Johnson S P P P T
-
Upload
eifelr -
Category
Health & Medicine
-
view
740 -
download
2
Transcript of Johnson S P P P T

Treatment of
hypertriglyceridemia:
Lovaza vs. Nicotinic acid
Melissa Johnson, PA-S
Shenandoah University PA Studies
December 10, 2008

Introduction1,2
Hypertriglyceridemia has a large impact on
healthcare today.
Hypertriglyceridemia is a major cause of
atherosclerosis which is a risk factor for
CAD, CVA, PVD, acute pancreatitis and is a
factor in metabolic syndrome.
Hypertriglyceridemia is exacerbated by
uncontrolled DM, obesity, tobacco
smoking, high fat diets and sedentary
lifestyle.

Impact on healthcare3-7
Hypertriglyceridemia accounts for 1-4% of hospitalized acute pancreatitis cases per year.
Prevalence of metabolic syndrome is 22% in US.
Heart disease is the 1st leading cause of death and CVA’s are the 3rd in US today accounting for more than 35% of deaths in the US.
The economic impact on US healthcare is estimated to be $448 billion dollars for the year 2008.

Background1,4,8,9
Two classification systems for
hypertriglyceridemia: Fredrickson and clinical.
Fredrickson is not used as much, but will still
be found in literature today.
Both classifications help to clarify the many
terms used today to describe derangements
in the lipid panel.

Background
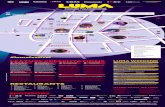
Hyperlipoproteinemia according to Fredrickson classificationa
Fredrickson
classification
Clinical
classification
terminology
Subset of clinical
classificationEtiology Laboratory findings
Type I
Triglyceride
dominant lipid
disorder
Familial
hyperchylomicronemiaDecreased LPL
Elevated chylomicrons
and
triglycerides
Type IIaLDL-dominant
lipid disorderFamilial hypercholesterolemia LDL receptor deficiency Elevated LDL only
Type IIbMixed lipid
disorder
Familial combined
hyperlipidemia
Decreased LDL receptor and
increased ApoB protein
Elevated LDL, VLDL, and
triglycerides
Type IIILDL-dominant
lipid disorder
Familial
dysbetalipoproteinemia
Defect in ApoE protein
synthesisIncreased IDL and LDL
Type IV
Triglyceride
dominant lipid
disorder
Endogenous hyperlipemia and
atherogenic dyslipidemia
Increased VLDL production
and decreased elimination
Increased VLDL and
Triglycerides and low
HDL
Type V
Triglyceride
dominant
disorder
Familial and severe
hypertriglyceridemia
Increased VLDL
production and decreased
LPL
Increased VLDL,
chylomicrons, and
triglycerides
aYuan, Al-Shali, Hegele and Eaton

Background6-14
Diagnosis:
Triglycerides:
<150: normal
150-199: borderline high
200-499: high
>/= 500: SEVERE
Clinical presentation:
Most often asymptomatic
Can present with acute
pancreatitis, eruptive
cutaneous xanthomas,
lipemia retinalis

Current First Line Therapy4-8,16
Current first line therapy recommended by
the NCEP-ATPIII guidelines are the use of
fibrates and nicotinic acid for the treatment of
elevated triglycerides.
Clinicians must also ensure that goal LDL has
been reached first in patients with elevated
triglycerides.

Purpose
To evaluate the treatment of severe
hypertriglyceridemia (triglycerides >/= 500mg/dl)
with Lovaza vs. Nicotinic Acid.
To evaluate which medication as a
monotherapy is more effective and with less
side effects for all patients including those
with comorbidities.

Literature Review/Methods
Databases available through Shenandoah University Library searched included: Cochran, PUBMED, and Medline.
Inclusion Criteria: Clinical overviews, RCT, open label trials, systemic
reviews and prospective studies.
Studies must have utilized Lovaza or Nicotinic Acid and include measurements of triglycerides.
Exclusion Criteria: Lipid derangements not including elevated
triglycerides.
Studies before 1997.
Studies using Lovaza or Nicotinic acid to treat elevated triglycerides induced by medications.

Study 1 Harris WS, et al. (1997). Safety and efficacy of omacor in
severe hypertriglyceridemia. Journal of Cardiovascular
Risk.1997;4(5/6), 385-391.
■ Objective: Evaluate the efficacy and safety of Omacor (now known as Lovaza) in patients with severe hypertriglyceridemia.
Methods: Randomized, double-blind, prospective, parallel-group study comparing Omacor to placebo in 42 patients with triglycerides between 500-2000mg/dl. Patients received 4g of Omacor once daily or placebo for four months.
Results: mean baseline triglycerides: 919mg/dl +/-381. Mean end triglycerides: 505mg/dl +/- 304.
Side effects: 7 patients reported GI problem: 3 of which were in placebo group. Most common was burping a fishy taste.

Study 2 Capuzzi DM, et al. Efficacy and safety of an extended-
release Niacin (Niaspan): a long term study. The American Journal
of Cardiology. 1998; 82(12A), 74U-81U
Objective: Evaluate long term safety and efficacy of Niaspan once nightly in patients with primary hypercholesterolemia. Secondary goal to evaluate effects on triglycerides.
Methods: Open-label extension trial evaluating Niacin doses of 1000-3000mg nightly. 723 patients at 27 sites were followed for 24 months.
Results: Triglycerides were lowered by 28% after 96 weeks of therapy.
Side effects: flushing, HA, abdominal pain, diarrhea, dyspepsia, N/V, rhinitis, pruritus and rash.
75 patients did experience serious & unexpected AE’s warranting hospitalization. 3 considered directly related to Niaspan, 64 were
considered not related and 8 were considered remotely related to Niaspan.

