
X2 88719.36 1 88719.36 31.17 0.0014
Y3In-vitro Drug Diffusion [R2= 0.8739]
Model [Linear]
69.95 2 34.97 20.80 0.0020 Significant
X1 3.08 1 3.08 1.83 0.2246
X2 66.87 1 66.87 39.77 0.0007
df - degrees of freedom, p < 0.05 are statistically significant.
Table 6. Final equation in terms of coded factors
Coded factor equation R2
Value
Y1 = 0.56002 + 0.068617 X1 + 0.17857 X2 0.9535
Y2 = 293.80 – 8.30 X1 – 121.60 X2 0.8392
Y3=92.13 + 0.72 X1 + 3.34 X2 0.8739
Table 7. Comparison of FTIR Peak of Ezogabine and Physical Mixture
Observed peaks in drug (cm-1)
Observed peaks in mixture (cm-1)
Reported peaks (cm-1)
Functional Group Interaction
3419.79 3420.52 3475-3150 -NH2 No Interaction
3375.43 3380.44 3475-3150 -NH No Interaction
3150 3155 3150-3050 -C-H No Interaction
1710 1709.12 1725-1705 -C=O No Interaction
1479.40 1480.26 1475 -C=C- No Interaction
1305.81 1300.28 1300-1000 R-O-R No Interaction
805 800 850-800 -C-X No Interaction
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
Fig.1. (a) Contour surface plot of saturation solubility (b) Three-dimensional response surface plots of saturation
Fig.2. (a) Contour surface plot of particle size (b) Three-dimensional response surface plots of particle size
Fig.3. (a) Contour surface plot of in-vitro diffusion (b) Three-dimensional response surface plots of in-vitro
diffusion
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
A
B
Fig.4. FT-IR spectra of A- Ezogabine, B-Physical Mixture
Pawar et al _____________________________________________________ ISSN-2347-5447
BBB[4][1][2016] 015-026
A
B
C
Fig.5. Histological photomicrograph of eosin-hematoxylin stained goat nasal mucosa treated with A- phosphate buffer pH-6.4(Negative control), B- Isopropyl
Alcohol (Positive control), C- Ezogabine Nanosuspension formulation