Results
Summary of results
Study 1a Study 2b
Sample size 42 723
Date of publication 1997 1998
Study design RCT-prospective Open label extension
Intervention 4g Omacor daily 1-3g Niaspan daily
Outcome Triglyceride level
1 LDL, apo B
2 triglycerides, total cholesterol,
HDL, lipoprotein (a)
Results Triglycerides down by 45% Triglycerides down by 28%
Conclusion Omacor reduces triglycerides Niaspan reduces triglycerides
Level of evidence 1b 1c
aHarris, Ginsberg, Arunakul, Shachter, Windsor, Adams, Berglund, OsmundsenbCapuzzi, Gyton, Morgan, Goldberg, Kreisberg, Brusco, Brody

Discussion
Study #1: Level of evidence 1b
Prospective randomized controlled study
Patients treated with Lovaza 4g or placebo
Study #2: Level of evidence 1c
Open label extension trial
All patients treated with Niaspan 1-3g
No placebo group

Strengths and limitations
Strengths:
Beneficial for primary care providers looking for an
appropriate, safe, and effective treatment for patients
with severe hypertriglyceridemia.
Limitations:
Limited to patients with triglyceride levels between 500-
2000mg/dl or at elevated triglycerides as a secondary
goal.
Limited by English language, available databases and
head to head study between Lovaza and Niaspan.

Conclusion
Lovaza yields higher results at lowering
triglycerides than Niaspan.
Lovaza has fewer side effects and adverse
events than Niaspan.
Lovaza is better tolerated than Niaspan.

Acknowledgements
Raymond Eifel, MS, PA-C
Advisor for scholarly project
Associate Professor Shenandoah University
Physician Assistant Studies

References
1. Pejic R, Lee DT. Hypertriglyceridemia. Journal of the American board of family medicine. 2006:19(3):310-316.
2. Citkowitz E. Hypertriglyceridemia. Emedince: The medscape Journal [serial online]. July 12, 2008. www.emedicine.com/med/TOPIC2921.HTM. Accessed June 23, 2008.
3. Ferrannini E. Metabolic syndrome: a solution in search of a problem. Journal of Endocrinology Metabolism. 2007;92:39-401.
4. Yuan G, Al-Shali K, Hegele R. Hypertriglyceridemia: its etiology, effects and treatment. Canadian Medical Association Journal. 2007;176:1113-1120.
5. National Health and Nutrition Examination Survey [webpage]. Center for disease control website. http://www.cdc.gov/nchs/nhanes.htm. Accessed July 10, 2008.
6. Grundy M, Becker D, Clark L, Cooper R, et al. National Cholesterol Education Program Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults (adult treatment panel III). NIH publication No. 02-5215. September 2002.
7. Grundy SM, Cleeman JI, Merz NB, et al. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. 2004. National Heart, Lung and Blood Institute: NIH. http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3upd04.htm. Assessed March 23, 2008
8. Eaton C. Hyperlipidemia. Primary care: clinics in office practice. 2005;32(4):1027-1055.

References Cont’
9. Rosenson R. Lipoprotein classification; metabolism; and role in atherosclerosis. UpToDate [database online]. Last updated January 31, 2008. www.uptodate.com/online/content/topic.do?topicKey=lipidis/7908&view=print. Assessed May 5, 2008.
10. Myers GL, Cooper GR, Greenberg N, Kimberly MM, Waymack PP, Hassemer DJ. Standardization of lipid and lipoprotein measurements. Handbook of lipoprotein testing. 2nd ed. Washington DC: AACC Press; 2000:717-748.
11. Caslake MJ, Packard C. The use of ultracentrifugation for the separation of lipoproteins. Handbook of lipoprotein testing. 2nd ed. Washington DC: AACC Press; 2000:625-646.
12. Kulkarni KR. Cholesterol profile measurement by vertical auto profile method. Clinics in Laboratory medicine. 2006;26(4):787-802.
13. Otvos, J. Measurement of lipoprotein subclass profiles by nuclear magnetic resonance spectroscopy. Handbook of lipoprotein testing. 2nd ed. Washington DC: AACC Press; 2000:609-624.
14. Schmitz G, Bottcher A, Barlage S, Lackner KJ. New approaches to the use of lipoprotein electrophoresis in the clinical laboratory. Handbook of lipoprotein testing. 2nd ed. Washington DC: AACC Press; 2000:593-608.
15. Hachem SB, Mooradian AD. Familial dyslipidaemias an overview of genetics, pathophysiology and management. Drugs. 2006;66(15):1949-1969
16. Garg A, Simha V. Update on dyslipidemia. Journal of clinical endocrinology and metabolism.2007;92(5):1581-1589.
17. Harris WS, et al. Safety and efficacy of Omacor in severe hypertriglyceridemia. Journal of Cardiovascular Risk. 1997;4(5/6):385-391.
18. Capuzzi DM, et al. Efficacy and safety of extended-release Niacin (Niaspan): a long term study. The American Journal of Cardiology. 1998;82(12A):74U-81U.